Professional Documents
Culture Documents
Sbar Communication Required Reading
Sbar Communication Required Reading
Uploaded by
TwilaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sbar Communication Required Reading
Sbar Communication Required Reading
Uploaded by
TwilaCopyright:
Available Formats
lOMoARcPSD|22846685
SBAR Communication Required Reading
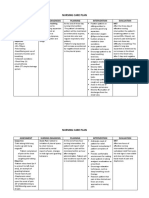
nursing care plan (Firelands School of Nursing)
Studocu is not sponsored or endorsed by any college or university
Downloaded by Twila Thurston (twilathurston5@gmail.com)
lOMoARcPSD|22846685
SBAR: Situation-Backgroun d-
Assessm ent-Recom m endation
The SBAR (Situation-Background-Assessm ent-Recom m endation) technique provides a fram ework for
com m unication between m em bers of the health care team about a patient's condition. SBAR is an easy-to-
rem em ber, concrete m echanism useful for fram ing any conversation, especially critical ones, requiring a
clinician’s im m ediate attention and action. It allows for an easy and focused way to set expectation s for what will
be com m unicated and how between m em bers of the team , which is essential for developing team work and
fostering a culture of patient safety.
This tool includes:
• SBAR Guidelin es (“Guidelines for Com m unicating with Physicians Using the SBAR Process”): Explains in
detail how to im plem ent the SBAR technique
• SBAR Worksheet: A worksheet/ script that a provider can use to organize inform ation in preparation for
com m unicating with a physician about a critically ill patient (includes both an exam ple and a blank SBAR
Worksheet tem plate)
Both the worksheet and the guidelines use the physician team m em ber as th e exam ple; however, they can be
adapted for use with all other health profession als.
Michael Leonard, MD, Physician Leader for Patient Safety, along w ith colleagues Doug Bonacum and Suzanne
Graham at Kaiser Perm anente of Colorado (Evergreen, Colorado, USA) developed this com m unication tool,
w hich w as adapted from the US Navy. The SBAR technique has been im plem ented w idely at health system s such
as Kaiser Perm anente.
NOTE: Before filling out the template, first save the file on your computer. Then open and use that version of the
tool. Otherwise, your changes will not be saved.
Copyright © 20 17 In stitute for Healthcare Im provement. All rights reserved. Individuals may photocopy these materials for educational, not-for-profit uses, provided that
the con ten ts are not altered in any way and that proper attribution is given to IHI as the source of the content. These m aterials may not be reproduced for com mercial,
for-profit use in an y form or by any means, or republished under any circum stances, without the written perm ission of the Institute for Healthcare Improvement.
Downloaded by Twila Thurston (twilathurston5@gmail.com)
lOMoARcPSD|22846685
SBAR: Situation-Backgrou n d-Assessmen t-Recommen dation
Guidelines for Communicating with
Physicians Using the SBAR Process
1) Use the following m odalities according to physician preferen ce, if known. Wait n o longer than
five minu tes between attempts.
o Direct page (if known)
o Physician’s Call Service
o During weekdays, the physician’s office directly
o On weekends and after hours during the week, physician’s hom e phone
o Cell phone
Before assuming that the physician you are attem pting to reach is not responding, utilize all
m odalities. For em ergent situations, use appropriate resident service as n eeded to ensure safe
patient care. Start by definin g the first and th e last step in the process — so that everyone has
a shared understanding of where the process you’re working on begins and ends.
2) Prior to calling the physician, follow these steps:
o Have I seen and assessed the patient m yself before calling?
o Has the situation been discussed with resource nurse or preceptor?
o Review the chart for appropriate physician to call.
o Know the admitting diagnosis and date of admission.
o Have I read the most recent MD progress notes and notes from the nurse who worked the
shift ahead of m e?
o Have available the following when speaking with the physician:
- Patient’s chart
- List of current m edications, allergies, IV fluids, and labs
- Most recent vital signs
- Reporting lab results: provide the date and time test was done and results of previous
tests for comparison
- Code status
3) When calling the physician , follow the SBAR process:
( S) Sit u a t io n : What is the situation you are calling about?
o Identify self, unit, patient, room num ber.
o Briefly state the problem , what is it, when it happened or started, and how severe.
( B) Ba ck gr o u n d : Pertinent background inform ation related to the situation could include
the following:
o The adm itting diagnosis and date of admission
o List of current m edications, allergies, IV fluids, and labs
Institute for Healthcare Improvement ∙ ihi.org | This SBAR tool was developed by Kaiser Permanente. Please feel free to use and reproduce these
materials in the spirit of patient safety, and please retain this footer in the spirit of appropriate recognition.
Downloaded by Twila Thurston (twilathurston5@gmail.com)
lOMoARcPSD|22846685
SBAR: Situation-Backgrou n d-Assessmen t-Recommen dation
o Most recent vital signs
o Lab results: provide the date and tim e test was don e and results of previous tests for
comparison
o Other clinical inform ation
o Code status
( A) As s e s s m e n t : What is the nurse’s assessm ent of the situation?
( R ) R e co m m e n d a t io n : What is the nurse’s recom m endation or what does he/ she want?
Examples:
o Notification that patient has been adm itted
o Patient needs to be seen now
o Order change
4) Docum ent the change in the patient’s condition and physician notification.
Example 1: SBAR Report to Physician about a Critical Situation
Situation
S Dr. Jones, this is Sharon Smith calling from the CCU. I have Mr. Holloway in Room 217, a 55-
year-old man who looks pale and sweaty, feels confused and weak, and is complaining of chest
pressure.
Background
B • He has a history of HTN.
• He was admitted for a GI bleed, received 2 units.
• His last crit two hours ago was 31.
• His vital signs are BP 90/50, pulse 120.
Assessment
A I think he’s got an active bleed and we can’t rule out an MI, but we don’t have a troponin or a
recent H&H.
Recommendation
R I’d like to get an EKG and labs, and I need for you to evaluate him right away.
Institute for Healthcare Improvement ∙ ihi.org | This SBAR tool was developed by Kaiser Permanente. Please feel free to use and reproduce these
materials in the spirit of patient safety, and please retain this footer in the spirit of appropriate recognition.
Downloaded by Twila Thurston (twilathurston5@gmail.com)
lOMoARcPSD|22846685
SBAR: Situation-Backgrou n d-Assessmen t-Recommen dation
Example 2: SBAR Report to a Primary Care Physician
Situation
S Patient arrived for appointment on wrong day.
Background
B • Patient arrived for 11:00AM appointment today.
• Appointment is scheduled for 11:00AM tomorrow.
• Patient comes from 40 miles away and needed to have friend drive them to
appointment.
• Doctor has 1+ appointment available on schedule.
• Doctor’s hall partner has some open times.
• We don’t know if the mistake was with the patient or the call center.
A Assessment
We should see the patient today.
Recommendation
R I recommend that we use the 1+ time or have your hall partner see this patient.
Institute for Healthcare Improvement ∙ ihi.org | This SBAR tool was developed by Kaiser Permanente. Please feel free to use and reproduce these
materials in the spirit of patient safety, and please retain this footer in the spirit of appropriate recognition.
Downloaded by Twila Thurston (twilathurston5@gmail.com)
lOMoARcPSD|22846685
SBAR: Situation-Backgrou n d-Assessmen t-Recommen dation
Before filling out the tem plate, first save the file on your com puter. Then open and use that version of the tool. Otherwise, your changes will not be saved.
Template: SBAR
Situation: What is the situation you are calling about?
S • Identify self, unit, patient, room number.
• Briefly state the problem, what is it, when it happened
or started, and how severe.
Background: Pertinent background information related to
B the situation could include the following:
• The admitting diagnosis and date of admission
• List of current medications, allergies, IV fluids, and labs
• Most recent vital signs
• Lab results: provide the date and time test was done
and results of previous tests for comparison
• Other clinical information
• Code status
Assessment: What is the nurse’s assessment of the
A situation?
Recommendation: What is the nurse’s recommendation
R or what does he/she want? Examples:
• Notification that patient has been admitted
• Patient needs to be seen now
• Order change
Institute for Healthcare Improvement ∙ ihi.org | This SBAR tool was developed by Kaiser Permanente. Please feel free to use and reproduce these materials in the spirit of patient safety, and please
retain this footer in the spirit of appropriate recognition.
Downloaded by Twila Thurston (twilathurston5@gmail.com)
You might also like
- Winninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualDocument66 pagesWinninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualTiglao, Camile Ann C.0% (1)
- Nursing Midwifery Staff CBAHI QuestionsDocument13 pagesNursing Midwifery Staff CBAHI QuestionsnasserjubranNo ratings yet
- Nurs 208 Final EvaluationDocument11 pagesNurs 208 Final Evaluationapi-351047631No ratings yet
- Strategic Considerations in Treatment Planning Deciding When To Treat, Extract, or Replace A Questionable Tooth PDFDocument12 pagesStrategic Considerations in Treatment Planning Deciding When To Treat, Extract, or Replace A Questionable Tooth PDFItzel Marquez100% (1)
- SBAR - Template PDFDocument5 pagesSBAR - Template PDFHosam GomaaNo ratings yet
- Hospital SopsDocument12 pagesHospital Sopspratimaz83% (6)
- SafetyToolkit SBARDocument5 pagesSafetyToolkit SBARILANGO T PNo ratings yet
- SBAR Technique For Communication: A Situational Briefing ModelDocument3 pagesSBAR Technique For Communication: A Situational Briefing ModelRuang DahliaNo ratings yet
- SbarDocument1 pageSbarchibimakuNo ratings yet
- Sbar Communication ToolDocument7 pagesSbar Communication ToolDyanne Bautista100% (1)
- SBAR Communication GuidelinesDocument2 pagesSBAR Communication GuidelinesmonabertNo ratings yet
- Bedside Shift Report Checklist: S B A RDocument2 pagesBedside Shift Report Checklist: S B A RKylie StangNo ratings yet
- ISBARDocument4 pagesISBARvhonNo ratings yet
- Prioritization LectureDocument6 pagesPrioritization LecturesamNo ratings yet
- NT1 - Sim - STD - 240306 2Document8 pagesNT1 - Sim - STD - 240306 2vitagp1124No ratings yet
- S Bar GuidelinesDocument2 pagesS Bar GuidelinesScribdNo ratings yet
- Sbar Communication ToolDocument1 pageSbar Communication ToolJay LoNo ratings yet
- Req AnswersDocument4 pagesReq AnswersANDREW DEL ROSARIONo ratings yet
- SBARDocument12 pagesSBARakoeljames8543No ratings yet
- Wm. Jennings Bryan Dorn VAMC Patient Safety TrainingDocument39 pagesWm. Jennings Bryan Dorn VAMC Patient Safety Trainingkamnasharma0907No ratings yet
- ReportingDocument4 pagesReportingErika MarieNo ratings yet
- Care of The Older Adult-SAS 1Document5 pagesCare of The Older Adult-SAS 1Gia Lourdes Camille AustriaNo ratings yet
- JCI PresentationDocument66 pagesJCI PresentationOsama MarzoukNo ratings yet
- My Hospital FacilitiesDocument10 pagesMy Hospital Facilities3E, KENNADY KARUNAKARAN, PRINCENo ratings yet
- Nursing: Ns. Ketut Lisnawati, S.Kep., M.Kep., SP - Kep.M.BDocument24 pagesNursing: Ns. Ketut Lisnawati, S.Kep., M.Kep., SP - Kep.M.BNi Made Ananda Candra Rahmitha Putri KepakisanNo ratings yet
- SBAR PresentationDocument44 pagesSBAR PresentationJelly Rose Bajao Otayde100% (1)
- IPSG May28Document62 pagesIPSG May28S. Pichammal - Quality ManagerNo ratings yet
- The Health Care Process: April T. CajandigDocument26 pagesThe Health Care Process: April T. CajandigIra Louise Paraguya ParejaNo ratings yet
- Disability FormDocument3 pagesDisability FormssansomNo ratings yet
- National Patient Safety Goals Allied Health Inservice July 2023Document7 pagesNational Patient Safety Goals Allied Health Inservice July 2023pjpriiiNo ratings yet
- "Hand-Off Communication" Sbar: Google Automatically Generates HTML Versions of Documents As We Crawl The WebDocument3 pages"Hand-Off Communication" Sbar: Google Automatically Generates HTML Versions of Documents As We Crawl The WebclarimerNo ratings yet
- Ipsg 2017Document41 pagesIpsg 2017hum JavedNo ratings yet
- Management and Legal Issues 1Document42 pagesManagement and Legal Issues 1Victor FabunmiNo ratings yet
- Care Plan Handbook TemplateDocument34 pagesCare Plan Handbook TemplateBreanna Hopkins100% (1)
- Dec 21 23 Case Study ModuleDocument7 pagesDec 21 23 Case Study ModuleKristian Karl Bautista Kiw-isNo ratings yet
- Nursing Staff & Anesthesia Technicians in DPUDocument10 pagesNursing Staff & Anesthesia Technicians in DPUnasserjubranNo ratings yet
- Nama: No. CM: Ruangan:: Formulir Potensi KegawatanDocument3 pagesNama: No. CM: Ruangan:: Formulir Potensi KegawatanriniNo ratings yet
- Pengkajian Modul 6 Materi EnglishDocument10 pagesPengkajian Modul 6 Materi EnglishNurmala Deska ApriliaNo ratings yet
- J Aorn 2015 02 012Document8 pagesJ Aorn 2015 02 012Yahia HassaanNo ratings yet
- Communication: Improving Patient Safety With SbarDocument7 pagesCommunication: Improving Patient Safety With Sbarria kartini panjaitanNo ratings yet
- Mostcommonquestionsofcbahi Azza 230211125221 89d97424Document58 pagesMostcommonquestionsofcbahi Azza 230211125221 89d97424amal.jaberNo ratings yet
- Ob-Gyn For The Generalist: International Patient Safety Goals (IPSG)Document8 pagesOb-Gyn For The Generalist: International Patient Safety Goals (IPSG)carmsNo ratings yet
- Winninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualDocument25 pagesWinninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualBryanEdwardsmqtj100% (41)
- Administrative Medical Assisting 8th Edition French Solutions ManualDocument25 pagesAdministrative Medical Assisting 8th Edition French Solutions ManualErikKeithnwmp100% (60)
- Evolution Note.Document22 pagesEvolution Note.ScribdTranslationsNo ratings yet
- Navy Corpsman Sick Call Screeners GuideDocument215 pagesNavy Corpsman Sick Call Screeners GuidejustanothergunnutNo ratings yet
- Presentation Title: Your Company InformationDocument46 pagesPresentation Title: Your Company InformationAli ElattarNo ratings yet
- Case Analysis OR Rotation Week 1 2 SASAN FINAL ADocument4 pagesCase Analysis OR Rotation Week 1 2 SASAN FINAL AJAN KRISTIAN JIMENEA TULIBASNo ratings yet
- Week 7 - Assignment 2Document6 pagesWeek 7 - Assignment 2cfrin86No ratings yet
- Triple Handoff: Spotlight Case September 2006Document28 pagesTriple Handoff: Spotlight Case September 2006Lakshay GuptaNo ratings yet
- Using SBAR A Culture of Patient Safety: Situation Background Assessment RecommendationDocument8 pagesUsing SBAR A Culture of Patient Safety: Situation Background Assessment RecommendationPrayitno SoebrataNo ratings yet
- Practice Station Acute Care HX Ex1Document6 pagesPractice Station Acute Care HX Ex1Wenbin GuoNo ratings yet
- Critical Tests & Critical ResultsDocument4 pagesCritical Tests & Critical ResultssehrNo ratings yet
- NCP MOdified #4Document39 pagesNCP MOdified #4Camille DelfinNo ratings yet
- HA WK4bDocument26 pagesHA WK4bMARY ROSE FAJUTINANo ratings yet
- SBAR Communication ModelDocument30 pagesSBAR Communication ModelTushar ChauhanNo ratings yet
- BONUS 1# - FONPracticeQuizBookDocument182 pagesBONUS 1# - FONPracticeQuizBookMandeq HasanNo ratings yet
- Komunikasi - 8Document28 pagesKomunikasi - 8Litiloly FatimaNo ratings yet
- Amendment of Microbiology ReportsDocument9 pagesAmendment of Microbiology ReportsChandrasreeNo ratings yet
- Manual for Iv Therapy Procedures & Pain Management: Fourth EditionFrom EverandManual for Iv Therapy Procedures & Pain Management: Fourth EditionNo ratings yet
- NCMB 316 Assignment NCP Part 2Document3 pagesNCMB 316 Assignment NCP Part 2I'm a PepegaNo ratings yet
- Emergency Medicine Privilege FormDocument4 pagesEmergency Medicine Privilege FormcaterappleyeNo ratings yet
- Gyula Mózsik, András Dömötör, Tibor Past, Viktória Vas, Pál Perjési, Mónika Kuzma, Gyula Blazics, János Szolcsányi Capsaicinoids, From The Plant Cultivation To The Production of The Human Medical DrugDocument252 pagesGyula Mózsik, András Dömötör, Tibor Past, Viktória Vas, Pál Perjési, Mónika Kuzma, Gyula Blazics, János Szolcsányi Capsaicinoids, From The Plant Cultivation To The Production of The Human Medical DrugCuong NguyenNo ratings yet
- BMC Dermatology: The Treatment of Melasma by Silymarin CreamDocument13 pagesBMC Dermatology: The Treatment of Melasma by Silymarin CreamAnna Listyana DewiNo ratings yet
- 177-Years-Medical-Experimentation Ebook Ty Charlene BollingerDocument59 pages177-Years-Medical-Experimentation Ebook Ty Charlene BollingerDan Mihaela100% (1)
- Legal, Ethical, Psychosocial & Rehabilitation Issues Related To Hiv/AidsDocument5 pagesLegal, Ethical, Psychosocial & Rehabilitation Issues Related To Hiv/AidsGandimarei0% (1)
- Formulating A Nursing Care Plan: S++aint Paul University PhilippinesDocument7 pagesFormulating A Nursing Care Plan: S++aint Paul University Philippinesninafatima allamNo ratings yet
- Astasthana Pariksha - A Diagnostic Method of Yogaratnakara and Its Clinical ImportanceDocument17 pagesAstasthana Pariksha - A Diagnostic Method of Yogaratnakara and Its Clinical Importancenarayana asso100% (1)
- Guideline Variceal BleedingDocument18 pagesGuideline Variceal BleedingLuh Putu Swastiyani Purnami, M.DNo ratings yet
- Unit 0000 Topik 9. Word Formation: Nouns: Bold) To Nouns. Do Not Change TheDocument5 pagesUnit 0000 Topik 9. Word Formation: Nouns: Bold) To Nouns. Do Not Change TheioakasNo ratings yet
- Efficacy of Homoeopathy in SarcoidosisDocument77 pagesEfficacy of Homoeopathy in SarcoidosisDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- Powerpoint - Prof Suzanne KurtzDocument80 pagesPowerpoint - Prof Suzanne Kurtzlizleeas100% (1)
- Neurotic, Stress Related and Somatoform Disorders 2Document73 pagesNeurotic, Stress Related and Somatoform Disorders 2Sonny JhaNo ratings yet
- Whooping Cough: Ardian Zakaria AmienDocument28 pagesWhooping Cough: Ardian Zakaria AmienArdian Zaka RANo ratings yet
- Bittner 2015 Acute and Perioperative Care of TheDocument34 pagesBittner 2015 Acute and Perioperative Care of TheJuan FelipeNo ratings yet
- NCP AnxietyDocument3 pagesNCP AnxietyPaolo EspinosaNo ratings yet
- BSN 2-4 - 2V - MCN CASE STUDY (Final)Document100 pagesBSN 2-4 - 2V - MCN CASE STUDY (Final)Angeline ShackletonNo ratings yet
- Dog, Cat, and Human Bites, A Review, 1995Document11 pagesDog, Cat, and Human Bites, A Review, 1995Biblioteca UMAE HE 1No ratings yet
- Homeopathic Remedy Pictures Gothe Drinnenberg.04000 - 1 PDFDocument6 pagesHomeopathic Remedy Pictures Gothe Drinnenberg.04000 - 1 PDFNeha MandloiNo ratings yet
- Introduction To ChemotherapyDocument28 pagesIntroduction To ChemotherapyShivsharan B. DhaddeNo ratings yet
- Case StudyDocument26 pagesCase Studyamazing grace mejia carlos100% (2)
- Nursing Care Plan: Assessment Nursing Diagnosis Planning Intervention EvaluationDocument4 pagesNursing Care Plan: Assessment Nursing Diagnosis Planning Intervention EvaluationGiddel Guerra PapellerasNo ratings yet
- Final MBBS Part 2Document5 pagesFinal MBBS Part 2Pavan Kumar DNo ratings yet
- Welcome Kit UHCGDocument18 pagesWelcome Kit UHCGluispariniNo ratings yet
- FNCPDocument2 pagesFNCPMa. Alexis DiezmoNo ratings yet
- CND 4.medication & Dispensing ErrorDocument32 pagesCND 4.medication & Dispensing Errorlisnawati farmasicbthNo ratings yet
- Psychopathology From Science To Clinical Practice Reprint Edition PDF Full Chapter PDFDocument53 pagesPsychopathology From Science To Clinical Practice Reprint Edition PDF Full Chapter PDFgoriahlhette100% (4)
- Hospital Waste ManagementDocument4 pagesHospital Waste ManagementMahrukh HaiderNo ratings yet
- Fdar Day 1 Psyche KarlDocument4 pagesFdar Day 1 Psyche KarlKristian Karl Bautista Kiw-is100% (1)