Professional Documents
Culture Documents
Phenylketonuria and Cystinuria
Phenylketonuria and Cystinuria
Uploaded by
mehrinOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Phenylketonuria and Cystinuria
Phenylketonuria and Cystinuria
Uploaded by
mehrinCopyright:
Available Formats
Phenylketonuria
General description of the disease
Phenylketonuria (PKU) is an autosomal recessive metabolic genetic disorder characterized by a mutation in the
gene for the hepatic enzyme phenylalanine hydroxylase (PAH), rendering it nonfunctional.
This enzyme is necessary to metabolize the amino acid phenylalanine(Phe) to the amino acid tyrosine.When PAH
activity is reduced, phenylalanine accumulates and is converted into phenylpyruvate (also known as
phenylketone), which can be detected in the urine.
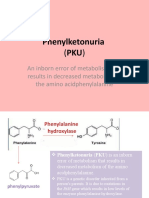
The enzyme phenylalanine hydroxylase (in the presence of co-factor tetrahydrobiopterin bh4) ormally converts the
amino acid phenylalanine into the amino acid tyrosine.
o If this reaction does not take place, phenylalanine accumulates and tyrosine is deficient
o excessive phenylalanine can be metabolized into phenylketones through the minor route, a transaminase pathway with glutamate.
Metabolites and diagnostic criteria
Metabolites include phenylacetate, phenylpyruvate and phenethylamine.
Elevated levels of phenylalanine in the blood and detection of phenylketones inthe urine is diagnostic, however most patients are
diagnosed via newborn screening.
PKU and Brain disability
Phenylalanine is a large, neutral amino acid .
LNAAs compete for transport across the blood– brain barrier via the large neutral amino acid transporter . If phenylalanine is in excess in
the blood, it will saturate the transporter. Excessive levels of phenylalanine tend to decrease the levels of other LNAAs in the brain.
However, as these amino acids are necessary for protein and neurotransmitter synthesis, Phe buildup hinders the development of the
brain, causing intellectual disability.
Normal (a&b) and abnormal (c) metabolism in phenylketonuric subjects
Levels of blood
phenylalanine
A normal blood phenylalanine level is about 1mg/dl.
In cases of pku, levels may range from 6- 80mg/dl, but are usually greater than 30mg/dl.
Symptoms
Chronically, high levels of phenylalanine and some of its breakdown products can cause
o Significant brain problems.
o There are other disorders of hyperphenylalaninemia, but classic PKU is the most common
cause of high levels of Phenylalanine in the blood
o Phenylalanine accumulates, causing rashes, seizures, hyperactivity, and mental retardation, if
untreated.
o Prominent cheek and jaw bones
o widely spaced teeth
o Poor development of tooth enamel.
o It is important to remember that some phenylalanine is needed to maintain normal body function.
o Insufficient phenylalanine intake may cause mental and physical sluggishness, loss of appetite, anemia, rashes, and diarrhea.
Heredity
A single mutant recessive allele of the Phenylalanine Hydroxylase (PAH)gene
Location : Long arm of Chromosome 1 2 -locus 22.
PAH only allow a tolerance of 20 mg/kg/day.
Missense mutations and deletions.
Dietary excess of plant proteins which results in the exhaustion of a protein cofactor
Tetrahydrobiopterin BH4 needed by the enzyme.
o Two people who conceive a child must both be the carriers of the defective gene
inorderfortheirchildtohavethe disorder.
o The “carrier” for pku does not have the symptoms.
Pregnancy and PKU
It is recommended that women with PKU who are of child bearing age, closely adhere to the
low-phenylalanine levels before conception and throughout pregnancy. The risk of
miscarriage, mental retardation, microcephaly, and congenital heart disease in the child is high if the mother’s blood phenylalanine is
poorly controlled.
Screening test
GUTHERIA
Usually a few drops of blood are obtained by a small prick on the heel, placed on
a card and then sent for measurement.
Newborn screening allows early identification and early implementation of
treatment.
All babies are screened for pku by heel- prick test. Blood tested for excess
phenylalanine.
Blood placed on agar plate with bacteria that need phenylalanine to grow.
Healthy babies’ blood doesn’t have extra phenylalanine, so bacteria can’t grow.
Babies with PKU have extra phenylalanine, so bacteria grow.
Ferric chloride +urine of new born baby Green colour in the presence of
ketone bodies.
Astrictly controlled phenylalanine free diet upto the age of about 14 years old
Phenylalanine is itself an essential amino acid small doses must besupplied.
After 14 years, the growth and development of the brain is not affected by high levels of phenylalanine in the body.
Treatment
Individuals with PKU must be alert for food sweetened with aspartame - artificial sweetener made from amino acids phenylalanine and
aspartic acid.
If PKU goes untreated or undetected, severe brain problems occur such as seizures and mental retardation.
More frequent Dr visits
Required dietary restrictions that may impact day today activities
Permanent monitoring of blood phenylalanine levels
Cystinuria
General description of the disease
Cystinuria is an autosomal-recessive defect in reabsorptive transport of cystine and the dibasic amino acids ornithine, arginine, and
lysine from the luminal fluid of the renal proximal tubule and small intestine. The only phenotypic manifestation of cystinuria is cystine
urolithiasis (kidney stones90
o 1 in 7000 births
Presentation
o 1-2% of all stone formers
Presentation is similar to that of other types of
renal calculi and includes renal colic, chronic
o Up to 5% in pediatric stone formers
urinary tract infections in a young person with a
family history of renal stones, passage of stones
Pathophysiology or gravel, hematuria, and dysuria.
Renal transport of cystine
o Amino acids filtered undergo nearly complete reabsorption by proximal tubular cells.
o Only 0.4% of the filtered cystine appears in the urine.
Intestinal transport of cystine
The high-affinity transporter is present in the apical brush-border membrane of the jejunum and is responsible for absorption of cystine
and dibasic amino acids.
Normally, cystine and the other dibasic amino acids (ie, ornithine, lysine, arginine) are filtered at the glomerulus and reabsorbed in the
proximal convoluted tubule
Defects in this channel cause elevated levels of dibasic amino acid secretion in the urine.
Whereas ornithine, lysine, and arginine are completely soluble, cystine is relatively insoluble at physiologic urine pH levels of 5-7
Diagnosis
Positive family history of cystinuria
Stone analysis showing cystine
Identification of pathognomonic hexagonal cystine crystals on urinalysis
A positive cyanide-nitroprusside screen indicates a urinary cystine concentration >75 mg/L
Quantitative 24-h urinary cystine excretion more than 30 mg/day are considered abnormal
Treatment
The aim of medical therapy is to maintain the cystine concentration in the
urine below its solubility level
Solubility of cystine in urine from 175 to 360 mg/L ≈ about 243 mg/L avoiding cystine crystallisation is to maintain urine pH
between 7.5. and 8.5
High fluid intake
Sodium and protein restriction
Urinary alkalinization
Surgical procedures
Large calculi that are unlikely to dissolve
Obstructing or otherwise symptomatic calculi.
The ultimate goal of surgery is to make the patient free of stones. While the risk of recurrence is unchanged
You might also like
- Instant Download Connect Core Concepts in Health Brief 16th Edition Ebook PDF PDF ScribdDocument41 pagesInstant Download Connect Core Concepts in Health Brief 16th Edition Ebook PDF PDF Scribdcarmine.adams474100% (47)
- Phenylketonuria (PKU) : PH Arn, Nemours Children's Clinic, Jacksonville, FL, USADocument3 pagesPhenylketonuria (PKU) : PH Arn, Nemours Children's Clinic, Jacksonville, FL, USAHappy612No ratings yet
- FWD Producst: Products For AllDocument44 pagesFWD Producst: Products For AllCharish DanaoNo ratings yet
- Subclinical Hypothyroidism TDocument6 pagesSubclinical Hypothyroidism TAnisa Iswari Pombaile-NgurawanNo ratings yet
- Approach To Differential Diagnosis PDFDocument62 pagesApproach To Differential Diagnosis PDFanasNo ratings yet
- PkuDocument6 pagesPkuAlbertEscanoNo ratings yet
- PhenylketonuriaDocument8 pagesPhenylketonuriaAmberlee PetiNo ratings yet
- Phenylketonuria: Abbas A. A. Shawka Medical Student 2 GradeDocument24 pagesPhenylketonuria: Abbas A. A. Shawka Medical Student 2 GradeAsfoor gake1No ratings yet
- Inborn Errors of MetabolismDocument60 pagesInborn Errors of MetabolismPyneandy KimberlyNo ratings yet
- PhenylketonuriaDocument17 pagesPhenylketonuriamovies villa hit hai broNo ratings yet
- Biochemistry - METABOLISM OF PROTEINDocument44 pagesBiochemistry - METABOLISM OF PROTEINrebeccaNo ratings yet
- PHENYLKETONURIADocument22 pagesPHENYLKETONURIAIvy Ann AguirreNo ratings yet
- Inborn Errors of MetabolismDocument40 pagesInborn Errors of MetabolismajjaNo ratings yet
- Endocrine DisordersDocument33 pagesEndocrine DisordersTinaNo ratings yet
- Inborn Errors of Metabolism Student LectureDocument81 pagesInborn Errors of Metabolism Student LectureFavourNo ratings yet
- Endocrine DisordersDocument33 pagesEndocrine DisordersBuvana VigneshNo ratings yet
- PhenylketonuriaDocument7 pagesPhenylketonuriaAnny AlvrzNo ratings yet
- PhenylketonuriaDocument7 pagesPhenylketonuriaReham QueNo ratings yet
- Clinical FirstDocument342 pagesClinical FirstYasmeen AtiehNo ratings yet
- Aminoacid MetabolismDocument25 pagesAminoacid MetabolismMischief ManagerNo ratings yet
- 23 Pku AkuDocument1 page23 Pku AkuJose DolletonNo ratings yet
- Fenilketonuria: Devi WuysangDocument23 pagesFenilketonuria: Devi WuysangChristantina Pradescha AssaNo ratings yet
- Phenylketonur IA: Done byDocument27 pagesPhenylketonur IA: Done byAsfoor gake1100% (1)
- DR Kumar Ponnusamy Biochemistry Genetics USMLE Preparatory Course BIOGEN Reusable On Line Resources For Large Group Teaching Learning in Relatively SHDocument2 pagesDR Kumar Ponnusamy Biochemistry Genetics USMLE Preparatory Course BIOGEN Reusable On Line Resources For Large Group Teaching Learning in Relatively SHPonnusamy KumarNo ratings yet
- Phenylketonuria: An Inborn Error of Metabolism That Results in Decreased Metabolism of The Amino AcidphenylalanineDocument8 pagesPhenylketonuria: An Inborn Error of Metabolism That Results in Decreased Metabolism of The Amino Acidphenylalanineელენე ბუჩუკურიNo ratings yet
- Munyame 2018Document6 pagesMunyame 2018kemoNo ratings yet
- PHENYLKETONURIADocument3 pagesPHENYLKETONURIAMiwa IshiiNo ratings yet
- DR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDocument1 pageDR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDr Kumar Ponnusamy100% (1)
- Articulo Final Verdadero!!!!Document6 pagesArticulo Final Verdadero!!!!lapzsssNo ratings yet
- Inborn Errors of Amino Acid Metabolism: (Advanced Nutrition)Document8 pagesInborn Errors of Amino Acid Metabolism: (Advanced Nutrition)Deepshikha PatelNo ratings yet
- Inborn Error of MetabolismDocument38 pagesInborn Error of MetabolismRubinaNo ratings yet
- Inherited Metabolic DisorderDocument12 pagesInherited Metabolic DisorderTrisha Dianne RaquenioNo ratings yet
- PhenylketonuriaDocument1 pagePhenylketonuriaHolly SevillanoNo ratings yet
- Phenyl Keto NuriaDocument3 pagesPhenyl Keto NuriawawawawaNo ratings yet
- MCH Group 8Document12 pagesMCH Group 8nafisatmuhammed452No ratings yet
- Phenylketonuria (PKU) : Diagnosis and ManagementDocument2 pagesPhenylketonuria (PKU) : Diagnosis and ManagementFerdianaNo ratings yet
- PhenylketonuriaDocument14 pagesPhenylketonuriaMonica MoralesNo ratings yet
- Inborn Error of Metabolism and Introduction To Cancer GeneticsDocument9 pagesInborn Error of Metabolism and Introduction To Cancer GeneticsviancaNo ratings yet
- Case3 PhenylketunuriaDocument2 pagesCase3 PhenylketunuriaKath BoniolNo ratings yet
- Urinalysis 2Document9 pagesUrinalysis 2Dawn GonzagaNo ratings yet
- Phenylketonuria (PKU) : (Metabolic Condition: Amino Acid Disorder)Document1 pagePhenylketonuria (PKU) : (Metabolic Condition: Amino Acid Disorder)reriti2008No ratings yet
- Phenylketonuria: Symposium: Inborn Errors of MetabolismDocument5 pagesPhenylketonuria: Symposium: Inborn Errors of MetabolismIntan RizanaNo ratings yet
- Unit 6 TransDocument8 pagesUnit 6 TransGrace FernandoNo ratings yet
- Pediatrics ReviewDocument275 pagesPediatrics ReviewHaslinNo ratings yet
- Amino Acid DisordersDocument7 pagesAmino Acid DisordersarshehadaNo ratings yet
- Group 4 - Pku (BSN 1-A)Document11 pagesGroup 4 - Pku (BSN 1-A)oluanah13No ratings yet
- Common IEM Solaf M Elsayed 2021Document13 pagesCommon IEM Solaf M Elsayed 2021anas barakahNo ratings yet
- Bio Chem Case ThreeDocument2 pagesBio Chem Case ThreeLeonard Rey Suratos ManabatNo ratings yet
- Inborn Errors of Metabolism: Albinism, Cystinuria, Pentosuria And, of Course, AlkaptonuriaDocument19 pagesInborn Errors of Metabolism: Albinism, Cystinuria, Pentosuria And, of Course, AlkaptonuriaSubhi MishraNo ratings yet
- Recurrent Kidney Stones in A Child With Lesch-Nyhan Syndrome: AnswersDocument3 pagesRecurrent Kidney Stones in A Child With Lesch-Nyhan Syndrome: AnswersAriani SetianingsihNo ratings yet
- Metabolic Disorders 01Document41 pagesMetabolic Disorders 01Brent LagartoNo ratings yet
- PHENYLKETONURIADocument4 pagesPHENYLKETONURIAmarsiel03No ratings yet
- AUBF Metabolic Disorders and Inborn Error of MetabolismDocument3 pagesAUBF Metabolic Disorders and Inborn Error of MetabolismAngela LaglivaNo ratings yet
- USMD, CSF, SEMEN - Professor'sDocument10 pagesUSMD, CSF, SEMEN - Professor'sMartin ClydeNo ratings yet
- PhenylketonuriaDocument10 pagesPhenylketonuriaMalathy Ravendran100% (1)
- Inborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Document4 pagesInborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Wen Jie LauNo ratings yet
- Aub F Urine Screening For Metabolic DisordersDocument4 pagesAub F Urine Screening For Metabolic DisordersRomie SolacitoNo ratings yet
- Vii. Urine Screening For Metabolic DisordersDocument4 pagesVii. Urine Screening For Metabolic DisordersDee GeeNo ratings yet
- Biochemistry & Genetics Important Concepts Q&as DR Kumar Ponnusamy & Jegathambigai RN, Biochemistry & Genetics, International Medical University (IMU) / AIMST University School of Medicine, MalaysiaDocument60 pagesBiochemistry & Genetics Important Concepts Q&as DR Kumar Ponnusamy & Jegathambigai RN, Biochemistry & Genetics, International Medical University (IMU) / AIMST University School of Medicine, MalaysiaDr Kumar Ponnusamy100% (3)
- Phenyl Keto NuriaDocument1 pagePhenyl Keto NuriamucwcburdwanNo ratings yet
- Metabolic DisordersDocument80 pagesMetabolic DisordersXeniyaFedoryakNo ratings yet
- Hypophosphatemia, (Low Phosphate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHypophosphatemia, (Low Phosphate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Blondin-Brosseau Et Al 2021Document28 pagesBlondin-Brosseau Et Al 2021JefersonMatosdeColaresNo ratings yet
- Physiotherapy Management: Otago Home Exercise ProgrammeDocument9 pagesPhysiotherapy Management: Otago Home Exercise ProgrammeanjelikaNo ratings yet
- Name of The Drug Mechanism of Action Dosage Indications Contraindications Adverse Reaction Nursing InterventionDocument4 pagesName of The Drug Mechanism of Action Dosage Indications Contraindications Adverse Reaction Nursing InterventionMary joy PaaNo ratings yet
- Disorders of The Endocrine SystemDocument12 pagesDisorders of The Endocrine SystemAlfred Jayson RuizNo ratings yet
- Paediatrics Workbook - Nuc304: SUMMER 2021Document10 pagesPaediatrics Workbook - Nuc304: SUMMER 2021Rawan KhateebNo ratings yet
- DecombDocument3 pagesDecombDr.2020No ratings yet
- Research Paper 4Document15 pagesResearch Paper 4api-548795523No ratings yet
- Acutescrotalemergencies: Molly M. Bourke,, Joshua Z. SilverbergDocument18 pagesAcutescrotalemergencies: Molly M. Bourke,, Joshua Z. SilverbergSebastian ChavesNo ratings yet
- Research Proposal FinalDocument35 pagesResearch Proposal FinalBienne Zyrus Earl CarpioNo ratings yet
- Principles of Inheritance and Variation - Revision WorksheetDocument5 pagesPrinciples of Inheritance and Variation - Revision Worksheetafsheenfatima2006No ratings yet
- Hyper Hyponatremia LERMADocument8 pagesHyper Hyponatremia LERMAJINYVEV APARICINo ratings yet
- Final SK Golden 7+8 ErrataDocument19 pagesFinal SK Golden 7+8 ErrataHassam ZulfiqarNo ratings yet
- Troponin Elevation in Coronary Vs Non Coronary DiseaseDocument10 pagesTroponin Elevation in Coronary Vs Non Coronary Diseasealejandro montesNo ratings yet
- HYPERMETROPIA and Myopia PDFDocument55 pagesHYPERMETROPIA and Myopia PDFDrashti ChudasamaNo ratings yet
- Week 13 CD COURSE TASK 7. Dengue Fever, Filariasis, Malaria and EncephalitisDocument5 pagesWeek 13 CD COURSE TASK 7. Dengue Fever, Filariasis, Malaria and EncephalitisRogelyn PatriarcaNo ratings yet
- History of Disease & Levels of Prevention 2Document39 pagesHistory of Disease & Levels of Prevention 2Nadine VillaretNo ratings yet
- Blueprints PsychiatryDocument432 pagesBlueprints PsychiatryFiona Fleming87% (15)
- Focal Segmental Glomerulosclerosis: State-of-the-Art and Clinical PerspectiveDocument15 pagesFocal Segmental Glomerulosclerosis: State-of-the-Art and Clinical PerspectiveGabriela CruzNo ratings yet
- AAMA - Anatomy and Physiology QuestionsDocument11 pagesAAMA - Anatomy and Physiology QuestionsHUAWEI HUAWEINo ratings yet
- Forensic PsychiatryDocument52 pagesForensic PsychiatrySiow Siow0% (1)
- Measuring The Occurrence of Disease: Dr. Elijah Kakande MBCHB, MPH Department of Public HealthDocument25 pagesMeasuring The Occurrence of Disease: Dr. Elijah Kakande MBCHB, MPH Department of Public HealthNawita JordanNo ratings yet
- Lumbar RadiculopathyDocument16 pagesLumbar Radiculopathyprince singhNo ratings yet
- GI BleedingDocument17 pagesGI BleedingBảo LongNo ratings yet
- Practical Paper 2Document32 pagesPractical Paper 2Ashika AshuNo ratings yet
- Trigemina Nerve Sem 2 WordDocument18 pagesTrigemina Nerve Sem 2 WordBharathi GudapatiNo ratings yet
- Dipiro PneumoniaDocument8 pagesDipiro Pneumoniameri dayaniNo ratings yet