Professional Documents
Culture Documents
Clinical Practice Guidelines Cellulitis and Other Bacterial Skin Infections
Clinical Practice Guidelines Cellulitis and Other Bacterial Skin Infections
Uploaded by
Marco SurgeonCopyright:
Available Formats
You might also like
- Drugs Generally Used On Veterinary Clinics in India PDFDocument17 pagesDrugs Generally Used On Veterinary Clinics in India PDFSwarup charan75% (4)
- Periorbital and Orbital CellulitisDocument6 pagesPeriorbital and Orbital Cellulitispi ngilNo ratings yet
- Bone and Joint Infections BNHFT 2010 PDFDocument3 pagesBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriNo ratings yet
- DRUGSTUDYDocument8 pagesDRUGSTUDYWinnie Salazar AriolaNo ratings yet
- Erysipelas and Cellulitis - MSF Medical GuidelinesDocument5 pagesErysipelas and Cellulitis - MSF Medical GuidelinesHamza RiazNo ratings yet
- 5 Cefuroxime Drug StudyDocument4 pages5 Cefuroxime Drug Studyshadow gonzalezNo ratings yet
- Guide Paed Bone JNTDocument11 pagesGuide Paed Bone JNTDorica GiurcaNo ratings yet
- CefaclorDocument3 pagesCefaclorAyah PaasaNo ratings yet
- Protocolos ATB MichiganDocument7 pagesProtocolos ATB MichiganDaniel Alejandro CastrilloNo ratings yet
- Generic NameDocument4 pagesGeneric NamePharmacist Amy CharlieNo ratings yet
- Antibiotic Guidelines For PediatricsDocument33 pagesAntibiotic Guidelines For PediatricsVarshini Tamil SelvanNo ratings yet
- Hook Worm InfectionsDocument10 pagesHook Worm InfectionsMaria Pina Barbado PonceNo ratings yet
- T21H0058SmPCV1Document22 pagesT21H0058SmPCV1tsegayed975No ratings yet
- Food Poisoning DefinitionDocument10 pagesFood Poisoning DefinitionMaria Pina Barbado PonceNo ratings yet
- Drug StudyDocument10 pagesDrug StudybaniniycsebNo ratings yet
- MeropenemDocument13 pagesMeropenemkhalil.kadasiNo ratings yet
- Navora OB WARD DRUG STUDYDocument7 pagesNavora OB WARD DRUG STUDYNavora, Bryle TrixthaneNo ratings yet
- Antibiotic Treatment Guidelines For Urinary Tract Infections in Children (60 Days Through 17 Years)Document3 pagesAntibiotic Treatment Guidelines For Urinary Tract Infections in Children (60 Days Through 17 Years)Zahid AbbasNo ratings yet
- Drug Study AZITHROMYCINDocument2 pagesDrug Study AZITHROMYCINDannah BulliandayNo ratings yet
- Cephalexin Drug Study RNpedia ComDocument2 pagesCephalexin Drug Study RNpedia ComKatyana Cesar100% (1)
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- AntibioticsDocument31 pagesAntibioticsAkash SrivastavaNo ratings yet
- Drugs PocDocument2 pagesDrugs PocJean SandoyNo ratings yet
- Chemo Related Toxicities CopybbbDocument25 pagesChemo Related Toxicities Copybbbhera.mahnur2102No ratings yet
- Drug Study: Adult: ChildDocument4 pagesDrug Study: Adult: ChildKristian Karl Bautista Kiw-isNo ratings yet
- Drug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityDocument2 pagesDrug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityJoshua DavantesNo ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- CeftriaxoneDocument3 pagesCeftriaxoneCiera YoungNo ratings yet
- Drugs Acting On Immune SystemDocument6 pagesDrugs Acting On Immune SystemSORENI SORENINo ratings yet
- CellulitisDocument3 pagesCellulitisshedNo ratings yet
- AntigoutDocument22 pagesAntigoutmsd627690No ratings yet
- Streptococcus Pneumoniae Haemophilus Influenzae: Click HereDocument3 pagesStreptococcus Pneumoniae Haemophilus Influenzae: Click HereSiti Hidayatul FitriNo ratings yet
- Cellulitis ConsensusDocument7 pagesCellulitis Consensusneela kantaNo ratings yet
- Ce Fur OximeDocument2 pagesCe Fur OximeDan Dan ManaoisNo ratings yet
- CaftriaxonedrugstudyDocument1 pageCaftriaxonedrugstudyAdrianne Khyle OngNo ratings yet
- ANTIFUNGALSDocument11 pagesANTIFUNGALSCalvoh Asap BiketiNo ratings yet
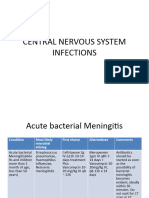
- Central Nervous System InfectionsDocument9 pagesCentral Nervous System InfectionsSaddamNo ratings yet
- DIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)Document31 pagesDIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)NingrumSindayaniNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- Colistin/ Colistimethate SodiumDocument2 pagesColistin/ Colistimethate SodiumnonameNo ratings yet
- Drug Study - LoperamideDocument3 pagesDrug Study - LoperamideCarissa Mae Tapec EstradaNo ratings yet
- Medication Fact Sheets: 3rd Edition ContributorsDocument50 pagesMedication Fact Sheets: 3rd Edition ContributorsIndumathi ThangathirupathiNo ratings yet
- Tetanus: Medical Faculty Tadulako University 2019Document21 pagesTetanus: Medical Faculty Tadulako University 2019Yayang MinansalNo ratings yet
- Ceftriaxone PDFDocument3 pagesCeftriaxone PDFLauren JalandoniNo ratings yet
- Chemo Related ToxicitiesDocument26 pagesChemo Related Toxicitieshera.mahnur2102No ratings yet
- AmikinDocument2 pagesAmikinLIEZEL GRACE VELAYONo ratings yet
- Penicillinase-Resistant AntibioticsDocument3 pagesPenicillinase-Resistant AntibioticsPrince Mark BadilloNo ratings yet
- COVID Clinical Management 14012022Document1 pageCOVID Clinical Management 14012022Naina DesaiNo ratings yet
- COVID Management 17th January 2022 DR Suvrankar Datta AIIMSDocument1 pageCOVID Management 17th January 2022 DR Suvrankar Datta AIIMSWhiteNo ratings yet
- Amoxicillin (Amoxycillin) : PresentationDocument4 pagesAmoxicillin (Amoxycillin) : PresentationRavikiran SuryanarayanamurthyNo ratings yet
- IMG EmpAposterDocument1 pageIMG EmpAposterChiu LeoNo ratings yet
- NICU Drugs GuideDocument49 pagesNICU Drugs GuideArhanNo ratings yet
- Targocid Article 30 Referral Annex III - enDocument32 pagesTargocid Article 30 Referral Annex III - enDR JAMAL WARISNo ratings yet
- Drug Study - CefuroximeDocument2 pagesDrug Study - CefuroximeErika Jane EsperanzaNo ratings yet
- Antibiotic Guidelines For BONE AND JOINT INFECTIONSDocument3 pagesAntibiotic Guidelines For BONE AND JOINT INFECTIONSKhurram NadeemNo ratings yet
- Guidelines For The Management of Psoriasis in Primary Care v12Document6 pagesGuidelines For The Management of Psoriasis in Primary Care v12ShamlazaghNo ratings yet
- Introduction To Antimicrobial/Anti-Infective DrugsDocument17 pagesIntroduction To Antimicrobial/Anti-Infective DrugsMaria Pina Barbado PonceNo ratings yet
- Drugs Acting On The GitDocument29 pagesDrugs Acting On The GitIsheanesu MugwisiNo ratings yet
- Toxic Megacolon, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandToxic Megacolon, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
Clinical Practice Guidelines Cellulitis and Other Bacterial Skin Infections
Clinical Practice Guidelines Cellulitis and Other Bacterial Skin Infections
Uploaded by
Marco SurgeonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Practice Guidelines Cellulitis and Other Bacterial Skin Infections
Clinical Practice Guidelines Cellulitis and Other Bacterial Skin Infections
Uploaded by
Marco SurgeonCopyright:
Available Formats
Stay informed with the latest updates on coronavirus (COVID-
19). Find out more >>
Clinical Practice Guidelines
Cellulitis and other bacterial skin
infections
See also
Antibiotics
Periorbital and orbital cellulitis
Sepsis
Key Points
1. Cellulitis is a spreading infection of the skin extending to
involve the subcutaneous tissues. Many conditions present
similarly to cellulitis — always consider differential
diagnoses
2. The typical presenting features of all skin infections include
soft tissue redness, warmth and swelling, but other features
are variable
3. Allergic reactions and contact dermatitis are frequently
misdiagnosed as cellulitis. If there is itch and no
tenderness, cellulitis is unlikely
Background
Cellulitis
The most common causes are Group A streptococcus
(GAS) and Staphylococcus aureus. Predisposing factors
include skin abrasions, lacerations, burns, eczematous
skin, chickenpox, etc. although the portal of entry of
organisms is often not seen
Impetigo (commonly called "school sores")
Highly contagious infection of the epidermis, particularly
common in young children Causative organisms are GAS
and S. aureus
May be associated with scabies
Staphylococcal scalded skin syndrome (SSSS)
Blistering skin disorder induced by the exfoliative
(epidermolytic) toxins of S. aureus. Primarily affects
neonates and young children
Necrotising fasciitis
Rapidly progressive soft tissue infection characterised by
necrosis of subcutaneous tissue
Causative organisms include GAS, S. aureus, anaerobes
and is often polymicrobial
It causes severe illness with a high mortality rate (~25%)
Recent infection with varicella is a risk factor
Cellulitis associated with water borne organisms
Aeromonas species (fresh or brackish water, and mud)
Mycobacterium marinum (fish tanks)
Vibrio species (salt or brackish water)
S. aureus, including MRSA
GAS (coral cuts)
Infected animal/human bites
Caused by different organisms and often require different
treatment
Other bites are discussed elsewhere, see Snakebite,
Spider bite – big black spider, Spider bite – red-back spider
There are many other forms of skin infection that are not covered
in this guideline
Assessment
Typical presentation of all skin infections
Soft tissue redness
Warmth and swelling
Pain/tenderness
Mild Cellulitis
Features above
No systemic features
No significant co-morbidities
Moderate Cellulitis
Features above with moderate swelling and tenderness
Systemic features (eg fever, tachycardia)
Severe Cellulitis
Features above with severe swelling or tenderness
Large body surface area involved (eg larger than the
patient’s handprint)
Marked systemic features (eg fever or hypothermia,
tachycardia, tachypnoea, altered conscious state, unwell
appearance, hypotension — this is a late sign). See Sepsis
Features suggestive of necrotising fasciitis include:
severe pain out of keeping with apparent severity of
infection
rapid progression
marked systemic features (eg high fever with rigors,
tachycardia, tachypnoea, hypotension, confusion,
vomiting). See Sepsis
Red flags
Abscess or suppuration
Animal or human bite
Deep structure involvement
Foreign body
Immunosuppression
Lymphangitis
MRSA infection
Multiple comorbidities
Periorbital/facial/hand involvement
Varicella associated infection
Differential Diagnosis
Large local reactions to insect bites are a common mimic of
cellulitis. Features include:
a punctum at the site
itch as a prominent feature
redness and induration, but rarely pain
Management
Investigations
Swab for Gram stain (charcoal / gel / bacterial transport
swab and slide) and culture if discharge present
Blood culture is not useful in mild/moderate cellulitis
Consider imaging (eg ultrasound) if abscess, deep infection
or foreign body suspected
Treatment
Manage sepsis if features present
Manage source if identifiable — ie remove foreign body,
drain abscess
For ongoing management refer to flowchart below
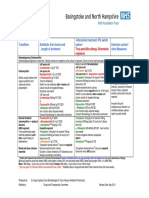
Summary of antibiotic therapy
Antimicrobial recommendations may vary according to local
antimicrobial susceptibility patterns; please refer to local guidelines
Cellulitis frequently looks worse after 24 hours of treatment;
consider waiting 48 hours to change therapies
Young, unvaccinated children are at risk of Haemophilus
influenzae type B (Hib)
Diagnosis Antibiotic Total Comments
duration
Impetigo Topical Mupirocin 2% ointment 5 days
or cream to crusted areas
tds OR
Cefalexin 33 mg/kg (max 500
mg) oral bd if widespread or
large lesions
Mild cellulitis Cefalexin 33 mg/kg (max 500 5 days
mg) oral tds
Moderate A trial of high-dose oral 5–10 days If oral
cellulitis antibiotics with close review antibiotics not
may be considered: tolerated or
Cefalexin 33 mg/kg (max 1 g) no
oral tds improvement
after 48
Consider Ambulatory/Hospital-
hours,
in-the-Home (HITH) if
manage as
available:
per severe
Ceftriaxone 50 mg/kg (max 2g)
cellulitis
IV daily
When
Cefazolin 50 mg/kg (max 2g)
improving,
IV bd
switch to oral
antibiotics as
per mild
cellulitis
Severe Flucloxacillin 50 mg/kg (max 2 5–10 days Consider
cellulitis g) IV 6H early
or (if rapidly progressive consider discharge to
Staphylococcal adding Clindamycin 10 mg/kg HITH once
scalded skin (max 600 mg) IV 6H) stable. When
syndrome improving,
switch to oral
antibiotics as
per mild
cellulitis
Necrotising Vancomycin and Meropenem Urgent
Fasciitis 20 mg/kg IV (max 1 g) 8H referral to
AND surgical team
Clindamycin 10 mg/kg (max for
600 mg) IV 6H debridement
Seek
specialist
advice for
antibiotics
Consider IVIg
Mammalian Often do not need prophylactic 5 days
bites antibiotics. When indicated*:
(uninfected / Amoxicillin/Clavulanate
prophylactic) 80 mg/mL amoxicillin oral
liquid (7:1)
22.5 mg/kg (max 875 mg) oral
bd
Animal/human Amoxicillin/Clavulanate 5 days Seek
bites 80 mg/mL amoxicillin oral (extend if specialist
(established liquid (7:1) severe, advice
infection) 22.5 mg/kg (max 875 mg) oral penetrating,
bd involving
If unable to tolerate oral deep
antibiotics: tissues)
25 mg/kg (max 1g) IV 6–8H
Waterborne Cefalexin 33 mg/kg (max 1 g) 5–10 days Clean and
skin infections oral tds and Ciprofloxacin 10 debride
– seawater or mg/kg (max 500 mg) oral bd wound as
fresh water OR needed
Trimethoprim/sulfamethoxazole Prophylactic
8/40 mg/kg (max 320/1600 mg) antibiotics are
oral bd not
recommended
*Indications for prophylactic antibiotics in a animal/human bite
Presentation delayed by >8 hours
Puncture wound unable to be adequately debrided
Bite on hands, feet, face
Involves deep tissues (eg bones, joints, tendons)
Involves an open fracture
Immunocompromised patient
Cat bites
Suggested antibiotic therapy where MRSA is suspected
Antimicrobial recommendations may vary according to local
antimicrobial susceptibility patterns; please refer to local guidelines
Diagnosis Antibiotic Total Comments
duration
Mild cellulitis Trimethoprim/sulfamethoxazole 5 days
8/40 mg/kg (max 320/1600 mg)
oral bd
OR
Clindamycin 10 mg/kg (max
450 mg) oral qid
Moderate A trial of oral antibiotics with When
cellulitis close review may be improving,
considered switch to
OR oral
Vancomycin IV antibiotics
as per mild
cellulitis
Severe Vancomycin IV When
cellulitis OR improving,
or Clindamycin 10 mg/kg (max switch to
Staphylococcal 600 mg) IV 6H oral
scalded skin antibiotics
syndrome as per
mild
cellulitis
Risk factors for MRSA infection
Residence in an area with high prevalence of MRSA, eg
Northern Territory, remote communities in northern
Queensland
Previous colonisation or infection with MRSA (particularly
recent)
Aboriginal and Torres Strait Islander or Pacific Islander child
Consider consultation with local
paediatric team when
No improvement or deterioration after 24–48 hours of
therapy
Deep abscess or necrotising fasciitis suspected — consider
surgical opinion
Consider transfer when
Child requires care above the level of comfort of local hospital
For emergency advice and paediatric or neonatal ICU transfers,
see Retrieval Services
Consider discharge when
Able to tolerate oral antibiotics
Parent Information
Cellulitis
Impetigo
Staphylococcal infections
Bleach Baths
Last Updated March 2020
! Reference List
Like 3 Tweet
" # $ %
Support us
The Royal Children's Hospital Melbourne
Telephone +61 3 9345 5522
50 Flemington Road Parkville Victoria 3052 Australia
Site Map | Copyright | Terms and Conditions
Staff Portal
You might also like
- Drugs Generally Used On Veterinary Clinics in India PDFDocument17 pagesDrugs Generally Used On Veterinary Clinics in India PDFSwarup charan75% (4)
- Periorbital and Orbital CellulitisDocument6 pagesPeriorbital and Orbital Cellulitispi ngilNo ratings yet
- Bone and Joint Infections BNHFT 2010 PDFDocument3 pagesBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriNo ratings yet
- DRUGSTUDYDocument8 pagesDRUGSTUDYWinnie Salazar AriolaNo ratings yet
- Erysipelas and Cellulitis - MSF Medical GuidelinesDocument5 pagesErysipelas and Cellulitis - MSF Medical GuidelinesHamza RiazNo ratings yet
- 5 Cefuroxime Drug StudyDocument4 pages5 Cefuroxime Drug Studyshadow gonzalezNo ratings yet
- Guide Paed Bone JNTDocument11 pagesGuide Paed Bone JNTDorica GiurcaNo ratings yet
- CefaclorDocument3 pagesCefaclorAyah PaasaNo ratings yet
- Protocolos ATB MichiganDocument7 pagesProtocolos ATB MichiganDaniel Alejandro CastrilloNo ratings yet
- Generic NameDocument4 pagesGeneric NamePharmacist Amy CharlieNo ratings yet
- Antibiotic Guidelines For PediatricsDocument33 pagesAntibiotic Guidelines For PediatricsVarshini Tamil SelvanNo ratings yet
- Hook Worm InfectionsDocument10 pagesHook Worm InfectionsMaria Pina Barbado PonceNo ratings yet
- T21H0058SmPCV1Document22 pagesT21H0058SmPCV1tsegayed975No ratings yet
- Food Poisoning DefinitionDocument10 pagesFood Poisoning DefinitionMaria Pina Barbado PonceNo ratings yet
- Drug StudyDocument10 pagesDrug StudybaniniycsebNo ratings yet
- MeropenemDocument13 pagesMeropenemkhalil.kadasiNo ratings yet
- Navora OB WARD DRUG STUDYDocument7 pagesNavora OB WARD DRUG STUDYNavora, Bryle TrixthaneNo ratings yet
- Antibiotic Treatment Guidelines For Urinary Tract Infections in Children (60 Days Through 17 Years)Document3 pagesAntibiotic Treatment Guidelines For Urinary Tract Infections in Children (60 Days Through 17 Years)Zahid AbbasNo ratings yet
- Drug Study AZITHROMYCINDocument2 pagesDrug Study AZITHROMYCINDannah BulliandayNo ratings yet
- Cephalexin Drug Study RNpedia ComDocument2 pagesCephalexin Drug Study RNpedia ComKatyana Cesar100% (1)
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- AntibioticsDocument31 pagesAntibioticsAkash SrivastavaNo ratings yet
- Drugs PocDocument2 pagesDrugs PocJean SandoyNo ratings yet
- Chemo Related Toxicities CopybbbDocument25 pagesChemo Related Toxicities Copybbbhera.mahnur2102No ratings yet
- Drug Study: Adult: ChildDocument4 pagesDrug Study: Adult: ChildKristian Karl Bautista Kiw-isNo ratings yet
- Drug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityDocument2 pagesDrug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityJoshua DavantesNo ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- CeftriaxoneDocument3 pagesCeftriaxoneCiera YoungNo ratings yet
- Drugs Acting On Immune SystemDocument6 pagesDrugs Acting On Immune SystemSORENI SORENINo ratings yet
- CellulitisDocument3 pagesCellulitisshedNo ratings yet
- AntigoutDocument22 pagesAntigoutmsd627690No ratings yet
- Streptococcus Pneumoniae Haemophilus Influenzae: Click HereDocument3 pagesStreptococcus Pneumoniae Haemophilus Influenzae: Click HereSiti Hidayatul FitriNo ratings yet
- Cellulitis ConsensusDocument7 pagesCellulitis Consensusneela kantaNo ratings yet
- Ce Fur OximeDocument2 pagesCe Fur OximeDan Dan ManaoisNo ratings yet
- CaftriaxonedrugstudyDocument1 pageCaftriaxonedrugstudyAdrianne Khyle OngNo ratings yet
- ANTIFUNGALSDocument11 pagesANTIFUNGALSCalvoh Asap BiketiNo ratings yet
- Central Nervous System InfectionsDocument9 pagesCentral Nervous System InfectionsSaddamNo ratings yet
- DIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)Document31 pagesDIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)NingrumSindayaniNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- Colistin/ Colistimethate SodiumDocument2 pagesColistin/ Colistimethate SodiumnonameNo ratings yet
- Drug Study - LoperamideDocument3 pagesDrug Study - LoperamideCarissa Mae Tapec EstradaNo ratings yet
- Medication Fact Sheets: 3rd Edition ContributorsDocument50 pagesMedication Fact Sheets: 3rd Edition ContributorsIndumathi ThangathirupathiNo ratings yet
- Tetanus: Medical Faculty Tadulako University 2019Document21 pagesTetanus: Medical Faculty Tadulako University 2019Yayang MinansalNo ratings yet
- Ceftriaxone PDFDocument3 pagesCeftriaxone PDFLauren JalandoniNo ratings yet
- Chemo Related ToxicitiesDocument26 pagesChemo Related Toxicitieshera.mahnur2102No ratings yet
- AmikinDocument2 pagesAmikinLIEZEL GRACE VELAYONo ratings yet
- Penicillinase-Resistant AntibioticsDocument3 pagesPenicillinase-Resistant AntibioticsPrince Mark BadilloNo ratings yet
- COVID Clinical Management 14012022Document1 pageCOVID Clinical Management 14012022Naina DesaiNo ratings yet
- COVID Management 17th January 2022 DR Suvrankar Datta AIIMSDocument1 pageCOVID Management 17th January 2022 DR Suvrankar Datta AIIMSWhiteNo ratings yet
- Amoxicillin (Amoxycillin) : PresentationDocument4 pagesAmoxicillin (Amoxycillin) : PresentationRavikiran SuryanarayanamurthyNo ratings yet
- IMG EmpAposterDocument1 pageIMG EmpAposterChiu LeoNo ratings yet
- NICU Drugs GuideDocument49 pagesNICU Drugs GuideArhanNo ratings yet
- Targocid Article 30 Referral Annex III - enDocument32 pagesTargocid Article 30 Referral Annex III - enDR JAMAL WARISNo ratings yet
- Drug Study - CefuroximeDocument2 pagesDrug Study - CefuroximeErika Jane EsperanzaNo ratings yet
- Antibiotic Guidelines For BONE AND JOINT INFECTIONSDocument3 pagesAntibiotic Guidelines For BONE AND JOINT INFECTIONSKhurram NadeemNo ratings yet
- Guidelines For The Management of Psoriasis in Primary Care v12Document6 pagesGuidelines For The Management of Psoriasis in Primary Care v12ShamlazaghNo ratings yet
- Introduction To Antimicrobial/Anti-Infective DrugsDocument17 pagesIntroduction To Antimicrobial/Anti-Infective DrugsMaria Pina Barbado PonceNo ratings yet
- Drugs Acting On The GitDocument29 pagesDrugs Acting On The GitIsheanesu MugwisiNo ratings yet
- Toxic Megacolon, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandToxic Megacolon, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)