Professional Documents
Culture Documents
Icu CP
Icu CP
Uploaded by
Jezner GamosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Icu CP
Icu CP
Uploaded by
Jezner GamosCopyright:
Available Formats
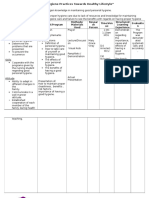
NURSING SYSTEM REVIEW CHART
Name___Omac, Alquin_______________________ Date_September 5, 2011 Vital Signs: Pulse_124__ BP_100/60__ TEMP.__39.7__ Heigth__55__ Weigth__65__
INSTRUCTIONS: Place an [X] in the area of abnormality. Comment at the space provided. Indicate the location of the problem in the figure using [X]. EENT: [ ] impaired vision [ ] blind [X] pain [ ] reddened [ ] drainage [ ] gums [ ] hard of hearing [ ] deaf [ ] burning [ ] edema [ ] lesion [ ] teeth Assess eyes, ears, nose throat for abnormalities. [ ] no problem RESPIRATORY: [ ] asymmetric [ ] tachypnea [ ] apnea [ ] rales [X] cough [ ] barrel chest [ ] bradypnea [ ] shallow [ ] rhonchi [X] sputum [ ] diminished [X] dyspnea [ ] orthopnea [ ] labored [X ] wheezing [ ] pain [ ] cyanotic Assess resp. rate, rhythm, pulse blood breath sounds, comfort [ ] no problem CARDIOVASCULAR: [ ] arrhythmia [X] tachycardia [ ] numbness [ ] diminished pulses [ ] edema [X ] fatigue [X] irregular [ ] bradycardia [ ] murmur [ ] tingling [ ] absent pulses [ ] pain Assess heart sound, rate, rhythm, pulse, blood pressure. circulation, fluid retention, comfort [ ] no problem GASTROINTESTINAL TRACT: [ ] obese [] distention [ ] mass [ ] dysphagia [ ] rigidity [ ] pain Assess abdomen, bowel habits, swallowing bowel sounds, comfort. [ X] no problem GENITO-URINARY AND GYNE: [ ] pain [ ] urine color [ ] vaginal bleeding [ ] hematuria [ ] discharge [ ] nocturia assess urine frequency, control, color, odor, comfort, gyne bleeding, discharge [X] no problem NEURO: [ ] paralysis [ ] stuporous [ ] unsteady [ ] seizures [ ] lethargic [X ] comatose [ ] vertigo [ ] tremors [ ] confused [ ] vision [ ] grip assess motor, function, sensation, LOC, strength grip, gait, coordination, speech [x] no problem MUSCULOSKELETAL AND SKIN: [ ] appliance [ ] stiffness [ ] itching [ ] petechiae [X ] hot [ ] drainage [ ] prosthesis [ ] swelling [ ] lesion [ ] poor turgor [ ] cool [] deformity [] wound [ ] rash [X ] skin color [X] flushed [ ] atrophy [] pain [ ] ecchymosis [ ] diaphoretic [ ] moist assess mobility, motion, gait, alignment, joint function skin color, texture, turgor, integrity [ ] no problem _-Endotracheal Tube _- manual ambubag ________________ ________________ __none eye opening_ ___________________ _ ____ ________ ___________ _-_cough, sputum, __dyspnea,_____ _- wheezing sound __both lungs____ __________________ __________________ __Tachycardia___ __irregular 124bpm_ __________________ __________________ ___foley bag catheter_ ___attached to uro bag __________________ __________________ __________________ __________________ __________________ __________________ _____________ __________________ _____________ ________________ __________________ ______________ _____________ _____ __________________ ___hot to touch_ ___flushed skin____ ___temp 39.7 C____ ______________ __________________ __________________ ___Comatose__ _____________ ____________ ___ __________ __________________ _________________ __________________ __________________ __________________ ______________ __ __________
Nursing System Review Chart II
SUBJECTIVE
OBJECTIVE
COMMUNICATION: ( ) Hearing Loss () Denied
( ) Glasses ( ) Contact Lenses Aide Pupil size ____3mm_
( ) Languages ( ) Hearing
( ) Speech Difficulties Reaction: PERRLA- Pupil Equally Round Reactive to Light and Accommodation OXYGENATION: ( ) Dyspnea (x) Smoking History _________________ ( ) Cough ( ) Sputum ( ) Denied CIRCULATION ( ) Chest Pain Heart Rhythm ( ) Regular Ankle Edema ( - ) Pulse R_ L_ Car Rad _+______+_ + _ _ _+_ ( ) Irregular Resp. ( x ) Regular ( ) Irregular Describe: SlightlyTachypneicR _______________________________
L_______________________________
() Leg Pain
( ) Numbness of Extremities ( x ) Denied NUTRITION Diet: _ [ ]N [ ]V DP _+ +
comments
(x ) Dentures Full Upper ( ) Lower ( )
( ) None Partial With Pt. ( ) ( ) ( ) ( )
( ) recent change in weight, appetite ( ) Swallowing Difficulty ( ) Denied
SUBJECTIVE Elimination: Usual Bowel pattern Urinary frequency ___ _ ________ Constipation remedy ( ) Urgency ___ ___ ( ) Dysuria Date of Last BM ( ) Hematuria ___ _ ( ) Incontinence Diarrhea (character) ( ) Polyuria _ _ ___ ( ) Foley in place (X ) Denied
OBJECTIVE Comments: Change in bowel habits noted Bowel sounds: audible hypoactive bowel sounds Abd. Distention ( ) yes (X) No
MNGT OF HEALTH & ILLNESS (x ) Alcohol ( ) Denied (amount and frequency) Last Pap Smear __ LMP SKIN INTEGRITY: ( ) Dry ( ) Itching ( ) Denied
Briefly describe patients ability to follow treatments (diet, meds, etc) Patient claims to follow prescribed treatment regimen as long as financially able. ( ) Dry ( ) Cold ( ) Flushed ( ) Warm ( ) Cyanotic ( )Pale ( ) Moist
ACTIVITY/SAFETY ( ) Convulsion ( ) Dizziness ( ) Limited motion of joints Limitation in ability to ( ) Ambulate ( ) Bathe Self ( ) other ( ) Denied
( ) LOC and Orientation . Gait: ( ) Walker ( ) Cane ( )others ( ) Steady ( ) Unsteady ( ) Sensory and Motor Losses in face or extremities: ( ) ROM Limitation
SUBJECTIVE COMFORT/SLEEP/AWAKE () Pain (Location, frequency Remedies) ( ) Nocturia ( ) Sleep difficulty ( ) Denied
OBJECTIVE () Facial Grimace ( ) Guarding ( ) Other signs of pain None
COPING: Occupation: Members of Household: Most Supportive Person:
Observe non verbal behavior Patient displays enthusiasm in answering the student nurses question although its clear that she is uncomfortable in her current state. Person and phone number that can be reached any time:
SPECIAL PATIENT INFORMATION (USE LEAD PENCIL) ________Daily Weight __________PT/OT____________ ________BP q Shift ________Irradiation___________ ________Neuro vs _________Urine Test__________ ________CVP/SG. Reading_______ ________24 Hour Urine collection
Date Ordered
Diagnostic/Laboratory Exams
Date done
Date Ordered
I.V Fluids/Blood
Date Disc
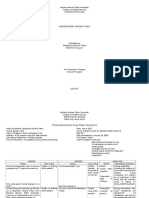
Liceo de Cagayan University Cagayan De Oro City
DATA BASE AND HISTORY
Name_________________________________ Civil Status_________ Income__________ Sex____ Age____ Rel _______ Nationality___________________ Informant______________________________
Date Adm.__________ Time_______
Temperature______ Pulse Rate ______ Resp. Rate _______ BP _______ Height ______ Weight ______
Chief complaint and History of Present Illness
Type of Previous Illness/ Pregnancy/Delivery Date
Type of Previous Illness/ Pregnancy/Delivery Date
Has received blood in the past:_____________ Yes __________ No if yes, list dates _______ Reaction _______________ Yes ___________ No Allergies:
Medication name
Dose/ Frequency
Time of Last Dose
Medication name
Dose/ Frequency
Time of Last Dose
Admitting diagnosis: __________________________________________________________________ Attending Physician: ______________________________
Score ___________Grade __________
You might also like
- ADHD RS IV Tear Pad With Adult PromptsDocument2 pagesADHD RS IV Tear Pad With Adult Promptsmihaela neacsu100% (1)
- Case Study Bell's PalsyDocument13 pagesCase Study Bell's PalsyEga ArnasyaNo ratings yet
- Nursing System Review ChartDocument2 pagesNursing System Review ChartifancyouuuNo ratings yet
- MS 3 Case Analysis DownloadableDocument1 pageMS 3 Case Analysis DownloadableCharissa Magistrado De LeonNo ratings yet
- NCP EsrdDocument2 pagesNCP EsrdAziil LiizaNo ratings yet
- Autism Pathways To Recovery Workbook PDFDocument84 pagesAutism Pathways To Recovery Workbook PDFfumiNo ratings yet
- About The Glucogauge Monitor - Kurt Stewart, Director, Customer InsightsDocument1 pageAbout The Glucogauge Monitor - Kurt Stewart, Director, Customer InsightsHarish RedquestNo ratings yet
- VI. Nursing Assessment: Nursing System Review ChartDocument3 pagesVI. Nursing Assessment: Nursing System Review ChartEleanor MaandigNo ratings yet
- PathophysiologyDocument9 pagesPathophysiologySuzette PipoNo ratings yet
- Log of Activities No. 2: San Francisco St. Butuan City 8600, Region XIII Caraga, Philippines NursingDocument2 pagesLog of Activities No. 2: San Francisco St. Butuan City 8600, Region XIII Caraga, Philippines NursingMay Chelle ErazoNo ratings yet
- ReflectionDocument42 pagesReflectionRaidis PangilinanNo ratings yet
- Potts DiseaseDocument8 pagesPotts Diseaseaimeeros0% (2)
- Family Health Assessment FormDocument7 pagesFamily Health Assessment FormBiway RegalaNo ratings yet
- NCM 118 Medsurg EndtermDocument25 pagesNCM 118 Medsurg EndtermJmarie Brillantes PopiocoNo ratings yet
- COPAR Tally SheetDocument3 pagesCOPAR Tally SheetAnna SarmientoNo ratings yet
- NVS Written ReportDocument20 pagesNVS Written ReportbabiNo ratings yet
- Chain of Survival: Adult and Pediatric Out of Hospital Cardiac ArrestDocument10 pagesChain of Survival: Adult and Pediatric Out of Hospital Cardiac ArrestJapeth John M. FloresNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationMary Hope BacutaNo ratings yet
- Personal-Soc Interpretation: Tower of 4 CubesDocument15 pagesPersonal-Soc Interpretation: Tower of 4 CubesteuuuuNo ratings yet
- Related To Limited Financial ResourcesDocument2 pagesRelated To Limited Financial ResourcesDan HizonNo ratings yet
- CHN Post Test MT2Document16 pagesCHN Post Test MT2Rika MaeNo ratings yet
- MARY GRACE (CHN) Final Presentation For FNCPDocument6 pagesMARY GRACE (CHN) Final Presentation For FNCPMary grace VirayNo ratings yet
- RiskforMaternal-FetalDyad CS#2Document2 pagesRiskforMaternal-FetalDyad CS#2Casilao, Mike Arone BSN-IVBNo ratings yet
- Intussusception: PathophysiologyDocument8 pagesIntussusception: PathophysiologyNaufal AndaluNo ratings yet
- Focus Charting in Pediatric Ward: Medsurgical ClinicalDocument2 pagesFocus Charting in Pediatric Ward: Medsurgical Clinical2A - Nicole Marrie HonradoNo ratings yet
- Bernard Narrative Evaluation ReportDocument4 pagesBernard Narrative Evaluation ReportAldwin Compra QuiñoNo ratings yet
- College of Nursing: Xavier University Ateneo de CagayanDocument7 pagesCollege of Nursing: Xavier University Ateneo de CagayanShamsa AfdalNo ratings yet
- Famacion - CHN - General Requirements Week 3Document3 pagesFamacion - CHN - General Requirements Week 3Kyra Bianca R. FamacionNo ratings yet
- AppendicitisDocument34 pagesAppendicitisLex Gabon-AndayaNo ratings yet
- CHN Notes PrelimDocument30 pagesCHN Notes PrelimCHINGCHONG SLAYERNo ratings yet
- FNCP On Elevated Blood Pressure 2Document4 pagesFNCP On Elevated Blood Pressure 2Aaron EspirituNo ratings yet
- Splints and Casts Indications and MethodsDocument9 pagesSplints and Casts Indications and MethodsJay GaneshNo ratings yet
- NPI NCMH StephDocument12 pagesNPI NCMH StephAnonymous 2fUBWme6wNo ratings yet
- Problems With The 4ps of LaborDocument10 pagesProblems With The 4ps of LaborhoohooNo ratings yet
- Social Investigation Report FormDocument10 pagesSocial Investigation Report FormPpd Pmo ZamboangaNo ratings yet
- CeferoximeDocument1 pageCeferoximeGwen Stefanie Lagrimas ValloyasNo ratings yet
- St. Paul University Philippines: Scenario 1Document2 pagesSt. Paul University Philippines: Scenario 1Miguel LigasNo ratings yet
- Case Study FormatDocument5 pagesCase Study FormatEden OlasabNo ratings yet
- BARANDINO, Jia Laurice (Gouty Arthritis)Document18 pagesBARANDINO, Jia Laurice (Gouty Arthritis)Deinielle Magdangal RomeroNo ratings yet
- Health Assessment ToolDocument3 pagesHealth Assessment ToolGail GenturalezNo ratings yet
- NCPDocument10 pagesNCPbabycheska08No ratings yet
- Family Nursing Care Plan TypologyDocument6 pagesFamily Nursing Care Plan TypologyLouwella RamosNo ratings yet
- Application Balanced Skeletal TractionDocument6 pagesApplication Balanced Skeletal TractionLorenz ChristopherNo ratings yet
- Midterm Topics After Hygiene 1Document39 pagesMidterm Topics After Hygiene 1Budoy WashupapiNo ratings yet
- Physical Examination and Review of Systems: Patient's Name / Room No. - 1Document3 pagesPhysical Examination and Review of Systems: Patient's Name / Room No. - 1Raf DalidigNo ratings yet
- Health Teaching Community Health NursingDocument3 pagesHealth Teaching Community Health NursingKyla Castro100% (1)
- Pathophysiology, Bone CancerDocument7 pagesPathophysiology, Bone CancerMaria Grace Raquel Ormeneta100% (1)
- Individual Activity 3 PDFDocument11 pagesIndividual Activity 3 PDFBanana QNo ratings yet
- Annotated Group 2 Impetigo Concept Mapping 1Document30 pagesAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANONo ratings yet
- Environmental SanitationDocument5 pagesEnvironmental SanitationNessa Layos MorilloNo ratings yet
- Problem IdentificationDocument3 pagesProblem IdentificationkgxviiNo ratings yet
- 100 Item MEDICAL SURGICAL Nursing Examination Correct Answers andDocument12 pages100 Item MEDICAL SURGICAL Nursing Examination Correct Answers andZyntrx VillasNo ratings yet
- Group 5 - Experiment No.10 - Culture and SensitivityDocument11 pagesGroup 5 - Experiment No.10 - Culture and SensitivityPMG BrightNo ratings yet
- Community Health Survey ToolDocument5 pagesCommunity Health Survey ToolJohn Alex Maramba MelencioNo ratings yet
- Case Study AGE With Signs of DehydrationDocument27 pagesCase Study AGE With Signs of DehydrationZhenmeiNo ratings yet
- Concept Map Group 1Document1 pageConcept Map Group 1eric macabiog100% (1)
- NCM 104 RLE Module 3 FinalsDocument22 pagesNCM 104 RLE Module 3 FinalsAlexander DontonNo ratings yet
- Acute Gastroenteritis With Severe DehydrationDocument22 pagesAcute Gastroenteritis With Severe DehydrationCess Dunwan100% (1)
- Impaired Tissue Integrity FinalDocument1 pageImpaired Tissue Integrity Finaljanine marie oraizNo ratings yet
- CHN 2 Lec - Week 12 Documentation and ReportingDocument12 pagesCHN 2 Lec - Week 12 Documentation and Reportingyuuki konnoNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- VI. Nursing Assessment (System Review & Nsg. Assessment II)Document11 pagesVI. Nursing Assessment (System Review & Nsg. Assessment II)NursingNooBNo ratings yet
- Drug StudyDocument3 pagesDrug StudyGladz Talla-ReyesNo ratings yet
- Cardiovascular Assessment LabDocument6 pagesCardiovascular Assessment Labahmad.a.touseefNo ratings yet
- Adat NontoniDocument20 pagesAdat NontoniArva RayhanNo ratings yet
- Unit 2. ConsequencesDocument9 pagesUnit 2. ConsequencesFabianaNo ratings yet
- Paho-Cdc Generic Protocol Influenza SurveillanceDocument45 pagesPaho-Cdc Generic Protocol Influenza SurveillanceSeptya Zee KaunangNo ratings yet
- Congestive Heart Failure: Dr. J. SaravananDocument31 pagesCongestive Heart Failure: Dr. J. Saravananpetervazhayil100% (1)
- Artemether LumefantrineDocument43 pagesArtemether LumefantrineneisslabsNo ratings yet
- Medicines For Children Rationale and Recent AdvancDocument15 pagesMedicines For Children Rationale and Recent AdvancSmruti RanjanNo ratings yet
- Juvenile Hallux Valgus PDFDocument14 pagesJuvenile Hallux Valgus PDFŞtefaniuc IulianNo ratings yet
- Tiens AculifeDocument6 pagesTiens AculifeKabir Ahmed Kamal100% (2)
- Urine Procedure WordDocument27 pagesUrine Procedure WordYashly VargheseNo ratings yet
- The Concise Surgery Review Manual For The ABSITE & BoardsDocument218 pagesThe Concise Surgery Review Manual For The ABSITE & BoardsAlena JosephNo ratings yet
- Hematuria: Gross Versus Microscopic HematuriaDocument2 pagesHematuria: Gross Versus Microscopic HematuriaShintia Theresia LumempouwNo ratings yet
- ITP Management of Adult Patients With Immune Thrombocytopenia ITPDocument12 pagesITP Management of Adult Patients With Immune Thrombocytopenia ITPqayyum consultantfpscNo ratings yet
- Day Laboratory Analysis Critical Care Sweet Mrs. Dee Sy 2Document4 pagesDay Laboratory Analysis Critical Care Sweet Mrs. Dee Sy 2MARIA HILARY TABLANTENo ratings yet
- Phrases and Process For HypnosisDocument45 pagesPhrases and Process For HypnosisUmair UsmanNo ratings yet
- Journal Club Presentation: DR Waleed AhmadDocument30 pagesJournal Club Presentation: DR Waleed Ahmadkaram aliNo ratings yet
- GEHealthcare Brochure Aespire 7900Document6 pagesGEHealthcare Brochure Aespire 7900Andy MolinaNo ratings yet
- Cruz BG 1Document408 pagesCruz BG 1kimNo ratings yet
- DNA Flow Technology - 2016Document2 pagesDNA Flow Technology - 2016Uswatun hasanah harifuddinNo ratings yet
- Cortisone InjectionDocument2 pagesCortisone InjectionJulioNo ratings yet
- Ascending Pathways (Physiology)Document4 pagesAscending Pathways (Physiology)Aswin AjayNo ratings yet
- Risk Assessment Film TrailerDocument1 pageRisk Assessment Film TrailerZara MartincevicNo ratings yet
- Nilai, Absen AtlsDocument7 pagesNilai, Absen AtlsAyu Yuyun PaembonanNo ratings yet
- Varcarolis Halter TherCommTechniqDocument5 pagesVarcarolis Halter TherCommTechniqeatthescrollNo ratings yet
- CordycepsDocument13 pagesCordycepsDa NaNo ratings yet
- Abdominal Wall Hernias - Principles and Management.Document797 pagesAbdominal Wall Hernias - Principles and Management.Hermina Dicu100% (3)