Professional Documents
Culture Documents
Chan 1997
Chan 1997
Uploaded by
Sree BanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chan 1997
Chan 1997
Uploaded by
Sree BanCopyright:
Available Formats
THE LANCET
Articles
Randomised trial of eradication of Helicobacter pylori
before non-steroidal anti-inflammatory drug therapy to prevent
peptic ulcers
Francis K L Chan, Joseph J Y Sung, S C Sydney Chung, K F To, M Y Yung, Vincent K S Leung, Y T Lee,
Cynthia S Y Chan, Edmund K M Li, Jean Woo
Summary Introduction
Peptic ulcer disease caused by non-steroidal anti-
Background Helicobacter pylori infection is common in
inflammatory drug (NSAID) therapy is a health-care
patients with peptic ulcers caused by the use of non-
issue worldwide. In the UK, about 1·5 million people
steroidal anti-inflammatory drugs (NSAIDs). But the
aged over 60 years take NSAIDs at any one time.1
pathogenic role of H pylori in this disease is controversial.
Patients who take NSAIDs have a four-fold to six-fold
We studied the efficacy of eradication of H pylori in the increased risk of developing peptic ulcers.2,3 Every year,
prevention of NSAID-induced peptic ulcers. about 12 000 ulcer complications occur in the UK as a
Methods We recruited patients with musculoskeletal pain result of NSAID therapy.4 Although chronic NSAID
who required NSAID treatment. None of the patients had users are at increased risk of ulcer disease, those who take
previous exposure to NSAID therapy. Patients who had intermittent short-course NSAID therapy are also at risk
H pylori infection but no pre-existing ulcers on endoscopy of the disease. Most ulcer complications tend to develop
in the first few weeks of therapy, particularly among
were randomly allocated naproxen alone (750 mg daily) for
individuals without previous exposure to NSAIDs.3,5 The
8 weeks or a 1-week course of triple therapy (bismuth
risk of ulcer complications is greatest among the elderly
subcitrate 120 mg, tetracycline 500 mg, metronidazole
and patients with comorbid disease.2,3 Up to 60% of ulcer
400 mg, each given orally four times daily) before
complications occur without antecedent symptoms.6 The
administration of naproxen (750 mg daily). Endoscopy was annual direct medical costs associated with these
repeated after 8 weeks of naproxen treatment or when complications is about $3·9 billion in the USA.7
naproxen treatment was stopped early because of bleeding Previous studies have shown that prophylactic therapy
or intractable dyspepsia. All endoscopic examinations were with misoprostol, famotidine, and omeprazole is effective
done by one endoscopist who was unaware of treatment in the prevention of NSAID-induced ulcers.8–10 However,
assignment. The primary endpoint was the cumulative rate these prophylactic regimens are very expensive.11 Cost-
of gastric and duodenal ulcers. effective measures to prevent NSAID-induced ulcer
disease are not available.
Findings 202 patients underwent endoscopic screening for
H pylori is present in about 50% of patients with
enrolment in the trial, and 100 eligible patients were
NSAID-associated ulcer disease.12,13 Studies of the
randomly assigned treatment. 92 patients completed the
interaction between H pylori infection and NSAIDs have
trial (47 in the naproxen group, 45 in the triple-therapy reported conflicting findings.12–26 Whether H pylori
group). At 8 weeks, H pylori had been eradicated from no infection increases the risk of ulcer development in users
patients in the naproxen group and 40 (89%) in the triple- of NSAIDs is not known.
therapy group (p<0·001). 12 (26%) naproxen-group The aim of our study was to investigate whether
patients developed ulcers: five had ulcer pain and one eradication of H pylori before the start of NSAID therapy
developed ulcer bleeding. Only three (7%) patients on reduced the occurrence of gastroduodenal ulcers in
triple therapy had ulcers, and two of these patients had patients without previous exposure to NSAIDs. We
failure of H pylori eradication (p=0·01). Thus, 12 (26%) postulated that underlying infection with H pylori
patients with persistent H pylori infection but only one increases the predisposition of NSAID users to develop
(3%) with successful H pylori eradication developed ulcers ulcers. Thus, eradication of H pylori could protect these
with naproxen (p=0·002). patients from developing peptic ulcers.
Interpretation Eradication of H pylori before NSAID therapy
reduces the occurrence of NSAID-induced peptic ulcers. Methods
Patients with musculoskeletal disorders that required NSAID
therapy were eligible for the study. We recruited patients from
Lancet 1997; 350: 975–79 the medical outpatient clinic at Prince of Wales Hospital, Hong
Kong, and from the family clinic of the Chinese University of
Hong Kong. We excluded patients if they: were younger than 18
Departments of Medicine (F K L Chan MRCP, J J Y Sung MD, years; had been previously exposed to NSAIDs (including
V K S Leung MRCP, Y T Lee MRCP, E K M Li FRCP, J Woo MD), Surgery aspirin) for longer than 1 month; had taken NSAIDs (including
(S C S Chung MD, M Y Yung BN), and Anatomical and Cellular aspirin), antiulcer drugs, steroid, anticoagulants, or cytotoxic
Pathology (K F To FRCPA), Prince of Wales Hospital, Shatin, New agents in the previous 8 weeks; had received antihelicobacter
Territories, Hong Kong; and Community and Family Medicine, The therapy; had a history of peptic ulcer disease or gastric surgery;
Chinese University of Hong Kong, Hong Kong (C S Y Chan MD) or if they had renal impairment (serum creatinine >200 mol/L).
Correspondence to: Dr Francis K L Chan Eligible patients were invited to take part in the study and were
Vol 350 • October 4, 1997 975
THE LANCET
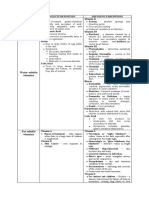
202 eligible patients underwent Naproxen alone Triple therapy plus p
endoscopic screening (n=47) naproxen (n=45)
Men/women 15/32 11/34 0·43*
93 excluded
Median (range) age in years 61 (40–84) 64 (33–79) 0·50†
H pylori negative (91)
Ulcers (2) Current smokers 14 (30%) 12 (27%) 0·74*
Alcohol use 2 (4%) 2 (4%) 1·00‡
109 positive for
Osteoarthritis/rheumatoid 36/2/9 37/2/6 0·51*
H pylori arthritis/other
Comorbid illness§ 27 (57%) 31 (69%) 0·26*
9 refusals after
first endoscopy Stomach
Subepithelial haemorrhage 0 1 1·00‡
Erosions 2 (4%) 7 (16%) 0·09‡
100 patients randomised Duodenum
Subepithelial haemorrhage 0 0 1·00‡
Erosions 1 1 1·00‡
50 naproxen 50 naproxen plus *Pearson 2 test. †Mann-Whitney U test. ‡Fisher’s exact test. §Comorbid illness
includes cerebrovascular accident, hypertension, ischaemic heart disease, heart
alone triple therapy
failure, diabetes mellitus, chronic obstructive airway disease, and liver cirrhosis.
11 (23%) patients in the naproxen group and 15 (33%) in the triple-therapy group
had more than one disease. No patients took aspirin or antacids before the study.
5 default follow-up
3 default follow-up Did not need naproxen (2) Table 1: Baseline characteristics of patients
Refusal (2) Refusal (1)
Intolerance to Intolerance to naproxen (1) intervals for 8 weeks. Dologesic (propoxyphene napsylate 50 mg,
naproxen (1) Intolerance to triple paracetamol 325 mg) was given to patients for temporary
therapy (1) pain relief during triple therapy, or as an adjuvant therapy to
naproxen if requested by patients.
A research nurse interviewed each patient about their smoking
habits, alcohol consumption, drug history, and concurrent
47 patients 45 patients medical illness. Complete blood count and renal function tests
were carried out. We assessed drug compliance by counting
unused tablets. Endoscopy was repeated by the same
endoscopist after 8 weeks of naproxen therapy to document
47 H pylori 40 H pylori 5 H pylori gastroduodenal ulcers. H pylori status was reassessed by
positive negative positive repeating antral biopsies. We defined eradication of H pylori
as negative rapid urease test and absence of the bacteria on
histology. The endoscopist and pathologist were unaware of the
treatment allocation and previous endoscopic or histological
12 with peptic ulcers 1 with 2 with findings. Those patients who developed intractable dyspeptic
peptic ulcers peptic ulcers symptoms that required the early termination of naproxen, or
who had gastrointestinal haemorrhage (defined as haematemesis
Trial profile or melaena) underwent endoscopy before 8 weeks.
The primary endpoint was the cumulative rate of gastric and
given a detailed explanation. Those who gave their informed
duodenal ulcers. All patients who returned for follow-up
written consent to take part in the study underwent upper-
endoscopy were included in the intention-to-treat analysis. We
gastroinestinal endoscopy. The study protocol was approved by
did a per-protocol analysis for those patients who took more than
the ethics committee of the Chinese University of Hong Kong.
60% of the prescribed naproxen, or at least 5 days of the triple
All endoscopic assessment was done by a one endoscopist
therapy in patients on antihelicobacter treatment. We also
(FKLC) to eliminate between-observer variation. We defined a
compared the clinical outcome of patients with or without
peptic ulcer as a circumscribed mucosal break 5 mm or more in
successful eradication of H pylori infection.
diameter with a well-defined ulcer crater, whereas smaller or
We estimated the sample size based on our previous study,
superficial lesions were classified as erosions. Ulcer size was
which showed an ulcer prevalence of 33% in NSAID users who
measured by standard Olympus biopsy forceps (Olympus FG-
were infected with H pylori compared with 6% in NSAID users
25K), with the fully open instrument equivalent to 5 mm. We
who did not have H pylori infection.19 To achieve a statistical
excluded patients with ulcers detected at baseline endoscopy.
power of 85%, with an ␣ error of 5%, 45 patients were needed in
Five random biopsy specimens were taken from the antrum;
each treatment group. Under the assumption of a drop-out rate
two specimens were used for the rapid urease test (CLO test,
of 10% in each group, we calculated that 100 patients were
Delta West, Bentley, Western Australia) and three samples were
required in the study. The results of the two treatment groups
sent for histological assessment with haematoxylin and eosin
were compared by two-tailed Fisher’s exact test, Pearson 2 test,
stain and Warthin-Starry stain. The histological assessment was
and Mann-Whitney U test. A p value less than 0·05 was taken
done by one pathologist (KFT) who was unaware of treatment
as significant.
assignment. A patient was judged to be infected with H pylori if
they had a positive rapid urease test that was confirmed by the
histology. A positive rapid urease test alone was not deemed Results
sufficient for the diagnosis of H pylori infection. 202 consecutive patients agreed to take part and
Patients who were confirmed to have H pylori infection and underwent endoscopy for enrolment in the trial. Of these
did not have an ulcer at baseline endoscopy were randomly patients, 91 were not infected by H pylori, two had ulcers
assigned to one of two treatment groups. We used a list of
at initial endoscopy, and nine patients with H pylori
computer-generated random numbers for treatment assignment.
Patients were assigned naproxen 750 mg daily in three divided
refused to participate in the study after endoscopy. 100
doses at 8 h intervals for 8 weeks, or a 1-week course of triple patients were randomly assigned treatment in two groups
therapy (bismuth subcitrate 120 mg, tetracycline 500 mg, and of 50. Eight withdrew after randomisation and defaulted
metronidazole 400 mg, each given orally four times daily) follow-up (naproxen group: one refused to undergo
followed by naproxen 750 mg daily in three divided doses at 8 h second endoscopy, one refused to take part, and one
976 Vol 350 • October 4, 1997
THE LANCET
Naproxen alone Triple therapy plus p Naproxen alone Triple therapy plus p
(n=47) naproxen (n=45) (n=43) naproxen (n=38)
Total number of ulcers 12 (26%) 3 (7%) 0·01* Total number of ulcers 12 (28%) 2 (5%) 0·007*
Gastric 9 3 Gastric 9 2 0·04*
Duodenal 2 0 Duodenal 2 0
Gastric and duodenal 1 0 Gastric and duodenal 1 0
Symptomatic ulcers 6 (13%) 1 (2%) 0·11† Symptomatic ulcers 6 (14%) 1 (3%)† 0·11‡
Pain 5 1‡ Pain 5 1
Bleeding 1 0 Bleeding 1 0
Stomach *Pearson 2 test. †Failure to eradicate H pylori infection. ‡Fisher’s exact test.
Subepithelial haemorrhage 6 2 0·27† Table 3: Per-protocol analysis
Erosions 15 18 0·55*
Duodenum
only one (2·5%) patient developed ulcer after successful
Subepithelial haemorrhage 1 0 1·00†
Erosions 4 6 0·52† eradication, whereas 12 (26%) patients infected with
*Pearson 2 test. †Fisher’s exact test. ‡Failure to eradicate H pylori infection. H pylori developed ulcers with naproxen (p=0·002). Of
Table 2: Intention-to-treat analysis the 15 patients who developed peptic ulcers in both
treatment groups, 11 (73%) were older than 60 years
patient had abdominal pain after taking naproxen; triple (range 49–84 years). Comorbid disease was present in 11
therapy plus naproxen group: adequate pain relief with (73%) patients (seven had more than one disease).
dologesic in two, one refused to take part, one patient The per-protocol analysis included 43 naproxen-group
with palpitation after taking naproxen, and one patient patients and 38 triple-therapy patients (table 3). Four
with intolerance to triple therapy). 92 patients completed patients in the naproxen group took less than 60% of
the study: 47 in the naproxen group and 45 in the triple- the drug prescribed: one had adequate pain relief with
therapy group. dologesic alone, one did not have adequate pain relief
The flow of patients is shown in the trial profile. The with naproxen, and two had dyspeptic symptoms that
two groups were well matched for age, sex, smoking and disappeared when the frequency of naproxen intake was
drinking habits, and underlying arthritis (table 1). In the reduced. In the triple-therapy group, three patients took
triple-therapy group, there were more patients with the antibiotics for less than 5 days because of gastro-
comorbid illness and gastric erosions were more frequent intestinal upset, and four did not take naproxen regularly
on baseline endoscopy than in the naproxen group, but (two had adequate pain relief with dologesic alone, one
the difference was not significant. 41 patients completed found naproxen ineffective, and one complained of leg
at least 5 days of the prescribed 1-week triple therapy. cramps and blurred vision after taking naproxen). These
40 (89%) triple-therapy patients had successful patients were excluded from the analysis. The cumulative
eradication of H pylori, versus none in the naproxen rate of gastric ulcers was significantly lower in patients
group (p<0·001). pretreated with triple therapy (p=0·04).
The cumulative rate of gastric and duodenal ulcers
after 8 weeks of treatment is shown in table 2. In the Discussion
intention-to-treat analysis, 12 (26%) patients in the The interaction between H pylori infection and use of
naproxen group compared with three (7%) in the triple- NSAIDs in the pathogenesis of peptic ulcer is unclear.
therapy group developed peptic ulcers (p=0·01). The size Most of the available data is from cross-sectional studies
of ulcers ranged from 5 mm to 10 mm (mean diameter of based on chronic NSAID users, with conflicting
6 mm). Seven patients had more than one ulcer; one results.12–20 Two studies reported a higher rate of H pylori
patient had both gastric and duodenal ulcers. In the in NSAID users with gastroduodenal lesions than in
naproxen group, six of the 12 patients developed those with normal mucosa.13,20 Others found significantly
symptomatic ulcers that required early termination of more ulcers in NSAID users who were H pylori positive
naproxen: five had intractable dyspepsia (two developed than in users not infected with H pylori.12,16,19 But these
ulcers after 2 weeks of naproxen, three had ulcers at findings were not confirmed by other investigators.14,15,17,18
5–7 weeks), and one had ulcer bleeding during week 7. Such conflicting findings arise from different study
Of the three patients who developed ulcers in the triple- designs and outcome measures—for example, they either
therapy group, two had failure of H pylori eradication assessed the rate of H pylori in NSAID users with or
(one completed triple therapy but developed intractable without mucosal damage13,14 or, conversley, the rate of
dyspepsia and an ulcer was detected after 1 week of mucosal damage in NSAID users with and without H
naproxen, and the other patient took triple therapy for pylori.15–19 Thus, direct comparison of results is difficult.
only 2 days because of gastrointestinal upset and an ulcer These cross-sectional studies do not, therefore, provide
was found on follow-up endoscopy at 8 weeks). Even definite evidence for or against a link between H pylori
when we assumed that all defaulters (except those who and NSAIDs in the development of peptic ulcers.
responded adequately to dologesic alone) were treatment Most of the few published prospective trials did not
failures, pretreatment with antihelicobacter therapy still indicate that H pylori is a risk factor for NSAID-induced
significantly reduced the rate of ulcers: 15 patients with gastroduodenal damage.21–25 Three studies reported that
ulcers in the naproxen group versus six in the triple- H pylori did not affect the severity of gastroduodenal
therapy group (p=0·048). One patient in each group had damage after short-term administration of NSAIDs.21–23
epigastric pain before 8 weeks, but endoscopy did not However, the data were mostly derived from studies that
reveal any ulcers. Other endoscopic lesions were also involved small numbers of young healthy volunteers. Any
detected (subepithelial haemorrhage and erosions), but interaction between H pylori and NSAIDs could have
there was no significant between-group differences. been obscured by the small number of individuals
Comparison of the rate of ulcers in patients with and included with low event rates in low-risk groups. Two
without successful eradication of H pylori, showed that long-term longitudinal studies of chronic NSAID users
Vol 350 • October 4, 1997 977
THE LANCET
gave conflicting results.25,26 Kim and colleagues25 reported factor for NSAID-induced ulcer disease. Coprescription
no significant increase in the rate of gastroduodenal of antiulcer prophylactic drugs can reduce the rate of
ulcers among chronic NSAID users with H pylori NSAID ulcers, but the high cost of such treatment
infection; patients with erosions detected at baseline were prevents its widespread use. Although it would be costly
excluded in the study. By contrast, Taha and colleagues26 and impractical to carry out endoscopy on every patient
found that patients with H pylori-positive duodenal before administration of NSAID, H pylori status can be
erosions were more likely than patients who were not easily determined by an office-based serology test.
infected with H pylori to develop ulcers during NSAID Determination of H pylori and eradication in infected
treatment. Selective recruitment of chronic users without patients should be recommended before the start of
complications may introduce bias, since those susceptible NSAID therapy.
individuals could have dropped out early because of
NSAID intolerance or complications.1,3 Contributors
The best evidence of a positive interaction between Francis K L Chan, Joseph J Y Sung, S C Sydney Chung, and Jean Woo
were responsible for the original design of the study. Francis K L Chan,
H pylori and NSAIDs in the pathogenesis of ulcer would Y T Lee, Vincent K S Leung, and Cynthia S Y Chan coordinated the
be obtained by investigating the effects of H pylori study. Data collection, statistical analysis, and independent outcome
eradication on the occurrence of NSAID-induced ulcers. assessment were conducted by Francis K L Chan, K F To, M Y Yung,
and Vincent K S Leung. The manuscript was edited by Joseph J Y Sung,
Seppala and co-workers27 observed that gastric ulcer S C Sydney Chung, Edmund K M Li, and Jean Woo. All the authors
relapse seemed to be reduced in a small group of NSAID contributed to the execution of the study and the writing of the paper.
users after eradication of H pylori. A prospectve study
by Bianchi and colleagues28 assessed the efficacy of Acknowledgments
We thank W K Leung, Henry L Y Chan, Justin Wu, W Y So, Teresa
amoxicillin-omeprazole dual therapy on the healing and Wong, Gabriel Yip, Thomas S T Li, and Lily Saw for recruitment of
recurrence of ulcers in chronic NSAID users who were patients and the nursing staff of the Endoscopy Centre, Prince of Wales
infected with H pylori. They found no significant benefit Hospital, for their generous support.
although there was a numerical trend towards a higher
rate of ulcer recurrence in patients with H pylori infection. References
However, the rate of H pylori eradication was very low, 1 Langman MJS. Anti-inflammatory drugs and the gut-ulcerative
and their result was further limited by the small number damage and protection from cancer. Excerpta Medica 1995; 72: 1–8.
of patients with ulcer recurrence and the use of different 2 Fries JF, Williams CA, Bloch DA, Michel BA. Nonsteroidal anti-
NSAIDs with variable ulcerogenic potentials. inflammatory drug-associated gastropathy: incidence and risk factors
model. Am J Med 1991; 91: 213–22.
Our present study is the first prospective randomised 3 Langman MJS, Weil J, Wainwright P, et al. Risks of bleeding peptic
trial to look at whether eradication of H pylori before the ulcer associated with individual non-steroidal anti-inflammatory drugs.
start of NSAID therapy reduces the subsequent risk of Lancet 1994; 343: 1075–78.
ulcer formation. Our findings establish a pathogenetic 4 Hawkey CJ. Non-steroidal anti-inflammatory drug gastropathy: causes
and treatment. Scand J Gastroenterol 1996; 31 (suppl 220): 124–27.
role for H pylori in the development of NSAID-induced 5 Gabriel SE, Jaakkimainen L, Bombardier C. Risks for serious
ulcers, in that prophylactic eradication of H pylori gastrointestinal complications related to the use of non-steroidal anti-
significantly reduced the 8-week cumulative rate of inflammatory drugs: a meta-analysis. Ann Intern Med 1991; 115:
787–96.
NSAID ulcers by almost four-fold. The degree of
6 Somerville K, Faulkner G, Langman MJS. Non-steroidal anti-
protection conferred by eradication of H pylori was inflammatory drugs and bleeding peptic ulcer. Lancet 1986; i: 452–54.
similar to that provided by acid-suppression drugs.9,10 The 7 Bloom BS. Direct medical costs of disease and gastrointestinal side
rate of ulcers in relation to H pylori status was consistent effects during treatment of arthritis. Am J Med 1984; 84 (suppl 2A):
20-24.
with our previous findings19 and those reported by
8 Silverstein FE, Graham DY, Senior JR, et al. Misoprostol reduces
Ekstrom and co-workers.10 Since the risk of ulcer is high serious gastrointestinal complications in patients with rheumatoid
during the first weeks of NSAID therapy, particularly in arthritis receiving nonsteroidal antiinflammatory drugs: a randomized,
those without previous exposure,3,5 our finding is relevant double-blind, placebo-controlled trial. Am Intern Med 1995; 123:
241–49.
to patients who need intermittent treatment for
9 Taha AS, Hudson N, Hawkey CJ, et al. Famotidine for the prevention
exacerbation of such disorders as osteoarthritis. of gastric and duodenal ulcers caused by nonsteroidal
Our study differs from others in that most patients in antiinflammatory drugs. N Engl J Med 1996; 334: 1435–39.
our series were elderly with concomitant illness—ie, 10 Ekstrom P, Carling L, Wetterhus S, et al. Prevention of peptic ulcer
and dyspeptic symptoms with omeprazole in patients receiving
at high risk of developing NSAID-induced ulcer continuous non-steroidal anti-inflammatory drug therapy: a Nordic
complications. We did not recruit patients who were multicentre study. Scand J Gastroenterol 1996; 31: 753–58.
already on long-term NSAIDs, or those with frequent 11 Levine JS. Misoprostol and nonsteroidal anti-inflammatory drugs: a
previous exposure to NSAIDs, to avoid any potential tale of effects, outcomes, and costs. Ann Intern Med 1995; 123:
309–10.
selection bias.3,5 All patients received the same dosage of 12 Taha AS, Nakshabendi I, Lee FD, Sturrock RD, Russell RI. Chemical
naproxen to eliminate any confounding effects associated gastritis and Helicobacter pylori related gastritis in patients receiving
with different doses and types of NSAIDs.3 In addition, non-steroidal anti-inflammatory drugs: comparison and correlation
all endoscopic examinations were done by one with peptic ulceration. J Clin Pathol 1992; 45: 135–39.
13 Heresbach D, Raoul JL, Bretagne JF, et al. Helicobacter pylori: a risk
endoscopist who was unaware of treatment allocation to and severity factor of non-steroidal anti-inflammatory drug induced
eliminate bias and between-observer variation. The lower gastropathy. Gut 1992; 33: 1608–11.
rate of ulcers in patients on antihelicobacter therapy 14 Upadhyay R, Howatson A, McKinlay A, Danesh BJZ, Sturrock RD,
might be related to the antiulcer effect of bismuth, but Russell RI. Campylobacter pylori associated gastritis in patients taking
non-steroidal anti-inflammatory drugs. Br J Rheumatol 1988; 27:
because bismuth was given for only 1 week before the 113–16.
start of NSAID therapy, this effect was kept to a 15 Graham DY, Lidsky MD, Cox AM, et al. Long-term non-steroidal
minimum. antiinflammatory drug use and Helicobacter pylori infection.
Gastroenterology 1991; 100: 1653–57.
Our results show that NSAID-induced ulceration can
16 Martin DF, Montgomery E, Dobek AS, Patrissi GA, Peura DA.
be reduced by eradication of H pylori before NSAID Campylobacter pylori NSAIDs, and smoking: risk factors for peptic
administration and establish H pylori infection as a risk ulcer disease. Am J Gastroenterol 1989; 84: 1268–72.
978 Vol 350 • October 4, 1997
THE LANCET
17 Shallcross TM, Rathbone BJ, Wyatt JI, Heatley RV. Helicobacter pylori 23 Laine L, Cominelli F, Sloane R, Casini-Raggi V, Marin-Sorensen M,
associated chronic gastritis and peptic ulceration in patients taking Weinstein WM. Interaction of NSAIDs and Helicobacter pylori on
non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther 1990; gastroduodenal injury and prostaglandin production: a controlled
4: 515–22. double-blind trial. Ailment Pharmacol Ther 1995; 9: 127–35.
18 Loeb DS, Talley NJ, Ahlquist DA, Carpenter HA, Zinsmeister AR. 24 Goggin PM, Collins DA, Jazrawi RP, et al. Prevalence of Helicobacter
Long-term non-steroidal anti-inflammatory drug use and pylori infection and its effects on symptoms and non-steroidal anti-
gastroduodenal injury: the role of Helicobacter pylori. Gastroenetrology inflammatory drug induced gastrointestinal damage in patients with
1992; 102: 1899–905. rheumatoid arthritis. Gut 1993; 34: 1677–80.
19 Li EKM, Sung JY, Suen R, et al. Helicobacter pylori infection increases 25 Kim JG, Graham DY, The Misoprostol Study group. Helicobacter
the risk of peptic ulcers in chronic users in chronic of non-steroidal pylori infection and the development of gastric or duodenal ulcer in
anti-inflammatory drugs. Scand J Rheumatol 1996; 25: 42–46. arthritic patients receiving chronic NSAID therapy. Am J Gastroenterol
20 Publig W, Wustinger C, Zandl C. Non-steroidal anti-inflammatory 1994; 89: 203–07.
drugs (NSAIDs) cause gastrointestinal ulcers mainly in Helicobacter 26 Taha AS, Sturrock RD, Russell RI. Mucosal erosions in longterm non-
pylori carriers. Wien Klin Wochenschr 1994; 106: 276–79. steroidal anti-inflammatory drug users: predisposition to ulceration
21 Lanza FL, Evans DG, Graham DY. Effect of Helicobacter pylori and relatiom to Helicobacter pylori. Gut 1995; 36: 334–36.
infection on the severity of gastroduodenal mucosal injury after acute 27 Seppala K, Pikkarainen P, Sipponen P, Kivilaakso E, Gormsen MH,
administration of naproxen or aspirin to normal volunteers. Am J and the Finnish Gastric Ulcer Study Group. Cure of peptic ulcer
Gastroenterol 1991; 86: 735–37. associated with eradication of Helicobacter pylori. Gut 1995; 36: 834–37.
22 Thillainayagam AV, tabaqchali S, warrington SJ, Farthing MJG. 28 Bianchi Porro G, Parente F, Imbesi V, Montrone F, Caruso I. Role of
Interrelationships between Helicobacter pylori infection, non-steroidal Helicobacter pylori in ulcer healing and recurrence of gastric and
anti-inflammatory drugs and gastroduodenal disease: a prospective duodenal ulcers in longterm NSAID users: response to omeprazole
study in healthy volunteers. Dig Dis Sci 1994; 39: 1085–89. dual therapy. Gut 1996; 59: 22–26.
Risk of ocular hypertension or open-angle glaucoma in elderly
patients on oral glucocorticoids
Edeltraut Garbe, Jacques LeLorier, Jean-Francois Boivin, Samy Suissa
Summary (1·01–1·56) for less than 40 mg per day of hydrocortisone,
1·37 (1·06–1·76) for patients on 40–79 mg per day, and
Background Ocular hypertension and open-angle glaucoma 1·88 (1·40–2·53) for patients on 80 mg or more per day.
are well-known side-effects of treatment with topical The odds ratios also increased with the duration of
ophthalmic glucocorticoids. There is uncertainty about the treatment over the first 11 months of exposure.
risk of these disorders with oral glucocorticoid therapy.
Interpretation The use of oral glucocorticoids increases the
Methods Data from the Quebec universal health insurance risk of ocular hypertension or open-angle glaucoma in
programme for the elderly were used to identify 9793 elderly patients. In patients in this age-group who need
patients with a new diagnosis of ocular hypertension or long-term treatment with high doses of oral
open-angle glaucoma, or on newly prescribed treatment for glucocorticoids, monitoring of intraocular pressure may be
these disorders (cases). 38 325 controls were randomly justified.
selected from ophthalmology patients seen in the same
month and year as the case (index date). Current use of Lancet 1997; 350: 979–82
oral glucocorticoids was defined as that within 14 days of
the index date. All glucocorticoid doses were converted to Introduction
the equivalent amount of hydrocortisone. The case-control Ocular hypertension is a well-known side-effect of topical
analysis was done by conditional logistic regression and ophthalmic glucocorticoids.1 The lack of symptoms with
adjusted for age, sex, systemic hypertension, diabetes raised intraocular pressure has prompted ophthalmol-
mellitus, ophthalmic glucocorticoids, glucocorticoid
ogists to recommend routine monitoring of intraocular
pressure in patients on long-term ophthalmic steroids.1,2
injections, and variables related to general health.
Several case reports have suggested that oral
Findings The mean ages of cases and controls were similar glucocorticoid therapy can also result in ocular
(74·9 [SD 6·3] vs 74·7 [6·4]). The adjusted odds ratio of hypertension and open-angle glaucoma.3-5 However,
ocular hypertension or open-angle glaucoma for current investigations into the effects of oral corticosteroids on
users of oral glucocorticoids compared with non-users was ocular pressure are scarce. There have been a few
1·41 (95% CI 1·22–1·63). There was a dose-related retrospective studies with small numbers of patients on
increase in the adjusted odds ratios for current users: 1·26 glucocorticoids for variable periods of time.6–10 In some of
these studies the mean intraocular pressure was higher in
Division of Clinical Epidemiology, Royal Victoria Hospital the steroid-treated group than in the control group.6,7
(E Garbe MD, S Suissa PhD); Department of Epidemiology and Most ophthalmologists believe that the risk of ocular
Biostatistics, McGill University (E Garbe, J-F Boivin ScD, S Suissa); hypertension or open-angle glaucoma is lower with
Centre de Recherche, Hôtel-Dieu de Montréal, Université de
oral glucocorticoids than with topical ophthalmic
Montréal, Montreal, Canada (E Garbe, J LeLorier PhD); and
Potsdam Institute of Pharmacoepidemiology and Technology
glucocorticoids, although the risk has not yet been
Assessment, Potsdam, Germany (E Garbe) quantified.11,12 Some investigators have hypothesised that
months or years of treatment with oral glucocorticoids are
Correspondence to: Dr Samy Suissa, Division of Clinical
Epidemiology, Royal Victoria Hospital, 687 Pine Avenue West,
needed to cause ocular hypertension. By contrast, most
Ross 4.29, Montreal, Quebec H3A 1A1, Canada clinicians recognise an increased risk with topical
(e-mail: SAMYS@EPID.LAN.MCGILL.CA) ophthalmic steroids after weeks of treatment.11,13
Vol 350 • October 4, 1997 979
You might also like
- Understated Dominance - Chapter 1501 To 1540Document114 pagesUnderstated Dominance - Chapter 1501 To 1540voipus12No ratings yet
- Cardiothoracicsurgery McqsDocument352 pagesCardiothoracicsurgery McqsMade Ayu50% (2)
- Lansoprazole For The Prevention of Recurrences of Ulcer Complications From Long-Term Low-Dose Aspirin UseDocument6 pagesLansoprazole For The Prevention of Recurrences of Ulcer Complications From Long-Term Low-Dose Aspirin UseAmalia NandiaNo ratings yet
- Journal of Population Therapeutics & Clinical PharmacologyDocument7 pagesJournal of Population Therapeutics & Clinical PharmacologyEka SetyariniNo ratings yet
- Journal of Population Therapeutics & Clinical PharmacologyDocument6 pagesJournal of Population Therapeutics & Clinical PharmacologyheryanggunNo ratings yet
- Acute Inflammatory: Laparoscopically (Salpingitis)Document7 pagesAcute Inflammatory: Laparoscopically (Salpingitis)Bella Ika LestariNo ratings yet
- Original Research PaperDocument2 pagesOriginal Research Paperيحيى الجبليNo ratings yet
- Artículo 14Document5 pagesArtículo 14Yeid EsquivelNo ratings yet
- Inflammatory: of Ofloxacin The of Laparoscopically DiseaseDocument18 pagesInflammatory: of Ofloxacin The of Laparoscopically DiseaseMuhajir NagallamzNo ratings yet
- Vol24 3-3 PDFDocument7 pagesVol24 3-3 PDFEliasNo ratings yet
- Efficacy of Omeprazole and Amoxicillin With Either Clarithromycin or Metronidazole On Eradication of in Chinese Peptic Ulcer PatientsDocument5 pagesEfficacy of Omeprazole and Amoxicillin With Either Clarithromycin or Metronidazole On Eradication of in Chinese Peptic Ulcer PatientsSyukron MakmunNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofFransisca PekertiNo ratings yet
- Nej Mo A 1507062Document11 pagesNej Mo A 1507062anggiNo ratings yet
- CAP - Risk Factors and TreatmentDocument5 pagesCAP - Risk Factors and Treatmentgrool29rNo ratings yet
- Isoniazid TuberculosisDocument10 pagesIsoniazid TuberculosisAisyah Aftita KamrasyidNo ratings yet
- Ne W Engl and Journal MedicineDocument11 pagesNe W Engl and Journal Medicinea4agarwalNo ratings yet
- Bacteriology and Drug Susceptibility Analysis of PusDocument5 pagesBacteriology and Drug Susceptibility Analysis of PusLuis Miguel Díaz VegaNo ratings yet
- A Prospective Observational Study of Prescribing Patterns in Peptic Ulcer DiseaseDocument40 pagesA Prospective Observational Study of Prescribing Patterns in Peptic Ulcer DiseaseGeet MaanNo ratings yet
- JOURNAL Treating Acute Urinary Tract InfectionsDocument5 pagesJOURNAL Treating Acute Urinary Tract InfectionsKhayelee PalosNo ratings yet
- Anderson01-27-12 Floroquinolone Prophilaxis PDFDocument22 pagesAnderson01-27-12 Floroquinolone Prophilaxis PDFSri WulandahNo ratings yet
- Short-Course Intraabdominal InfectionDocument10 pagesShort-Course Intraabdominal Infectionnicolás idárragaNo ratings yet
- The Role of Antibiotic Prophylaxis in Prevention of Wound Infection After Lichtenstein Open Mesh Repair of Primary Inguinal HerniaDocument7 pagesThe Role of Antibiotic Prophylaxis in Prevention of Wound Infection After Lichtenstein Open Mesh Repair of Primary Inguinal Herniaيحيى الجبليNo ratings yet
- Meningitis 3Document12 pagesMeningitis 3Kelly MuñozNo ratings yet
- Methisoprinol y VPHDocument4 pagesMethisoprinol y VPHAndres Gonzalez Cruz100% (1)
- Dokazano Dejstvo Nigelle Sative (Crnog Kumina) U Eliminaciji Helicobacter PyloriDocument11 pagesDokazano Dejstvo Nigelle Sative (Crnog Kumina) U Eliminaciji Helicobacter PylorirbcollegeNo ratings yet
- Management of The Urologic Sepsis SyndromeDocument10 pagesManagement of The Urologic Sepsis SyndromeNur Syamsiah MNo ratings yet
- Crossm: Efficacy of Doxycycline in The Treatment of SyphilisDocument7 pagesCrossm: Efficacy of Doxycycline in The Treatment of SyphilisHerdian KusumaNo ratings yet
- Atorvastatin Improves Sputum Conversion and Chest X-Ray Severity ScoreDocument6 pagesAtorvastatin Improves Sputum Conversion and Chest X-Ray Severity Scorecharmainemargaret.parreno.medNo ratings yet
- Effectiveness of Antacids Reducing Digestive Patients Treated With Prednisone and PrednisoloneDocument5 pagesEffectiveness of Antacids Reducing Digestive Patients Treated With Prednisone and PrednisoloneSantri Akhir ZamanNo ratings yet
- Abcesele FicatuluiDocument4 pagesAbcesele FicatuluiMihaela AlinaNo ratings yet
- Screenshot 2021-06-19 at 21.33.17Document11 pagesScreenshot 2021-06-19 at 21.33.17bagus aldiNo ratings yet
- Tofacitinib As Induction and Maintenance Therapy For Ulcerative ColitisDocument14 pagesTofacitinib As Induction and Maintenance Therapy For Ulcerative Colitismichal ben meronNo ratings yet
- A Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesDocument4 pagesA Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesSake Cinema21No ratings yet
- Single-Dose Azithromycin Versus Benzathine Benzylpenicillin For Treatment of Yaws in Children in Papua New Guinea: An Open-Label, Non-Inferiority, Randomised TrialDocument7 pagesSingle-Dose Azithromycin Versus Benzathine Benzylpenicillin For Treatment of Yaws in Children in Papua New Guinea: An Open-Label, Non-Inferiority, Randomised TrialOlivia Halim KumalaNo ratings yet
- Real-World Data of Helicobacter Pylori Prevalence, Eradicationregimens, and Antibiotic Resistance in Thailand, 2013-201Document5 pagesReal-World Data of Helicobacter Pylori Prevalence, Eradicationregimens, and Antibiotic Resistance in Thailand, 2013-201andi kulokNo ratings yet
- Tubo-Ovarian Abscess - Contemporary Approach To ManagementDocument9 pagesTubo-Ovarian Abscess - Contemporary Approach To ManagementDanny. JayNo ratings yet
- Jur DingDocument11 pagesJur DingI'am AjhaNo ratings yet
- Azithromycin in Rheumatic FeverDocument4 pagesAzithromycin in Rheumatic Feverhussien abd elwahedNo ratings yet
- Comparative Study On The Efficacy of Non-Steroidal, Steroid and Non-Use Anti Inflammatory in The Treatment of Epidemic ConjungtivitisDocument6 pagesComparative Study On The Efficacy of Non-Steroidal, Steroid and Non-Use Anti Inflammatory in The Treatment of Epidemic ConjungtivitisVisakha VidyadeviNo ratings yet
- EsomeprazoleDocument7 pagesEsomeprazoleSanjay NavaleNo ratings yet
- The Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioDocument7 pagesThe Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioMaharaniNo ratings yet
- Rcse9505 345Document4 pagesRcse9505 345Swekshya PandeyNo ratings yet
- Nebul Nacl 3Document7 pagesNebul Nacl 3Arif RSNo ratings yet
- The Clinical Relevance of Microbiology Specimens in Head and Neck Space Infections of Odontogenic OriginDocument3 pagesThe Clinical Relevance of Microbiology Specimens in Head and Neck Space Infections of Odontogenic OriginkaarlaamendezNo ratings yet
- Haron 1989Document8 pagesHaron 1989georgios031No ratings yet
- Corticosteroids For Bacterial Meningitis in Adults in Sub-Saharan AfricaDocument10 pagesCorticosteroids For Bacterial Meningitis in Adults in Sub-Saharan AfricaMutiara KhalishNo ratings yet
- 43 Pukar EtalDocument3 pages43 Pukar EtaleditorijmrhsNo ratings yet
- Helicobacter Pylori Triple Versus Dual Therapy For EradicatingDocument7 pagesHelicobacter Pylori Triple Versus Dual Therapy For EradicatingAna Lívia AzevedoNo ratings yet
- Tugas RCT SenaDocument10 pagesTugas RCT SenaArfad El HabibieNo ratings yet
- Critical Apprisal of A Prospective StudyDocument7 pagesCritical Apprisal of A Prospective StudyVK LabasanNo ratings yet
- Early Use of TIPS in Cirrhosis and Variceal BleedingDocument10 pagesEarly Use of TIPS in Cirrhosis and Variceal Bleedingray liNo ratings yet
- 10 1016@j Bja 2020 05 003Document10 pages10 1016@j Bja 2020 05 003Robert ChristevenNo ratings yet
- Bacterial Tonsillar Microbiota and Antibiogram in Recurrent TonsillitisDocument5 pagesBacterial Tonsillar Microbiota and Antibiogram in Recurrent TonsillitisResianaPutriNo ratings yet
- Management of Perforated Appendicitis in Children: A Decade of Aggressive TreatmentDocument5 pagesManagement of Perforated Appendicitis in Children: A Decade of Aggressive Treatmentapi-308365861No ratings yet
- Enema. Jal. Pancha Bhuta-323Document6 pagesEnema. Jal. Pancha Bhuta-323Shree GaneshNo ratings yet
- Zhu 2017Document3 pagesZhu 2017Muchamad Wisuda RiswantoNo ratings yet
- Trial of Short-Course Antimicrobial Therapy For Intraabdominal InfectionDocument10 pagesTrial of Short-Course Antimicrobial Therapy For Intraabdominal InfectionMeygan CórdovaNo ratings yet
- Analysis of Antibiotics Selection in Patients Undergoing Appendectomy in A Chinese Tertiary Care HospitalDocument5 pagesAnalysis of Antibiotics Selection in Patients Undergoing Appendectomy in A Chinese Tertiary Care HospitalYuanico LiraukaNo ratings yet
- Apendik KoesnadiDocument4 pagesApendik KoesnadiUbay'z DillahNo ratings yet
- RF - Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Treatment UpdateDocument2 pagesRF - Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Treatment Updatedoc.kentoNo ratings yet
- Gulati 2020Document14 pagesGulati 2020Anisha MDNo ratings yet
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Study of Radiographic Features of Renal Osteodystrophy in Chronic Kidney Disease (CKD) and Their Correlation With Clinical and Biochemical ParametersDocument10 pagesStudy of Radiographic Features of Renal Osteodystrophy in Chronic Kidney Disease (CKD) and Their Correlation With Clinical and Biochemical ParametersIJAR JOURNALNo ratings yet
- Reivew On Equine Colic With Special Attention To Its Diagnosis and TreatmentDocument45 pagesReivew On Equine Colic With Special Attention To Its Diagnosis and TreatmentTola dinkuNo ratings yet
- Positive Affect Treatment For Depression and Anxiety Workbook Alicia E Meuret All ChapterDocument67 pagesPositive Affect Treatment For Depression and Anxiety Workbook Alicia E Meuret All Chapterkaren.dixon505100% (9)
- Medical+language+practice+ NotesDocument7 pagesMedical+language+practice+ NotesmanethNo ratings yet
- WORKSHEET 6 Breath Spray PCOS111 PH3Y2 1 LABDocument8 pagesWORKSHEET 6 Breath Spray PCOS111 PH3Y2 1 LABAngelica PaguintoNo ratings yet
- CNS Related DiseasesDocument4 pagesCNS Related DiseasesYzabelle EncoyNo ratings yet
- FULL Download Ebook PDF Health Psychology 10th Edition PDF EbookDocument41 pagesFULL Download Ebook PDF Health Psychology 10th Edition PDF Ebooklawrence.kibbe472100% (44)
- CHN Family Assessment Interview GuideDocument9 pagesCHN Family Assessment Interview GuideBianca Denise RopilaNo ratings yet
- The Cure For All DiseasesDocument888 pagesThe Cure For All Diseasesmihai968100% (1)
- Aily Equirements: Case: Patient With Tuberculosis General Objectives (5pts)Document31 pagesAily Equirements: Case: Patient With Tuberculosis General Objectives (5pts)janna mae patriarcaNo ratings yet
- Water Soluble Vitamins: Vitamins Toxicity/Definition Deficiency/Definition Niacin Vitamin ADocument3 pagesWater Soluble Vitamins: Vitamins Toxicity/Definition Deficiency/Definition Niacin Vitamin ARoshin TejeroNo ratings yet
- WWW - Reliancegeneral.co - In: Important Note: This Is An Electronically Generated Document and Requires No Seal / StampDocument1 pageWWW - Reliancegeneral.co - In: Important Note: This Is An Electronically Generated Document and Requires No Seal / StampdhanishlNo ratings yet
- Radiology Primary Pq.Document34 pagesRadiology Primary Pq.AbosedeNo ratings yet
- Strep A Infection Guidance For Parents and CarersDocument2 pagesStrep A Infection Guidance For Parents and CarersnaziaNo ratings yet
- Article On Prevalence of Substance AbuseDocument32 pagesArticle On Prevalence of Substance AbuseJanice ScatesNo ratings yet
- 10-OBGYN-Glory GroupDocument46 pages10-OBGYN-Glory Groupanmar alkhudhriNo ratings yet
- Occupational Lung DiseasesDocument3 pagesOccupational Lung DiseasesDjdjjd SiisusNo ratings yet
- (05 - 27 - 23) GI DISORDERS - PUD Continuation and GI CancerDocument6 pages(05 - 27 - 23) GI DISORDERS - PUD Continuation and GI CancerMarcus Andrei J RamosNo ratings yet
- Case-Based Textbook of Echocardiography (PDFDrive)Document572 pagesCase-Based Textbook of Echocardiography (PDFDrive)Ringo StoneNo ratings yet
- Psych Nursing Post Test 2 Doc F PDFDocument5 pagesPsych Nursing Post Test 2 Doc F PDFTrisha Mae MarquezNo ratings yet
- Helping Patient With WoundDocument3 pagesHelping Patient With WoundSevina Eka ChannelNo ratings yet
- Module 12Document24 pagesModule 12dasilvashleyNo ratings yet
- Formulation Stabilisation and Encapsulation of Bacteriophage For Phage TherapyDocument34 pagesFormulation Stabilisation and Encapsulation of Bacteriophage For Phage TherapyGerman GodiNo ratings yet
- الوصفة الطبية للعلاج بالتغذية جيمس ف. بالش المكتبة نتDocument705 pagesالوصفة الطبية للعلاج بالتغذية جيمس ف. بالش المكتبة نتDy UwoNo ratings yet
- 1700 Questions Not in PLABABLEDocument131 pages1700 Questions Not in PLABABLEDaniah Marwan Dawood DAWOODNo ratings yet
- FC MS3 (SC)Document8 pagesFC MS3 (SC)madlahuddindayangNo ratings yet
- A Psychobiological Perspective On The Personality Disorders: LarryDocument12 pagesA Psychobiological Perspective On The Personality Disorders: LarryDrobota MirunaNo ratings yet
- Understanding The Six Stages of Disease - Maharishi AyurVedaDocument9 pagesUnderstanding The Six Stages of Disease - Maharishi AyurVedaAlbar MattaNo ratings yet