Professional Documents
Culture Documents
Solar Powered Noninvasive
Solar Powered Noninvasive
Uploaded by
12deep2001Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Solar Powered Noninvasive
Solar Powered Noninvasive
Uploaded by
12deep2001Copyright:
Available Formats
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
Solar Powered Non-Invasive Pulse Oximeter
and Heart Rate Meter
Srushti Chavan, Prarthana Gadekar, Manjunath Patil, S.P. Tondare, S.P. Gaikwad
Department of Electronics, Bharati Vidyapeeth(Deemed to be University)College of Engineering, Pune.
Maharashtra, India.
ABSTRACT: Use of technology in healthcare is growing importance as a result of the tendency to acquire chronic
disease like heart attack and high blood pressure. Heart rate and blood oxygen saturation is a couple of such biometrics
that is monitored in this project to provide information regarding the health of the body.
Pulse Oximeter is a non-invasive medical diagnostic device used to detect the oxygen saturation of the blood. Heart
rate meter detects the number of beats per minute of the patient, normally referred to as bpm.
Our proposed pulse oximeter and Heart Rate Meter device is designed using the MAX30100 chip, integrated with
Arduino Uno and an LCD keypad shield. The chip acts as an integrated pulse oximetry and heart-rate monitor sensor
solution.
The goal of the project is to develop a low cost, small in size, easy to use, pulse oximeter and heart rate meter powered
by solar energy. The idea was conceptualized due to the fact that the oxygen saturation of blood is one of the most
important parameter to be monitored, and the pulse oximeter being low cost and solar powered, allows it to be accessed
by the developing and under developed nations.
KEYWORDS: Pulse Oximeter, Solar Energy, Micro-controller, Arduino uno, Hear-rate and SPO2 Sensor.
I. INTRODUCTION
Measurement of heart rate and pulse oximetry are very important factors to access the condition of human
cardiovascular system. Heart rate is formerly measured by placing the thumb over the arterial pulsation, and counting
the pulses usually in a 30 second period. Heart rate is then found by multiplying the obtained number by 2. This
method although simple, is not accurate and can give errors when the rate is high. In clinical environment, heart rate is
measured under controlled conditions like blood measurement, heart voice measurement, and Electrocardiogram
(ECG). ECG is one of frequently used and accurate methods for measuring the heart rate. But ECG is not economical.
The heart rate of a healthy adult at rest is around 75(+-15) (or greater for females) beats per minute (bpm).
Pulse oximetry is a noninvasive method for monitoring a person's oxygen saturation (SO2). Though its reading
of SpO2 (peripheral oxygen saturation) is not always identical to the more desirable reading of SaO2 (arterial oxygen
saturation) from arterial blood gas analysis, the two are correlated well enough that the safe, convenient, noninvasive,
inexpensive pulse oximetry method is valuable for measuring oxygen saturation in clinical use.
In its most common (transmissive) application mode, a sensor device is placed on a thin part of the patient's body,
usually a fingertip or earlobe, or in the case of an infant, across a foot. The device passes two wavelengths of light
through the body part to a photodetector. It measures the changing absorbance at each of the wavelengths, allowing it
to determine the absorbances due to the pulsing arterial blood alone, excluding venous blood, skin, bone, muscle, fat,
and (in most cases) nail polish.
Less commonly, reflectance pulse oximetry is used as an alternative to transmissive pulse oximetery described above.
This method does not require a thin section of the person's body and is therefore well suited to a universal application
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5279
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
such as the feet, forehead, and chest, but it also has some limitations. Vasodilation and pooling of venous blood in the
head due to compromised venous return to the heart can cause a combination of arterial and venous pulsations in the
forehead region and lead to spurious SpO2 results.
II. RELATED WORK
Looking back at the history of the oximeter, the first device to measure the oxygen saturation by transilluminating it
with colored light “ red and green filters”, was invented in 1935 by a German physician called Karl Matthes (1905-
1962). To include both the venous and capillary blood, an attempt was made in the period of the Second World War as
a part of a project to investigate the problem of the loss of consciousness by the American physiologist Glenn Allan
Milikan (1906-1947). However, the transmitted light through the ear is not attenuated by the arterial, venous and
capillary blood only, it is also attenuated by the skin whose pigmentation and because of that the absorption properties
varies from one person to another. In 1964, Shaw was able to assemble the world’s first absolute reading ear oximeter.
The device uses eight wavelength of light to obtain the absolute O2 saturation level in the blood. The device was
commercialized by Hewlett-Packard. The device’s use was limited to pulmonary functions and to the sleep laboratories
because of its cost and size. The first pulse oximetry was developed in 1972 by two Japanese Bioengineers, Takuo
Aoyagi and Michio Kishi who were working at Nihon Kohden Corporation. The device used the ratio of red to infrared
light absorption of the pulsating the components in the measuring site. After that, the device was commercialized by
Biox and Nellcor (which is now part of Corvidien Ltd.) in 1981 and 1983 respectively. The invention of the pulse
oximeter was a breakthrough which helped doctors and especially surgeons to get quick but yet an accurate reading to
the patient’s oxygen saturation levels. Due to its quick and accurate readings, the pulse oximeter was directly used in
the operating rooms to monitor the patient’s oxygen level. This encouraged Biox to shift their attention from initially
being concerned with respiratory care towards expanding their marketing resources to focus on operating rooms market
in late 1982. In 1983, Nellcon started to compete with Biox for the U.S operating room market. By 1987, the standard
of care in the administration of anesthetic decided to include the pulse oximeter in all the operating rooms across the
U.S. After the operating room, the use of the device spared into being used in the recovery rooms and then into the
intensive care units. In 2009, Nonin Medical Inc. introduced the world’s first fingertip pulse oximeter with Bluetooth
technology [3][4][5]. The main purpose for that was to help with the increasing need for the remote disease
management.
III. LITERATURE REVIEW
Pulse oximetry and heart rate monitoring has become most commonly used tools in the clinical environment for
assessing patients' oxygenation status. It is employed almost continuously in critical care areas and frequently in the
general ward environment. Although it is a much better tool for determining hypoxia than the human eye, its use is
limited if clinicians do not understand relevant physiological principles, such as the oxyhaemoglobin dissociation
curve and the inherent limitations of the device.
1. According to Handbook of Biomedical Instrumentation by R.S. Khandpur, techniques of measuring heart rate
are:
Average Calculation: An average rate is calculated by counting the number of pulses in given time. This method does
not show changes in time between beats and thus does not represent the true picture of hearts response to exercise,
stress and environment
Beat To Beat Calculation: This is done by measuring the time (T) in seconds, between two consecutive pulses, and
converting the time into beats/min, using the formula beat/min = 60/T.
Combination Of Beat To Beat Calculation With Averaging: This is based on four or six beats average. The advantage
of this technique over the averaging techniques is its similarity with beat to beat monitoring system. Pulse oximetry
relies on measurement of physiological signal called photoplethismography, which is an optical measurement of the
change in blood volume in the arteries. Pulse oximetry acquires PPG signals by irradiating two different wavelengths of
light through the tissue, and compares the light absorption characteristics of blood under these wavelengths. These
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5280
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
absorptions obey Beer Lamberts law. According to Beer Lamberts law transmittance of light through the tissue can be
calculated using:
Iout = Iin eA (1)
Where Iout is the light intensity transmitted through fingertip tissue, Iin is the intensity of the light going into the tissue
and A is the absorption factor.
2. According to Yousuf Jawahar, Pulse oximetry can be done by two methods :
Fig 1: Light Reflection Method Fig 2: Light Transmission Method.
Transmittance Method: In this method, light is transmitted through tissue using the LED and is detected on the other
end using a photo-detector. It is more suited to the areas of body that lend themselves better to light transmittance
through them, e.g. fingers or ear lobe. This configuration cannot be used in other areas of body when there are obstacles
such as bones or muscles.
Reflectance Method: In reflectance pulse oximetry it uses a photo detector on the same side as the LED to detect the
light reflected by the tissue. This method is more useful where the vasculature is available close to the surface of skin
e.g. forehead, wrist, forearm.
IV. METHODOLOGY
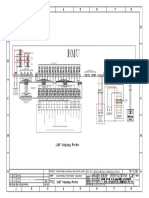
The hardware design for this project can be divided into four major parts; sensor, amplifier-filter, microcontroller and
power supply.
Fig 3: Block Diagram of Solar Powered Pulse Oximeter
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5281
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
1. Sensor:The MAX30100 chip integrates two LEDs: red and infrared (IR), a photodetector and low-noise signal
processing to detect pulse oximetry and heart rate signals. The absorption data for both IR and red light is stored
in a FIFO buffer up to 64 bytes. It provides two operating modes; the heart rate mode, and the heart rate and
oxygen saturation mode. In the heart rate mode, only the IR LED is switched on, while in the dual mode both IR
and red LEDs are switched on. It also has an integrated 60 Hz low-pass filter. While it can filter out power line
noise, it still does not account for environmental noise and fluctuations.From the LEDs, red and IR light is
transmitted through the finger and the photodetector integrated within the chip senses the light absorption of the
two separate wavelengths. In this project, we used both the oximetry and heart rate detection operations with the
MAX30100, so we can detect both heart rate and oxygen saturation at the same time.
2. Integrating the MAX30100 to the Arduino: The MAX30100 is an I2C device, therefore through code it requires
the Wire library to interface with the Arduino. Physically, the MAX30100 (in this case, the breakout board) is
connected to the Arduino through special pins that are able to read data from the SCL and SDA lines, which are
A4 and A5. The SCL and SDL lines provide the data signal and the clock signal. The ground and Vin lines are
connected to the GND and 5V lines respectively.
3. LCD : The LCD Shield is connected to the Arduino by pins 4-8 so that we can provide a user-friendly display. We
can also utilizetwo buttons on the LCD Keypad Shield, which are used to select between two modes: the heart rate
monitor and the oxygen concentration monitor.
4. Power Supply: The goal of this project, as mentioned before, is to power this device using solar cells; 12V/1.5W
solar panel is used. The output current of the solar panel in bright sunlight is about 120mA. The solar panel is
used to charge NimH rechargeable batteries having charge capacity of 2500mA. Batteries are used to power the
device during low light or no light conditions, i.e. when the solar panel is not efficient enough to drive the
electronic circuit. The output of the solar panel is given to a decoupling capacitor of 0.2uF to filter out the high
frequency noise. It is then given to a linear voltage regulator LM340LAZ-5.0 which gives out a constant DC
voltage of 5 V. The output is further given to a decoupling capacitor of 0.01uF and later given to a schottky diode
IN5817. A diode is very crucial element in the design, as it acts as reverse charge protection, i.e. it will prevent the
battery to discharge backwards into the regulator and hence into the solar panel, thus avoiding damage to those.
Schottky diode is used due to very low forward voltage drop, i.e. about 0.2-0.3V. The output of diode is about
4.8V and is appropriate in charging the rechargeable batteries. Two switches have been used, one in between the
solar panel output and the voltage regulator and second between the output of the batteries and the Vcc terminal of
main electronic circuit.
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5282
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
Fig 4: Circuit diagram of pulse oximeter
V. IMPLEMENTATION FLOW
The following flowchart shows the implementation process for finding pulse oximeter values using our project.
Fig 5: Implementation Flowchart for calculating Spo2, BPM, Temperature
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5283
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
VI. EXPERIMENTAL RESULTS
The results were checked during panting condition, and the heart rate boosted up to 105, and gradually settled for 75-80
over 5 minutes. The project does not have any safety concerns due to low input power. The product is well fabricated
and easy to use, just switch on the power and push your finger in the sensor, the display will show you the readings. The
device drew about 60mA of current, and as the charge capacity of the batteries is about 2500mAH, the device will run
efficiently for over 40 hours, which is exceptionally good time duration. Also, assuming 120mA of current from the solar
panel in bright sunlight, it will take about 20 hours to charge the batteries completely, which is fairly reasonable.
PERSON AGE SPO2 (%) HEART TEMPERATURE
RATE(BPM) (OC)
Person A 50 97 78 39
Person B 40 98 84 41
Person C 22 96 88 43
Person D 22 98 86 42
Person E 22 97 79 40
Person F 21 98 83 44
Person G 25 97 88 41
Observation Chart: For Analysis of SPO2,Heart Rate and Temperature
With our implementation of the MAX30100, we noticed that position and movement of the finger dramatically affect
the registered readings. This may be caused by how the measurement of heart rate is greatly dependent on the volume
of blood flowing through the finger, and the thickness of skin also comes into play here. If the fingers are moving
around, this may cause nonuniform light levels while acquiring a reading.
VII. CONCLUSION AND FUTURE WORK
The Heart rate and SpO2 for me was on an average 80 beats per minute and 98.23% respectively. The heart rate for
normal person is about 72 beats per minute and a normal range is about 60-90 beats per minute. The SpO2 for normal
person lies between 95-99%. SpO2 below 94% may be fatal and may cause unconsciousness. The device was designed
efficiently and met all expectations as set earlier. Due to shortage of time, the charge capacity of the batteries could not
be monitored and displayed on the LCD. The current sensor probe is not flexible for a thick finger, and can be made
much more flexible. More complex algorithm can be written to change the brightness of the LEDs with variation in the
skin thickness. Smaller solar panel could not be bought, and its inclusion will make the project really robust and ready to
use in any environment. As mentioned earlier, the device has a capability of running for over 40 hours, which will really
revolutionize the health care in under developed and developing nations which has many electricity problems. With
higher charge capacity batteries, time duration for its usage can be made longer.
People testing out our project should not move their fingers/hands around in order to acquire a stable reading. This
project can be improved by placing the sensor within an actual finger cuff that can further reduce the effects of ambient
light and also keep the finger in place, instead of just using a simple Velcro strip.
REFERENCES
1. Yoshiya I, Shimady Y, Tanake K. “Spectrophotometric monitoring of arterial oxygen saturation on the fingertip”. Med Biol Eng
Comput. 18(1):27–32(1980).
2. Wieben O. Light absorbance in pulse oximetry. In: Webster JG, editor. Design of Pulse Oximeters.Bristol: Institute of Physics; pp. 40–
55(1997).
3. Mannheimer PD, Casciani JR, Fein ME, Nierlich SL. Wavelength selection for low-saturation pulse oximetry. IEEE Trans Biomed
Eng. ;44(3):148–158(1997).
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5284
ISSN(Online): 2320-9801
ISSN (Print) : 2320-9798
International Journal of Innovative Research in Computer
and Communication Engineering
(A High Impact Factor, Monthly, Peer Reviewed Journal)
Website: www.ijircce.com
Vol. 6, Issue 5, May 2018
4. Zourabian A, Siegel A, Chance B, Ramanujan N, Rode M, Boas DA. Trans-abdominal monitoring of fetal arterial blood oxygenation using
pulse oximetry. J Biomed Optics.5(4):391–405(2000).
5. Babchenko A, Davidson E, Ginosar Y, et al. Photoplethysmographic measurement of changes in total and pulsatile tissue blood volume,
following sympathetic blockade. Physiol Meas.22(2):389–396(2001).
6. Matcher SJ. Signal quantification and localization in tissue near-infrared spectroscopy. In: Tuchin VV, editor. Handbook of Optical
Biomedical Diagnostics. Bellingham (WA): SPIE; . pp. 487–584(2002).
7. Nitzan M, Engelberg S. Three-waveleng7th technique for the measurement of oxygen saturation in arterial blood and in venous blood. J
Biomed Opt. 14(2):024046(2009).
8. Batchelder PB, Raley DM. Maximizing the laboratory setting for testing devices and understanding statistical output in pulse oximetry. Anesth
Analg. 105(Suppl 6):S85–S94(2007).
9. Seguin P, Le Rouzo A, Tanguy M, Guillou YM, Feuillu A. Evidence for the need of bedside accuracy of pulse oximetry in an intensive care
unit. Crit Care Med.28(3):703-706(2000).
10. Van de Louw A, Cracco C, Cerf C, et al. Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med. 27(10):1606–1613(2001).
11. Poets CF, Southall DP. Noninvasive monitoring of oxygenation in infants and children: practical considerations and areas of
concern. Pediatrics.93(5):737–746(1994).
12. Tungjitkusolmun S. Accuracy and errors. In: Webster JG, editor. Design of Pulse Oximeters. Bristol: Institute of Physics; pp. 176–198(1997).
13. Rosychuk RJ, Hudson-Mason A, Eklund D, Lacaze-Masmonteil T. Discrepancies between arterial oxygen saturation and functional oxygen
saturation measured with pulse oximetry in very preterm infants. Neonatology. 101(1):14–19(2012).
14. A. Milenkovic, C. Otto, and E. Jovanov, “Wireless Sensor Network for Personal Health Monitoring: Issues and an Implementation,” in
Computer Communications, vol. 29 (13- 14), August 2006.
15. F. Tay, D. Guo, L. Xu, M. Nyan, and K. Yap, “MEMS Wear bio monitoring System for Remote Vital Signs Monitoring,” in Journal of the
Franklin Institute, 346(6), 531-542, August 2009
16. Y. Shieh, Y. Tsai, A. Anavim, M. Shieh, and M. Lin, “Mobile Healthcare: Opportunities and Challenges,” in International Journal of
Electronic Healthcare, 4(2), 208-219, 2008.
17. De Kock, J. P., Tarassenko, L., Glynn, C. J., & Hill, A. R. “Reflectance pulse oximetry measurements from the retinal fundus. Biomedical
Engineering”, IEEE Transactions on, 40(8), 817-823(1993).
Copyright to IJIRCCE DOI: 10.15680/IJIRCCE.2018.0605036 5285
You might also like
- Remote Tool For Heart Control and Diagnostic Through Phonocardiography SignalDocument8 pagesRemote Tool For Heart Control and Diagnostic Through Phonocardiography SignalLionel LapinouNo ratings yet
- A Review of Wearable Health Monitoring SystemsDocument5 pagesA Review of Wearable Health Monitoring SystemsVijay KumarNo ratings yet
- IOT Based Heartbeat and Oxygen Level Monitoring SystemDocument6 pagesIOT Based Heartbeat and Oxygen Level Monitoring SystemVinay McNo ratings yet
- 14 71 Icete16 Elc Pid125Document5 pages14 71 Icete16 Elc Pid125Alaa AlauqyNo ratings yet
- Iot Based System For Heart Rate Monitoring IJERTV9IS070673Document9 pagesIot Based System For Heart Rate Monitoring IJERTV9IS070673Penrose LearningNo ratings yet
- Iot: Heart Rate Monitoring Tool Using Android With Alert Messanger Telegram SystemDocument7 pagesIot: Heart Rate Monitoring Tool Using Android With Alert Messanger Telegram Systemriki capoeiristaNo ratings yet
- Poximeter 2.0Document34 pagesPoximeter 2.0Srinivasa Reddy Devireddy100% (1)
- Real Time Self Health Monitoring System: Nternational Ournal of Nnovative Esearch in Omputer and Ommunication NgineeringDocument8 pagesReal Time Self Health Monitoring System: Nternational Ournal of Nnovative Esearch in Omputer and Ommunication NgineeringJoy loboNo ratings yet
- IOT Based Health Monitoring System UsingDocument8 pagesIOT Based Health Monitoring System UsingDoctor IggyNo ratings yet
- IoT Based Wearable Smart Health Monitoring SystemDocument9 pagesIoT Based Wearable Smart Health Monitoring SystemSneha SreenathNo ratings yet
- IOT Based Health Monitoring System Using Arduino UNODocument8 pagesIOT Based Health Monitoring System Using Arduino UNOIJRASETPublications100% (1)
- The EndDocument9 pagesThe Endahmad rehmanNo ratings yet
- Document - 2 - 6ob9 - 05042017 3Document4 pagesDocument - 2 - 6ob9 - 05042017 3SEA163TANISHA POOJARINo ratings yet
- Development of A System For Monitoring The Functional Parameters of The Heart Using A SmartphoneDocument5 pagesDevelopment of A System For Monitoring The Functional Parameters of The Heart Using A SmartphoneOpen Access JournalNo ratings yet
- Heart Rate MonitorDocument9 pagesHeart Rate MonitorLong TrầnNo ratings yet
- Internet-Of-Things-Based Sensor Module For Respiratory Tracking SystemDocument11 pagesInternet-Of-Things-Based Sensor Module For Respiratory Tracking SystemAulia AgistaNo ratings yet
- Iot in Healthcare Sector Covid 19 PatienDocument7 pagesIot in Healthcare Sector Covid 19 PatienAmol KhatkhateNo ratings yet
- Yellow Light The Next Technology For Smart WatchesDocument8 pagesYellow Light The Next Technology For Smart WatchesIJAR JOURNALNo ratings yet
- IoT Based Wearable Smart Health Monitoring System PDFDocument9 pagesIoT Based Wearable Smart Health Monitoring System PDFabishek sNo ratings yet
- WirelessBloodPressureMonitoringSystem FinalReportDocument21 pagesWirelessBloodPressureMonitoringSystem FinalReportMishti SiyaNo ratings yet
- Health Monitoring KIOSK: An Effective System For Rural Health ManagementDocument4 pagesHealth Monitoring KIOSK: An Effective System For Rural Health ManagementIJIERT-International Journal of Innovations in Engineering Research and TechnologyNo ratings yet
- Sewage Environment and Workers Health Monitoring System Using IOT and MLDocument9 pagesSewage Environment and Workers Health Monitoring System Using IOT and MLIJRASETPublicationsNo ratings yet
- 103 Aniot IeeeDocument7 pages103 Aniot IeeeBhaskar Rao PNo ratings yet
- Design and Implementation of Heartbeat Rate and Spo2 Detector by Using Iot For PatientsDocument7 pagesDesign and Implementation of Heartbeat Rate and Spo2 Detector by Using Iot For PatientsnatashaNo ratings yet
- Nanotechnology Week 5Document4 pagesNanotechnology Week 5TransHour ساعت ترجمهNo ratings yet
- Sensors: Development and Test of A Portable ECG Device With Dry Capacitive Electrodes and Driven Right Leg CircuitDocument15 pagesSensors: Development and Test of A Portable ECG Device With Dry Capacitive Electrodes and Driven Right Leg CircuitArham SheikhNo ratings yet
- Back To TopSkip To Main ContentDocument37 pagesBack To TopSkip To Main Contentskallesh21No ratings yet
- Darrshiny Ravindran Eeee PaperDocument12 pagesDarrshiny Ravindran Eeee PaperNagalingeswaran A/l ArmugamNo ratings yet
- Croptor - The Crop ProtectorDocument7 pagesCroptor - The Crop ProtectorIJRASETPublicationsNo ratings yet
- Paper 358Document8 pagesPaper 358PRATEEK SARKARNo ratings yet
- 15 - Batch 15Document7 pages15 - Batch 15DHINESHKUMAR MNo ratings yet
- Sensors: Optical Fibre Pressure Sensors in Medical ApplicationsDocument34 pagesSensors: Optical Fibre Pressure Sensors in Medical ApplicationsShwaraj TuseNo ratings yet
- Presented By: Shaikh Yusuf Babu M.SC 2 Year (Industrial Automation) J.E.S College Jalna-431203Document20 pagesPresented By: Shaikh Yusuf Babu M.SC 2 Year (Industrial Automation) J.E.S College Jalna-431203aman lakherwalNo ratings yet
- Health Monitoring Tracking System Using GPS and GSM ModuleDocument2 pagesHealth Monitoring Tracking System Using GPS and GSM ModuleEditor IJTSRDNo ratings yet
- Low-Cost Phonocardiogram Board With Graphic LCD, Solar Panel and Embedded Heart Sound AnalyserDocument7 pagesLow-Cost Phonocardiogram Board With Graphic LCD, Solar Panel and Embedded Heart Sound AnalyserLionel LapinouNo ratings yet
- Impact Factor: 8.423: Volume 12, Issue 4, April 2023Document9 pagesImpact Factor: 8.423: Volume 12, Issue 4, April 2023ted gcgdNo ratings yet
- On Development of Mysignals Based Prototype For Application in Health Vitals MonitoringDocument18 pagesOn Development of Mysignals Based Prototype For Application in Health Vitals Monitoringbiomedical bpiNo ratings yet
- IOT Based Wearable Health Monitoring System For Pregnant LadiesDocument5 pagesIOT Based Wearable Health Monitoring System For Pregnant LadiesPenrose LearningNo ratings yet
- IoT Based Wearable Smart Health Monitoring SystemDocument18 pagesIoT Based Wearable Smart Health Monitoring SystemRutuja VartaleNo ratings yet
- Design of A SpO 2 Pulse Oximeter Prototy PDFDocument63 pagesDesign of A SpO 2 Pulse Oximeter Prototy PDFPedro Augusto AlvesNo ratings yet
- Heart Rate EngineeringDocument7 pagesHeart Rate EngineeringSathishKumarNo ratings yet
- Smart Mobile App For Remote Health Monitoring System Using Iot IJERTCONV9IS12016Document7 pagesSmart Mobile App For Remote Health Monitoring System Using Iot IJERTCONV9IS12016Ajay SinghNo ratings yet
- Design and Evaluation of A Low-Cost Smartphone Pulse OximeterDocument13 pagesDesign and Evaluation of A Low-Cost Smartphone Pulse Oximetermahsa sherbafiNo ratings yet
- Internet of Things IoT Based Healthcare Monitoring System Using NodeMCU and Arduino UNODocument5 pagesInternet of Things IoT Based Healthcare Monitoring System Using NodeMCU and Arduino UNOEditor IJTSRD100% (1)
- 204 Patients SPCETDocument5 pages204 Patients SPCETluv_angel88No ratings yet
- Real Time Wireless Health Monitoring SystemDocument9 pagesReal Time Wireless Health Monitoring SystemWekesa RobinsonNo ratings yet
- 9B Documentation (MAJOR)Document55 pages9B Documentation (MAJOR)dulipala alekya gupthaNo ratings yet
- Boe 10 11 5940Document12 pagesBoe 10 11 5940puma flyerNo ratings yet
- Optical Fibre Pressure Sensors in Medical ApplicationsDocument35 pagesOptical Fibre Pressure Sensors in Medical Applicationsabhist singhNo ratings yet
- Wireless Monitoring of Physiological Data Using Nexus-10 & BiotraceDocument64 pagesWireless Monitoring of Physiological Data Using Nexus-10 & BiotraceInternational Journal of Application or Innovation in Engineering & ManagementNo ratings yet
- A Simple Portable ECG Monitor With IOTDocument8 pagesA Simple Portable ECG Monitor With IOTArham SheikhNo ratings yet
- Implementation of Home Monitoring System Using Labview For CHFDocument4 pagesImplementation of Home Monitoring System Using Labview For CHFIJIERT-International Journal of Innovations in Engineering Research and TechnologyNo ratings yet
- Design and Development of Patient Monitoring SysteDocument7 pagesDesign and Development of Patient Monitoring SysteMuhammad MustakimNo ratings yet
- IOT Based Smart Wearable Health Monitoring System For Corona DiagnosisDocument28 pagesIOT Based Smart Wearable Health Monitoring System For Corona DiagnosisIJRASETPublicationsNo ratings yet
- 105 1460353115 - 11-04-2016 PDFDocument4 pages105 1460353115 - 11-04-2016 PDFEditor IJRITCCNo ratings yet
- Asthma ZigbeeDocument4 pagesAsthma ZigbeeBlue OceanNo ratings yet
- Telemedicine ReportDocument26 pagesTelemedicine ReportFaiyaz FarahNo ratings yet
- Design of Body Vitals Measurement SystemDocument4 pagesDesign of Body Vitals Measurement Systempratik16892No ratings yet
- Health Monitoring System Using MicrocontrollerDocument8 pagesHealth Monitoring System Using MicrocontrollerIJRASETPublicationsNo ratings yet
- New Frontiers of Cardiovascular Screening using Unobtrusive Sensors, AI, and IoTFrom EverandNew Frontiers of Cardiovascular Screening using Unobtrusive Sensors, AI, and IoTNo ratings yet
- 13 - L-7 (DK) (Pe) ( (Ee) Nptel)Document1 page13 - L-7 (DK) (Pe) ( (Ee) Nptel)GagneNo ratings yet
- ELEC4810: Introduction To Biosensors and Bioinstrumentation: Lecture Notes - Set #10Document17 pagesELEC4810: Introduction To Biosensors and Bioinstrumentation: Lecture Notes - Set #10Kwan ChanNo ratings yet
- Millermatic 211: Processes OM265809BDocument52 pagesMillermatic 211: Processes OM265809BronaldmarcelleNo ratings yet
- Display, Operate, Switch, Control, Regulate and Communicate: For Sales and SupportDocument24 pagesDisplay, Operate, Switch, Control, Regulate and Communicate: For Sales and SupportVictor Rolando Tarifa BlancoNo ratings yet
- Single Phase Inverter With HD-Wave Technology: For North AmericaDocument3 pagesSingle Phase Inverter With HD-Wave Technology: For North AmericaDAVID ALEX DE OLIVEIRA SOUSANo ratings yet
- Product Specifications 40" WXGA Color TFT-LCD Module Model Name: T400XW01 V5Document27 pagesProduct Specifications 40" WXGA Color TFT-LCD Module Model Name: T400XW01 V5marciocambruzziNo ratings yet
- GrandMA3 ManualDocument41 pagesGrandMA3 ManualMisael HernándezNo ratings yet
- Raymarine - Ray230 Technical ManualDocument72 pagesRaymarine - Ray230 Technical ManualJonathan LeivaNo ratings yet
- Industrial Training Lab: Swami Keshvanand Institute of Technology& Gramothan, JaipurDocument18 pagesIndustrial Training Lab: Swami Keshvanand Institute of Technology& Gramothan, JaipurAviral JainNo ratings yet
- RS485 Wi-Fi: Digital InputDocument1 pageRS485 Wi-Fi: Digital InputDeepak KumarNo ratings yet
- Types of Solar Power Systems - Grid-Connected System, Off-Grid, DCDocument4 pagesTypes of Solar Power Systems - Grid-Connected System, Off-Grid, DCAnas Abd RahmanNo ratings yet
- Start-Up Inspection For Generac Power Systems Industrial Product - EditableDocument8 pagesStart-Up Inspection For Generac Power Systems Industrial Product - EditableasdrubalaraujoNo ratings yet
- S Feature D Escriptio: LTC1487 Ultra-Low Power RS485 With Low EMI, Shutdown and High Input ImpedanceDocument8 pagesS Feature D Escriptio: LTC1487 Ultra-Low Power RS485 With Low EMI, Shutdown and High Input ImpedanceIndra CandraNo ratings yet
- Gls 17 User ManualDocument13 pagesGls 17 User ManualRobertoNo ratings yet
- 10m Microphone Cable PDFDocument3 pages10m Microphone Cable PDFmasudur rahmanNo ratings yet
- Daewoo Dvd-p480 SMDocument67 pagesDaewoo Dvd-p480 SMfrewellNo ratings yet
- E10-S01 - 0 Adjustable Freq Drive For Low Voltage MotorDocument11 pagesE10-S01 - 0 Adjustable Freq Drive For Low Voltage MotorMuhammad IrfanNo ratings yet
- Product Information: Industrial X-Ray Tube I-2115A Toshiba X-Ray Tube For Industrial UseDocument5 pagesProduct Information: Industrial X-Ray Tube I-2115A Toshiba X-Ray Tube For Industrial UseKamilNo ratings yet
- AC-DC Converter - Single PhaseDocument16 pagesAC-DC Converter - Single Phasebishnu prasad muniNo ratings yet
- Dcss 5 Guide 2Document43 pagesDcss 5 Guide 2Isaac MangochiNo ratings yet
- EE3405 Electrical Machines II PDFDocument6 pagesEE3405 Electrical Machines II PDFkaviinfoenggNo ratings yet
- Chapter 3Document25 pagesChapter 3Ahmed 4testNo ratings yet
- Performance Enhancement of Photovoltaic Water Pumping System Based On BLDC Motor Under Partial Shading ConditionDocument9 pagesPerformance Enhancement of Photovoltaic Water Pumping System Based On BLDC Motor Under Partial Shading ConditionRahul KrishnaNo ratings yet
- Raman PDFDocument3 pagesRaman PDFAla TulleNo ratings yet
- AN02 How To Draw Schematic DiagramsDocument7 pagesAN02 How To Draw Schematic DiagramsÎQbãl HãikãmNo ratings yet
- Single-Phase To Three-Phase Power Converters: State of The ArtDocument16 pagesSingle-Phase To Three-Phase Power Converters: State of The Artnl vinay kumarNo ratings yet
- BR FD1 6 en 2022 08 23Document1 pageBR FD1 6 en 2022 08 23M SNo ratings yet
- 6SL3210 1PE18 0AL1 Datasheet enDocument2 pages6SL3210 1PE18 0AL1 Datasheet enJose ValenciaNo ratings yet
- sv2 PiDocument35 pagessv2 PiM. U.100% (1)
- Article-No.: 303004: Gas Detection Control Unit ET-1D in Wall Mounted Housing, 24 V DCDocument2 pagesArticle-No.: 303004: Gas Detection Control Unit ET-1D in Wall Mounted Housing, 24 V DCDraganNo ratings yet