Professional Documents
Culture Documents
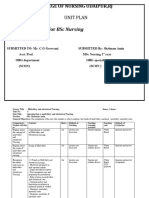
(Pob) Vaginal Delivery
(Pob) Vaginal Delivery
Uploaded by
Cherie thompsonCopyright:
Available Formats
You might also like
- Postpartum Report SheetDocument1 pagePostpartum Report SheetHeather McCormick100% (8)
- DR Write UpDocument15 pagesDR Write Upjansestacio100% (3)
- Chapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationDocument9 pagesChapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationAlyssaGrandeMontimor100% (1)
- Lesson 1.1 Maternal Anatomy Dr. Jane PublicoDocument11 pagesLesson 1.1 Maternal Anatomy Dr. Jane PublicoKristel Saturn SalvadNo ratings yet
- Airway ManagementDocument48 pagesAirway ManagementRea Dominique CabanillaNo ratings yet
- Osce - D&CDocument2 pagesOsce - D&Cmkct111No ratings yet
- ESL Progress Report COMMENT BANKDocument9 pagesESL Progress Report COMMENT BANKCherie thompson100% (2)
- Partograph: Jillian A. Bejoc, MSN, RNDocument44 pagesPartograph: Jillian A. Bejoc, MSN, RNJiezl Abellano AfinidadNo ratings yet
- ANA.S4.CA21.Female Reproductive SystempdfDocument6 pagesANA.S4.CA21.Female Reproductive SystempdfCazz HeyNo ratings yet
- PPT Book ReadingDocument20 pagesPPT Book ReadingOctaria SaputraNo ratings yet
- NCM109 Maternal - Child Nursing (A-C) - Module 5Document6 pagesNCM109 Maternal - Child Nursing (A-C) - Module 5iratsyukieNo ratings yet
- HEALTH ASSESSMENT - Breasts & Regional LymphaticsDocument5 pagesHEALTH ASSESSMENT - Breasts & Regional LymphaticsMich Hiel OforraNo ratings yet
- Operative Vaginal DeliveryDocument8 pagesOperative Vaginal DeliveryGerben VillanuevaNo ratings yet
- 05.3 Problems of The Power and Psyche PDFDocument12 pages05.3 Problems of The Power and Psyche PDFJAN CAMILLE LENONNo ratings yet
- Mechanisms of LaborDocument4 pagesMechanisms of LaborIrish Paulene NiroNo ratings yet
- Obstetrics and GynecologyDocument44 pagesObstetrics and Gynecologyjaisanatandharma7No ratings yet
- Destructive Operations. PDFDocument63 pagesDestructive Operations. PDFFeba SajanNo ratings yet
- 04 Third Trimester ConditionsDocument11 pages04 Third Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- Rle DR Rot 2ND SemDocument2 pagesRle DR Rot 2ND SemRae LebrilloNo ratings yet
- AC MS Post-Operative FINALDocument8 pagesAC MS Post-Operative FINALCiaraNo ratings yet
- NCM107 Leopolds ManeuverDocument4 pagesNCM107 Leopolds Maneuverchloepaxton030No ratings yet
- 1.03 General Survey, Skin and Anthropometric AssessmentDocument14 pages1.03 General Survey, Skin and Anthropometric AssessmentKim DeeNo ratings yet
- CCE1 AirwayDocument8 pagesCCE1 AirwayHoward ChangNo ratings yet
- Normal Labor: Kevin Marcial I. Aralar, MD 1 Year ResidentDocument46 pagesNormal Labor: Kevin Marcial I. Aralar, MD 1 Year ResidentKevin AralarNo ratings yet
- PGI MANIMTIM - Vaginal Delivery, Breech Delivery and Operative Vaginal DeliveryDocument8 pagesPGI MANIMTIM - Vaginal Delivery, Breech Delivery and Operative Vaginal DeliveryKim Adarem Joy ManimtimNo ratings yet
- Obstetric & Gynecology Health Care Center by SlidesgoDocument64 pagesObstetric & Gynecology Health Care Center by SlidesgoShane mNo ratings yet
- Normal LabourDocument88 pagesNormal LabourDebayan KhanNo ratings yet
- Manual Removal of PlacentaDocument25 pagesManual Removal of PlacentaLoorthu Selvi M0% (1)
- Pedia Gi-GuDocument16 pagesPedia Gi-GuZhantelle A. Santos100% (1)
- nots shoulder dystociaDocument4 pagesnots shoulder dystociamelly novNo ratings yet
- Obstetric Emergencies 28072020Document84 pagesObstetric Emergencies 28072020Arief NorddinNo ratings yet
- Abnormal LaborDocument26 pagesAbnormal LaborShane mNo ratings yet
- 85297.1606818947gyne SampleDocument10 pages85297.1606818947gyne SampleRithikaNo ratings yet
- Toag 2000 2 4 53Document1 pageToag 2000 2 4 53Sharmela BrijmohanNo ratings yet
- S3-06 Ophthalmology Eyelid, Lacrimal - Orbital Disorders (v2) PDFDocument13 pagesS3-06 Ophthalmology Eyelid, Lacrimal - Orbital Disorders (v2) PDFAl SyNo ratings yet
- Shoulder Dystocia RetdemDocument2 pagesShoulder Dystocia RetdemDarwin QuirimitNo ratings yet
- Augmentation of LabourDocument45 pagesAugmentation of LabourLamnunnem HaokipNo ratings yet
- P4P REPRO 2.0Document54 pagesP4P REPRO 2.0william atmadjiNo ratings yet
- Delivery of Baby (Actual, Assist, and Cord Care)Document3 pagesDelivery of Baby (Actual, Assist, and Cord Care)Jasmin AdoraNo ratings yet
- Week 11 - Assessment of Breast and Lymphatic SystemDocument5 pagesWeek 11 - Assessment of Breast and Lymphatic SystemJuan Miguel TevesNo ratings yet
- Unit 5 Newborn ConceptsDocument5 pagesUnit 5 Newborn ConceptsEunice TrinidadNo ratings yet
- (OBS) 2.01 Physiology of Labor, Normal Labor, and Delivery - Junio (Final V.02 - Sep 26)Document18 pages(OBS) 2.01 Physiology of Labor, Normal Labor, and Delivery - Junio (Final V.02 - Sep 26)Sam MataNo ratings yet
- His.s4.Sr MergedpdfDocument190 pagesHis.s4.Sr Mergedpdfsky vallartaNo ratings yet
- Shoulder Dystocia Guideline 280720Document10 pagesShoulder Dystocia Guideline 280720Ahmed SamyNo ratings yet
- NSD ChecklistDocument3 pagesNSD ChecklistChristine Evan HoNo ratings yet
- 19 - Vaginal DeliveryDocument16 pages19 - Vaginal DeliveryGen XNo ratings yet
- Operative DeliveriesDocument58 pagesOperative DeliveriesDanduuNo ratings yet
- 2nd Year All Clinicals AIMC AcademiaDocument64 pages2nd Year All Clinicals AIMC Academiasaleempanwar96No ratings yet
- Assesment and Monitoring During 2nd Stage of LabourDocument11 pagesAssesment and Monitoring During 2nd Stage of LabourPragati BholeNo ratings yet
- Postpartal ComplicationDocument4 pagesPostpartal ComplicationHanna AligatoNo ratings yet
- 3 Priority Nursing Care Plans During DeliveryDocument11 pages3 Priority Nursing Care Plans During DeliveryRyan Robert V. VentoleroNo ratings yet
- 07 - LEC Care of The NewbornDocument17 pages07 - LEC Care of The NewbornJAN CAMILLE LENONNo ratings yet
- Perioperative NursingDocument9 pagesPerioperative NursingHannah PatriciaNo ratings yet
- Nursing Care of A Family Experiencing A Complication of Labor or BirthDocument25 pagesNursing Care of A Family Experiencing A Complication of Labor or BirthZhantelle A. SantosNo ratings yet
- MaternalDocument2 pagesMaternalqweyo yhuNo ratings yet
- NCM - 207 RLE (Delivery Room Nursing)Document9 pagesNCM - 207 RLE (Delivery Room Nursing)Tintin HonraNo ratings yet
- 5.9.5 Shoulder Dystocia M: AnagementDocument8 pages5.9.5 Shoulder Dystocia M: AnagementTriponiaNo ratings yet
- Perineal Trauma & Epsiotomy: Pembimbing: Dr. Arief Budiono, SP - OGDocument42 pagesPerineal Trauma & Epsiotomy: Pembimbing: Dr. Arief Budiono, SP - OGHans Natanael PosoNo ratings yet
- Narrow Pelvis. Anomalies of Position and Fetal Presentation. Pregnancy and Childbirth During Pelvic Presentation.Document18 pagesNarrow Pelvis. Anomalies of Position and Fetal Presentation. Pregnancy and Childbirth During Pelvic Presentation.mudeyNo ratings yet
- Persalinan, Episiotomi, Dan Nifas: Vaulinne BasyirDocument33 pagesPersalinan, Episiotomi, Dan Nifas: Vaulinne BasyirKhairunnisa KhairunnisaNo ratings yet
- Case Presentation On Normal LaborDocument62 pagesCase Presentation On Normal LaborB34-YvesJethro ReyesNo ratings yet
- LEOPOLDS MANEUVER ReviewerDocument3 pagesLEOPOLDS MANEUVER ReviewerLloyd BaylonNo ratings yet
- 10 Post Partum 1Document3 pages10 Post Partum 1Gwen CastroNo ratings yet
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesRating: 5 out of 5 stars5/5 (2)
- Hello! Nice To See You Again!Document14 pagesHello! Nice To See You Again!Cherie thompsonNo ratings yet
- Microbiology - 2nd LE 2018Document9 pagesMicrobiology - 2nd LE 2018Cherie thompsonNo ratings yet
- FF - Get Ready211Document12 pagesFF - Get Ready211Cherie thompsonNo ratings yet
- FF - Market Talk1032Document7 pagesFF - Market Talk1032Cherie thompsonNo ratings yet
- Parasitology - Lab Pracs MidtermDocument54 pagesParasitology - Lab Pracs MidtermCherie thompsonNo ratings yet
- FF - Cyle A001Document8 pagesFF - Cyle A001Cherie thompsonNo ratings yet
- L Esson31 The Bird's NestDocument11 pagesL Esson31 The Bird's NestCherie thompsonNo ratings yet
- FF LightningA07Document13 pagesFF LightningA07Cherie thompsonNo ratings yet
- FF - KB214 - Unit 6 - Lesson 2Document13 pagesFF - KB214 - Unit 6 - Lesson 2Cherie thompsonNo ratings yet
- Homework From The Last LessonDocument12 pagesHomework From The Last LessonCherie thompsonNo ratings yet
- Homework From The Last LessonDocument13 pagesHomework From The Last LessonCherie thompsonNo ratings yet
- Homework From The Last LessonDocument14 pagesHomework From The Last LessonCherie thompsonNo ratings yet
- FF LightningB06Document14 pagesFF LightningB06Cherie thompsonNo ratings yet
- Monthly Test Evaluation: Criteria Score (10) Strengths Weaknesses RecommendationDocument1 pageMonthly Test Evaluation: Criteria Score (10) Strengths Weaknesses RecommendationCherie thompsonNo ratings yet
- Renzel Franz B. DanaoDocument2 pagesRenzel Franz B. DanaoCherie thompsonNo ratings yet
- PCEID Report FormatsDocument2 pagesPCEID Report FormatsCherie thompsonNo ratings yet
- High School Grade 1A: Travel JournalDocument17 pagesHigh School Grade 1A: Travel JournalCherie thompsonNo ratings yet
- Nircmd Mic Locker Setup Without Using Task SchedulerDocument2 pagesNircmd Mic Locker Setup Without Using Task SchedulerCherie thompsonNo ratings yet
- Avelino E. Sadiao: Special Program For The Employment of Students June-July 2018 Benguet Provincial CapitolDocument2 pagesAvelino E. Sadiao: Special Program For The Employment of Students June-July 2018 Benguet Provincial CapitolCherie thompsonNo ratings yet
- National Health Situation of The Philippines For CHNDocument5 pagesNational Health Situation of The Philippines For CHNanreilegarde100% (1)
- Inducing Labour: Clinical Guideline Published: 23 July 2008Document35 pagesInducing Labour: Clinical Guideline Published: 23 July 2008dNo ratings yet
- Pregnancy & ChildbirthDocument12 pagesPregnancy & Childbirthrobert tambuliNo ratings yet
- Cheska Maternal AssignmentDocument3 pagesCheska Maternal AssignmentJoule PeirreNo ratings yet
- Proximity of Magnesium Exposure To Delivery and Neonatal Outcomes 2016 American Journal of Obstetrics and GynecologyDocument6 pagesProximity of Magnesium Exposure To Delivery and Neonatal Outcomes 2016 American Journal of Obstetrics and GynecologyFarin MauliaNo ratings yet
- Revision Long Case Obs Gynae PDF FreeDocument10 pagesRevision Long Case Obs Gynae PDF Freesirajulislam6017No ratings yet
- Microbiology: Submitted by Sherwin N. Genova Submitted To Ms. Reah FojasDocument9 pagesMicrobiology: Submitted by Sherwin N. Genova Submitted To Ms. Reah FojasSherwin Nicolas GenovaNo ratings yet
- 15 Physio OB - Normal LaborDocument8 pages15 Physio OB - Normal LabormaqmmNo ratings yet
- Resume Update 12 2019Document2 pagesResume Update 12 2019api-354751775No ratings yet
- Emergencies ObsDocument7 pagesEmergencies ObsAshish GuptaNo ratings yet
- Postnatal Care: Samson Udho MSC, BSCDocument34 pagesPostnatal Care: Samson Udho MSC, BSCAYO NELSON0% (1)
- Bahasa Inggris NURHALIMAH-1Document3 pagesBahasa Inggris NURHALIMAH-1NurhalimahNo ratings yet
- Ashrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarDocument4 pagesAshrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarWilliam AdiputraNo ratings yet
- Emonc ProtocolDocument38 pagesEmonc ProtocolXerxes MalagaNo ratings yet
- 2M Intrapartal Complications Written Report 109Document72 pages2M Intrapartal Complications Written Report 109kai xoxoNo ratings yet
- MK Polyhydramnios and Oligohydramnios (OBGY)Document14 pagesMK Polyhydramnios and Oligohydramnios (OBGY)Moses Jr KazevuNo ratings yet
- Enhancing Childbirth Satisfaction Through A Brief, Targeted Educational InterventionDocument25 pagesEnhancing Childbirth Satisfaction Through A Brief, Targeted Educational InterventionekinooristiqomahNo ratings yet
- Ernawati - PIT Feto 2023 PreeklampsiaDocument21 pagesErnawati - PIT Feto 2023 PreeklampsiaHeldasari SianturiNo ratings yet
- A Thesis ProtocolDocument3 pagesA Thesis ProtocolOmar TousifNo ratings yet
- Abnormal LabourDocument15 pagesAbnormal LabourAshish GuptaNo ratings yet
- Pengaruh Body Massage Terhadap Tingkat Depresi Ibu Nifas Di Bidan Praktik Mandiri Siyamtiningsih KaranganyarDocument8 pagesPengaruh Body Massage Terhadap Tingkat Depresi Ibu Nifas Di Bidan Praktik Mandiri Siyamtiningsih KaranganyarEnzel LinaNo ratings yet
- Asuhan Kebidanan Komprehensif Pada Ny I Umur 35 TaDocument6 pagesAsuhan Kebidanan Komprehensif Pada Ny I Umur 35 TaWienta dsNo ratings yet
- Jurnal PERKEMBANGAN PENDIDIKAN KEBIDANAnDocument7 pagesJurnal PERKEMBANGAN PENDIDIKAN KEBIDANAnSurti PartiningsihNo ratings yet
- Jurnal Rupture Perineum 3Document6 pagesJurnal Rupture Perineum 3Muh AqwilNo ratings yet
- CPD Concept MapDocument1 pageCPD Concept MapShandle Dynne Baena100% (1)
- Kpsea Online RegslipDocument14 pagesKpsea Online RegslipNeldia CyberNo ratings yet
- Unit Plan Obg 1Document24 pagesUnit Plan Obg 1Daily DoseNo ratings yet
(Pob) Vaginal Delivery
(Pob) Vaginal Delivery
Uploaded by
Cherie thompsonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(Pob) Vaginal Delivery
(Pob) Vaginal Delivery
Uploaded by
Cherie thompsonCopyright:
Available Formats
VAGINAL DELIVERY
Dr. Roselyn Collado-Garcia – December 01, 2021
OUTLINE ● Describe the maneuvers employed in the
I. MANAGEMENT OF SECOND STAGE LABOR management of shoulder dystocia
A. LITHOTOMY POSITION ● Outline the management of the 3rd stage of labor
B. OCCIPUT ANTERIOR POSITION ● Differentiate the degrees of perineal laceration
1. MODIFIED RITGEN MANEUVER ● Differentiate the median from mediolateral episiotomy
2. DELIVERY OF THE SHOULDERS
3. CLAMPING OF THE CORD
C. PERSISTENT OCCIPUT POSTERIOR
MANAGEMENT OF SECOND STAGE OF LABOR
1. MANAGEMENT ● When caring for a mother at the labor room in
D. PERSISTENT OCCIPUT TRANSVERSE monitoring the contractions, its interval and cervical
E. SHOULDER DYSTOCIA dilatation, effacement and maximal descending part,
1. TURTLE SIGN all this constitutes the 2nd stage of Labor
2. MANAGEMENT ● Primiparous
● SUPRAPUBIC PRESSURE
○ Full cervical dilatation may be monitored in
● McROBERTS MANEUVER
the labor room
● DELIVERY OF THE POSTERIOR
SHOULDER ○ Maternal expulsive efforts may help bring
● WOOD’S CORKSCREW down the present part further down the birth
● RUBIN MANEUVER canal
● GASKIN MANEUVER ● Multiparous
● POSTERIOR AXILLA SLING ○ Better monitored on the delivery table,
TRACTION equipped with stirrups
● DELIBERATE FRACTURE OF
● Expulsive efforts - distend the perineum
ANTERIOR CLAVICLE
● HIBBARD MANEUVER
● Prepare the woman for delivery
● ZAVANELLI MANEUVER ○ Dorsal lithotomy
● SYMPHYSIOTOMY ○ Proper positioning at the delivery table
● CLEIDOTOMY ○ Perineal Prep
II. MANAGEMENT OF THIRD STAGE LABOR ○ Observe aseptic technique
A. EXPECTANT OF PHYSIOLOGICAL ● The end of second-stage labor is heralded as:
B. ACTIVE MANAGEMENT (AMTSL)
○ The perineum begins to distend
1. STEPS OF AMTSL
○ Overlying skin becomes stretched,
2. MEDICATIONS
C. MANUAL REMOVAL ○ Fetal scalp is seen through the separating
III. FOURTH STAGE OF LABOR labia.
A. BIRTH CANAL LACERATIONS ● Increased perineal pressure from the fetal head
1. FIRST DEGREE creates reflexive bearing-down efforts, which are
2. SECOND DEGREE encouraged when appropriate.
3. THIRD DEGREE ● At this time, preparations are made for delivery.
4. FOURTH DEGREE
● If the bladder is distended, catheterization may be
B. EPISIOTOMY
necessary
References: ● Continued attention is also given to fetal heart rate
William’s Obstetrics, 25th Edition monitoring.
Dr. Garcia’s Lecture ● As one example, a nuchal cord often tightens with
Notes descent and may lead to deepening variable
decelerations
OBJECTIVES
At the end of the session, a second year medical student must LITHOTOMY POSITION
be able to:
● Discuss the management of 2nd stage of labor and
the mechanics of vaginal delivery in variety of fetal
position
○ Occiput Anterior
○ Occiput Posterior
○ Occiput Transverse
USE AT YOUR OWN RISK page 1 of 12
VAGINAL DELIVERY
● Dorsal lithotomy position is most common and often ■ Mediolateral episiotomy
the most satisfactory ○ Routine episiotomy is no longer
● For better exposure, leg holders or stirrups are used recommended, and selective use aims to
● The delivery bed is enough to accommodate the body enlarge the vaginal opening for specific
of the mother indications
● The popliteal fossa rests on the curvature of the ● To limit vaginal lacerations - perineal massage
stirrups ○ With the perineal massage, you would know
○ Within the leg holder, the popliteal region that the support is placed there
should rest comfortably in the proximal ○ Aside from perineal massage, you may also
portion and the heel in the distal portion use perineal support
● The stirrups are padded so the legs of the mother are ● RITGEN MANEUVER
comfortable ○ As the head distends the vulva and
○ The legs are not strapped into the stirrups, perineum, perineal support allows fetal head
thereby allowing quick flexion of the thighs delivery
backward onto the abdomen should shoulder
dystocia develop
○ Legs may cramp during second-stage
pushing, and cramping is relieved by
repositioning the affected leg or by brief
massage
● The distance between the thighs must be comfortable
enough not to strain the legs
○ If too much distance or the legs are wider
apart, this may cause temporary paralysis of ● Following the WHO Practice Guideline, they would
the lower extremities only advocate perineal support
● Properly drape the upper body of the mother ○ But it is quite difficult, because in the real
● The buttocks should be flat on the delivery table world, you would rather suture or care of a
● Make sure the perineal area is aseptic and properly wound that is cleanly cut
draped
○ Scrubbing, gowning, gloving, and donning
protective mask and eyewear protect both
MODIFIED RITGEN MANEUVER
the laboring woman and accoucheur from
infectious agents
OCCIPUT ANTERIOR POSITION
● Most common form of rotation
● Delivery of the head
○ Encirclement of the largest diameter by the
vulvar ring (crowning)
○ Perineum thins
■ When the mother bears down, it
propels the head downwards,
pushing and stretching the perineal
body then thinning it out
■ May spontaneously lacerate
○ Anus becomes greatly stretched and ● Alternatively done if expulsive efforts are inadequate
distended or expeditious delivery is needed
■ Anterior wall of the rectum is seen ● As the head emerges down the perineum or pelvic
● ~90% of cases, the fetal head would present at floor and through the birth canal, you can hook the
occiput anterior position (triangular occipital chin, the head is pushed even forward, you assume
fontanelle) - vertex or occiput presentation exaggerated extension of the head
○ Anterior towards the symphysis pubis ● Image: Moderate upward pressure is applied to the
○ The head descends in full flexion fetal chin by the posterior hand covered by a sterile
● Episiotomy may be employed towel. The other hand applies occipital pressure.
○ Incision = episiotomy ● Now, you favor neck extension
■ Median episiotomy
USE AT YOUR OWN RISK page 2 of 12
VAGINAL DELIVERY
MANAGEMENT OF NORMAL LABOR AND DELIVERY ● The sides of the head are grasped with two hands,
● Sequence of fetal head movement upon delivery and gentle downward traction is applied until the
○ Emerging anterior shoulder appears under the pubic arch.
■ Flexion ● Next, by an upward movement, the posterior shoulder
■ Extension is delivered. During delivery, abrupt or powerful force
■ Rotation to the side is avoided to avert fetal brachial plexus injury.
DELIVERY OF THE SHOULDERS CLAMPING OF THE CORD
● As the head goes into extension, it rotates ● The umbilical cord is cut between two clamps placed
○ The most common rotation, as it enters the 6 to 8 cm from the fetal abdomen and later an
birth canal or pelvic inlet in >90% of cases, is umbilical cord clamp is applied 2 to 3 cm from its
the left occiput transverse rotation insertion into the fetal abdomen
● Following delivery of the fetal head, a finger is passed ● Umbilical cord cut in between clamps
across the fetal neck to determine whether it is ○ 2 to 3 cms plastic clamp from fetal
encircled by one or more umbilical cord loops. abdomen
● If an umbilical cord coil is felt, it is slipped over the ● Delayed cord clamping ( 60 seconds ) benefits:
head if loose enough. If applied too tightly, the loop is ○ Increase total body iron stores
cut between two clamps. ○ Expand blood volume
● External rotation allows head to assume transverse ○ Decrease neonatal anemia
position ● Downside: Increase bilirubin, causing
● Sh- Sh occupies the AP diameter hyperbilirubinemia
● Check for cord loops ( found in 25% of cases) ● For the preterm neonates, delayed cord clamping has
● Observe for the rest of the cardinal movements to several benefits:
proceed ○ Higher red cell volume
● Assist delivery of the rest of the body ○ Decreased need for blood transfusion
● Over traction may cause injury ○ Lower rates of intraventricular hemorrhage
● Suctioning of nasopharynx - was the previous practice and of necrotizing enterocolitis
○ Previously, immediate nasopharyngeal bulb ● “Milking” the cord - benefits the baby if rapid cord
suctioning of the newborn was routine to clamping is to be done
remove secretions. It was found that ○ If baby is asphyxiated,has non-reassuring
suctioning of the nasopharynx may lead to fetal heart rate pattern or fetal distress what
neonatal bradycardia. you can do is milk the cord towards the fetus
● Observe EINC ( Essential Intrapartum Newborn Care) ● Preterm neonates: delayed clamping benefits:
● Should assume the AP diameter ○ High red cell volume
○ Decrease need for transfusion
○ Better circulatory stability
○ Lower rate for UVH/Necrotizing Enterocolitis
PERSISTENT OCCIPUT POSTERIOR
● As it subtends the birth canal, it undergoes rotation to
occiput posterior
● Occurs in 2-10% of singleton term
● Predisposing factors:
● Following its delivery, the fetal head falls posteriorly, ○ Epidural analgesia
bringing the face almost into contact with the maternal ■ During labor, when there is strong
anus. The occiput promptly turns toward one of the contraction, it arrests the baby’s
maternal thighs, and the head assumes a transverse rotation in occiput posterior
position. ○ Nulliparity
● This external rotation indicates that the bisacromial ■ Tout abdomen
diameter, which is the distance between the ○ Big baby
shoulders, has rotated into the anteroposterior ■ No room for rotation
diameter of the pelvis. ○ Prior OP delivery
● Most often, the shoulders appear at the vulva just ○ Anthropoid pelvis
after external rotation and are born spontaneously. If ○ Narrow subpubic angle
delayed, extraction aids controlled delivery.
USE AT YOUR OWN RISK page 3 of 12
VAGINAL DELIVERY
● Complications: ○ fetal macrosomia + maternal diabetes= ↑
○ Higher rates for prolonged second stage of frequency of shoulder dystocia
labor ● Greater risk to the fetus than the mother
○ Cesarean deliveries ○ significant neonatal neuromuscular injury
○ Operative vaginal delivery and asphyxia
○ Increased rate for higher-order vaginal ○ brachial plexus injury (11%)
lacerations ○ Clavicular & humeral fracture (2%)
○ Acidosis at delivery (7%)
MANAGEMENT ○ Required cardiac resuscitation or developed
● Manual rotation to OA hypoxic ischemic encephalopathy (1.5%)
○ Do an internal examination, grasp and rotate ○ Severe fetal acidosis & HIE (0.5% if delivery
it 180 degrees. completed w/in 5 mins)
○ Lower rates of cesarean ■ case rate increase 6 and 24 % w/
○ Lower incidence of vaginal laceration delivery delays > 5 minutes
■ Because the occipito bregmatic ● Main maternal risk:
subtending the symphysis pubis ○ Serious perineal tears
and at a shorter duration ○ Postpartum hemorrhage
○ Few cases of maternal blood loss ■ usually from uterine atony but also
○ Disadvantage: increase incidence for from lacerations
cervical laceration (inspect after delivery) ● Fetal macrosomia, maternal obesity, prolonged
■ Due to the grasping of the head second-stage labor and a prior event raise risks for
● Delivery in OP shoulder dystocia
○ **both may be accomplished by Forceps ● The American college of obstetricians and
● Cesarean delivery gynecologist reviewed studies & concluded that:
1. Most cases of shoulder dystocia cannot be
PERSISTENT OCCIPUT TRANSVERSE accurately predicted or prevented
● When the head enters the birth canal it is often in this 2. Elective induction of labor or elective
rotation more than 95% cesarean delivery for all women suspected
● OT is a transitory position of having a macrosomic fetus is not
● Spontaneously rotates to anterior appropriate
● Persistence: Platypelloid/android 3. Planned cesarean delivery may be
● Management: considered for the nondiabetic woman with
○ Manual rotation to OA (90 degree rotation) a fetus whose estimated fetal weight is
○ Rotation by kielland forceps >5000g or for the diabetic woman whose
fetus is estimated to weigh >4500 g
SHOULDER DYSTOCIA ● Risk of recurrent shoulder dystocia (1-3%)
● Vaginal delivery→ complete emergence of fetal ● Trial of labor- reasonable for women with prior
head→ remainder of body may not rapidly follow shoulder dystocia
○ The anterior fetal shoulder can become ● The American college of obstetricians and
wedged behind the symphysis pubis and fail gynecologist recommends that Estimated fetal
to deliver using normally exerted downward weight, Gestational age, Maternal glucose
traction & maternal pushing tolerance & severity of prior neonatal injury be
● Obstetric emergency evaluated & risks and benefits of cesarean delivery
○ umbilical cord is compressed within the birth discussed with any woman with a history of shoulder
canal dystocia
● Increasing birthweight has been associated with TURTLE SIGN
increasing incidence for SD
● not a very common finding ● Inability of the head, opposed
● Material characteristics that favor increase BW: to the perineum / tightly opposing
○ Maternal obesity - obese/ big fetus head? (not clear)
○ Postterm pregnancy ● As the head emerges, it does
○ Multiparity not spontaneously rotate
○ DM- babies have smaller heads with wider ● If a turtle sign is present, you
shoulder to shoulder diameter will know that you are dealing with
○ GDM a shoulder dystocia
USE AT YOUR OWN RISK page 4 of 12
VAGINAL DELIVERY
MANAGEMENT
● Shoulder dystocia cannot be accurately predicted,
clinicians should be well versed in its management
and principles
○ Know that you are dealing with shoulder
dystocia. It is a must that you need help, you
cannot do it on your own ● Lifting the popliteal fossa away from the stirrups, and
● Goals: the thigh is pushed against the maternal abdomen or
○ Reduce the head-to-body delivery time side, the pelvic tilt is now orienting the pubic
○ Avoid fetal and maternal injury from symphysis more horizontally leading to 1.5cm
aggressive manipulation allowance to deliver the shoulders of the feus
● Recommended: initial gentle attempt at traction,
assisted by maternal expulsive efforts DELIVERY OF THE POSTERIOR SHOULDER
○ Adequate analgesia- ideal ● Arm is splinted, swept across chest, keep the elbow
● Generous episiotomy- to provide room for flexed
manipulation ● Fetal head is grasped and the arm extended along
○ Do mediolateral episiotomy→ can extend the side of the face
to the rectal mucosa ● Posterior arm delivered
○ Episiotomy→ does not lower brachial plexus ● Posterior shoulder girdle rotated obliquely to deliver
injury rates but raises third- and fourth- the anterior shoulder
degree laceration rates
SUPRAPUBIC PRESSURE
● Used to free the
anterior shoulder from its
impacted position behind
the symphysis pubis
WOOD’S CORKSCREW
● Applied by an
● Rotate posterior shoulder in a 180° degrees fashion
assistant, while
freeing the anterior shoulder
downward traction is
● High risk for humeral fracture
applied to fetal head
● Pressure is applied
with the heel of the hand
to the anterior shoulder
wedged above and
behind the symphysis
● The anterior shoulder is thus either depressed or RUBIN MANEUVER
rotated, or both, so the shoulders occupy the oblique ● 1st maneuver – Fetal shoulder are rocked from side
plane of the pelvis to side by applying force to the maternal abdomen
○ anterior shoulder can be freed ● 2nd maneuver – Fetal shoulder which pushed
toward the anterior surface of the chest
McROBERTS MANEUVER ● This maneuver abducts both shoulders, that turn
● Removing the legs from the stirrups and sharply produces a smaller bisacromial diameter
flexing them up towards the abdomen ○ smaller S-S diameter
● Caused – straightening of the sacrum relative to the ● This permits displacement of the anterior shoulder
lumbar vertebrae, rotation of the symphysis pubis from behind the symphysis
toward the maternal head, and decrease in the angle
of pelvic inclination
● Does not – increase pelvic dimension, pelvic rotation
cephalad tends to free the impacted anterior shoulder
USE AT YOUR OWN RISK page 5 of 12
VAGINAL DELIVERY
GASKIN MANEUVER
● “all-fours maneuver”
● “knees and hand position” against the bed
● Downward traction on head and neck to free the
posterior shoulder
POSTERIOR AXILLA SLING TRACTION
● Suction catheter hooked under the axilla and tied
around the posterior shoulder
SYMPHYSIOTOMY or PUBIOTOMY
● Upward and outward traction applied
● Complication: ● Old technique of 1960s when there was no possibility
○ Humeral fracture to do emergent C-section
○ Erb’s palsy
DELIBERATE FRACTURE OF ANTERIOR CLAVICLE
● Thumb pressing the clavicle against the pubic rami
● Decrease the transverse diameter of the chest and
shoulders
● Look at where the incision is made, we know that the
symphysis pubis is held together by a membranous
and the fibrous tissue, so that is where you incise the
symphysis pubis.
● When the bones are separated, now it is easy for you
to remove that head.
● Babies with fractured clavicles when delivered, are CLEIDOTOMY
treated with splinting which is formed in a figure 8. ● Usually done on a dead fetus
Neonate bones heal rapidly.
HIBBARD MANEUVER
● Apply pressure to the fetal jaw and neck in the
direction of maternal anus with strong fundal pressure ● We don’t want to end up doing this that’s why it's a
must that planning the delivery of the baby would
There are 3 destructive maneuvers for shoulder dystocia be the better and most acceptable fashion
which are:
● Zavanelli maneuver SHOULDER DYSTOCIA VIDEO
● Symphysiotomy or pubiotomy
● Cleidotomy ● Shoulder dystocia is a complication that can occur
during a vaginal delivery
○ An obstetrical emergency
ZAVANELLI MANEUVER
○ Occurs when after delivery of the fetal head
● Replacement of the fetal head into the pelvis followed additional obstetrical maneuvers are
by CS delivery required to deliver the fetal shoulders
● Flexing the fetal head and pushing it back up into the (occurs in approximately 1% of births)
vagina to get the fetal head back into the pelvis ○ Can be caused by impaction of the anterior
● Perform an emergency CS or posterior shoulder during vaginal delivery
● Complication: ■ Anterior shoulder is more common
○ Neonatal death and is caused by impaction at the
○ Stillbirth maternal pubic symphysis
○ Brain damage ■ Posterior shoulder is less common
○ Uterine rupture and is caused by impaction at the
maternal sacral promontory
USE AT YOUR OWN RISK page 6 of 12
VAGINAL DELIVERY
● Risk factors: ○ Apply Suprapubic Pressure & Anterior
○ Maternal diabetes Shoulder Disimpaction
○ Suspected macrosomia ■ To do this, one of the team
○ Gestational age >42 weeks members should grab a stool to
○ Previous shoulder dystocia stand on and then use their palm or
○ Operative delivery fist to apply downward and lateral
● Over 50% of cases are not predictable and have no pressure suprapubicly
risk factors so you need to be prepared for the ■ This maneuver adducts and rotates
possibility of shoulder dystocia at every delivery the fetal shoulders to disimpact the
● Shoulder dystocia is a clinical diagnosis that should anterior shoulder
be made promptly.
○ Diagnosis is made when the routine practice
of gentle downward traction of the fetal head
fails to deliver the anterior shoulder
○ It is very important to diagnose shoulder
dystocia as soon as it occurs so that the
obstetrical team can start to manage it right
away
● Goal of management: To deliver the infant before
asphyxia from umbilical cord compression occurs ■ Another way to disimpact the
without causing any fetal or maternal trauma anterior shoulder is using the Rubin
maneuver
CASE STUDY:
■ Done by placing one hand into
● SARAH is a 28 year old G1 at 40 weeks gestation
that has been laboring for the past 10 hours. She is vagina and on the back surface
healthy and takes no medications. She has had a of the posterior fetal shoulder
normal pregnancy so far. Sarah had an epidural to and rotating it anteriorly to
manage her labor pain when she was 4cms dilated. disimpact the anterior shoulder
Now, she is fully dilated and has been pushing well
for the past 2 hours. You and the resident notice ■ If you’re unable to do so, move
that the fetal head delivered but then retracted on to the next step
back into the perineum (turtle sign). What do you
and the resident do next?
○ Release the posterior shoulder
● Management: (ALARMER) ■ One hand is in the vagina after
○ Ask for help finding the fetal arm, flex the
○ Legs (McRoberts maneuver) elbow crossed the chest to grasp
the forearm or hand and pull it out
■ The patient’s legs should be flexed of the vagina
all the way back so that her thighs ■ If you can’t deliver the fetal arm it
are above her abdomen. may be possible to deliver the
■ This movement rotates the pubis shoulder. If not, move on to the
symphysis and flattens the sacrum next step.
to relieve obstruction in up to 42%
of patients ○ Maneuver of Woods (Screw maneuver)
■ if shoulder dystocia persists move ■ Rotate the fetus or unscrew it by
on to the next step putting pressure on the clavicle of
the posterior shoulder and rotating
it until it becomes anterior
USE AT YOUR OWN RISK page 7 of 12
VAGINAL DELIVERY
○ Episiotomy STEPS OF AMTSL IN SEQUENCE
■ surgical cut made at the opening of 1. Check the uterus for the presence of a second baby
the vagina to allow more room and 2. In less that 1 minute, administer a uterotonic drug
better access to the posterior arm ● Uterotonics play an important role to
○ Roll onto all fours decrease postpartum blood loss
■ The patient is helped onto her 3. Apply controlled cord traction
hands and knees ● Do not jerk the delivery of the placenta
■ This is an effort to take advantage because it might still be attached to the
of gravity to facilitate delivery borders/walls of the uterus
○ If none of the steps of the acronym work ● Deliberate cord traction- eversion of the
there are several last resort methods that fundus
can be considered. However, these are 4. After delivery of the placenta, immediate massage of
associated with a significant increase in fetal uterus
and maternal morbidity. These include: 5. Check for completeness of placenta
■ Fracture of the fetal clavicle ● Lay it down on the side table and make sure
■ Zavanelli maneuver that you have complete cotyledon
● Returning the fetal head & 6. Examine the woman’s vagina, perineum and external
Attempting Cesarean genitalia for lacerations or active bleeding
delivery
MEDICATIONS USED FOR AMTSL
■ Symphysiotomy
● separation of the maternal
pubic bones OXYTOCIN
● High dose, produced in the posterior pituitary
● Effects in 1 min; mean half-life of 3-5 min
Back in the case…
● Can cause hypotension- if given in bolus
● You and your resident suspect shoulder dystocia
and initiate the ALARMER acronym. ○ It should be given as dilute solution by
continuous intravenous infusion or as an
intramuscular injection
MANAGEMENT OF THIRD STAGE OF LABOR
● Has an antidiuretic hormone effect- can cause
● Delivery of the placenta
water intoxication
○ If administered in high doses for a
EXPECTANT OR PHYSIOLOGICAL
considerable amount of time, concentration
● Waiting for placental separation signs and allow
should be increased instead of the infusion
spontaneous placental delivery
flow rate
● By nipple stimulation
● Contraindicated in patients with heart disease and
● By gravity
hypovolemic hemorrhage
● Median time: 4-12 minutes
● Dose: 20 U/L (10-20mL/min infusion) until the uterus
● Cut the umbilical cord in between the two clamps.
remains firmly contracted and bleeding is controlled
After cutting, you will end up with one clamp, roll it
● The infusion rate is then reduced to 1 to 2mL/min until
and do a gentle traction horizontally.
the mother is ready for transfer from recovery to the
postpartum unit
ACTIVE MANAGEMENT (AMTSL)
● Triad of:
ERGONOVINE AND METHYLERGONOVINE
○ Early cord clamping
■ Though we do not advocate early ● Ergot alkaloids
cord clamping, it goes without ● Alternative in settings that lack oxytocin
saying that once the umbilical ● Strict storage requirements
pulsation has cease, clamp the cord ● IM or oral (dose: 0.2mg)
immediately ● Never given antepartum- can cause tetanic
○ Controlled cord traction during placental contraction
delivery ● Recommended as given 12 hourly due to its
○ Immediate administration of prophylactic sustained effect
uterotonics ● Causes maternal hypertension
● AIM of AMTSL: Limit Postpartum Hemorrhage ● Less effective compared to oxytocin
USE AT YOUR OWN RISK page 8 of 12
VAGINAL DELIVERY
MISOPROSTOL
● Off-label drug 2. When the placenta
○ This drug is used for gastrointestinal detaches, it is grasped
problems, however, its side effect is smooth and removed.
muscle contraction and therefore very good ● Once the hand is inside
for contracting the uterus the uterine cavity, like
● Prostaglandin E1 analog turning the pages of
● Alternative in settings that lack oxytocin the book, you try to
● Given as a single oral dose of 600mcg detach its attachment
● Side effects: to the uterine fundus or
○ chills- 30% to the uterine surface -
○ fever- 5% until you are able to
grasp the full detached
OTHER ALTERNATIVE DRUG placenta before the
● Carboprost- synthetic prostaglandin analogue of placenta is grasped and removed.
PGF2α with oxytocic properties ● Never grasp the placenta without it being
● Carbetocin- an alternative uterotonic drug detached from its attachment, otherwise you
might puncture of perforate the uterine cavity or
MANUAL REMOVAL OF PLACENTA uterine musculature
● If the placenta could not be delivered spontaneously,
then you can go for manual removal of the placenta FOURTH STAGE OF LABOR
○ In approximately 2 percent of singleton ● An hour immediately following delivery of the
births, the placenta may not deliver promptly. placenta.
● Threshold for spontaneous delivery for placenta ○ The hour immediately following delivery of
range: 15 - 60 minutes the placenta is critical.
● Retained placenta: ○ During this time, lacerations are repaired.
○ Placenta adherens ● Check for laceration as cause for bleeding
■ Adherent placenta that would not ○ Although uterotonics are administered,
separate on its own. postpartum hemorrhage as the result of
■ Uterine contractions are insufficient uterine atony is most likely at this time.
to detach the placenta ● Hematoma may likely expand.
○ Lower uterine segment constriction ○ Consequently, uterine tone and the perineum
■ Detached but trapped placenta are frequently evaluated.
■ The placenta has detached already ● Uterine atony is most likely at this time
but gets trapped inside.
○ Morbidly adherent placenta ● The American Academy of Pediatrics and the
● Consistent risks for retained placenta include: American College of Obstetricians and Gynecologists
○ Stillbirth (2017b) recommend that:
○ Prior cesarean delivery ○ Maternal blood pressure and pulse are
○ Prior retention recorded immediately after delivery and
○ Preterm delivery every 15 minutes for the first 2 hours.
○ The placenta, membranes, and umbilical
cord are examined for completeness and for
STEPS IN MANUAL REMOVAL OF PLACENTA
anomalies.
BIRTH CANAL LACERATIONS
1. One hand grasps the ● Lower genital tract lacerations may involve the cervix,
fundus and the other vagina, or perineum.
hand into the uterine ○ Those of the perineum often follow vaginal
cavity and and the delivery, and most are first- and second-
fingers are swept from degree lacerations.
side to side as they are ● Lacerations are classified by their depth, and
advanced. complete definitions.
USE AT YOUR OWN RISK page 9 of 12
VAGINAL DELIVERY
FIRST DEGREE
● Superficial only
○ Fourchette
○ Perineal skin C. Third-degree laceration: EAS
○ Vaginal mucous and IAS are torn.
membrane
● May Include periurethral
lacerations
● First-degree perineal
laceration: injury to only the
vaginal epithelium or FOURTH DEGREE
perineal skin. ● The perineal body, entire anal sphincter complex, and
anorectal mucosa are lacerated.
SECOND DEGREE ● Third- and fourth-degree lacerations are considered
● Fascia and muscles of obstetrical anal sphincter injuries (OASIS), and their
perineal body combined incidence varies from 0.5 to 5 percent.
● May be midline ○ Risk factors for these more complex
● May extend upward or to both lacerations include:
sides of vagina ■ Nulliparity
● Second-degree laceration: ■ Midline episiotomy
injury to perineum that spares ■ Persistent OP position
the anal sphincter complex ■ Operative vaginal delivery
but involves the perineal ■ Asian race
muscles, which are the ■ Short perineal length
bulbospongiosus and ■ Increasing fetal birth weight
superficial transverse ● Morbidity rates rise as laceration severity increases.
perineal muscles. ○ Compared with simpler lacerations, anal
sphincter injuries are associated with greater
blood loss and puerperal pain.
THIRD DEGREE
○ Wound disruption and infection rates are
other risks
EPISIOTOMY
● Episiotomy is an incision of the pudendum–the
A. <50 percent of the external external genital organs.
anal sphincter (EAS) is torn. ○ In contrast to spontaneous lacerations,
perineotomy is an intended incision of the
perineum.
● Midline and mediolateral episiotomies
○ The two main types
○ Vary by the angle of perineal incision.
MIDLINE MEDIOLATERAL
The midline episiotomy The mediolateral episiotomy
B. >50 percent of the EAS is begins at the fourchette, begins at the midline of the
torn, but the internal anal incises the perineal body in fourchette and is directed to
sphincter (IAS) remains intact. the midline, and ends well the right or left at an angle
before the external anal 60 degrees off the midline.
sphincter is reached. The This angle accounts for
incision length varies from 2 perineal anatomy distortion
to 3 cm depending on during crowning and
perineal length and degree ultimately yields an incision
of tissue thinning. 45 degrees off the midline
for suturing.
USE AT YOUR OWN RISK page 10 of 12
VAGINAL DELIVERY
● Benefit: easier to repair compared to a laceration ○ You may see a brownish or reddish mucus
○ Proven Incorrect: discharge which could be the mucus plug at
■ Less post op pain the opening of your cervix falling out.
■ Healing is improved ○ Your water may break which can either be a
■ Prevents pelvic floor disorders large gush of fluid or continuous trickle.
■ If you experience any of these
COMPARISON symptoms, contact your doctor or
midwife to see if you should go to
the hospital.
TYPE OF EPISIOTOMY
CHARACTERISTICS MIDLINE MEDIOLATERAL
● At the beginning of stage two of the labor which can
last from a few minutes to three hours, your cervix is
Surgical Repair Easy More difficult fully dilated top 10 cm and your baby’s head has
moved beyond the cervical opening into your birth
Faulty Healing Rare More common
canal.
Post operative pain Minimal Common ○ During this stage, you will begin to push your
baby out.
Anatomical Results Excellent Occasionally faulty ■ You may instinctively push when
you feel the urge or you may need
Blood loss Less More
coaching from your doctor, midwife
Dyspareunia Rare Occasional or labor nurse as when to push and
when to rest.
Extensions Common Uncommon ● In a normal delivery your baby’s head will rotate to
face your back.
● During active labor, your uterus is divided into an
○ Active segment that contracts pushing the
baby downward
○ Flexible passive segment that remains
relaxed, stretching to provide more room for
the baby to pass through.
● In some cases, when the top of your baby’s head
appears or crowns, your doctor may make a small cut
called an episiotomy to enlarge the vaginal opening.
○ Then you will continue pushing your baby
out.
● As your baby’s head passess through the birth canal,
A mediolateral episiotomy is cut as the baby’s head crowns. it molds into an elongated shape.
Fingers are insinuated between the perineum and head. The ○ An elongated head shape will resolve itself
incision begins in the midline and is directed toward the within a few days as the skull bones shift
ipsilateral ischial tuberosity at an angle 60 degrees off the
midline. back into place.
● After your baby’s head exits the birth canal his or her
head and shoulders will rotate to help the shoulders
VIDEO pass through the birth canal.
● Your baby’s shoulders are delivered one after the
LABOR AND DELIVERY other in order to fit through your pelvis.
● Once the shoulders emerge, the rest of your baby
● During a vaginal childbirth the first stage of labor slides out easily.
lasts about 12 to 19 hours and starts when your baby ● After your baby is born, his or her umbilical cord will
settles lower into your pelvis. be cut.
● In response, your cervix begins to efface or become
thinner and dilate or widen. ● In stage 3 of labor which may last 5 - 30 minutes,
○ During this time you may feel strong, mild contractions will help to push the placenta out of
regular contractions occurring every 5 - the uterus.
20 minutes and lower back pain and ● During this stage, you and your baby may begin
cramping that does not go away. bonding through skin to skin contact or through breast
feeding
USE AT YOUR OWN RISK page 11 of 12
VAGINAL DELIVERY
EPISIOTOMY
● If you are having a vaginal delivery, your doctor may
perform an episiotomy to enlarge the vaginal opening.
● During pregnancy, your baby grows inside your uterus
or womb and is nourished by the placenta.
● When your baby is ready to be born, labor begins.
● During labor, your uterus squeezes or contracts to
push your baby through the open cervix and into the
vagina which expands to allow your baby to pass
through and be born.
● An episiotomy may be done in an effort to avoid
spontaneous tearing during delivery if your baby is
large, or in the breech position, labor is going on too
quickly or if instruments such as forceps or a vacuum
extractor are needed to remove your baby from the
birth canal.
● An episiotomy may be done to help speed up delivery
if your labor is going too slowly or if you or the baby
are in distress.
● If you have not already received anesthesia before
your delivery, your doctor will inject medication to
numb your vaginal opening and perineum, which is
the area separating the vagina and anus.
● Using surgical scissors, your doctor will make a 1 to 3
inch midline or mediolateral incision in the perineum.
○ A midline incision extends straight down
from the vagina towards the anus.
○ A mediolateral incision is made on an angle
from the vagina in the direction of the anus.
● The benefit of the mediolateral incision is that it is less
likely to tear through to the anus.
● The downside however is that it can also be more
painful and take longer to heal.
● Once your doctor delivers your baby and the
placenta, he or she will close the episiotomy incision
with stitches.
● These stitches will be absorbed by your body and do
not need to be removed.
● An episiotomy usually heals without complications,
although it may take several weeks.
● Within the first 24 hours, your nurse will likely help
you apply ice packs to the stiches.
USE AT YOUR OWN RISK page 12 of 12
You might also like
- Postpartum Report SheetDocument1 pagePostpartum Report SheetHeather McCormick100% (8)
- DR Write UpDocument15 pagesDR Write Upjansestacio100% (3)
- Chapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationDocument9 pagesChapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationAlyssaGrandeMontimor100% (1)
- Lesson 1.1 Maternal Anatomy Dr. Jane PublicoDocument11 pagesLesson 1.1 Maternal Anatomy Dr. Jane PublicoKristel Saturn SalvadNo ratings yet
- Airway ManagementDocument48 pagesAirway ManagementRea Dominique CabanillaNo ratings yet
- Osce - D&CDocument2 pagesOsce - D&Cmkct111No ratings yet
- ESL Progress Report COMMENT BANKDocument9 pagesESL Progress Report COMMENT BANKCherie thompson100% (2)
- Partograph: Jillian A. Bejoc, MSN, RNDocument44 pagesPartograph: Jillian A. Bejoc, MSN, RNJiezl Abellano AfinidadNo ratings yet
- ANA.S4.CA21.Female Reproductive SystempdfDocument6 pagesANA.S4.CA21.Female Reproductive SystempdfCazz HeyNo ratings yet
- PPT Book ReadingDocument20 pagesPPT Book ReadingOctaria SaputraNo ratings yet
- NCM109 Maternal - Child Nursing (A-C) - Module 5Document6 pagesNCM109 Maternal - Child Nursing (A-C) - Module 5iratsyukieNo ratings yet
- HEALTH ASSESSMENT - Breasts & Regional LymphaticsDocument5 pagesHEALTH ASSESSMENT - Breasts & Regional LymphaticsMich Hiel OforraNo ratings yet
- Operative Vaginal DeliveryDocument8 pagesOperative Vaginal DeliveryGerben VillanuevaNo ratings yet
- 05.3 Problems of The Power and Psyche PDFDocument12 pages05.3 Problems of The Power and Psyche PDFJAN CAMILLE LENONNo ratings yet
- Mechanisms of LaborDocument4 pagesMechanisms of LaborIrish Paulene NiroNo ratings yet
- Obstetrics and GynecologyDocument44 pagesObstetrics and Gynecologyjaisanatandharma7No ratings yet
- Destructive Operations. PDFDocument63 pagesDestructive Operations. PDFFeba SajanNo ratings yet
- 04 Third Trimester ConditionsDocument11 pages04 Third Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- Rle DR Rot 2ND SemDocument2 pagesRle DR Rot 2ND SemRae LebrilloNo ratings yet
- AC MS Post-Operative FINALDocument8 pagesAC MS Post-Operative FINALCiaraNo ratings yet
- NCM107 Leopolds ManeuverDocument4 pagesNCM107 Leopolds Maneuverchloepaxton030No ratings yet
- 1.03 General Survey, Skin and Anthropometric AssessmentDocument14 pages1.03 General Survey, Skin and Anthropometric AssessmentKim DeeNo ratings yet
- CCE1 AirwayDocument8 pagesCCE1 AirwayHoward ChangNo ratings yet
- Normal Labor: Kevin Marcial I. Aralar, MD 1 Year ResidentDocument46 pagesNormal Labor: Kevin Marcial I. Aralar, MD 1 Year ResidentKevin AralarNo ratings yet
- PGI MANIMTIM - Vaginal Delivery, Breech Delivery and Operative Vaginal DeliveryDocument8 pagesPGI MANIMTIM - Vaginal Delivery, Breech Delivery and Operative Vaginal DeliveryKim Adarem Joy ManimtimNo ratings yet
- Obstetric & Gynecology Health Care Center by SlidesgoDocument64 pagesObstetric & Gynecology Health Care Center by SlidesgoShane mNo ratings yet
- Normal LabourDocument88 pagesNormal LabourDebayan KhanNo ratings yet
- Manual Removal of PlacentaDocument25 pagesManual Removal of PlacentaLoorthu Selvi M0% (1)
- Pedia Gi-GuDocument16 pagesPedia Gi-GuZhantelle A. Santos100% (1)
- nots shoulder dystociaDocument4 pagesnots shoulder dystociamelly novNo ratings yet
- Obstetric Emergencies 28072020Document84 pagesObstetric Emergencies 28072020Arief NorddinNo ratings yet
- Abnormal LaborDocument26 pagesAbnormal LaborShane mNo ratings yet
- 85297.1606818947gyne SampleDocument10 pages85297.1606818947gyne SampleRithikaNo ratings yet
- Toag 2000 2 4 53Document1 pageToag 2000 2 4 53Sharmela BrijmohanNo ratings yet
- S3-06 Ophthalmology Eyelid, Lacrimal - Orbital Disorders (v2) PDFDocument13 pagesS3-06 Ophthalmology Eyelid, Lacrimal - Orbital Disorders (v2) PDFAl SyNo ratings yet
- Shoulder Dystocia RetdemDocument2 pagesShoulder Dystocia RetdemDarwin QuirimitNo ratings yet
- Augmentation of LabourDocument45 pagesAugmentation of LabourLamnunnem HaokipNo ratings yet
- P4P REPRO 2.0Document54 pagesP4P REPRO 2.0william atmadjiNo ratings yet
- Delivery of Baby (Actual, Assist, and Cord Care)Document3 pagesDelivery of Baby (Actual, Assist, and Cord Care)Jasmin AdoraNo ratings yet
- Week 11 - Assessment of Breast and Lymphatic SystemDocument5 pagesWeek 11 - Assessment of Breast and Lymphatic SystemJuan Miguel TevesNo ratings yet
- Unit 5 Newborn ConceptsDocument5 pagesUnit 5 Newborn ConceptsEunice TrinidadNo ratings yet
- (OBS) 2.01 Physiology of Labor, Normal Labor, and Delivery - Junio (Final V.02 - Sep 26)Document18 pages(OBS) 2.01 Physiology of Labor, Normal Labor, and Delivery - Junio (Final V.02 - Sep 26)Sam MataNo ratings yet
- His.s4.Sr MergedpdfDocument190 pagesHis.s4.Sr Mergedpdfsky vallartaNo ratings yet
- Shoulder Dystocia Guideline 280720Document10 pagesShoulder Dystocia Guideline 280720Ahmed SamyNo ratings yet
- NSD ChecklistDocument3 pagesNSD ChecklistChristine Evan HoNo ratings yet
- 19 - Vaginal DeliveryDocument16 pages19 - Vaginal DeliveryGen XNo ratings yet
- Operative DeliveriesDocument58 pagesOperative DeliveriesDanduuNo ratings yet
- 2nd Year All Clinicals AIMC AcademiaDocument64 pages2nd Year All Clinicals AIMC Academiasaleempanwar96No ratings yet
- Assesment and Monitoring During 2nd Stage of LabourDocument11 pagesAssesment and Monitoring During 2nd Stage of LabourPragati BholeNo ratings yet
- Postpartal ComplicationDocument4 pagesPostpartal ComplicationHanna AligatoNo ratings yet
- 3 Priority Nursing Care Plans During DeliveryDocument11 pages3 Priority Nursing Care Plans During DeliveryRyan Robert V. VentoleroNo ratings yet
- 07 - LEC Care of The NewbornDocument17 pages07 - LEC Care of The NewbornJAN CAMILLE LENONNo ratings yet
- Perioperative NursingDocument9 pagesPerioperative NursingHannah PatriciaNo ratings yet
- Nursing Care of A Family Experiencing A Complication of Labor or BirthDocument25 pagesNursing Care of A Family Experiencing A Complication of Labor or BirthZhantelle A. SantosNo ratings yet
- MaternalDocument2 pagesMaternalqweyo yhuNo ratings yet
- NCM - 207 RLE (Delivery Room Nursing)Document9 pagesNCM - 207 RLE (Delivery Room Nursing)Tintin HonraNo ratings yet
- 5.9.5 Shoulder Dystocia M: AnagementDocument8 pages5.9.5 Shoulder Dystocia M: AnagementTriponiaNo ratings yet
- Perineal Trauma & Epsiotomy: Pembimbing: Dr. Arief Budiono, SP - OGDocument42 pagesPerineal Trauma & Epsiotomy: Pembimbing: Dr. Arief Budiono, SP - OGHans Natanael PosoNo ratings yet
- Narrow Pelvis. Anomalies of Position and Fetal Presentation. Pregnancy and Childbirth During Pelvic Presentation.Document18 pagesNarrow Pelvis. Anomalies of Position and Fetal Presentation. Pregnancy and Childbirth During Pelvic Presentation.mudeyNo ratings yet
- Persalinan, Episiotomi, Dan Nifas: Vaulinne BasyirDocument33 pagesPersalinan, Episiotomi, Dan Nifas: Vaulinne BasyirKhairunnisa KhairunnisaNo ratings yet
- Case Presentation On Normal LaborDocument62 pagesCase Presentation On Normal LaborB34-YvesJethro ReyesNo ratings yet
- LEOPOLDS MANEUVER ReviewerDocument3 pagesLEOPOLDS MANEUVER ReviewerLloyd BaylonNo ratings yet
- 10 Post Partum 1Document3 pages10 Post Partum 1Gwen CastroNo ratings yet
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesRating: 5 out of 5 stars5/5 (2)
- Hello! Nice To See You Again!Document14 pagesHello! Nice To See You Again!Cherie thompsonNo ratings yet
- Microbiology - 2nd LE 2018Document9 pagesMicrobiology - 2nd LE 2018Cherie thompsonNo ratings yet
- FF - Get Ready211Document12 pagesFF - Get Ready211Cherie thompsonNo ratings yet
- FF - Market Talk1032Document7 pagesFF - Market Talk1032Cherie thompsonNo ratings yet
- Parasitology - Lab Pracs MidtermDocument54 pagesParasitology - Lab Pracs MidtermCherie thompsonNo ratings yet
- FF - Cyle A001Document8 pagesFF - Cyle A001Cherie thompsonNo ratings yet
- L Esson31 The Bird's NestDocument11 pagesL Esson31 The Bird's NestCherie thompsonNo ratings yet
- FF LightningA07Document13 pagesFF LightningA07Cherie thompsonNo ratings yet
- FF - KB214 - Unit 6 - Lesson 2Document13 pagesFF - KB214 - Unit 6 - Lesson 2Cherie thompsonNo ratings yet
- Homework From The Last LessonDocument12 pagesHomework From The Last LessonCherie thompsonNo ratings yet
- Homework From The Last LessonDocument13 pagesHomework From The Last LessonCherie thompsonNo ratings yet
- Homework From The Last LessonDocument14 pagesHomework From The Last LessonCherie thompsonNo ratings yet
- FF LightningB06Document14 pagesFF LightningB06Cherie thompsonNo ratings yet
- Monthly Test Evaluation: Criteria Score (10) Strengths Weaknesses RecommendationDocument1 pageMonthly Test Evaluation: Criteria Score (10) Strengths Weaknesses RecommendationCherie thompsonNo ratings yet
- Renzel Franz B. DanaoDocument2 pagesRenzel Franz B. DanaoCherie thompsonNo ratings yet
- PCEID Report FormatsDocument2 pagesPCEID Report FormatsCherie thompsonNo ratings yet
- High School Grade 1A: Travel JournalDocument17 pagesHigh School Grade 1A: Travel JournalCherie thompsonNo ratings yet
- Nircmd Mic Locker Setup Without Using Task SchedulerDocument2 pagesNircmd Mic Locker Setup Without Using Task SchedulerCherie thompsonNo ratings yet
- Avelino E. Sadiao: Special Program For The Employment of Students June-July 2018 Benguet Provincial CapitolDocument2 pagesAvelino E. Sadiao: Special Program For The Employment of Students June-July 2018 Benguet Provincial CapitolCherie thompsonNo ratings yet
- National Health Situation of The Philippines For CHNDocument5 pagesNational Health Situation of The Philippines For CHNanreilegarde100% (1)
- Inducing Labour: Clinical Guideline Published: 23 July 2008Document35 pagesInducing Labour: Clinical Guideline Published: 23 July 2008dNo ratings yet
- Pregnancy & ChildbirthDocument12 pagesPregnancy & Childbirthrobert tambuliNo ratings yet
- Cheska Maternal AssignmentDocument3 pagesCheska Maternal AssignmentJoule PeirreNo ratings yet
- Proximity of Magnesium Exposure To Delivery and Neonatal Outcomes 2016 American Journal of Obstetrics and GynecologyDocument6 pagesProximity of Magnesium Exposure To Delivery and Neonatal Outcomes 2016 American Journal of Obstetrics and GynecologyFarin MauliaNo ratings yet
- Revision Long Case Obs Gynae PDF FreeDocument10 pagesRevision Long Case Obs Gynae PDF Freesirajulislam6017No ratings yet
- Microbiology: Submitted by Sherwin N. Genova Submitted To Ms. Reah FojasDocument9 pagesMicrobiology: Submitted by Sherwin N. Genova Submitted To Ms. Reah FojasSherwin Nicolas GenovaNo ratings yet
- 15 Physio OB - Normal LaborDocument8 pages15 Physio OB - Normal LabormaqmmNo ratings yet
- Resume Update 12 2019Document2 pagesResume Update 12 2019api-354751775No ratings yet
- Emergencies ObsDocument7 pagesEmergencies ObsAshish GuptaNo ratings yet
- Postnatal Care: Samson Udho MSC, BSCDocument34 pagesPostnatal Care: Samson Udho MSC, BSCAYO NELSON0% (1)
- Bahasa Inggris NURHALIMAH-1Document3 pagesBahasa Inggris NURHALIMAH-1NurhalimahNo ratings yet
- Ashrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarDocument4 pagesAshrafian, Hutan Sunzi Surgical Philosophy Concepts of Modern Surgery Paralleled To Sun Tzus Art of WarWilliam AdiputraNo ratings yet
- Emonc ProtocolDocument38 pagesEmonc ProtocolXerxes MalagaNo ratings yet
- 2M Intrapartal Complications Written Report 109Document72 pages2M Intrapartal Complications Written Report 109kai xoxoNo ratings yet
- MK Polyhydramnios and Oligohydramnios (OBGY)Document14 pagesMK Polyhydramnios and Oligohydramnios (OBGY)Moses Jr KazevuNo ratings yet
- Enhancing Childbirth Satisfaction Through A Brief, Targeted Educational InterventionDocument25 pagesEnhancing Childbirth Satisfaction Through A Brief, Targeted Educational InterventionekinooristiqomahNo ratings yet
- Ernawati - PIT Feto 2023 PreeklampsiaDocument21 pagesErnawati - PIT Feto 2023 PreeklampsiaHeldasari SianturiNo ratings yet
- A Thesis ProtocolDocument3 pagesA Thesis ProtocolOmar TousifNo ratings yet
- Abnormal LabourDocument15 pagesAbnormal LabourAshish GuptaNo ratings yet
- Pengaruh Body Massage Terhadap Tingkat Depresi Ibu Nifas Di Bidan Praktik Mandiri Siyamtiningsih KaranganyarDocument8 pagesPengaruh Body Massage Terhadap Tingkat Depresi Ibu Nifas Di Bidan Praktik Mandiri Siyamtiningsih KaranganyarEnzel LinaNo ratings yet
- Asuhan Kebidanan Komprehensif Pada Ny I Umur 35 TaDocument6 pagesAsuhan Kebidanan Komprehensif Pada Ny I Umur 35 TaWienta dsNo ratings yet
- Jurnal PERKEMBANGAN PENDIDIKAN KEBIDANAnDocument7 pagesJurnal PERKEMBANGAN PENDIDIKAN KEBIDANAnSurti PartiningsihNo ratings yet
- Jurnal Rupture Perineum 3Document6 pagesJurnal Rupture Perineum 3Muh AqwilNo ratings yet
- CPD Concept MapDocument1 pageCPD Concept MapShandle Dynne Baena100% (1)
- Kpsea Online RegslipDocument14 pagesKpsea Online RegslipNeldia CyberNo ratings yet
- Unit Plan Obg 1Document24 pagesUnit Plan Obg 1Daily DoseNo ratings yet