Professional Documents
Culture Documents
Visual Loss
Visual Loss
Uploaded by
Tanya HoCopyright:
Available Formats
You might also like
- Prophecy Neuro ICU Exam Content OutlineDocument5 pagesProphecy Neuro ICU Exam Content OutlineDarren DawkinsNo ratings yet
- Osteopathic Considerations in Systemic Dysfunction (2nd Ed)Document296 pagesOsteopathic Considerations in Systemic Dysfunction (2nd Ed)Natan Babek100% (1)
- GLAUCOMA Revised Concept MapDocument5 pagesGLAUCOMA Revised Concept MapJanselle H ArmaNo ratings yet
- EOE Diplopia Flow-ChartDocument1 pageEOE Diplopia Flow-ChartPaulaNo ratings yet
- Cataract Week 13Document9 pagesCataract Week 13Janselle H ArmaNo ratings yet
- Woc Trauma MataDocument4 pagesWoc Trauma MataChairunnisa Permata SariNo ratings yet
- Special Senses) 3. Photoreceptors - Rods and Cones - KeyDocument1 pageSpecial Senses) 3. Photoreceptors - Rods and Cones - Keyranag59100No ratings yet
- EmergenciesDocument16 pagesEmergenciesJack Ortega PuruggananNo ratings yet
- VisualDocument1 pageVisualGeraldine TeneclanNo ratings yet
- Notes On Meniere's DiseaseDocument5 pagesNotes On Meniere's DiseaseDipson HamalNo ratings yet
- EGurukul GlaucomaDocument15 pagesEGurukul GlaucomaOscar Daniel Mendez100% (1)
- Reniyasw: Ioptnlnosnsisunwnsionlsngdngims VioovyDocument3 pagesReniyasw: Ioptnlnosnsisunwnsionlsngdngims Vioovyวชิรพล คำแก้วNo ratings yet
- Disseminated Intravascular CoagulationDocument1 pageDisseminated Intravascular CoagulationAnn Justine OrbetaNo ratings yet
- Glaucoma: AetiologyDocument3 pagesGlaucoma: Aetiologyjames cordenNo ratings yet
- EGurukul - RetinaDocument23 pagesEGurukul - RetinaOscar Daniel Mendez100% (1)
- ARRYTHMIASDocument3 pagesARRYTHMIASitstheboyjayyNo ratings yet
- Benign Prostatic HyperplasiaDocument1 pageBenign Prostatic HyperplasiaAli SafaaNo ratings yet
- Augenheilkunde FragenDocument3 pagesAugenheilkunde FragenWise AmroNo ratings yet
- OphthalmologyDocument143 pagesOphthalmologyOscar Daniel Mendez100% (1)
- Bells PalsyDocument5 pagesBells PalsydeasyNo ratings yet
- PHA 618: Human Physiology and Pathophysiology Cardiovascular ExercisesDocument2 pagesPHA 618: Human Physiology and Pathophysiology Cardiovascular Exerciseskaila lunaNo ratings yet
- CNS PathologyDocument1 pageCNS Pathologydr.rohit9098No ratings yet
- Doping Pada OlahragaDocument4 pagesDoping Pada OlahragaAlya ArnoldNo ratings yet
- Lov AssignmentDocument1 pageLov AssignmentfaamcxclepiaNo ratings yet
- General Surgery 5Document19 pagesGeneral Surgery 5MaggieNo ratings yet
- ESRD PathoDocument1 pageESRD PathoPrecious VernalNo ratings yet
- Med Surg Notes 4Document11 pagesMed Surg Notes 4trashhhtineNo ratings yet
- Forensic MedicineDocument60 pagesForensic MedicineKoushal Sharma, JammuNo ratings yet
- Glaucoma: DR - Fitratul Ilahi, SPM (K)Document47 pagesGlaucoma: DR - Fitratul Ilahi, SPM (K)nurul ramadhiniNo ratings yet
- Pathophysiology: ThinningDocument1 pagePathophysiology: ThinningArwaNo ratings yet
- Safe FESS To Avoid Complication: CT-scan InterpretationDocument33 pagesSafe FESS To Avoid Complication: CT-scan InterpretationBebekNo ratings yet
- Materi Bimbingan Kepaniteraan Klinik Ilmu Penyakit Mata: No Pembimbing Topik Sub TopikDocument2 pagesMateri Bimbingan Kepaniteraan Klinik Ilmu Penyakit Mata: No Pembimbing Topik Sub TopikRizka ChairaniNo ratings yet
- ulcers ملخصDocument2 pagesulcers ملخصmohamed awaadNo ratings yet
- MRI and X-Ray ImagingDocument6 pagesMRI and X-Ray ImagingbeatriceosNo ratings yet
- CICUTA VIROSA (Cic)Document1 pageCICUTA VIROSA (Cic)mohd18160No ratings yet
- Optha RevisionDocument38 pagesOptha Revisionpriyanka chikotiNo ratings yet
- Arthroscopic Repair of Dorsal Radiocarpal Ligament Tear - Report of Four CasesDocument1 pageArthroscopic Repair of Dorsal Radiocarpal Ligament Tear - Report of Four CasesKamijou-sanNo ratings yet
- S3-04 Ophthalmology Chronic Vision Loss PDFDocument12 pagesS3-04 Ophthalmology Chronic Vision Loss PDFAl SyNo ratings yet
- Diencephalon, Brainstem & CerebellumDocument1 pageDiencephalon, Brainstem & CerebellumwinNo ratings yet
- Case Study: Object PhotosDocument8 pagesCase Study: Object PhotosDiwanNo ratings yet
- Haemorrhoids: Acute PresentationsDocument1 pageHaemorrhoids: Acute PresentationsMuhammad AkhyarNo ratings yet
- Eye Anatomy (R)Document3 pagesEye Anatomy (R)Nikster LuNo ratings yet
- Winslow PathwayDocument3 pagesWinslow PathwayMia MadalinaNo ratings yet
- MSK W4 Lec 6Document20 pagesMSK W4 Lec 6sharon christieNo ratings yet
- Common Indications For Gadolinium (MR Contrast) in MRIDocument2 pagesCommon Indications For Gadolinium (MR Contrast) in MRId dNo ratings yet
- Pain PerceptionDocument3 pagesPain PerceptionCarlos RodriguezNo ratings yet
- EpitheliumDocument1 pageEpitheliumhawdeng xalitNo ratings yet
- All-CVS HematologyDocument8 pagesAll-CVS HematologyRitika AgrawalNo ratings yet
- Note 17 Nov 2022Document19 pagesNote 17 Nov 2022Raghad RNo ratings yet
- MindMap Butterfly Anna-MariyaDocument1 pageMindMap Butterfly Anna-MariyaAnna-Maria LevenovaNo ratings yet
- Vitals: Stridor (Upper Airway Obstruction), Use of Acc. Muscles, DroolingDocument1 pageVitals: Stridor (Upper Airway Obstruction), Use of Acc. Muscles, DroolingSean LamNo ratings yet
- Ar 706Document1 pageAr 706Victor YeoNo ratings yet
- Pathophysio CRF2 - RevisedDocument1 pagePathophysio CRF2 - Reviseddeborah malnegroNo ratings yet
- GlaucomaDocument23 pagesGlaucomasnivetha96No ratings yet
- NystagmusDocument1 pageNystagmusArwa100% (1)
- Diagrams of EyeballDocument7 pagesDiagrams of EyeballHelworNo ratings yet
- Self-Declaration by TCS Associates Resuming OfficeDocument2 pagesSelf-Declaration by TCS Associates Resuming OfficeAlamuru SrinidhiNo ratings yet
- Antimicrobial Approach To Intra-Abdominal Infections in Adults - UpToDateDocument29 pagesAntimicrobial Approach To Intra-Abdominal Infections in Adults - UpToDatecontateste197789No ratings yet
- Drug StudyDocument7 pagesDrug StudyCarson BirthNo ratings yet
- Vitiligo A Review 2020 PDFDocument22 pagesVitiligo A Review 2020 PDFhannah khumairahNo ratings yet
- Intellectual Disability: Menchie M. Garachico Freddie C. Santos JRDocument42 pagesIntellectual Disability: Menchie M. Garachico Freddie C. Santos JRTEAM SPORTS GADTCNo ratings yet
- Hirac Installation Panel FPV SubstationDocument3 pagesHirac Installation Panel FPV SubstationekapadwiNo ratings yet
- Sr. No.3, Laxmi Nagar, Lane No.8, Near Paratibhtai School, Kondhwa BK, Pune - 48 Self - Bike NO NO NO NO NO NODocument6 pagesSr. No.3, Laxmi Nagar, Lane No.8, Near Paratibhtai School, Kondhwa BK, Pune - 48 Self - Bike NO NO NO NO NO NORamNo ratings yet
- Phenytoin: Phenytoin (PHT), Sold Under The Brand Name Dilantin AmongDocument13 pagesPhenytoin: Phenytoin (PHT), Sold Under The Brand Name Dilantin AmongMunna SahaniNo ratings yet
- New Study in Candida InfectionsDocument3 pagesNew Study in Candida InfectionsHenz FreemanNo ratings yet
- Pathophysiology of FeverDocument4 pagesPathophysiology of FeverEasha Jamil AbbasiNo ratings yet
- Ni 2021 69 6 1524 333440Document18 pagesNi 2021 69 6 1524 333440Krit KritNo ratings yet
- Oet 2 PDFDocument96 pagesOet 2 PDFSharika SayedNo ratings yet
- Multiple Endocrine NeoplasiaDocument10 pagesMultiple Endocrine NeoplasiacarmenNo ratings yet
- Orbital Cellulitis 2018Document20 pagesOrbital Cellulitis 2018María Alejandra Rojas MontenegroNo ratings yet
- An MRIDocument41 pagesAn MRIAsim AliNo ratings yet
- Endoscope Reprocessing Risk and Current Risk PracticeDocument65 pagesEndoscope Reprocessing Risk and Current Risk PracticeHosam GomaaNo ratings yet
- Prolonged StandingDocument2 pagesProlonged StandingMadalena CrespoNo ratings yet
- Psychiatric BookDocument268 pagesPsychiatric BookFan Eli100% (2)
- Cilia 2018Document1 pageCilia 2018Anna Beatriz Silva EspindolaNo ratings yet
- Polycythemia Vera: What Are The Symptoms of Polycythemia?Document10 pagesPolycythemia Vera: What Are The Symptoms of Polycythemia?Dimpal ChoudharyNo ratings yet
- 7 - Common Psychiatric Problems - Mubarak-SubaieDocument62 pages7 - Common Psychiatric Problems - Mubarak-SubaieLavitSutcharitkulNo ratings yet
- Revlimid Epar Medicine Overview - en PDFDocument4 pagesRevlimid Epar Medicine Overview - en PDFManju JNo ratings yet
- Death Claim Checklist 2017Document4 pagesDeath Claim Checklist 2017Cheche GonzalesNo ratings yet
- CarbimazoleDocument3 pagesCarbimazoleManish SharmaNo ratings yet
- Sade, Robert M. 2012 "The Graying of America Challenges and ControversiesDocument8 pagesSade, Robert M. 2012 "The Graying of America Challenges and ControversiesTengiz VerulavaNo ratings yet
- Exam 1 Practice QuestionsDocument31 pagesExam 1 Practice QuestionsJoslyn Gross0% (1)
- COVID-19 Shipboard Contingency Plan - Rev.1 - FULL VERSION - UPDATED 24.05.2020 PDFDocument88 pagesCOVID-19 Shipboard Contingency Plan - Rev.1 - FULL VERSION - UPDATED 24.05.2020 PDFbuzbonNo ratings yet
- ELEMENTS OF CHILD DEVELOPMENT - SplitDocument97 pagesELEMENTS OF CHILD DEVELOPMENT - SplitIndian learnerNo ratings yet
Visual Loss
Visual Loss
Uploaded by
Tanya HoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Visual Loss
Visual Loss
Uploaded by
Tanya HoCopyright:
Available Formats
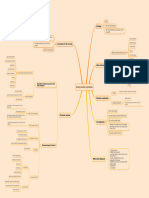
Increased IOP
Common Causes Corneal dystrophies
Dulling of the normally crisp reflection of
incident light off the cornea due to sudden Cataract surgery
CORNEAL EDEMA
opacification; ground-glass appearance of
the cornea Visual loss accompanying an attach of angle-
Ocular Emergency
closure glaucoma
Blunt trauma
Common Causes
Presence and leakage of abnormal vessels
HYPHEMA Blood in the anterior chamber Bed rest
Mild May not affect visual acuity
Ocular antihypertensive drugs
Severity Significant Reduced visual acuity
Treatment Topical corticosteroid
Complete VA Light Perception
Cycloplegic drops
Oral aminocaproic acid
Aging
Trauma
Media Opacities
Toxins
Common Causes
Systemic disease
Smoking
CATARACT Any opacity in the lens
Heredity
Based on clinical judgement + Patient's
Treatment visual acuity and assessment of interference Cataract Surgery
of ADLs
Trauma
Conditions that lead to retinal
Common Causes
neovascularization
Aneurysm rupture
Severe loss of vision with - RAPD
VITEROUS HEMORRHAGE Bleeding into the vitreous Common Findings VA never NLP
Opaque upon fundoscopy
Hemorrhage + Mobile vitreous + Attached
Observation
retina + No foreign body
Treatment
Hemorrhage + Vitreous contraction indicated
Vitrectomy
by decreased motility
7-10 days after initial wound repair
After posterior separation occurs
Requirements
After active bleeding subsides
After cornea is clearer
Chief Complaint: Flashing lights followed
by large numbers of floaters and then a
shade over the vision in one eye
RETINAL DETACHMENT Retinal tear leads to separation of retina
Rhegmatogenous
from epithelium
Fibrosis or fibrovascular proliferation leads
Types Traction
to scar tissue that pulls off retina
Accumulation of subretinal fluid leads to
Serous
retinal detachment
Reduced visual acuity
Retinal Disease Disease causing deterioration of the central
MACULAR DISEASE Common Findings +/- RAPD Treatment Laser Surgery
portion of the retina
Preceded by metamorphopsia
Sudden, painless loss of vision in one eye;
CRAO Cherry-red spot on fovea centralis
described as a "descending curtain"
Sudden onset of visual field defects (
BRAO
scotomas)
Occlusion of the central retinal artery or its Differentiate using RAPD and
RETINAL VASCULAR OCCLUSION Ophthalmoscopy
branches resulting to retinal ischemia NON-ISCHEMIC Subacute to mild-moderate loss of vision
CRVO
ISCHEMIC Sudden, severe loss of vision
BRVO Usually asymptomatic
Idiopathic
Common Causes
ACUTE VISUAL Inflammation of the optic nerve OPTIC NEURITIS
Multiple Sclerosis
Refer to an ophthalmologist
LOSS Common Findings Hyperemic and swollen optic disc
Chief Complaint: Monocular vision loss Inflammation of the orbital portion of the No abnormalities on ophthalmoscopic
that has developed over hours to days + Reduced VA and + RAPD RETROBULBAR OPTIC NEURITIS
optic nerve examination
Pain on movement of the eye
Swollen disc with blurred margins
Inflammation of the optic nerve papilla PAPILLITIS Common Findings Hyperemic disc
Usually unilateral
Elevated optic disc with indistinct margins
Microvascular congestion on disc
Common Findings Dilated retinal veins
Presence of flame-shaped hemorrhages
Usually bilateral
Signs of increased ICP
Swelling of the optic disc due to increased
Normal VA and - RAPD PAPILLEDEMA Pulsatile tinnitus
ICP
Loss of vision for a few seconds
Optic Nerve Disease
Orthostatic changes in vision
History Worsening headache when supine
Bilateral CN VI nerve palsies
Transient or persistent? With associated malaise, headache, fever,
weight loss, pain, polymyalgia rheumatica,
Monocular or binocular? Patient > 60 years old GIANT-CELL or TEMPORAL ARTERITIS Refer to an ophthalmologist
scalp tenderness or discomfort, jaw
claudication; ESR > 60 mm/hr
Timing and duration?
Common Causes
Vascular event
Patient's age?
Patient's comorbidities?
VISUAL LOSS ISCHEMIC OPTIC NEUROPATHY
Infammation
Pale, swollen disc
Did the patient have documented normal
vision in the past? Common Findings Splinter hemorrhages
Reduced VA and VF Altitudinal visual field loss
Direct or Penetrating trauma
CT Scan
TRAUMATIC OPTIC NEUROPATHY For neuroimaging
Diagnostics Indirect or Blunt trauma
Transmission of the shearing force to the
MRI
optic nerve
Vascular events
HEMIANOPSIA Common Causes
Visual Acuity Tumors
Confrontation Field Test Visual Pathway Disorders Extensive bilateral damage to the cerebral
visual pathways resulting in complete loss of
Pupillary Light Reaction vision
CORTICAL BLINDNESS
Ophthalmoscopy Normal PLR
Penlight Examination Special Tests for
Functional
Disorders
Tonometry
Tangent Screen Test
Slit-lamp Examination
Functional Disorders Visual loss without organic basis Mirror Test
Optokinetic Drum Test
Acute Discovery of Chronic Visual
Loss
CHRONIC VISUAL
LOSS
Impaired outflow of aqueous resulting from
abnormalities within the drainage system of GLAUCOMA CATARACT MACULAR DEGENERATION
the anterior chamber angle
Acquired chronic optic neuropathy Any opacity in the lens Age-related macular degeneration (AMD) is a Beckman Initiative for Macular Research
Open-angle glaucoma characterized by optic disc cupping and complex multifactorial progressive disease Classification Committee staging based on
visual field loss and usually associated with characterized initially by accumulation of lesions within two disc diameters of the
raised intraocular pressure all of lens substance is opaque Mature Cataract material (drusen) beneath the RPE fovea in either eye
Impaired outflow of aqueous resulting from
impaired access of aqueous to the drainage Angle-closure glaucoma some regions of the lens are transparent Immature Cataract
system Prophylactic Therapy to prevent progression No apparent aging changes
Diagnostics to Late AMD: Oral vitamins (Vit C and Vit E),
lens takes up water Intumescent Cataract Ophthalmoscopy
Antioxidants (Beta-carotene), Zinc, Copper
Digital Palpation Normal aging changes No drusen and no pigmentary abnormalities
cortical proteins have become liquid Hypermature Cataract
RAPD Treatment of Neovascular AMD:
hypermature cataract in which the lens
Morgagnian Cataract Bevacizumab, Ranibizumab, Aflibercept Early AMD Only small drusen (drupelets) and no
nucleus floats freely in the capsular bag
Visual acuity pigmentary abnormalities
Color vision Intermediate AMD Medium drusen and no pigmentary
Treatment abnormalities
Moderate or high-risk patient Visual field testing
Late AMD Large drusen and/or any pigmentary
IOP > 21 mmHg Ophthalmoscopy Based on clinical judgement + Patient's abnormalities
visual acuity and assessment of interference
IOP not elevated, but a difference of 5 of ADLs Neovascular AMD and/or geographic atrophy
mmHg or more between both eyes
Optic disc color
Optic cup diameter one half or more of the Refer to an ophthalmologist if Cataract Surgery
Optic disc size
disc diameter (cup:disc ratio of 0.5 or
greater)
Vessel displacement
One cup significantly larger in one eye than
in the other Glaucomatous cupping
Symptoms of acute glaucoma Temporal pallor of the ON
Papilledema
Reduced or obliterated cup
Tonometry
Perimetry
Gonioscopy
You might also like
- Prophecy Neuro ICU Exam Content OutlineDocument5 pagesProphecy Neuro ICU Exam Content OutlineDarren DawkinsNo ratings yet
- Osteopathic Considerations in Systemic Dysfunction (2nd Ed)Document296 pagesOsteopathic Considerations in Systemic Dysfunction (2nd Ed)Natan Babek100% (1)
- GLAUCOMA Revised Concept MapDocument5 pagesGLAUCOMA Revised Concept MapJanselle H ArmaNo ratings yet
- EOE Diplopia Flow-ChartDocument1 pageEOE Diplopia Flow-ChartPaulaNo ratings yet
- Cataract Week 13Document9 pagesCataract Week 13Janselle H ArmaNo ratings yet
- Woc Trauma MataDocument4 pagesWoc Trauma MataChairunnisa Permata SariNo ratings yet
- Special Senses) 3. Photoreceptors - Rods and Cones - KeyDocument1 pageSpecial Senses) 3. Photoreceptors - Rods and Cones - Keyranag59100No ratings yet
- EmergenciesDocument16 pagesEmergenciesJack Ortega PuruggananNo ratings yet
- VisualDocument1 pageVisualGeraldine TeneclanNo ratings yet
- Notes On Meniere's DiseaseDocument5 pagesNotes On Meniere's DiseaseDipson HamalNo ratings yet
- EGurukul GlaucomaDocument15 pagesEGurukul GlaucomaOscar Daniel Mendez100% (1)
- Reniyasw: Ioptnlnosnsisunwnsionlsngdngims VioovyDocument3 pagesReniyasw: Ioptnlnosnsisunwnsionlsngdngims Vioovyวชิรพล คำแก้วNo ratings yet
- Disseminated Intravascular CoagulationDocument1 pageDisseminated Intravascular CoagulationAnn Justine OrbetaNo ratings yet
- Glaucoma: AetiologyDocument3 pagesGlaucoma: Aetiologyjames cordenNo ratings yet
- EGurukul - RetinaDocument23 pagesEGurukul - RetinaOscar Daniel Mendez100% (1)
- ARRYTHMIASDocument3 pagesARRYTHMIASitstheboyjayyNo ratings yet
- Benign Prostatic HyperplasiaDocument1 pageBenign Prostatic HyperplasiaAli SafaaNo ratings yet
- Augenheilkunde FragenDocument3 pagesAugenheilkunde FragenWise AmroNo ratings yet
- OphthalmologyDocument143 pagesOphthalmologyOscar Daniel Mendez100% (1)
- Bells PalsyDocument5 pagesBells PalsydeasyNo ratings yet
- PHA 618: Human Physiology and Pathophysiology Cardiovascular ExercisesDocument2 pagesPHA 618: Human Physiology and Pathophysiology Cardiovascular Exerciseskaila lunaNo ratings yet
- CNS PathologyDocument1 pageCNS Pathologydr.rohit9098No ratings yet
- Doping Pada OlahragaDocument4 pagesDoping Pada OlahragaAlya ArnoldNo ratings yet
- Lov AssignmentDocument1 pageLov AssignmentfaamcxclepiaNo ratings yet
- General Surgery 5Document19 pagesGeneral Surgery 5MaggieNo ratings yet
- ESRD PathoDocument1 pageESRD PathoPrecious VernalNo ratings yet
- Med Surg Notes 4Document11 pagesMed Surg Notes 4trashhhtineNo ratings yet
- Forensic MedicineDocument60 pagesForensic MedicineKoushal Sharma, JammuNo ratings yet
- Glaucoma: DR - Fitratul Ilahi, SPM (K)Document47 pagesGlaucoma: DR - Fitratul Ilahi, SPM (K)nurul ramadhiniNo ratings yet
- Pathophysiology: ThinningDocument1 pagePathophysiology: ThinningArwaNo ratings yet
- Safe FESS To Avoid Complication: CT-scan InterpretationDocument33 pagesSafe FESS To Avoid Complication: CT-scan InterpretationBebekNo ratings yet
- Materi Bimbingan Kepaniteraan Klinik Ilmu Penyakit Mata: No Pembimbing Topik Sub TopikDocument2 pagesMateri Bimbingan Kepaniteraan Klinik Ilmu Penyakit Mata: No Pembimbing Topik Sub TopikRizka ChairaniNo ratings yet
- ulcers ملخصDocument2 pagesulcers ملخصmohamed awaadNo ratings yet
- MRI and X-Ray ImagingDocument6 pagesMRI and X-Ray ImagingbeatriceosNo ratings yet
- CICUTA VIROSA (Cic)Document1 pageCICUTA VIROSA (Cic)mohd18160No ratings yet
- Optha RevisionDocument38 pagesOptha Revisionpriyanka chikotiNo ratings yet
- Arthroscopic Repair of Dorsal Radiocarpal Ligament Tear - Report of Four CasesDocument1 pageArthroscopic Repair of Dorsal Radiocarpal Ligament Tear - Report of Four CasesKamijou-sanNo ratings yet
- S3-04 Ophthalmology Chronic Vision Loss PDFDocument12 pagesS3-04 Ophthalmology Chronic Vision Loss PDFAl SyNo ratings yet
- Diencephalon, Brainstem & CerebellumDocument1 pageDiencephalon, Brainstem & CerebellumwinNo ratings yet
- Case Study: Object PhotosDocument8 pagesCase Study: Object PhotosDiwanNo ratings yet
- Haemorrhoids: Acute PresentationsDocument1 pageHaemorrhoids: Acute PresentationsMuhammad AkhyarNo ratings yet
- Eye Anatomy (R)Document3 pagesEye Anatomy (R)Nikster LuNo ratings yet
- Winslow PathwayDocument3 pagesWinslow PathwayMia MadalinaNo ratings yet
- MSK W4 Lec 6Document20 pagesMSK W4 Lec 6sharon christieNo ratings yet
- Common Indications For Gadolinium (MR Contrast) in MRIDocument2 pagesCommon Indications For Gadolinium (MR Contrast) in MRId dNo ratings yet
- Pain PerceptionDocument3 pagesPain PerceptionCarlos RodriguezNo ratings yet
- EpitheliumDocument1 pageEpitheliumhawdeng xalitNo ratings yet
- All-CVS HematologyDocument8 pagesAll-CVS HematologyRitika AgrawalNo ratings yet
- Note 17 Nov 2022Document19 pagesNote 17 Nov 2022Raghad RNo ratings yet
- MindMap Butterfly Anna-MariyaDocument1 pageMindMap Butterfly Anna-MariyaAnna-Maria LevenovaNo ratings yet
- Vitals: Stridor (Upper Airway Obstruction), Use of Acc. Muscles, DroolingDocument1 pageVitals: Stridor (Upper Airway Obstruction), Use of Acc. Muscles, DroolingSean LamNo ratings yet
- Ar 706Document1 pageAr 706Victor YeoNo ratings yet
- Pathophysio CRF2 - RevisedDocument1 pagePathophysio CRF2 - Reviseddeborah malnegroNo ratings yet
- GlaucomaDocument23 pagesGlaucomasnivetha96No ratings yet
- NystagmusDocument1 pageNystagmusArwa100% (1)
- Diagrams of EyeballDocument7 pagesDiagrams of EyeballHelworNo ratings yet
- Self-Declaration by TCS Associates Resuming OfficeDocument2 pagesSelf-Declaration by TCS Associates Resuming OfficeAlamuru SrinidhiNo ratings yet
- Antimicrobial Approach To Intra-Abdominal Infections in Adults - UpToDateDocument29 pagesAntimicrobial Approach To Intra-Abdominal Infections in Adults - UpToDatecontateste197789No ratings yet
- Drug StudyDocument7 pagesDrug StudyCarson BirthNo ratings yet
- Vitiligo A Review 2020 PDFDocument22 pagesVitiligo A Review 2020 PDFhannah khumairahNo ratings yet
- Intellectual Disability: Menchie M. Garachico Freddie C. Santos JRDocument42 pagesIntellectual Disability: Menchie M. Garachico Freddie C. Santos JRTEAM SPORTS GADTCNo ratings yet
- Hirac Installation Panel FPV SubstationDocument3 pagesHirac Installation Panel FPV SubstationekapadwiNo ratings yet
- Sr. No.3, Laxmi Nagar, Lane No.8, Near Paratibhtai School, Kondhwa BK, Pune - 48 Self - Bike NO NO NO NO NO NODocument6 pagesSr. No.3, Laxmi Nagar, Lane No.8, Near Paratibhtai School, Kondhwa BK, Pune - 48 Self - Bike NO NO NO NO NO NORamNo ratings yet
- Phenytoin: Phenytoin (PHT), Sold Under The Brand Name Dilantin AmongDocument13 pagesPhenytoin: Phenytoin (PHT), Sold Under The Brand Name Dilantin AmongMunna SahaniNo ratings yet
- New Study in Candida InfectionsDocument3 pagesNew Study in Candida InfectionsHenz FreemanNo ratings yet
- Pathophysiology of FeverDocument4 pagesPathophysiology of FeverEasha Jamil AbbasiNo ratings yet
- Ni 2021 69 6 1524 333440Document18 pagesNi 2021 69 6 1524 333440Krit KritNo ratings yet
- Oet 2 PDFDocument96 pagesOet 2 PDFSharika SayedNo ratings yet
- Multiple Endocrine NeoplasiaDocument10 pagesMultiple Endocrine NeoplasiacarmenNo ratings yet
- Orbital Cellulitis 2018Document20 pagesOrbital Cellulitis 2018María Alejandra Rojas MontenegroNo ratings yet
- An MRIDocument41 pagesAn MRIAsim AliNo ratings yet
- Endoscope Reprocessing Risk and Current Risk PracticeDocument65 pagesEndoscope Reprocessing Risk and Current Risk PracticeHosam GomaaNo ratings yet
- Prolonged StandingDocument2 pagesProlonged StandingMadalena CrespoNo ratings yet
- Psychiatric BookDocument268 pagesPsychiatric BookFan Eli100% (2)
- Cilia 2018Document1 pageCilia 2018Anna Beatriz Silva EspindolaNo ratings yet
- Polycythemia Vera: What Are The Symptoms of Polycythemia?Document10 pagesPolycythemia Vera: What Are The Symptoms of Polycythemia?Dimpal ChoudharyNo ratings yet
- 7 - Common Psychiatric Problems - Mubarak-SubaieDocument62 pages7 - Common Psychiatric Problems - Mubarak-SubaieLavitSutcharitkulNo ratings yet
- Revlimid Epar Medicine Overview - en PDFDocument4 pagesRevlimid Epar Medicine Overview - en PDFManju JNo ratings yet
- Death Claim Checklist 2017Document4 pagesDeath Claim Checklist 2017Cheche GonzalesNo ratings yet
- CarbimazoleDocument3 pagesCarbimazoleManish SharmaNo ratings yet
- Sade, Robert M. 2012 "The Graying of America Challenges and ControversiesDocument8 pagesSade, Robert M. 2012 "The Graying of America Challenges and ControversiesTengiz VerulavaNo ratings yet
- Exam 1 Practice QuestionsDocument31 pagesExam 1 Practice QuestionsJoslyn Gross0% (1)
- COVID-19 Shipboard Contingency Plan - Rev.1 - FULL VERSION - UPDATED 24.05.2020 PDFDocument88 pagesCOVID-19 Shipboard Contingency Plan - Rev.1 - FULL VERSION - UPDATED 24.05.2020 PDFbuzbonNo ratings yet
- ELEMENTS OF CHILD DEVELOPMENT - SplitDocument97 pagesELEMENTS OF CHILD DEVELOPMENT - SplitIndian learnerNo ratings yet