Professional Documents
Culture Documents
A Magnetic Resonance Approach To Metabolic Disorders in Childhood
A Magnetic Resonance Approach To Metabolic Disorders in Childhood
Uploaded by
Ana TelloOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Magnetic Resonance Approach To Metabolic Disorders in Childhood
A Magnetic Resonance Approach To Metabolic Disorders in Childhood
Uploaded by
Ana TelloCopyright:
Available Formats
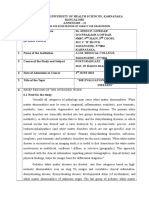
CONFERENCIA MAGISTRAL
A magnetic resonance approach
to metabolic disorders in childhood
A.J. Barkovich
A MAGNETIC RESONANCE APPROACH TO METABOLIC DISORDERS IN CHILDHOOD
Summary. Introduction. Inborn errors of metabolism are a difficult group of disorders to diagnose. Clinical signs and symptoms
overlap among the different diseases, biochemical tests are often nonspecific or unrevealing, and genetic analyses are time
consuming, expensive, and often not commercially available. Imaging can aid in diagnosing some disorders, but the imaging
findings of many disorders seem to overlap, particularly as more and more disorders are identified and described.
Development. Several groups have proposed an imaging approach based upon pattern recognition on magnetic resonance
imaging, supplemented by metabolic data from proton magnetic resonance spectroscopy and microstructural data, as assessed by
diffusion weighted imaging. Conclusion. When properly used, this pattern recognition approach in conjunction with the other
imaging tools can be very useful for separating the complex group of metabolic disorders into more manageable groups.
Indeed, sometimes this approach allows a specific diagnosis to be made. [REV NEUROL 2006; 43 (Supl 1): S5-16]
Key words. Brain diseases. Canavan disease. Diffusion magnetic resonance imaging. Drug toxicity. Inborn errors of metabolism.
Leukodystrophy. Magnetic resonance imaging. Magnetic resonance spectroscopy. Mitochondrial diseases.
INTRODUCTION PATTERN-BASED APPROACHES
Inborn errors of metabolism are a complicated and difficult TO METABOLIC DISEASE
group of disorders for most clinicians. Many such disorders The use of a systematic approach based on the pattern of brain
have been described and more are being discovered every year. involvement is useful in the analysis of neurometabolic disor-
Part of the confusion in dealing with these disorders stems from ders by imaging [1-3]. Such an approach has been described by
the fact that they are classified in many different ways; some van der Knaap and Valk; they initially created a database and
authors classify them by biochemical characteristics or the bio- subsequently developed a computer-assisted pattern recognition
chemical pathway that is affected, some by the cellular program to help in the imaging-guided identification of the dis-
organelle in which the affected protein or biochemical pathway orders [3,4]. The information entered into the database detailed
is located, others by clinical characteristics, and still others by precisely what parts of the brain where involved in the disease
the gene that is affected. Affected patients are not easy to segre- process and the specific type of involvement in each affected
gate by clinical criteria, as patients with metabolic disorders can area. In each cerebral lobe, they recorded the presence or
present at nearly any age, depending on the precise mutation to absence of involvement of the cerebral cortex, subcortical U
the affected gene, and their clinical signs and symptoms are fibers (arcuate fibers), deep white matter, and periventricular
almost invariably nonspecific in separating one disorder from white matter. Next, they assessed the presence or absence of
another. The imaging features of these disorders, too, can be involvement of multiple smaller structures: the internal capsule
particularly confusing if not approached methodically. The (anterior and posterior limb), external capsule, caudate nucleus,
imaging appearances of many disorders overlap and, often, vary putamen, globus pallidus, thalamus, corpus callosum (rostrum,
with the stage and the variant of the disease. The white matter is genu, body, and splenium), cerebellar cortex, cerebellar white
very commonly involved, sometimes primarily (a true leukody- matter, cerebellar dentate nucleus, cerebellar peduncles, hilus of
strophy) or sometimes by Wallerian degeneration resulting from the dentate nucleus, midbrain, pons, and medulla. Subsequently,
damage to cortical neurons. Involvement of the deep cerebral they analyzed which areas were predominantly involved (i.e.,
nuclei (the thalami and basal ganglia) may be the result of gray supratentorial or infratentorial, cerebral lobe, subcortical or deep
matter or white matter injury (about half of the basal nuclei is or periventricular white matter), degree of left-right symmetry,
composed of white matter). In the end stage, all disorders look extension of the lesions (small or large, isolated or confluent),
much the same, with atrophy of the cerebral cortex, reduced appearance (swelling, atrophy, cystic degeneration), signal
volume of gliotic or demyelinated white matter, and shrunken intensity, homogeneity, and demarcation from surrounding brain
basal ganglia. Therefore, it is important to image the patient (sharp, vague, or mixed). Finally, they listed extra characteris-
early in the course of the disease, when the pattern of injury tics: calcium, hemorrhage, contrast enhancement, enlargement
may be more characteristic. of subarachnoid spaces, presence of absence of cerebellar atro-
phy, and myelination (normal, delayed, absent). This data was
carefully recorded for nearly 1,500 patients with known diag-
Aceptado: 14.09.06.
noses; it was subsequently entered into their database.
Professor of Radiology, Neurology, Pediatrics, and Neurosurgery Neurora-
diology. UCSF. San Francisco, CA, Estados Unidos.
The availability of this database greatly facilitates their abili-
ty to establish diagnoses. When a new patient is encountered, the
Correspondencia: A. James Barkovich, M.D. Professor of Radiology, Neu-
rology, Pediatrics, and Neurosurgery Neuroradiology. Rm L-371. UCSF. magnetic resonance imaging (MRI) is analyzed, the MRI data is
505 Parnassus Ave. San Francisco, CA 94143-0628, USA. E-mail: jim. entered into their database, and it is compared with the data
barkovich@radiology.ucsf.edu already entered for known metabolic disorders. With some
© 2006, REVISTA DE NEUROLOGÍA patients, an exact (or nearly exact) match is achieved and the
REV NEUROL 2006; 43 (Supl 1): S5-S16 S5
A.J. BARKOVICH
diagnosis is established. If the match is not precise, the patient Table I. Metabolic disorders causing T2 or FLAIR hyperintensity of the
may be put into a group in which several diagnoses remain pos- corpus striatum.
sible based upon clinical and imaging criteria. By entering the
Leigh syndrome (includes pyruvate dehydrogenase deficiency,
patient into a smaller group of potential diagnoses, the amount respiratory complex I and complex II disorders)
of biochemical and genetic testing that must be performed is
substantially reduced, saving time and money. Sometimes, the Wilson disease
data is clearly different from all known syndromes, but matches Glutaric aciduria type I
one or more previously entered patients with unknown diag-
noses. This sort of observation is sometimes the first step in the Juvenile Huntington disease
identification of a new syndrome. Examples of disorders identi- Molybdenum co-factor deficiency
fied in this manner include hypomyelination with atrophy of the
basal ganglia and cerebellum [5], megalencephaly with leukoen- Propionic acidemia
cephalopathy and cysts [6], and cerebellar ataxia with cerebral
hypomyelination (vanishing white matter disease) [7].
A similarly systematic, but less sophisticated, approach to mass effect, upon adjacent structures [14]. Alternatively, many
the analysis of metabolic disorders, based upon the pattern of white matter disorders, such as adrenoleukodystrophy and fibri-
brain involvement on neuroimaging studies, is presented in this noid leukodystrophy (Alexander disease), start locally and
manuscript. This analysis will be primarily based upon the ear- advance over time to involve adjacent areas. Neither of these
ly appearance of disorders on MRI. Disorders with similar MRI appearances is seen in the white matter of gray matter disorders.
patterns can sometimes be differentiated on the basis of their White matter diseases can result in devastation of the involved
microstructural characteristics, which can be analyzed by diffu- areas, with necrosis and cavitation of the affected regions and
sion weighted imaging, or by in vivo biochemical analysis, subsequent ex vacuo dilation of the ventricles, whereas the
which can be grossly performed by proton magnetic resonance abnormal white matter in gray matter disorders appears less
spectroscopy. This approach does not replace a thorough bio- severely damaged. Finally, the clinical presentation of patients
chemical and genetic work-up, but it provides an excellent ini- with cortical gray matter disorders (seizures, dementia in early
tial screening process; proper analysis of the MR studies can stages) differs from that of deep gray matter disorders (chorea,
reduce the extent of the biochemical and genetic analyses. athetosis, dystonia) and both differ from the presentation of
white matter disorders (spasticity, hyperreflexia, ataxia). Although
First analysis: white matter versus gray matter such clinical criteria are sometimes misleading, they can some-
The first important determination to be made is whether the dis- times be helpful to get started on the right track.
ease involves primarily gray matter, primarily white matter, or
both gray and white matter. If the gray matter is primarily MRI in gray matter disorders
involved, both the cortex and deep nuclei should be scrutinized to As discussed above, gray matter disorders need to be further
determine whether involvement is primarily cortical, primarily analyzed in order to determine whether the disorder primarily
deep nuclear, or both. Sometimes, disorders that primarily affect involves the cerebral cortex or the deep gray matter nuclei. This
cortical gray matter will show cortical swelling with effaced sulci is most easily determined by examining the deep gray nuclei to
early in the course of the disease; more commonly, cortical thin- look for abnormal signal intensity on T2 weighted or FLAIR
ning is found, with prominent cortical sulci [8-11]. In later stages, images. Some disorders will manifest cortical edema in the
cortical thinning is the rule in all such disorders. The cerebral acute phase, appearing as T2 or FLAIR hyperintensity; if imag-
white matter will often have an abnormal appearance in these ing is not performed until later stages of the disease, cortical
patients, as Wallerian degeneration of axons causes diminished involvement will be manifested as sulcal enlargement, cortical
white matter volume and mild to moderate hyperintensity on thinning, and, sometimes, abnormal signal intensity.
FLAIR and T2 weighted images. This white matter appearance
can often be differentiated from that of primary white matter dis- Deep gray matter involvement
orders if the study is performed early in the course of the disease, When only deep gray matter is involved, it is important to iden-
as primarily affected white matter will often be edematous and, tify the specific structures that are affected and their signal
therefore, brighter and more voluminous (causing compressed, intensities. Involvement of the striatum (caudate and putamen)
smaller sulci) than the white matter that has undergone secondary is typically seen in mitochondrial disorders –primarily Leigh
(Wallerian) degeneration. In the acute phase, disorders primarily syndrome, mitochondrial encephalopathy with lactic acidosis and
affecting deep gray matter will typically show edema with FLAIR stroke-like symptoms (MELAS), and the glutaric acidurias–,
hyperintensity and prolonged T1 and T2 relaxation times on MRI propionic acidemia, Wilson disease, juvenile Huntington dis-
in the involved structures (the major exception to this is pan- ease, molybdenum cofactor deficiency, asphyxia, and hypo-
tothenate kinase associated neuropathy, in which iron accumula- glycemia (Table I). Associated white matter or cortical injury is
tion in the globus pallidus results in T2 hypointensity [12,13]) and frequently present in many of these disorders. If isolated globus
may show loss of volume with gliosis (resulting in slit-like con- pallidus involvement shows T2 prolongation, succinate semi-
figuration with T2 hyperintensity) in more chronic stages. aldehyde dehydrogenase deficiency, methylmalonic acidemia,
Disorders primarily affecting white matter cause marked sig- guanidinoacetate methyltransferase deficiency (a creatine syn-
nal abnormality before any volume loss is apparent. Some white thesis disorder), isovaleric acidemia, pyruvate dehydrogenase
matter disorders cause spongiform changes, result in intra- deficiency –due to mutation of the dihydrolipoamide acetyl-
myelinic edema, or have an inflammatory component in the ear- transferase (E2) component–, carbon monoxide poisoning, or
ly stages; these conditions cause edema, with accompanying the chronic phase of kernicterus should be considered (Table II)
S6 REV NEUROL 2006; 43 (Supl 1): S5-S16
CONFERENCIA MAGISTRAL
b
Figure 2. Citrullinemia: axial SE 2500/80 image shows abnormal hyperin-
tensity of the globus pallidus (small arrows) and the insular cortex (large
arrows).
Table II. Metabolic disorders causing T2 or FLAIR hyperintensity of the globus
pallidus.
Methylmalonic acidemia
Succinic semialdehyde dehydrogenase deficiency
Urea cycle disorders
Guanidinoacetate methyltransferase deficiency
Pyruvate dehydrogenase (E2) deficiency
Systemic lupus erythematosis
Hemolytic-uremic syndrome
Bilirubin toxicity
Figure 1. L-2-hydroxyglutaric aciduria: a) Axial SE 2500/30 image shows Isovaleric acidemia
bilateral hyperintensity (arrows) of the globus pallidus. Note that the peri-
ventricular white matter around the frontal horns and trigones is myelina- Carbon monoxide toxicity
ted, but the subcortical white matter is not; b) Coronal FSE 3000/100 ima-
ge better shows the hyperintensity of the subcortical white matter with Cyanide toxicity
sparing of the periventricular white matter.
[2,15]. If T2 or FLAIR hyperintensity of the globus pallidus is a neonate or young infant, consider acute hyperbilirubinemia
seen in association with subcortical white matter demyelination, of infancy [21-23], systemic lupus erythematosis [24,25], and
sparing of the periventricular white matter, and involvement hemolytic-uremic syndrome [26,27]; in the presence of edema
of the cerebellar dentate nuclei, L-2-hydroxyglutaric aciduria involving the external and extreme capsules and the claustrum,
(Fig. 1) [16] and Kearns-Sayre syndrome [17] should be consid- hemolytic-uremic syndrome is the most likely [27]. If the
ered. When the MRI shows atrophy of the dorsal brain stem and globus pallidus, the insula and perirolandic cortex are all hyper-
cerebellar dentate nuclei, one should consider dentatorubral and intense on T2 weighted or FLAIR images (Fig. 2), the diagnosis
pallidoluysian atrophy [18,19]. If T1 hyperintensity of the of a urea cycle disorder should be suggested [28,29]. If the
globus pallidus is seen associated with normal T2 signal, and involvement of the globus pallidus is manifested on MR as T2
the patient is not receiving hyperalimentation, consider chronic shortening or T2 shortening with central T2 prolongation (Fig.
hepatic disease [20]. If both T1 and T2 hyperintensity are seen in 3), the diagnosis of pantothenate kinase associated neuropathy
REV NEUROL 2006; 43 (Supl 1): S5-S16 S7
A.J. BARKOVICH
Figure 3. Pantothenate kinase associated neuropathy (formerly Hallervor-
den-Spatz disease): coronal FSE 3000/120 image shows marked hypo-
intensity of the globus pallidus with central hyperintensity; this is the so-
called ‘eye of the tiger’ appearance.
(formerly called Hallervorden-Spatz disease) can be made with
some confidence [12,13].
Figure 4. Pelizaeus-Merzbacher disease: axial SE 2500/80 image shows
minimal myelination restricted to the internal capsule; this is the pattern
Cerebral cortical involvement of an infant aged maybe 6 months, but this child is 3 years old! Pelizaeus-
Merzbacher disease results in a nearly complete lack of myelination, fol-
If the pattern of the imaging study indicates that the metabolic lowed by slow loss of myelin.
disorder is primarily one of cortical involvement (cortical thin-
ning with enlarged cortical sulci), consideration should be given
to such disorders as the neuronal ceroid lipofuscinoses [8,9,30],
the mucolipidoses [31], glycogen storage diseases [32], or GM1
gangliosidosis [2,15].
White matter disorders
White matter disorders can be divided into [1] those disorders in
which white matter never myelinates completely (hypomyelina-
tion) and those disorders in which myelin forms and is subse-
quently destroyed (demyelination). In the latter group, it is
important to determine whether myelin destruction is in the
periventricular, deep or subcortical white matter and what part of
the white matter (specific gyrus or lobe) is affected.
Hypomyelination
The pattern of a lack of myelination, or hypomyelination, is
seen in very few disorders. This group of disorders is known as
the hypomyelinating leukoencephalopathies; several of these
diseases are listed below. The hypomyelination pattern is most
commonly found in Pelizaeus-Merzbacher disease, a disorder
that affects the PLP1 gene that codes for the production of pro-
teolipid protein, one of the major structural proteins of myelin
[33,34]. The appearance of the brain in this disorder is that of a
normal, much more immature brain. For example, the MRI of
a 5-year-old child with this disorder might be mistaken for that
of a 5-month-old infant (Fig. 4). Similar appearances can be
seen in patients with Pelizaeus-Merzbacher-like disease (identi-
cal to PMD other than the causative genes [35,36]) leukodystro- Figure 5. Alexander disease: axial SE 2500/80 image shows abnormal
phies with trichothiodystrophy and photosensitivity [37,38], in hyperintensity of the frontal white matter including the subcortical arcu-
ate fibers. The heads of the caudate nuclei and the anterior putamina are
patients with Tay syndrome [39], in patients with the 18q-syn- also affected, along with the external and extreme capsules. This pattern
drome (deletion of a large portion of the long arm of chromo- in a macrocephalic patient is specific for Alexander disease.
S8 REV NEUROL 2006; 43 (Supl 1): S5-S16
CONFERENCIA MAGISTRAL
Figure 6. X-linked adrenoleukodystrophy: axial SE 2500/90 image shows Figure 7. X-linked adrenoleukodystrophy, very early stage. Brain involve-
marked hyperintensity of the callosal splenium and the parietal white ment of this disorder typically starts in the corpus callosum (arrows) as
matter, extending anteriorly into the internal and external capsules. Note seen in this patient.
the sparing of the subcortical arcuate fibers (arrows).
Table III. Metabolic disorders causing early involvement of subcortical white matter or the subcortical white matter. Table III lists some
white matter. disorders with early involvement of the subcortical white mat-
ter. If the subcortical white matter is involved, it should be care-
Alexander disease
fully analyzed to see if the subcortical U fibers (the arcuate
Kearns-Sayre syndrome fibers at the cortical-white matter junction) are affected. If
so, an attempt should be made to find out whether the patient
Megalencephalic leukoencephalopathy with subcortical cysts
has macrocephaly. Bilateral, symmetrical, frontal white matter
Galactosemia involvement involving the U fibers in a macrocephalic patient is
quite specific for Alexander disease, particularly if it extends
Mitochondrial disorders
posteriorly to involve the caudate heads and putamen (Fig. 5)
[46]. Bilateral, diffuse and symmetric, peripheral white matter
involvement without involvement of the deep or periventricular
some 18) [40,41], and in patients with Salla disease (a disorder white matter and without macrocephaly should raise suspicion
of sialic acid transport) [42,43]. If there is a question about the for organic acidurias or early Kearns-Sayre syndrome [2,17].
diagnosis of Pelizaeus-Merzbacher disease, proton MR spec- Diffuse white matter abnormality involving the subcortical U
troscopy may help, as it shows an elevated NAA peak [44]. fibers and associated with subcortical cysts in a macrocephalic
infant or young child suggests megalencephalic leukoen-
Loss of myelin (demyelination and dysmyelination) cephalopathy with subcortical cysts (MLC) [6,47,48].
When myelin develops but is subsequently damaged, it is not It is uncommon to see early myelin injury restricted to the
clear from imaging whether the myelin that was initially formed deep white matter without periventricular white matter involve-
was normal or abnormal. The former condition (destruction of ment. Table IV lists some disorders with early involvement of
normal myelin) is sometimes referred to as demyelination to the deep and periventricular white matter. If early involvement
differentiate if from breakdown of abnormal myelin, sometimes affects both periventricular and deep white matter, the thalami
called dysmyelination. By the use of diffusion tensor imaging, should be specifically analyzed. High attenuation on computer-
it may eventually be possible to differentiate these two entities ized tomography (CT) or short T1 (hyperintensity) or T2 (hypo-
[45], but the differentiation cannot currently be made. intensity) on MR bilaterally in the thalami strongly suggests
When such myelin breakdown and loss occurs, the white globoid cell leukodystrophy (Krabbe disease) or GM2 gan-
matter becomes more hypointense on T1 weighted images and gliosidosis [2,49-51]. If the thalami are normal, the brain stem
more hyperintense on T2 weighted images. In these situations, should be evaluated for involvement of specific tracts, particu-
the brain should be analyzed to determine whether the region larly the corticospinal tracts. If specific tracts (the corticospinal
primarily affected is the periventricular white matter, the deep tracts, in particular) are involved, peroxisomal disorders such
REV NEUROL 2006; 43 (Supl 1): S5-S16 S9
A.J. BARKOVICH
as X-linked adrenoleukodystrophy (Fig. 6) should be strongly Table IV. Metabolic disorders causing early involvement of periventricular
considered [52] –of note, the earliest radiologic sign of adreno- and deep white matter with sparing of subcortical white matter.
leukodystrophy is T2 hyperintensity in the central part of the cal-
X-linked adrenoleukodystrophy
losal splenium, not in the hemispheric white matter; therefore, so
if adrenoleukodystrophy is suspected clinically or if there is a Krabbe disease (globoid cell leukodystrophy)
family history, the corpus callosum should be intensely scruti-
Metachromatic leukodystrophy
nized (Fig. 7)–. If not, consideration should be given to meta-
chromatic leukodystrophy, cerebellar ataxia with cerebral hypo- GM2 gangliosidoses
myelination (vanishing white matter disease), phenylketonuria,
Childhood ataxia with CNS hypomyelination
Lowe syndrome (oculocerebrorenal syndrome), mucolipidosis (vanishing white matter disease)
type IV, merosin deficient congenital muscular dystrophies, and,
in the proper clinical setting, damage from radiation or chemo- Lowe syndrome (oculocerebrorenal syndrome)
therapy [2,15]. Among these, vanishing white matter disease Mucolipidosis type IV
should be considered if the clinical history is one of periodic
acute worsening after trauma or infection and if areas of cystic Merosin deficient congenital muscular dystrophy
degeneration (seen as hypointense on FLAIR images) develop in Damage from radiation or chemotherapy
the hemispheric white matter [7,53]. Lowe syndrome should be
suspected in many small cysts are seen in the affected white mat-
ter, particularly in the periventricular region [54,55]. If the dorsal
brain stem, internal capsules, cerebral peduncles, and cerebellar MCD is present in addition to a lack of myelination, the differ-
white matter are affected in a newborn, maple syrup urine dis- ential diagnosis includes the generalized peroxisomal disorders
ease should be considered; this diagnosis can be confirmed by [67,68], congenital cytomegalovirus disease [69-71], and con-
the finding of reduced diffusion on diffusion weighted images genital muscular dystrophies with cerebral involvement. Con-
and the presence of a broad peak from branched chain ketoacids genital muscular dystrophies will typically have pontine hypo-
at 0.9 ppm on proton MR spectroscopy –for details, see the later plasia and cerebellar dysplasia, as well [63] (Fig. 8)–. If no cor-
section of uses of MR spectroscopy [56,57]–. tical dysplasia is present, differential considerations include Al-
Few metabolic disorders affect the periventricular white mat- pers disease and Menkes disease, both of which cause consider-
ter while sparing the deep white matter. Observation of this pat- able cerebral cortical destruction [17]. If the bones are abnor-
tern should raise the possibility of prenatal or (in prematurely mal, the differential diagnoses include primarily storage dis-
born infants) neonatal or early postnatal white matter injury. eases, such as the mucopolysaccharidoses and lipid storage
Other causes of periventricular white matter injury include infec- disorders [72-75]. A description of the bony findings of these
tion (specifically ventriculitis), small periventricular hemorrhag- disorders is beyond the scope of this manuscript.
ic venous infarctions, and (rarely) demyelinating disease [58].
Some metabolic disorders have nonspecific white matter Cerebral nuclear involvement
patterns; this group includes disorders with involvement of If deep gray matter is involved, the first task is to determine pre-
both superficial and deep or periventricular white matter, cisely which nuclei are affected (Table I). If the thalami are
those with unilateral white matter involvement, those with dif- involved, differential considerations include Krabbe disease and
fuse white matter involvement, and those with bilateral asym- the GM1 and GM2 gangliosidoses; the thalami in these disor-
metric white matter involvement. Among the disorders includ- ders display high attenuation on CT and short T1 and T2 relax-
ed under this category are the collagen vascular diseases, such ations times (hyperintense on T1 weighted images and hypo-
as systemic lupus erythematosis (which tend to involve the intense on T2 weighted images) on MR. Krabbe disease is dis-
white matter bilaterally and asymmetrically [59,60]), congen- tinguished from the others by the presence of abnormal T2
ital muscular dystrophies with neurologic impairment [61-64], hyperintensity along the corticospinal tracts and in the cere-
and demyelinating diseases, such as multiple sclerosis and bellar dentate nuclei (Fig. 9). Another disorder with thalamic
acute disseminated encephalomyelitis (which affect the white involvement is profound neonatal hypoxic-ischemic injury,
matter bilaterally and asymmetrically and may affect deep which typically involves the ventrolateral thalami along with
cerebral nuclei) [65,66]. End stage white matter disease of any posterior putamina and perirolandic cortices [76-78]; these
cause results in diffuse (superficial and deep), bilateral white patients typically have a characteristic history of perinatal dis-
matter damage that is completely nonspecific. tress and neonatal encephalopathy that simplifies the diagnosis
[79-81]. Another consideration when thalamic involvement is
Metabolic disorders affecting both gray and white matter identified is autosomal dominant acute necrotizing encephalitis
Disorders involving both gray and white matter are first separat- [82,83], particularly if T2 hyperintensity is lso seen in the dor-
ed by the type of gray matter involvement: those involving only sal brain stem. Thalami may also be affected in mitochondrial
the cerebral cortex and those involving deep gray matter (with disorders, Wilson disease, and Canavan disease; typically other
or without cortical involvement). deep gray matter nuclei will be affected, as well (putamina in
mitochondrial disorders and Wilson disease, globus pallidus in
Cerebral cortex involvement Canavan disease).
Those disorders involving only cortical gray matter can be sub- Globus pallidus involvement in association with diffuse
divided depending on involvement of long bones and the spinal white matter disease including the subcortical, deep, and periven-
column. If the long bones are normal, the cortex should be ana- tricular regions suggests a diagnosis of Canavan disease (Fig. 10)
lyzed for malformations of cortical development (MCD). If an [84]. Association of globus pallidus involvement with affected
S10 REV NEUROL 2006; 43 (Supl 1): S5-S16
CONFERENCIA MAGISTRAL
a b the affected regions, and a
characteristic peak at 0.9
ppm on proton MR spec-
troscopy (see below) [56,
57,85]. Carbon monoxide
and cyanide toxicity typical-
ly involve the cerebral cortex
and striatum and, sometimes,
the cerebellum [86-89]. Ta-
a ble V lists some disorders
with involvement of both
white matter and the globus
pallidus.
White matter disease
associated with striatal (pu-
tamen and caudate) involve-
ment suggests Leigh syn-
drome, MELAS, propionic
acidemia, glutaric aciduria
type 1 (glutaryl CoA de-
hydrogenase deficiency),
Figure 8. Congenital muscular dystrophy with brain involvement: a) Axial SE 2500/80 image shows abnormal
hyperintensity in the frontal and parietal white matter. The cortical gyral pattern in the frontal lobes (arrows) is dys- molybdenum cofactor defi-
plastic; b) Axial image through the cerebellum shows dysplastic cortex with multiple subcortical cysts (arrows). ciency, isolated sulfite oxi-
dase deficiency, hypomyeli-
a b nation with atrophy of the
basal ganglia and cerebel-
lum, toxic exposure, later
infantile or childhood pro-
found hypoxic-ischemic in-
jury, or childhood hypo-
glycemia (Table VI). Regions
of involvement in Leigh syn-
drome vary with the underly-
ing molecular cause of the
disorder, although no consis-
tently reproducible geno-
type-phenotype associations
have been identified. In
MELAS, cortical lesions are
more common than basal
ganglia lesions, and are usu-
ally present by the time basal
ganglia involvement is iden-
tified. Two imaging features
Figure 9. Globoid cell leukodystrophy (Krabbe disease): a) Axial SE 3000/120 in this infant shows abnormal hyper- can help to differentiate the
intensity (arrows) along the corticospinal tracts in the posterior limbs of the internal capsules; b) Axial image in the cortical lesions of MELAS
posterior fossa shows abnormal hyperintensity in the hila of the cerebellar dentate nuclei (white arrows) and in
the medullary pyramids (black arrowheads).
from those of ischemic in-
farcts: the locations do not
correspond to vascular terri-
subcortical white matter but sparing of periventricular white mat- tories; and premature senescent calcifications in the globus pal-
ter suggests a later phase of Kearns-Sayre syndrome (globus pal- lidus are typically identified on CT [90]. Glutaric aciduria type 1
lidus are spared in early phases) or L-2-hydroxyglutaric aciduria is typically associated with enlarged subarachnoid spaces, partic-
(Fig. 1); the latter will often show involvement of the cerebellar ularly in the anterior sylvian fissures, and central white matter T2
dentate nuclei [16]. Diffuse white matter involvement, with spar- hyperintensity. Isolated sulfite oxidase deficiency is rapidly pro-
ing the subcortical white matter during the early stages of the dis- gressive and causes multicystic encephalomalacia of the cerebral
ease, suggests methylmalonic acidemia, maple syrup urine dis- white matter to develop within the first weeks after birth [91].
ease, carbon monoxide toxicity, or cyanide toxicity. MRI of Cockayne disease will show calcification of the striatum, as well
maple syrup urine disease during the acute neonatal phase of the as characteristic facies and other aspects of the syndrome.
disease typically shows involvement of the corticospinal tracts in Proper analysis of the MR scans using this pattern system
the centrum semiovale, internal capsules, cerebral peduncles, can facilitate the work-up of patients with inborn errors of
dorsal pons, and cerebellar white matter, reduced diffusivity in metabolism.
REV NEUROL 2006; 43 (Supl 1): S5-S16 S11
A.J. BARKOVICH
PROTON MR
a b
SPECTROSCOPY
IN METABOLIC
DISORDERS
At the University of California
at San Francisco, we have
found that proton MR spec-
troscopy (MRS) can be an
extremely useful adjunct when
a patient is being imaged for
clinical suspicion of an inborn
error of metabolism. In some
cases, the spectroscopy serves
mainly to help verify a diagno-
sis already suspected by clinical
suspicion or by the analysis of
pattern on MRI. For example,
the pattern of brain involvement
in neonatal maple syrup urine Figure 10. Canavan disease in a 12-month-old infant: a) Axial SE 2500/80 image shows diffuse white matter
disease is very specific. Edema hyperintensity, including the subcortical, deep, and periventricular white matter. Abnormal hyperintensity is also
(FLAIR and T2 hyperintensity) seen in the globus pallidus (g); b) Calculated diffusivity map shows abnormally reduced diffusivity in the white
matter and globus pallidus.
is present in the dorsal brain
stem, the cerebellar white matter, the internal capsules and cere- Table V. Metabolic disorders with globus pallidus and white matter involve-
bral corticospinal tracts, and the globus pallidus (Fig. 11) [85]. ment.
Proton MRS helps to confirm the findings when it shows a charac- Canavan disease
teristic broad peak centered at 0.9 ppm (Fig. 11d) that represents
branched chain amino acids and ketoacids [57]. Similarly, Cana- Methylmalonic acidemia
van disease has a characteristic pattern of diffuse white matter Kearns-Sayre syndrome
edema, involving periventricular, deep, and subcortical white mat-
ter, in addition to bilateral globus pallidus and, sometimes, thala- L-2-hydroxyglutaric aciduria
mic involvement [84,92]. Proton MRS helps to confirm this sus- Maple syrup urine disease
pected diagnosis by revealing a very large NAA peak at 2.01 ppm.
In other disorders, MRS is essential for making the diagnosis. Carbon monoxide poisoning
The clinical features and MRI imaging pattern of patients with Cyanide toxicity
nonketotic hyperglycinemia, for example, is nonspecific. Proton
MRS, however, shows an elevated glycine peak at 3.55 ppm on
both long and short echo spectra. Using a short echo time, one Table VI. Metabolic disorders with striatal (caudate and putaminal) and
might confuse the peak with that of myo-Inositol, but if the peak white matter involvement.
persists at long echo times such as 270 or 288 ms, it represents
Leigh syndrome
glycine and strongly suggests the diagnosis. Many other disor-
ders have spectroscopic findings that are nearly specific in mak- Mitochondrial encephalopathy with lactic acidosis
ing the diagnosis: a single peak for pyruvate (2.36 ppm) and a and stroke-like symptoms (MELAS)
doublet for lactate (1.33 ppm) in pyruvate dehydrogenase defi- Other mitochondrial leukoencephalopathies
ciency; a singlet for succinate at 2.40 ppm in succinate dehydro-
genase deficiency; a singlet at 1.3 ppm in Sjögren-Larsson syn- Propionic acidemia
drome; two singlets (at 3.67 and 3.74 ppm) in untreated galac- Glutaric acidemia type I
tosemia; and a singlet at 7.36 ppm in phenylketonuria [15]. In
creatine deficiency syndromes, MRS is the most important tech- Isolated sulfite oxidase deficiency
nique in making the diagnosis. Creatine deficiency syndromes Late infantile/childhood profound hypoxic-ischemic injury
include disorders due to defects in synthesis –guanidinoacetate
methyltransferase (GAMT) deficiency [93,94] and arginine:gly- Childhood hypoglycemia
cine amidinotransferase (AGAT) deficiency [95]– and defects in
the transport of creatine across the blood-brain barrier (X-linked
creatine transporter defect) [96,97]. Patients with GAMT defi- Proton MRS can also be important in assessing response to
ciency often have abnormal hyperintensity of the globus pallidus therapy of metabolic disorders. Response to oral creatine sup-
on FLAIR and T2 weighted images, but patients with AGAT defi- plementation by following brain creatine levels with MRS has
ciency and creatine transporter defects can only be detected by already been discussed in the previous paragraph. Proton MRS
appreciated the low or absent creatine peak on proton MRS of the also allows monitoring of the brain phenylalanine levels in
brain (Fig. 12). As oral creatine supplementation leads to striking patients with phenylketonuria (PKU), although it requires the
improvements in neurological exam and intellectual development use of a very short echo time (20 ms or less), because of the
[98], detection of this disorder with MRS is extremely important. short T2 relaxation time of the phenyl protons, and a large field
S12 REV NEUROL 2006; 43 (Supl 1): S5-S16
CONFERENCIA MAGISTRAL
a b develop the serious form of ALD.
Waiting until the child has rapidly
advancing or severe cerebral
involvement is not recommended,
either, as the procedure may lead
to acceleration of the disease
[101-103]. Proton MRS provides
important information in this
regard, as it shows abnormalities
before the MR imaging study
becomes abnormal in some chil-
dren [104] and in normal appear-
ing white matter peripheral to the
regions of T2 prolongation and
enhancement; this area of abnor-
mal MRS may represent zone C.
Indeed, it is suggested that reduc-
tion in the NAA/choline ratio to
below 5.0 is predictive of disease
c d progression within the next 2 to
3 years [101]. Therefore, proton
MRS should be performed in all
individuals with ALD, particular-
ly those with stable MR imaging
exams and in siblings (of patients
with ALD) who are known to
have the ALD mutation but are
as yet asymptomatic. A list of
disorders in which proton spec-
troscopy is particularly useful is
provided in table VII.
DIFFUSION WEIGHTED
IMAGING IN METABOLIC
DISORDERS
Figure 11. Maple syrup urine disease in a young infant: utility of proton MR spectroscopy and diffusion
weighted imaging: a,b) Axial SE 3000/120 images show abnormal hyperintensity in the globus pallidus and The literature about diffusion
posterior limbs of the internal capsules (black arrows) in a, and along the corticospinal tracts in the cerebral weighted imaging in metabolic
hemispheres (black arrows) in b. c) Axial calculated diffusivity image at the same level as (b) shows reduced
diffusion (hypointensity) in the corticospinal tracts in the cerebral hemispheres (black arrows); d) Proton MR disorders is contradictory and
spectroscopy (TE: 26 ms) shows a large peak at 0.9 ppm (arrow) that represents branched chain ketoacids. rather confusing because the
This peak is characteristic of maple syrup urine disease. The spectrum is otherwise normal for age. results depend upon the acuity
of the disease at the time of the
of view because cerebral phenylalanine level is typically very study. During an acute exacerbation of metachromatic leukody-
low (less than 1 mM/L). The resonances of the phenyl protons strophy or globoid cell leukodystrophy, for example, diffusion
are visualized in a single peak at 7.36 ppm; this peak has large weighted imaging shows reduced diffusion in the affected
enough amplitude that it can be quantified. Direct analysis of white matter, while in later, more quiescent phases, diffusivity
the brain is important because phenylalanine levels in the brain in increased [105]. This likely results from the fact that acute
do not correlate closely with those in the blood [99,100]. cellular injury, whether from toxins, ischemia, trauma, or infec-
In some disorders, proton MRS can aid in making a diagnosis tion, results in the slowing of the motion of water molecules
and instituting therapy before clinical signs and symptoms devel- (reduced diffusivity). Later, after axons, cell bodies, or myelin
op. An excellent example of this is X-linked adrenoleukodystro- have been damaged, there are fewer barriers to water motion
phy (ALD). In this disorder, the central issue is whether a boy car- and diffusivity is increased. Other disorders cause a specific
rying the biochemical/genetic defect should undergo hematopoiet- type of myelinopathy (myelin vacuolization [105]) that results
ic stem cell transplantation, a form of treatment reserved for the in a marked decrease in diffusivity. An example of this type of
rapidly progressive cerebral disease (an not for the later-onset disorder is neonatal onset maple syrup urine disease. During
variant known as adrenomyeloneuropathy). If bone marrow trans- the acute phase of the disease, myelin (mature and immature)
plantation is performed early in the course of the rapidly progres- becomes edematous and the spirals become slightly separated;
sive disease, it may prevent further deterioration or even lead to during this phase of the disease, all myelinated parts of the
improvement [101-103]. However, the therapy is not recommend- brain show up to an 80% reduction in diffusivity, resulting in
ed for asymptomatic children, as the morbidity and mortality asso- markedly increased signal intensity on diffusion weighted images
ciated with transplantation is high and more than 50% will never and markedly decreased signal intensity on diffusivity images
REV NEUROL 2006; 43 (Supl 1): S5-S16 S13
A.J. BARKOVICH
Table VII. Utility of proton spectroscopy in metabolic disorders.
Identification of a specific peak
Canavan disease
Maple syrup urine disease
Nonketotic hyperglycinemia
Succinate dehydrogenase deficiency
Sjögren-Larsson syndrome
Phenylketonuria
Pyruvate dehydrogenase deficiency
Absence of a normal peak
Creatine deficiency disorders
Identification of a nonspecific peak
Mitochondrial disorders (lactate) Figure 12. Creatine deficiency due to arginine:glycine amidinotransferase
(AGAT) mutation: proton MR spectrum from the patient’s basal ganglia
Alexander disease (myo-Inositol) region shows only two peaks, choline (Ch) and N-acetylaspartate (NAA).
The creatine peak, normally at 3.03 ppm (see figure 11d) is absent.
–also called apparent diffusion coefficient images (Fig. 11c) CONCLUSION
[56]–. Several other disorders show markedly reduced diffu- The analysis and diagnosis of metabolic disorders is extremely
sion in the acute state, including nonketotic hyperglycinemia, complicated and difficult. If a practical methodological approach
Kearns-Sayre syndrome, and Canavan disease (Fig. 10), is used in the interpretation of MRI studies of the brain, these
although the precise mechanism by which the diffusivity de- studies can be extremely useful in helping to narrow the differ-
creases is not known. The precise timing of the changes in dif- ential diagnosis of affected patients. Proper understanding and
fusivity with respect to onset of the disease and its histologic analysis of proton MR spectroscopy and diffusion weighted
progression is not know, but it is well established that, after imaging can further help, in some patients, to narrow the diagno-
the acute stage of encephalopathy, myelin will break down sis. The use of this approach can significantly simplify the job of
and diffusivity will increase. the neurologist or geneticist trying to make the proper diagnosis.
REFERENCES
1. Van der Knaap M, Breiter S, Naidu S, Hart A, Valk J. Defining and cat- 11. Vanhanen SL, Raininko R, Santavuori P. Early differential diagnosis of
egorizing leukoencephalopathies of unknown origin: MR imaging infantile neuronal ceroid lipofuscinosis, Rett syndrome, and Krabbe
approach. Radiology 1999; 213: 121-33. disease by CT and MR. AJNR Am J Neuroradiol 1994; 15: 1443-453.
2. Barkovich AJ. Toxic and metabolic brain disorders. In Barkovich AJ, 12. Hayflick S, Westaway S, Levinson B, Zhou B, Johnson M, Ching K, et
ed. Pediatric neuroimaging. 4 ed. Philadelphia: Lippincott Williams & al. Genetic, clinical and radiographic delineation of Hallervorden-
Wilkins; 2005. p. 76-189. Spatz syndrome. N Engl J Med 2003; 348: 33-40.
3. Van der Knaap MS, Valk J. Pattern recognition in white matter disor- 13. Hayflick SJ, Penzien JM, Michl W, Sharif UM, Rosman NP, Wheeler
ders. In van der Knaap MS, Valk J, eds. Magnetic resonance of myeli- PG. Cranial MRI changes may precede symptoms in Hallervorden-
nation and myelin disorders. 3 ed. Berlin: Springer; 2005. p. 881-904. Spatz syndrome. Pediatr Neurol 2001; 25: 166-9.
4. Van der Knaap MS, Valk J, De Neeling N, Nauta JJ. Pattern recogni- 14. Moser HW. Adrenoleukodystrophy: from bedside to molecular biolo-
tion in magnetic resonance imaging of white matter disorders in chil- gy. J Child Neurol 1987; 2: 140-50.
dren and young adults. Neuroradiology 1991; 33: 478-93. 15. Van der Knaap MS, Valk J. Magnetic resonance of myelination and
5. Van der Knaap M, Naidu S, Pouwels P, Bonacita S, Van Coster R, myelin disorders. 3 ed. Berlin: Springer; 2005.
Lagae L, et al. New syndrome characterized by hypomyelination with 16. D’Incerti L, Farina L, Moroni I, Uziel G, Savoiardo M. L-2-hydroxyg-
atrophy of the basal ganglia and cerebellum. AJNR Am J Neuroradiol lutaric aciduria: MRI in seven cases. Neuroradiology 1998; 40: 727-33.
002; 23: 1466-74. 17. Barkovich AJ, Good W, Koch TK, Berg BO. Mitochondrial disorders:
6. Van der Knaap MS, Barth PG, Stroink H, Van Nieuwenhuizen O, Arts analysis of their clinical and imaging characteristics. AJNR Am J Neu-
WFM, Hoogenraad F, et al. Leukoencephalopathy with swelling and a roradiol 1993; 14: 1119-37.
discrepantly mild clinical course in eight children. Ann Neurol 1995; 18. Imamura A, Ito R, Tanaka S. High intensity proton and T2 weighted
37: 324-34. MR signals in the globus pallidus in juvenile type of dentatorubral and
7. Van der Knaap MS, Barth PG, Gabreëls FJM, Franzoni E, Begeer JH, pallidoluysian atrophy. Neuropediatrics 1994; 25: 234-7.
Stroink H, et al. A new leukoencephalopathy with vanishing white 19. Miyazaki M, Kato T, Hashimoto T, Harada M, Kondo I, Kuroda Y. MR
matter. Neurology 1997; 48: 845-55. of childhood onset dentatorubral-pallidoluysian atrophy. AJNR Am J
8. Autti T, Raininko R, Vanhanen SL, Santavuori P. Magnetic resonance Neuroradiol 1995; 16: 1834-6.
techniques in neuronal ceroid lipofuscinoses and some other lysosomal 20. Fukuzawa T, Matsutani S, Maruyama H, Akiike T, Saisho H, Hattori T.
diseases affecting the brain. Curr Opin Neurol 1997; 10: 519-24. Magnetic resonance images of the globus pallidus in patients with
9. Autti T, Raininko R, Vanhanen SL, Santavuori P. MRI of neuronal idiopathic portal hypertension: a quantitative analysis of the relation-
ceroid lipofuscinosis. I. Cranial MRI of 30 patients with juvenile neu- ship between signal intensity and the grade of portosystemic shunt. J
ronal ceroid lipofuscinosis. Neuroradiology 1996; 38: 476-82. Gastroenterol Hepatol 2006; 21: 902-7.
10. Vanhanen SL, Raininko R, Autti T, Santavuori P. MRI evaluation of the 21. Govaert P, Lequin M, Swarte R, Robben S, De Coo R, Weisglas-Kupe-
brain in infantile neuronal ceroid-lipofuscinoses. II. MRI findings in rus N, et al. Changes in globus pallidus with (pre)term kernicterus.
21 patients. J Child Neurol 1995; 10: 444-50. Pediatrics 2003; 112: 1256-63.
S14 REV NEUROL 2006; 43 (Supl 1): S5-S16
CONFERENCIA MAGISTRAL
22. Martich-Kriss V, Kollias S, Ball WS. MR findings in kernicterus. 49. Kwan E, Drace J, Enzmann D. Specific CT findings in Krabbe disease.
AJNR Am J Neuroradiol 1995; 16: 819-21. AJR Am J Roentgenol 1984; 143: 665-70.
23. Penn A, Enzmann D, Hahn J, Stevenson D. Kernicterus in a full term 50. Koelfen W, Freund M, Jaschke W, Koenig S, Schultze C. GM2 gan-
infant. Pediatrics 1994; 93: 1003-6. gliosidosis (Sandhoff’s disease): two year follow-up by MRI. Neurora-
24. Lim MK, Suh CH, Kim JK, Cho YK, Choi SH, Kang JH, et al. Sys- diology 1994; 36: 152-4.
temic lupus erythematosus: brain MR imaging and single-voxel hydro- 51. Mugikura S, Takahashi S, Higano S, Kurihara N, Kon K, Sakamoto K.
gen 1 MR spectroscopy. Radiology 2000; 217: 43-9. MR findings in Tay-Sachs disease. J Comput Assist Tomogr 1996; 20:
25. Oku K, Atsumi T, Furukawa S, Horita T, Sakai Y, Jodo S, et al. Cerebral 551-5.
imaging of magnetic resonance imaging and single photon emission 52. Barkovich AJ, Ferriero DM, Bass N, Boyer R. Involvement of the ponto-
computed tomography in systemic lupus erythmatosus with central medullary corticospinal tracts: a useful finding in the diagnosis of X-link-
nervous system involvement. Rheumatology (Oxford) 2003; 42: 773-7. ed adrenoleukodystrophy. AJNR Am J Neuroradiol 1997; 19: 95-100.
26. Sherwood JW, Wagle WA. Hemolytic uremic syndrome: MR findings 53. Schiffmann R, Moller JR, Trapp BD. Childhood ataxia with diffuse cen-
of CNS complications. AJNR Am J Neuroradiol 1991; 12: 703-4. tral nervous system hypomyelination. Ann Neurol 1994; 35: 331-40.
27. Hager A, Staudt M, Klare B, Von Einsiedel H, Krägeloh-Mann I. 54. Charnas L, Bernar J, Pezeshkpour GH, Kalakas M, Harper GS, Gahl
Hemolytic-uremic syndrome with involvement of basal ganglia and WA. MRI findings and peripheral neuropathy in Lowe’s syndrome.
cerebellum. Neuropediatrics 1999; 30: 210-3. Neuropediatrics 1988; 19: 7-9.
28. Takanashi J, Barkovich A, Cheng S, Kostiner D, Baker J, Packman S. 55. Schneider JF, Boltshauser E, Neuhaus TJ, Rauscher C, Martin E. MRI and
Brain MR imaging in acute hyperammonemic encephalopathy arising proton spectroscopy in Lowe syndrome. Neuropediatrics 2001; 32: 45-8.
from late-onset ornithine transcarbamylase deficiency. AJNR Am J 56. Cavalleri F, Bernardi A, Burlina A, Ferrari F, Mavilla L. Diffusion-
Neuroradiol 2003; 24: 390-3. weighted MRI of maple syrup urine disease encephalopathy. Neurora-
29. Takanashi J, Barkovich AJ, Cheng SF, Weisiger K, Zlatunich CO, diology 2002; 44: 499-502.
Mudge C, et al. Brain MR imaging in neonatal hyperammonemic 57. Jan W, Zimmerman R, Wang Z, Berry G, Kaplan P, Kaye E. MR diffu-
encephalopathy resulting from proximal urea cycle disorders. AJNR sion imaging and MR spectroscopy of maple syrup urine disease dur-
Am J Neuroradiol 2003; 24: 1184-7. ing acute metabolic decompensation. Neuroradiology 2003; 45: 393-9.
30. Autti T, Raininko R, Santavuori P, Vanhanen SL, Poutanen VP, Haltia M. 58. Barkovich AJ. Pediatric neuroimaging. 4 ed. Philadelphia: Lippincott
MRI of neuronal ceroid lipofuscinosis. II. Postmortem MRI and histo- Williams & Wilkins; 2005.
pathological study of the brain in 16 cases of neuronal ceroid lipofusci- 59. Graham JW, Jan W. MRI and the brain in systemic lupus erythemato-
nosis of juvenile or late infantile type. Neuroradiology 1997; 39: 371-7. sus. Lupus 2003; 12: 891-6.
31. Frei KP, Patronas NJ, Crutchfield KE, Altarescu G, Schiffmann R. 60. Lalani TA, Kanne JP, Hatfiled GA, Chen P. Imaging findings in sys-
Mucolipidosis type IV: characteristic MRI findings. Neurology 1998; temic lupus erythematosus. Radiographics 2004; 24: 1069-86.
51: 565-9. 61. Aida N, Tamagawa K, Takada K, Yagishita A, Kobayashi N, Chiku-
32. Melis D, Parenti G, Casa RD, Sibilio M, Romano A, Di Salle F, et al. maru K, et al. Brain MR in Fukuyama congenital muscular dystrophy.
Brain damage in glycogen storage disease type I. J Pediatr 2004; 144: 637. AJNR Am J Neuroradiol 1996; 17: 605-14.
33. Van der Knaap MS, Valk J. The reflection of histology in MR imaging 62. Leite CC, Reed UC, Otaduy MCG, Lacerda MTC, Costa MOR, Fer-
of Pelizaeus-Merzbacher disease. AJNR Am J Neuroradiol 1989; 10: reira LG, et al. Congenital muscular dystrophy with merosin deficien-
99-103. cy: H1 MR spectroscopy and diffusion-weighted MR imaging. Radiol-
34. Van der Knaap MS, Valk J. Pelizaeus-Merzbacher disease and X- ogy 2005; 235: 190-6.
linked spastic paraplegia type 2. In van der Knaap MS, Valk J, eds. 63. Barkovich AJ. Neuroimaging manifestations and classification of congen-
Magnetic resonance of myelin, myelination, and myelin disorders. 3 ital muscular dystrophies. AJNR Am J Neuroradiol 1998; 19: 1389-96.
ed. Berlin: Springer; 2005. p. 272-80. 64. Van der Knaap MS, Smit LME, Barth PG, Catsman-Berrevoets CE,
35. Bugiani M, Al Shahwan S, Lamantea E, Bizzi A, Bakhsh E, Moroni I, Brouwer OF, Begeer JH, et al. MRI in classification of congenital mus-
et al. GJA12 mutations in children with recessive hypomyelinating cular dystrophies with brain abnormalities. Ann Neurol 1997; 42: 50-9.
leukoencephalopathy. Neurology 2006; 67: 273-9. 65. Baum P, Barkovich AJ, Koch T, Berg BO. Deep gray matter involve-
36. Uhlenberg B, Schuelke M, Rüschendorf F, Ruf N, Kaindl AM, Hen- ment in children with acute disseminated encephalomyelitis. AJNR
neke M, et al. Mutations in the gene encoding gap junction protein Am J Neuroradiol 1994; 15: 1275-83.
alpha-12 (Connexin 46.6) cause Pelizaeus-Merzbacher-like disease. 66. Leake JA, Albani S, Kao AS, Senac MO, Billman GF, Nespeca MP, et
Am J Hum Genet 2004; 75: 251-60. al. Acute disseminated encephalomyelitis in childhood: epidemiologic,
37. Battistella PA, Peserico A. Central nervous system dysmyelination in clinical and laboratory features. Pediatr Infect Dis J 2004; 23: 756-64.
PIBI(D)S syndrome: a further case. Childs Nerv Syst 1996; 12: 110-3. 67. Braverman N, Dodt G, Gould SJ, Valle D. Disorders of peroxisome
38. Porto L, Weis R, Schulz C, Reichel P, Lanfermann H, Zanella FE. biogenesis. Hum Mol Genet 1995; 4: 1791-8.
Tay’s syndrome: MRI. Neuroradiology 2000; 42: 849-51. 68. Faust PL, Banka D, Siriratsivawong R, Ng VG, Wikander TM. Peroxi-
39. Ostergaard JR, Christensen T. The central nervous system in Tay syn- some biogenesis disorders: the role of peroxisomes and metabolic dys-
drome. Neuropediatrics 1996; 27: 326-30. function in developing brain. J Inherit Metab Dis 2005; 28: 369.
40. Linnankivi T, Autti T, Pihko S, Somer M, Tienari P, Wirtavuori K, et al. 69. Barkovich AJ, Linden CL. Congenital cytomegalovirus infection of the
18q-syndrome: brain MRI shows poor differentiation of gray and white brain: imaging analysis and embryologic considerations. AJNR Am J
matter on T2-weighted images. J Magn Reson Imaging 2003; 18: 414-9. Neuroradiol 1994; 15: 703-15.
41. Loevner LA, Shapiro RM, Grossman RI, Overhauser J, Kamholz J. 70. Boppana S, Fowler K, Vaid Y, Hedlund G, Stagno S, Britt W, et al.
White matter changes associated with deletions of the long arm of Neuroradiographic findings in the newborn period and long-term out-
chromosome 18 (18q-syndrome): a dysmyelinating disorder? AJNR come in children with symptomatic congenital cytomegalovirus infe-
Am J Neuroradiol 1996; 17: 1843-8. cion. Pediatrics 1997; 99: 409-14.
42. Linnankivi T, Lonnqvist T, Autti T. A case of Salla disease with involve- 71. Steinlin MI, Nadal D, Eich GF, Martin E, Boltshauser EJ. Late intra-
ment of the cerebellar white matter. Neuroradiology 2003; 45: 107-9. uterine cytomegalovirus infection: clinical and neuroimaging findings.
43. Sonninen P, Autti T, Varho T, Hämäläinen M, Raininko R. Brain involve- Pediatr Neurol 1996; 15: 249-53.
ment in Salla disease. AJNR Am J Neuroradiol 1999; 20: 433-43. 72. Barone R, Nigro F, Triulzi F, Musumeci S, Fiumara A, Pavone L. Clin-
44. Takanashi J, Inoue K, Tomita M, Kurihara A, Morita F, Ikehira H, et al. ical and neuroradiological follow-up in mucopolysaccaridosis type III
Brain N-acetylaspartate is elevated in Pelizaeus-Merzbacher disease (Sanfilipo syndrome). Neuropediatrics 1999; 30: 270-4.
with PLP1 duplication. Neurology 2002; 58: 237-41. 73. Barone R, Parano E, Trifiletti R, Fiumara A, Pavone P. White matter
45. Song SK, Sun SW, Ramsbottom MJ, Chang C, Russell J, Cross AH. changes mimicking a leukodystrophy in a patient with mucopolysac-
Dysmyelination revealed through MRI as increased radial (but un- charidosis: characterization by MRI. J Neurol Sci 2002; 195: 171-5.
changed axial) diffusion of water. Neuroimage 2002; 17: 1429. 74. Lee C, Dineen TE, Brack M, Kirsch JE, Runge VM. Mucopolysaccha-
46. Van der Knaap MS, Naidu S, Breiter SN, Blaser S, Stroink H, Springer ridoses: characterization by cranial MR imaging. AJNR Am J Neurora-
S, et al. Alexander disease: diagnosis with MR imaging. AJNR Am J diol 1993; 14: 1285-92.
Neuroradiol 2001; 22: 541-52. 75. Murata R, Nakajima S, Tanaka A. MR imaging of the brain in patients
47. Topçu M, Saatci I, Topcuoglu MA, Kose G, Kunak B. Megalencephaly with mucopolysaccharidosis. AJNR Am J Neuroradiol 1989; 10: 1165-70.
and leukodystrophy with mild clinical course: a report on 12 new cas- 76. Barkovich AJ. MR and CT evaluation of profound neonatal and infan-
es. Brain Dev 1998; 20: 142-53. tile asphyxia. AJNR Am J Neuroradiol 1992; 13: 959-72.
48. Van der Knaap MS, Kamphorst W, Barth PG, Kraaijeveld CL, Gut E, 77. Barkovich AJ, Hallam D. Neuroimaging in perinatal hypoxic-ischemic
Valk J. Phenotypic variation with leukoencephalopathy with vanishing injury. MRDD Research Reviews 1997; 3: 28-41.
white matter. Neurology 1998; 51: 540-7. 78. Barkovich AJ, Westmark KD, Ferriero D, Sola A, Partridge C. Perina-
REV NEUROL 2006; 43 (Supl 1): S5-S16 S15
A.J. BARKOVICH
tal asphyxia: MR findings in the first 10 days. AJNR Am J Neuroradiol 93. Schulze A, Hess T, Wevers R, Mayatepek E, Bachert P, Marescau B, et
1995; 16: 427-38. al. Creatine deficiency syndrome caused by guanidinoacetate methyl-
79. Barnett A, Mercuri E, Rutherford M, Haataja L, Frisone M, Henderson transferase deficiency: diagnostic tools for a new inborn error of
S, et al. Neurological and perceptual-motor outcome at 5-6 years of metabolism. J Pediatr 1997; 131: 616-31.
age in children with neonatal encephalopathy: relationship with neona- 94. Stockler S, Isbrandt D, Hanefeld F, Schmidt B, Von Figura K. Guanidi-
tal brain MRI. Neuropediatrics 2002; 33: 242-8. noacetate methyltransferase deficiency: the first inborn error of crea-
80. Mercuri E, Rutherford M, Barnett A, Foglia C, Haataja L, Counsell S, tine metabolism in man. Am J Hum Genet 1996; 58: 914-22.
et al. MRI lesions and infants with neonatal encephalopathy. Is the 95. Item C, Stockler-Ipsiroglu S, Stromberger C, Muhl A, Alessandri M,
Apgar score predictive? Neuropediatrics 2002; 33: 150-6. Bianchi M, et al. Arginine:glycine amidinotransferase deficiency: the
81. Rutherford M, Pennock J, Schwieso J, Cowan F, Dubowitz L. Hypoxic third inborn error of creatine metabolism in humans. Am J Hum Genet
ischaemic encephalopathy: early and late magnetic resonance findings in 2001; 69: 1127-33.
relation to outcome. Arch Dis Child Fetal Neonatal Ed 1996; 75: 145-51. 96. Salomons G, Van Dooren S, Verhoeven N, Cecil K, Ball W, Degrauw
82. Neilson DE, Eiben RM, Waniewski S, Hoppel CL, Varnes ME, T, et al. X-linked creatine-transporter gene (SLC6A8) defect: a new
Bangert BA, et al. Autosomal dominant acute necrotizing encephalo- creatine-deficiency syndrome. Am J Hum Genet 2001; 68: 1497-500.
pathy. Neurology 2003; 61: 226-30. 97. Degrauw T, Salomons G, Cecil K, Chuck G, Newmeyer A, Schapiro
83. Neilson DE, Feiler HS, Wilhelmsen KC, Lynn A, Eiben RM, Kerr DS, M, et al. Congenital creatine transporter deficiency. Neuropediatrics
et al. Autosomal dominant acute necrotizing encephalopathy maps to 2002; 33: 232-8.
2q12.1-2q13. Ann Neurol 2004; 55: 291-4. 98. Stockler S, Hanefeld F, Frahm J. Creatine replacement in guanidinoac-
84. Brismar J, Brismar G, Gascon G, Ozand P. Canavan disease: CT and etate methyltransferase deficiency, a novel inborn error of metabolism.
MR imaging of the brain. AJNR Am J Neuroradiol 1990; 11: 805-10. Lancet 1996; 348: 789-90.
85. Brismar J, Aqueel A, Brismar G. Maple syrup urine disease. AJNR Am 99. Moats RA, Mosely KD, Koch R, Nelson M Jr Brain phenylalanine
J Neuroradiol 1990; 11: 1219-28. concentrations in phenylketonuria: research and treatment of adults.
86. Rachinger J, Fellner FA, Stieglbauer K, Trenkler J. MR changes after Pediatrics 2003; 112: 1575-9.
acute cyanide intoxication. AJNR Am J Neuroradiol 2002; 23: 1398-401. 100. Möller HE, Weglage J, Bick U, Wiedermann D, Feldmann R, Ullrich
87. Rosenberg NL, Myers JA, Martin WR. Cyanide-induced parkinsonism: K. Brain imaging and proton magnetic resonance spectroscopy in
clinical, MRI, and 6-fluorodopa PET studies. Neurology 1989; 39: 142-4. patients with phenylketonuria. Pediatrics 2003; 112: 1580-3.
88. Kinoshita T, Sugihara S, Matsusue E, Fujii S, Ametani M, Ogawa T. 101. Eichler F, Barker P, Cox C, Edwin D, Ulug A, Moser H, et al. Proton
Pallidoreticular damage in acute carbon monoxide poisoning: diffu- MR spectroscopic imaging predicts lesion progression on MRI in X-
sion-weighted MR imaging findings. AJNR Am J Neuroradiol 2005; linked andrenoleukodystrophy. Neurology 2002; 26: 901-7.
26: 1845-8. 102. Eichler F, Itoh R, Barker P, Mori S, Garrett E, Van Zijl P, et al. Proton
89. O’Donnell P, Buxton PJ, Pitkin A, Jarvis LJ. The magnetic resonance MR spectroscopic and diffusion tensor brain MR imaging in X-linked
imaging appearances of the brain in acute carbon monoxide poisoning. adrenoleukodystrophy: initial experience. Radiology 2002; 225: 245-52.
Clin Radiol 2000; 55: 273. 103. Wilken B, Dechent P, Brockmann K, Finsterbusch J, Baumann M,
90. Van der Knaap MS, Valk J. Mitochondrial encephalopathy with lactic Ebell W, et al. Quantitative proton magnetic resonance spectroscopy of
acidosis and stroke-like episodes. In van der Knaap MS, Valk J, eds. children with adrenoleukodystrophy before and after hematopoietic
Magnetic resonance of myelination and myelin disorders. 3 ed. Berlin: stem cell transplantation. Neuropediatrics 2003; 34: 237-46.
Springer; 2005. p. 204-11. 104. Tzika A, Ball W Jr, Vigneron D, Dunn RS, Nelson SJ, Kirks D. Child-
91. Dublin A, Hald J, Wootton-Gorges S. Isolated sulfite oxidase deficien- hood adrenoleukodystrophy: assessment with proton MR spectroscopy.
cy: MR imaging features. AJNR Am J Neuroradiol 2002; 23: 484-5. Radiology 1993; 189: 467-80.
92. Topçu M, Erdem G, Saatci I, Aktan G, Limlek A, Renda Y, et al. Clini- 105. Van der Knaap MS, Valk J. Diffusion-weighted imaging. In van der
cal and magnetic resonance imaging features of L-2-hydroxyglutaric Knaap MS, Valk J, eds. Magnetic resonance of myelination and myelin
acidemia: report of three cases in comparison with Canavan disease. J disorders. 3 ed. Berlin: Springer; 2005. p. 839-53.
Child Neurol 1996; 11: 373-7.
ABORDAJE DE LOS TRASTORNOS METABÓLICOS ABORDAGEM AOS DISTÚRBIOS METABÓLICOS
EN LA INFANCIA POR RESONANCIA MAGNÉTICA NA INFÂNCIA POR RESSONÂNCIA MAGNÉTICA
Resumen. Introducción. Los errores congénitos del metabolismo Resumo. Introdução. Os erros congénitos do metabolismo consti-
constituyen un grupo de trastornos cuyo diagnóstico no resulta fácil. tuem um grupo de distúrbios cujo diagnóstico não é fácil. As sinto-
Las sintomatologías de las distintas enfermedades se solapan, con matologias das diferentes doenças sobrepõem-se; frequentemente
frecuencia las pruebas bioquímicas no son específicas o bien son os exames bioquímicos ou não são específicos ou são pouco revela-
poco reveladoras, y los análisis genéticos son laboriosos, caros y dores e as análises genéticas são morosas, caras e muitas vezes
muchas veces no están disponibles en el mercado. Las técnicas de não estão disponíveis no mercado. As técnicas de diagnóstico por
diagnóstico por imagen pueden ser útiles en algunos trastornos, pero imagem podem ser úteis em alguns distúrbios, mas à medida que o
a medida que aumenta el número de enfermedades identificadas y número de doenças identificadas e descritas aumenta, em muitos
descritas, en muchos casos los resultados de las exploraciones por casos, os resultados dos exames por imagem parecem sobrepor-se.
imagen parecen solaparse. Desarrollo. Varios grupos han propuesto Desenvolvimento. Vários grupos propuseram uma abordagem por
un abordaje por técnicas de imagen basado en el reconocimiento de técnicas de imagem baseada no reconhecimento de padrões na res-
patrones en la resonancia magnética (RM), lo cual se complementa sonância magnética (RM), a qual é completada com dados sobre o
con datos sobre el metabolismo procedentes de la espectroscopia por metabolismo resultantes da espectroscopia por RM e dados micro-
RM y datos microestructurales proporcionados por la RM por difu- estruturais proporcionados pela RM por difusão ponderada. Con-
sión ponderada. Conclusión. Si se utiliza adecuadamente, este méto- clusão. Se for adequadamente utilizado, este método de reconheci-
do de reconocimiento de patrones empleado conjuntamente con otras mento de padrões utilizado conjuntamente com outras ferramentas
herramientas de imagen puede ser muy útil para dividir el complejo de imagem pode ser muito útil para dividir o complexo grupo de
grupo de trastornos metabólicos en otros grupos más fáciles de ma- distúrbios metabólicos noutros grupos mais fáceis de manejar. De
nejar. De hecho, esta aproximación permite, a veces, llegar a un diag- facto, esta abordagem permite, por vezes, chegar a um diagnóstico
nóstico específico. [REV NEUROL 2006; 43 (Supl 1): S5-16] específico. [REV NEUROL 2006; 43 (Supl 1): S5-16]
Palabras clave. Enfermedad de Canavan. Enfermedades cerebra- Palavras chave. Doença de Canavan. Doenças cerebrais. Doenças
les. Enfermedades mitocondriales. Errores congénitos del metabo- mitocondriais. Erros congénitos do metabolismo. Espectroscopia
lismo. Espectroscopia por resonancia magnética. Imágenes de re- por ressonância magnética. Imagens da ressonância magnética por
sonancia magnética por difusión. Leucodistrofia. Resonancia mag- difusão. Leucodistrofia. Ressonância magnética. Toxicidade dos me-
nética. Toxicidad de los medicamentos. dicamentos.
S16 REV NEUROL 2006; 43 (Supl 1): S5-S16
You might also like
- Baxarias-Herrerin Atlas of PaleopathologyDocument300 pagesBaxarias-Herrerin Atlas of PaleopathologyNardy100% (1)
- Money-Kyrle Counter-TransferenceDocument9 pagesMoney-Kyrle Counter-TransferenceAna Tello100% (1)
- Cardiopulmonary PhysiotherapyDocument181 pagesCardiopulmonary PhysiotherapyOana Moza100% (4)
- Catalogue Euroimmun Medical LaboratoryDocument297 pagesCatalogue Euroimmun Medical LaboratoryVlad100% (1)
- Krabbe DiseaseDocument6 pagesKrabbe DiseaseUrko GoroquietaNo ratings yet
- Terminología y Clasificación de Las Displasias (2004) PDFDocument7 pagesTerminología y Clasificación de Las Displasias (2004) PDFlucasher35No ratings yet
- LDM - Bionature 2021-06-03-32Document8 pagesLDM - Bionature 2021-06-03-32JUAN CAMILO GONZALEZ JULIONo ratings yet
- AsfixiaDocument3 pagesAsfixiaClaudia LópezNo ratings yet
- Neuroimaging Biomarkers in Alzheimer's DiseaseDocument136 pagesNeuroimaging Biomarkers in Alzheimer's DiseaseInternational Medical PublisherNo ratings yet
- 2020 Clinical Association of White MatterDocument9 pages2020 Clinical Association of White MatterMarco MerazNo ratings yet
- Future Neurol. (2012) 7 (5), 595-612Document18 pagesFuture Neurol. (2012) 7 (5), 595-612Anonymous fg5XXFOSj4No ratings yet
- Proforma For Registration of Subject For Dissertation: TH RDDocument10 pagesProforma For Registration of Subject For Dissertation: TH RDHariNo ratings yet
- Ams Postmortem - GDocument6 pagesAms Postmortem - GJUAN ANDRES GUARDIAS GARZONNo ratings yet
- Imagen Mas Epilepsia en NiñosDocument14 pagesImagen Mas Epilepsia en NiñosPosadasLoezaJosueKarlaNo ratings yet
- Sca IiDocument8 pagesSca IiAlfredo Enrique Marin AliagaNo ratings yet
- JR 5Document9 pagesJR 5rahmat feryadiNo ratings yet
- Matter and Its Changes JournalDocument17 pagesMatter and Its Changes JournalMuahmmad Aidil PahleviNo ratings yet
- MRI in ChildrenDocument12 pagesMRI in ChildrenNita HandayaniNo ratings yet
- Isolated Corpus Callosum AgenesisDocument3 pagesIsolated Corpus Callosum AgenesisaptivaxrayNo ratings yet
- Fneur 12 648740Document7 pagesFneur 12 648740june.talon7No ratings yet
- Ejemplo ArtículoDocument11 pagesEjemplo ArtículoAmaia AitanaNo ratings yet
- Adult Onset LeukodistrophiesDocument12 pagesAdult Onset LeukodistrophiesIvan MihailovicNo ratings yet
- Spinal DisDocument32 pagesSpinal DisAkmal Niam FirdausiNo ratings yet
- Leukodystrophies and Genetic Leukoencephalopathies in Children Specified by Exome Sequencing in An Expanded Gene PanelDocument9 pagesLeukodystrophies and Genetic Leukoencephalopathies in Children Specified by Exome Sequencing in An Expanded Gene PanelEduardo Rios DuboisNo ratings yet
- Adult LeucodystrophyDocument12 pagesAdult LeucodystrophylauraalvisNo ratings yet
- Erros Inatos Do MetabolismoDocument33 pagesErros Inatos Do MetabolismosurtosedeliriosNo ratings yet
- Journal AlzheimerDocument10 pagesJournal AlzheimerFaza KeumalasariNo ratings yet
- Neuropsychological Profile Associated To PKAN in Its Initial Phase A Case Series ReportDocument7 pagesNeuropsychological Profile Associated To PKAN in Its Initial Phase A Case Series ReportNataly CastañedaNo ratings yet
- Alzheimer Mechanisms and Therapeutic StrategiesDocument19 pagesAlzheimer Mechanisms and Therapeutic StrategiesArtemis LiNo ratings yet
- Brainsci 12 00885Document14 pagesBrainsci 12 00885José Ernesto AlonsoNo ratings yet
- Terminology and Classification of The Cortical Dysplasias PalminiDocument9 pagesTerminology and Classification of The Cortical Dysplasias PalminiAyhan BölükNo ratings yet
- Khachaturian 1985Document9 pagesKhachaturian 1985Abu Bakar SiddiqueNo ratings yet
- Espectro Taupatías Parkinson Demencias 2022Document25 pagesEspectro Taupatías Parkinson Demencias 2022Oscar BushNo ratings yet
- Zhang 2019Document10 pagesZhang 2019NATALIA MARTINEZ CORDOBANo ratings yet
- Neuroimaging in Bipolar DisorderDocument13 pagesNeuroimaging in Bipolar DisorderAngie GiraldoNo ratings yet
- Disruptions Result From Destruction of A NorDocument6 pagesDisruptions Result From Destruction of A NorAsri RachmawatiNo ratings yet
- Marchiafava-Bignami Disease Literature Review and Case ReportDocument4 pagesMarchiafava-Bignami Disease Literature Review and Case Reportc5nazs86No ratings yet
- Noonan Syndrome: Clinical Aspects and Molecular PathogenesisDocument25 pagesNoonan Syndrome: Clinical Aspects and Molecular PathogenesisFlavia ChNo ratings yet
- Alzheimers Biology CourseworkDocument8 pagesAlzheimers Biology Courseworkpqltufajd100% (2)
- New Treatments, Tests For Alzheimer'S in PipelineDocument3 pagesNew Treatments, Tests For Alzheimer'S in PipelineChoi Gong JuNo ratings yet
- Brain 2009 Barkovich 3199 230 Neuroembyology1Document32 pagesBrain 2009 Barkovich 3199 230 Neuroembyology1Azalia BahatNo ratings yet
- Ataxia AcutaDocument17 pagesAtaxia AcutaAlina AndreiNo ratings yet
- Akinetic MutismDocument9 pagesAkinetic MutismAlin CiubotaruNo ratings yet
- 10.1007@s00381 020 04746 9Document12 pages10.1007@s00381 020 04746 9Alvaro Perez HenriquezNo ratings yet
- Dementia LjubekovDocument8 pagesDementia LjubekovTea FelbarNo ratings yet
- 2002 - Alzheimer's Neurofibrillary Pathology and The Spectrum of Cognitive Function - Findings From The Nun StudyDocument11 pages2002 - Alzheimer's Neurofibrillary Pathology and The Spectrum of Cognitive Function - Findings From The Nun StudyEl Tal RuleiroNo ratings yet
- Peripheral Neuropathy Associated With Mitochondrial Disease in ChildrenDocument8 pagesPeripheral Neuropathy Associated With Mitochondrial Disease in ChildrenRenata CardosoNo ratings yet
- Limperopoulos Bolduc09 Neurodevelopmental Outcomes After CB Injury REVIEWDocument12 pagesLimperopoulos Bolduc09 Neurodevelopmental Outcomes After CB Injury REVIEWEccoNo ratings yet
- Childhood Leukodystrophies: A Clinical Perspective: ReviewDocument12 pagesChildhood Leukodystrophies: A Clinical Perspective: ReviewAnonymous fg5XXFOSj4No ratings yet
- AlzaimerDocument13 pagesAlzaimerAfni Panggar BesiNo ratings yet
- Sindrome de WestDocument8 pagesSindrome de Westmaria laura ramirezNo ratings yet
- Molecular Basis of Leigh Syndrome: A Current Look: Review Open AccessDocument14 pagesMolecular Basis of Leigh Syndrome: A Current Look: Review Open AccessValeria DomireliNo ratings yet
- Autism Pathogenesis 2Document18 pagesAutism Pathogenesis 2Prateek Kumar PandaNo ratings yet
- Bipolar Disorder and Epilepsy A Bidirectional Relation Neurobiological Underpinnings Current Hypotheses and Future Research DirectionsDocument14 pagesBipolar Disorder and Epilepsy A Bidirectional Relation Neurobiological Underpinnings Current Hypotheses and Future Research DirectionsRudolph MuliawanNo ratings yet
- Cortical Tubers, Cognition, and Epilepsy in Tuberous SclerosisDocument5 pagesCortical Tubers, Cognition, and Epilepsy in Tuberous SclerosisR BNo ratings yet
- Donepezil in Patients With Subcortical Vascular CognitiveDocument9 pagesDonepezil in Patients With Subcortical Vascular CognitiveStefanie KarinaNo ratings yet
- Advantage of Modified MRI Protocol For HDocument148 pagesAdvantage of Modified MRI Protocol For HasasakopNo ratings yet
- Epilepsy Patients With MalformationsDocument10 pagesEpilepsy Patients With MalformationsndiayesidyelndiayeNo ratings yet
- 人工智能在神经病理学中的应用:基于深度学习的tau蛋白病变评估Document23 pages人工智能在神经病理学中的应用:基于深度学习的tau蛋白病变评估meiwanlanjunNo ratings yet
- Murphy 2010Document13 pagesMurphy 2010Nadia SaiNo ratings yet
- SCAR1Document17 pagesSCAR1ADRIANA DE FREITAS SOUSANo ratings yet
- Overview of The Hereditary Ataxias - UpToDateDocument15 pagesOverview of The Hereditary Ataxias - UpToDatericanoy191No ratings yet
- Neurogenic BladderDocument8 pagesNeurogenic BladderrafendyfendyNo ratings yet
- Desarrollo Emocional PrimitivoDocument9 pagesDesarrollo Emocional PrimitivoAna TelloNo ratings yet
- Preocupación Maternal PrimariaDocument5 pagesPreocupación Maternal PrimariaAna TelloNo ratings yet
- Psychoanysis OnlineDocument10 pagesPsychoanysis OnlineAna TelloNo ratings yet
- Health ProblemsDocument51 pagesHealth ProblemsJerome Manaig SueltoNo ratings yet
- UtiDocument2 pagesUtiBasant karn50% (2)
- NephEasy-3 4 09Document181 pagesNephEasy-3 4 09mouhamedmaloulieNo ratings yet
- Untitled16 PDFDocument17 pagesUntitled16 PDFElizabeth LeonNo ratings yet
- Mdcat Bio W 1Document11 pagesMdcat Bio W 1jawad ashrafNo ratings yet
- Urolithiasis CampbellDocument54 pagesUrolithiasis CampbellMariana B.No ratings yet
- Premature Baby AssessmentDocument20 pagesPremature Baby AssessmentSREEDEVI T SURESHNo ratings yet
- Krok1 - Medicine - 2016Document20 pagesKrok1 - Medicine - 2016Anfas VNo ratings yet
- Case Write Up 1: Dengue Haemorrhagic Fever Saarah Huurieyah BT Wan Rosli 1050024 Year 4 Internal MedicineDocument16 pagesCase Write Up 1: Dengue Haemorrhagic Fever Saarah Huurieyah BT Wan Rosli 1050024 Year 4 Internal MedicineRoshandiep GillNo ratings yet
- Clinical Manifestations and Diagnosis of Bronchiectasis in AdultsDocument16 pagesClinical Manifestations and Diagnosis of Bronchiectasis in AdultsDAT TRANNo ratings yet
- Chemical Urinalysis TransDocument8 pagesChemical Urinalysis TransIan Carlo B GalangNo ratings yet
- Military Medicine: Romanian Journal ofDocument76 pagesMilitary Medicine: Romanian Journal ofÁbilson FabianiNo ratings yet
- Characteristics of Uveitis Presenting For The First Time in The Elderly Analysis of 91 Patients in A Tertiary CenterDocument9 pagesCharacteristics of Uveitis Presenting For The First Time in The Elderly Analysis of 91 Patients in A Tertiary CenterFrancescFranquesaNo ratings yet
- Rnpedia MCHNDocument27 pagesRnpedia MCHNlykanotmatroNo ratings yet
- Buerger Disease 1Document27 pagesBuerger Disease 1nadiaNo ratings yet
- Year 3 Undergraduate Progressive Test - Attempt reviewPDF - 231031 - 194511Document49 pagesYear 3 Undergraduate Progressive Test - Attempt reviewPDF - 231031 - 194511DR BUYINZA TITUSNo ratings yet
- Jha Sheth 2023 2023 Neurocritical Care Updates in Cerebrovascular DiseaseDocument5 pagesJha Sheth 2023 2023 Neurocritical Care Updates in Cerebrovascular DiseaseProdi Bedah SarafNo ratings yet
- 19 Kommuri Sahithi ReddyDocument14 pages19 Kommuri Sahithi ReddyAlina AlexandraNo ratings yet
- Hypolipidemic DrugsDocument34 pagesHypolipidemic Drugsmrudul harneNo ratings yet
- Chapter II: When To Use The Milk DietDocument11 pagesChapter II: When To Use The Milk Dietgibrambo5770No ratings yet
- Dermatology Images PDFDocument122 pagesDermatology Images PDFswethaNo ratings yet
- Pedia AbnormalDocument34 pagesPedia Abnormallight_tyrNo ratings yet
- Propofol Drug StudyDocument3 pagesPropofol Drug StudyAngelica shane Navarro100% (2)
- Dipiro 9 (012-047) PDFDocument36 pagesDipiro 9 (012-047) PDFNingrumSindayaniNo ratings yet
- Symptoms PDFDocument3 pagesSymptoms PDFVita AmiliaNo ratings yet
- Pharma QuestionsDocument13 pagesPharma QuestionsSarah Mae SinceroNo ratings yet
- Supplementary DataDocument8 pagesSupplementary DataMaria Luisa RomeroNo ratings yet