Professional Documents
Culture Documents
869 Full
869 Full
Uploaded by
Aris BayuCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5824)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Intravenous Iron in Heart Failure and Chronic Kidney DiseaseDocument9 pagesIntravenous Iron in Heart Failure and Chronic Kidney DiseaseAris BayuNo ratings yet
- Daftar Harga Jualan OmaDocument1 pageDaftar Harga Jualan OmaAris BayuNo ratings yet
- KT/V or Bicarbonate: What Is More Important For Growth in Pediatric Peritoneal Dialysis Patients?Document7 pagesKT/V or Bicarbonate: What Is More Important For Growth in Pediatric Peritoneal Dialysis Patients?Aris BayuNo ratings yet
- The Association of Parent - IndDocument15 pagesThe Association of Parent - IndAris BayuNo ratings yet
- Association of Screen Time With Parent - Reported Cognitive Delay in Preschool Children of Kerala, IndiaDocument8 pagesAssociation of Screen Time With Parent - Reported Cognitive Delay in Preschool Children of Kerala, IndiaAris BayuNo ratings yet
- Ijph 66 630700Document7 pagesIjph 66 630700Aris BayuNo ratings yet
- Stepwise Approach in Longterm Management of Asthma in ChildrenDocument41 pagesStepwise Approach in Longterm Management of Asthma in ChildrenAris BayuNo ratings yet
- 10 1001@jamapediatrics 2018 5056Document7 pages10 1001@jamapediatrics 2018 5056Aris BayuNo ratings yet
- Height-For-Age BOYS: 2 To 5 Years (Z-Scores)Document3 pagesHeight-For-Age BOYS: 2 To 5 Years (Z-Scores)Aris BayuNo ratings yet
- MainDocument10 pagesMainAris BayuNo ratings yet
- Original Article: Virendra K. Pal, Ajai Agrawal, Suwarna Suman, V. B. PratapDocument4 pagesOriginal Article: Virendra K. Pal, Ajai Agrawal, Suwarna Suman, V. B. PratapAris BayuNo ratings yet
- 49 - Modul Perdarahan Periventrikuler IntraventikulerPada Neonatus-27Document15 pages49 - Modul Perdarahan Periventrikuler IntraventikulerPada Neonatus-27Aris BayuNo ratings yet
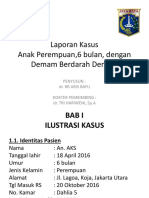
- Laporan Kasus DBDDocument33 pagesLaporan Kasus DBDAris BayuNo ratings yet
- Laser in Situ Keratomileusis For Astigmatism 0.75 Diopter Combined With Low Myopia: A Retrospective Data AnalysisDocument9 pagesLaser in Situ Keratomileusis For Astigmatism 0.75 Diopter Combined With Low Myopia: A Retrospective Data AnalysisAris BayuNo ratings yet
869 Full
869 Full
Uploaded by
Aris BayuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
869 Full
869 Full
Uploaded by
Aris BayuCopyright:
Available Formats
Posterior Reversible Encephalopathy Syndrome On the MR images, lesions may be observed in detail.
They are
hypointense on T1 and hyperintense on T2 images, with greater sensitivity
To the Editor:
of the fluid-attenuated inversion recovery and of the apparent diffusion
We read with interest the article by Varaprasad, et al1 in which the authors coefficient map. They are typically bilateral and symmetrical and they fol-
studied 13 patients with systemic lupus erythematosus (SLE) and posteri- low the calcarine and paramedian occipital lobe structures. This allows a
or reversible encephalopathy syndrome (PRES) presenting clinical and differentiation from those observed in the obstructions of the posterior
magnetic resonance imaging (MRI) features. All patients were female, cerebral artery or in the top of the basilar artery, where the calcarine region
ranging in age from 14 to 37 years. The duration of SLE ranged from 1.5 is invariably compromised. Less frequently, they may be found in the cere-
to 36 months. Eleven patients had seizures, 10 had headaches, 7 had loss bral cortex, cerebellum, basal ganglia, and frontal lobe6,8. These latter atyp-
of consciousness and vomiting, 3 had transient vision loss, and each pre- ical characteristics and the report of some cases with permanent sequels
sented paraparesis and left hemiplegia. All patients showed both early allowed Alurralde, et al to question the use of the prefix “leuco” and the
stages of SLE and hypertension. Eight patients were receiving corticos- terms “posterior” and “reversible” in the PRES nomenclature9.
teroids and 4 were taking monthly cyclophosphamide. Our patients’ MRI presented PRES with diffuse bilateral gray and
In 2007, we described the first case of PRES associated with SLE and white matter involvement, especially in the posterior fossa. One patient’s
thrombotic thrombocytopenic purpura2. In that case, the neurologic symp- MRI also showed lesions in the cerebral cortex, cerebellum, basal ganglia,
toms, the characteristic MR images, and the prompt full response to treat- and frontal lobe. These lesions normalized after the treatment.
ment enabled the diagnosis (Figure 1). The 3 patients were treated with antihypertensive drugs. Two also
After that, we followed 2 other patients with PRES. Of the 3 total cases, received methylprednisolone intravenously (IV), 1 received meprednisone
1 had SLE, another presented with SLE and thrombotic thrombocytopenic 40 mg/day orally, 2 were treated with antiepileptic drugs, and 2 with
purpura, and the third with postinfection glomerulonephritis. Two were cyclophosphamide IV. Plasmapheresis was used with 1 patient. Similar to
women and all ages ranged from 15 to 31 years. The duration of SLE was Varaprasad’s series, the time for recovery from PRES was 10 days in 2
1 month and 108 months, respectively, and SLE was active in both patients patients and 1 day in the third patient.
(SLE Disease Activity Index of 28 and 12). Similar to Varaprasad’s series, Urgent and aggressive treatment of arterial hypertension, seizures, and
all our patients presented with headaches, hypertension, renal involvement, renal failure, in addition to dose decreases or suspension of treatment with
and seizures; 1 patient had loss of consciousness and hemiplegia. immunosuppressive agents, is the key to reversibility of PRES2.
Although some authors do not specify the duration of SLE in their PRES is a serious clinical multifactor radiologic manifestation and
reports, others describe the diagnosis of PRES in patients with SLE should be included in the differential diagnosis of all patients with connec-
between 1 and 20 years’ duration3,4,5. tive tissue disease who have seizures, severe arterial hypertension, and
Most patients showed active lupus, with nephritis being the most com- renal failure, or who are treated with immunosuppressive drugs.
mon accompaniment. Renal failure and severe hypertension are known risk MRI is the chosen technique for a fast differential diagnosis, as it
factors for the development of PRES6. The occurrence of PRES in nor- allows prompt treatment and therefore helps decrease the risk of permanent
motensives and treatment-naive patients may explain that the endothelial sequelae.
dysfunction due to disease activity plays an important pathogenetic role7.
ACKNOWLEDGMENT
The authors are grateful to Raúl A. Galoppe, PhD (Montclair State
University, Montclair, NJ, USA) for his help in translating this report.
ALBERTO ORTIZ, MD; SUSANA ROVERANO, MD; SERGIO PAIRA,
MD, Rheumatology Section, Hospital J.M. Cullen, Santa Fe, Argentina.
Address correspondence to Dr. A. Ortiz, Rheumatology Section,
Department of Internal Medicine, Hospital J.M. Cullen, Crespo
2752-(3000), Santa Fe, Argentina. E-mail: albertoortiz_4@hotmail.com
REFERENCES
1. Varaprasad IR, Agrawal S, Prabu VNN, Rajasekhar L, Kanikannan
MA, Narsimulu G. Posterior reversible encephalopathy syndrome
in systemic lupus erythematosus. J Rheumatol 2011;38:1607-11.
2. Cassano G, Zunino A, Gongora V, Roverano S, Paira S. Reversible
posterior leukoencephalopathy in systemic lupus erythematosus
with thrombotic thrombocytopenic purpura. J Clin Rheum
2007;13:55-7.
3. Shin KC, Choi HJ, Bae YD, Lee JC, Lee EB, Song YW. Reversible
posterior leukoencephalopathy syndrome in systemic lupus
erythematosus with thrombocytopenia treated with cyclosporine.
J Clin Rheumatol 2005;11:164-6.
4. Thaipisuttikul I, Phanthumchinda K. Recurrent reversible posterior
leukoencephalopathy in a patient with systemic lupus
erythematosus. J Neurol 2005;252:230-1.
5. Primavera A, Audenino D, Mavilio N, Cocito L. Reversible
posterior leucoencephalopathy syndrome in systemic lupus and
vasculitis. Ann Rheum Dis 2001;60:534-7.
6. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al.
Figure 1. Magnetic resonance image shows occipital bilateral hyperintense A reversible posterior leukoencephalopathy syndrome. N Engl J
images on T2 and fluid-attenuated inversion recovery sparing the calcarine Med 1996;334:494-500.
and paramedian occipital lobe structures. 7. Johnson SR, Harvey PJ, Floras JS, Iwanochko M, Ivanez D,
Personal non-commercial use only. The Journal of Rheumatology Copyright © 2012. All rights reserved.
Letter 869
Downloaded on September 28, 2023 from www.jrheum.org
Gladman DD, et al. Impaired brachial artery endothelium 9. Alurralde AM, di Egidio M, Saizar R, Consalvo D, Villa AM.
dependent flow mediated dilation in systemic lupus erythematosus: Reversible posterior leucoencephalopathy syndrome: A case report
preliminary observations. Lupus 2004;13:590-3. and review of its physiopathology based on neuroradiological
8. Garg RK. Posterior leukoencephalopathy syndrome. Postgrad Med findings [Spanish]. Rev Neurol 2004;38:541-4.
J 2001;77:24-8.
J Rheumatol 2012;39;4; doi:10.3899/jrheum.111192
Personal non-commercial use only. The Journal of Rheumatology Copyright © 2012. All rights reserved.
870 The Journal of Rheumatology 2012; 39:4
Downloaded on September 28, 2023 from www.jrheum.org
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5824)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Intravenous Iron in Heart Failure and Chronic Kidney DiseaseDocument9 pagesIntravenous Iron in Heart Failure and Chronic Kidney DiseaseAris BayuNo ratings yet
- Daftar Harga Jualan OmaDocument1 pageDaftar Harga Jualan OmaAris BayuNo ratings yet
- KT/V or Bicarbonate: What Is More Important For Growth in Pediatric Peritoneal Dialysis Patients?Document7 pagesKT/V or Bicarbonate: What Is More Important For Growth in Pediatric Peritoneal Dialysis Patients?Aris BayuNo ratings yet
- The Association of Parent - IndDocument15 pagesThe Association of Parent - IndAris BayuNo ratings yet
- Association of Screen Time With Parent - Reported Cognitive Delay in Preschool Children of Kerala, IndiaDocument8 pagesAssociation of Screen Time With Parent - Reported Cognitive Delay in Preschool Children of Kerala, IndiaAris BayuNo ratings yet
- Ijph 66 630700Document7 pagesIjph 66 630700Aris BayuNo ratings yet
- Stepwise Approach in Longterm Management of Asthma in ChildrenDocument41 pagesStepwise Approach in Longterm Management of Asthma in ChildrenAris BayuNo ratings yet
- 10 1001@jamapediatrics 2018 5056Document7 pages10 1001@jamapediatrics 2018 5056Aris BayuNo ratings yet
- Height-For-Age BOYS: 2 To 5 Years (Z-Scores)Document3 pagesHeight-For-Age BOYS: 2 To 5 Years (Z-Scores)Aris BayuNo ratings yet
- MainDocument10 pagesMainAris BayuNo ratings yet
- Original Article: Virendra K. Pal, Ajai Agrawal, Suwarna Suman, V. B. PratapDocument4 pagesOriginal Article: Virendra K. Pal, Ajai Agrawal, Suwarna Suman, V. B. PratapAris BayuNo ratings yet
- 49 - Modul Perdarahan Periventrikuler IntraventikulerPada Neonatus-27Document15 pages49 - Modul Perdarahan Periventrikuler IntraventikulerPada Neonatus-27Aris BayuNo ratings yet
- Laporan Kasus DBDDocument33 pagesLaporan Kasus DBDAris BayuNo ratings yet
- Laser in Situ Keratomileusis For Astigmatism 0.75 Diopter Combined With Low Myopia: A Retrospective Data AnalysisDocument9 pagesLaser in Situ Keratomileusis For Astigmatism 0.75 Diopter Combined With Low Myopia: A Retrospective Data AnalysisAris BayuNo ratings yet