Professional Documents
Culture Documents
Postterm Pregnancy
Postterm Pregnancy
Uploaded by
icOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postterm Pregnancy
Postterm Pregnancy
Uploaded by
icCopyright:
Available Formats
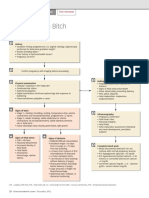
Reviewer: POSTTERM PREGNANCY • ↓ Fetal renal blood flow →
POSTTERM PREGNANCY ↓ urination → oligohydramios
• Definition: • Meconium release during oligo-
> 42 0/7 weeks hydramnios → meconium aspiration
294 days after LMP syndrome
LMP was followed by ovulation after 2 weeks
• Common result: Stillbirth (in growth
• There may be errors in the estimation of AOG d/t faulty
Fetal Growth restricted postterm newborns
menstrual date or delayed ovulation → may not really postterm
Restriction delivered after 42 weeks)
Means of getting AOG: • ↑ risk of morbidity and mortality
• 1st tri. sonography – MOST ACCURATE to conform
AOG; at 9 weeks; MOE: 5 days POSTTERM COMPLICATIONS
• 2nd & 3rd tri. US – correction of AOG • Oligohydramnios
• 1st few weeks of missed menses and (+) pregnancy test • Macrosomia
• Fundic height – At 18 – 32 weeks → FUNDIC HEIGHT • Measurement: AFI or deepest
(cm) = AOG vertical pocket ≤ 1 cm
12 weeks AOG Just above symphysis pubis • Associated w: CS and operative
Oligohydramnios
16 weeks AOG B/w symphysis pubis & umbilicus vaginal delivery, low 5 min APGAR,
20 weeks AOG Level of umbilicus fetal acidemia, fetal compromise
during labor admission to NICU
Predisposing Factors to Postterm Pregnancy
• Peak velocity of weight gain: 37
BMI ≥ 25 Altered metabolic function weeks (most continue to grow)
Macrosomia
• Hard to initiate contraction + ↓ gap • 4475 at 42 weeks: 95th percentile
Nulliparity junctions in myometrium • VAGINAL delivery if (-) DM
• Long cervix (3rd/4th quartile)
• ↓ ESTROGEN but rare ANTEPARTUM MANAGEMENT
Fetal & placental
• Anencephaly, Adrenal hypoplasia, X- • Depends if labor induction is warranted or if expectant
factors
linked placental sulfatase deficiency management with fetal surveillance is best
Biological • Includes:
Maternal genes ONLY Induction factors
predisposition
Fetal testing at 41 weeks
PRENATAL MORTALITY AND MORBIDITY
Induction Factors
• Increased risk of:
• Unfavourable cervix
Rates of still birth, fetal death, infant morbidity
Has no precise objective definition
CS → dystocia, fetal distress
Undilated cervix – seen in some pregnancy >41 weeks,
Cerebral palsy
has higher CS rate for dystocia
Lower IQ at 6.5 y/o
< 3 cm or < 25 mm cervical length = successful infection
Neonatal seizures
• NOT effective:
• Autism NOT associated w/ postterm birth
PGE2 gel
• Pathophysiology:
Sweeping or stripping of the membranes – does not
Postmature Syndrome
induce labor; can l/t pain, vaginal bleeding, irregular
Placental dysfunction
contractions without labor, high rates of CS
Fetal distress and oligohydramnios
Fetal growth restriction Fetal Testing at 41 weeks
• Fetal movement (FM) – 2 hours/day
• Skin: wrinkling (palms & soles), • Nonstress test (NST) – 3x/week
patchy, peeling → d/t loss of vernix • Amniotic fluid volume (AFV) – 2 – 3x/week (abnormal: < 3cm)
caseosa
Postmature • Wasting – long and thin baby MANAGEMENT of Postterm Pregnancy
Syndrome • Advanced maturity: open eyes, old
and worried, unusually alert
• Long nails
• NOT technically growth restricted
• PLACENTAL APOPTOSIS
✓ Greater at 41 – 42 weeks
✓ Upregulated: Kisspeptin
Placental (proapoptotic gene)
dysfunction • ↑ Cord blood erythropoietin level:
suggests decreased oxygenation
• Placental senescence – postmaturity
syndrome
• CORD COMPRESSION associated
Fetal distress &
w/ oligohydramnios → PROLONED
oligohydramnios
DECELERATION (fetal distress)
• If AOG is uncertain → delivery at 41 WEEKS using best
estimate for AOG
• DO NOT DO AMNIOCENTESIS for fetal lung maturity
• Uncertain postterm pregnancies → manage by:
Weekly NST
Assess AFV
LABOR INDUCTION
• Known AOG, induced at completion of 42 weeks
• AFV ≤ 5 cm
• (+) Diminished fetal movement
• IF: Does not deliver during 1st induction → 2nd induction
WITHIN 3 DAYS
INTRAPARTUM MANAGEMENT
• Monitor labor
• Amniotomy
• Cesarean section if remote from delivery
Monitor Labor
• Monitor FHR and uterine contractions
• Scalp electrode and intrauterine pressure catherer – can
be placed AFTER membrane rupture → provides more
precise data about FHR and uterine contractions
Amniotomy
• Aids in identification of thick meconium (worrisome)
Signifies lack of liquid (oligohydramnios)
Aspiration of thick meconium → severe pulmonary
dysfunction, neonatal death
Amnioinfusion – diluting meconium; not effective
• Reduced successful vaginal delivery in nullipara with thick,
meconium-stained amniotic fluid → prompt CS
• Amniotomy during labor → can further reduce fluid volume
→ cord compression
Cesarean Section
• Indications:
Woman is remote from delivery
Suspected cephalopelvic disproportion
Evident hypotonic or hypertonic dysfunction labor
You might also like
- Ebook Developing Person Through Childhood and Adolescence 11Th Edition Ebook PDF All Chapter PDF Docx KindleDocument47 pagesEbook Developing Person Through Childhood and Adolescence 11Th Edition Ebook PDF All Chapter PDF Docx Kindlehazel.field513100% (31)
- OB 1st PNCUDocument8 pagesOB 1st PNCUAngelo Erispe100% (1)
- 2 - Pre Gestational ConditionDocument11 pages2 - Pre Gestational ConditionAngelica Dalit MendozaNo ratings yet
- CME Miscarriages Combined 1Document76 pagesCME Miscarriages Combined 1syawal zulfitriNo ratings yet
- Nle - High-Risk PregnancyDocument113 pagesNle - High-Risk Pregnancytachycardia01No ratings yet
- NCM 109 Problems With Power DraftDocument3 pagesNCM 109 Problems With Power DraftJP Porras Ali100% (1)
- Assessment of Fetal Well-Being 1. Fetal MovementDocument6 pagesAssessment of Fetal Well-Being 1. Fetal MovementClaire Julianne CapatiNo ratings yet
- Post TermDocument16 pagesPost Termahmed shorsh100% (1)
- Rachel PpromDocument15 pagesRachel PpromGeneNo ratings yet
- Placenta IsuogDocument40 pagesPlacenta IsuogKARINA BASTIDAS IBARRA100% (1)
- NCM 102 OB Abnormal 2Document113 pagesNCM 102 OB Abnormal 2Maria Garcia Pimentel Vanguardia IINo ratings yet
- Post Term PregnancyDocument12 pagesPost Term PregnancyRizky Putra Ismeldi100% (1)
- PaedsDocument72 pagesPaedsOlivia Genevieve El JassarNo ratings yet
- O&G LO SlidesDocument60 pagesO&G LO Slideskatherine nunnNo ratings yet
- By Gemechu M (MD)Document26 pagesBy Gemechu M (MD)Semon YohannesNo ratings yet
- Gestational 1Document8 pagesGestational 1RoseAngelyne VicenteNo ratings yet
- ? - PEDIA PRELIMS Lessons 1 and 2Document8 pages? - PEDIA PRELIMS Lessons 1 and 2ysabel.mendozaNo ratings yet
- ObsGyn RR @academycerebellumDocument180 pagesObsGyn RR @academycerebellumNeeladri DawnNo ratings yet
- Einc-Updates 231024 214348Document7 pagesEinc-Updates 231024 214348Alexander Nicole DomingoNo ratings yet
- High Risk Pregnancy:: A Woman Who Develops A Complication of PregnancyDocument79 pagesHigh Risk Pregnancy:: A Woman Who Develops A Complication of PregnancyMike Faustino SolangonNo ratings yet
- Preterm Labour and PROMDocument25 pagesPreterm Labour and PROMNinaNo ratings yet
- Bleeding During PregnancyDocument4 pagesBleeding During PregnancyCarl Andre ReyesNo ratings yet
- Obg AbortionDocument62 pagesObg Abortionkashyap priyankaNo ratings yet
- Dystocia in The BitchDocument2 pagesDystocia in The BitchGissele ParaisoNo ratings yet
- Trans SaVi Lec08 Obstetrics Post Term Pregnancy 1st SemesterDocument7 pagesTrans SaVi Lec08 Obstetrics Post Term Pregnancy 1st SemesterAdrian CaballesNo ratings yet
- Jose, Leana Louisse D. Cornell Notes On Ncm109 Module 1 & 2 (Complications of Pregnancy) 02/18/21 Assessment For Risk FactorsDocument19 pagesJose, Leana Louisse D. Cornell Notes On Ncm109 Module 1 & 2 (Complications of Pregnancy) 02/18/21 Assessment For Risk FactorsLiana Louisse JoseNo ratings yet
- Antepartum HaemorrhageDocument21 pagesAntepartum HaemorrhageDavina DakapNo ratings yet
- Obstetric Highlights, Elmar P. SakalaDocument47 pagesObstetric Highlights, Elmar P. Sakaladukelist5660% (1)
- Abruptio Placenta and AbortionDocument10 pagesAbruptio Placenta and Abortiondanica grace gubaNo ratings yet
- Intrapartal ComplicationsDocument8 pagesIntrapartal ComplicationsLizeth Querubin100% (4)
- K-Medics Placental Previa - AbruptionDocument28 pagesK-Medics Placental Previa - AbruptionMichael AdjeiNo ratings yet
- GEMS Obstetrics and GynaecologyDocument59 pagesGEMS Obstetrics and GynaecologyUMARRA SHAFIQUENo ratings yet
- PromDocument26 pagesPromAhmed MohammedNo ratings yet
- Antepartum BleedingDocument37 pagesAntepartum BleedingMae Importers IncNo ratings yet
- 9 - Postterm PregnancyDocument22 pages9 - Postterm PregnancyMara Medina - BorleoNo ratings yet
- Usg Webinar Bioprofil Bayi PrintDocument36 pagesUsg Webinar Bioprofil Bayi PrintElfan WinotoNo ratings yet
- Multifetal Pregnancy: Herman Sumawan FK Unsoed/Rs Margono SoekarjoDocument70 pagesMultifetal Pregnancy: Herman Sumawan FK Unsoed/Rs Margono SoekarjoTitisPudyatikaDestyaAndiraNo ratings yet
- Umbilical Cord AccidentsDocument16 pagesUmbilical Cord Accidentschebetnaomi945No ratings yet
- HemorrhagesDocument3 pagesHemorrhagesARAugustoNo ratings yet
- MCN ReviewerDocument4 pagesMCN ReviewerMaria Arabella LanacaNo ratings yet
- Alarm-Perdarahan Antepartum PDFDocument5 pagesAlarm-Perdarahan Antepartum PDFUmmu Qonitah AfnidawatiNo ratings yet
- Case 2 TG Retype PDFDocument15 pagesCase 2 TG Retype PDFElma CorpusNo ratings yet
- ABORTIONDocument3 pagesABORTIONAngel MoncadaNo ratings yet
- Prolonged PregnancyDocument29 pagesProlonged PregnancyNur Agami100% (1)
- Maternity Nursing NotesDocument7 pagesMaternity Nursing NotesazitaaaaaNo ratings yet
- CH 5 MDocument6 pagesCH 5 MShaafieNo ratings yet
- Student Unit 2 Topic 2.5 Jan 2018 TAYLORDocument42 pagesStudent Unit 2 Topic 2.5 Jan 2018 TAYLORKrista KloseNo ratings yet
- Pedia GyneDocument13 pagesPedia Gynerjh1895No ratings yet
- University of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingDocument94 pagesUniversity of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingErica Veluz LuyunNo ratings yet
- Pprom 1 1Document20 pagesPprom 1 1Tehreem AzharNo ratings yet
- Gestational ConditionsDocument4 pagesGestational ConditionsHyacinth Mae Virtudazo RaganasNo ratings yet
- Abnormal Uterine Bleeding: Presented By: Shubhangi A Redij Guided By: Dr. Ashwini Morale MamDocument15 pagesAbnormal Uterine Bleeding: Presented By: Shubhangi A Redij Guided By: Dr. Ashwini Morale MamS RedijNo ratings yet
- Physiologic SignsDocument59 pagesPhysiologic SignsChari RivoNo ratings yet
- Abortion Chapter 18 Willobs 25th EdDocument40 pagesAbortion Chapter 18 Willobs 25th EdNabil MaulanaNo ratings yet
- 19 - Obstetric ImagingDocument12 pages19 - Obstetric ImagingAbhijith J PuttananickalNo ratings yet
- Antepartum Fetal Surveillance: Chandani PandeyDocument98 pagesAntepartum Fetal Surveillance: Chandani Pandeychandani pandeyNo ratings yet
- Management of Placenta Previa During Pregnancy: M Hadyan Syahputra 71 2016 055Document14 pagesManagement of Placenta Previa During Pregnancy: M Hadyan Syahputra 71 2016 055khaira_nNo ratings yet
- Ectopic Pregnancy: ObgyneDocument2 pagesEctopic Pregnancy: ObgyneLuis PadillaNo ratings yet
- OralsOB EctopicDocument2 pagesOralsOB EctopicKrista P. AguinaldoNo ratings yet
- AbortionsDocument25 pagesAbortionsaravindNo ratings yet
- It's Not Just a Heavy Period; The Miscarriage HandbookFrom EverandIt's Not Just a Heavy Period; The Miscarriage HandbookRating: 2 out of 5 stars2/5 (1)
- Pharma 2nd Sem Prelims RatioDocument11 pagesPharma 2nd Sem Prelims RatioicNo ratings yet
- OPIATESDocument2 pagesOPIATESicNo ratings yet
- Psych Finals CompiledDocument13 pagesPsych Finals CompiledicNo ratings yet
- Compiled Psych MidtermsDocument13 pagesCompiled Psych MidtermsicNo ratings yet
- Psych Finals PlatingsDocument13 pagesPsych Finals PlatingsicNo ratings yet
- Basic SuturingDocument14 pagesBasic SuturingicNo ratings yet
- Family Planning (Hormonal Contraceptives)Document2 pagesFamily Planning (Hormonal Contraceptives)icNo ratings yet
- Primary AmenorrheaDocument2 pagesPrimary AmenorrheaicNo ratings yet
- NRP ppt1Document29 pagesNRP ppt1sumana BanerjeeNo ratings yet
- Obstetrical Nursing AntepartumDocument28 pagesObstetrical Nursing AntepartumAyeza DuaNo ratings yet
- Pregnancy: Signs/Symptoms and Common Health ConcernsDocument5 pagesPregnancy: Signs/Symptoms and Common Health ConcernsTracy50% (2)
- Prenatal Period of Development EportfolioDocument4 pagesPrenatal Period of Development Eportfolioapi-367895274No ratings yet
- Grande MultiparaDocument6 pagesGrande MultiparaAgus Wijaya100% (2)
- Maternal HealthcareDocument124 pagesMaternal HealthcareEstellaNo ratings yet
- The Effect of Maternal - Fetal Attachment Education On Maternal MenDocument7 pagesThe Effect of Maternal - Fetal Attachment Education On Maternal MenNadia RifeldaNo ratings yet
- Prevention of Congenital Syphilis Through Antenatal Screenings in Lusaka, Zambia: A Systematic ReviewDocument11 pagesPrevention of Congenital Syphilis Through Antenatal Screenings in Lusaka, Zambia: A Systematic ReviewlianaNo ratings yet
- Lesson 4 Infancy by HurlockDocument44 pagesLesson 4 Infancy by HurlockJessica Recaido100% (1)
- Antecedents of CPDocument8 pagesAntecedents of CPЯковлев АлександрNo ratings yet
- Beversdorf 2018 DissDocument12 pagesBeversdorf 2018 DissJacob NotHank FrancisNo ratings yet
- High Risk Pregnancy HB TranxDocument11 pagesHigh Risk Pregnancy HB TranxangeliquepastranaNo ratings yet
- Advanced Maternal Age & PregnancyDocument67 pagesAdvanced Maternal Age & PregnancyMa Pilar Peñaflor AñonuevoNo ratings yet
- W1-L3-Human Development - Heredity and Environment200414060604044949Document14 pagesW1-L3-Human Development - Heredity and Environment200414060604044949Sachidananda AngomNo ratings yet
- NURS325 04 Antepartum PeriodDocument58 pagesNURS325 04 Antepartum PeriodaliNo ratings yet
- Human Development A Life Span View 8th Edition Ebook PDFDocument61 pagesHuman Development A Life Span View 8th Edition Ebook PDFnaomi.parker972100% (56)
- No. 197b-Fetal Health SurveillanceDocument25 pagesNo. 197b-Fetal Health SurveillanceMaríaNo ratings yet
- Care of New BornDocument14 pagesCare of New Bornshubham vermaNo ratings yet
- ANC Guideline PresentationDocument42 pagesANC Guideline PresentationDeepak BamNo ratings yet
- NSG Seminar Sas 1 13 CompilationDocument94 pagesNSG Seminar Sas 1 13 CompilationNiceniadas CaraballeNo ratings yet
- The Earliest Relationship Parents, Infants, and The Drama of EaDocument280 pagesThe Earliest Relationship Parents, Infants, and The Drama of EaBogdan BNo ratings yet
- Maternal NursingDocument48 pagesMaternal NursingMarwa DaghNo ratings yet
- Intellectual DiabilityDocument10 pagesIntellectual DiabilityAngelo PapimNo ratings yet
- Preterm and Posterm Birth: Oleh: DR Adi Setyawan Prianto SP - OG (K)Document31 pagesPreterm and Posterm Birth: Oleh: DR Adi Setyawan Prianto SP - OG (K)ATIKAH NUR HAFIZHAHNo ratings yet
- Fetal Growth RestrictionDocument56 pagesFetal Growth RestrictionKanika VermaNo ratings yet
- PDF Children Thirteenth Edition Edition John W Santrock Ebook Full ChapterDocument53 pagesPDF Children Thirteenth Edition Edition John W Santrock Ebook Full Chapterjoy.james964100% (2)
- Fetal DevelopmentDocument51 pagesFetal DevelopmentLhiet Aguilar Hipolito67% (3)
- Browne 2011Document11 pagesBrowne 2011Gisele Elise MeninNo ratings yet