Professional Documents
Culture Documents
JR DAZ Digestif Senior - Hirschsprung's Complication Jurnal
JR DAZ Digestif Senior - Hirschsprung's Complication Jurnal
Uploaded by
diaz.azpOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JR DAZ Digestif Senior - Hirschsprung's Complication Jurnal
JR DAZ Digestif Senior - Hirschsprung's Complication Jurnal
Uploaded by
diaz.azpCopyright:
Available Formats
Am J Transl Res 2022;14(7):4830-4837
www.ajtr.org /ISSN:1943-8141/AJTR0143213
Original Article
Clinical outcomes and risk factors for postoperative
complications in children with Hirschsprung’s disease
Tingting Gao, Weijue Xu, Qingfeng Sheng, Ting Xu, Wei Wu, Zhibao Lv
Department of General Surgery, Shanghai Children’s Hospital, School of Medicine, Shanghai Jiao Tong University,
Shanghai 200000, China
Received March 30, 2022; Accepted June 22, 2022; Epub July 15, 2022; Published July 30, 2022
Abstract: Objective: To explore and analyze the risk factors for postoperative complications in patients with
Hirschsprung’s disease (HD). Methods: Patients with HD admitted to the hospital from 2015 to 2020 were reviewed
in this retrospective study. Follow-up data collected included constipation, fecal incontinence, anastomotic fistula,
Hirschsprung’s-associated enterocolitis (HAEC), and readmission. The putative risk factors for postoperative com-
plications in patients with HD were as follows: clinical classification, gender, operative age, hemoglobin and serum
albumin levels and preoperative HAEC. A follow-up survey was conducted for all patients by telephone. Data were
analyzed statistically using SPSS version 23.0. Results: A total of 154 patients were included in the study, of whom
119 patients were followed up successfully. 53 patients who had complications postoperatively were compared
to 66 patients who had no related complications. Among patients with complications: 8 had constipation, 22 had
fecal incontinence and 33 had HAEC. The gender, operative age, hemoglobin levels and preoperative HAEC did not
differ significantly between the two groups. However, significant differences were observed between the 2 groups
in clinical classification, surgical method, serum albumin level, and whether or not a one-stage operation was per-
formed (P<0.05). Conclusion: Clinical classification, surgical method, preoperative albumin level and whether or not
a one-stage operation was performed emerged as risk factors affecting the postoperative complications of patients
with HD. Therefore, the prognosis in HD can be improved by strengthening the preoperative nutritional support and
selecting appropriate surgical methods according to the clinical subtype.
Keywords: Hirschsprung’s disease, risk factors, complications, Hirschsprung’s-associated enterocolitis, surgery
Introduction technique for HD has dramatically improved
over the years, the incidence of postoperative
Hirschsprung’s disease (HD) is one of the most complications remains high at 20-40% [4, 5].
common congenital gastrointestinal abnormali- The prevalence of fecal incontinence was 20%
ties in infants, occurring in approximately 1 in (range: 3-48%) and that of constipation was
5000 births. It is caused by a congenital de- 14% (range: 1-56%) in a meta-analysis of HD
velopmental defect of the enteric nervous sys- patients >10 years-old [6]. Studies demons-
tem (ENS). The bowel movement is impaired trated that impaired bowel function with fecal
because of the malfunctioning ENS. Therefore, incontinence, soiling, and constipation, has a
abdominal distension, delayed passage of negative influence on the generic health-relat-
meconium, and intractable constipation are ed quality of life (HrQoL) of HD patients. A
typical clinical symptoms of HD [1-3]. Currently, meta-analysis reported a lower HrQoL in HD
resection and anastomosis of the bowel is the patients >10 years-old compared to the ge-
most widely accepted method for managing neral population with regard to fecal inconti-
HD. The common operations include Swenson, nence or constipation [6, 7].
Duhamel, Rehbein, and Soave. Operations for
HD are complex, giving rise to many postopera- Importantly, fecal incontinence, soiling, and
tive complications, including but not limited to constipation are short- and long-term issues in
constipation, fecal incontinence, anastomotic patients with HD, that alter the HrQoL [8].
fistula, and enterocolitis. Although the surgical Several studies have reported bowel function,
Complications in children with HD
QoL and postoperative complications in pa- 4. Total colon aganglionosis: refers to the ileum
tients with HD over the last few years, but the within 30 cm from the ileocecal valve in the
results were varied [9-11]. Therefore, exploring narrow segment of the ascending colon.
and analyzing the risk factors associated with
postoperative complications in patients with 5. Total intestinal aganglionosis: refers to ste-
HD is an urgent need. The present study aimed nosis involving the whole colon and small in-
to identify the risk factors for postoperative testine that is >30 cm away from the ileoce-
complications by a retrospective analysis of cum, or the duodenum.
patients with HD at our center from 2015 to
2020 in order to reduce future complications All patients were operated on after diagnosis.
and consequently improve their QoL. Soave, improved Soave, laparoscopic surgery
and modified Duhamel were the primary treat-
Materials and methods ment of HD at our center.
Patients Statistical analysis
Patients from the Department of General Sur- SPSS 23.0 statistical software was used for
gery of Shanghai Children’s Hospital, Shanghai, data collation and analysis. The counted data
China who presented and had symptoms vary- were expressed as a percentage, and χ2 test
ing from neonatal intestinal obstruction to was used.
intractable constipation and enterocolitis were
recruited for this study. These patients also Univariate model analysis and multivariate con-
showed a delayed passage of meconium. ditional logistic regression analysis of risk fac-
tors for postoperative complications in patients
A retrospective analysis of clinical outcomes
and risk factors related to postoperative com- with HD were performed to assess the risk fac-
plications was conducted. Data collected from tors for the occurrence of complications. The
patients included: clinical classification, gen- possible risk factors included clinical classi-
der, age at operation, preoperative Hirschs- fication, gender, operative age, preoperative
prung’s-associated enterocolitis (HAEC), hemo- HAEC, hemoglobin and serum albumin level,
globin and serum albumin levels, and whether and whether or not one-stage operation was
or not a one-stage operation was performed. performed. P<0.05 indicated a significant dif-
All patients were followed up by phone. The fol- ference. The area under the ROC curve (AUC)
low-up survey asked for information regarding was used to determine the diagnostic perfor-
postoperative constipation, fecal incontinence, mance, and values >0.7 were considered to
anastomotic fistula, HAEC, and readmission. represent good performance.
HD diagnosis and treatment Results
The diagnosis of HD was based on symptoms, Patient characteristics
barium enema, and biopsy results. The biopsy
methods included full-thickness rectal biopsy A total of 154 patients with HD were enrolled
and rectal submucosal biopsy. According to the in this study, of whom 119 were successfully
extent of aganglionosis, the clinical classifica- followed up over the phone. The age of the pa-
tion of HD included: tients conducted in the follow-up ranged from
1-6 years, (average: 37) months. The median
1. Short segment: narrow segment located in age at operation was 11 (range: 1 month-7
the mid to distal rectum. years). Most of the patients were males, and
2. Ordinary: narrow segment located in the most were >3 months-old. In clinical classifica-
anus to proximal rectum or rectosigmoid junc- tion, the ordinary type was the primary type,
tion, even up to the distal sigmoid colon. and Soave was the primary surgical method.
Almost all patients had an enema before the
3. Long segment: narrow segment extending operation. In addition, most patients under-
from the anus to the descending colon or even went a one-stage operation (Table 1). Patients
transverse colon. who underwent reoperation at other hospitals
4831 Am J Transl Res 2022;14(7):4830-4837
Complications in children with HD
Table 1. Demographics and characteristics of patients
Total number 119 (%)
Age at operation ≤3 month 36 (30.2%)
>3 month 83 (69.8%)
Gender male 98 (82.4%)
female 21 (17.6%)
Clinical classification Short segment 10 (8.4%)
Ordinary 74 (62.2%)
Long 22 (18.5%)
Total colonic 13 (10.9%)
Surgical approach Soave 40 (33.6%)
Improved Soave 10 (8.4%)
Laparoscopic-assisted Soave 50 (42.0%)
Laparoscopic-assisted improved soave 9 (7.6%)
modified Duhamel 10 (8.4%)
HAEC before operation Yes 27 (22.7%)
No 92 (77.3%)
Enema before operation Yes 113 (95.0%)
No 6 (5.0%)
Primary surgery Yes 91 (76.5%)
No 28 (23.5%)
Albumin level Normal 93 (78.2%)
Low 26 (21.8%)
Hemoglobin level Normal 70 (58.8%)
Low 49 (41.2%)
or did not undergo a radical operation after In addition, clinical classification, surgical me-
diagnosis were excluded from this study. thod, and one-stage radical surgery were sta-
tistically significant in causing complications
Clinical outcomes (P<0.05) (Table 3). Furthermore, multivariate
logistic regression analysis showed that clini-
53/119 (44.5%) patients with HD had postop- cal classification and preoperative albumin
erative complications, such as constipation, level were independent risk factors for postop-
fecal incontinence, and HAEC. Constipation erative complications (Table 4).
occurred in 8 (6.7%), fecal incontinence in 22
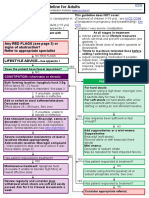
(18.5%) and enterocolitis in 33 (27.7%). Intri- Receiver operating characteristic (ROC) curve
guingly, 10 (8.4%) patients had two complica- analysis revealed that the area under the ROC
tions and the remaining 66 patients had no curve (AUC) of the combination of clinical clas-
related complications. sification, surgical approach, and albumin level
for predicting postoperative complications was
Univariate analysis was conducted according 0.70 (Figure 1). Thus, the combination of clini-
to the age at operation, gender, clinical classifi- cal classification, surgical approach, and albu-
cation, surgical approach, preoperative HAEC, min level may have a predictive value.
and preoperative hemoglobin and albumin lev-
els. Analysis of postoperative HAEC patients Discussion
showed that clinical classification, surgical me-
thod, and whether one-stage radical surgery Hirschsprung’s disease (HD) is a congenital
was performed caused complications (P< defect due to an abnormality in migration, pro-
0.05). These results also showed that there liferation, differentiation, and preservation of
were no significant complications of constipa- enteric neural crest derived cells (ENCCs) [3,
tion or fecal incontinence (Table 2). 13]. This alteration causes aganglionosis in the
4832 Am J Transl Res 2022;14(7):4830-4837
Complications in children with HD
Table 2. Univariate analysis of risk factors related to complications
Constipation Fecal incontinence HAEC
number P-Value number P-Value number P-Value
Age at operation ≤3 month 1 0.432 8 0.608 9 0.824
>3 month 7 14 24
Gender male 6 0.630 20 0.357 24 0.109
female 2 2 9
Clinical classification Short segment 2 0.099 1 0.880 2 0.014
Ordinary 3 14 15
Long 3 4 8
Total colonic 0 3 8
Surgical approach Soave 4 0.655 8 0.980 10 0.040
Improved Soave 0 2 3
Laparoscopic-assisted Soave 3 9 11
Laparoscopic-assisted improved soave 1 1 2
modified Duhamel 0 2 7
HAEC before operation Yes 1 0.683 4 0.435 25 1.000
No 7 18 8
Enema before operation Yes 8 1.000 22 0.590 31 0.664
No 0 0 2
Primary surgery Yes 4 0.090 18 0.589 22 0.014
No 4 4 11
Albumin level Normal 8 0.196 18 0.779 27 0.803
Low 0 4 6
Hemoglobin level Normal 4 0.717 15 0.346 18 0.531
Low 4 7 15
Table 3. Univariate analysis of risk factors of complications in patients with HD
Complications No complications P-Value
Age at operation ≤3 month 15 21 0.694
>3 month 38 45
Gender male 41 57 0.232
female 12 9
Clinical classification Short segment 3 7 0.007
Ordinary 27 47
Long 12 10
Total colonic 11 2
Surgical approach Soave 18 22 0.042
Improved Soave 4 6
Laparoscopic-assisted Soave 18 32
Laparoscopic-assisted improved soave 4 5
modified Duhamel 9 1
HAEC before operation Yes 11 16 0.655
No 42 50
Enema before operation Yes 51 62 0.695
No 2 4
Primary surgery Yes 34 57 0.005
No 19 9
Albumin level Normal 45 48 0.124
Low 8 18
Hemoglobin level Normal 32 38 0.853
Low 21 28
4833 Am J Transl Res 2022;14(7):4830-4837
Complications in children with HD
Table 4. Logistic regression analysis of risk factors for complications
β SE χ2 OR 95% CI P-Value
Age at operation 0.562 0.509 1.219 1.754 0.647-4.754 0.270
Gender 0.172 0.573 0.090 1.188 0.386-3.656 0.764
Clinical classification -.765 0.340 5.072 0.465 0.239-0.906 0.024
Surgical approach -.218 0.197 1.223 0.804 0.546-1.184 0.269
HAEC before operation 0.361 0.507 0.509 1.435 0.532-3.874 0.476
Enema before operation 0.153 0.989 0.024 1.165 0.168-8.093 0.877
Primary surgery -.830 0.627 1.753 0.436 0.128-1.490 0.186
Albumin level 1.168 0.591 3.898 3.214 1.009-10.244 0.048
Hemoglobin level -.210 0.451 0.217 0.811 0.335-1.961 0.642
Over the last few decades sin-
gle-center and multi-center
studies have mainly focused
on postoperative complica-
tions in children with HD. The
incidence of postoperative
complications in patients who
underwent Soave surgery ran-
ged from 14.7-67% [12]. Vari-
ous factors including the age
of the child at the time of oper-
ation, the duration of the dis-
ease, associated anomalies,
and the type of surgical proce-
dure, contributed to the occur-
rence of complications [13,
14].
In this retrospective study,
119 patients diagnosed with
HD who underwent radical sur-
gery were analyzed. HAEC, con-
stipation, and fecal inconti-
nence were the most common
Figure 1. Predictive efficacy of clinical classification, surgical approach, and postoperative complications in
serum albumin level. AUC: 0.7. this study. We also observed
that clinical classification, sur-
gical method, and whether a
distal intestine, resulting in intestinal obstruc- one-stage operation was performed were sig-
tion. Surgery is the primary treatment causing nificant risk factors related to postoperative
several postoperative complications that se- complications in children with HD.
verely affect the QoL of patients, and some
patients even need reoperation [10]. There- In this study, HAEC was the main postoperative
fore, it is crucial to analyze and explore the risk complication in patients, with an incidence of
factors for postoperative complications in 27.7%. 20/33 patients were readmitted to the
patients HD. According to the results, we can hospital. The occurrence of HAEC varies ac-
formulate corresponding preventive measures cording to different reports. Le-Nguyen et al.
to reduce the incidence of postoperative com- [15] reported that the incidences of HAEC
plications and improve the overall treatment. before and after surgery were 25% and 19%
4834 Am J Transl Res 2022;14(7):4830-4837
Complications in children with HD
respectively. Chung et al. [16] reported that the main risk factors for complications in
the incidence of HAEC after 1 year of surgery patients with HD. Typically, constipation occurs
was 20.8%. Addtionally, Neuvonen et al. [17] in patients undergoing Soave surgery, which
reported postoperative recurrent enterocolitis might be caused by simple mucosal stripping
in 44%. and large residual muscle sheaths lacking gan-
glion cells. Then these patients required a pro-
Some studies indicate that common risk fac- longed duration for anal expansion.
tors for HAEC include low weight, low IgA, the
length of intestine involved in HD, preoperative Conversely, the modified Soave method excis-
enteritis, and other congenital diseases [18]. ed a part of the muscle sheath, and our analy-
However, only a few studies have analyzed the sis showed that the incidence of postoperative
effect of age, pathologic typing, and surgical constipation in such patients was extremely
method on HAEC, although the conclusions low. Early intervention such as dietary adjust-
were varied [16]. In the current study, the risk ment and defecation training, may improve the
factors included clinical classification, surgical patient’s defecation control ability, thereby im-
method, and whether or not one-stage radical proving their QoL [23, 27].
surgery was performed. The incidence of enter-
ocolitis in the long segment (36.4%), and total Furthermore, primary or staged surgery for HD
colon aganglionosis (61.4%) was significantly remains controversial. Presently, most doctors
higher than that in the common type and short adopt the one-staged operation for HD pa-
segment aganglionsis. The longer the agangli- tients due to the safety and efficacy of the pro-
cedure. In a multicenter, large-sample retro-
onic segment, the greater the intestinal ENS
spective study [28], the surgical complications
defect, and the more severely impaired the
not including anastomotic stenosis, HAEC inci-
intestinal barrier and immune function. More-
dence, and reoperation rate were lower than
over, fecal stasis and intestinal microflora dis-
those for the secondary surgery. A meta-analy-
order also increased intestinal susceptibility.
sis by Zimmer et al. [29] showed that there
Some studies reported that oral probiotics
were neither significant differences in the rate
reduce the incidence and severity of postoper-
of good bowel function after the first and sec-
ative HAEC [19]. Some researchers used differ-
ond-stage operation nor in the incidence of
ent cuff lengths for the Soave technique and
fecal fouling and fecal incontinence. However,
found that the incidence of enterocolitis was the incidence of constipation in the first-stage
lower in patients with short cuff lengths (9% vs was lower than that of the second-stage opera-
30%) [20, 21]. tion (P=0.006) in this analysis, indicating that
the early radical surgery was beneficial to the
In addition to HAEC, constipation and fecal
recovery of the bowel function of patients.
incontinence are also common postoperative
Additionally, the incidences of constipation and
complications in patients with HD. Constipation
HAEC were lower after primary surgery than
and fecal incontinence have been recognized
after secondary surgery, while the incidence of
as chronic problems in a large proportion of
fecal contamination was higher after second-
patients with HD [5, 22, 23]. In this study, the
ary surgery. Notably, most patients who under-
incidence of these complications was 6.7% and
went staged surgery in our study were in an
18.5%, respectively. Widyasari et al. [5] report-
unstable condition or presented with severe
ed constipation in 24% of patients who under-
complications. The outcome of such patients
went Soave’s procedure. Wang et al. showed
may not be ideal for primary surgery. Thus, we
that the probability of early postoperative fecal hypothesize that primary surgery would be
contamination in HD children is 30-40% [24], most feasible for patients with HD in a stable
which is caused by intraoperative injury of the condition when not diagnosed with HAEC. Con-
internal sphincter and the pelvic floor nerves. versely, staging surgery would be recommend-
The major contributors to fecal continence are ed for patients who have severe complications
the anal sphincters, colonic motility, anorectal such as HAEC, bowel perforation, malnutrition,
sensation, and the sub-epithelium of the anal or severe proximal bowel expansion.
canal [25, 26]. All these factors can be effectu-
ated during transanal surgery, causing soiling. The current study was carried out using an
In this study, the surgical approach was one of extensive data analysis and the results provid-
4835 Am J Transl Res 2022;14(7):4830-4837
Complications in children with HD
ed a reliable theory. Nonetheless, these find- [3] Diposarosa R, Bustam NA, Sahiratmadja E, Su-
ings were not in agreement with those from santo PS and Sribudiani Y. Literature review:
previous studies, which might be related to enteric nervous system development, genetic
and epigenetic regulation in the etiology of
the patient’s characteristics, the number of
Hirschsprung’s disease. Heliyon 2021; 7:
patients, and time of follow-up. Therefore, in
e07308.
future studies, a large sample size with data [4] Parahita IG, Makhmudi A and Gunadi. Com-
from multiple centers should be used to evalu- parison of Hirschsprung-associated enterocoli-
ate the risk factors related to postoperative tis following Soave and Duhamel procedures. J
complications in patients with HD. Pediatr Surg 2018; 53: 1351-1354.
[5] Widyasari A, Pavitasari WA, Dwihantoro A and
Conclusion Gunadi. Functional outcomes in Hirschsprung
disease patients after transabdominal Soave
This study shows the clinical outcomes and and Duhamel procedures. BMC Gastroenterol
risk factors of complications after surgery for 2018; 18: 56.
[6] Dai Y, Deng Y, Lin Y, Ouyang R and Li L. Long-
HD. Postoperative complications such as fecal
term outcomes and quality of life of patients
incontinence, constipation, and enterocolitis
with Hirschsprung disease: a systematic re-
severely affect the quality of life of patients view and meta-analysis. BMC Gastroenterol
with HD. Clinical classification, surgical meth- 2020; 20: 67.
od, preoperative albumin level, and one-stage [7] Kyrklund K, Neuvonen MI, Pakarinen MP and
operation, if performed are related risk factors Rintala RJ. Social morbidity in relation to bowel
affecting the postoperative complications of functional outcomes and quality of life in ano-
patients with HD. Therefore, the prognosis of rectal malformations and Hirschsprung’s dis-
HD can be improved by strengthening preoper- ease. Eur J Pediatr Surg 2018; 28: 522-528.
[8] Veras LV, Arnold M, Avansino JR, Bove K,
ative nutritional support and selecting appro-
Cowles RA, Durham MM, Goldstein AM, Krish-
priate surgical methods according to different nan C, Langer JC, Levitt M, Monforte-Munoz H,
clinical types and the preoperative condition of Rabah R, Reyes-Mugica M, Rollins MD 2nd,
the patients. Kapur RP and Gosain A; American Pediatric
Surgical Association Hirschsprung Disease In-
Acknowledgements terest Group. Guidelines for synoptic reporting
of surgery and pathology in Hirschsprung dis-
The procedures mentioned in the present study ease. J Pediatr Surg 2019; 54: 2017-2023.
have been approved by the Ethics Committee [9] Sood S, Lim R, Collins L, Trajanovska M, Hut-
of Shanghai Children’s Hospital (approval No. son JM, Teague WJ and King SK. The long-term
2020RY023-E01). quality of life outcomes in adolescents with
Hirschsprung disease. J Pediatr Surg 2018;
53: 2430-2434.
Disclosure of conflict of interest
[10] Townley OG, Lindley RM, Cohen MC and Murthi
GV. Functional outcome, quality of life, and
None. ‘failures’ following pull-through surgery for
Hirschsprung’s disease: a review of practice at
Address correspondence to: Dr. Zhibao Lv, Depart- a single-center. J Pediatr Surg 2020; 55: 273-
ment of General Surgery, Shanghai Children’s 277.
Hospital, School of Medicine, Shanghai Jiao Tong [11] Espeso L, Coutable A, Flaum V, Rebeuh J,
University, 355 Luding Road, Putuo District, Shang- Lavrand F, Podevin G, Lamireau T, Enaud R
hai 200000, China. Tel: +86-18930658851; E-mail: and Talon I. Persistent soiling affects quality of
zhibaolyu@163.com life in children with Hirschsprung’s disease. J
Pediatr Gastroenterol Nutr 2020; 70: 238-
References 242.
[12] Askarpour S, Peyvasteh M, Imanipour MH, Ja-
[1] Klein M and Varga I. Hirschsprung’s disease- vaherizadeh H and Hesam S. Complications
recent understanding of embryonic aspects, after transabdominal Soave’s procedure in
etiopathogenesis and future treatment ave- children with Hirschsprung’s disease. Arq Bras
nues. Medicina (Kaunas) 2020; 56: 611. Cir Dig 2019; 32: e1421.
[2] Ambartsumyan L, Smith C and Kapur RP. Diag- [13] Stensrud KJ, Emblem R and Bjørnland K. Func-
nosis of Hirschsprung disease. Pediatr Dev tional outcome after operation for Hirschs-
Pathol 2020; 23: 8-22. prung disease--transanal vs transabdominal
4836 Am J Transl Res 2022;14(7):4830-4837
Complications in children with HD
approach. J Pediatr Surg 2010; 45: 1640- [23] Neuvonen MI, Kyrklund K, Rintala RJ and Pak-
1644. arinen MP. Bowel function and quality of life
[14] Anderson JE, Vanover MA, Saadai P, Stark RA, after transanal endorectal pull-through for
Stephenson JT and Hirose S. Epidemiology of Hirschsprung disease: controlled outcomes up
Hirschsprung disease in California from 1995 to adulthood. Ann Surg 2017; 265: 622-629.
to 2013. Pediatr Surg Int 2018; 34: 1299- [24] Wang G, Sun XY, Wei MF and Weng YZ. Heart-
1303. shaped anastomosis for Hirschsprung’s dis-
[15] Le-Nguyen A, Righini-Grunder F, Piché N, Faure ease: operative technique and long-term fol-
C and Aspirot A. Factors influencing the inci- low-up. World J Gastroenterol 2005; 11:
dence of Hirschsprung associated enterocoli- 296-298.
tis (HAEC). J Pediatr Surg 2019; 54: 959-963. [25] Bischoff A, Frischer J, Knod JL, Dickie B, Levitt
[16] Chung PHY, Yu MON, Wong KKY and Tam PKH. MA, Holder M, Jackson L and Peña A. Dam-
Risk factors for the development of post-oper- aged anal canal as a cause of fecal inconti-
ative enterocolitis in short segment Hirschs- nence after surgical repair for Hirschsprung
prung’s disease. Pediatr Surg Int 2019; 35: disease - a preventable and under-reported
187-191. complication. J Pediatr Surg 2017; 52: 549-
[17] Neuvonen MI, Kyrklund K, Lindahl HG, Koi- 553.
vusalo AI, Rintala RJ and Pakarinen MP. A pop- [26] De la Torre L, Cogley K, Santos K, Morales O
ulation-based, complete follow-up of 146 con- and Calisto J. The anal canal is the fine line
secutive patients after transanal mucosectomy between “fecal incontinence and colitis” after
for Hirschsprung disease. J Pediatr Surg 2015; a pull-through for Hirschsprung disease. J Pedi-
50: 1653-1658. atr Surg 2017; 52: 2011-2017.
[18] Pini Prato A, Arnoldi R, Sgrò A, Felici E, Racca F, [27] Bjørnland K, Pakarinen MP, Stenstrøm P, Sten-
Nozza P, Mariani N, Mosconi M, Mazzola C and srud KJ, Neuvonen M, Granstrom AL, Graneli
Mattioli G. Hirschsprung disease and Down C, Pripp AH, Arnbjörnsson E, Emblem R, Wester
syndrome: from the reappraisal of risk factors T and Rintala RJ; Nordic Pediatric Surgery
to the impact of surgery. J Pediatr Surg 2019; Study Consortium. A Nordic multicenter survey
54: 1838-1842. of long-term bowel function after transanal en-
[19] Mei F, Wu M, Zhao L, Hu K, Gao Q, Chen F, dorectal pull-through in 200 patients with rec-
Kwong JS, Wang Y, Shen XP and Ma B. Probiot- tosigmoid Hirschsprung disease. J Pediatr
ics for the prevention of Hirschsprung-associ- Surg 2017; 52: 1458-1464.
ated enterocolitis. Cochrane Database Syst [28] Sulkowski JP, Cooper JN, Congeni A, Pearson
Rev 2022; 4: CD013714. EG, Nwomeh BC, Doolin EJ, Blakely ML, Min-
[20] Ram AD, Scholfield DW and Pimpalwar A. Nov- neci PC and Deans KJ. Single-stage versus
el technique of mapping biopsies during lapa- multi-stage pull-through for Hirschsprung’s dis-
roscopic assisted transanal Soave endorectal ease: practice trends and outcomes in infants.
pull-through surgery for Hirschsprung’s dis- J Pediatr Surg 2014; 49: 1619-1625.
ease’s. Ann R Coll Surg Engl 2017; 99: 504. [29] Zimmer J, Tomuschat C and Puri P. Long-term
[21] Khazdouz M, Sezavar M, Imani B, Akhavan H, results of transanal pull-through for Hirschs-
Babapour A and Khademi G. Clinical outcome prung’s disease: a meta-analysis. Pediatr Surg
and bowel function after surgical treatment in Int 2016; 32: 743-749.
Hirschsprung’s disease. Afr J Paediatr Surg
2015; 12: 143-147.
[22] Menezes M, Corbally M and Puri P. Long-term
results of bowel function after treatment for
Hirschsprung’s disease: a 29-year review. Pe-
diatr Surg Int 2006; 22: 987-990.
4837 Am J Transl Res 2022;14(7):4830-4837
You might also like
- Optimal Time For Single-Stage Pull-Through Colectomy in Infants With Short-Segment Hirschsprung DiseaseDocument5 pagesOptimal Time For Single-Stage Pull-Through Colectomy in Infants With Short-Segment Hirschsprung DiseaseNate MichalakNo ratings yet
- 872 2540 2 PBDocument4 pages872 2540 2 PBSteve D'HamsNo ratings yet
- Uses of ERCP in The Management of Post-Cholecystectomy ComplicationsDocument6 pagesUses of ERCP in The Management of Post-Cholecystectomy ComplicationsAliA.RamadhanNo ratings yet
- Laparoscopic Appendectomy For Perforated Appendicitis in Children Has Complication Rates Comparable With Those of Open AppendectomyDocument7 pagesLaparoscopic Appendectomy For Perforated Appendicitis in Children Has Complication Rates Comparable With Those of Open AppendectomyGina Kristina NanginNo ratings yet
- Manejo de SX Adherencial Con GastrografinDocument7 pagesManejo de SX Adherencial Con Gastrografinmanuel barrientosNo ratings yet
- 3Document8 pages3Agung SentosaNo ratings yet
- Journal of Pediatric Surgery: Isidora Galuh Parahita, Akhmad Makhmudi, GunadiDocument4 pagesJournal of Pediatric Surgery: Isidora Galuh Parahita, Akhmad Makhmudi, GunadijeannchristyNo ratings yet
- Colonic InertiaDocument5 pagesColonic InertiaEmilio SanchezNo ratings yet
- Types Sites and Causes of Mechanical Intestinal ObDocument5 pagesTypes Sites and Causes of Mechanical Intestinal ObPutra FebdianNo ratings yet
- Cholelithiasis: Causative Factors, Clinical Manifestations and ManagementDocument6 pagesCholelithiasis: Causative Factors, Clinical Manifestations and ManagementmusdalifahNo ratings yet
- Project MoralesDocument6 pagesProject MoralesDiane Krystel G. MoralesNo ratings yet
- Hirschsprung's Disease: Epidemiology, Diagnosis, and Treatment in A Retrospective Hospital-Based StudyDocument8 pagesHirschsprung's Disease: Epidemiology, Diagnosis, and Treatment in A Retrospective Hospital-Based StudyDandhy Irwan MasdarNo ratings yet
- Pini Prato2010Document8 pagesPini Prato2010AndikaNo ratings yet
- JurnalDocument4 pagesJurnalsyairodhi rodziNo ratings yet
- Functional Outcomes of Patients With Short-Segment Hirschsprung Disease After Transanal Endorectal Pull-ThroughDocument6 pagesFunctional Outcomes of Patients With Short-Segment Hirschsprung Disease After Transanal Endorectal Pull-ThroughAndikaNo ratings yet
- Oesophagal PerfDocument7 pagesOesophagal PerfShiva KumarNo ratings yet
- Ianuarie 2017Document6 pagesIanuarie 2017Radu MiricaNo ratings yet
- 7114 28088 1 PBDocument4 pages7114 28088 1 PBShashidhara PuttarajNo ratings yet
- Document Heading Doi: 10.21276/apjhs.2016.3.4s.2 Research ArticleDocument9 pagesDocument Heading Doi: 10.21276/apjhs.2016.3.4s.2 Research ArticleluckystarNo ratings yet
- Infantile Hypertrophic Pyloric Stenosis at A TertiDocument7 pagesInfantile Hypertrophic Pyloric Stenosis at A TertiVașadi Razvan CristianNo ratings yet
- EchografyDocument6 pagesEchografyMiha ElaNo ratings yet
- A Study On Acute Surgical Abdomen in Paediatric Age Group: Original Research ArticleDocument5 pagesA Study On Acute Surgical Abdomen in Paediatric Age Group: Original Research ArticleApple IdeaNo ratings yet
- Saar 2016Document7 pagesSaar 2016iinmsNo ratings yet
- Optimal Timing For Soave Primary Pull-Through in Short-SegmentDocument7 pagesOptimal Timing For Soave Primary Pull-Through in Short-SegmentNate MichalakNo ratings yet
- Acute Cholecystitis: From ER To Surgery: Riginal RticleDocument5 pagesAcute Cholecystitis: From ER To Surgery: Riginal RticleKrystel Joy AuroNo ratings yet
- Vrecenak 2014Document5 pagesVrecenak 2014sigitdwimulyoNo ratings yet
- Roux-en-Y Longitudinal Pancreatico Jejunostomy For Pancreatic Calculi in ChildrenDocument4 pagesRoux-en-Y Longitudinal Pancreatico Jejunostomy For Pancreatic Calculi in ChildrenDiani Wulan AsmuandiNo ratings yet
- The Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014Document7 pagesThe Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014alemago90No ratings yet
- 1475 2891 12 118Document8 pages1475 2891 12 118SunardiasihNo ratings yet
- SudaniwawiDocument7 pagesSudaniwawiMouhammed SleiayNo ratings yet
- Laparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisDocument10 pagesLaparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisFerdian PriantoNo ratings yet
- Long-Term Follow-Up of Gastric Banding 10 Years and Beyond: Original ContributionsDocument7 pagesLong-Term Follow-Up of Gastric Banding 10 Years and Beyond: Original ContributionsRadu MiricaNo ratings yet
- Research Paper Effectiveness of Conservative Management of Uncomplicated Acute Appendicitis: A Single Hospital Based Prospective StudyDocument8 pagesResearch Paper Effectiveness of Conservative Management of Uncomplicated Acute Appendicitis: A Single Hospital Based Prospective StudyAnsoriNo ratings yet
- VolvulusDocument10 pagesVolvuluswatsonmexNo ratings yet
- Ahn2008 Article ClinicopathologicalFeaturesAndDocument8 pagesAhn2008 Article ClinicopathologicalFeaturesAndXavier QuinteroNo ratings yet
- A Prospective Study On Appendicular MassDocument4 pagesA Prospective Study On Appendicular MassA BNo ratings yet
- Paper AbdAllah RefaatDocument13 pagesPaper AbdAllah RefaatAbdAllah A. RefaatNo ratings yet
- Pathologically Assessed Grade of Hirschsprung Associated EnterocolitisDocument6 pagesPathologically Assessed Grade of Hirschsprung Associated EnterocolitisSurgeon RANo ratings yet
- Original Research PaperDocument4 pagesOriginal Research PaperDr SrigopalNo ratings yet
- PimpaleDocument6 pagesPimpaleMariano BritoNo ratings yet
- Acute Appendicitis in AdultsDocument19 pagesAcute Appendicitis in Adultsdimi firmatoNo ratings yet
- Apendisitis MRM 3Document8 pagesApendisitis MRM 3siti solikhaNo ratings yet
- Etiology, Treatment Outcome and Prognostic Factors Among Patients With Secondary Peritonitis at Bugando Medical Centre, Mwanza, TanzaniaDocument13 pagesEtiology, Treatment Outcome and Prognostic Factors Among Patients With Secondary Peritonitis at Bugando Medical Centre, Mwanza, Tanzaniayossy aciNo ratings yet
- Journal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesDocument3 pagesJournal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesVmiguel LcastilloNo ratings yet
- EASY TrialDocument8 pagesEASY TrialDpxeir PapanikolaouNo ratings yet
- Outcome of Total Laparoscopic HysterectomyDocument4 pagesOutcome of Total Laparoscopic HysterectomyDanica SavićNo ratings yet
- Appendicitis NaddlerDocument6 pagesAppendicitis NaddlerMedardo ApoloNo ratings yet
- Cytoreductive Surgery and IntraperitonealDocument11 pagesCytoreductive Surgery and IntraperitonealJorge FallasNo ratings yet
- Challenges and Outcome of Wilms' Tumour Management in A Resource-Constrained SettingDocument3 pagesChallenges and Outcome of Wilms' Tumour Management in A Resource-Constrained Settingcallisto3487No ratings yet
- Vol. 229, No. 4S2, October 2019 Scientific Poster Presentations E69Document2 pagesVol. 229, No. 4S2, October 2019 Scientific Poster Presentations E69Mateo TamayoNo ratings yet
- Clinical Study: Delorme's Procedure For Complete Rectal Prolapse: A Study of Recurrence Patterns in The Long TermDocument6 pagesClinical Study: Delorme's Procedure For Complete Rectal Prolapse: A Study of Recurrence Patterns in The Long TermAnonymous A1ycUQ9zVINo ratings yet
- UC Irvine Previously Published WorksDocument14 pagesUC Irvine Previously Published WorksBig BearNo ratings yet
- Stress Ulcer, Gastritis, and Gastrointestinal Bleeding Prophylaxis in Critically Ill Pediatric Patients: A Systematic ReviewDocument9 pagesStress Ulcer, Gastritis, and Gastrointestinal Bleeding Prophylaxis in Critically Ill Pediatric Patients: A Systematic ReviewIkrima MuhdarmuhallyNo ratings yet
- Guidelines For The Diagnosis and Management of Hirschsprung-Associated EnterocolitisDocument5 pagesGuidelines For The Diagnosis and Management of Hirschsprung-Associated EnterocolitisNasrudin EfendiNo ratings yet
- Ijo 24 69 PDFDocument6 pagesIjo 24 69 PDFPutri Nisrina HamdanNo ratings yet
- Current Success in The Treatment of Intussusception in ChildrenDocument9 pagesCurrent Success in The Treatment of Intussusception in ChildrenOby RomdhoniNo ratings yet
- Mertens2021 Article TransthoracicVersusTranshiatalDocument9 pagesMertens2021 Article TransthoracicVersusTranshiatalDr Shiv ChopraNo ratings yet
- Chirurgie 3 NissenDocument5 pagesChirurgie 3 Nissendansilviu11No ratings yet
- 65 Stenoza GDDDocument7 pages65 Stenoza GDDGabriela MilitaruNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- 3 MS Physical Assessment and Review of SystemDocument2 pages3 MS Physical Assessment and Review of SystemJanah Calit100% (1)
- Care of Patient With Acute Gastroenteritis With DehydrationDocument19 pagesCare of Patient With Acute Gastroenteritis With DehydrationSilhouette DreamNo ratings yet
- Management of Common Benign Anorectal Disease: What All Physicians Need To KnowDocument7 pagesManagement of Common Benign Anorectal Disease: What All Physicians Need To KnowNeri JaramilloNo ratings yet
- Hirschsprung DiseaseDocument13 pagesHirschsprung Diseaseganesh reddyNo ratings yet
- Bowel IncontinenceDocument4 pagesBowel IncontinenceprashanthNo ratings yet
- Causes of Anal Sphincter DamageDocument4 pagesCauses of Anal Sphincter DamageHadi ZavarehNo ratings yet
- Diarrhea PPTDocument82 pagesDiarrhea PPTIshwar HavaragiNo ratings yet
- Fundam Nursing Skill Lab ManualDocument97 pagesFundam Nursing Skill Lab ManualBirhanu AyenewNo ratings yet
- Bowel EliminationDocument37 pagesBowel EliminationLamirah ThomasNo ratings yet
- Advances in The Treatment of Anal FistulaDocument9 pagesAdvances in The Treatment of Anal FistuladevbyNo ratings yet
- Bowel EliminationDocument34 pagesBowel EliminationAnastasia LubertaNo ratings yet
- CONCEPT MAP FistulaDocument1 pageCONCEPT MAP FistulaDaryl TarucNo ratings yet
- Gynecological Assessment: DateDocument4 pagesGynecological Assessment: Dateanne laureNo ratings yet
- Up To Date. Myelomeningocele ManagmentDocument29 pagesUp To Date. Myelomeningocele ManagmentGuardito PequeñoNo ratings yet
- Case Presentation On ARMsDocument39 pagesCase Presentation On ARMsSomyee PachuauNo ratings yet
- AbstractDocument23 pagesAbstractaashish21081986No ratings yet
- NCMB 316 Assignment NCP Part 2Document3 pagesNCMB 316 Assignment NCP Part 2I'm a PepegaNo ratings yet
- GynecoDocument3 pagesGynecoanne laureNo ratings yet
- Management of Third and Fourth Degree TearsDocument4 pagesManagement of Third and Fourth Degree TearsYwagar YwagarNo ratings yet
- Anal GlandsDocument7 pagesAnal GlandsSuraj_Subedi100% (2)
- Anorectal ManometryDocument6 pagesAnorectal ManometryCesar QuirozNo ratings yet
- Treat Constipation With AcupressureDocument72 pagesTreat Constipation With AcupressurePrabha VanniarNo ratings yet
- A Systematic Review and Meta-Analysis of The Treatment of Anal FissureDocument21 pagesA Systematic Review and Meta-Analysis of The Treatment of Anal FissureNicolás CopaniNo ratings yet
- Jacquet Erosive DermatitisDocument15 pagesJacquet Erosive DermatitisRitchie StefanusNo ratings yet
- Approach To A Patient With Diarrhea Dr. Mohamed Abu HmaidDocument61 pagesApproach To A Patient With Diarrhea Dr. Mohamed Abu Hmaidoss-20502745No ratings yet
- RectumDocument129 pagesRectumRadhika SethuNo ratings yet
- Laxative Treatment Guideline For AdultsDocument7 pagesLaxative Treatment Guideline For AdultsPurim KTshipNo ratings yet
- A Nursing Care Plan On: Loose Bowel MovementDocument6 pagesA Nursing Care Plan On: Loose Bowel MovementakoitsmeNo ratings yet
- Constipation Guideline PDFDocument13 pagesConstipation Guideline PDFCarimaGhalieNo ratings yet
- Defecation - Rectum - Control - TeachMePhysiologyDocument2 pagesDefecation - Rectum - Control - TeachMePhysiologyLaiba AliNo ratings yet