Professional Documents
Culture Documents
TBM HCP
TBM HCP
Uploaded by
MogiMediawanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TBM HCP
TBM HCP
Uploaded by
MogiMediawanCopyright:
Available Formats
http://www.pediatriconcall.
com
TEACHING FILE
GRAND ROUNDS
Ira Shah
SPACE OCCUPYING LESION IN THE BRAIN- fluid examination was done which
WHAT IS IT? grew mycobacterium tuberculosis
on culture, thus confirming the
Case: A 7 years old boy presented with fever and
diagnosis.
headache for 1 month, projectile vomiting for 15 days
and altered sensorium for 1 day. There was no contact DOI No.: 10.7199/ped.
with a patient having tuberculosis. On examination, oncall.2016.38
he had signs of raised intracranial tension. An MRI
brain was done HOW TO TREAT CONGENITAL SYPHILIS WHEN
that showed AQUEOUS PENICILLIN IS NOT AVAILABLE?
obstructive
Case: A 3 days old baby is diagnosed to have
lateral ventricle
congenital syphilis on testing with VDRL. The child is
hydrocephalus
asymptomatic and had normal birth with birth weight
with irregularly
of 3kg. Cerebrospinal fluid (CSF) VDRL is negative.
s h a p e d
Injectable crystalline penicillin and procaine penicillin
heterogeneously
is not available.
enhancing
periventricular How should this child be treated?
masses in the Expert’s opinion: Congenital syphilis, either proved
antero-mesial or presumed, is treated with a 10-day course of
aspects of both temporal lobes and in medial aspect of aqueous penicillin G (100,000–150,000 U/kg/day,
right occipital lobe with areas of vasogenic edema and administered as 50,000 U/kg/dose, intravenously,
leptomeningeal enhancement. A differential diagnosis every 12 hours during the first 7 days of life and every
of tuberculoma or a neoplasm was considered. The 8 hous thereafter for a total of 10 days) or procaine
child’s condition was too unstable to do a lumbar penicillin G (daily single dose of 50 000 U/kg/day,
puncture. A neurosurgery opinion was taken regarding intramuscularly for 10 days). In case of shortage of
biopsy of the lesion but was not considered, again due aqueous penicillin, CDC recommends that some or
to unstable condition of the child. all daily doses should be substituted with procaine
penicillin G (50,000 U/kg/dose IM a day in a single dose
How to differentiate between tuberculoma and
for 10 days). If both aqueous or procaine penicillin G
other space occupying lesions?
are not available, ceftriaxone may be considered with
Expert’s opinion: MRI is frequently performed in
careful clinical and serologic follow-up. Ceftriaxone
patients suspected to have central nervous system
must be used with caution in jaundiced infants. For
space occupying lesions to help in differentiating
infants = 30 days old, it is given in dose of 75 mg/kg
tuberculoma and other causes. Sometimes, MRI
IV or IM/day in a single dose for 10-14 days. For older
features are similar and usually not useful for
infants, this dose should be 100 mg/kg/day in a single
differentiation. MR spectroscopy (MRS) helps to
dose. Studies that strongly support ceftriaxone for the
differentiate tuberculoma from other infective
treatment of congenital syphilis have not been done. In
granulomas. While the MRI uses signals from hydrogen
case of abnormal CSF examination at the beginning, a
protons to form anatomic images, the proton MRS
repeat CSF exam at 6 months of age if the initial exam
uses this information to determine the concentration
was abnormal is recommended. (1)
of brain metabolites such as N-acetyl aspartate
In patients, if the diagnosis of congenital syphilis is not
(NAA), choline (Cho), creatine (Cr), and lactate in
completely established, then benzathine penicillin G,
the tissue examined. MRS of brain tuberculomas
50,000 U/kg IM as a single dose can be used.
commonly detects peaks of lipids attributable to
Treated infants should be followed-up at 3, 6 and
large lipid fractions in tuberculosis bacillus. It will also
12 months of age, until serologic non-treponemal
have increased choline levels and decreased N acetyl
tests become non-reactive or the titre has decreased
aspartate and creatine levels. The choline, creatine
fourfold. With adequate treatment or in cases in which
ratio is greater than 1 in tuberculomas. (1)
antibody is transplacentally acquired in the absence
In our patient, MRS was done and samples from the
of congenital infection, non-treponemal antibody
right occipital lobe lesion were taken and compared
titres should decrease by 3 months of age and be
with the normal right frontal parenchyma. In the
non- reactive by 6 months of age. Previously treated
occipital lesion, there was increase in choline relative
infants at 6–12 months of age with increasing or
to creatine and NAA. There was a lactate-lipid peak
persistent titres should be re-evaluated, including CSF
between 1.49 and 1.28 ppm suggestive of tuberculoma.
examination, and treated with a further 10-day course
The child was started on steroids and anti-tuberculous
of if the results are abnormal.
therapy. Once his condition stabilized, a cerebrospinal
Pediatric Oncall Journal July - September 2016. Volume 13 Issue 3 81
http://www.pediatriconcall.com
References The criteria for performing VP Shunt are CSF
1. CDC. 2002 CDC Sexually Transmitted polymorphs less than 5 cells/cumm, CSF protein less
Diseases Treatment Guidelines. MMWR than 100 mg/dl with evidence of hydrocephalus on CT
2002 ;51 (RR-6):1-80. scan irrespective of the number of CSF lymphocytes.
In patients with Grade 1 and 2 based on Palur Grading
DOI No.: 10.7199/ped.oncall.2016.41
system (1) (Table 1), in presence of periventricular
edema on CT scan, shunt surgery may be required.
HYDROCEPHALUS IN TUBERCULOUS
For patients in Grade III, surgery may be performed
MENINGITIS?
either if external ventricular drainage causes an
Case: A 4 years old girl was referred as she had improvement in sensorium or without selection. As
been on antituberculous therapy (ATT) for past 2 per Palur et al, all patients in Grade IV should undergo
years 8 months. At age of 1 year 4 months, she external ventricular drainage and only those who show
was diagnosed as tuberculous meningitis (TBM) a significant change in their neurological status within
with hydrocephalus and was started on ATT and 24 to 48 hours of drainage, should have shunt surgery.
underwent ventriculoperitoneal (VP) shunt insertion. (1) However, recent studies have depicted that there
She was alright was next 6 months and at 2 years she may be improvement in patients with Grade 4 also
developed drowsiness with right sided hemiparesis. when VP shunt is inserted. (2,3)
A CT brain showed large granuloma anterior to brain
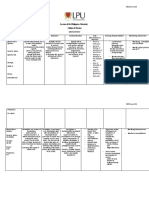
Table 1 : Palur grading system for need for shunt
stem causing upper cervical cord compression. She
in TBM (1)
was thus restarted on steroids which was given for
2 months. At 2 years 4 months, she developed an Grade Clinical Features Glasgow
encysted collection of fluid 16.4 x 13.9 cm underneath Coma
the anterior abdominal wall that required excision. At Scale
2 years 7 months of age she developed a peritoneal I No neurological deficit, normal 15
pseudocyst and hence VP shunt was removed and sensorium
a ventriculo-atrial (VA shunt) was put. Abdominal
II Neurological deficit present, 15
lymphnode biopsy was done at the same time where
normal sensorium
mycobacterium tuberculosis was isolated and 2 drugs
ATT consisting of Isoniazid (H), Rifampicin (R) were III Altered sensorium, easily 9-14
continued. At 3 years 4 months of age, MRI brain was arousable; neurological defici
done which showed substantial regression of confluent present or absent
granulomas in retroclivum region. At 3 years 10 months IV Deeply comatose; decerebrate 3-8
of age, she had headache and a fall following which or decorticate posturing present
VA shunt broke and again a VP shunt was reinserted. or absent
CT brain now showed disappearance of granuloma. At
4 years of age, at the time of referral, the child was References
asymptomatic, had normal milestones and no focal 1. Palur R, Rajshekhar V, Chandy MJ, Joseph T, Abraham J.
neurological deficit. Her weight was 14 kg, height was Shunt surgery for hydrocephalous in tubercular meningitis:
84.5 cm, head circumference was 46 cm. Her hearing A long-term follow up study. J Neurosurg 1991; 74: 64-69.
assessment, ophthalmological assessment was normal 2 . S r i k a n t h a U, M o ra b J V, S a s t r y S, A b ra h a m R ,
and EEG was also normal. Her ATT was thus stopped Balasubramaniam A, Somanna S, et al. Outcome of
and she was advised regular follow up. ventriculoperitoneal shunt placement in Grade IV
tubercular meningitis with hydrocephalus: a retrospective
Do all patients with TBM and hydrocephalus analysis in 95 patients. Clinical article. J Neurosurg Pediatr.
require a VP shunt? 2009;4(2):176-83.
3. Peng J, Deng X, He F, Omran A, Zhang C, Yin F, et al.
Expert Opinion : Hydrocephalus is the most common
Role of ventriculoperitoneal shunt surgery in grade IV
complication of TBM seen in up to 87 percent of patients.
tubercular meningitis with hydrocephalus. Childs Nerv
Early shunting with drugs therapy may offer the best
Syst. 2012;28:209-215
therapeutic outcome. Shunt surgery does not alter the
prognosis of stage III TBM as these patients usually DOI No. : 10.7199/ped.oncall.2016.31
have high mortality or are left with major disability like
mental retardation, hemiparesis or blindness. Shunt From: Medical Sciences Department, Pediatric Oncall,
surgery is indicated in patients who have failure of Mumbai.
medical management, or have TBM with hydrocephalus
Address for Correspondence Dr Ira Shah,
and uncontrolled raised intracranial pressure. Shunt 1/B Saguna, 271, B St Francis Road, Vile
prevents the development of subsequent visual Parle (W), Mumbai 400056.
deterioration. VP shunt is preferred as it can be done
in presence of active disease and early shunting with
anti-TB therapy improves outcome.
Pediatric Oncall Journal July - September 2016. Volume 13 Issue 3 82
You might also like
- Nurse Practitioner Board ReviewFrom EverandNurse Practitioner Board ReviewRating: 5 out of 5 stars5/5 (1)
- Neurological Examination What Do Psychiatrists Need To KnowDocument7 pagesNeurological Examination What Do Psychiatrists Need To Knowkaram aliNo ratings yet
- The Problem KneeDocument253 pagesThe Problem Kneedrbane100% (4)
- Journal Neuropediatri PDFDocument8 pagesJournal Neuropediatri PDFHalimah PramudiyantiNo ratings yet
- Untitled 4Document1 pageUntitled 4Giga HasabiNo ratings yet
- 09 2019 Pediatric Neonatology LAYOUT R2Document50 pages09 2019 Pediatric Neonatology LAYOUT R2khalid alharbiNo ratings yet
- EA VigaDocument5 pagesEA VigaMaria Gratzia OrdoñezNo ratings yet
- Encefalopatia Neonatal PDFDocument13 pagesEncefalopatia Neonatal PDFVanessa RomeroNo ratings yet
- Pituitary Tumour Apoplexy Within Prolactinomas in Children A More Aggressive ConditionDocument6 pagesPituitary Tumour Apoplexy Within Prolactinomas in Children A More Aggressive ConditionTony Miguel Saba SabaNo ratings yet
- Repeat 3Document3 pagesRepeat 3ntnquynhproNo ratings yet
- Ambispective Cohort StudyDocument9 pagesAmbispective Cohort StudyMãnoj MaheshwariNo ratings yet
- CorrespndenceDocument1 pageCorrespndenceTajul TajNo ratings yet
- A432 4 FullDocument2 pagesA432 4 FullArturo ArturoNo ratings yet
- Management and Investigation of Neonatal Encephalopathy: 2017 UpdateDocument13 pagesManagement and Investigation of Neonatal Encephalopathy: 2017 Updatenuge putriNo ratings yet
- Nuevas Curvas 2022Document6 pagesNuevas Curvas 2022rossanar147No ratings yet
- Northrop 2015Document4 pagesNorthrop 2015Annisa Badriyyah HakimahNo ratings yet
- Serum Prolactin Level in Children With Febrile Seizure and Epileptic Seizure Comparative StudyDocument5 pagesSerum Prolactin Level in Children With Febrile Seizure and Epileptic Seizure Comparative StudyjumrainiNo ratings yet
- Typhoid GuidelinesDocument3 pagesTyphoid GuidelinesMuthia Rahma AninditaNo ratings yet
- Analysis Blotting (Immunoblotting) Technique: of in Diagnosis of Congenital SyphilisDocument5 pagesAnalysis Blotting (Immunoblotting) Technique: of in Diagnosis of Congenital SyphilisDyahNo ratings yet
- Of The Asphyxiated Full Infant: ManagementDocument6 pagesOf The Asphyxiated Full Infant: Managementputri vinia /ilove cuteNo ratings yet
- Can Tey 2015Document4 pagesCan Tey 2015irenesmbNo ratings yet
- Desmopressin Stimulation Test in A Pregnant Patient - 2022 - AACE Clinical CaseDocument4 pagesDesmopressin Stimulation Test in A Pregnant Patient - 2022 - AACE Clinical CaseSameerNo ratings yet
- UntitledDocument9 pagesUntitledPurilarp Dao-aroonkietNo ratings yet
- p1348 PDFDocument2 pagesp1348 PDFElvia HarlenNo ratings yet
- Congenital Hyperinsulinism of The Newborn: A Case ReportDocument6 pagesCongenital Hyperinsulinism of The Newborn: A Case ReportEdi SetiawanNo ratings yet
- Management of Childhood Onset Nephrotic Syndrome: PediatricsDocument13 pagesManagement of Childhood Onset Nephrotic Syndrome: PediatricssarabisimonaNo ratings yet
- Learning From Claims Hyperbilirubinaemia and KerniDocument4 pagesLearning From Claims Hyperbilirubinaemia and Kernihgz1 urgNo ratings yet
- Chapter 42: Pediatric and Adolescent Gynecology Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument3 pagesChapter 42: Pediatric and Adolescent Gynecology Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- CORD Albumin JAUNDICEDocument3 pagesCORD Albumin JAUNDICESuman MondalNo ratings yet
- Ampicillin PDFDocument3 pagesAmpicillin PDFandriNo ratings yet
- Perinatal Transient Myeloproliferative Disorder in Trisomy 21Document11 pagesPerinatal Transient Myeloproliferative Disorder in Trisomy 21Carina SuarezNo ratings yet
- Cerebral Palsy in Pakistani Children: A Hospital Based SurveyDocument8 pagesCerebral Palsy in Pakistani Children: A Hospital Based Surveyclaimstudent3515No ratings yet
- Panc FuncDocument6 pagesPanc Funcm waltersNo ratings yet
- Tetanus Neonatorum A Review of ManagementDocument5 pagesTetanus Neonatorum A Review of ManagementFrisiliakombaitan BaubauNo ratings yet
- Tetanus Neonatorum A Review of Management PDFDocument5 pagesTetanus Neonatorum A Review of Management PDFFrisiliakombaitan BaubauNo ratings yet
- Congenital Syphilis - DynaMedDocument47 pagesCongenital Syphilis - DynaMededwinNo ratings yet
- Eposter Infants of Mothers With Syphilis Glabela CPDocument1 pageEposter Infants of Mothers With Syphilis Glabela CPGlabela Christiana PandangoNo ratings yet
- Hemolytic DiseaseDocument10 pagesHemolytic DiseaseChino Paolo SamsonNo ratings yet
- Absceso Hepático NeonatalDocument6 pagesAbsceso Hepático NeonatalNabila Peña ZapataNo ratings yet
- CyclophospamideDocument4 pagesCyclophospamidemrkoyoNo ratings yet
- Neck Abcess in ChildrenDocument6 pagesNeck Abcess in ChildrenNandaNo ratings yet
- Glycerin Suppository in Preterm Neonates: OrrespondenceDocument2 pagesGlycerin Suppository in Preterm Neonates: OrrespondenceAryanto DedyNo ratings yet
- Short-Term Outcome of Neonates Treated With AllopurinolDocument5 pagesShort-Term Outcome of Neonates Treated With AllopurinolJunarto Butar ButarNo ratings yet
- Pyridoxine-Dependent Seizures PDFDocument5 pagesPyridoxine-Dependent Seizures PDFdrtgodeNo ratings yet
- Congenital Hepatic Cyst: Aldo Recinos, Tarik Zahouani, Juan Guillen and Benamanahalli RajegowdaDocument4 pagesCongenital Hepatic Cyst: Aldo Recinos, Tarik Zahouani, Juan Guillen and Benamanahalli RajegowdaSatyaja KinnaraNo ratings yet
- MCQ NasDocument16 pagesMCQ NasDwi HerawatiNo ratings yet
- Meningitis Protocole المعدل 1-2-2016Document3 pagesMeningitis Protocole المعدل 1-2-2016Hamza El-ȜfifiNo ratings yet
- Robert J. Adderley, MD, FRCP (C) Paul C.J. Rogers, T MB, MRCP, FRCP (C) Dorothy Shaw,. MB, FRCP (Ci Louis D. Wadsworth, MB, FRCP (C)Document3 pagesRobert J. Adderley, MD, FRCP (C) Paul C.J. Rogers, T MB, MRCP, FRCP (C) Dorothy Shaw,. MB, FRCP (Ci Louis D. Wadsworth, MB, FRCP (C)Sri HariNo ratings yet
- Brachial Plexus Injury PDFDocument2 pagesBrachial Plexus Injury PDFKamran AfzalNo ratings yet
- HalpinDocument3 pagesHalpinjaya adinugrohoNo ratings yet
- A Case Report On Catamenial Epilepsy PDFDocument6 pagesA Case Report On Catamenial Epilepsy PDFAyuNo ratings yet
- A Behavioral Method For Efficient Screening of Visual Acuity in Young InfantsDocument9 pagesA Behavioral Method For Efficient Screening of Visual Acuity in Young InfantsWistya Eka mahadewiNo ratings yet
- Kesici 2019Document7 pagesKesici 2019nurahmi widyani ratriNo ratings yet
- AKI Child W NS 2018Document4 pagesAKI Child W NS 2018Indah Nur LathifahNo ratings yet
- JurnalDocument5 pagesJurnalQarina El-HarizahNo ratings yet
- Pneumonia: Fever Cough Breathlessnes S DR J Pap/ich/ GMC Kottayam/19723Document4 pagesPneumonia: Fever Cough Breathlessnes S DR J Pap/ich/ GMC Kottayam/19723Firdouse ShajiNo ratings yet
- Cervical Insufficiency A New Issue For Guidelines On Prevention of Perinatal Group B Streptococcal DiseaseDocument6 pagesCervical Insufficiency A New Issue For Guidelines On Prevention of Perinatal Group B Streptococcal Diseaseatika sgrtNo ratings yet
- Paediatric Guidelines Nephrotic Syndrome 2018Document8 pagesPaediatric Guidelines Nephrotic Syndrome 2018lilydariniNo ratings yet
- BCMJ 53 Vol6 Febrile SeizuresDocument6 pagesBCMJ 53 Vol6 Febrile SeizuresdyyyaNo ratings yet
- Cit230 PDFDocument4 pagesCit230 PDFJoyBoyXNo ratings yet
- Chapter 41: Genitourinary Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument6 pagesChapter 41: Genitourinary Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Congenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementFrom EverandCongenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDiva D. De León-CrutchlowNo ratings yet
- Vitamin E - Ischemic - Annexin TunnelDocument7 pagesVitamin E - Ischemic - Annexin TunnelMogiMediawanNo ratings yet
- Vitamin E-Cva Iskemi-Tunnel BAX BCLDocument7 pagesVitamin E-Cva Iskemi-Tunnel BAX BCLMogiMediawanNo ratings yet
- Cerebral Lobes: Department of Neurosurgery Dr. Soetomo General Hospital - Airlangga UniversityDocument46 pagesCerebral Lobes: Department of Neurosurgery Dr. Soetomo General Hospital - Airlangga UniversityMogiMediawanNo ratings yet
- Annsurg00602 0014Document7 pagesAnnsurg00602 0014MogiMediawanNo ratings yet
- My Mama DonDocument1 pageMy Mama DonMogiMediawanNo ratings yet
- Give A Man But LuckDocument2 pagesGive A Man But LuckMogiMediawanNo ratings yet
- Dento Alveolar FracturesDocument16 pagesDento Alveolar FracturesafifrspmNo ratings yet
- Reproductive System DrugsDocument100 pagesReproductive System DrugsR-jay Guevara100% (1)
- Genitourinary TuberculosisDocument10 pagesGenitourinary TuberculosisMrunal DiveNo ratings yet
- All Conditions Data NCTDocument506 pagesAll Conditions Data NCTMuneer Ashraf0% (1)
- High Yield Psychiatry: Shelf Exam Review Emma Holliday RamahiDocument71 pagesHigh Yield Psychiatry: Shelf Exam Review Emma Holliday RamahisamNo ratings yet
- Theme 17-3 Acquired - Valvular - Diseases.Document3 pagesTheme 17-3 Acquired - Valvular - Diseases.Taranbir SainiNo ratings yet
- Common DrugsDocument15 pagesCommon DrugsKate Penelope DalidNo ratings yet
- 1700 Ebook DiseasesDocument250 pages1700 Ebook DiseasesAhmad Arif100% (1)
- Cumin (Cuminum Cyminum) and Black CuminDocument16 pagesCumin (Cuminum Cyminum) and Black Cuminharoon arshadNo ratings yet
- 144 DAFTAR DIAGNOSA NON-SPESIALISTIK (Dr. M. GENTA)Document8 pages144 DAFTAR DIAGNOSA NON-SPESIALISTIK (Dr. M. GENTA)lucianaayu febrina67% (3)
- S2 FKU 2007 Hasmija Bibliography - PDFDocument3 pagesS2 FKU 2007 Hasmija Bibliography - PDFAngel KoteNo ratings yet
- Treatment of Hypovolemia (Dehydration) in Children - UpToDateDocument13 pagesTreatment of Hypovolemia (Dehydration) in Children - UpToDateNedelcu MirunaNo ratings yet
- Diagnosis & Management of NstemiDocument26 pagesDiagnosis & Management of NstemiwlshakespeareNo ratings yet
- Carcinoma Gall BladderDocument25 pagesCarcinoma Gall Bladderrajan kumarNo ratings yet
- Drug StudyDocument22 pagesDrug StudySandra MedinaNo ratings yet
- My Fracture NotesDocument20 pagesMy Fracture NotesZai AkmaNo ratings yet
- Perinatal Asphyxia: Berhane G/her (MD, Ped.Y3R) Lecture Slides For C1 Medical Students of Adigrat UniversityDocument80 pagesPerinatal Asphyxia: Berhane G/her (MD, Ped.Y3R) Lecture Slides For C1 Medical Students of Adigrat UniversityAlemuNo ratings yet
- DRUG STUDY - OmeprazoleDocument1 pageDRUG STUDY - OmeprazoleKristine AsuncionNo ratings yet
- Differentials of Abnormal Urine Color ADocument6 pagesDifferentials of Abnormal Urine Color ALarysaNo ratings yet
- NCM116 Module 3 Cerebrovascular Disease QuizDocument5 pagesNCM116 Module 3 Cerebrovascular Disease QuizIvan FernandezNo ratings yet
- Adam Riner PD and Fall PreventionDocument48 pagesAdam Riner PD and Fall PreventionSupriNo ratings yet
- Pocket PediaDocument76 pagesPocket PediaDonna Labaniego100% (1)
- Clinical Practice Guidelines For The Diagnosis and Management of Children With Mental RetardationDocument25 pagesClinical Practice Guidelines For The Diagnosis and Management of Children With Mental RetardationDanielNo ratings yet
- Adrenergic ReceptorsDocument9 pagesAdrenergic Receptorsrababmohsin110100% (1)
- CDC Fact SheetDocument1 pageCDC Fact SheetAnonymous Pb39klJNo ratings yet
- Mixed Group: Name: Age: Sex: Weight: Address: OccupationDocument23 pagesMixed Group: Name: Age: Sex: Weight: Address: OccupationKristian Karl Bautista Kiw-isNo ratings yet
- Oculomotor NerveDocument23 pagesOculomotor NerveBismah Mudassar100% (1)
- Kidney and Urinary ManagementDocument39 pagesKidney and Urinary ManagementAlyssa MontimorNo ratings yet
- Lyceum of The Philippines University College of Nursing: MCN Form 014Document3 pagesLyceum of The Philippines University College of Nursing: MCN Form 014twinkleNo ratings yet