Professional Documents
Culture Documents
Generalized Anxiety Disorder Psychiatric Comorbidities
Generalized Anxiety Disorder Psychiatric Comorbidities
Uploaded by
Carlos Luque GOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Generalized Anxiety Disorder Psychiatric Comorbidities
Generalized Anxiety Disorder Psychiatric Comorbidities
Uploaded by
Carlos Luque GCopyright:
Available Formats
Naomi M.
Simon
Generalized Anxiety Disorder and Psychiatric Comorbidities
Such as Depression, Bipolar Disorder, and Substance Abuse
Naomi M. Simon, MD, MSc
Generalized anxiety disorder (GAD) has a high rate of comorbidity with other psychiatric disor-
ders, including major depressive disorder (MDD), bipolar disorder, other anxiety disorders, and sub-
stance use disorders. The similarities between GAD and MDD have led some to suggest that GAD
should be reclassified as a mood disorder. The concurrence of GAD with another disorder heightens a
patient’s risk for impairment, disability, and suicidality. Clinical trials for GAD and disorders that are
most likely to occur with GAD have generally not taken comorbidity into account, and there is a pau-
city of data guiding how comorbidity should inform treatment selection. Research into the biology
and psychopathology underlying the high rate of comorbidity of GAD and into efficacious interven-
tions for GAD with comorbidity is needed. (J Clin Psychiatry 2009;70[suppl 2]:10–14)
G eneralized anxiety disorder (GAD) is one of the
most common anxiety disorders1 and is frequently
comorbid with several other psychiatric disorders, each of
the National Comorbidity Survey suggest that 67% of in-
dividuals with GAD have a lifetime unipolar depressive
disorder, 17% have bipolar disorder, and only 16% have
which may complicate the diagnosis, treatment, and out- no lifetime mood disorder.3 Wittchen et al4 similarly re-
come for the patient. Anxiety disorders and comorbid dis- ported that individuals with GAD have a 90% likelihood
orders can be difficult to detect when evaluating patients if of at least 1 comorbid psychiatric diagnosis in their life-
the diagnostic process does not include a clinical interview time. Highest among these comorbidities were MDD and
specifically structured to detect anxiety disorders. One dysthymia, while alcohol abuse and dependence, simple
study2 supporting this notion found that a substantially phobia, and social anxiety disorder were also common
higher percentage of individuals with major depressive (Figure 1).
disorder (MDD) who were assessed with a semistructured
diagnostic interview were diagnosed with GAD, whereas GAD and MDD
a smaller percentage assessed with an unstructured inter- Anxiety disorders tend to develop relatively early in
view were diagnosed with GAD. life, and, therefore, as many studies suggest, they fre-
quently occur before the first episode of MDD.5 GAD may
GAD COMORBIDITIES be a prodrome to MDD in the individuals who later de-
velop this comorbidity. In fact, after an individual has a
Individuals with lifetime GAD have an extremely high new onset of GAD, he or she has an increased likelihood
rate of lifetime mood disorders. Epidemiologic data from of developing a major depressive episode within the year
than someone without an anxiety disorder.5
Conversely, some longitudinal prospective data of chil-
From the Center for Anxiety and Traumatic Stress Disorders, dren and young adults suggest that order of onset may be
Massachusetts General Hospital, and the Department of Psychiatry,
Harvard Medical School, Boston. more varied, with about one third of individuals with GAD
This article is derived from the planning teleconference series having anxiety onset prior to the onset of MDD, about one
“Insights Into Generalized Anxiety Disorder,” which was held
June–August 2008, and supported by an educational grant from third having the disorders onset concurrently, and about
AstraZeneca Pharmaceuticals LP. one third having onset of MDD first.6 Of note, one study
Dr Simon has served as a consultant for the American that followed individuals until age 32 years found that
Foundation for Suicide Prevention and Pfizer; has received grants
or research support from AstraZeneca, Cephalon, Forest, 72% of cases of lifetime GAD also had lifetime MDD.
GlaxoSmithKline, Janssen, Eli Lilly, the National Alliance for Even GAD defined more loosely, with only a 1-month
Research on Schizophrenia and Depression, the National Institute
of Mental Health, Pfizer, UCB Pharma, and Sepracor; has been a requirement for symptom duration, has a substantial co-
speaker for MGH Psychiatry Academy and AstraZeneca; and has morbidity with mood and anxiety disorders, although in-
participated in sponsored trials for Janssen, UCB Pharma, and
Sepracor.
creased severity of GAD is associated with greater likeli-
Corresponding author and reprints: Naomi M. Simon, MD, MSc, hood of prediction of subsequent depression.7
Massachusetts General Hospital, Center for Anxiety and Traumatic Impairment and disability. A primary care study8 that
Stress Disorders, Department of Psychiatry, Simches 2200, 185
Cambridge St, Boston, MA 02114 (e-mail: nsimon@partners.org). defined impairment as an inability to work on at least 1
© Copyright 2009 Physicians Postgraduate Press, Inc. day within the past month found that 67% of patients with
10 PSYCHIATRIST.COM J Clin Psychiatry 2009;70 (suppl 2)
Generalized Anxiety Disorder and Comorbidities
FOR CLINICAL USE
◆ Generalized anxiety disorder (GAD) can be difficult to detect as a comorbid condition.
Clinicians should use structured evaluations designed to detect the presence of anxiety and
other comorbid disorders.
◆ The comorbidity of GAD and other psychiatric disorders puts patients at risk for increased
impairment and disability. Although comorbidity treatment data are limited, clinicians can
consider each concurrent disorder when selecting treatment to minimize these risks.
◆ The onset of secondary MDD in GAD may be preventable with appropriate intervention,
although additional research is needed.
pure GAD and 68% of patients with pure MDD were be determined by environmental factors such as stressful
impaired, but those with comorbid GAD and MDD had life events.
an 81% rate of impairment. The impairment rate was Pursuing this hypothesis, Kendler et al12 classified
17% if neither GAD nor MDD were present. stressful life events into categories of loss, humiliation,
In general, additive psychiatric comorbidity has been danger, and entrapment and examined how subjects with
associated with greater disability; one study9 found an GAD, MDD, or both described their stressful experiences
increase in the level of disability as the number of comor- within 1 month of onset. Of the 4 categories, loss and dan-
bid psychiatric disorders increased. A meta-analysis by ger were associated with the most risk for GAD, while loss
Hoffman et al10 analyzed the impact of both pure GAD and humiliation were associated with the most risk for
and GAD comorbid with depression or other disorders MDD and comorbid GAD and MDD. Entrapment was as-
on functioning and quality of life. While GAD alone is sociated only with comorbid GAD and MDD.
clearly associated with disability and impaired quality Debate is ongoing about whether genetics will ulti-
of life, patients with comorbidity increased impairment mately better explain mood-related and anxiety-related
overall. This finding highlights the importance of not traits such as neuroticism rather than specific DSM mood
only diagnosing the first disorder but also testing for the and anxiety diagnoses.13 Neuroticism has been found to be
presence of comorbid conditions. a risk factor for both GAD and MDD.14 Kendler et al15
Biologic and environmental risks. There is a paucity demonstrated that, if one has a high level of neuroticism, a
of data examining the biology underlying the presence of less severe stressful life event is more likely to trigger the
comorbidity in GAD, and more attention to this is needed onset of a major depressive episode than if an individual
in pathophysiology studies of GAD in general. One hy- has a low level of neuroticism. This finding may be true
pothesis is that the onset of the anxiety disorder may for anxiety disorders as well; data suggest that underlying
serve as a stressor triggering an underlying neurobiologic vulnerability and life stressors have additive risk for the
vulnerability to MDD, perhaps mediated by serotonergic development of anxiety in late life.16
dysregulation. Similarly, the overlapping risk may be Another possibility for individuals with GAD is that
related to hypothalamic-pituitary-adrenal axis dysfunc- the negative psychological impact of work and social dys-
tion. More research examining the underlying neurobiol- function due to GAD itself may result in depression and
ogy of GAD and MDD comorbidity is needed, with atten- demoralization about the anxiety disorder and associated
tion to comorbidity in ongoing studies of GAD. impairment which, in some cases, may trigger MDD. This
One contributing factor to the high comorbidity rate pathway would support the possibility that early interven-
of GAD and MDD may be overlapping genetic factors. tion for GAD could reduce the prevalence of later MDD.
In a study of identical and nonidentical female twin pairs, Questions concerning classification. Some overlap
Kendler11 found the same genetic risk factors for GAD in the diagnostic criteria for GAD and MDD exists in
and MDD. Another possibility is that environmental DSM-IV, and contemporary researchers continue to ques-
stressors interact with underlying genetic risks to produce tion whether GAD and depression should be classified as
anxiety and depressive disorders. Researchers have hy- distinct disorders in the upcoming DSM-V.17–20 Because
pothesized that the environmental risk factors that pre- of the symptom overlap (i.e., irritability, insomnia, and
dispose an individual to GAD might be distinct from trouble with concentration), high rate of lifetime comor-
those that increase the risk for MDD. Thus, the develop- bidity, overlapping antidepressant response, shared trait
ment of one disorder instead of the other may be due risk factor of neuroticism, and shared genetic risks be-
to a difference in the patterns of life stress. In other tween GAD and MDD, some in the field have questioned
words, someone may have an underlying biologic risk, whether GAD should be reclassified as a mood disorder
but whether it becomes expressed as GAD or MDD could instead of as an anxiety disorder. Slade and Watson21 have
J Clin Psychiatry 2009;70 (suppl 2) PSYCHIATRIST.COM 11
Naomi M. Simon
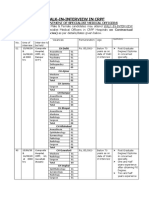
Figure 1. Lifetime Prevalence of Comorbid Disorders in Figure 2. Lifetime Anxiety Comorbidity in 475 Patients With
Patients With GADa Bipolar Disordera
100
60
Patients With Comorbid Disorder, %
Bipolar I Disorder
90
Bipolar II Disorder
80 50
Lifetime Prevalence, %
70
60 40
50
30
40
30 20
20
10 10
0
0
r
ia
ia
ia
ia
de
de
Any Anxiety Disorder Generalized Anxiety Disorder
io
nc
nc
bi
ym
ob
an
ss
ho
ho
or
or
de
de
Ph
M
th
is
re
is
P
ap
en
en
ys
D
D
ep
al
or
ep
ep
D
pl
y
c
ci
D
Ag
a
Data from Simon et al.24
An
ni
m
So
D
D
or
Pa
Si
d
d
aj
an
an
M
se
e
us
bu
Ab
lA
g
ho
ru
co
As with MDD, comorbid anxiety can worsen the course
Al
a
Data from Wittchen et al. 4 of bipolar disorder. Anxiety disorders concurrent with bi-
polar disorder are associated with a younger age at bipolar
onset, poorer role functioning and decreased quality of
suggested that GAD and MDD should both be classified life, substantially less time spent euthymic, lower likeli-
as distress-based internalizing disorders along with post- hood of recovery, greater risk of comorbid substance use
traumatic stress disorder and dysthymic disorder, as op- disorder (SUD), and a greater lifetime risk of suicide at-
posed to fear-based internalizing disorders such as panic, tempts.24 The mean duration of the longest euthymic pe-
social anxiety, and obsessive-compulsive disorders and riod during the prior 2 years for patients entering the
agoraphobia. STEP-BD study with current GAD was less than half that
Despite the commonalities between GAD and MDD, of those who had bipolar disorder only. Further, a prospec-
the syndromes do have distinguishing factors. For tive follow-up25 of patients with bipolar disorder in the
instance, as already noted, the environmental triggers STEP-BD study documented that those with comorbid
appear to differ. Additionally, neuropsychological stud- GAD lost an estimated 29 days well (defined as relative
ies22,23 have shown that the attentional bias differs be- euthymia) during the 12 months they were followed com-
tween individuals with depression, who focus on negative pared with individuals without an anxiety disorder.
affect, and individuals with GAD, who focus on threat. About twice as many patients with bipolar disorder and
Finally, benzodiazepines are not effective treatment for comorbid GAD appear to have a history of at least 1 sui-
depression, as they are for GAD, suggesting that some dif- cide attempt compared with those without GAD.24 Among
ferences in the underlying biology of GAD and MDD are patients with bipolar disorder and current GAD, 62% re-
likely. ported having attempted suicide, and, among patients with
Given the available data, it is probably premature to bipolar disorder and lifetime GAD, the rate was about
make a judgment concerning the reclassification of GAD. 53% compared to 22% of those without a lifetime anxiety
The issue will be a topic of discussion for DSM-V evalua- disorder.24
tion groups. Impulsivity is a core feature of bipolar disorder, and the
presence of a comorbid anxiety disorder has been theo-
GAD and Bipolar Disorder rized to reduce the likelihood of impulsiveness. However,
Until recently, the frequent comorbidity of GAD and Taylor and colleagues26 demonstrated that individuals with
bipolar disorder has been underappreciated in the clinical bipolar disorder and a current anxiety disorder have a sig-
setting. Baseline data from the Systematic Treatment En- nificantly higher level of impulsivity, as measured by the
hancement Program for Bipolar Disorder (STEP-BD)24 Barratt Impulsiveness Scale, than those without an anxiety
showed that approximately 18% of subjects with bipolar disorder (P = .002). Higher impulsivity was predicted at
disorder had a lifetime occurrence of GAD, with rates be- 9-month follow-up by higher levels of baseline panic at-
ing somewhat higher for bipolar I than for bipolar II disor- tack frequency, phobic avoidance, anxiety sensitivity, fear
der; fully 51% of bipolar disorder patients overall had at of negative evaluation, and worry. The association of anx-
least 1 type of lifetime anxiety disorder (Figure 2). iety symptoms with increased impulsivity was present
12 PSYCHIATRIST.COM J Clin Psychiatry 2009;70 (suppl 2)
Generalized Anxiety Disorder and Comorbidities
Figure 3. Risk of Developing MDD in Untreated GADa psychotropic doses for the treated group. Targeted, pro-
spective research examining the impact of both pharma-
20 cotherapy and psychotherapy interventions for GAD on
Risk of Developing Secondary MDD, %
MDD prevention is needed, but initial results support the
hypothesis that treating GAD early may help prevent the
onset of later MDD for the subset of patients with GAD
but no current depression.
10 The presence of anxiety comorbidity in patients with
primary depression has also been demonstrated to inter-
*
fere with treatment response. Researchers with the Se-
quenced Treatment Alternatives to Relieve Depression
(STAR*D) study evaluated 2,876 adult outpatients who
0
Untreated Treated
were given first-line pharmacotherapy treatment with ci-
talopram and found that those with anxious depression
a
Data from Goodwin and Gorman.28 had significantly lower remission rates—22% versus 33%
*At least 4 doses of psychotropic medication.
Abbreviations: GAD = generalized anxiety disorder, MDD = major (P < .0001)—according to the 17-item Hamilton Rating
depressive disorder. Scale for Depression scores and a longer time to remission
than those with nonanxious depression.29 Anxious depres-
sion was also associated with a worse side-effect profile
even after statistical adjustments for age, gender, SUD co- and a poorer response in the next treatment stages for ci-
morbidity, and current mood episode. talopram nonresponders in STAR*D.
Examining baseline data from the STEP-BD database,
GAD and Substance Use Disorders Simon et al30 evaluated whether comorbid anxiety disor-
Using data from the National Epidemiologic Survey ders had any impact on naturalistic pharmacotherapy
on Alcohol and Related Conditions, Compton and col- treatment of bipolar disorder. The presence of anxiety dis-
leagues27 reported that GAD is associated with signifi- orders was minimally associated with pharmacotherapy
cantly increased odds for 12-month SUD. They reported selection. In fact, only 59% of all patients met study crite-
odds ratios of 4.5 for drug use disorders, 2.0 for drug ria for receiving adequate mood stabilizer treatment, sug-
abuse, and 9.5 for drug dependence in the presence of gesting that clinicians do not have optimal, evidence-
GAD, after adjusting for demographic characteristics. Af- based pharmacotherapies available for bipolar disorder
ter adjusting for other psychiatric comorbidities as well, regardless of the presence of comorbidity. Of patients with
the odds ratios were lower, but the risk for drug depen- current GAD comorbidity, 33% were receiving minimally
dence was still significant (OR = 2.5). The investigators adequate anxiolytic pharmacotherapy. Likely reasons for
recommended further research on common factors, such inadequate treatment include a lack of data to support ap-
as genetic risk, that may underlie both types of disorders. propriate choices in the setting of comorbid anxiety and
bipolar disorder, risk of mania and possibly increased cy-
PHARMACOTHERAPY AND RELATED ISSUES FOR cling with antidepressant use in patients with bipolar dis-
GAD AND COMORBID CONDITIONS order, and concerns about using benzodiazepines in pa-
tients who have a higher risk of SUD comorbidity. A
Although comorbidity between GAD and other disor- simple lack of anxiety disorder detection in the bipolar set-
ders is common, and patients with GAD and comorbid ting, as with MDD, may also contribute to the problem of
conditions clearly present for treatment in the clinical set- treatment inadequacy.
ting, few data about how these comorbidities should in-
form treatment selection are available. Unfortunately, SUMMARY
pharmaceutical trials have generally not attended to the is-
sue of comorbidity, with large US Food and Drug Admin- Despite high rates of comorbidity, GAD is commonly
istration randomized controlled trials specifically exclud- underdiagnosed and undertreated in patients with other
ing most comorbid psychiatric disorders. psychiatric disorders, especially MDD, bipolar disorder,
Limited but intriguing data, however, suggest that treat- and SUD. Clinicians should evaluate patients with GAD
ing GAD may serve to limit the onset of secondary MDD. for medical, psychiatric, and substance comorbidities. Pa-
One study28 compared patients with GAD who had been tients with GAD and comorbid disorders are at risk for in-
treated with psychotropics to patients with GAD who were creased impairment, disability, and suicidality, as well as
untreated. A higher incidence of secondary MDD was for poorer quality of life and role function. Careful treat-
found among the untreated group (Figure 3). These results ment selection must take into consideration each disorder
were acquired using a minimum requirement of 4 known to offer the best outcome.
J Clin Psychiatry 2009;70 (suppl 2) PSYCHIATRIST.COM 13
Naomi M. Simon
Drug name: citalopram (Celexa). between major depression and generalized anxiety disorder in a Swedish
national twin sample. Psychol Med. 2007;37(3):453–462.
Disclosure of off-label usage: The author has determined that, to the 15. Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism,
best of her knowledge, citalopram is not approved by the US Food sex, and stressful life events in the prediction of episodes of major
and Drug Administration for the treatment of anxious depression. depression. Am J Psychiatry. 2004;161(4):631–636.
16. de Beurs E, Beekman AT, Deeg DJ, et al. Predictors of change in anxiety
symptoms of older persons: results from the Longitudinal Aging Study
REFERENCES Amsterdam. Psychol Med. 2000;30(3):515–527.
17. Hettema JM. The nosologic relationship between generalized anxiety
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age- disorder and major depression. Depress Anxiety. 2008;25(4):300–316.
of-onset distributions of DSM-IV disorders in the National Comorbidity 18. Stein MB. Neurobiology of generalized anxiety disorder. J Clin Psychi-
Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. atry. 2009;70(suppl 2):15–19.
2. Zimmerman M, Chelminski I. Clinician recognition of anxiety disorders 19. Andrews G, Anderson TM, Slade T, et al. Classification of anxiety and
in depressed outpatients. J Psychiatr Res. 2003;37(4):325–333. depressive disorders: problems and solutions. Depress Anxiety. 2008;
3. Judd LL, Kessler RC, Paulus MP, et al. Comorbidity as a fundamental 25(4):278–281.
feature of generalized anxiety disorders: results from the National Comor- 20. Kessler RC, Keller MB, Wittchen HU. The epidemiology of generalized
bidity Study (NCS). Acta Psychiatr Scand Suppl. 1998;98(393):6–11. anxiety disorder. Psychiatr Clin North Am. 2001;24(1):19–39.
4. Wittchen HU, Zhao S, Kessler RC, et al. DSM-III-R generalized anxiety 21. Slade T, Watson D. The structure of common DSM-IV and ICD-10
disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994; mental disorders in the Australian general population. Psychol Med.
51(5):355–364. 2006;36(11):1593–1600.
5. Kessler RC, Nelson CB, McGonagle KA, et al. Comorbidity of DSM-III- 22. Leppanen JM. Emotional information processing in mood disorders: a
R major depressive disorder in the general population: results from the review of behavioral and neuroimaging findings. Curr Opin Psychiatry.
US National Comorbidity Survey. Br J Psychiatry. 1996;168(suppl 30): 2006;19(1):34–39.
17–30. 23. Hazen RA, Vasey MW, Schmidt NB. Attentional retraining: a random-
6. Moffitt TE, Harrington H, Caspi A, et al. Cumulative and sequential co- ized clinical trial for pathological worry [published online ahead of print
morbidity in a birth cohort followed prospectively to age 32 years. Arch Aug 21, 2008]. J Psychiatry Res. doi: 10.1016/j.j psychives.2008.07.004
Gen Psychiatry. 2007;64(6):651–660. 24. Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comor-
7. Ruscio AM, Chiu WT, Roy-Byrne P, et al. Broadening the definition of bidity in bipolar disorder patients: data from the first 500 participants in
generalized anxiety disorder: effects on prevalence and associations with the Systematic Treatment Enhancement Program for Bipolar Disorder
other disorders in the National Comorbidity Survey Replication. J Anxiety (STEP-BD). Am J Psychiatry. 2004;161(12):2222–2229.
Disord. 2007;21(5):662–676. 25. Otto MW, Simon NM, Wisniewski SR, et al. Prospective 12-month
8. Wittchen HU, Kessler RC, Beesdo K, et al. Generalized anxiety and course of bipolar disorder in out-patients with and without comorbid
depression in primary care: prevalence, recognition, and management. anxiety disorders. Br J Psychiatry. 2006;189(1):20–25.
J Clin Psychiatry. 2002;63(suppl 8):24–34. 26. Taylor CT, Hirshfeld-Becker DR, Ostacher MJ, et al. Anxiety is
9. Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: associated with impulsivity in bipolar disorder. J Anxiety Disord. 2007;
data from the Australian National Survey of Mental Health and Well- 22(5):868–876.
Being. Br J Psychiatry. 2002;181(4):306–314. 27. Compton WM, Thomas YF, Stinson FS, et al. Prevalence, correlates,
10. Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden disability, and comorbidity of DSM-IV drug abuse and dependence in
of generalized anxiety disorder. Depress Anxiety. 2008;25(1):72–90. the United States: results from the National Epidemiologic Survey on
11. Kendler KS. Major depression and generalised anxiety disorder: same Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(5):
genes, (partly) different environments revisited. Br J Psychiatry Suppl. 566–576.
1996;30(6):68–75. 28. Goodwin RD, Gorman JM. Psychopharmacologic treatment of general-
12. Kendler KS, Hettema JM, Butera F, et al. Life event dimensions of loss, ized anxiety disorder and the risk of major depression. Am J Psychiatry.
humiliation, entrapment, and danger in the prediction of onsets of major 2002;159(11):1935–1937.
depression and generalized anxiety. Arch Gen Psychiatry. 2003;60(8): 29. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in
789–796. patients with anxious versus nonanxious depression: a STAR*D report.
13. Smoller JW, Gardner-Schuster E, Misiaszek M. Genetics of anxiety: Am J Psychiatry. 2008;165(3):342–351.
would the genome recognize the DSM? Depress Anxiety. 2008;25(4): 30. Simon NM, Otto MW, Weiss RD, et al. Pharmacotherapy for bipolar
368–377. disorder and comorbid conditions: baseline data from STEP-BD. J Clin
14. Kendler KS, Gardner CO, Gatz M, et al. The sources of co-morbidity Psychopharmacol. 2004;24(5):512–520.
14 PSYCHIATRIST.COM J Clin Psychiatry 2009;70 (suppl 2)
You might also like
- LPL - PSC Rajouri Garden Home Visit: Patientreportscsuperpanel - SP - General - Template01 - SC (Version: 7)Document2 pagesLPL - PSC Rajouri Garden Home Visit: Patientreportscsuperpanel - SP - General - Template01 - SC (Version: 7)Rabinder BakhshiNo ratings yet
- Bipolar Disorder and ADHD - BrusDocument10 pagesBipolar Disorder and ADHD - BrusKaitNo ratings yet
- Advocacy Letter To LegislatorDocument3 pagesAdvocacy Letter To LegislatorDenisse CastilloNo ratings yet
- Final Capstone PaperDocument15 pagesFinal Capstone Paperapi-478784238No ratings yet
- 1 s2.0 S0924977X0600071X MainDocument10 pages1 s2.0 S0924977X0600071X MainCarlos Luque GNo ratings yet
- Generalized Anxiety Disorder: The Diagnosis and Treatment ofDocument20 pagesGeneralized Anxiety Disorder: The Diagnosis and Treatment ofRonaMaulidiaBakhitaNo ratings yet
- Generalized Anxiety Disorder Nature CourseDocument5 pagesGeneralized Anxiety Disorder Nature Course11. Nguyễn Võ Như HuỳnhNo ratings yet
- Goldberg 2012Document8 pagesGoldberg 2012Carlos Luque GNo ratings yet
- Treating Generalized Anxiety DisorderDocument3 pagesTreating Generalized Anxiety DisordermarnitNo ratings yet
- Major Depressive Disorder. NatureDocument20 pagesMajor Depressive Disorder. NatureMANUEL ALCIDES PUERTA BARRETO100% (1)
- Overview of Generalized Anxiety DisorderDocument6 pagesOverview of Generalized Anxiety Disordernandaas887No ratings yet
- Generalized Anxiety Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis PDFDocument7 pagesGeneralized Anxiety Disorder - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis PDFdreaming100% (1)
- Treatment of Anxiety DisordersDocument16 pagesTreatment of Anxiety DisordersNabilaa MaidinNo ratings yet
- Park, 2019 - NEJM - DepressionDocument10 pagesPark, 2019 - NEJM - DepressionFabian WelchNo ratings yet
- Manejo Depresion 1Document10 pagesManejo Depresion 1Luis HaroNo ratings yet
- Suicide and Treatm EntDocument8 pagesSuicide and Treatm EntSourav DasNo ratings yet
- Jamapsychiatry Ruscio 2017 Oi 170004Document11 pagesJamapsychiatry Ruscio 2017 Oi 170004Koas aningNo ratings yet
- Comorbid Depression in Medical DiseasesDocument22 pagesComorbid Depression in Medical DiseasesArmando Marín FloresNo ratings yet
- Unipolar Late-Onset Depression: A ComprehensiveDocument18 pagesUnipolar Late-Onset Depression: A ComprehensiveargatuNo ratings yet
- STEPPS Preliminary Report 2002Document11 pagesSTEPPS Preliminary Report 2002MARGARITA ALONSO ESCAMILLANo ratings yet
- MODULE 3-Neurotic DisordersDocument4 pagesMODULE 3-Neurotic Disordersmiit yadavNo ratings yet
- Psy Class ProjectDocument6 pagesPsy Class Projecttatar.antonio.adrianNo ratings yet
- Depression Research Paper PDFDocument8 pagesDepression Research Paper PDFgz9g97ha100% (1)
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptSnehaNo ratings yet
- Bordeline Personality DisorderDocument6 pagesBordeline Personality DisorderWilliam Donato Rodriguez PacahualaNo ratings yet
- GAD General Anxiety DisorderDocument9 pagesGAD General Anxiety Disorderselina shakyaNo ratings yet
- Major Depressive Disorder in Children and Adolescents: Sandra Mullen, Pharmd, BCPPDocument9 pagesMajor Depressive Disorder in Children and Adolescents: Sandra Mullen, Pharmd, BCPPbogdancoticaNo ratings yet
- 10.1038@s41380 019 0634 7Document16 pages10.1038@s41380 019 0634 7Steven MenaNo ratings yet
- Borderline Personality DisorderDocument6 pagesBorderline Personality DisorderPetrovecNo ratings yet
- C5 Anxiety Disorders and General Medical ConditionsDocument9 pagesC5 Anxiety Disorders and General Medical ConditionsMilagros Saavedra RecharteNo ratings yet
- Terapia Cognitivo Conductual para Trastorno de Ansiedad GeneralizadaDocument13 pagesTerapia Cognitivo Conductual para Trastorno de Ansiedad GeneralizadaDavid Andrés BravoNo ratings yet
- Dysthymia: More Than Minor DepressionDocument6 pagesDysthymia: More Than Minor DepressionMasithaNo ratings yet
- Major Depressive Disorder: Continuing Education ActivityDocument9 pagesMajor Depressive Disorder: Continuing Education Activityaluri venkatarajaNo ratings yet
- 2020 Nemeroff - DeP ReviewDocument15 pages2020 Nemeroff - DeP Reviewnermal93No ratings yet
- Neurocognition in Individuals at High Familial Risk of Mood Disorders With or Without Subsequent Onset of DepressionDocument11 pagesNeurocognition in Individuals at High Familial Risk of Mood Disorders With or Without Subsequent Onset of DepressionNerea Montero GarcíaNo ratings yet
- Pages From Pages From JurnlDocument10 pagesPages From Pages From Jurnlofficial.takoheroNo ratings yet
- MHP 3Document6 pagesMHP 3Asna anwerNo ratings yet
- Guia Depresion N&ADocument24 pagesGuia Depresion N&APedro Y. LuyoNo ratings yet
- Tebbenkamp DepressionDocument8 pagesTebbenkamp Depressionapi-523012644No ratings yet
- Depression and Anxiety in Multisomatoform DisorderDocument4 pagesDepression and Anxiety in Multisomatoform DisorderAdeyemi OlusolaNo ratings yet
- Dic 8 212573 PDFDocument13 pagesDic 8 212573 PDFDona Parenta NantaliaNo ratings yet
- Trastorno Depresivo en Edades TempranasDocument15 pagesTrastorno Depresivo en Edades TempranasManuel Dacio Castañeda CabelloNo ratings yet
- Mental Health Literacy and Anxiety Disorder PDFDocument11 pagesMental Health Literacy and Anxiety Disorder PDFShabrina Patriavy BennaradictaNo ratings yet
- Overview of Major Depressive DisorderDocument11 pagesOverview of Major Depressive DisorderCharpapathNo ratings yet
- v15n3 Original Article 4Document8 pagesv15n3 Original Article 4Shazwani KKTSNo ratings yet
- Estudo. Espectro BipolarDocument9 pagesEstudo. Espectro BipolarGabriel LemosNo ratings yet
- Depression: Lezan Marewan MhammadDocument8 pagesDepression: Lezan Marewan MhammadDlzar AbubakrNo ratings yet
- Seminar: Epidemiology, Comorbidity, and DiagnosisDocument11 pagesSeminar: Epidemiology, Comorbidity, and DiagnosisMartin GiraudoNo ratings yet
- Major Depressive Disorder: Hypothesis, Mechanism, Prevention and TreatmentDocument32 pagesMajor Depressive Disorder: Hypothesis, Mechanism, Prevention and Treatmentracm89No ratings yet
- Risk Factors Associated With Relapse in Major Depressive Disorder in Primary Care Patients: A Systematic ReviewDocument9 pagesRisk Factors Associated With Relapse in Major Depressive Disorder in Primary Care Patients: A Systematic Reviewngurah jiyestaNo ratings yet
- Nejmp 1311047Document3 pagesNejmp 1311047Sebastian Andres Salazar VidalNo ratings yet
- Ketamine For Rapid Reduction of Suicidal Ideation: A Randomized Controlled TrialDocument10 pagesKetamine For Rapid Reduction of Suicidal Ideation: A Randomized Controlled TrialDeepaNo ratings yet
- Generalized Anxiety Disorder in Adults - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDateDocument17 pagesGeneralized Anxiety Disorder in Adults - Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and Diagnosis - UpToDateThaiane BarcelosNo ratings yet
- Professional Practice PaperDocument11 pagesProfessional Practice PaperronarudoNo ratings yet
- Generalized Anxiety DisorderDocument16 pagesGeneralized Anxiety Disordernns5rrg2rdNo ratings yet
- Goldberg Depression Test ScoresDocument3 pagesGoldberg Depression Test ScoresBrittanyNo ratings yet
- Repensando Depresion Con Los RcDOCS 2023Document16 pagesRepensando Depresion Con Los RcDOCS 2023Psiquiatria Clinica ProyectarteNo ratings yet
- Depression in The Elderly: Clinical PracticeDocument9 pagesDepression in The Elderly: Clinical PracticejpenasotoNo ratings yet
- Gangguan CemasssDocument6 pagesGangguan CemasssbNo ratings yet
- Geriatric Depression: The Use of Antidepressants in The ElderlyDocument7 pagesGeriatric Depression: The Use of Antidepressants in The ElderlyBilly D. Justia WahidNo ratings yet
- International Clinical Fellowship Programme Brochure - September - 2023Document29 pagesInternational Clinical Fellowship Programme Brochure - September - 2023Anam QadeerNo ratings yet
- NON Communicable DiseasesDocument45 pagesNON Communicable DiseaseshemihemaNo ratings yet
- LOPERAMIDEDocument3 pagesLOPERAMIDEfaye kimNo ratings yet
- Tiklos (Also Called "Pintakasi") Is The Waray Equivalent To The "Bayanihan". Groups ofDocument2 pagesTiklos (Also Called "Pintakasi") Is The Waray Equivalent To The "Bayanihan". Groups ofJanine Ginog FerrerNo ratings yet
- Assessment of Hand Hygiene of Nursing and Medical Students: Rev Rene April 2017Document12 pagesAssessment of Hand Hygiene of Nursing and Medical Students: Rev Rene April 2017Durga Shankar DhakarNo ratings yet
- A Healthy Diet Is Essential For Good Health and NutritionDocument2 pagesA Healthy Diet Is Essential For Good Health and NutritionthenameisvijayNo ratings yet
- Microsoft Word - DS03 - Paper - 1.1Document8 pagesMicrosoft Word - DS03 - Paper - 1.1kuridisanjeevNo ratings yet
- We Are Stew: Drugs Effects On Our BodiesDocument12 pagesWe Are Stew: Drugs Effects On Our BodiesUy HenryNo ratings yet
- Merck CaseDocument8 pagesMerck Casemariebelle moussaNo ratings yet
- Chapter One: Introduction To Psychotherapy and Counseling Theory and TechniqueDocument19 pagesChapter One: Introduction To Psychotherapy and Counseling Theory and TechniquechetankumarbhumireddyNo ratings yet
- NSO7Document3 pagesNSO7Edmund RufinoNo ratings yet
- Sdgs Vaibhav Bisaria VIII-B (Roll No.28)Document11 pagesSdgs Vaibhav Bisaria VIII-B (Roll No.28)Rishi BisariaNo ratings yet
- Reading Practice 2Document2 pagesReading Practice 2Marta Gil RodríguezNo ratings yet
- ScriptDocument27 pagesScriptIqrarNo ratings yet
- Uterovesical FistulaDocument42 pagesUterovesical Fistulakhadzx100% (2)
- 0 BOSH FrameworkDocument18 pages0 BOSH Frameworkharold fontiveros100% (1)
- Healthy Aging-A Better Way of Life After 50s: Bone Health and Immune Function)Document2 pagesHealthy Aging-A Better Way of Life After 50s: Bone Health and Immune Function)Kamakshi KhannaNo ratings yet
- Screening For Psychological Burden of Vitiligo Using Vitiligo Impact ScaleDocument6 pagesScreening For Psychological Burden of Vitiligo Using Vitiligo Impact ScaleNadaaFahmiShofiNo ratings yet
- Hand HygieneDocument35 pagesHand HygieneNur IkhsanNo ratings yet
- MS Rle Go, So, Dpa, Assessment (07-29-21)Document8 pagesMS Rle Go, So, Dpa, Assessment (07-29-21)Rhea Mala-Ay TorregosaNo ratings yet
- USP General Chapter : Pharmaceutical Compounding - Sterile PreparationsDocument37 pagesUSP General Chapter : Pharmaceutical Compounding - Sterile PreparationsRRR1No ratings yet
- Information of Noise PollutionDocument6 pagesInformation of Noise PollutionJasvinder SinghNo ratings yet
- Oxcarbazepine For Preventing Seizures 1Document2 pagesOxcarbazepine For Preventing Seizures 1William ImpNo ratings yet
- GTPS20 Stage 8Document36 pagesGTPS20 Stage 8Robert DansoNo ratings yet
- Analysis of The National Commission For Allied and Healthcare Professions Act 2021.Document11 pagesAnalysis of The National Commission For Allied and Healthcare Professions Act 2021.Tanvi ManjrekarNo ratings yet
- Nursing Facilities Clinical Audits: 28-Point Infection Control ChecklistDocument10 pagesNursing Facilities Clinical Audits: 28-Point Infection Control ChecklistRobert FucciNo ratings yet
- NCP Allergic Reaction To FoodDocument3 pagesNCP Allergic Reaction To FoodCassie ValderramaNo ratings yet
- Walk-In-Interview in CRPFDocument4 pagesWalk-In-Interview in CRPFDebashis MahantaNo ratings yet