Professional Documents
Culture Documents
Maternal and Child Nursing From Tina Complete
Maternal and Child Nursing From Tina Complete
Uploaded by
Argee AlonsabeCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maternal and Child Nursing From Tina Complete
Maternal and Child Nursing From Tina Complete
Uploaded by
Argee AlonsabeCopyright:
Available Formats
NCM 201: Promotive and Preventive Care Management
Maternal and Child Nursing Child-bearing Age -> when woman starts menstrual period until the woman is still in her menstruating years Anatomy and Physiology : Unit 1 Preparing Families for Childbearing and Childrearing Male Reproductive System Internal : testis, epididymis, ductus/vas deferens, seminal vesicle, prostate External: scrotal area / scrotum, penis I. Internal 1. Testes male gonads - exocrine function : sperm - endocrine function : testosterone - olive sizes; 4 cm (1 in) long and 2.5cm (1in) wide Tunica Albuginea fibrous connective tissues that surround or encapsulates each testis Seminiferous tubules actual sperm forming factory Rete testis set of tubules in each of the testis where the sperm passes 2. Duct System a). Epididymis temporary storage site for immature sperm from the testis - comma shaped; highly coiled tube about 6m long (20ft) that caps the superior part of each testis and runs down its postero lateral side - first part of the male duct system - takes 20 days for sperm to travel the entire epididymis (1day/1ft) - its walls contract when a male is sexually stimulated b). Vas Deferens / Ductus Deferens - runs upward from the epididymis through the inguinal canal in to the pelvic cavity and arches over the superior aspect of the bladder
- spermatic cord; - main function: to propel live sperms from their storage sites, the epididymis and distal part of the ductus deferens, into the urethra - vasectomy
c). Urethra approximately 8inches long - hollow tube descending from the base of the bladder, continues to the outside through the shaft and glans penis - terminal part of the male duct system 3 regions: Prostatic Urethra near prostate Membranous Urethra Spongy Urethra Ejaculation bladder sphincter constricts to prevent passage of urine into urethra and prevent sperm from entering the urinary bladder 1
NCM 201: Promotive and Preventive Care Management
3. Accessory Glands: Semen possible without sperm - pre-ejaculatory secretion secretions without sperm - sperm containing fluid that is propelled out of the males reproductive tract during ejaculation - milky white, sticky mixture of sperm and accessory glands secretions
pH 7.2 2.6; 2-5ml/ejaculation with 50 130M of sperm/ml sperm count provides a transport medium and nutrients, and contains chemicals that protect the sperm and aid their movement
a). Seminal Vesicles base of the bladder - produces about 60% of the fluid volume of semen - their thick, yellowish secretions is rich in sugar (fructose), vit. C, prostaglandins and other substances which nourish and activate the sperm passing through the tract ( sperm becomes motile with added fluid) - its duct joins that of the ductus deferens on the same side to form the ejaculatory duct b). Prostate Gland - a single gland about the size and shape of a chestnut - encircles the upper ( prostatic) part of the urethra just below the bladder - secretion is milky fluid that plays a role in activating sperm (further protects the sperm from being immobilized by naturally low pH level of urethra). - to regulate hormone (androgen) - located immediately anterior to the rectum so its size and texture can be palpated by digital examination through the anterior rectal wall
c). Bulbourethral glands / Cowpers glands tiny pea-sized glands inferior to the prostate gland - produce a thick mucus secretion that drains into the penile urethra - first to pass down the urethra when a man becomes sexually excited - cleans the urethra of traces of acidic urine and serves as lubricant during sexual intercourse II. External Genitalia 1. Scrotum rugated, skin-covered muscular pouch suspended from the perineum - a divided sac of skin that hangs outside the abdominal cavity, between legs and at the root of penis changes in position according to the temperature 2. Penis designed to deliver the sperm to the female reproductive tract Shaft skin-covered penis Glans Penis enlarged tip at the end of the shaft (retractable casing of the skin) Prepuce or Foreskin cut off skin around the proximal end of the glans; Circumcision (part that is being sliced) - also called the major organ of copulation - 3 elongated areas of erectile tissue
2 main functions of the male reproductive system: Spermatogenesis production of sperm which begins during puberty and continues throughout life Testosterone production performed by the interstitial cells and continues throughout life
NCM 201: Promotive and Preventive Care Management
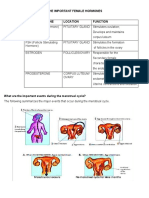
Female Reproductive System I. Internal 1. Ovaries almond size and shape (4cm long, 2cm in diameter) - primary reproductive organ of the female - produce estrogen and progesterone, initiate and regulate menstrual cycle Parts of the ovary: A. Primary Follicle tiny sac-like structure - contains immature egg B. Antrum fluid-filled central region - surrounds the egg - provides nourishment; cushions or prevents injury to growing immature egg C. Graafian Follicle / Vesicular Follicle mature follicle with the developing egg D. Corpus Luteum ruptured follicle after ovulation - means yellow body * Corpus Alba white body Ovulation an event wherein the developing egg in the mature follicle is ready to be ejected from the ovary 2. Duct Systems a. Uterine / Fallopian Tubes receives the ovulated oocyte and provides a site for fertilization to occur - approximately 10cm long - 3 parts: isthmus ampulla infundibulum - bilateral tubal litigation - outer third - ectopic pregnancy b. Uterus hollow organ that functions to receive, retain and nourish a fertilized egg - can never be implanted to a males body - site of implantation = fertilized egg will burrow on uterus - non-pregnant = pear (60gms) - 3 parts: Fundus Body Cervix - 3 layers: Endometrium (inner) Myometrium (muscular) Epimetrium or Perimetrium (outer) c. Vagina hollow musculomembranous canal - 3 4 inches long - birth canal - female organ of copulation = receives penis during sex Hymen thin fold of mucosa which partially close the distal end of the vagina
II. External Genitalia Mons Pubis fatty rounded portion usually covered with hair 3
NCM 201: Promotive and Preventive Care Management
protection of internal organs from injury Labia Majora elongated fold of skin that runs posteriorly from the mons pubis covered with hair protects from injury and invading microorganisms Prepuce of clitoris skin-covering of clitoris Clitoris for sexual arousal Vestibule region where external part of urethra is located Urethral orifice Vaginal Orifice (hole) entrance toward vagina Orifice of greater vestibular gland Bartholins Gland; Skenes Gland Labia Minora hairless; inner fold Perineum Anus not part of female reproductive system
Female Reproductive Functions: Oogenesis production of oocytes Hormone productions estrogen and progesterone III. Breast (Mammary Gland) part of sexual arousal physiologic function is milk production to feed infants Maturity of breast: as long as it can provide milk; only attained once breast is producing milk Lactating: 400 500g Non-lactating: 150 250g Parts: a). Parenchyma contains tubules and ductules where milk is produced and milk passes by from the iner part to the outward b). Nipple terminal end of ducts / tubules c). Montgomerys gland sebaceous gland that prevents drying and cracked nipples - breast composed of fatty tissues
MENSTRUAL CYCLE Menstruation periodic uterine bleeding in response to cyclic hormonal changes - refers mainly to changes in uterus and ovaries which recur cyclically from the time of menarche to menopause (physiological end of menstrual cycle) - shedding off of endometrial lining - average: 28days (+/- 5-10 days) - duration: 2-8 days bleeding episodes - average blood loss: 30ml of blood - loss of Fe averaging 0.5mg to 1mg daily
Estrogen very high when ovulating Progesterone increase if ever during ovulation there is fertilization; needed for pregnancy Pre menstrual syndrome because of the play of hormones
NCM 201: Promotive and Preventive Care Management
4 Phases of Menstrual Cycle: a). Menstrual Phase characterized by shedding of the endometrium with the discharge exiting through the vagina prostaglandin content of the endometrium reaches its highest levels estrogen and progesterone levels are relatively low, which stimulates the release of FSH combined with a steady low level of LH secretion, ovarian estrogen secretion begins b). Follicular (ovary) or Proliferative (endometrium) - endometrium regenerates and thickens in preparation for possible implantation - rising blood levels of estradiol exert negative feedback on FSH secretion and positive feedback on LH secretion - ovulation begins - ovum remains viable for 24 46 hours c). Luteal (ovary) or Secretory (endometrium) - begins after ovulation and is relatively finite period of about 12 14 days - under continuing LH secretion, a temporary endocrine gland is formed (corpus luteum) from the ruptured follicle - progesterone and estrogen levels drop, the negative feedback effect of estrogen on FSH ceases d). Ischemic Phase blood vessels rupture - endometrium becomes pale
SEXUALITY AND SEXUAL IDENTITY Sexuality includes all aspects of human being that relates specifically to being a boy / girl, woman or man - a multidimensional phenomenon that includes feelings, attitude and actions - has both biologic and cultural components - encompasses and gives direction to a persons physical, emotional, social and intellectual responses throughout life - born a sexual being, a childs gender identity and gender role behavior evolve from and usually conform to the social expectations within the childs culture Factors that influence a persons sexuality: 1. Developmental level acceptable forms of sexual expression in each stage of development 2. Culture homosexual behavior is tolerated 3. Religious Values religion provides guidelines for sexual behaviors 4. Personal Ethics codes of conduct based on ethical principles (what you hold is true) 5. Health Status may affect sexual activity of client who is suffering from cardiac problems Gender denotes male or female - 3 aspects of gender: a). Biologic Gender chromosomal sexual development, male XY female XX b). Gender or Sexual Identity inner sense of a person has of being a male or female, which may be the same as or different from biologic gender c). Gender Role outward expression of a persons sense of femaleness or maleness
NCM 201: Promotive and Preventive Care Management
Development of Gender / Sexual Identity: Infancy from the day of birth, male and female babies are treated differently by their parents - baby has no concept of sexuality yet - dressing and grooming, toys, and methods of play - penile erection and girls have clitoral erection; vaginal lubrication is present Toddler and Pre school Period can distinguish men and women as early as 2 years old by age 3 or 4 years old, they know what sex they are and have absorbed cultural expectations of that sex role parents and friends help to govern their choice of actions Sex role modeling also comes from watching TV programs If child lives in a home where both mother and father are kind, loving people, sex role identification progresses smoothly If the parent does not have nurturing capacity, child with same sex finds it hard to identify with that person Adult must use correct names of the body parts There is interest in genitalia School Age early school age children typically spend playtime imitating adult roles as a way of learning gender roles Oedipus / Electra Complex
developing a sense of curiosity about their bodies and explore their own and often those of their peers doctor / nurse or mother / father Adolescent most early adolescent maintain strong ties to their gender group; boys with boys, girls with girls some adolescents choose a child of their own gender or a few years older than themselves to use as model of gender role behavior most youngsters obtain sexual information and misinformation from friends, the mass media or movies sexual fantasies occupy much of an adolescents time develops relationship with the opposite sex (boy meets girl) masturbation is common curiosity about sex becomes intense Young Adult search for intimacy and most young adults marry with a commitment to one sexual partner while others establish relationships less binding by legal definitions or perhaps equally binding in concern and concern homosexuality / bisexuality may be overtly expressed for the first time during this period Gender identity influences many aspects of life such as health perceptions. It can affect parenting. Middle Aged Adult for many women and men in midlife sexuality ahs achieved a degree of stability adults in midlife have resolved earlier conflicts with mates and have the freedom to satisfy their sexual needs, including freedom to remain with a partner or return to single state following menopause, reproductive functioning alters but not sexual functioning in men, neither reproductive nor sexual functioning alters in midlife but often reported to be the most difficult period of adjustment in a mans life (ego enhancement reassurance) Older aged Adult both male and female older adults can enjoy active sexual relationships some men experiences less erectile firmness / ejaculatory force than they were younger but others discover that they are able to maintain an erection longer. They must continue to be responsible for sex partners in terms of reproductive life planning men produce fewer sperm 6
NCM 201: Promotive and Preventive Care Management
older women may have less vaginal secretions because of less estrogen after menopause
Sexual Response Cycle 1. Excitement / Foreplay longest phase - both couples need to be aroused - occurs with physical and psychologic stimulation that causes parasympathetic nerve stimulation - this leads to arterial dilation and venous constriction in the genital area - vasocongestion and increasing muscular tension - in women, clitoris increases in size and mucoid fluid to appear on vaginal walls as lubrication - the vagina widens in diameter and increases in length - the breast nipples become erect. Reddening of the labia minora and vaginal wall occur
in men, erction occurs; there is scrotal thickening and elevation of the testes in both sexes, there is an increase in heart rate and respiratory rate and blood pressure
2. Plateau starting to escalate - it is reached just before orgasm - in women, clitoris is drawn forward and retracts under the clitoral prepuce; the lower part of the vagina becomes extremely congested and there is increased nipple engorgement. in men, the vasocongestion leads to full distention of the penis
heart rate increases to 100 to 175bpm and respiratory rate to approximately 40cpm
3. Orgasm peak of sexual response cycle - occurs when stimulation proceeds through the plateau stage to a point at which the body suddenly discharges accumulated sexual tension - vigorous contraction of muscles in the pelvic area expels / dissipates blood and fluid from the area of congestion start of ejaculation for women, the average number of contractions is from 8 15 at intervals of one every 0.8 seconds in men, muscle contractions surrounding the seminal vessels and prostate project semen into the proximal urethra. Theses contractions are followed immediately by 3 7 propulsive ejaculatory contractions, occurring at the same time interval as in women which force semen from the penis. As the shortest stage in the sexual response cycle, orgasm is usually experienced as intense pleasure affecting the whole body, not just the pelvic area It is also highly personal experience; descriptions vary greatly from person to person
4. Resolution internal and external genital organs return to an unaroused state (organs go back to normal size) - Refractory period -> women do not have refractory period; they can have sex again after orgasmic phase -> but men cant have another erection because they have refractory period -> only after 30mins could men have sex again and have an erection; men cant have erection after orgasmic phase - For both men and women, this period generally takes 30 minutes
NCM 201: Promotive and Preventive Care Management
Definition of Terms Pregnancy state of having a developing fetus in the womb Gravida / Gravidity number of pregnancies including the present pregnancy regardless of the outcome and duration Gravid pregnant woman Parity / Para total number of pregnancies that had reached the age of viability whether born dead or alive Abortion any pregnancy terminated before the age of viability; miscarriage Age of Viability Primigravida a woman who is pregnant for the first time Primipara first time completed pregnancy Diagnosis of Pregnancy Signs and symptoms are divided into 3: - Presumptive Signs subjective signs - Probable signs there could be objective signs - Positive signs * Diagnosis of pregnancy is based on pregnancy related physical and hormonal changes and is classified as presumptive, probable or positive. I. Presumptive Signs and Symptoms (Subjective) - These changes may be noticed by mother / health care provider but are not conclusive for pregnancy - Amenorrhea (cessation of menstruation) - Nausea and vomiting (5-12 wks) - Urinary frequency (6-12 wks) - Fatigue - Breast changes - Weight change - Skin changes - Vaginal changes including leucorrhea ( white vaginal discharge present from day of pregnancy to day of delivery) - Quickening fetal movement Maternal perception of fetal movement occurring between 16 20 weeks of gestation (if indeed pregnant) - Chadwick sign (either probable or presumptive) blue-purple discoloration of the vagina 8 12 weeks Pigmentation Striae Gravidarum stretch marks ; - red / purple . pinkish streaks on the abdomen due to tearing of connective tissue - will not disapper after pregnancy because they are ruptured connective tissues Chloasma / Melasma mask of pregnancy - on cheecks and bridge of nose; looks like freckles; disappears when woman has delivered Linea Nigra straight line found on the abdomen, below navel down to pubis symphysis
II. Probable Signs health professionals can now see signs and symptoms - Uterine changes Chadwicks sign Hegars sign softening of the uterus Goodells sign softening of the cervix - Fetal Outline - Pregnancy Test HCG (Human Chorionic Gonadotropin) hormone produced by placenta; during fertilization, corpus luteum produce HCG. During implantation, the placenta produce HCG 8
NCM 201: Promotive and Preventive Care Management
III. -
Braxton Hicks contraction painless uterine contractions Ballottement (Balloter toss about) bouncing back of fetus upon internal examination Positive Signs FHB Doppler Fetal outline and movement Ultrasound X-ray of fetal skeleton
Psychological Tasks of Pregnancy I am pregnant acceptance of the biological fact of pregnancy I am going to have a baby acceptance of fetus as a distinct individual and a person to care for I am going to be a mother prepare realistically for the birth and parenting of the child mother has nesting behavior
Physiologic Changes to Pregnancy - local changes changes that occur in the reproductive system - systemic changes all systems of the body undergo changes symptoms as verbalized by client signs which client and caregiver could directly identify
I. Reproductive Tract Changes a). Uterine changes - increase in size - increase in weight - increase in uterine blood flow - Hegars sign softening of lower segment of uterus
Ballottement Braxton Hicks contraction Amenorrhea
b). Cervical Changes - More vascular and edematous - Goodells sign - Operculum mucus plug on the cervix that prevent fetus from infection c). Vaginal Changes - Chadwicks sign - Change in pH
Leukorrhea Candidal infection Candida Albicans
d). Ovarian Changes - Ovulation stops 9
NCM 201: Promotive and Preventive Care Management
16th week placenta
e). Breast changes - fullness, tingling and tenderness - Hyperplasia of mammary alveoli and fat deposits (in preparation for milk production) - Size increases - Areola darkens and its diameter increases - Montgomerys tubercles become protuberant - By 16th week, colostrums can be expelled II. Integumentary changes - Striae Gravidarum - Melasma / Chloasma mask of pregnancy - Linea Nigra - Diaphoresis excessive sweating - Palmar Erythema redness / itchiness of palm due to increase in circulating estrogen - Vascular spiders small dilated veins usually found on legs (popliteal) ecause of weight exerted by growing fetus in the lower part of the body
III. Systemic Changes a). Respiratory Changes - Sensations of shortness of breath * Lordosis position of pregnant women; to facilitate breathing and to expand lungs Residual volume decreases by 20% Tidal volume increases by 40% Marked congestions or stuffiness due to estrogen Total oxygen consumption increases up to 20%
b). Temperature - Light increase in the body temperature due to increase in metabolic rate c). Circulatory - Increase in total blood volume - Increase by 30 50% near the end of 1st trimester - Pseudoanemia / physiologic anemia of pregnancy plasma too high, but hemoglobin is only normal **iron supplements - Increased cardiac output (oxygenated blood) - Heart is shifted to a more transverse position - Edema and varicosities of the vulva, rectum and legs - Palpitations due to sympathetic nervous system Blood pressure slightly decrease during 2nd trimester Pregnancy Induced Hypotension Supine Hypotension Syndrome feeling of lightheadedness, faintness and palpitation when lying supine 10
NCM 201: Promotive and Preventive Care Management
Blood constitution > increased fibrinogen > total WBC rises serves as buffer system; to prepare just incase an infection sets in > total CHON level of blood decreases > lipids and cholesterol serum level increases
d). Gastrointestinal System - Heartburn / pyrosis acid reflex; cardiac sphincter Relaxin tends to relax GIT and cardiac sphincter Constipation and flatulence -> relaxin relaxes small and large intestine leading to collection of fetal matter in large intestine; collection of fluids that will try to pass through fetal matter Decreases gastric motility (difficulty in digesting food) Nausea and vomiting due to decreased amount of calories in the body Hyperptyalism excessive salivation Hypertropy of the gumlines and bleeding of gingival tissue Pica abnormal cravings Decreased gallbladder emptying time
e). Urinary System - Increased frequency - Spilling of glucose in the urine - Increase in diameter of bladder f). Skeletal System - Gradual softening of the pelvic ligaments and joints - Lordosis pride of pregnancy; for easy breathing and balance - Backache due to lordosis g). Endocrine System - Addition of placenta (estrogen, progesterone, Human Placental Lactogen, HCG) - No FSH, LH - Increased production of growth hormone and MSH - PPG (Posterior Pituitary Gland) produce oxytocin and prolactin Thyroid gland increases Insulin is less effective Gestational Diabetes Mellitus (GDM)
h). Immune System - Decreases - Increase WBC Growing Fetus Beliefs: Medieval Arts - >fetus immobile, miniature creature Leonardo da Vinci -> fetus is an integral part of mother that shares the same blood with her Kaspar Wolff (1758) -> child share equal amount of chromosomes from both parents Stages of Fetal Development: 11
NCM 201: Promotive and Preventive Care Management
1. Pre embryonic Stage from fertilization up to 2 weeks 2. Embryonic Stage 2-8 weeks 3. Fetal Stage 8weeks to birth Terms used to denote fetal growth Ovum from ovulation to fertilization Zygote from fertilization to implantation Embryo 2-8 weeks Fetus 8weeks to birth Conceptus fetus and placental parts Fertilization the beginning of pregnancy union of ovum and spermatozoa conception, impregnation, fecundation ampulla 72 hours ** functional life of sperm = 24 48 hours Ovulation ovum extruded from Graafian follicle ovum propelled in fallopian tube peristaltic action of the fallopian tube proples the ovum to the ampulla fertilization occurs 24 hours after ovulation
Ovum
Corona radiata
Ovum
Zona pellucida
> 2 protective layers increase the bulk to facilitate migration to the uterus protects ovum against injury Sperm - takes 80 seconds to reach cervix and 5 minutes to reach fallopian tube
After sex : elevate legs. Do not stand up for 5 minutes; put pilllow at the back to elevate legs to help sperm reach fallopian tube faster Capacitation - final process that the sperm must undergo to be ready for fertilization starting from testes, the sperm already goes through capacitation + 64days for sperm to mature
Hyaluronidase top of head of pserm contains hyaluronidase 12
NCM 201: Promotive and Preventive Care Management
proteolytic enzyme that acts to dissolve the layer of the cells protecting the ovum
Hydatidiform Mole H mole multiple sperm entering the ovum signs and symptoms same with pregnancy except for fetal heart beat considered cancer cells, so after D&C, client must have chemotherapeutic drug Implantation contact between the growing structure and the uterine endometrium ** Fertilization pregnancy test + because of ovulation Day 1 of pregnancy fertilization Day 2 of pregnancy first cell division (zygote) Day 3 of pregnancy morula Day 4 of pregnancy blastocyst Day 8 10 of pregnancy implantation ** implantation occurs 8 10 days after fertilization: CRUCIAL! Embryonic and Fetal Structures 1. Decidua - falling off - endometrium, instead of sloughing off during menstruatin, continues to grow in thickness and vascularity; inner part of uterus 3 separate areas: > Basalis lying directly under the embryo > Decidua Capsularis portion that encapsulates the surface of the trophoblast > Decidua Vera remaining portion of uterine lining that is not used in formation of fetus 2. Chorionic Villi probing fingers reach out later on to uterus for attachment nearly 200 villis formed at term ( during pregnancy) reach to uterus for proper implantation
Syncytiotrophoblast (syncytial layer)
Connective tissues that contain capillaries
Cytotrophoblast / Langhan's layer - protects fetus from infection caused by bacteria and viruses - only protects fetus from 18 20 weeks of pregnancy - even with Langhan's layer, Syphillis / Herpes can still cross 3. Placenta - pancake; size 8 shape - arises out of trophoblast serves as: fetal lungs, kidneys, GIT ( fetus set of kidneys and lungs are nonfunctional) separate endocrine organ (provides necessary hormones) ** fetal veins carry oxygenated blood ** baby mommy carried by artery carrying unoxygenated blood 13
NCM 201: Promotive and Preventive Care Management
Hormones Produced by Placenta a. Human Chorionic Gonadotropin (HCG) first hormone produced by placenta (16th week) detected by using maternal blood and urine suppresses maternal immunologic response so placental tissue is not rejected prone to miscarriage if not producing HCG b. Estrogen (estradiol) hormone of women gives feminine characteristics 2nd product of placenta contributes to mammary gland secretions stimulate uterine growth c. Progesterone hormone for pregnant women hormone of mothers maintains the endometrial lining of the uterus during pregnancy prevents miscarriage reduces contractility of uterine muscle prevents premature uterine contractions d. Human Placental Lactogen (HPL) / Human Chorionic Somatomammotropin growth promoting and lactogenic 6th week of pregnancy promotes mammary gland growth regulates maternal glucose, protein and fat levels 4. Umbilical cord formed from the amnion and chorion (membranes) provides a circulatory pathway connecting the embryo to the chorionic villi fuction: transport of oxygen and nutrients to the fetus one vein that carries O2 and blood 2 arteries that carries unoxygenated blood Wharton's jelly gelatinous mucopolysaccharide that gives bulk to umbilical cord prevent compression of vein and arteries prevents tying of umbilical cord no nerve supply, therefore no pain
5. Membranes Chorionic Membrane outermost fetal membrane offer support to the sac that contain amniotic fluid Amniotic Membrane lines the chorionic membrane - covers fetal surface of the placenta - no nerve supply - produce phospholipid ** many membranes to prevent leaking of amniotic fluid ** amniotomy prick amniotic and chorionic membrane Yolk sac cavity provides further nourishment Amniotic Fluid clear, slighty yellowish liquid (green means fetus had already defecated therefore must open up because it could lead to pneumonia) ** Meconium first fecal matter of fetus ** Gastric Lavage withdraw 14
NCM 201: Promotive and Preventive Care Management
constantly being formed and reabsorbed by mother and process it as waste products some are being swallowed by the baby 800 1200 ml of amniotic fluid/ day Hydramnios / Polyhydramnios excessive amount of amniotic fluid; > 2000ml; could lead to fetal distres; hard for mother = poor oxygenation, balance, uterus too big Oligohydramnios amount of fluid < 600 ml; possibility of cord compression = fetal distress Purposes of Amniotic Fluid protective mechanism = serves as cushion protects fetus from temporary changes aids in muscular development contents: albumin, urea, uric acid, creatinine, lecithin and sphingomyelin ** amniotic fluid index ultrasound to measure amniotic fluid; 14& above = normal! Origin and Development of Organ System Germ Layers specific tissue layers where body organs develop (ectoderm, mesoderm, endoderm) 2 cavities: > Amniotic Cavity > Yolk Sac supply nourishment; provide source of RBCs Organogenesis formation of organs A. Cardiovascular one of the 1st system to develop 24th day after fertilization heart starts to beat; shows fetal circulation distinct from mother 10th - 12th week FHB can be heard via Doppler; but very faint 11th week ECG may be traced; to check whether heart of fetus is functioning well Fetal Circulation contains mixed blood with less than maximal oxygen concentration fetus receives oxygen through the placenta Special Vessels: (should not be seen in an adult) 1. Ductus Venosus- connection between umbilical vein and ascending vena cava, bypassing the fetal liver 2. Ductus Arteriosus connection between pulmonary artery and aorta, bypassing the fetal lungs 3. Foramen Ovale opening between the right and left atria during fetal life, bypassing fetal lungs ** right after birth, these immediately closes and becomes a ligament in adults B. Respiratory System 3rd week ofl ife, the respiratory and digestive tract exist as one (trachea & esophagus are one) ** esophageal atresia digestive and respiratory tract failed to separate end of 4th week, septum divides esophagus from trachea 6th week, lung buds extend into the abdomen 7th week, diaphragm divides thoracic cavity from abdomen ** teratogen could cause birth defect 3 months, spontaneous respiratory movement Surfactant prevents atelectasis (lung collapse) creates surface tension; phospholipid substance which decreases alveolar surface tension on expiration ( if no surfactant, when inhalation occurs, lungs will just stick) chief components: lecithin, sphingomyelin 2:1 15
NCM 201: Promotive and Preventive Care Management
C. Nervous System develop extremely early in pregnancy 3rd / 4th week active formation of nervous system Neural plate thickened protion of the ectoderm a. Neural tube central nervous system b. Neural crest peripheral nervous system 8th week brain waves can be detected by EEG (electroencephalogram) 24th week ear is capable of responding to sound eyes exhibit papillary reaction D. Endocrine System fetal adrenal glands supply a precursor for estrogen synthesis by the placenta fetal pancreas produces insulin thyroid and parathyroid glands metabolic functions and calcium balance
E. Digestive System 4th week intestinal tract grows rapidly 10th week intestine remains in the base of the umbilical cord Meconium cellular wastes, bile, fats, mucoprotein, mucopolysaccharide, vernix caseosa black or dark green; not happening in the 1st and 2nd trimester gastric lavage GIT is sterile before birth 32nd week sucking and swallowing reflex liver is active but immature Hypoglycemia (cover baby to prevent heat loss) and hyperbilirubinemia (bilirubin causes sclera and yellow skin) ** sunlight causes maturity of liver therefore capable of changing bilirubin to a form that could be excreted ** indirect bilirubin (causes yellow skin color) should be turned to direct bilirubin ** liver then produces glucoronyl transferase that converts indirect B to direct B. F. G. > Musculoskeletal System original cartilages that 2nd week cartilage prototypes provide position and support 11th week fetal movement can be seen in ultrasound
Reproductive System sex is determined at the moment of conception 6th week gonad form 2 ducts present: > Wolfian Duct for male Mullerian for female ** Pseudohermaphroditism - during first trimester, parents are discouraged to have ultrasound because reproductive system is not clear yet. If testosterone level is high, mullerian duct will disappear and vice versa. On 1 st trimester, mother will be surprised tha fetus has 2 ducts! H. Urinary System 12th week urine is formed (adds up to the amount of amniotic fluid), excreted into the amniotic fluid by 16 th week at term, 500 ml/day oligohydramnios
16
NCM 201: Promotive and Preventive Care Management
I. Integumentary System fetal skin appears thin and almost translucent 36th week subcutaneous fat begins to be deposited Lanugo soft downy hair for temperature regulation; preterm no lanugo; post term increased lanugo Vernix Caseosa white cheesy substance that prevents maceration; helps in regulation of temperature ** spread vernix caseosa at newborn care to prevent hypothermia J. Immune System maternal antibodies crosses the placenta on the 3rd trimester ** first month of life, maternal antibodies still cover the baby; that is why only after 6 weeks of life that doctors give vaccines except for Hepa and BCG vaccines passive immunity against polio, German measles, Rubeola, tetanus, pertussis Assessment of Fetal Growth and Development Nursing Responsibilites: Obtain consent patient voluntarily submitted herself; consent for anything considered invasive; for legal protection of nurses; even ultrasound needs consent(verbal) Schedule the procedure Explain the procedure to alleviate anxiety of patient; to gain cooperation Prepare the client physically and psychologically (presence of nurse) Provide support during the procedure either assisting with the doctor or staying with pt. Assessing both fetal and maternal responses Providing after care to the client, equipment, and specimens Estimating Fetal Growth 1. McDonald's Rule method of determining that the fetus is growing in uterus by measuring Fundal Height Formula: AOG in months = FH in cm x 2/7 AOG in weeks = FH in cm x 8/7 ** Greater Fundal Height (than AOG) multiple pregnancy, miscalculated due date, LGA infant, hydramnios, H-mole ** Lesser Fundal Height SGA, pregnancy length miscalculated, or an anomaly is developing, IUGR (intrauterine growth restriction) 2. Bartholomew's Rule of 4's measures AOG by determining the position of the uterus in the abdominal cavity - 4 months below the umbilicus and 4 months above the umbilicus 6, 7, 8, 9 months level of fundus above umbilicus 1, 2, 3, 4, 5 months level of fundus below umbilicus 12 weeks fundus over the symphysis pubis 16 weeks halfway between symphysis pubis and umbilicus 20 weeks at umbilicus 36 weeks at the xyphoid process; lightening and engagement ** descent more than 36 weeks ** 37 40 weeks - ideal AOG Assessing Fetal Wellbeing a. Fetal Movement / Fetal Quick Count SANDOVSKY METHOD best time is early morning (8-9am) after a meal; flat, recumbent position for 1 straight hr; no changing positions, no interruptions; 1x/ week Quickening at 18 20 weeks of pregnancy 17
NCM 201: Promotive and Preventive Care Management
30 weeks and above AOG to start counting kicks normal: 2 times every 10mins or 10 12 times/hr urinate first before procedure because it should be uninterrupted less than 5 fetus experiencing distress; poor placental perfussion (unable to provide sufficient O2) in a chosen hr, there are no kicks at all could mean fetus is asleep. Let pt. Drink milk or eat to stimulate fetus, or use a bell (vibroacoustic); call doctor if nothing happened ** when legs are flexed, perineal muscles are relaxed; cant feel fetal movement if there's a contraction b. Fetal Heart Rate Monitoring normal: 120 160bpm can be heard using Doppler as early as 11th week; or use stethoscope use Leoplod's maneuver first to find position of fetal back smooth and contour Electronic Fetal Monitor (EFM)
c. Rhythm Strip Testing 2 probes in uterine Assessment of FHR > Baseline Reading average rate of the FHR/min dont have to count manually > Short Term Variability beat-to-beat variability denotes PNS activity > Long Term Variability denotes the differences in FHR that occur over the 20min time period denotes CNS activity CTG / Cardiotocogram measures FHB against mother's uterine contractions ** when contracting, there should be an increase in FHB ** placental insufficiency if FHB goes up when not contracting d. Non stress Test (NST) monitor uterine contraction and FHB uses electronic fetal monitor to obtain the response of the FHR to fetal movement FHR increass about 15bpm when fetus moves if no increase, poor O2 perfussion Reactive: 2 accelerations of FHR within the chosen period Non reactive: no accelerations occur with fetal movement; fetal distress or abnormality ** fetal heart rate increases only if there's fetal movement and uterine contractions e. Vibroacoustic Stimulation application of an instrument to produce a sharp sound to startle or wake the fetus could be done with NST/CTG; bell just on top of tummy of pt. f. Contraction Stress Test (Nipple Stimulation Test) fetal heart rate is analyzed in reference to contraction once nipple is stimulated, oxytocin is delivered therefore muscle contractions in uterus g. Ultrasound response of sound waves to object used to diagnose pregnancy, confirm the presence, size and location of placenta preferably 2x: during confirmation (as early as 3wks) and during 3rd trimester used to discover complications of pregnancy (eg. Placenta previa) 18
NCM 201: Promotive and Preventive Care Management
h. Doppler Umbilical Velocimetry study blood flow changes that occur in maternal and fetal circulation to assess placental function vascular resistance blood in placenta very viscous; mother may have hypertension or GDM i. Placental Grading based on changes, particularly on the amount of Calcium deposits in the bas of placenta grading of placenta assess AOG grade O 12 24 weeks 1 30 32 weeks 2 36 weeks 3 mature (placental aging = woman has to give birth)
j. Amniotic Fluid Volume Assessment a decrease amniotic fluid volume puts the fetus at risk for compression of the umbilical cord 800 1200 ml of amniotic fluid fetal kidney output = to check! Average index: 15 cm for 38 40 weeks; more than 20 24cm = hydramnios/polyhydramnios less than 14 cm = oligohydramnios k. Electrocardiography (ECG) done as early as 11th week to trace heart activity with aid of fetal monitoring device l. Magnetic Resonance Imaging CT scan radiographic!; contraindicated; should be used only in the 2 nd and 3rd trimester very clear picture; can get a glimpse of inch by inch part of fetus m. Assay of Maternal Serum may be used to determine levels of various hormones as assessments of fetal well-being important to know if baby has Down's syndrome / other abnormalities n. Alpha Fetoproten (AFP) glycogen substance produced by the fetal liver specimen: maternal blood ** MSAFP maternal serum alpha fetoprotein found in amniotic fluid and maternal serum abnormally high opening on fetal abdomen low child may have Down's syndrome, Trisomy 21 o. Chorionic Villi Sampling biopsy and analysis of chorionic villi for chromosome analysis done at 5 10 weeks of pregnancy early assessment of fetal anomaly p. Coelocentesis transvaginal aspiration of the coelomic fluid done as early as 6th - 10th week 19
NCM 201: Promotive and Preventive Care Management
** coelomic pouch q. Amniocentesis done with the aid of ultrasound aspiration of amniotic fluid from the uterus color: as clear as tap water lecithin / sphingomyelin determines fetal lung maturity; 2:1 used to determine fetal maturity and detect certain birth defects such as down's syndrome, spnial bifida, hemolytic disease of the newborn, sex and chromosomal abnormalities r. Biophysical Profile (Fetal Apgar) assess fetus at risk for intrauterine compromise with aid of ultrasound Parameters used in BPP: > fetal breathing movements 2nd trimester = visible rising and falling of chest > fetal movement > fetal heart reactivity done by NST > fetal tone > placental grade > amniotic fluid volume ** perfect score: 2 per parameter Interpretations: scores 8 12: doing well scores 4 6: fetus in jeopardy 2 most important components: NST, AFI s. Triple Marker Screening maternal blood sample is taken to determine the levels of HCG, estriol, MSAFP Interpretations: ** low MSAFP, low estriol, high HCG Down's syndrome ** low levels of the 3 hormones trisomy 18 very rare fetal disorder t. Percutaneous Umbilical Blood Sampling involves inserting a needle into the fetal umbilical cord and aspirating blood for analysis guided by ultrasound and is used to screen karyotypes (chromosomes); examine ativodies for teratogenic viruses and provide assessment for fetal blood transfusions.
20
NCM 201: Promotive and Preventive Care Management
Assessment of Maternal Wellbeing During Pregnancy prenatal visits / check up for confirmation; missed menstrual period = usual reason First Prenatal Visit occurs as soon as the woman thinks she might be pregnant the longest period Objectives: to confirm or rule out pregnancy to ascertain risk factors to determine the due date (using Naegele's rule) to provide education on maintaining a healthy pregnancy Components: 1. History most important element - written questionnaire or by face-to-face interview Parts of History Taking: a. Chief complaint amenorrhea b. Reproductive history LMP, GTPAL (gravida, term, para, abortion, living children), menarche, length of menstrual cycle c. Medical surgical ooectomy, breast augmentation, colicystectomy d. Family History hypertension, diabetes e. Social History occupation 2. Physical Examination covers all body system - head-to-toe examination - vaginal speculum examination > Papanicolaou Test / Pap Smear for early detection of cervical cancer 3. Laboratory Assessment CBC to determine hemoglobin level (if low affect O2 of fetus) Blood Type and Antibody Screen Rubella Titer Urine Culture TB Screening Purified Protein Derivative (PPD) Ultrasound Subsequent Visits: o Schedule Week 01 32 32 - 36 36 - delivery Include Specific Assessments: Weight 3 -12 12 (to avoid striae gravidarum) BP Urine protein and glucose Fetal Heart Rate ultrasound in 2nd trimester 21 Number of Visits once/month 2x/month Every week
NCM 201: Promotive and Preventive Care Management
Danger signs of pregnancy Fetal movement Contractions for cases of miscarriage in 1st trimester Membrane rupture Fundal Height
Danger Signs of Pregnancy Fevere or severe vomiting Severe or continuous headache Blurred vision or spots before the eyes Pain in the epigastric or abdominal area Sudden weight gain or sudden onset of edema Vaginal bleeding Painful urination Sudden gush or constant, uncontrollable leaking of fluid from the vagina Decreased fetal movement Signs of Pre-term Labor ** Labor series of events that end in the product of conception Uterine Contractions regular, painful Lower, dull backache due to crowning or engagement Pelvic pressure engagement Menstrual-like cramps uterine contractions Increase vaginal discharge SHOW bloody mucoid vaginal discharges; ROM A feeling that something is not right Markers in Fetal Development **milestones of fetal development 4 weeks embryo is 4 5 mm in length trophoblasts embedded in decidua foundations for nervous system, genitourinary system, skin, bones and lungs are formed rudiments of eyes, ears and nose appear 5 8 weeks fetus is 27 31mm in length and weighs 2 4gms fetus is markedly bent head is disproportionately large as a result of brain development sex differentiation begins centers of bone begin to ossify 9 12 weeks fetus average length is 50 87mm and weighs 45 gms fingers and toes are distinct placenta is complete rudimentary kidneys secrete urine fetal circulation is complete external genitalia show definite characteristics 13 16 weeks fetus is 94 140mm in length and weighs 97 200gms head is erect lower limbs are well developed 22
NCM 201: Promotive and Preventive Care Management
coordinated limb movements are present heart beat is present lanugo develops nasal septum and palate close fingerprints are set 17 20 weeks fetus is 150 190mm in length and weighs approximately 260 460 gms lanugo covers entire body eyebrows and scalp hair is present heart sounds are perceptible by auscultation vernix caseosa cover skin 21 25 weeks fetus is about 200 240mm in length and weighs 495 910 gms skin appears wrinkled and pink to red REM begins eyebrow and fingernails develop sustained weight gain occurs 26 29 weeks fetus is 250 275mm in length and weighs 910 1500 gms skin is red rhythmic breathing occurs pupillary membrane disappears from eyes the fetus often survives if born prematurely 30 34 weeks fetus is 280 320mm in length and weighs 1700 2500 gms toenails become visible steady weight gain occurs vigorous fetal movement occurs 35 37 weeks fetus average length is 330 360mm and weighs 2700 3400 gms face and body have a loose, wrinkled appearance because of subcutaneous fat deposit body is usually plump lanugo disappears nails reach fingertip edge amniotic fluid decreases 38 40 weeks (full term) average fetus is 360mm in length and weighs 3400 3600 gms skin is smooth chest is prominent eyes are uniformly slate colored bones of skull are ossified and nearly together at sutures testes are in scrotum Relieving the Common Discomforts of Pregnancy Ankle edema rest with your feet elevated avoid prolonged standing avoid restrictive garments in the lower half of your body Backache apply local heat avoid prolonged standing stoop to pick up objects 23
NCM 201: Promotive and Preventive Care Management
Tylenol in usual adult dose may help wear low heeled shoes maintain correct posture tailor sitting, pelvic rocking and shoulder circling exercises and strengthen back Breast Tenderness wear a supportive bra decrease the amount of caffeine and carbonated beverages ingested Constipation increase fiber in diet drink additional fluids have a regular time for bowel movements Difficulty sleeping drink a warm caffeine-free drink before bed and practice relaxation techniques Fatigue schedule rest periods daily; have a regular bedtime routine use extra pillow for comfort Faintness move slowly avoid crowds remain in a cool environment lie on your left side when at rest Headache avoid eye strain visit your eye doctor rest with a cool cloth on your forehead take Tylenol in a regular adult dose, as needed report frequent persistent headaches to your primary care provider Heartburn eat small, frequent meals each day avoid overeating, as well as spicy, fatty and fried foods Hemorrhoids avoid constipation and straining with a bowel movement take a sitz bath. Apply a witch hazel compress. Leg cramps avoid pointing your toes straighten your leg and dorsiflex your ankle avoid crossing legs Nausea eat 6 small meals/day rather than 3 eat a piece of dry toast or some crackers before getting out of bed avoid foods or situations that worsen the nausea. If it persist, report this problem to your primary care provider. drink fluids separately rather than with your meals avoid fried, greasy, gas - producing, or spicy foods and foods with strong odors Nasal stuffiness use cool air vaporizer or humidifier; increase fluid intake; place moist towel on the sinuses, and massage the sinuses Ptyalism use mouthwash as needed chew gum / suck on hard candy Round Ligament Pain avoid twisting motions rise to a standing position slowly and use your hands to support the abdomen bend forward to relieve discomfort Shortness of breath use proper posture use pillows behind head and shoulders at night Urinary frequency void as necessary at least every 2 hours increase fluid intake avoid caffeine practice Kegel exercise (to prevent straining of muscles during labor and delivery) Vaginal discharge wear cotton underwear bathe daily avoid tight pantyhose 24
NCM 201: Promotive and Preventive Care Management
Varicose veins walk regularly. Rest with feet elevated. avoid prolonged standing dont cross your legs when sitting avoid knee-high stockings; wear support hosiery
Teaching Self-care during Pregnancy: Self Care Needs 1. Maintaining a balanced nutritional intake. **weight an indicator of maternal stability and health **folic acid CNS development; green leafy vegetables 2. Bathing personal hygiene - daily tub baths and shower are recommended. - as pregnancy advances, change tub bath to sponge bath - if vaginal bleeding/rupture of membrane are present, tub bath is contraindicated 3. Breast Care general rule is to wear a firm, supportive bra with wide straps and is non-wired - wash breast with clear tap water (no soap) daily to remove colostrum - if colostrum secretion is profuse, place gauze or breast pads inside the bra 4. Dental Care good tooth brushing habits should continue throughout pregnancy - encourage pregnant woman to see her dentist regularly - encourage snacking of nutritious food 5. Perineal Hygiene douching is contraindicated - wash perineal area regularly with mild soap and water 6. Dressing avoid garters, extremely firm girdles with panty legs and knee-high stockings - shoes should be moderately high or flat 7. Sexual Activity Common Myths: - Coitus on the expected date will initiate labor - Orgasm will initiate labor - Coitus during fertile days of a cycle will cause a 2 nd pregnancy or twins - Coitus might cause rupture of membrane 8. Exercise to prevent circulatory statis on the lower extremities - it can also offer a general feeling of well-being - exercise program should consist of: > 5 minutes warm up > 20 minutes stimulus phase > 5 minutes cool down 9. Sleep needs an increased amount of sleep to build new body cells during pregnancy - if the woman has trouble falling asleep, drinking a glass of warm milk may help and relaxation exercises - left Sim's lateral position with top leg forward 10. Travel early in normal pregnancy, there is no restrictions - when traveling, avoid eating uncooked food and drinking unpurified water - if long trip, plan for frequent stretch/rest periods
Prevention of Fetal Exposure to Teratogens Teratogen any factor, chemical or physical that adversely affects the fertilized ovum, embryo, or fetus. Factors that influence the effect of teratogen to the fetus: a. strength of teratogen 25
NCM 201: Promotive and Preventive Care Management
b. timing of teratogenic insult c. Teratogen's affinity to specific tissue Thalidomide causes limb defects. Tetracycline causes tooth enamel deficiency. I. Teratogenic Maternal Infections - either sexually transmitted or systemic infection (syphillis, herpes, gonorrhea) - TORCH group of diseases II. Toxoplasmosis protozoan infection uncooked meat, handling a cat stool in soil or cat litter almost no symptoms for fetus: CNS damage, hydrocephalus, microcephaly, retinaldeformities Rubella mother: causes mild rash and mild systemic illness flu-like symptoms for fetus: deafness, mental and motor challenges, cataracts, cardiac defects, retardation, cleft lip and palate Cytomegalovirus (CMV) member of the herpes virus family transmitted by droplet infection from person to person fetus: severely neurologically challenged, eye damage, deafness, chronic liver disease Herpes Simplex Virus (Genital Herpes Infection) virus spreads into the bloodstream and crosses the placenta 1st trimester severe congenital anomalies or spontaneous miscarriage 2nd / 3rd trimester premature birth, IUGR (intrauterine growth retardation)
Medication use General principle: almost all medications cross the placenta and can potentially affect the fetus - no meds (including OTC and herbal) should be used during pregnancy without the approval of primary caregiver
III. Substance Use and Abuse a) Caffeine may be safe if taken in moderation during pregnancy - increases the risk of spontaneous abortion b) Tobacco contraindicated - LBW, preterm labor, abortions, stillbirths, SIDS, birth defects and neonatal respiratory disorders c) Alcohol no safe amount of alcohol consumption during pregnancy d) Marijuana fetus: stressed nervous system e) Cocaine spontaneous abortion and premature labor - infants are small and have higher incidence of low birth weight IV. Environmental Teratogens Mental and Chemical Hazards - pesticides and carbon monoxide - arsenics (by product of copper and lead smelting) - paints - mercury - formaldehyde Radiation (x-ray, photocopiers) Hyperthermia and Hypothermia
V.
Teratogenicity of Maternal Stress Common Myths: - if a woman sees a mouse during pregnancy, her child will be born with a furry / mole-like birthmark 26
NCM 201: Promotive and Preventive Care Management
- eating strawberries causes strawberry birthmark - looking at a handicapped child while pregnant will cause child in utero to be handicapped the same way ** common sense and awareness of fetal maternal physiology have dispelled these superstitions Childbirth Education - classes conducted to prepare parents for childbirth - not synonymous to painless or drugless delivery Common topics: o psychological and emotional aspects of pregnancy o induction of labor o partners role in providing support o medications and anesthesia options o what to pack for the hospital o hospital admission routine o caesarian birth Specific Goals: prepare expectant mother and her partner for the childbirth experience create clients who are knowledgeable consumers of OB care help client reduce and manage pain with both pharmacologic and non-pharmacologic method help increase couples overall enjoyment of and satisfaction of the childbirth experience Other classes: o pregnancy and postpartum exercises o baby care classes for 1st time parents o breastfeeding classes o siblings classes
Perineal and Abdominal Exercises: a. Tailor Sitting b. Squatting c. Pelvic floor contractions
d. Abdominal muscle contractions e. Pelvic rocking
Methods of Pain Management: Techniques to control pain during labor: Premises: - discomfort during delivery can be minimized if the woman comes into labor informed about what is happening - if the womans abdomen is relaxed and the uterus is allowed to rise freely against abdominal wall during contractions - pain perception can be altered by techniques based on Gate Control Theory of Pain Management 1. Cutaneous Stimulation - involves sensory input from touch - can be achieved by: A. rubbing or patting the site B. applying heat or cold C. effleurage
D. holding clients hand firmly during contraction
27
NCM 201: Promotive and Preventive Care Management
2. Distraction - can be achieved by: A. breathing techniques B. focusing or sensate focus C. auditory stimuli 3. Reduction of Anxiety - teaching what to expect - presence of the nurse Methods of Prepared Childbirth I. Bradley Method - partner coached method - Robert Bradley (1981) - childbirth is a joyful natural process and stresses the importance of husbands Principles: need for solitude and darkness quiet environment for physical comfort II. III.
physical relaxation controlled breathing closed eyes and appearance of sleep
Dick Read Method Grantly Dick read (1987) Fear leads to tension which leads to pain Believed that pregnant women can interrupt the fear tension pain cycle Lamaze Method Psychoprophylactic method Fernant Lamaze Techniques: conscious relaxation cleansing breath (deep exhalation) consciously controlled breathing effleurage
focusing or imagery - 2nd stage breathing
Alternative Methods of Birth Leboyer Method - room is darkened - music playing - newborn is handled gently cutting of cord may be delayed for mother and child to bond Underwater Birth Method - enhances relaxation - less likely to release stress-related hormones - increased elasticity of the perineum
Hypnotherapy Birth - incorporating Dick-read and Lamaze 28
NCM 201: Promotive and Preventive Care Management
reduces number of complications
Birthing chairs pull of gravity helps expulsion of fetus Birthing beds Unit III: Caring for the Family during Labor and Birth Labor involuntary physiologic process whereby the contents of the gravid uterus are expelled through the birth canal into the external environment Delivery - actual event of birth or expulsion of fetus - takes only a few minutes Components of Labor: 1. Passage (pelvis) adequate size and contour 2. Passenger (fetus) appropriate size and in an advantageous position and presentation 3. Power (uterine contractions) adequate ; mothers ability to push with aid of uterine contractions 4. Psyche (womans reaction) favorable; psychological perception of mother 5. Placenta Passage Factors Affecting Labor: A. Pelvic Measurements a)Diagonal Conjugate from lower border of symphysis pubis to sacral promontory - should be 12.5 13cm; may be obtained by vaginal examination Landmarks: o lower border of symphysis pubis o sacral promontory b)Obstetric conjugate shortest distance between inner surface of symphysis pubis and sacral promontory - measured by subtracting 1.5 2cm (thickness of symphysis) from the diagonal conjugate - usually 11cm - most important pelvic measurement narrowest! Fetus will definitely pass here c)True conjugate/conjugate vera measured from upper margin of symphysis pubis to sacral promontory - should be at least 11 cm; may be obtained by x-ray or ultrasound d)Tuber ischial diameter/intertuberous diameter - measures the outlet between the inner borders of ischial tuberosities; should be at least 8-9cm - estimated on pelvic exam B. Ability of the uterine segment to distend, the cervix to dilate and the vaginal canal and introitus to distend C. Type of Pelvis D. Structure of pelvis (false vs. true pelvis) Pelvis 2 parts: False Pelvis provides support for the internal organs and upper part of the body - considered the superior half or portion above the pelvic inlet True Pelvis 29
NCM 201: Promotive and Preventive Care Management
- Pelvic inlet - Pelvic outlet - Pelvic cavity (canal) ***linea terminalis imaginary line that separates the true from the false pelvis Classification of Pelvis Gynecoid favorable! - most common type = occurs in about 50% of females - inlet is round - midpelvic diameter is adequate - except in macrocephaly and hydrocephalus - outlet is wide and round Android normal male pelvis - antero-posterior diameter = problem! - Occurs in 20% of females - Heart shaped - Fetal passage may be difficult Anthropoid oval-shaped - occurs in 25% of females - problem: transverse diameter is narrow (no room for rotation) - may pose difficulty in passage except when the fetus is occiput posterior position Platypelloid occurs in 5% of females - flat shaped - fetus may have difficulty rotating sufficiently - problem: antero-posterior diameter Passenger fetus and its ability to move through the passage I. Fetal Skull Bones (8) - 4 superior bones - 4 other bones Sutures (4) - allows the cranial bones to move and overlap sagittal between parietal coronal between parietal and frontal lambdoid between occipital and parietal temporal between temporal and parietal Fontanelles intersection of cranial sutures 2 parts: o anterior / bregma (diamond shape) disappears during 18th month o posterior (triangular shaped) between parietal and occipital ; disappears in the first 3 months Diameters of the Skull: Anteroposterior diameter a. suboccipitobregmatic diameter narrowest diameter (9.5cm) - from the anterior aspect of the occiput to the center of the anterior fontanelle - done during ultrasound b. occipitofrontal from the bride of the nose to the occipital prominence; 11.75 12cm 30
NCM 201: Promotive and Preventive Care Management
c. occipitomental widest diameter - from the chin to the posterior fontanelle Transverse diameter Biparietal 9.5cm Bitemporal 8cm II. Fetal Attitude / Habitus relationship of the fetal parts to one another - degree of flexion 1) complete flexion most common - neck is flexed, chest and the chin touching the sternum; arms are folded - one could see the suboccipitobregmatic diameter favorable 2) moderate flexion 2nd most common - military position (at attention) - neck slightly flexed but chin doesnt touch the chest - may deliver vaginally 3) partial extension poor - face occupies mothers vaginal orifice - unknown fetal attitude - head partially extended - sinciput (forehead) presenting part - can cause a difficult delivery; trial labor OR/DR 4) complete extension occipitomental presenting part - relatively rare and is considered abnormal (1:500 births) - neck and head hyperextended with occiput touching the upper back - involves face presentation (usually chin) III. Fetal Lie - relationship of the long axis of the fetus to the long axis of the mother vertical / longitudinal long axis of the fetus is parallel to the womans spine - nearly all fetuses assumes this lie (99%) - either cephalic or breech horizontal / transverse long axis of the fetus is horizontal to the long axis of the mother - less than 1% - never deliver vaginally: shoulder presentation diagonal / oblique lie fetal spine and maternal spine are at 45 angle to each other - head towards groin of mother - cant deliver vaginally - OB can manipulate in ultrasound provided umbilical cord is long IV. Fetal Presentation fetal body part that engages in the true pelvis Cephalic: vertex, brow, face Breech: frank, complete, single or double footling Shoulder cant deliver vaginally V. Fetal Position relationship of the presenting parts to the four quadrants of the mothers pelvis 1st letter = right or left 2nd letter = presenting part (O, S, M) 3rd letter = anterior or posterior 31
NCM 201: Promotive and Preventive Care Management
***neither left nor right DirectSA, DSP, DOA, DOP neither posterior nor anterior LST, RST, LOT, ROT VI. Station relationship of the presenting part to the true and false pelvis - landmark: ischial spine - presenting part at ischial spine = 0 - above ischial spine = negative - below ischial spine = positive a) floating presenting part movable above the true pelvic inlet b) engaged suboccipitobregmatic diameter fixed into the pelvic inlet c) station 0 representing part at the level of the ischial spine d) crowning station +4cm of the perineum e) dipping neither at station 0 nor floating; at station -4 or -5 ** precipitate delivery mother delivered outside the delivery room Power force of the uterine contractions primary source uterine contraction ultimately result in complete cervical effacement and dilatation secondary source contraction of the abdominal muscles such as with pushing and bearing down *** fundal push augmentation at tip of fundus 3 Phases: o Increment building up of the contraction (longest phase) o Acme peak of contraction o Decrement the letting down of the contraction Frequency time between the beginning of one contraction and the beginning of the next contraction Duration beginning of the contraction to the end of the same contraction - beginning of labor : duration of contractions = 30 40s - as labor continues: duration = 60 90s - more than 90s = fetal distress; lack of oxygen supply during contraction Intensity strength of uterine contraction during acme - cant be measured accurately mild uterine wall can still be indented (chin); 30 40s moderate fall between the 2 ranges (nose) strong uterine wall cant be indented (forehead); 60 90s Interval 1-2 minutes if near delivery Psyche feelings that the woman brings to labor - ambivalence, fear, anxiety, excitement - major component womans psychological readiness for labor Theories of Labor Onset 1. Uterine Stretch Theory believed that any hollow organ such as uterus tends to contract and empty itself when distended
32
NCM 201: Promotive and Preventive Care Management
2. Oxytocin Theory believed to increase just before the pregnancy comes to term and initiates labor due to its contractile activity on the myometrium - oxytocin stimulates contractions thus facilitating sealing of ruptured capillaries which then stops bleeding - known to be a patent uterotoxin (uterine muscle contractant) 3. Progesterone Deprivation Theory progestore produced by the placenta relaxes uterine smooth muscles by interfering with conduction of the impulses from one cell to the next - decreased amount of progesterone inhibits the relaxation effect on the uterus 4. Prostaglandin Initiation Theory amnion and deciduas, source of prostaglandin - rising fetal cortisol level increases the formation of prostaglandin which stimulates contraction - prostaglandin causes smooth muscle contractions 5. Theory of the Aging Placenta aging placenta cannot anymore support the growing fetus Premonitory Signs of Labor a) Lightening descent of the fetus and uterus into the pelvic cavity before labor onset - occurs 2 3 weeks earlier in primipara - in multipara, may not occur until labor begins; thus not a good premonitory sign for multipara b) Cervical changes Effacement progressive softening, ripening and thinning of the cervix - bloody show (expulsion of mucous plug) Dilation opening of cervical os during labor c) Regular Braxton Hicks contractions d) Rupture of amniotic membranes e) Nestling behaviors f) Weight loss of about 1-3lbs 2-3 days before labor onset Comparison of True and False Labor False Labor Irregular contractions Decrease in frequency and intensity Longer intervals between contractions Discomfort in lower abdomen and groin Activity such as walking either has no effect or decreases contraction Disappear while sleeping Sedation decreases or stops contractions Bloody show usually not present No appreciable change in the cervix Regular contractions Progressive frequency and intensity Shorter intervals between contractions Discomfort begins in back and radiates to the abdomen Activity such as walking increases contraction Continues while sleeping Sedation does not stop contraction Bloody show usually present Progressive thinning and opening of the cervix
True Labor
Fetal Monitoring during Labor and Delivery Normal fetal heart rate CTG used in labor room Normal fetal heart rate is 120-160bpm; must obtain a baseline Abnormal Fetal Heart Rate 1. Variability irregular fluctuations in the baseline of fetal heart rate of 2 cycles per minute or greater - absent / decreased withfetal sleep, fetal prematurity - drugs (anesthetics) 33
NCM 201: Promotive and Preventive Care Management
hypoxia; acidosis if persists longer than 30mins = indicator of fetal distress
2. Tachycardia more than 160 bpm lasting longer than 10mins - early signs of hypoxia; sign = increased vital signs - associated with maternal fever, fetal anemia, fetal or maternal infection - drugs (atropine sedative effect, vistaril antihistamine) maternal hyperthyroidism, heart failure
3. Bradycardia less than 110bpm lasting longer than 10mins - late sign of fetal hypoxia - associated with maternal drugs (anesthetics), maternal supine hypotension syndrome - prolonged cord compression - fetal heart block 4. Accelerations 15bpm rise above baseline followed by a return to baseline - usually in response to fetal movement or contractions = good! - Indicates fetal wellbeing 5. Decelerations fall below baseline lasting 15s or more followed by a return to baseline - if go down during decrement stage or go down after fetal movement = okay! - Classified into early, late and variable decelarations Type 1 (Early deceleration) - cause: fetal head compression - there is already engagement - FHR decreases with onset of contraction and mirrors the pattern of contractions - Range of drop in FHR within normal parameters - Has a uniform shape - Innocuous = non-life threatening - Nursing implications: continue observation Type 2 (late deceleration) - cause: uteroplacental insufficiency causing fetal hypoxia - FHR decreases after the onset of contraction - FHR deceleration persists beyond completion of contraction - Range of drop in FHR within normal parameters - Has a uniform shape - Ominous = life threatening! - Nursing implications: turn client to left side, give oxygen and summon physician Type 3 (Variable deceleration) - cause: umbilical cord compression - FHR decreases at any point during or between contractions - Decelerations may be jagged V or U-shaped - Range of drop in FHR is large and extends below normal - Not uniform in shape - Ominous - Nursing implications: turn client to left side, give oxygen and summon physician 34
NCM 201: Promotive and Preventive Care Management
Stages during Labor and Delivery A. Stage 1:Dilatation Stage - from 0-10cm cervical dilatation - beginning of true labor to full cervical dilatation (10cm) - 6-18hrs for primigravida - 2-10hrs for multipara 3 phases of 1st stage: o Latent Phase mild short contractions - 0-3cm - pain is tolerable; can still walk - excited and happy; good time to get data for babys birth certificate - follows directions readily - walking assists labor; facilitates cervical dilatation - any analgesia given early in labor may prolong the stage - 6hrs for primi and 4 for multi o Active Phase moderate to strong contractions, 5mins apart - 4-7cm - best time to inform client not to go to toilet and cant eat - bloody show, ROM - slow, deep breathing techniques can help in relaxing - has difficulty in following instructions - supportive measures - 3hrs in primi and 2hrs in multi o Transition Phase strong contractions 1-2 mins apart - 7-10cm with bloody show - shortest! Less than 1hr - urge to push; allow to push if 10cm already Signs and Symptoms of Impending 2nd stage of Labor - beads of perspiration - increase bloody show - urge to urinate/defecate in every contraction
- urge to push at every contraction (wait for intense contraction) - vomiting/nausea
B. Stage 2: Delivery Stage - complete cervical dilatation to delivery of the neonate - clients emotions heightened - duration: 2-60mins - contractions causes the labia to part - head of the fetus descends further until crowning occurs **Ritgens maneuver apply pressure on perineal area to prevent laceration; use gauze Cardinal Movements of Labor - Engagement - Flexion - Extension - Descent - Internal Rotation - External Rotation C. Stage 3: Placental Expulsion Stage - time between the delivery of the neonate and the delivery of the placenta - uterus can be felt as round mass, firm to touch, just below the level of the umbilicus - duration: 5 -30mins
- Expulsion
35
NCM 201: Promotive and Preventive Care Management
**Placenta accrete deeply attached placenta **manual = could result to retained placental fragments hemorrhage 2 Phases of the 3rd Stage Placental Separation occurs after the uterus resumes contractions Signs of Placental Separation - globular-shaped uterus - rise of the fundus in the abdomen - sudden gush/trickle of blood - lengthening of the umbilical cord **about 80% of all placenta begin separation at the center and fold into themselves Mechanisms: schultze, Duncan - normal blood loss 300-500ml Placental Expulsion accomplished with the natural bearing down of the mother or gentle pressure on the fundus of the contracting uterus (Credes maneuver) ** if not delivered spontaneously, it may need to be removed manually D. Stage 4: Recovery Stage first 2-4 hrs after delivery; monitor every 15mins time immediately after the delivery of the placenta encompasses the 1st hour after delivery
Nursing Responsibilities - palpate the fundus every 15mins for firmness and height in relation to umbilicus - monitor vital signs - check for bladder distention; determine voiding pattern - chck the perineum for vaginal and suture line bleeding - check episiotomy or laceration site for hematoma - keep the client warm and comfortable - provide fluids and food as tolerated - administer oxytocic medication as orered - promote bonding - assist with breastfeeding - assess lochia for color and amount Lochia post-partum vaginal discharge containing blood, mucus and placental tissue; present till 6wks 3 Stages of Lochia Lochia rubra first discharge - red in color - 3-5days after delivery Lochia serosa thinned and turned brownish/pinkish in color - contains serous exudate, erythrocytes, leukocytes and cervical mucus - continues until around the 10th day after delivery Lochia alba turned whitish/yellowish white - 2nd to 3rd or 6th week after delivery General Nursing Care During Intrapartal Period A. Assessment (on admission) 36
NCM 201: Promotive and Preventive Care Management
Age, weight, height, vital signs, allergies OB hx, EDB, intent to breastfeed or bottlefeed, prenatal care time and type of last meal time of onset of contractions, frequency, duration and intensity presence of bloody show, status of amniotic fluid FHR and pattern Leopold's maneuver emotional response to labor, presence of support system
B. Planning / Implementation First stage - orient to unit - time and assess contraction - assist with or perform vaginal exam - test urine for protein, glucose and ketones - assess bladder and bowel function - collect blood for CBC - provide emotional support to mother &labor coach - monitor frequency - monitor danger signs of labor > prolonged strong contractions > taut, boardlike abdomen > increase in pulse rate and temperature > hypertension > hypotension > bright red vaginal bleeding > meconium stained amniotic fluid > abnormal variations in FHR pattern
monitor FHR by Doppler interpret data of fetal monitoring prevent supine hypotension assist mother with breathing techniques use measures to promote comfort and rest observe perineum for bloody show keep mother on NPO approaching 2nd stage
2nd stage - assist mother with pushing, transfer to delivery room or prepare birthing bed when perineum bulges with contraction - make certain mother's legs are positioned simultaneously 3rd stage care of infant assist with delivery of placenta promote attachment provide support for parents if infant has an abnormality record birth and accompanying events 4th stage palpate the fundus every 15mins for firmness and height in relation to umbilicus monitor vital signs assess lochia for color and amount check for bladder distention, determine voiding pattern check perineum and vagina for bleeding check episiotomy or laceration site keep client warm and comfortable provide fluids and food as tolerated administer oxytocin medication as ordered 37
NCM 201: Promotive and Preventive Care Management
- promote bonding - assist with breastfeeding
Electronic Fetal Monitoring External Electric Monitoring to monitor both uterine contractions and FHR continuously and intermittently - sensors strapped to the woman's abdomen - contractions are monitored by means of a pressure transducer/tocodynamometer - only attached in LR; most common!; more sensitive than doppler Internal Electronic Monitor a pressure-sensing catheter is passed through the vagina to monitor contraction - FHR recording is obtained from fetal scalp electrode - contraindicated: placenta previa - used in severe cases of fetal distress Telemetry allows monitoring of both FHR and uterine contractions to be carried out free of connecting wires Fetal Heart Rate Tracing trace both FHR and the duration and interval of uterine contractions onto paper rolls Pharmacologic Relief during Labor and Birth a. Narcotic analgesia (Demerol) b. Lumbar epidural block administered for 1st stage of labor (Marcaine) c. Pudendal block administered just before delivery for perineal anesthesia (Lidocaine) d. Local infiltration of perineum injected just before delivery for episiotomy incision (Lidocaine) e. General intravenous anesthetic (Thiopental)
Cesarian Births derived from Latin word: Caedore to cut 2 types: Scheduled and Emergency
Intraoperative Care Measures Administration of anesthesia Skin prep.
Surgical Incision 2 types: > classic > transverse
*** VBAC vaginal birth after cesarian
Unit IV: Postpartum Postpartum care medical and nursing care given to a woman during the puerperium 6 week period after delivery 38
NCM 201: Promotive and Preventive Care Management
client's body goes back to pre-pregnant state 2 classifications of maternal changes: > Retrogressive changes > Progressive changes
Puerperium puer = child; parere = to bring forth Puerpera the woman in puerperium Nursing Objectives o provide psychological support o promote uterine involution o promote successful breastfeeding o prevent common discomforts of puerperium o prevent complications of puerperium o initiate contraception Postpartum Psychosocial Adaptation Taking in Phase beginning to be meditative - dependently = vulnerable - 1-2 days postpartum - passive and dependent; concerned with own needs - verbalizes about the delivery experience - sleep/food important - need help with everyday activities as ell as childcare - exercise helps in uterine involution, except for CS Taking Hold Phase (dependent / independent) - 3-10 days postpartum - strives for independence and begins to reassert herself - mood swings occur; may cry for no reason - maximal stage of learning readiness - requires reassurance that she can perform tasks of motherhood Letting Go Phase (Interdependence) - 10 days-6 weeks postpartum - realistic regarding role transition - shows pattern of lifestyle that includes the new baby but still focuses on entire family as a unit - accepts baby as a separate person - Postpartum blues Physiologic Changes A. Reproductive Changes I. Uterus - process of involution takes 4-6weeks to complete - weight of the uterus - fundus steadily descends into true pelvis - 1 fingerbreadth (1cm)/day - by 10-14 days postpartum, cannot be palpated abdominally - lochia Measures to Promote Involution of the Uterus proper position prone; for CS= sit down with legs touching chest (fetal position) 39
NCM 201: Promotive and Preventive Care Management
oxytocin drugs as ordered breastfeeding early ambulation regular bladder emptying every 2hrs proper postpartum diet 3000kCal for breastfeeding; 2500kCal for nonbreastfeeding clients
Factors Delaying Uterine Involution o multiparity o overdistention of uterus o infection o hormonal deficiencies o retained placental membranes o bladder distention II.Cervix - thicker and firmer - 3-4 months - permanent change in the cervical os from round to elongated III.Vagina - smooth and smaller with poor tone after delivery - rugae reappear by 3-4 postpartum weeks - hymen permanently torn - Kegel exercise IV. Perineum - edematous and bruised after delivery - episiotomy and lacerations may be present V. Breast - colostrum present at birth; breast milk is produced by the 3rd or 4th postpartum day - congestion subsides in 1-2days - the average amount of milk produced in 24hrs increases with time (1) first week = 6-10oz (2) 1-4th week = 20oz (3) after 4 weeks = 30 oz
B. Systemic Changes I.Respiratory System - pulmonary function return to nonpregnant state by 6months post-delivery II.Endocrine System - ovulation and resumption of menstruation are influenced by whether or not the client breastfeeds - 48% (lactating women) resume menstruation by 12weeks - 80% have 1 or more anovulatory cycles the 1st ovulation - 40% (nonlactating women) resume menstruation by 6weeks - 65% by 12weeks 40
NCM 201: Promotive and Preventive Care Management
- 90% by 24weeks - 50% ovulate during the 1st cycle III.Circulatory System - diuresis + blood loss at birth = normal blood volume of mother - 1st - 2nd week postpartum, blood volume has returned to normal - increased fibrinogen level - increased leukocytes IV.Immune System - slight increase in temperature after delivery is normal V.Renal and Urinary Changes - over distention of the bladder is common due to: > increased bladder capacity > bruising of the tissues around urethra > diminished sensation to increased pressure - adequate bladder emptying resumes in 5-7 days after delivery - puerperal diaphoresis and diuresis occur within 24hrs post-delivery VI. Gastrointestinal System - constipation and hemorrhoids are common - bowel sounds are active - bowel evacuation may be difficult VII. Integumentary System - striae will fade to silvery white ***Diastasis Recti hollow portion felt in between ruptured connective tissues - chloasma and linea nigra barely noticeable Effects of Retrogressive Changes Exhaustion Weight loss - diuresis and diaphoresis during the 2nd to 5th day postpartum - weight after 6weeks = baseline weight Postpartum Warning Signs and Symptoms to Report to the Physician increased bleeding, clots or passage of tissue bright red vaginal bleeding anytime after birth pain greater than expected (abdomen) temperature elevation to 104 F feeling of full bladder accompanied by inability to void enlarging hematoma (specifically on vulvar area) feeling restless accompanied by pallor, cool, clammy skin, rapid heart rate, dizziness, and usual disturbances signs of hypovolemic shock pain, redness, and warmth accompanied by a firm area in the calf Homan's sign difficulty breathing, rapid heart rate, chest pain, cough, feeling of apprehension, pale, cold or blue skin pneumonia/other respiratory problems 41
NCM 201: Promotive and Preventive Care Management
atelectasis because of a very high amount of fibrinogen Progressive Changes 1. Lactation formation of breast milk is initiated whether or not the woman plans to breastfeed. Physiology of Breastmilk Production Placental Expulsion decreased estrogen and progesterone levels stimulate APG to produce prolactin stored in collecting tubules infant sucks PPG is stimulated to produce oxytocin causes contraction of smooth muscles milk ejected forward let down or milk ejection reflex production of hindmilk
Factors to Successful Breastfeeding a. start early within 4hrs after delivery b. feed early and frequency every 2hrs c. empty the breasts totally with each feeding time d. allow newborn to nurse in short frequent periods e. provide a relaxed, warm and supportive environment f. benefits of breastfeeding g. proper diet Measures to Promote Breast Comfort and Hygiene
express a small amount of milk wear a well-fitting bra use of compresses breast massage analgesics as ordered 42
NCM 201: Promotive and Preventive Care Management breast hygiene
2. Return of Menstrual Flow - decrease in hormones cause a rise in the production of FSH - if not breastfeeding, return of menstrual flow is expected within 6-10weeks - if breastfeeding, may not return for 3-4months Common Discomforts of the Puerperium A. Breast engorgement B. Afterpains C. Urinary Retention D. Hemorrhoids E. Constipation F. Painful Episiotomy Wound Muscle Strengthening Exercises
abdominal breathing - 1st day postpartum Chin-to-chest - 2nd day Perineal contraction - 3rd day Arm raising (sidewards) - 4th day leg raising sit-ups wait until 10th or 12th day after delivery
Postpartal Discharge Instruction a. Work avoid heavy work b. return to work only after 3weeks or later c. Rest atleast one rest period a day and try to get a good night's rest d. Exercise one flight of stair/day for the 1st week at home e. Hygiene may take either tub bath /shower f. continue apply cream on perineal area g. clean perineum from front to back h. no vaginal douche i. Coitus safe if lochia is whitish in color j. Contraception should begin with the initiation of coitus Unit V: Pregnancy at Risk Hypovolemic Shock 25% of blood is lost, could lead to fetal distress decrease blood flow to the peripheral organs 10% of blood is lost (2 units of blood; 1 unit = 400-500ml) s/s: decreased BP, CVP, Urine output, LOC
43
NCM 201: Promotive and Preventive Care Management
increased PR, RR - cold, clammy skin Pathophysiology of Hypovolemic Shock Bleeding Constriction of peripheral blood vessels HR and BP When shock worsens, compensatory mechanisms fail Inadequate tissue perfusion cellular O2 metabolism
Build up of lactic acid & devt. of metabolic acidosis Vasodilation Bleeding Circulating blood becomes insufficient to perfuse cardiac and brain tissue Maternal death
Bleeding during Pregnancy 1st Trimester Bleeding Abortion any interruption of pregnancy before the fetus is viable Abortus conceptus which is expelled Miscarriage lay term for abortion Causes: (a) Abnormal fetal formation (b) Implantation abnormalities (c) Lack of progesterone production by the corpus luteum (d) Trauma (e) Infection (f) Ingestion of teratogenic drugs Types: 1. Spontaneous Abortion loss of pregnancy that occurs naturally for unknown reasons s/s: vaginal bleeding Pathophysiology Loss of HCG, progesterone & estrogen level 44
NCM 201: Promotive and Preventive Care Management
Uterine decidua sloughs off Vaginal bleeding Uterus becomes irritable Contracts & expels the fetus 2. Induced Abortion abortion done intentionally - 2 types: > therapeutic / medical abortion > criminal abortion
3. Threatened Abortion unexplained vaginal bleeding without cramping or dilatation - s/s: vaginal bleeding rhythmic uterine cramping persistent backache feelings of pelvic pressure 4. Imminent or Inevitable situation where irreversible uterine evacuation has begun - D&C is done if no FHB 5. Complete entire contents of the conception is expelled spontaneously without any assistance - bleeding is minimal and observed for 24-48hrs 6. Incomplete part of the conceptus is expelled but the membranes or placenta are retained in the uterus - major manifestations: > uterine bleeding > severe abdominal cramping 7. Missed Abortion fetus dies in utero and is retained for 2 or more months - early s/s: uterus stops growing painless vaginal bleeding - marked degenerative changes: * maceration * mummification * Lithopedian formation 8. Habitual or Recurrent abortion that occurs following 2 previous consecutive pregnancy losses - common cause: Incompetent cervix - other causes: > autoimmune > infection of the developing fetus > deviation of the uterus > defective sperm or ovum 9. Septic Abortion abortion that is complicated by infection - causes: > prolonged unrecognized rupture of membrane > pregnant with IUD in utero > criminal attempts to terminate pregnancy 45
NCM 201: Promotive and Preventive Care Management
- s/s:
* fever * crampy abdominal pain * uterus feels tender on palpation
- if untreated: > toxic shock syndrome > septicemia > kidney failure > death - management for septic abortion: IVF high doses of antibiotics removal of infected and necrotic tissue TT immunization
General Nursing Care for Abortion - monitor BP/PR - observe for behaviors indicative of shock - count pads and weigh them - assess FHB - prepare IV therapy - have O2 available - complete bedrest without BP - inform client to abstain from coitus Nursing Diagnosis Fear r/t possible pregnancy loss Alteration in comfort: pain r/t abdominal cramping Anticipatory grieving r/t expected loss of unborn child Ectopic Pregnancy refers to pregnancy outside the uterine cavity - unknown cause Sites of implantation: > fallopian tube > surface of the cervix > cervix > intestine/abdominal
- s/s: a. early signs - usual symptom of pregnancy - dull pain on the affected side b. tubal rupture (6-14wks) - sudden, sharp, severe low quadrant pain that radiates to the shoulders
vaginal bleeding signs of shock Cullens sign bluish discoloration just under the navel excruciating pain in the cervix upon examination 46
NCM 201: Promotive and Preventive Care Management
- tender mass is usually palpable in the Cul-de-sac of Douglas
- decreased hgb, hct, increased WBC Diagnostic Evaluation transvaginal ultrasound pregnancy test high resolution ultrasound culdocentesis laparoscopy
Therapeutic Management o Medical Management - methotrexate folic acid antagonist that interferes cellular regeneration or building up of new cells o Surgical - linear salphingostomy ***TAHBSO total abdominal hysterectomy with bilateral salphingo-oophorectemy o Nursing Care - modified trendelenburg position observe for increasing pain especially on the shoulders assess for vaginal bleeding observe for signs and symptoms of hypovolemic shock monitor vital signs advise to avoid sexual intercourse until medical treatment is successful
2nd Trimester Bleeding Gestational Trophoblastic Disease also known as H-mole, molar pregnancy proliferation and degeneration of trophoblastic villi filled with fluid can be considered as pregnancy grape-like clusters ovum too immature penetrated by multiple number of sperm may / may not lead to cancer risk factors: low CHON intake age below 18 y.o. and above 35 y.o. asian heritage
- types: a. Complete mole - characterized by large amount of edematous villi but no fetus / fetal membrane - due to entrance of multiple sperm 47
NCM 201: Promotive and Preventive Care Management
- anuclear ovum without maternal genetic material - associated with choriocarcinoma
b. Partial mole - 69 chromosomes - no embryo but fetal blood is present in the villi - if with embryo, multiple fetal abnormalities - rarely leads to carcinoma - s/s: * * * * * * * s/s of pregnancy uterus grows more rapidly than expected UTZ shows no developing fetus HCG titer is usually high vaginal spotting no FHB unusually early devt. of PIH
- therapeutic management: immediate evacuation of the mole follow up to detect malignant changes curettage to remove all molar tissues hysterectomy need for follow-up 1 year after molar evacuation - Nursing Diagnosis Fluid-volume deficit r/t uterine blood loss Grieving r/t loss of pregnancy Anxiety r/t potential malignancy Incompetent Cervix - painless condition in which cervix dilates without uterine contraction and allows passage of the fetus - causes: > congenital anomalies > trauma to the cervix > endocrine imbalance > infection / inflammation > increased maternal age - surgical management: cervical cerclage pursestring suture - 12th 14th wk of gestation - types: Shirodkar Technique vaginal mucous membrane is elevated and narrow strip is carried around the inernal os and tied - suture is absorbable McDonald Technique nonabsorbable suture around the cervix - temporary closure - Post op Care 48
NCM 201: Promotive and Preventive Care Management Bedrest after the procedure Ritrodine Hcl Monitor FHB Observe for signs of rupture of membrane Limit activity Avoid douching and coitus for 2 weeks
3rd Trimester Bleeding Placenta Previa - low implantation of the placenta - degrees: low-lying implanted near cervical os (on lower segment of the uterus) marginal placental edge is approaching the cervical os partial half or portion of the cervical os is covered by the placenta total covers entire cervical os - no internal examination because it may rupture the placenta - Conditions associated with Placenta Previa Multiparity integrity of uterine lining is very poor for attachment Multiple gestation placenta requires a large amount of space Alteration in uterine structure congenital defects Uterine scars from previous surgery - s/s: * sudden onset of painless uterine bleeding * boggy uterus * FHB and activity are weak * Fetus is usually in an abnormal presentation - Nursing alert!!!! Do not perform internal examination until location and position of placenta have been verified by UTZ. - Management: Conservative Treatment Active approach - vaginal delivery - C-section - medications Abruptio Placenta premature separation of placenta accidental hemorrhage apoplexy of the placenta ablatio placenta unknown primary cause Increased maternal age
- Predisposing factors: Chronic hypertensive disorders Cocaine use by the mother Multiple gestation 49
NCM 201: Promotive and Preventive Care Management
- s/s:
Short umbilical cord Direct trauma Manual manipulation of the uterus during pregnancy Nutritional deficiency (folate)
* if marginal, painless vaginal bleeding * if central, bleeding is painful, dark red in color types of hemorrhage: (a) Concealed edge is still attached; pooling of blood in the center (b) Apparent leaks of blood; edge is detached * abdomen is hard with board-like uterus * couvelaire uterus bluish discoloration of uterus signifying bleeding inside - types: 1. Covert / Severe / Central central separation 2. Overt / Partial / Marginal separation occurs at the margin 3. Placental Prolapse / Complete complete or almost total separation associated with massive vaginal bleeding - Management
If mild, fetus is immature and shows no sign of distress:
- bedrest - tocolytic drugs
If fetus shows signs of compromise or when there is excessive bleeding:
- CS - Vaginal Delivery - Nursing Care a. on admission, assess bleeding b. initial blood works c. oxygen mask (for both mother and fetus) d. monitor maternal and fetal status e. regulate IVF / BT as ordered f. CBR g. No vaginal exam h. prepare patient for surgery - Nursing Diagnosis Fluid volume deficit r/t excessive blood loss Risk for altered tissue perfusion r/t blood loss Knowledge deficit
50
NCM 201: Promotive and Preventive Care Management
51
You might also like
- Framework For Maternal and Child NursingDocument7 pagesFramework For Maternal and Child NursingPatricia Mae Macahilos100% (1)
- Pentagon Maternal and Child PDFDocument38 pagesPentagon Maternal and Child PDFmarie89meNo ratings yet
- Ob Penta NotesDocument56 pagesOb Penta Notesstuffednurse100% (1)
- Maternal and Child Nursing - Student - HandoutsDocument40 pagesMaternal and Child Nursing - Student - HandoutsPaulAliboghaNo ratings yet
- OB Nursing Ma'Am PacabisDocument16 pagesOB Nursing Ma'Am PacabisArgee AlonsabeNo ratings yet
- Curative and Rehabilitative Nursing Care Management of Clients in Acute Biologic CrisisDocument44 pagesCurative and Rehabilitative Nursing Care Management of Clients in Acute Biologic CrisisArgee AlonsabeNo ratings yet
- Maternal NursingDocument37 pagesMaternal NursingCai Velasco DecenaNo ratings yet
- Maternal and Child NotesDocument9 pagesMaternal and Child NotesAngela Marjorie JimenezNo ratings yet
- New Born CareDocument7 pagesNew Born CareFreisanChenMandumotanNo ratings yet
- Pediatric Nursing FinalDocument35 pagesPediatric Nursing FinalMariquita BuenafeNo ratings yet
- Maternity Nursing Lecture PresentationDocument69 pagesMaternity Nursing Lecture Presentationapi-3764215100% (8)
- Pediatric Nursing-Course AuditDocument305 pagesPediatric Nursing-Course AuditMarites Santos Aquino100% (1)
- Course Outline-Ncm109Document10 pagesCourse Outline-Ncm109Charmagne Yanga EpantoNo ratings yet
- Maternal and Child Health NursingDocument22 pagesMaternal and Child Health NursingRam Van MunsterNo ratings yet
- Maternal & Child Care Nursing Table of ContentsDocument2 pagesMaternal & Child Care Nursing Table of Contentsɹǝʍdןnos100% (4)
- Maternal and Child Health Nursing (NCM 101 Lect) Part 2Document2 pagesMaternal and Child Health Nursing (NCM 101 Lect) Part 2yunjung0518100% (1)
- Cemonc: Esmas, Lexi MCN 2 Le 1 1Document8 pagesCemonc: Esmas, Lexi MCN 2 Le 1 1EmpieNo ratings yet
- NCM 107 Maternal and Child Nursing Related Learning Experience BSN 2 AY 2020-2021Document18 pagesNCM 107 Maternal and Child Nursing Related Learning Experience BSN 2 AY 2020-2021janina myka100% (1)
- Maternal Child Nursing 2Document10 pagesMaternal Child Nursing 2eli_b1540% (5)
- Lecture Maternal and Child Health NursingDocument6 pagesLecture Maternal and Child Health NursingAmpie EmNo ratings yet
- Care of Mother, Child, Family and Population Group At-Risk or With ProblemsDocument52 pagesCare of Mother, Child, Family and Population Group At-Risk or With ProblemsMelchor Felipe Salvosa100% (1)
- Quiz On Pediatric NursingDocument3 pagesQuiz On Pediatric NursingFelecidario TaerNo ratings yet
- Answer and Rationale FundamentalsDocument20 pagesAnswer and Rationale FundamentalsCharles Gerard B. BeluanNo ratings yet
- Gynecology Test QuestionsDocument6 pagesGynecology Test Questionsdhodejun lizhaldeNo ratings yet
- Pedia Set B PRNDocument9 pagesPedia Set B PRNEdgar RebuyasNo ratings yet
- Maternal and Child HealthDocument7 pagesMaternal and Child HealthNessa Layos MorilloNo ratings yet
- Maternity and Newborn Nursing ReviewerDocument40 pagesMaternity and Newborn Nursing Reviewerrahkel08No ratings yet
- Maternal and Child Health Nursing (NCM 101 Lect) Part 1Document4 pagesMaternal and Child Health Nursing (NCM 101 Lect) Part 1yunjung0518100% (7)
- NCM 101 FinalsDocument3 pagesNCM 101 FinalsPaul Jhon Vergara100% (2)
- Health Educ Handout #11Document3 pagesHealth Educ Handout #11Ram AugustNo ratings yet
- Obstetrical Nursing, Trinidad IgnacioDocument26 pagesObstetrical Nursing, Trinidad IgnaciojeshemaNo ratings yet
- Maternal and Child Health Nursing Exam 2Document9 pagesMaternal and Child Health Nursing Exam 2danielle ordoñezNo ratings yet
- Pediatric NursingDocument46 pagesPediatric Nursingjoy de castroNo ratings yet
- Gravidity and ParityDocument11 pagesGravidity and ParityShahad HakimuddinNo ratings yet
- Compre - Maternal Answer KeyDocument8 pagesCompre - Maternal Answer KeyrabsibalaNo ratings yet
- Nursingnotes - Info Maternal and Child NursingDocument54 pagesNursingnotes - Info Maternal and Child Nursinggrey26100% (1)
- CHN GapuzDocument23 pagesCHN GapuzMabes100% (1)
- Immediate Newborn Care-DOH 2010Document2 pagesImmediate Newborn Care-DOH 2010fegerilene100% (2)
- Practice Test NCLEX-Suddarts: Compiled by ZudotaDocument55 pagesPractice Test NCLEX-Suddarts: Compiled by ZudotaNicholas TagleNo ratings yet
- Nursing Care Management - 107: de La Salle Lipa College of NursingDocument3 pagesNursing Care Management - 107: de La Salle Lipa College of NursingThe Blue and Gold RvdNo ratings yet
- Immaculate Conception College-Albay Daraga, Albay NCM 102Document2 pagesImmaculate Conception College-Albay Daraga, Albay NCM 102Paul Jhon Vergara100% (3)
- My Reviewer On Funda Epaphras Joel T. MilitarDocument82 pagesMy Reviewer On Funda Epaphras Joel T. MilitarEpaphras Joel MilitarNo ratings yet
- Pediatric Nursing IDocument2 pagesPediatric Nursing IFilipino Nurses CentralNo ratings yet
- Obstetric Nursing Practice Test Part 1Document10 pagesObstetric Nursing Practice Test Part 1yanee06No ratings yet
- Reviewer For Fundamental of NursingDocument37 pagesReviewer For Fundamental of NursingtabiNo ratings yet
- Maternal and Child Health Nursing CompressDocument15 pagesMaternal and Child Health Nursing CompressRy Llanes100% (1)
- OB Definition of TermsDocument9 pagesOB Definition of TermsWarrenSandovalNo ratings yet
- 2013 Maternal and Child Health Nursing Reviewer CompleteDocument40 pages2013 Maternal and Child Health Nursing Reviewer CompleteHarley Justiniani Dela CruzNo ratings yet
- Delivery ComplicationDocument85 pagesDelivery Complicationirina100% (1)
- EINC Handout by Nicole Honrado BSN 2ADocument7 pagesEINC Handout by Nicole Honrado BSN 2A2A - Nicole Marrie HonradoNo ratings yet
- Prenatal Management (Part 5)Document36 pagesPrenatal Management (Part 5)Austine James Sabenicio PantiloNo ratings yet
- MATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideFrom EverandMATERNAL AND CHILD HEALTH NURSE: Passbooks Study GuideNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Gynecological Anatomy & PhysiologyDocument39 pagesGynecological Anatomy & Physiologynursereview100% (3)
- Bio NotesDocument180 pagesBio NotesjyotibhalaNo ratings yet
- 1a. Reproductive OrgansDocument60 pages1a. Reproductive OrgansJerrald Meyer L. BayaniNo ratings yet
- Femalereproductiveorgan 150117083020 Conversion Gate01Document57 pagesFemalereproductiveorgan 150117083020 Conversion Gate01SARABIA, ARVIN JR.No ratings yet
- Review of The Reproductive System 4Document44 pagesReview of The Reproductive System 4Shermaigne Ananayo BuyaNo ratings yet
- Ob Notes EditedDocument28 pagesOb Notes EditedJake IliganNo ratings yet
- Ra 9173Document12 pagesRa 9173Argee AlonsabeNo ratings yet
- Nursingbulletin Laws Affecting The Practice of NursingDocument4 pagesNursingbulletin Laws Affecting The Practice of Nursingseigelystic100% (43)
- HAAD Antidote ListDocument2 pagesHAAD Antidote Listashazainniz100% (5)
- EKG Self Study GuideDocument40 pagesEKG Self Study GuideArgee AlonsabeNo ratings yet
- Perioperative Nursing ConceptDocument21 pagesPerioperative Nursing ConceptArgee Alonsabe100% (9)
- Professional AdjustmentDocument22 pagesProfessional AdjustmentArgee Alonsabe100% (1)
- Pedia NotesDocument47 pagesPedia NotesArgee AlonsabeNo ratings yet
- Nursing JurisprudenceDocument1 pageNursing JurisprudenceArgee AlonsabeNo ratings yet
- NCM of Clients With Endocrine DisordersDocument24 pagesNCM of Clients With Endocrine DisordersArgee Alonsabe100% (1)
- L and MDocument26 pagesL and MArgee AlonsabeNo ratings yet
- An Assessment of The Necessity of Sexual Education For AdolescentsDocument4 pagesAn Assessment of The Necessity of Sexual Education For AdolescentsKIU PUBLICATION AND EXTENSIONNo ratings yet
- Ob RVG Panda ManilaDocument45 pagesOb RVG Panda ManilaMikaelle GasparNo ratings yet
- PLE Review OBGYN Chap 1 Overview of ObstetricsDocument2 pagesPLE Review OBGYN Chap 1 Overview of ObstetricsRemelou Garchitorena Alfelor100% (1)
- (IIEF) : Patient QuestionnaireDocument3 pages(IIEF) : Patient Questionnairerag manduaruwrNo ratings yet
- Female Precocious Puberty AlgorithmDocument1 pageFemale Precocious Puberty AlgorithmRICHI ADITYANo ratings yet
- Gender Identity Issues and Workplace Discrimination The Transgender ExperiDocument21 pagesGender Identity Issues and Workplace Discrimination The Transgender ExperijuaromerNo ratings yet
- Lec. 3 - Abnormal Uterine BleedingDocument14 pagesLec. 3 - Abnormal Uterine BleedingDr-Saja O. DmourNo ratings yet
- Rosenfield2015 PDFDocument27 pagesRosenfield2015 PDFdanilacezaraalinaNo ratings yet
- Worksheet. Menstrual Cycle.Document5 pagesWorksheet. Menstrual Cycle.Rigel Del CastilloNo ratings yet
- Female Foeticide in IndiaDocument2 pagesFemale Foeticide in IndiaPitamber RohtanNo ratings yet
- Pelvic Inflammatory DiseaseDocument71 pagesPelvic Inflammatory DiseaseGraceline Margaretha Marsintauly SianiparNo ratings yet
- Health Talk On Episiotomy CareDocument22 pagesHealth Talk On Episiotomy Carejyoti singh86% (7)
- Polyhydramnios and OligohyramniosDocument35 pagesPolyhydramnios and Oligohyramniosaymanway50% (2)
- CFP Febby HerayonoDocument7 pagesCFP Febby HerayonoFebby HerayonoNo ratings yet
- Fertility and Family Planning: 2011 Family Health Survey For 2011Document43 pagesFertility and Family Planning: 2011 Family Health Survey For 2011Misyel Avelino100% (3)
- Smyth Et Al-2013Document87 pagesSmyth Et Al-2013dshkfdjsfhkjNo ratings yet
- Instructional Module: Republic of The Philippines Nueva Vizcaya State University Bayombong, Nueva VizcayaDocument4 pagesInstructional Module: Republic of The Philippines Nueva Vizcaya State University Bayombong, Nueva VizcayaJayson VelascoNo ratings yet
- Anamnesis FormatDocument12 pagesAnamnesis FormatJeffrey Hardy100% (1)
- Puerperium:: Psychological DisordersDocument5 pagesPuerperium:: Psychological DisordersManisha ThakurNo ratings yet
- ASSE Project Final ExamDocument7 pagesASSE Project Final ExamMycz DoñaNo ratings yet
- Sex Outside MarriageDocument15 pagesSex Outside MarriageTimmons GwenNo ratings yet
- Postpartum CollapseDocument54 pagesPostpartum Collapsemedical chroniclesNo ratings yet
- Study Guide 6 - Transcultural Perspectives in ChildbearingDocument12 pagesStudy Guide 6 - Transcultural Perspectives in ChildbearingTim john louie RancudoNo ratings yet
- Bemonc: Basic Emergency Obstetric and Newborn CareDocument32 pagesBemonc: Basic Emergency Obstetric and Newborn CareIzhra MargateNo ratings yet
- MCN 80 114Document35 pagesMCN 80 114Jianne CaloNo ratings yet
- Dilation and CurettageDocument8 pagesDilation and CurettageIrish Eunice FelixNo ratings yet
- Moral Standpoints of Senior High School StudentsDocument14 pagesMoral Standpoints of Senior High School StudentsFaye OgaoNo ratings yet
- My Husband Became My Best GirlfriendDocument5 pagesMy Husband Became My Best GirlfriendRoshni Mahapatra71% (7)
- Ethiopia MOH - Obstetrics Protocol 2020Document223 pagesEthiopia MOH - Obstetrics Protocol 2020CHALIE MEQU93% (89)
- Antenatal Care ProcedureDocument18 pagesAntenatal Care ProcedureNeha SinghNo ratings yet