Professional Documents
Culture Documents
Artigo TRATAMENTO ANEMIA FERROPRIVA2
Artigo TRATAMENTO ANEMIA FERROPRIVA2
Uploaded by
adriana félixOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Artigo TRATAMENTO ANEMIA FERROPRIVA2
Artigo TRATAMENTO ANEMIA FERROPRIVA2
Uploaded by
adriana félixCopyright:
Available Formats
Original Investigation | Hematology
The Efficacy and Safety of Vitamin C for Iron Supplementation
in Adult Patients With Iron Deficiency Anemia
A Randomized Clinical Trial
Nianyi Li, MD, PhD; Guangjie Zhao, MD; Wanling Wu, MD; Mengxue Zhang, MD; Weiyang Liu, MD; Qinfen Chen, MD; Xiaoqin Wang, MD, PhD
Abstract Key Points
Question Are the effects of oral iron
IMPORTANCE It remains uncertain whether vitamin C routinely used with oral iron supplements is
supplements alone equivalent to a
essential for patients with iron deficiency anemia (IDA).
regimen of oral iron supplements plus
vitamin C in the treatment of iron
OBJECTIVE To compare the equivalence and assess the safety of oral iron supplements plus vitamin
deficiency anemia?
C or oral iron supplements alone in patients with IDA.
Findings In this randomized clinical trial
DESIGN, SETTING, AND PARTICIPANTS This single-center, open-label, equivalence randomized that included 440 adults with iron
clinical trial was conducted from January 1, 2016, to December 30, 2017, in Huashan Hospital, Fudan deficiency anemia, the mean change in
University. Adult patients with newly diagnosed IDA were enrolled. Participants were randomly hemoglobin level after 2 weeks was
assigned (1:1) to the oral iron supplements plus vitamin C group or the oral iron supplements–only 2.00 g/dL in the oral iron supplements
group. Data analysis was performed from March to December 2018. plus vitamin C group, compared with
1.84 g/dL in the oral iron supplements–
INTERVENTIONS Patients were randomized to receive a 100-mg oral iron tablet plus 200 mg of only group. This difference met
vitamin C or a 100-mg iron tablet alone every 8 hours daily for 3 months. prespecified criteria for equivalence.
Meaning The use of oral iron
MAIN OUTCOMES AND MEASURES The primary outcome was the change in hemoglobin level
supplements alone is comparable to a
from baseline to 2 weeks of treatment, and an equivalence margin of 1 g/dL in hemoglobin was
regimen of vitamin C supplemented
chosen for the demonstration of comparable efficacy. Secondary outcomes included the change in
with oral iron for patients with iron
the reticulocyte percentage after 2 weeks of treatment, the increase in hemoglobin level after 4
deficiency anemia.
weeks of treatment, the increase in serum ferritin level after 8 weeks of treatment, and
adverse events.
+ Visual Abstract
RESULTS Among the 440 randomized patients (220 each in the oral iron supplements plus vitamin
C group and iron-only group; 426 women [96.8%]; mean [SD] age, 38.3 [11.7] years), all were
+ Supplemental content
Author affiliations and article information are
assessed for the primary outcome, and 432 (98.2%) completed the trial. From baseline to the 2-week
listed at the end of this article.
follow-up, the mean (SD) change in hemoglobin level was 2.00 (1.08) g/dL in the oral iron
supplements plus vitamin C group and 1.84 (0.97) g/dL in the oral iron supplements–only group
(between-group difference, 0.16 g/dL; 95% CI, −0.03 to 0.35 g/dL), thus meeting the criteria for
equivalence. The mean (SD) change in serum ferritin level from baseline to 8-week follow-up was
35.75 (11.52) ng/mL in the vitamin C plus iron group and 34.48 (9.50) ng/mL in the iron-only group
(between-group difference, 1.27 ng/mL; 95% CI, −0.70 to 3.24 ng/mL; P = .21). There were no
significant differences between the 2 groups regarding the rates of adverse events (46 [20.9%] vs 45
[20.5%]; difference, 0.4%; 95% CI, −6.7% to 8.5%; P = .82). No patient withdrew because of
adverse events.
CONCLUSIONS AND RELEVANCE Among patients with IDA, oral iron supplements alone were
equivalent to oral iron supplements plus vitamin C in improving hemoglobin recovery and iron
(continued)
Open Access. This is an open access article distributed under the terms of the CC-BY License.
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 1/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
Abstract (continued)
absorption. These findings suggest that on-demand vitamin C supplements are not essential to take
along with oral iron supplements for patients with IDA.
TRIAL REGISTRATION ClinicalTrials.gov Identifier: NCT02631668
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644
Introduction
Iron deficiency anemia (IDA) is associated with a decrease in erythropoiesis caused by a deficit in
total body iron.1 Iron deficiency is the leading cause of anemia worldwide. According to the World
Health Organization guideline,2 IDA affects 30% of the world’s population, indicating that it is a
problem requiring attention.
Iron deficiency can be divided into 3 stages: prelatent iron deficiency, latent iron deficiency (also
called iron-deficient erythropoiesis), and iron deficiency anemia (IDA).2,3 At the first stage, iron
intake lower than the required amount causes progressive depletion of iron storage primarily in the
liver and muscle cells. Patients at this stage generally have no symptoms, and the diagnosis of iron
deficiency is made when levels of serum ferritin (the storage form of iron) decrease below 20 ng/mL
(to convert to micrograms per liter, multiply by 1.0). Sustained iron storage depletion leads to the
second stage of iron deficiency, iron-deficient erythropoiesis, in which iron deficiencies progress and
begin to affect erythropoiesis. Despite an increased transferrin level, serum iron level decreases
along with transferrin saturation. Erythropoiesis impairment appears when the serum iron level
decreases to less than 50.3 μg/dL (to convert to micromoles per liter, multiply by 0.179) and
transferrin saturation is less than 16%.4 Hemoglobin level is still within the normal range until the
development of the IDA stage. Iron storage levels deplete to the point that they can no longer
support the hemoglobin production and generate enough red blood cells (RBCs). Iron deficiency
impairs RBC synthesis and hemoglobin production, leading to anemia.5
During the prelatent iron deficiency phase, an iron-rich diet can treat most cases. However,
patients with IDA require iron supplements to replenish storage iron, restore normal hematopoiesis,
treat anemia, and relieve symptoms.3
Oral iron supplementation is the primary approach to restore iron levels for patients with IDA.
Numerous nonheme iron supplements are available, and ferrous sulfate and ferric succinate
supplements are the most commonly used. Vitamin C is the only dietary constituent other than
animal tissue that has been shown to promote iron absorption.6-9 Iron absorption occurs
predominantly in the duodenum and upper jejunum, where ferrous iron can be transported into
small intestine mucosal epithelial cells. When taken orally, iron is always oxidized to the Fe3+ state
from its original form. It requires an acidic gastrointestinal environment to be dissolved adequately
for absorption. Vitamin C can create a more acidic environment in the stomach and prevent the
oxidization of ferrous iron to ferric iron.10 However, in a series of 12 individuals treated with iron
during intake of a regular or vitamin C–supplemented diet,8 the effect of vitamin C on promoting iron
absorption from a complete diet was far less pronounced than that from a single meal. The facilitating
impact of vitamin C with food on iron status is minimal.8,11 Therefore, whether vitamin C has
additional advantages, such as improving the efficacy of iron tablets and, thus, speeding up the
recovery of anemia, remains poorly understood. Whether iron tablets with vitamin C supplements
should be recommended is controversial.
To our knowledge, until now there has not been a randomized clinical trial (RCT) to assess
whether vitamin C supplements are necessary for patients with IDA taking iron tablets. Therefore, it
is necessary to conduct a rigorous RCT to assess the efficacy and safety of oral iron supplements
alone or combined with vitamin C in patients with IDA. We designed a single-center, equivalence RCT
to evaluate whether oral iron supplements alone were comparable with oral iron supplements plus
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 2/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
vitamin C and to verify whether vitamin C routinely used with iron supplements can improve iron
absorption.
Methods
Study Design
This 2-year, open-label, single-center, RCT was conducted at Huashan Hospital, Fudan University,
Shanghai, China. All patients provided written informed consent before the commencement of the
study. The institutional review board of Huashan Hospital, Fudan University, approved this research.
This study follows the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Randomization of participants at a 1:1 ratio was performed using Stata statistical software
version 11.0 (StataCorp) by a randomization procedure (Figure 1). Sequentially numbered, opaque,
sealed envelopes ensured the concealment of randomization. The serial numbers on the outside of
the envelopes were consistent with the patients’ visit numbers. After baseline measurements, the
physician provided the sealed envelope marked with the eligible patient’s consulting number. Then
the patient opened the sealed envelope, which contained the information on the assigned
randomization group.
The intervention group received a 100-mg oral iron tablet (ferrous succinate, 100 mg/tablet)
plus 200 mg of vitamin C (vitamin C, 100 mg/tablet) every 8 hours daily; the control group received
a 100-mg iron tablet (ferrous succinate, 100 mg/tablet) every 8 hours daily. All patients took the
supplements with warm water half an hour after a meal. Compliance was addressed by determining
the actual number of iron and vitamin C tablets returned by the participants. The complete trial
protocol can be seen in Supplement 1.
Study Population
We screened patients newly diagnosed with IDA who had not received any iron supplement therapy
in Huashan Hospital, Fudan University, from January 1, 2016, to December 30, 2017. Some of these
patients were found to have anemia during a routine checkup. Most patients presented because of
symptoms such as dizziness and palpitation. The nurse prechecked first. If the patients were found to
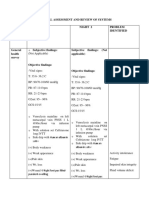
Figure 1. CONSORT Flow Diagram
530 Patients assessed for eligibility
90 Excluded
51 Met exclusion criteria
27 Declined to participate
12 Unknown
440 Randomized
220 Randomized to receive vitamin C supplement with 220 Randomized to receive single oral iron tablet
oral iron tablets 220 Received therapy as randomized
220 Received therapy as randomized
5 Did not complete study after 2 wk 4 Did not complete study after 2 wk
5 Lost to follow-up 4 Lost to follow-up
4 Transferred to other hospitals because of distance 3 Transferred to other hospitals because of distance
1 Unknown 1 Did not receive randomized therapy
220 Included in primary analysis 220 Included in primary analysis
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 3/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
have anemia, the nurse would recommend them to the anemia clinic to receive examination and
treatment. Then our team screened these patients for enrollment.
The inclusion criteria were age 18 years or older, voluntarily signing the informed consent form,
and meeting the diagnostic criteria for IDA, which include a hemoglobin level less than 13 g/dL for
men or less than 12 g/dL for women (to convert hemoglobin to grams per liter, multiply by 10.0),
mean corpuscular volume (MCV) less than 80 μm3 (to convert MCV to femtoliters, multiply by 1.0),
mean corpuscular hemoglobin (MCH) less than 27 pg/cell, mean corpuscular hemoglobin
concentration (MCHC) less than 32 g/dL (to convert MCHC to grams per liter, multiply by 10), serum
ferritin level less than 14 ng/mL for women or 30 ng/mL for men, serum iron less than 39 μg/dL for
women or 56 μg/dL for men, transferring saturation less than 20%, and total iron-binding capacity
(TIBC) exceeding 428 μg/dL (to convert TIBC to micromoles per liter, multiply by 0.179). Exclusion
criteria were pregnancy, severe uncorrectable bleeding, identified stomachache or intestinal ulcers,
any inflammatory diseases, or identified gastrointestinal tumors.
Study Monitor
Patients were treated for 3 months and assessed with a complete blood count every 2 weeks for 2
months; iron metabolism was measured at week 8. The primary outcome was the change in
hemoglobin level from baseline to the 2-week follow-up. The secondary outcomes included the
change in the reticulocyte percentage after 2 weeks of treatment, the increase in hemoglobin after 4
weeks of treatment, the increase in serum ferritin after 8 weeks of treatment, and adverse events.
Exploratory outcomes included MCV, MCH, and MCHC levels every 2 weeks at all time points and
serum iron level, transferring saturation, and TIBC at 8 weeks. The Department of Laboratory
Medicine in Huashan Hospital, Fudan University, conducted the measurements and biochemical
analyses.
Statistical Analysis
Sample size calculations were performed for the change in hemoglobin level from baseline using an
equivalence design; with bounds of 1 g/dL for the mean difference and a significance level of .05, a
total sample size of 392 participants (assuming no difference between groups), a common SD of 1.5
g/dL, an allowable error of 0.5 g/dL, and an allocation ratio of 1:1 would correspond to a power of
90%. Considering a dropout rate of 10%, 440 patients in total were enrolled in the study.
Results with normal distributions were confirmed by a normal distribution test and were
presented as mean (SD) values. Comparison of ages, the baseline of complete blood count, and iron
metabolism parameters between the 2 groups was performed with the t test. Comparison of sexes
and the incidence of adverse reactions between the 2 groups were based on 2-sided Pearson χ2 test.
The 95% CIs for the difference of the changes of hemoglobin level between the 2 groups were
calculated at each time point, and the equivalence was evaluated using the predefined margins of
equivalence (±1 g/dL). Efficacy variables were analyzed on an intention-to-treat basis. If patients
dropped out, missing data were imputed by the last observation carried forward method. For
analysis of adverse events, patients who received at least 1 dose of study drug were included in the
safety population. The threshold of a statistical significance was set as a P < .05. All tests were
performed using Stata statistical software version 11.0 (StataCorp) from March to December 2018.
The full statistical analysis plan is available in Supplement 2.
Results
Participants
Of 530 patients assessed for eligibility, 90 were excluded. The remaining 440 patients (mean [SD]
age, 38.3 [11.7] years) underwent randomization. All patients completed the follow-up until 5 patients
in the vitamin C plus iron group and 4 patients in the iron-only group dropped out after 2 weeks. The
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 4/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
proportion of compliance was 98.2% (432 participants). Figure 1 shows the flow of participants in
this trial.
Of the 440 patients, 426 (96.8%) were women with a mean age of 38.1 years (range, 18-90
years). The most common cause of IDA in women was menorrhagia due to uterine fibroids or
endometriosis, which was found in 389 women (91.3%) in this study. Other reasons included
hemorrhoidal hemorrhage (9 patients [2.1%]), vegetarian diet (7 patients [1.6%]), fecal occult blood
positive due to gastrointestinal bleeding (4 patients [0.9%]), repeated hematuria (1 patients [0.2%]),
and unknown (16 patients [3.8%]). Fourteen of the patients (3.2%) were men with a mean age of
61.4 years (range, 24-80 years), with causes of IDA including hemorrhoidal hemorrhage (5 patients
[35.7%]), bleeding ulcer (4 patients [28.6%]), gastric cancer after surgery (3 patients [21.4%]),
intestinal inflammation (1 patient [7.1%]), and colon cancer after surgery (1 patient [7.1%]). There
were no significant differences between the 2 groups in terms of baseline characteristics (Table 1).
Outcomes
Primary Outcome: Change in Hemoglobin Level
From baseline to 2-week follow-up, the mean (SD) change in hemoglobin level was 2.00 (1.08) g/dL
in the vitamin C plus iron group and 1.84 (0.97) g/dL in the iron-only group (mean between-group
difference, 0.16 g/dL; 95% CI, −0.03 to 0.35 g/dL). For the primary outcome, the change in
hemoglobin level from baseline to 2-week follow-up was contained within the equivalence margin of
1 g/dL (Figure 2); thus, there was no significant difference in hemoglobin level increase between the
2 groups. Similarly, there was no significant difference in the change in hemoglobin level at weeks 4,
6, and 8 (Table 2).
Secondary Outcomes: Changes in RBC Parameters
The median (interquartile range) change in reticulocyte percentage after a 2-week follow-up was
1.03% (0.74%-1.20%) in the vitamin C plus iron group and 1.04% (0.50%-1.20%) in the iron-only
group (between-group difference, 0.11%; 95% CI, 0.10% to 0.32%); the difference was not
Table 1. Baseline Characteristics of Patients by Treatment Group
Mean (SD)
Characteristic Vitamin C plus iron (n = 220) Iron only (n = 220)
Sex, patients, No. (%)
Female 215 (97.7) 211 (95.9)
Male 9 (2.3) 5 (4.1)
Age, y 38.0 (11.0) 39.6 (12.3)
Severity of anemia, patients, No.a
Mild 105 (47.7) 109 (49.5)
Moderate 96 (43.6) 91 (41.4)
Severe 19 (8.6) 20 (9.1)
Hemoglobin, g/dL 8.76 (1.70) 8.82 (1.72)
SI conversion factors: To convert hemoglobin to grams
Red blood cell count, ×106/μL 4.18 (0.58) 4.17 (0.63)
per liter, multiply by 10.0; mean corpuscular volume
3
Mean corpuscular volume, μm 72.85 (9.29) 72.99 (9.00) to femtoliters, multiply by 1.0; mean corpuscular
Mean corpuscular hemoglobin, pg/cell 21.51 (7.71) 22.38 (6.41) hemoglobin concentration to grams per liter, multiply
Mean corpuscular hemoglobin concentration, g/dL 28.72 (1.94) 28.85 (3.19) by 10.0; platelet count to ×109 per liter, multiply by 1.0;
serum ferritin to micrograms per liter, multiply by 1.0;
Red blood cell distribution width coefficient of variation, % 17.82 (2.65) 17.99 (3.16)
serum iron to micromoles per liter, multiply by 0.179;
Reticulocyte, % 1.36 (0.87) 1.45 (0.94)
red blood cell count to ×1012 per liter, multiply by 1;
White blood cell count, /μL 6150 (3900) 5950 (2120) total iron-binding capacity to micromoles per liter,
Platelet count, ×103/μL 314.02 (101.92) 304.52 (99.38) multiply by 0.179; white blood cell count to ×109 per
Serum ferritin, ng/mL 5.89 (4.01) 6.34 (3.69) liter, multiply by 0.001.
a
Serum iron, μg/dL 23.12 (17.77) 25.08 (13.46) Severe anemia is defined as hemoglobin less than or
Iron saturation, % 5.99 (1.97) 6.15 (3.69) equal to 6 g/dL, moderate anemia is defined as
hemoglobin 6 to 9 g/dL, and mild anemia is defined
Total iron-binding capacity, μg/dL 431.01 (50.22) 423.46 (56.37)
as hemoglobin greater than 9 g/dL.
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 5/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
significant. Similar results were obtained at week 4, 6, and 8 showing no significant differences
between the 2 groups (Table 2).
MCV and MCH levels increased slightly (all 95% CIs were positive) in the vitamin C plus iron
group at all follow-up points (Table 2). The increase in MCHC level was higher in the vitamin C plus
iron group at 6 weeks, with mean (SD) changes in MCHC of 3.10 (1.33) g/dL in vitamin C plus iron
group and 2.82 (1.41) g/dL in the iron-only group (between-group difference, 0.28 g/dL; 95% CI,
0.02-0.53 g/dL). Changes of RBC distribution width coefficient of variation showed no significant
difference between the 2 groups at all follow-up points (Table 2).
Iron Metabolism Parameters
Likewise, no difference was observed between groups for the change in serum ferritin level from
baseline to 8-week follow-up. The mean (SD) change was 35.75 (11.52) ng/mL in the vitamin C plus
iron group and 34.48 (9.50) ng/mL in the iron-only group (mean between-group difference, 1.27
ng/mL; 95% CI, −0.70 to 3.24 ng/mL; P = .21). The mean changes in serum iron, transferring
saturation, and TIBC were also comparable between the 2 groups (Table 2).
Adverse Events
The treatment was similarly well tolerated during 8 weeks of follow-up. The most frequent adverse
events were stomach upset, nausea, and acid reflux (Table 3). The proportion of patients with
adverse events was comparable between the 2 groups, 46 (20.9%) in the vitamin C plus iron group
and 45 (20.5%) in the iron-only group after 2 weeks of follow-up (difference, 0.4%; 95% CI, −6.7% to
8.5%; P = .82). After 2 weeks of treatment, 68 patients with adverse events felt better and another
23 patients could tolerate the adverse events. No patients opted out because of adverse events
(Table 3).
Discussion
These findings demonstrate that oral iron supplements alone provide hemoglobin level and iron
storage recovery efficacy equivalent to that of oral iron supplemented with vitamin C in patients with
IDA. To our knowledge, this RCT is the first to evaluate the efficacy and safety of vitamin C
supplements combined with oral iron in patients with IDA.
Oral iron provides an inexpensive and effective means of restoring iron balance in patients with
IDA. Vitamin C is the only dietary constituent other than animal tissue that has been shown to
promote the absorption of nonheme iron in humans.9 Thus, some clinicians, who believe that
vitamin C can improve the efficacy of oral iron and speed up the treatment of anemia, recommend
taking vitamin C supplements combined with oral iron tablets. However, the absolute dose of vitamin
C did not appear to be associated with iron absorption with a complete diet, and the improvement
in iron status was not noticeable,8,11 which was consistent with our findings that oral iron alone
provides efficacy equivalent to that of oral iron with vitamin C. The changes in hemoglobin level were
similar between the 2 groups at weeks 2, 4, 6, and 8. The mean difference in hemoglobin level change
was within the equivalence margin of ±1 g/dL, which is the threshold for clinically significant change
Figure 2. Differences of Changes in Hemoglobin Level Between the Vitamin C Plus Iron Group
and the Iron-only Group
Subgroup Mean difference (95% CI) Favors iron Favors iron plus vitamin C
Hemoglobin at wk 2 vs baseline 0.16 (–0.03 to 0.35)
Hemoglobin at wk 4 vs baseline 0.22 (–0.03 to 0.46)
Hemoglobin at wk 6 vs baseline 0.20 (–0.07 to 0.46)
Hemoglobin at wk 8 vs baseline 0.13 (–0.14 to 0.41) The prespecified equivalence margin for the clinical
–1 –0.5 0 0.5 1 significance of changes in hemoglobin between groups
Difference in hemoglobin level, mean (95% CI), g/dL was 1 g/dL. Error bars indicate 95% CIs.
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 6/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
Table 3. Adverse Events by Treatment Group
Patients, No. (%)
Adverse event Vitamin C plus iron (n = 220) Iron only (n = 220)
Stomach upset, nausea and acid reflux 30 (13.64) 29 (13.18)
Constipation 7 (3.18) 8 (3.64)
Diarrhea 4 (1.82) 3 (1.36)
Xerostomia 3 (1.36) 2 (0.91)
Abdominal pain 2 (0.91) 2 (0.91)
Chest distress 0 1 (0.45)
Table 2. Changes in Red Blood Cell Parameters From Baseline to Weeks 2, 4, 6, and 8 and Iron Metabolism
Parameters from Baseline to Week 8
Mean (SD)
Between-group
Variable Vitamin C plus iron Iron only difference (95% CI)
Change in hemoglobin level, g/dL
2 wk 2.00 (1.08) 1.84 (0.97) 0.16 (−0.03 to 0.35)
4 wk 3.20 (1.32) 2.98 (1.28) 0.22 (−0.03 to 0.46)
6 wk 3.82 (1.37) 3.62 (1.45) 0.20 (−0.07 to 0.46)
8 wk 4.20 (1.47) 4.07 (1.48) 0.13 (−0.14 to 0.41)
Change in reticulocyte percentages
2 wk 1.10 (1.18) 0.99 (1.06) 0.11 (−0.10 to 0.32)
4 wk 0.51 (1.05) 0.40 (1.29) 0.11 (−0.11 to 0.33)
6 wk 0.31 (0.88) 0.16 (0.86) 0.15 (−0.01 to 0.31)
8 wk 0.16 (0.82) 0.02 (0.81) 0.14 (−0.01 to 0.29)
Change in mean corpuscular
volume, μm3
2 wk 7.42 (4.67) 6.14 (4.06) 1.28 (0.46 to 2.09)
4 wk 10.52 (5.36) 9.25 (5.17) 1.27 (0.28 to 2.25)
6 wk 12.80 (5.89) 11.49 (5.84) 1.31 (0.21 to 2.41)
8 wk 14.16 (6.35) 12.72 (6.12) 1.44 (0.27 to 2.60)
Change in mean corpuscular
hemoglobin, pg/cell
2 wk 2.83 (1.77) 2.36 (1.49) 0.47 (0.16 to 0.77)
4 wk 4.87 (2.04) 4.29 (2.28) 0.58 (0.17 to 0.98)
6 wk 6.19 (2.40) 5.69 (2.61) 0.50 (0.03 to 0.97)
8 wk 7.18 (2.70) 6.47 (2.66) 0.71 (0.21 to 1.21)
Change in mean corpuscular
hemoglobin concentration, g/dL
2 wk 0.92 (1.02) 0.82 (0.79) 0.10 (−0.07 to 0.27)
4 wk 2.21 (1.23) 2.04 (1.22) 0.17 (−0.06 to 0.40)
6 weeks 3.10 (1.33) 2.82 (1.41) 0.28 (0.02 to 0.53)
8 weeks 3.47 (1.44) 3.27 (1.47) 0.20 (−0.07 to 0.47)
Change in red blood cell distribution
width coefficient of variation, %
2 wk 4.44 (2.49) 4.53 (2.41) −0.09 (−0.55 to 0.37)
4 wk 3.61 (2.72) 3.49 (3.01) 0.12 (−0.42 to 0.66)
6 wk 2.54 (2.75) 2.22 (3.54) 0.32 (−0.27 to 0.91)
8 wk −0.93 (2.95) −0.53 (3.51) −0.38 (−0.98 to 0.26)
Changes in iron metabolism SI conversion factors: To convert hemoglobin to g/L,
parameters at wk 8 multiply by 10.0; mean corpuscular volume to fL,
Serum ferritin, ng/mL 35.75 (11.52) 34.48 (9.50) 1.27 (−0.70 to 3.24) multiply by 1.0; mean corpuscular hemoglobin
Serum iron, μg/dL 70.11 (30.67) 73.41 (25.47) −3.30 (−8.55 to 1.96) concentration to g/L, multiply by 10; serum ferritin to
Transferrin saturation, % 24.25 (8.84) 27.11 (9.86) −2.86 (−4.61 to −1.11) μg/L, multiply by 1.0; serum iron to μmol/L, multiply by
0.179; total iron-binding capacity to μmol/L, multiply
Total iron-binding capacity, μg/dL −122.63 (27.77) −112.79 (33.80) −9.83 (−15.59 to −4.08)
by 0.179.
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 7/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
recommended by hematologists. Notably, the changes in MCV from baseline to all time points were
slightly greater in the vitamin C plus iron group. MCV is a measure of the mean size of RBCs, and
patients with IDA typically have lower than normal values. The RBC parameters MCH, MCV, and
MCHC are more sensitive and helpful to monitor the response to a treatment.12 However, the aim of
treatment was restoring hemoglobin levels and replenishing iron stores, neither of which was
sensitive to the treatment. Iron metabolism parameters such as serum ferritin, serum iron, iron
saturation, and TIBC at week 8 were comparable between the 2 groups. Adverse events were also
equivalent between the 2 groups.
These results challenge the recommendation to take vitamin C supplements with oral iron to
improve the efficacy and speed up the recovery from anemia. Iron is absorbed as the ferrous salt
(Fe++) in a mildly acidic medium. In theory, vitamin C is helpful in its absorption. However, in light of
the results of this RCT, vitamin C may be less beneficial than reported and expected.
Limitations
This study has some limitations. First, 426 of the included patients were women and 19 were men,
which was an imbalance. Second, the overall follow-up period was not long enough. We found that
iron deficiency anemia relapsed easily if the underlying causes, such as iron-absorption defects and
bleeding, were not investigated and addressed. Some patients came back to our clinic approximately
1 year after the trial ended because of relapse. The time when iron deficiency reappeared again and
whether the proportion of relapse was comparable for the 2 groups were both unknown. Future
research should extend the observation period to obtain more accurate and reliable results.
Conclusions
The findings of this equivalence RCT demonstrate that in patients with IDA, taking oral iron alone was
equivalent to taking oral iron supplemented with vitamin C in improving hemoglobin level and iron
stores. Our results suggest that vitamin C is not essential for patients with IDA.
ARTICLE INFORMATION
Accepted for Publication: August 31, 2020.
Published: November 2, 2020. doi:10.1001/jamanetworkopen.2020.23644
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2020 Li N et al. JAMA
Network Open.
Corresponding Author: Xiaoqin Wang, MD, PhD, Department of Hematology, Huashan Hospital, Fudan
University, 12 Wulumuqi Rd, Shanghai 200024, China (wangxiaoqin@shmu.edu.cn).
Author Affiliations: Department of Hematology, Huashan Hospital, Fudan University, Shanghai, China.
Author Contributions: Dr Wang had full access to all of the data in the study and takes responsibility for the
integrity of the data and the accuracy of the data analysis. Drs Li and Zhao are co–first authors.
Concept and design: Li, Zhao, Chen, Wang.
Acquisition, analysis, or interpretation of data: Wu, Zhang, Liu.
Drafting of the manuscript: Li, Zhao.
Critical revision of the manuscript for important intellectual content: Wu, Zhang, Liu, Chen, Wang.
Statistical analysis: Li, Zhao, Wang.
Obtained funding: Wang.
Administrative, technical, or material support: Li, Wu, Zhang, Liu, Chen, Wang.
Supervision: Zhao, Wang.
Conflict of Interest Disclosures: None reported.
Data Sharing Statement: See Supplement 3.
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 8/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
JAMA Network Open | Hematology Efficacy and Safety of Vitamin C for Iron Supplementation in Adults With Iron Deficiency Anemia
REFERENCES
1. Brugnara C. A hematologic “gold standard” for iron-deficient states? Clin Chem. 2002;48(7):981-982. doi:10.
1093/clinchem/48.7.981
2. Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832-1843. doi:10.1056/NEJMra1401038
3. Centers for Disease Control and Prevention (CDC). Iron deficiency—United States, 1999-2000. MMWR Morb
Mortal Wkly Rep. 2002;51(40):897-899.
4. Moretti D, Goede JS, Zeder C, et al. Oral iron supplements increase hepcidin and decrease iron absorption from
daily or twice-daily doses in iron-depleted young women. Blood. 2015;126(17):1981-1989. doi:10.1182/blood-2015-
05-642223
5. Silberstein L, Anastasi J. In: Hoffman R, Benz E, Heslop H, Weitz J, eds. Hematology: Basic Principles and
Practice. 7th ed. Elsevier Health Sciences; 2017.
6. Sayers MH, Lynch SR, Charlton RW, Bothwell TH, Walker RB, Mayet F. Iron absorption from rice meals cooked
with fortified salt containing ferrous sulphate and ascorbic acid. Br J Nutr. 1974;31(3):367-375. doi:10.1079/
BJN19740045
7. Cook JD, Monsen ER. Vitamin C, the common cold, and iron absorption. Am J Clin Nutr. 1977;30(2):235-241.
doi:10.1093/ajcn/30.2.235
8. Cook JD, Reddy MB. Effect of ascorbic acid intake on nonheme-iron absorption from a complete diet. Am J Clin
Nutr. 2001;73(1):93-98. doi:10.1093/ajcn/73.1.93
9. Hallberg L, Brune M, Rossander L. Effect of ascorbic acid on iron absorption from different types of meals.
studies with ascorbic-acid-rich foods and synthetic ascorbic acid given in different amounts with different meals.
Hum Nutr Appl Nutr. 1986;40(2):97-113.
10. da Silva Rocha D, Capanema FD, Netto MP, Noguiera de Almeida CA, do Carmo Castro Franceschini S,
Lamounier JA. Effectiveness of fortification of drinking water with iron and vitamin C in the reduction of anemia
and improvement of nutritional status in children attending day-care centers in Belo Horizonte, Brazil. Food Nutr
Bull. 2011;32(4):340-346. doi:10.1177/156482651103200405
11. Hunt JR, Gallagher SK, Johnson LK. Effect of ascorbic acid on apparent iron absorption by women with low iron
stores. Am J Clin Nutr. 1994;59(6):1381-1385. doi:10.1093/ajcn/59.6.1381
12. Goddard AF, James MW, McIntyre AS, Scott BB; British Society of Gastroenterology. Guidelines for the
management of iron deficiency anaemia. Gut. 2011;60(10):1309-1316. doi:10.1136/gut.2010.228874
SUPPLEMENT 1.
Trial Protocol
SUPPLEMENT 2.
Statistical Analysis Plan
SUPPLEMENT 3.
Data Sharing Statement
JAMA Network Open. 2020;3(11):e2023644. doi:10.1001/jamanetworkopen.2020.23644 (Reprinted) November 2, 2020 9/9
Downloaded From: https://jamanetwork.com/ on 07/24/2023
You might also like
- CASE STUDY On AnemiaDocument28 pagesCASE STUDY On Anemiapriyanka86% (14)
- Dietary Supplements in Dermatology: A Review of The Evidence For Zinc, Biotin, Vitamin D, Nicotinamide, and PolypodiumDocument9 pagesDietary Supplements in Dermatology: A Review of The Evidence For Zinc, Biotin, Vitamin D, Nicotinamide, and PolypodiumNazihan Safitri AlkatiriNo ratings yet
- PANDU Compilation Final - DocxhhDocument13 pagesPANDU Compilation Final - DocxhhBinal Patel100% (1)
- NCP FatigueDocument3 pagesNCP FatigueKateLayaog100% (2)
- The Antisickling Effects of Some Micronutrients and Antioxidant Vitamins in Sickle Cell Disease ManagementDocument7 pagesThe Antisickling Effects of Some Micronutrients and Antioxidant Vitamins in Sickle Cell Disease ManagementVeraNo ratings yet
- RCT Irondose AdultsDocument8 pagesRCT Irondose AdultsCristobal MendozaNo ratings yet
- A Study of Efficacy and Safety of Intravenous Iron Sucrose For The Treatment of Moderate Anaemia in Antenatal Women in South IndiaDocument6 pagesA Study of Efficacy and Safety of Intravenous Iron Sucrose For The Treatment of Moderate Anaemia in Antenatal Women in South Indianazzz12No ratings yet
- Seminar 4Document8 pagesSeminar 4Dessy Erlyani Mugita SariNo ratings yet
- Drueke AnemT KDIGO Standpoint 2019Document23 pagesDrueke AnemT KDIGO Standpoint 2019A9 El-EbidiNo ratings yet
- Guideline Exposicion A Hierro 2005Document18 pagesGuideline Exposicion A Hierro 2005Baltazar Pérez AlfaroNo ratings yet
- Comparative Study On Efficacy, Tolerability, and Cost of Different Iron Supplements Among Antenatal Women With Iron-Deficiency AnemiaDocument8 pagesComparative Study On Efficacy, Tolerability, and Cost of Different Iron Supplements Among Antenatal Women With Iron-Deficiency AnemiaAjay DNo ratings yet
- JurnalDocument8 pagesJurnaldhea handyaraNo ratings yet
- Houston 2018 Efficacy of Iron Supplementation OnDocument9 pagesHouston 2018 Efficacy of Iron Supplementation OnQonita RachmahNo ratings yet
- Molecular Aspects of Medicine: SciencedirectDocument9 pagesMolecular Aspects of Medicine: SciencedirectMostafa hosnyNo ratings yet
- Ijrcog 13010oDocument5 pagesIjrcog 13010oEllen KopaNo ratings yet
- Giordano2021 Article OralHigh-doseSucrosomialIronVsDocument7 pagesGiordano2021 Article OralHigh-doseSucrosomialIronVsPopaNo ratings yet
- Antioxidant Enzymes and Oxidative Stress in The Erythrocytes of Iron Deficiency Anemic Patients Supplemented With VitaminsDocument7 pagesAntioxidant Enzymes and Oxidative Stress in The Erythrocytes of Iron Deficiency Anemic Patients Supplemented With VitaminsAndyk Strapilococus AureusNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyMostafa hosnyNo ratings yet
- Proton Pump Inhibitor and Histamine 2 Receptor Antagonist Use and Vitamin B DeficiencyDocument8 pagesProton Pump Inhibitor and Histamine 2 Receptor Antagonist Use and Vitamin B DeficiencyjcNo ratings yet
- Jurnal Pemberian Terapi Mingguan Besi-Asam Folat Dengan Atau Tanpa B12 Pada Remaja: RCTDocument8 pagesJurnal Pemberian Terapi Mingguan Besi-Asam Folat Dengan Atau Tanpa B12 Pada Remaja: RCTDyah FiharjatinNo ratings yet
- Oral Iron Supplementation in Iron-Deficient Women-How Much and How OftenDocument9 pagesOral Iron Supplementation in Iron-Deficient Women-How Much and How Oftenshofa nur rahmannisaNo ratings yet
- Jkms 29 965Document9 pagesJkms 29 965M AbhiNo ratings yet
- Randomized Controlled Trial of Vitamin D Supplementation in Older People To Optimize Bone HealthDocument11 pagesRandomized Controlled Trial of Vitamin D Supplementation in Older People To Optimize Bone HealthsmartgalgemscribdNo ratings yet
- Vitmain B12 Asseverity and Prognostic Marker in Chronic Liver DiseaseDocument7 pagesVitmain B12 Asseverity and Prognostic Marker in Chronic Liver DiseaseIJAR JOURNALNo ratings yet
- Rajkumari Linthoingambi - MeeDocument6 pagesRajkumari Linthoingambi - Meechaitanya suryawanshiNo ratings yet
- Alternate Day Versus Consecutive Day Oral Iron Supplementation - 2023 - EclinicDocument11 pagesAlternate Day Versus Consecutive Day Oral Iron Supplementation - 2023 - Eclinicronaldquezada038No ratings yet
- Ijtk 11 (1) 78-80Document3 pagesIjtk 11 (1) 78-80ZordaaaNo ratings yet
- DMSO 450738 Correlation Between Serum Vitamin e and Homa Ir in PatientsDocument11 pagesDMSO 450738 Correlation Between Serum Vitamin e and Homa Ir in Patientsgabe_babe0010No ratings yet
- Saudi Journal of Biological SciencesDocument6 pagesSaudi Journal of Biological SciencesEstefaníaNo ratings yet
- Special Report Diagnosis and Management of Iron Deficiency in CKD: A Summary of The NICE Guideline Recommendations and Their RationaleDocument11 pagesSpecial Report Diagnosis and Management of Iron Deficiency in CKD: A Summary of The NICE Guideline Recommendations and Their RationaledrnattoNo ratings yet
- Pathological Ossification High Dose D and CADocument7 pagesPathological Ossification High Dose D and CA0xcffaaNo ratings yet
- Bocchio Et Al 2022, A RCT Pilot Study To Compare Efficacy of Different Iron FormulationsDocument6 pagesBocchio Et Al 2022, A RCT Pilot Study To Compare Efficacy of Different Iron Formulationsedo adimastaNo ratings yet
- Aniket Publication EditedDocument10 pagesAniket Publication EditedAniket TripathiNo ratings yet
- Effect of Weekly Iron Supplementation On Iron Indices in Pregnant WomenDocument4 pagesEffect of Weekly Iron Supplementation On Iron Indices in Pregnant WomeneditorijmrhsNo ratings yet
- 10 1001@jama 2019 11889Document10 pages10 1001@jama 2019 11889Andreea GociuNo ratings yet
- SelviDocument81 pagesSelvichaitanya suryawanshiNo ratings yet
- Two Case Reports of Desensitization in Patients With Hypersensitivity To IronDocument4 pagesTwo Case Reports of Desensitization in Patients With Hypersensitivity To Irondleal12_357008892No ratings yet
- Iron Supplementation in PregnaDocument3 pagesIron Supplementation in PregnaYoki VirgoNo ratings yet
- Ijmrhs Vol 2 Issue 4Document321 pagesIjmrhs Vol 2 Issue 4editorijmrhsNo ratings yet
- Obesity Medicine: Irina A. Lapik, Alexey V. Galchenko, Kamilat M. Gapparova TDocument9 pagesObesity Medicine: Irina A. Lapik, Alexey V. Galchenko, Kamilat M. Gapparova TMakbule ERÇAKIRNo ratings yet
- Pengaruh Asupan Fe Vitamin A Vitamin B12 Dan VitamDocument8 pagesPengaruh Asupan Fe Vitamin A Vitamin B12 Dan VitamNaura Laras Rif'atiNo ratings yet
- The Relationship Between Depression and Serum Ferritin Level - Shariatpanaahi 2007Document4 pagesThe Relationship Between Depression and Serum Ferritin Level - Shariatpanaahi 2007Julio JuarezNo ratings yet
- Study of Vitamin B12 Deficiency and Its Relation With Metformin Treatment Among Diabetics in Prince Rashid Hospital PDFDocument7 pagesStudy of Vitamin B12 Deficiency and Its Relation With Metformin Treatment Among Diabetics in Prince Rashid Hospital PDFGladiatorx SuperbNo ratings yet
- Journal 2Document8 pagesJournal 2nana nurdahliaNo ratings yet
- Role of Vitamin D in Dental Health: A ReviewDocument4 pagesRole of Vitamin D in Dental Health: A ReviewArka SahaNo ratings yet
- Jurnal Anemia DefisiensiDocument3 pagesJurnal Anemia DefisiensiAirin Nurul Syahdiva RamliNo ratings yet
- Fruit VegetableDocument10 pagesFruit VegetableEzhaty Diah RianiNo ratings yet
- Iron Isomaltoside Monofer Final April 2011 Amended 030511 For WebsiteDocument8 pagesIron Isomaltoside Monofer Final April 2011 Amended 030511 For WebsiteUmaima faizNo ratings yet
- Criteria and Recommendations For Vitamin C Intake: Special CommunicationDocument9 pagesCriteria and Recommendations For Vitamin C Intake: Special CommunicationhasdiniNo ratings yet
- 64e1f17f3847ecc3b3d0c20aa424cf09Document1 page64e1f17f3847ecc3b3d0c20aa424cf09RismaAyuSaraswatiNo ratings yet
- Comparison of Therapeutic Efficacy of Ferrous Ascorbate and Iron Polymaltose-EditedDocument6 pagesComparison of Therapeutic Efficacy of Ferrous Ascorbate and Iron Polymaltose-EditedmariskaNo ratings yet
- Anemia and Iron Deficiency in Gastrointestinal and Liver ConditionsDocument19 pagesAnemia and Iron Deficiency in Gastrointestinal and Liver ConditionsOcha24 TupamahuNo ratings yet
- Vitamin A Dan Zinc TBDocument13 pagesVitamin A Dan Zinc TBTarafainy BasalamahNo ratings yet
- Efficacy and Tolerability of Oral Iron Protein Succinylate: A Systematic Review of Three Decades of ResearchDocument12 pagesEfficacy and Tolerability of Oral Iron Protein Succinylate: A Systematic Review of Three Decades of Researchali laftaNo ratings yet
- Association Between Metformin Dose and VitaminDocument8 pagesAssociation Between Metformin Dose and VitaminMaria Bernardino CorrêaNo ratings yet
- Impact of Iron, Folate and Vitamin CDocument3 pagesImpact of Iron, Folate and Vitamin CRiyun RiyaniNo ratings yet
- Study of Vitamin B12 Levels in Patient With Type 2 Diabetes MellitusDocument5 pagesStudy of Vitamin B12 Levels in Patient With Type 2 Diabetes MellitusIJAR JOURNALNo ratings yet
- Effects of Vitamin A, Vitamin A Plus Zinc, and Multiple Micronutrients On Anemia in Preschool Children in Chongqing, ChinaDocument10 pagesEffects of Vitamin A, Vitamin A Plus Zinc, and Multiple Micronutrients On Anemia in Preschool Children in Chongqing, ChinaFentiNo ratings yet
- Prevalenceof Vitamin b12 Deficiency in Highersocio-Economical Class Ofbhuj-KutchDocument3 pagesPrevalenceof Vitamin b12 Deficiency in Highersocio-Economical Class Ofbhuj-KutchIOSR Journal of PharmacyNo ratings yet
- ELZEN Et Al-2008-Alimentary Pharmacology & Therapeutics Vit B12Document7 pagesELZEN Et Al-2008-Alimentary Pharmacology & Therapeutics Vit B12jcNo ratings yet
- Intravenous Iron For Iron Deficiency Anaemia Full ReportDocument124 pagesIntravenous Iron For Iron Deficiency Anaemia Full ReportSitha DeviNo ratings yet
- Iron Deficiency Anemia in PregnancyDocument6 pagesIron Deficiency Anemia in PregnancyAjay DNo ratings yet
- Anemia Mini ProjectDocument7 pagesAnemia Mini Projectمحمد الزراريNo ratings yet
- Blood & Blood ProductsDocument126 pagesBlood & Blood ProductsdrprasadingleyNo ratings yet
- Choose The Correct Answer For Question (1 - 86)Document13 pagesChoose The Correct Answer For Question (1 - 86)Ahmed Fouad100% (2)
- DRUG STUDY For DR Rotation OGHDocument11 pagesDRUG STUDY For DR Rotation OGHSamantha TangubNo ratings yet
- Aplastic AnemiaDocument21 pagesAplastic AnemiaJennifer DixonNo ratings yet
- Design Thinking Process - Phạm Thị Ngọc Ánh - 1915550703Document2 pagesDesign Thinking Process - Phạm Thị Ngọc Ánh - 1915550703Ngoc Anh PhamNo ratings yet
- 506 Qs Mohammad Mordi @NAJMDocument115 pages506 Qs Mohammad Mordi @NAJMElsayedNo ratings yet
- Differential Diagnosis of Microcytic Anemia PDFDocument5 pagesDifferential Diagnosis of Microcytic Anemia PDFayms99No ratings yet
- Arensman - Pediatric SurgeryDocument486 pagesArensman - Pediatric Surgeryedrons0% (1)
- SURGERY History and Counselling NotesDocument27 pagesSURGERY History and Counselling NotesaminaNo ratings yet
- FMStudent OME VideoGuideForFMDocument4 pagesFMStudent OME VideoGuideForFMFiorellaBeatriz100% (1)
- Anemia in CKD and DialysisDocument38 pagesAnemia in CKD and Dialysisapoorva jainNo ratings yet
- Immunohematology ASCPi Review Booklet (Part 1)Document22 pagesImmunohematology ASCPi Review Booklet (Part 1)Mark Justin OcampoNo ratings yet
- Physical Assessment and Review of Systems Areas Assesse D Night 1 Night 2 Problem IdentifiedDocument9 pagesPhysical Assessment and Review of Systems Areas Assesse D Night 1 Night 2 Problem IdentifiedAsniah Hadjiadatu AbdullahNo ratings yet
- Hematology QuestionsDocument171 pagesHematology QuestionsVikkineshwaran Siva SubramaniamNo ratings yet
- How I Treat Anemia in Pregnancy: Iron, Cobalamin, and FolateDocument11 pagesHow I Treat Anemia in Pregnancy: Iron, Cobalamin, and FolateAgungBudiPamungkasNo ratings yet
- MCQ of HematologyDocument37 pagesMCQ of Hematologyalemante92% (13)
- Clinical Significance of Immature Reticulocyte Fraction Determined by Automated Reticulocyte CountingDocument5 pagesClinical Significance of Immature Reticulocyte Fraction Determined by Automated Reticulocyte CountingAngelNo ratings yet
- Module 3 Special Hematologic Examination 1Document8 pagesModule 3 Special Hematologic Examination 1Pauline Louise S. DURANNo ratings yet
- Group 5 Bahasa Inggris 2Document12 pagesGroup 5 Bahasa Inggris 2Desri AjengNo ratings yet
- Fefol SPC Mhra Con1372742133502Document5 pagesFefol SPC Mhra Con1372742133502danandonieNo ratings yet
- Hydronephrosis Fred LuceDocument69 pagesHydronephrosis Fred LuceKMNo ratings yet
- Hematology Study GuideDocument2 pagesHematology Study Guideclower112No ratings yet
- Hematological DisordersDocument5 pagesHematological DisordersRash PaltepNo ratings yet
- Neetpg LRR Pathology Part 2 PDFDocument92 pagesNeetpg LRR Pathology Part 2 PDFMaheshNo ratings yet
- GARCIA, JESSIE POCHOLO - JournalAnalysisDocument8 pagesGARCIA, JESSIE POCHOLO - JournalAnalysisJojo GarciaNo ratings yet
- MRCPCH DhanDocument26 pagesMRCPCH DhanRajiv KabadNo ratings yet