Professional Documents
Culture Documents
Davies 2013 Acupuncture Treatment of Phantom Limb Pain and Phantom Limb Sensation in A Primary Care Setting
Davies 2013 Acupuncture Treatment of Phantom Limb Pain and Phantom Limb Sensation in A Primary Care Setting
Uploaded by
rezteevicOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Davies 2013 Acupuncture Treatment of Phantom Limb Pain and Phantom Limb Sensation in A Primary Care Setting
Davies 2013 Acupuncture Treatment of Phantom Limb Pain and Phantom Limb Sensation in A Primary Care Setting
Uploaded by
rezteevicCopyright:
Available Formats
Case report
Acupuncture treatment of phantom
limb pain and phantom limb
sensation in a primary care setting
Arwel Davies
Correspondence to ABSTRACT to have a crush injury and compartment
Dr Arwel Davies, Brynhyfryd
A 45-year-old man presented with phantom limb syndrome of his right arm. Despite fas-
Surgery, Brynhyfryd Square,
Swansea SA5 9EB, UK; pain and phantom limb sensation 12 weeks after ciotomy, his arm was not salvageable and
agdavies.1@sky.com an above-elbow amputation of his right arm. He he underwent a high above-elbow ampu-
underwent seven sessions of acupuncture at tation of his dominant right arm 2 days
Received 31 October 2012
Revised 5 November 2012
weekly intervals carried out by his general after admission. The level of amputation
Accepted 15 November 2012 practitioner on his intact left arm, with complete was such that he is unlikely to be suitable
Published Online First relief of the phantom limb pain and considerable for future fitting with a useful prosthetic
6 December 2012 improvement of the phantom limb sensation of arm.
his right arm. This case demonstrates the He was first seen by his GP 6 weeks
possible benefits from the use of short after surgery for a review of his medica-
acupuncture sessions for a potentially chronic tion and care package. At the time he was
condition undertaken within the constraints of a complaining of pain and an uncomfort-
busy general medical practice. able sensation in his absent right arm. He
was further reviewed by his GP 12 weeks
after surgery with the pain and sensation
This case report details the successful use
in his right arm still causing him consid-
of acupuncture of an intact left arm to
erable problems.
treat phantom limb pain (PLP) and
phantom limb sensation (PLS) following
amputation of a patient’s right arm. The
Assessment
treatment took place in a community-
At 12 weeks after amputation the patient
based general medical practice, with the
described an overall unpleasant sensation
acupuncture sessions included within the
of his right arm still being present. This
normal surgery sessions of a general prac-
sensation was particularly prominent at
titioner (GP) with an interest in
the hand and wrist. Although in normal
acupuncture.
proportion to his left, he described the
right arm as being shorter (approximately
CASE REPORT three-quarters the length of his left arm).
History He described the pain in his amputated
The patient was a 45-year-old man with a right arm as a burning type pain in the
long history of chaotic drug and alcohol hand and a separate sharp pain shooting
misuse. He had been under the care of up his arm.
the local drug and alcohol services on an As acupuncture of his intact left arm
intermittent basis for some years. He had was being considered as a treatment
been stable from a drug and alcohol per- option, the left arm was assessed. He was
spective for many months prior to his sensitive to palpation at certain points
amputation and there was no history of along his left arm—most notably at
significant mental health problems. points corresponding to the Traditional
In early 2012 he was found uncon- Chinese Medicine (TCM) points of LI11
scious on the floor of his home after an and LI14.
unintentional overdose of illicit street The clinical impression was of PLP and
drugs. He had been lying on his right PLS following amputation of his right
To cite: Davies A. Acupunct side for an unknown period of time and, arm. The patient had undergone a course
Med 2013;31:101–104. on admission to hospital, he was found of acupuncture by the same GP for a
Davies A. Acupunct Med 2013;31:101–104. doi:10.1136/acupmed-2012-010270 101
Case report
neck problem some 5 years previously with good At follow-up a week later the patient described the
effect. He was amenable to the idea of a trial of acu- first session from his perspective. While the needles
puncture to his left arm in an attempt to alleviate the were in his left arm, the area surrounding the needle
pain and sensation in his right arm. points felt hot but he had no sensation in his ampu-
tated right arm for the duration of needling. He also
felt euphoric during the session. He had not experi-
Medication
enced any right arm pain since the first session, but
During the course of acupuncture he was taking a
there had been a gradual return of sensation. The
number of prescribed medications including clonidine,
right arm was perceived to be shorter at the second
diazepam, pregabalin, paracetamol, tramadol and ven-
session—being about half the size of his left arm.
lafaxine. These medications were all being prescribed,
At this second session, four left arm points were
and he was already suffering from PLP and PLS before
needled: LI4, LI8, LI11 and LI14. These points
he started his course of acupuncture. In fact he had
became the standard points used for all subsequent
been taking prescribed venlafaxine for some years
sessions, with the duration of needling being increased
before his amputation and had a long history of
to 5 min for this and subsequent sessions. All needles
buying illicit diazepam from street sources. Prescribed
were stimulated after insertion to achieve de qi.
clonidine, pregabalin and tramadol had been initiated
Overall, the patient underwent seven sessions of
during his postoperative recovery in hospital.
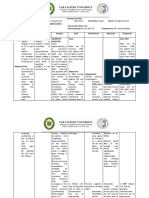
acupuncture at weekly intervals. As shown in figure 1,
The only medication dose changed around the start
the PLP completely resolved during the course of the
of the acupuncture treatment was diazepam, which
acupuncture sessions while there was a considerable
had previously been taken haphazardly and was stan-
improvement in the VAS scores for the PLS over the
dardised at a daily prescribed dose of 14 mg. The
first five sessions—from 94 at the first session to 19 at
dose of diazepam was increased to 20 mg daily after
the fifth.
session 7. However, this remained a relatively low
Between sessions 5 and 6 the patient had a heavy
dose of diazepam for this patient with his past history
fall onto his right shoulder, resulting in a severe
of prolonged drug misuse.
flare-up of both pain and sensation. However, he
During the early sessions the patient was taking
responded well to the sixth session of acupuncture
pregabalin for neuropathic pain at a dose of 600 mg
2 days after the fall, to such an extent that the PLS
twice daily, which was double the maximum recom-
disappeared completely for 2 weeks. After the sixth
mended dose.1 The dose of pregabalin was halved
session he did not experience sensations such as
after the third session, with a further reduction to
feeling the need to lean on his right elbow or to pull
300 mg once daily before the fifth session. A reduc-
down cuffs at his right wrist. This was the only time
tion in the dose of pregabalin would be expected to
during the course of sessions that his PLS disappeared
result in a worsening experience of pain.
completely.
The patient has been reviewed since completing his
Treatment acupuncture. When seen 3 weeks after his final acu-
At the first session, 13 weeks after his amputation, puncture session (22 weeks after amputation), he
baseline PLP and PLS were measured on a visual ana-
logue scale (VAS) graded from 0 to 100. The VAS
score at the first session was 73 for PLP and 94 for
PLS. The VAS was measured at each subsequent
session and at intervals after the end of the
acupuncture.
At the first session, five points in the patient’s left
arm and neck were needled. Needles were inserted at
TCM points LI8, LI11, LI14 and GB21 (Dong Bang
needles 0.25×30) as these points were sensitive on
palpation. In addition, LI4 was needled (Dong Bang
0.20×15) for its general analgesic effect. The needles
were stimulated after insertion and there was a
marked de qi effect, especially at LI4, LI8 and LI14,
and the patient mentioned an immediate reduction in
pain intensity in his right arm. All needles were
removed after only 3 min at this first session owing to
the strong de qi at some of the points. Immediately Figure 1 Visual analogue scale scores for phantom limb pain
after removal of the needles the patient noted that his (PLP) and phantom limb sensation (PLS) during 7 weeks of
right arm was less painful and also felt numb and acupuncture and 3 weeks follow-up (week 26 scores were
shorter compared with the start of the session. PLP=0, PLS=7).
102 Davies A. Acupunct Med 2013;31:101–104. doi:10.1136/acupmed-2012-010270
Case report
reported that he was completely free of right arm appointment system. There is little flexibility within
pain. He did have some sensation (VAS score 30), but such a system to allow dedicated acupuncture sessions
said it was bearable compared with before the acu- with longer appointment slots, and there is minimal
puncture. He felt his right arm continued to be about scope for arranging sessions more frequently than
half the length of his left arm. once weekly.
He was reviewed again 19 weeks after his final acu- The patient and GP had developed a good thera-
puncture session (38 weeks after amputation). At this peutic relationship over a number of years, and the
time he was still free of pain and his PLS had contin- patient had had a good response from acupuncture
ued to improve (VAS score 7). Interestingly, he felt some years previously for an unrelated problem. This
that his right arm was now shorter than previously, previous experience may have influenced his agree-
being approximately one-third the length of his left ment to the idea of undergoing acupuncture of his
arm. This represents a considerable improvement on intact limb for PLP and PLS.
his initial presentation when he felt the right arm to As acupuncture was used as an early intervention
be about three-quarters the length of his left arm. with the first session being only 13 weeks after
surgery, the good response may be due to the fact that
DISCUSSION PLP and PLS had not become established in this
PLP and PLS are types of perceptual sensitive phe- patient.
nomena and are common complaints after amputation In this particular case the patient derived consider-
of limbs. Painless sensations can occur in up to 90% able benefit from short sessions of acupuncture. This
of patients, often stabilising in the first year after benefit was commented on when he attended a sec-
amputation.2 PLP and PLS after upper limb amputa- ondary care pain control clinic which was unaware
tion can become chronic problems, with over 80% of that he was having acupuncture in primary care. The
patients experiencing some sensation or pain many clinic letter noted a dramatic improvement in his
years after surgery.3 symptoms to the extent that the patient no longer had
A number of possible contributing mechanisms to any pain whatsoever in his phantom limb.
PLP, including stump-related pathology, spinal and Even 5 months after the end of his acupuncture ses-
cortical changes, have been proposed, and it has sions he remained free of PLP, his PLS was continuing
proved notoriously difficult to treat, with the most to improve and his perception of his right arm was
promising methods complementing pharmacological that it was shortening. His VAS scores for PLP had
approaches with physical, psychological and behav- fallen from 73 at the first session of acupuncture to
ioural intervention.4 PLP has variously been described 0 at review 3 weeks after ending the acupuncture ses-
as burning, tearing, electric shock in type. It is par- sions and 0 again on further review 19 weeks after the
ticularly problematic after traumatic amputation, with end of acupuncture. The VAS scores for PLS were 94
up to two in three patients being affected.5 at the start, 30 on review 3 weeks after the end of acu-
Acupuncture has previously been reported to be of puncture and 7 on further review 19 weeks after the
benefit in PLP and PLS,6 7 although the total numbers end of acupuncture. This may represent the continued
of patients included in these reports were low. Most effect of the acupuncture or may have represented
recently, Bradbrook needled the asymptomatic intact continued healing after his amputation. Only time will
limb in three patients in a rehabilitation clinic for tell how long this benefit will last. It will be interest-
patients with lower limb amputation.8 It was this ing to see what his PLP and PLS VAS scores will be
short series which provided the inspiration for consid- over the next 12–18 months.
ering acupuncture as a treatment option for the Funding None.
patient described in this report but, in contrast to the
cases described by Bradbrook, all of which involved Competing interests None.
lower limb amputations, the patient in this report Patient consent Obtained.
underwent amputation of his upper limb. Provenance and peer review Not commissioned;
There appears to be little consensus on the optimal internally peer reviewed.
duration of needling to obtain the optimal effect from
acupuncture sessions, with needling time often influ-
enced by personal preference. There are schools of
thought suggesting that brief periods of needling are REFERENCES
1 Anon. British National Formulary 64, September 2012.
effective.9 Needling time during the first session was
London: BMJ Group and Pharmaceutical Press, 2012.
short at 3 min due to the marked de qi effect. Since 2 Rasulic L, Ivanovic S, Bascarevic V, et al. Phantom pain and
the symptomatic response at the first session was posttraumatic pain conditions. Acta Chir Iugosl
good, subsequent sessions were limited to a maximum 2004;51:71–80.
of 5 min needling time each session. This worked well 3 Modirian E, Shojaei H, Soroush MR, et al. Phantom pain in
for this patient, as the sessions were fitted into busy bilateral upper limb amputation. Disabil Rehabil
general practice surgeries running on a 10 min 2009;31:1878–81.
Davies A. Acupunct Med 2013;31:101–104. doi:10.1136/acupmed-2012-010270 103
Case report
4 Giummarra MJ, Moseley GL. Phantom limb pain and bodily 7 Monga TN, Jaksic T. Acupuncture in phantom limb pain. Arch
awareness: current concepts and future directions. Curr Opin Phys Med Rehabil 1981;62:229–31.
Anaesthesiol 2011;24:524–31. 8 Bradbrook D. Acupuncture treatment of phantom limb pain
5 Carlen PL, Wall PD, Nadvorna H, et al. Phantom limbs and and phantom limb sensation in amputees. Acupunct Med
related phenomena in recent traumatic amputations. Neurology 2004;22:93–7.
1978;28:211–17. 9 Campbell A. Acupuncture in practice—beyond points and
6 Xing G. Acupuncture treatment of phantom limb pain—a meridians. Oxford: Butterworth-Heinemann, 2001.
report of 9 cases. J Tradit Chin Med 1998;18:199–201.
104 Davies A. Acupunct Med 2013;31:101–104. doi:10.1136/acupmed-2012-010270
You might also like
- Septic Arthritis NCPDocument3 pagesSeptic Arthritis NCPMae Therese B. MAGNO0% (1)
- Autonomic Nervous System Drugs Simple Complement Type QuestionsDocument11 pagesAutonomic Nervous System Drugs Simple Complement Type QuestionsIrina Panciu Stefan100% (1)
- Assessment of Mental RetardationDocument56 pagesAssessment of Mental Retardationdrkadiyala2No ratings yet
- Case Study: Mulligan Concept Management of "Tennis Elbow"Document3 pagesCase Study: Mulligan Concept Management of "Tennis Elbow"noonoons100% (1)
- Case Report Example and AbstractDocument8 pagesCase Report Example and AbstractMyra Lyn OloresNo ratings yet
- NCP (Acute Pain, Episiotomy)Document6 pagesNCP (Acute Pain, Episiotomy)Jenny AjocNo ratings yet
- Physical Activity Readiness Questionnaire (PAR-Q)Document2 pagesPhysical Activity Readiness Questionnaire (PAR-Q)eternalkainNo ratings yet
- Chapter 14 - Fluid and Electrolytes - Balance and DisturbanceDocument20 pagesChapter 14 - Fluid and Electrolytes - Balance and DisturbanceEmily Cormier100% (1)
- Chinese Scalp Acup (Military Cases)Document4 pagesChinese Scalp Acup (Military Cases)AngelaNo ratings yet
- Bradbrook 2004 Acupuncture Treatment of Phantom Limb Pain and Phantom Limb Sensation in AmputeesDocument5 pagesBradbrook 2004 Acupuncture Treatment of Phantom Limb Pain and Phantom Limb Sensation in AmputeesrezteevicNo ratings yet
- Differential Diagnosis of Shoulder and Cervical PaDocument7 pagesDifferential Diagnosis of Shoulder and Cervical PagursangeetNo ratings yet
- Lumbar Lateral ShiftDocument8 pagesLumbar Lateral Shiftiretama_No ratings yet
- 3CNCPDocument7 pages3CNCPHelen MontesNo ratings yet
- Rotator Cuff Case Report Diagnosis and TDocument4 pagesRotator Cuff Case Report Diagnosis and TCarla SeguelNo ratings yet
- Subcutaneous Prolotherapy Treatment of Refractory Knee, Shoulder, and Lateral Elbow PainDocument4 pagesSubcutaneous Prolotherapy Treatment of Refractory Knee, Shoulder, and Lateral Elbow PainEsteban J CaletaNo ratings yet
- Right Incomplete Brachial Plexus Injury (Upper Trunk Lesion) Post Ganglionic TypeDocument35 pagesRight Incomplete Brachial Plexus Injury (Upper Trunk Lesion) Post Ganglionic TypeJeanie WangsaNo ratings yet
- EffectivenessDocument5 pagesEffectivenessHari25885No ratings yet
- The Way of Making OkDocument3 pagesThe Way of Making OkPrabal Frank NandwaniNo ratings yet
- Case ICM I Week 4 JumatDocument3 pagesCase ICM I Week 4 JumatnaynaNo ratings yet
- Us Guided PRP InjDocument6 pagesUs Guided PRP InjNoura Rose100% (1)
- Soapie Charting: Date, Time, and Shift Progress NotesDocument3 pagesSoapie Charting: Date, Time, and Shift Progress NotesBianx Flores DosdosNo ratings yet
- LBP Case ReportDocument4 pagesLBP Case ReportMichele MarengoNo ratings yet
- Team 1Document4 pagesTeam 1JangMedNo ratings yet
- Balancing Method MirroringDocument9 pagesBalancing Method MirroringYoshua Viventius100% (1)
- AMSSM Poster 2020Document1 pageAMSSM Poster 2020Thang TruongNo ratings yet
- Musculoskeletal Sample ChartsDocument27 pagesMusculoskeletal Sample Chartschaitanya varmaNo ratings yet
- Efficacy of Mckenzie Approach Combined With Sustained Traction in Improving The Quality of Life Following Low Back Ache - A Case ReportDocument6 pagesEfficacy of Mckenzie Approach Combined With Sustained Traction in Improving The Quality of Life Following Low Back Ache - A Case ReportDr. Krishna N. SharmaNo ratings yet
- DystrophyDocument3 pagesDystrophyzbhabhaNo ratings yet
- Protocolo Core ExaminationDocument8 pagesProtocolo Core ExaminationBia DiasNo ratings yet
- Hands Function and Rheumatoid Arthritis Case ReporDocument4 pagesHands Function and Rheumatoid Arthritis Case ReporMuhammad RaflirNo ratings yet
- PIIS2589514123001214Document2 pagesPIIS2589514123001214abrariyy ma'hadiyyNo ratings yet
- Solomon Sallfors: Ambulatory Morning Report 1: ARM PAINDocument1 pageSolomon Sallfors: Ambulatory Morning Report 1: ARM PAINSolomon Seth SallforsNo ratings yet
- Assignment McqsDocument13 pagesAssignment Mcqsfaria ashrafNo ratings yet
- Anaesthetic Considerations in Patients With Transverse MyelitisDocument3 pagesAnaesthetic Considerations in Patients With Transverse MyelitisIniya RajendranNo ratings yet
- Assign Men 1Document6 pagesAssign Men 1Rashi JainNo ratings yet
- NCP Proper Assessment Explanation of The Problem Objective Nursing Interventions Rationale EvaluationDocument4 pagesNCP Proper Assessment Explanation of The Problem Objective Nursing Interventions Rationale EvaluationMarc Jordan EstebanNo ratings yet
- Cases Patient 1: FIG. 2. The X-Ray Depicting Neck Facet Degenerative Changes of Patient 1Document1 pageCases Patient 1: FIG. 2. The X-Ray Depicting Neck Facet Degenerative Changes of Patient 1dasdsaNo ratings yet
- BSN 1 H Case Application Nursing Care PlanDocument3 pagesBSN 1 H Case Application Nursing Care PlanAntonio EscotoNo ratings yet
- Pancoast Tumour Presenting As Shoulder Pain With Horner's SyndromeDocument3 pagesPancoast Tumour Presenting As Shoulder Pain With Horner's SyndromesuzilaNo ratings yet
- Saphenous Nerve EntrapmentDocument2 pagesSaphenous Nerve Entrapmentemilio9fernandez9gatNo ratings yet
- NCP Impaired Physical Mobility Acute PainDocument8 pagesNCP Impaired Physical Mobility Acute PainAi RouNo ratings yet
- Nursing Care Plan: Assessmen T (Cues / Clues) Nursing Diagnosis Rationale Planning Intervention Rationale Evaluatio NDocument7 pagesNursing Care Plan: Assessmen T (Cues / Clues) Nursing Diagnosis Rationale Planning Intervention Rationale Evaluatio NNajla Kaye PerezNo ratings yet
- Treatment of Scapulohumeral Periarthritis by Massotherapy and Functional ExerciseDocument3 pagesTreatment of Scapulohumeral Periarthritis by Massotherapy and Functional ExerciseRaluca CostandacheNo ratings yet
- Group 1A - 1 Nursing Care PlanDocument9 pagesGroup 1A - 1 Nursing Care PlanZent AquinoNo ratings yet
- Ehr PDFDocument31 pagesEhr PDFNicolai MabituinNo ratings yet
- Activity Intolerance For CvaDocument2 pagesActivity Intolerance For Cvalouie roderosNo ratings yet
- Lower Leg Fracture Compartment SyndromeDocument8 pagesLower Leg Fracture Compartment SyndromeKyuSheenNo ratings yet
- Case Studies of Documentation For PAMSDocument1 pageCase Studies of Documentation For PAMSmissbxbyNo ratings yet
- Iadt 07 I 1 P 50Document3 pagesIadt 07 I 1 P 50ariscoraNo ratings yet
- Demonstrate: Pain Coping TechniquesDocument4 pagesDemonstrate: Pain Coping TechniquesMae Therese B. MAGNO100% (1)
- 3 s2.0 B9780443067167000074 MainDocument3 pages3 s2.0 B9780443067167000074 MainKarthik BhashyamNo ratings yet
- Resolution of Intractable After Near-Infrared Irradiation of Relevant AcupointsDocument7 pagesResolution of Intractable After Near-Infrared Irradiation of Relevant Acupointsalcontado_80No ratings yet
- Plantar FasciitisDocument2 pagesPlantar FasciitisMouna MhedhbiNo ratings yet
- Ankylosing SpondylitisDocument4 pagesAnkylosing SpondylitisSHIVENDRA YADAVNo ratings yet
- Pancoast SyndromeDocument16 pagesPancoast SyndromePrincess HerreraNo ratings yet
- 2020 Hand and Wrist Pain - Clinical Diagnosis in Physical Medicine and RehabilitationDocument14 pages2020 Hand and Wrist Pain - Clinical Diagnosis in Physical Medicine and RehabilitationLộc Nguyễn ĐìnhNo ratings yet
- NCP Acute-PainDocument4 pagesNCP Acute-PainMarie CatapiaNo ratings yet
- Anton'S Syndrome and Cortical Blindness: Case ReportDocument3 pagesAnton'S Syndrome and Cortical Blindness: Case ReportDevasyaNo ratings yet
- NCP Ruq PainDocument3 pagesNCP Ruq PainKristine YoungNo ratings yet
- 1156 The Effects of Acupuncture Versus Sham Acupuncture in The Treatment of Fibromyalgia A Randomized Controlled Clinical Trial FileDocument6 pages1156 The Effects of Acupuncture Versus Sham Acupuncture in The Treatment of Fibromyalgia A Randomized Controlled Clinical Trial FileValdemar Caumo JuniorNo ratings yet
- Alvin Case 32 EDocument2 pagesAlvin Case 32 EIvyNo ratings yet
- Fascial Distortion Model - Vol.4Document76 pagesFascial Distortion Model - Vol.4Magno FilhoNo ratings yet
- Get. Better. Faster.: Integrative Sports Medicine as a Transformative Approach to Body, Bone, & Joint HealthFrom EverandGet. Better. Faster.: Integrative Sports Medicine as a Transformative Approach to Body, Bone, & Joint HealthNo ratings yet
- The Role of Acupuncture in Cancer Care From Symptom Alleviation To Tumor Suppression A Narrative ReviewDocument7 pagesThe Role of Acupuncture in Cancer Care From Symptom Alleviation To Tumor Suppression A Narrative ReviewrezteevicNo ratings yet
- Do Electrical Stimulation Devices Reduce Pain and Improve Function?-A Comparative ReviewDocument16 pagesDo Electrical Stimulation Devices Reduce Pain and Improve Function?-A Comparative ReviewrezteevicNo ratings yet
- Fpain 03 925013Document18 pagesFpain 03 925013rezteevicNo ratings yet
- Pharmacopuncture in Korea: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument20 pagesPharmacopuncture in Korea: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsrezteevicNo ratings yet
- Comparison of Electroacupuncture and Body Acupuncture On Gastrocnemius Muscle Tone in Children With Spastic Cerebral Palsy: A Single Blinded, Randomized Controlled Pilot TrialDocument6 pagesComparison of Electroacupuncture and Body Acupuncture On Gastrocnemius Muscle Tone in Children With Spastic Cerebral Palsy: A Single Blinded, Randomized Controlled Pilot TrialrezteevicNo ratings yet
- Effectiveness of Pharmacopuncture For Cervical Spondylosis: A Systematic Review and Meta-AnalysisDocument11 pagesEffectiveness of Pharmacopuncture For Cervical Spondylosis: A Systematic Review and Meta-AnalysisrezteevicNo ratings yet
- Ten-Year Phantom Limb Pain With Only Four Sessions of Fu's Subcutaneous Needling: A Case Report and Systematic ReviewDocument12 pagesTen-Year Phantom Limb Pain With Only Four Sessions of Fu's Subcutaneous Needling: A Case Report and Systematic ReviewrezteevicNo ratings yet
- Study of Latest Trend On Acupuncture For Obesity TreatmentDocument9 pagesStudy of Latest Trend On Acupuncture For Obesity TreatmentrezteevicNo ratings yet
- ELECTROACUPUNCTURE FOR ALLEVIATION OF PHANTOM LIMB PAIN : Case ReportDocument5 pagesELECTROACUPUNCTURE FOR ALLEVIATION OF PHANTOM LIMB PAIN : Case ReportrezteevicNo ratings yet
- The Effectiveness of acupuncture:TENS For Phantom Limb Syndrome. I - A Systematic Review of Controlled Clinical TrialsDocument10 pagesThe Effectiveness of acupuncture:TENS For Phantom Limb Syndrome. I - A Systematic Review of Controlled Clinical TrialsrezteevicNo ratings yet
- Auricular Therapy For Treating Phantom Limb Pain Accompanied by Jumping Residual Limb: A Short Review and Case StudyDocument11 pagesAuricular Therapy For Treating Phantom Limb Pain Accompanied by Jumping Residual Limb: A Short Review and Case StudyrezteevicNo ratings yet
- Brain Responses To Acupuncture Stimulation in The Prosthetic Hand of An Amputee PatientDocument6 pagesBrain Responses To Acupuncture Stimulation in The Prosthetic Hand of An Amputee Patientrezteevic100% (1)
- Legalizing MarijuanaDocument3 pagesLegalizing MarijuanaAlyssa MabalotNo ratings yet
- Tall StatureDocument24 pagesTall StaturedianmutiaNo ratings yet
- A R Are Case of Amyands Hernia With Mucocele AppendixDocument2 pagesA R Are Case of Amyands Hernia With Mucocele AppendixRajeev ThilakNo ratings yet
- Soft Contact Lens FitiingDocument2 pagesSoft Contact Lens FitiingLigia BoazuNo ratings yet
- AUBF LAB - Exams and QuizzesDocument18 pagesAUBF LAB - Exams and QuizzesLUALHATI VILLASNo ratings yet
- BOLILE ESOFAGUL Mia TareDocument12 pagesBOLILE ESOFAGUL Mia Tareelisabeth-ward-skipNo ratings yet
- STEMI Care Reperfusions Trategy - DR Eka GinanjarDocument39 pagesSTEMI Care Reperfusions Trategy - DR Eka GinanjarIra MashadiNo ratings yet
- Mechanism of AutoimmunityDocument29 pagesMechanism of AutoimmunityMalliga SundareshanNo ratings yet
- Safety Evaluation of Ethanol Extracts From Bosenbergia Rotunda L. Mansf. in Male RatsDocument4 pagesSafety Evaluation of Ethanol Extracts From Bosenbergia Rotunda L. Mansf. in Male RatsdanisujanaNo ratings yet
- Robertson2013 PDFDocument88 pagesRobertson2013 PDFArini NurlelaNo ratings yet
- Sodium Bicarbonate: PresentationDocument3 pagesSodium Bicarbonate: Presentationmadimadi11100% (1)
- Braun Neurology Endoscope SystemDocument132 pagesBraun Neurology Endoscope SystemMārcis RancānsNo ratings yet
- History Taking: Ma. Sheila Blossom B. Bo RM, RN, MmeDocument14 pagesHistory Taking: Ma. Sheila Blossom B. Bo RM, RN, Mmejhayrus pletaNo ratings yet
- Homeostasis Grade XDocument32 pagesHomeostasis Grade XFebrian Andrei100% (1)
- MCN ExamDocument3 pagesMCN ExamronronNo ratings yet
- Compartment Syndrome: Kyle MillerDocument17 pagesCompartment Syndrome: Kyle MillerBudiono Gunawan SutantoNo ratings yet
- Psychiatry: Psychology-Psychiatric Evaluation - 1 (Medical Transcription Sample Report)Document7 pagesPsychiatry: Psychology-Psychiatric Evaluation - 1 (Medical Transcription Sample Report)Nguyên VũNo ratings yet
- Original Article: Objective MethodsDocument9 pagesOriginal Article: Objective MethodsI Made AryanaNo ratings yet
- What Is Blood Pressure MonitoringDocument1 pageWhat Is Blood Pressure Monitoringapi-725875845No ratings yet
- Lilbm3: Adita Ayu Aprilia 30101407112Document16 pagesLilbm3: Adita Ayu Aprilia 30101407112Adita AyuNo ratings yet
- Impetigo and CHMDocument2 pagesImpetigo and CHMcbrammah9357No ratings yet
- HeunceutDocument8 pagesHeunceutSovian Anugrah Lumban GaolNo ratings yet
- Jelkd Jeo QWNDocument25 pagesJelkd Jeo QWNcd_armand1885No ratings yet
- Vulvodynia New Concepts and Review of The LiteratureDocument16 pagesVulvodynia New Concepts and Review of The LiteratureMuhammad SyamaniNo ratings yet
- Chapter 2 Death and Postmortem ChangesDocument72 pagesChapter 2 Death and Postmortem Changesdebbytenri100% (1)
- National Filaria Control ProgrammeDocument2 pagesNational Filaria Control ProgrammeFoysal Sirazee100% (1)