Professional Documents
Culture Documents
Relapsed Acute Myeloid Leukemia in Children and Adolescents: Current Treatment Options and Future Strategies
Relapsed Acute Myeloid Leukemia in Children and Adolescents: Current Treatment Options and Future Strategies
Uploaded by
Yo MeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Relapsed Acute Myeloid Leukemia in Children and Adolescents: Current Treatment Options and Future Strategies
Relapsed Acute Myeloid Leukemia in Children and Adolescents: Current Treatment Options and Future Strategies
Uploaded by
Yo MeCopyright:
Available Formats
Leukemia www.nature.
com/leu
REVIEW ARTICLE
ACUTE MYELOID LEUKEMIA
Relapsed acute myeloid leukemia in children and adolescents:
current treatment options and future strategies
1 3✉
Sara Zarnegar-Lumley , Kenneth J. Caldwell2 and Jeffrey E. Rubnitz
© The Author(s), under exclusive licence to Springer Nature Limited 2022
Pediatric acute myeloid leukemia (AML) develops from clonal expansion of hematopoietic precursor cells and is characterized by
morphologic and cytomolecular heterogeneity. Although the past 40 years have seen significant improvements in overall survival,
the prevailing treatment challenges in pediatric AML are the prevention of relapse and the management of relapsed disease.
Approximately 25% of children and adolescents with AML suffer disease relapse and face a poor prognosis. Our greater
understanding of the genomic, epigenomic, metabolomic, and immunologic pathophysiology of relapsed AML allows for better
therapeutic strategies that are being developed for pediatric clinical trials. The development of biologically rational agents is critical
1234567890();,:
as conventional chemotherapeutic salvage regimens are not effective for all patients and pose risk of organ toxicity in heavily
pretreated patients. Another major barrier to improvement in outcomes for relapsed pediatric AML is the historic lack of availability
and participation in clinical trials. There are ongoing efforts to launch multinational clinical trials of emerging therapies. The purpose
of this review is to summarize currently available and newly developed therapies for relapsed pediatric AML.
Leukemia (2022) 36:1951–1960; https://doi.org/10.1038/s41375-022-01619-9
INTRODUCTION evolution occurred in about 30% of AML patients who relapsed
Approximately 25% of children with acute myeloid leukemia [5]. Approximately 30 years later, whole-genome sequencing of
(AML) suffer relapse of their disease, and despite aggressive eight adult AML patients at diagnosis and at relapse demonstrated
chemotherapy and hematopoietic cell transplantation (HCT), only clonal evolution in all cases [6]. In three cases, the founding
about 40% of these patients become long-term survivors. The (dominant) clone at diagnosis gained mutations and evolved into
outcome of children with relapsed AML has only slightly improved the relapse clone. In the other five cases, a subclone of the
over the past 20 years, likely related to improvements in dominant clone gained mutations and expanded to become the
supportive care and better outcomes after HCT [1]. This slow relapse clone. In both scenarios, it is likely that at least a subset of
progress is partly related to the lack of enrollment of such patients the mutations acquired at relapse contributed to chemotherapy
on clinical trials. We previously estimated that from 2006 to 2016, resistance. Another mechanism by which clonal evolution
less than 25% of children with relapsed AML in the US and Canada contributes to relapse is human leukocyte antigen (HLA)
were treated on clinical trials [2], and a literature review identified haplotype loss after HCT [7, 8]. In the first report of this
only a single report of a randomized trial for children with phenomenon of immune escape, the leukemic blasts of five
relapsed AML [3, 4]. In addition, the lack of improvement can be patients who relapsed after haploidentical HCT had lost the HLA
attributed to a shortage of new agents, a paucity of targeted haplotype that differed from the donor haplotype though
therapies, and the slow development of immunotherapy. We uniparental disomy of chromosome 6p, including the HLA region
predict, however, that recent advances in our understanding of [7]. A similar mechanism of immune escape has been reported
the biology and genomics of relapsed AML, the expansion of after matched unrelated HCT [9].
therapies directed at leukemia-selective abnormalities, and the Among children with relapsed AML, karyotypic evolution is
organization of international collaborative clinical trials will soon observed in ~50% of cases, similar to the findings that have been
lead to novel therapies and improved outcomes. reported in adults [10]. Until recently, however, little was known
about the genomics of relapsed childhood AML. As part of the
Therapeutically Applicable Research to Generate Effective Treat-
BIOLOGY AT RELAPSE ment AML initiative of the National Cancer Institute (NCI) and the
In the 1970s, conventional banding techniques on paired samples Children’s Oncology Group (COG), whole-exome sequencing was
from diagnosis and relapse demonstrated that karyotypic performed from diagnostic, remission, and relapse samples for 20
1
Division of Pediatric Hematology and Oncology, Vanderbilt University Medical Center, Nashville, TN, USA. 2Cancer and Blood Disorders Institute, Johns Hopkins All Children’s
Hospital, St. Petersburg, FL, USA. 3Department of Oncology, St. Jude Children’s Research Hospital, Memphis, TN, USA. ✉email: Jeffrey.Rubnitz@stjude.org
Received: 31 March 2022 Revised: 18 May 2022 Accepted: 26 May 2022
Published online: 6 June 2022
S. Zarnegar-Lumley et al.
1952
pediatric patients, excluding those with high-risk cytogenetics attainment of remission, was associated with better outcome [27].
[11]. This group identified significant clonal heterogeneity An analysis of 379 children with AML who relapsed after treatment
between diagnostic and relapse specimens with resolution of on the AML-Berlin/Frankfurt/Muenster (BFM) 87, 93, and 98
diagnostic somatic mutations and emergence of new mutations at protocols from 1987–2003 revealed a 5-year survival rate of 23%
relapse. They also noted change in the variant allele frequency overall and 31% for patients treated on the most recent protocol
(VAF) at the two time points; a somatic mutation with a higher VAF (AML-BFM 98). Late relapse, no HCT in first remission, and the
at diagnosis was more likely to persist at relapse. Similar to the presence of core-binding-factor (CBF) leukemia were all associated
clonal evolution of somatic mutations, divergence was observed with better survival [28]. Similarly, a retrospective study of 99
for copy number alterations. Overall, this work highlights the children with relapsed AML treated at Therapeutic Advances in
heterogeneity and evolving genomic profile of pediatric AML at Childhood Leukemia & Lymphoma (TACL) institutions between
relapse. It should be noted, however, that the simple presence of a 1995–2004 revealed a 5-year survival rate of 29% [29]. A slightly
new mutation at the time of relapse does not necessary imply that higher survival rate of 37% was reported for the 71 patients who
the mutation confers drug resistance or is a therapeutic target. In relapsed after treatment on the Japanese AML99 trial (2000–2002).
addition, some mutations may be subclonal, in which case In multivariate analysis, early relapse and the presence of FLT3-ITD
targeting those mutations may not be effective. were significantly associated with worse outcome [30]. A nearly
Researchers at St. Jude Children’s Research Hospital (St. Jude) identical survival rate of 36% was reported in an analysis of 111
recently performed RNA sequencing, whole-genome sequencing, patients who relapsed after treatment on the subsequent Japanese
and target-capture sequencing on 136 relapsed cases [12]. This Pediatric Leukemia-Lymphoma Study Group AML-05 trial
relapse cohort was characterized by fusions that are known to be (2006–2010). Again, multivariate analysis identified early relapse
associated with a high risk of relapse, including KMT2A fusions and the presence of FLT3-ITD as negative prognostic factors [31].
(n = 36) [13], NUP98 fusions (n = 18) [14], GLIS fusions (n = 3) [15], Likewise, the 5-year survival rate among 208 children who relapsed
PICALM-MLLT10 (n = 5) [16], FUS-ERG (n = 4) [17], and DEK-NUP214 after treatment on the Nordic Society for Paediatric Haematology
(n = 4) [18]. In addition, in-frame exon 13 tandem duplications and Oncology (NOPHO)-AML93 or NOPHO-AML 2004 (1993–2012)
(TD) in upstream binding transcription factor (UBTF) were trials was 39%. As in all forementioned studies, the strongest
identified in 12 (8.8%) cases. Because UBTF-TDs have rarely been predictor of survival after relapse was time to relapse. Late relapse,
reported in pediatric AML, 417 pediatric AML cases from previous no HCT in first remission, and the presence of CBF leukemia were
studies were re-analyzed and 15 additional cases with UBTF-TDs all associated with better survival [32]. In a retrospective analysis of
were detected. In multivariable analysis, UBTF-TD was associated patients in the most recent treatment era, investigators from the
with a poor outcome, even in patients with FLT3-ITD, suggesting BFM and COG reported survival rates of 42% and 35% respectively,
that UBTF-TD is the driver mutation in patients whose blasts with high-risk cytomolecular features, poor initial induction
harbor FLT3-ITD without known driver mutations. Importantly, response, and early relapse predictive of worse outcome [1]. In
although first characterized in a relapsed cohort, this study this analysis, there was a trend toward improved survival rates in
indicates that UBTF-TD is more prevalent at diagnosis than recent years, possibly related to a greater number of such patients
previously recognized and identifies a novel subtype of childhood undergoing HCT from alternative donor sources or proceeding to
AML that is associated with a high risk of relapse. HCT prior to count recovery. In fact, this report demonstrated that
Leukemia stem cells (LSCs) are a key contributor to the biology full hematopoietic recovery after salvage therapy was not
of AML relapse and the focus of enhanced risk stratification and predictive of survival [1]. In addition, improvements in supportive
new therapies. First identified as rare subpopulations responsible care, including the availability of more potent antifungal agents,
for engraftment in xenotransplantation assays [19, 20], LSCs likely contributed to the improvement in outcome.
maintain the properties of self-renewal and cell cycle quiescence Although the outcome after second relapse is poor, a subset of
and can evade standard chemotherapeutic agents, thus allowing these patients can be cured even without novel interventions. For
for disease persistence and relapse [21]. Stemness in AML has example, in an analysis of 73 patients who suffered second
been characterized by unique immunophenotypic signatures, relapses after treatment on AML-BFM trials from 2004–2017, the
designated LSC17 and pLSC6, that have been proposed as 5-year survival was 15%. Whereas patients with early second
surrogate biomarkers for adverse prognosis [22–24]. Other relapses and those who failed to achieve a third remission had
biomarkers of stemness have emerged as potential predictors of dismal outcomes, 31% of those who underwent subsequent HCT
relapse and targets for therapy including calcitonin receptor-like survived [33]. A recent review of 157 patients on NOPHO-DB SHIP
(CALCRL) [25]. More recently, better understanding of LSC consortium trials who experienced a first relapse that was
machinery has allowed for investigation into metabolic and refractory (n = 98) or a second relapse (n = 59) indicated similar
epigenetic differences between LSCs and normal hematopoietic outcomes, with 1-year and 5-year survival rates of 22% and 14%,
stem cells (HSCs) allowing for exploitation of differences in respectively [34]. At St. Jude, outcomes among AML patients who
emerging therapeutics [21]. relapsed after undergoing HCT have increased over time, with a
Epigenetic dysregulation has been implicated in the pathophy- second HCT being the only curative modality [35]. Thus, patients
siology of pediatric AML [26]. Pathologic modification of DNA, who suffer second relapses may be candidates for intensive
histones, and chromatin promote aberrant cell proliferation, self- chemotherapy or second transplants, options that may hamper
renewal, and differentiation block. These mechanisms are the enrollment of such patients on phase 1 trials.
essential for chemotherapy resistance and may underlie AML
relapse. Therapeutic epigenetic reprogramming has the potential Completed trials
to restore gene expression of silenced tumor suppressor genes New combinations of cytotoxic chemotherapy. Until recently, the
and enhance chemo-sensitivity of AML blasts. mainstay of relapse treatment had been reinduction therapy with
new combinations of conventional cytotoxic chemotherapy with a
Retrospective studies goal of achieving remission prior to HCT. Many combinations have
Reports published over the past 20 years indicate that the shown activity, but few have led to significantly better outcomes.
prognosis of children with relapsed AML has remained unaccep- A Children’s Cancer Group study that enrolled children with
tably low. Among 106 children with AML who relapsed after relapsed or refractory (R/R) AML showed that reinduction with
treatment on the Leucemie Aique Myeloide Enfant 89/91 protocol mitoxantrone and cytarabine was effective with reasonable
from 1988–1998, the 5-year overall survival rate was 33%. In this toxicity [36]. Clofarabine, a nucleoside analog that induced a
study, late relapse, defined as relapse greater than 1 year from the response rate of 30% as single agent [37], has been studied in a
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1953
variety of combinations. Among 49 children with R/R AML who demonstrated increases in acetylation. In addition, this regimen
received clofarabine and cytarabine on the COG study AAML0523, was safe and 8 patients achieved CR, of whom 6 had negative
the overall response rate was 48% [38]. Similar response rates MRD, suggesting that priming with HDAC inhibitors should be
were reported after treatment with the combinations of clofar- further studied in patients with AML [50]. Using a similar design,
abine, high-dose cytarabine and liposomal daunorubicin [39], the TACL consortium conducted a phase 1 study in which the
clofarabine, cyclophosphamide and etoposide [40], and clofar- DNMT inhibitor azacitidine was given prior to fludarabine and
abine, topotecan, vinorelbine, and thiotepa [41]. Other combina- cytarabine in children with R/R leukemia [51]. This regimen was
tions of conventional therapy that have been studied include well-tolerated and 7 of 12 patients achieved CR, suggesting that it,
cladribine and topotecan [42] and topotecan, vinorelbine, too, be studied further. The TACL consortium recently completed a
thiotepa, dexamethasone, and gemcitabine [43]. trial that combined these two strategies of epigenetic reprogram-
ming in which pediatric patients with R/R AML received decitabine
New formulations of cytotoxic chemotherapy. Several clinical trials and vorinostat prior to conventional therapy. In this study, 19 of 35
have focused on new formulations of cytotoxic chemotherapy of patients achieved CR or CR with incomplete count recovery
rather than on novel agents. In the only published randomized (CRi) and 17 achieved MRD negativity [53]. Based on the
clinical trial for relapsed pediatric AML, 394 patients were randomly encouraging results of the aforementioned studies, epigenetic
assigned to receive fludarabine, cytarabine, and GCSF (FLAG) or priming is now being tested in a phase 2 trial in children with
FLAG plus liposomal daunorubicin [4]. The complete remission (CR) newly diagnosed AML at St. Jude (NCT03164057).
rates were 69 and 59% for patients who were treated with FLAG Overexpression of the antiapoptotic proteins BCL2, BCL-XL, and
plus liposomal daunorubicin vs. FLAG alone, but survival rates were MCL1, which sequester pro-apoptotic BH3-only proteins and
similar across treatment groups. However, treatment with liposo- prevent activation of the death effector proteins BAX and BAK,
mal daunorubicin was associated with improved survival among is associated with resistance to chemotherapy and represent
patients with CBF leukemia [4]. More recently, investigators from another therapeutic target to which potent inhibitors have been
the COG reported that Vyxeos (formerly CPX-351), a liposomal developed [54, 55]. Venetoclax, a selective inhibitor of BCL2,
formulation of daunorubicin and cytarabine, was safe and active in induces apoptosis in AML cell lines, primary samples, and mouse
children with relapsed AML, with a CR rate of 54% and an minimal xenograft models [56]. Clinical trials demonstrated the safety and
residual disease (MRD) negative rate of 84% among patients who activity of venetoclax in combination with hypomethylating
achieved CR or CR with incomplete platelet recovery (CRp) [44]. It agents or low-dose cytarabine in elderly patients with AML,
should be noted, however, that the results of aforementioned trials leading to FDA approval of these combinations [57–59]. A pilot
should not be directly compared, as the number of patients in the study (VENAML) demonstrated that venetoclax could be safely
latter trial was quite small (n = 38) and the confidence intervals combined with intensive chemotherapy in children with R/R AML
large (e.g., CR + CRp rate = 68.3%, CI, 52.9–78.0%). Nevertheless, [52]. Overall responses were observed in 24 (69%) of 35 evaluable
these encouraging results have led to a randomized trial patients, including 16 CR (11 MRD negative), 4 CRi (2 MRD
(AAML1831, NCT: 04293562) of Vyxeos and gemtuzumab ozoga- negative), and 4 partial response (PR). Among the 20 patients
micin (GO) vs. conventional daunorubicin, cytarabine, and GO in treated at the recommended phase 2 dose 14 (70%) achieved CR
children with newly diagnosed AML. or CRi and 16 (80%) CR/CRi/PR. This trial has been amended to
include the combination of azacitidine, venetoclax, and high-dose
Novel and targeted agents. The results of phase 1 or 2 studies of a cytarabine and remains open to accrual (NCT03194932).
variety of agents, including valspodar [45], lenalidomide [46], Exportin 1 (XPO1) is a nuclear exporter of tumor suppressor and
bortezomib [47], plerixafor [48], selinexor [49], panobinostat [50], growth regulatory proteins that AML cells can co-opt to proliferate
azacitidine [51], and venetoclax [52] have been reported. and evade apoptosis. Selective inhibitors of nuclear export, such
Valspodar, an inhibitor of potent P-glycoprotein, was tested in as selinexor, bind XPO1, prevent nuclear export of cargo proteins,
combination with mitoxantrone and etoposide in pediatric and restore tumor suppressor function in AML. A phase I pediatric
patients with R/R leukemia. The regimen was safe, but blasts study from St. Jude characterized the toxicity, pharmacokinetics,
from only one patient demonstrated inhibition of P-glycoprotein and pharmacodynamics of selinexor combined with fludarabine
and no patients with AML responded [45]. Similarly, in a phase and cytarabine in children with R/R leukemia [49]. The results of
2 study of lenalidomide in 17 pediatric patients with R/R AML, only this trial demonstrated that selinexor was tolerable at doses up to
1 patient responded [46]. Notably, the responding patient had a 55 mg/m2 given twice weekly and that all patients who received
complex karyotype that included del(5q), consistent with reports selinexor at ≥40 mg/m2 demonstrated XPO1 target inhibition. In
that lenalidomide is active in this genetic subtype of AML in this group of heavily pretreated patients, 7 of 15 evaluable
adults. A phase 2 study of bortezomib combined with either patients achieved CR or CRi, including two patients who became
idarubicin and cytarabine or cytarabine and etoposide in patients MRD negative after receiving only four doses of selinexor without
with R/R AML demonstrated that both regimens were tolerable. chemotherapy [49]. The striking single-agent activity of selinexor
However, low CR rates led to closure of both study arms during in these patients indicates that there is a subgroup of patients
the first stage of the two-stage design [47]. In a phase 1 trial of the who may benefit from this agent, even in the absence of cytotoxic
CXCR4 antagonist plerixafor in combination with cytarabine and chemotherapy. However, the lack of biomarkers to identify which
etoposide, treatment with plerixafor resulted in mobilization of patients will respond to selinexor has slowed the further
leukemia blasts into the blood in 14 of 16 patients. However, development of this agent in pediatric AML.
among the 13 patients with relapsed AML, only 2 achieved CR
[48]. The disappointing response rates observed in these studies Current and future targets and trials
of valspodar, lenalidomide, bortezomib, and plerixafor suggest The development of new agents for pediatric AML has been slow,
that they should not be studied further, except in specific in part because of the low incidence of the disease and the
subgroups of patients who are likely to benefit. different spectrum of mutations in childhood AML compared to
Epigenetic priming with histone deacetylase (HDAC) inhibitors AML in older adults. Prioritizing agents for clinical trials and
or DNA methyltransferase (DNMT) inhibitors has been used in efficiently conducting such trials will require international
attempts to sensitize leukemic blasts to standard chemotherapy. A collaboration. The Leukemia and Lymphoma Society Pediatric
phase 1 study in which 17 children with R/R AML received the Acute Leukemia initiative is currently working with the European
HDAC inhibitor panobinostat before, and in combination with, Pediatric Acute Myeloid Leukemia consortium to coordinate
fludarabine and cytarabine showed that blasts from 7 of 9 patients preclinical testing, prioritize targets, screen patients, and develop
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1954
Table 1. Current and future studies.
Target Regimen ClinicalTrials.gov ID Study group Status
BCL2 Venetoclax + azacitidine + cytarabine NCT03194932 St. Jude Recruiting
BCL2 and CD33 Fludarabine/cytarabine/gemtuzumab with or NCT05183035 LLS PedAL Initiative, LLC Planned
without venetoclax
BCL2 and XPO1 Venetoclax + selinexor + fludarabine/cytarabine NCT04898894 St. Jude Recruiting
PD-1 Nivolumab + azacitidine NCT03825367 TACL Recruiting
IDH2 Enasidenib NCT04203316 COG Recruiting
MDM2 Idasanutlin + chemotherapy or venetoclax NCT04029688 Hoffmann-La Roche Recruiting
Menin SNDX-5613 + fludarabine/cytarabine NCT04065399 Syndax Pharmaceuticals Recruiting
Menin KO-539 + fludarabine/cytarabine Pending Kura Oncology Planned
E-selectin Uproleselan + fludarabine/cytarabine Pending LLS PedAL Initiative, LLC Planned
CD123 CD123 CAR T cells NCT04318678 St. Jude Recruiting
CD123 CD123 CAR T cells NCT04678336 University of Pennsylvania Recruiting
CD123 Flotetuzumab NCT04158739 COG/PEP-CTN Closed
CD123 IMGN632 Pending LLS PedAL Initiative, LLC Planned
CD123 Tagraxofusp IL3 Pending TACL Planned
CD33 CD33 CAR T cells NCT03971799 CIBMTR Recruiting
CD33 CD33 x CD3 bispecific T-cell-engager NCT05077423 COG/PEP-CTN Planned
Non-specific NK cells + DLI NCT03068819 Washington University Recruiting
CD38 Isatuximab + chemotherapy NCT03860844 Sanofi Recruiting
CD33 Vyxeos + gemtuzumab NCT04915612 M.D. Anderson Cancer Center Recruiting
XPO1 exportin 1, PD-1 programmed death-1, IDH2 isocitrate dehydrogenase 2, MDM2 mouse double minute 2, CAR chimeric antigen receptor, NK natural killer,
DLI donor lymphocyte infusion, LLS Leukemia & Lymphoma Society, PedAL pediatric acute leukemia, TACL Therapeutic Advances in Childhood Leukemia &
Lymphoma, COG Children’s Oncology Group, CIBMTR Center for International Blood and Marrow Transplant Research, PEP-CTN The Pediatric Early Phase Clinical
Trials Network.
Bispecific antibodies:
• CD3xCD123
Epigenetic priming • CD3xCD33
i ng Im
Menin inhibitors mm mu
ro g ra no
-th
CD123 CART
LSD1 inhibitors r ep era PD-1 (Nivolumab) + azacitidine
n etic p eu
ige ti cs
Ep
Antibody-drug conjugate
Monoclonal antibody
Cell cycle & signaling
IMGN632
SYK inhibitors
Tagraxofsup
CDK4/6 inhibitors
Magrolimab
MEK inhibitors
Isatuximab
FLT3 inhibitors
Venteoclax + Azacitidine + HiDAC
al
M
viv
et FLA + GO ± Venetoclax
ur
ab
ls
ol Selinexor + Venetoclax
ism
l
Ce
Idasanutlin + Venetoclax
IDH inhibitors
Microenvironment ALRN-6924
Talazoparib
Pevonedistat
Uproselan
SYK: spleen tyrosine kinase, CDK: cyclin dependent kinase, MEK: mitogen-activated protein kinase kinase, FLT3: fms-like tyrosine kinase 3, HiDAC: high dose cytarabine, FLA: fludarabine + cytarabine, GO: gemtuzumab ozogamicin, CART: chimeric antigen receptor, PD-1: programmed death-1, LSD1: lysine-specific demethylase 1
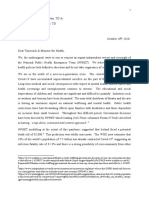
Fig. 1 Current and future targets by therapeutic subclass. Therapeutic targets are indicated in the circle and potential therapies are listed in
the boxes. Abbreviations: SYK, spleen tyrosine kinase; CDK, cyclin dependent kinase; MEK, mitogen-activated protein kinase; FLT3, fms-like
tyrosine kinase 3; HiDAC, high-dose cytarabine; FLA, fludarabine + cytarabine; GO, gemtuzumab ozogamicin; CART, chimeric antigen receptor;
PD-1, programmed death-1; LSD1, lysine-specific demethylase 1.
clinical trials that will be conducted in North America, Europe, BCL2/BCL-XL/MCL1 inhibitors
Australia, and New Zealand [60]. A partial list of trials that are This excellent response rate observed in the VENAML trial
currently recruiting or planned is shown in Table 1. Current and described above has led to the development of an international
future targets are represented schematically by therapeutic randomized trial (NCT05183035) that will compare the outcome of
subclass in Fig. 1 and discussed below. patients with relapsed AML treated with fludarabine, cytarabine,
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1955
and GO to that of patients treated with the same agents plus stratification of KMT2A fusions by translocation partner in upfront
venetoclax. Although venetoclax is active in a variety of AML pediatric AML trials. The KMT2A oncoprotein binds to DNA in a
subtypes, resistance can develop through changes in mitochon- chromatin-associated protein complexes which is required for
drial metabolism and structure, as well as through overexpression maintenance of the gene expression program required for
and increased dependence on the antiapoptotic proteins BCL-XL leukemic transformation. Proteins of therapeutic interest in these
or MCL1 [61–64]. In patients with acute lymphoblastic leukemia complexes have included the histone methyltransferase, disruptor
(ALL), dependence on BCL-XL or both BCL-XL and BCL2 suggests of telomeric silencing 1 like (DOT1L), and more recently menin.
that targeting both proteins may be an effective strategy [65]. Whereas DOT1L enzymatic inhibition was promising in preclinical
Indeed, a recent study of navitoclax, a BCL-XL/BCL2 inhibitor, experiments [80], translation to a clinical trial was not successful
combined with venetoclax, in children and adults with ALL due to only modest response [81]. Subsequent preclinical
demonstrated that this combination is safe and active [65]. In investigation of the KMT2A-menin complex has led to intense
AML, overexpression of MCL1, rather than BCL-XL, is a more interest in therapeutic targeting of this interaction. Several
common mechanism of venetoclax resistance [66]. Selective preclinical studies demonstrated that small-molecule inhibition
inhibitors of MCL1 alone and in combination with venetoclax of KMT2A-menin induced remission and, in some cases, eradi-
are highly active in preclinical AML models [66–68]. However, the cated disease, in KMT2A-rearranged and NPM1-mutated leukemia
role of MCL1 in cardiac, neuronal, hepatic, and intestinal cell [82–85]. Similarities in gene expression patterns, particularly
development and survival may limit the use of MCL1 inhibitors, overexpression of HOXA9 and MEIS1, in other leukemia subtypes
especially in pediatric patients [64]. suggests that additional subtypes may be amenable to menin
Although selective MCL1 inhibitors are currently undergoing inhibition. Notably, a recent study indicated that NUP98-rear-
safety testing in adults and are not yet ready to be studied in ranged AML, which is characterized by high expression of HOXA9
children, MCL1 can potentially be targeted indirectly. In one study, and MEIS1, is dependent on the KMT2A-menin interaction and is
the combination of selinexor and venetoclax synergistically sensitive to menin inhibition [86]. Based on these very strong
induced apoptosis in AML samples through modulation of MCL1 preclinical data, at least five menin inhibitors are in clinical
by selinexor [69]. In this study, selinexor and venetoclax development (Syndax, NCT04065399; Kura, NCT04067336; Daiichi
reciprocally abrogated apoptosis resistance to the other agent Sankyo, NCT04752163; Janssen, NCT04811560; Biomea Fusion,
via selinexor-mediated inhibition of the binding of Bim to MCL1 NCT05153330) [87].
and venetoclax-mediated inhibition of the binding of BCL2 to Bim.
In a similar report, venetoclax plus selinexor or eltanexor induced SYK inhibitors
apoptosis and reduced tumor growth in AML xenografts, effects Integrated proteomic and genetic studies designed to identify the
that were partly due to decreases in MCL1 expression [70]. In mechanism by which epidermal growth factor receptor inhibitors
addition, primary leukemia samples from venetoclax-resistant AML induce AML differentiation identified spleen tyrosine kinase (SYK)
patients responded to the combination of selinexor and veneto- as a potential therapeutic target in AML [88]. More recent studies
clax, providing further evidence that treatment with selinexor may demonstrated that expression of the homeodomain-containing
reverse venetoclax resistance. Based on these data, we recently transcription factors HOXA9 and MEIS1 is associated with SYK
opened a phase I study to assess the safety and activity of dependence [89]. Mutations in NPM1 lead to activation and high
venetoclax and selinexor in combination with chemotherapy in expression of HOXA9 and MEIS1, suggesting that targeting SYK is a
pediatric patients with R/R AML (NCT04898894). Other potential rational approach to the treatment of NPM1-mutated AML. The
approaches to MCL1 inhibition include the use of conventional results of a clinical trial of entospletinib (formerly GS-9973), a
chemotherapy [71, 72] or inhibitors of cyclin dependent kinase selective inhibitor of SYK, combined with chemotherapy demon-
(CDK)9 [73, 74]. strated higher CR rates and OS among patients with NPM1
Given the key role of TP53 in the transcriptional activation of mutations and high HOXA9 and MEIS1 expression, further
apoptosis machinery, it is not surprising that loss or inactivation of supporting the role of SYK in NPM1-mutated AML [90]. Entosple-
TP53 confers resistance to BCL2 inhibition by venetoclax [75, 76]. tinib is now being tested in a phase 3 trial in adults with newly
As predicted, clinical studies have indicated that TP53 loss is diagnosed AML and should be considered in future trials for
associated with poor response to venetoclax or the development children with relapsed NPM1-mutated AML.
of resistance [77, 78]. Elegant preclinical studies demonstrate that
simultaneous inhibition of BCL2 with venetoclax and activation of LSD1 inhibitors
TP53 with the MDM2 inhibitor idasanutlin induce synthetic Lysine-specific demethylase 1 (LSD1) is a chromatin modifier that
lethality and overcome resistance to BCL2 inhibition [76]. In is expressed in HSCs and AML blasts and plays a role in terminal
several models, activation of TP53 promoted MCL1 degradation differentiation in normal hematopoiesis [91]. Pharmacologic LSD1
and thus abrogated BCL2 resistance, while BCL2 inhibition inhibition induces monocytic differentiation of AML blasts and
overcame resistance to TP53 activation. Clinical trial substantially impairs their self-renewal capacity [92]. Iadademstat,
NCT04029688 is now evaluating the safety, pharmacokinetics, a selective inhibitor of LSD1 was shown to be safe and active in a
and activity of idasanutlin in combination with venetoclax in phase I study of adult patients with R/R AML [93].
pediatric patients with R/R leukemia or solid tumors. In addition,
ALRN-6924, a duel MDM2/MDMX inhibitor, is being studied in Proteosome inhibitors
children with relapsed cancer in an ongoing phase I trial Pevonedistat is a small-molecule inhibitor of the NEDD8-activating
(NCT03654716). enzyme. It is a proteasome inhibitor that specifically blocks
degradation of key proteins involved in cell proliferation and
Menin inhibitors survival. Preclinical studies demonstrate that pevonedistat in
KMT2A (formerly MLL) was initially cloned in 1991 as a result of cancer cell models leads to potent cell death [94]. Pevonedistat
translocations involving 11q23 in AML and ALL and was has been studied in combination with azacytidine in adult patients
subsequently found to bind menin, the product of the MEN1 with treatment-naïve AML who were unfit for standard induction
tumor suppressor gene [79]. The KMT2A oncoprotein is a chimeric chemotherapy. The combination was tolerable with 50% overall
fusion of the N-terminus of KMT2A with one of more than 80 response rate [34]. The COG has recently completed a feasibility
translocation partners, which have demonstrated variable ther- study of pevonedistat in combination with azacytidine, fludar-
apeutic response in pediatric AML, thereby leading to risk abine, and cytarabine in pediatric R/R AML (NCT03813147).
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1956
PARP inhibitors patients with FLT3 activating mutations [107]. Although there are
Poly(ADP-ribose) polymerase 1 (PARP1) is a key mediator of DNA no active trials of FLT3 inhibitors in pediatric patients with
repair, is activated in response to DNA damage, and is a potential relapsed AML in the US, quizartinib is being evaluated in children
therapeutic target in AML [95]. PARP inhibitors were first with R/R FLT3-ITD-positive AML in Europe, while gilteritinib is
developed for the treatment of BRCA-mutated tumors based on being investigated in the COG AAML1831 trial in newly diagnosed
the demonstration of synthetic lethality in preclinical models and children with this AML subtype.
several inhibitors are now FDA-approved for BRCA-mutated breast
and ovarian cancer [96, 97]. Preclinical data suggest that the Immunotherapy
effects of PARP inhibitors may be potentiated by cytotoxic The lack of known leukemia-specific antigens that are not
chemotherapy or DNMT inhibitors, even in BRCA wild-type AML expressed on normal hematopoietic precursors has hampered
models. For example, the addition of PARP inhibitors led to the development of immunotherapy for AML, which lags
increased double-strand breaks and synergistically enhanced the significantly behind immunotherapy for ALL [108]. The targets
effects of cytarabine and doxorubicin in an MLL-AF9 AML model. against which most current efforts are directed are CD33 and
However, it is not yet known if this effect is limited to specific AML CD123, both of which are expressed in ~90% of AML cases. Several
subtypes or is a general phenomenon [98]. A trial of talazoparib additional targets are the focus of preclinical and early phase trials.
plus chemotherapy for pediatric patients with R/R AML will open
in 2022. CD123
CD123 is expressed in most AML cases, as well as many cases of
E-selectin inhibitors precursor B-cell ALL, some cases of T-cell ALL, and, most
AML blasts commonly express E-selectin ligand, which enhances importantly, AML LSCs. Although CD123 is expressed on normal
adherence to the vasculature of the bone marrow niche. E-selectin- hematopoietic precursors, its lower expression on normal stem
mediated binding of leukemic blasts leads to sequestration of AML cells compared to LSCs may offer a therapeutic window. High
blasts and LSC, and ultimately to chemoresistance [99]. Uprolese- CD123 expression in pediatric AML is associated with high-risk
lan, an E-selectin antagonist, disrupts leukemic cell adhesion to the KMT2A rearrangements and FLT3-ITD mutations and is indepen-
bone marrow microenvironment. It was shown to be safe and dently prognostic of inferior outcomes [109]. CD123-directed
active when combined with chemotherapy in adults with R/R AML therapies include flotetuzumab, a CD123 x CD3 bispecific
[100]. Planning is underway for trial in pediatric relapsed AML. designed to target CD123+ blasts for recognition by CD3+
T cells [110, 111]; CD123-targeted chimeric antigen receptor (CAR)
Hedgehog pathway T-cell therapy; IMGN632, in which a humanized anti-CD123
The Hedgehog (Hh) signaling pathway plays an important role in antibody is conjugated to indolino-benzodiazepine dimers [112];
embryogenesis and stem cell maintenance and has been shown and tagraxofusp (SL-401), a CD123-directed protein consisting of
to play a role in the development and expansion of LSCs. PTCH1, human interleukin-3 fused to truncated diphtheria toxin [113].
SMO, and GLI are all components of the Hh pathway that can be Flotetuzumab has recently been investigated in pediatric patients
upregulated in patients with AML and therefore serve as potential in the PEPN1812 trial (NCT04158739), while CD123-directed CAR T
targets. Glasdegib is the first SMO inhibitor approved by the FDA therapy is being explored by the CATCHAML trial (NCT04318678)
for treatment of AML in adults unsuitable for intensive at St. Jude and with a different product at the Children’s Hospital
chemotherapy [101]. of Philadelphia (CHOP) (NCT04678336). Clinical trials of IMGN632
and tagraxofusp are expected to open in 2022.
CDK inhibitors
CDK6 and CDK4 are key regulators of the cell cycle. CDK6 is highly CD33
expressed in murine and human AML samples and loss of CDK6 CD33 is commonly expressed on pediatric AML blasts and was an
attenuated leukemogenesis in some AML, specifically NUP98 early immunotherapy target, leading to the development of
fusion driven AML [102]. Palbociclib inhibits CDK4/CDK6, was antibody drug conjugate, GO. Increased expression of CD33 is
shown in preclinical models to be active in vitro and in vivo associated with FLT3-ITD and NPM1 mutations and was associated
against NUP98-rearranged AML, and is therefore a potential with favorable response to GO [114]. The safety and activity of GO
therapy option for future studies [102]. A phase I/II study of against CD33+ AML has led to the development of CD33-directed
palbociclib and Vyxeos is ongoing in adults. CAR T-cell therapy, including a pediatric trial (NCT03971799) that
is recruiting patients at CHOP and the NCI. Bispecific T-cell
MEK inhibitors engagers that target CD33 [115] have been developed and a
Ras/MAPK pathway mutations are frequently activated in relapsed pediatric clinical trial will open to accrual this year (NCT05077423).
AML. Trametinib, a MEK1/2 inhibitor has been studied in RAS-
mutated leukemia and demonstrated ex-vivo activity in primary CD47
patient samples [103]. A phase I/II study performed in adults with Over 10 years ago, Majeti et al. identified CD47 as a key LSC
RAS-mutated AML showed that single-agent trametinib was marker that contributes to the pathogenesis of myeloid malig-
tolerated and had activity in some patients [104]. nancies by inhibiting phagocytosis through its binding to SIRP1-
alpha on macrophages [116, 117]. Their early studies demon-
Other inhibitors strated that CD47 expression was preferentially higher in AML
Mutations in isocitrate dehydrogenase (IDH) alter cellular meta- stem cells compared to normal hematopoietic precursors and
bolism by formation of a neomorphic metabolite, 2-hydroxyglu- higher levels were associated with a worse outcome. Importantly,
tarate, that alters cellular epigenetics blocks differentiation. For treatment of xenografted mice with an anti-CD47 antibody led to
patients with IDH mutations, IDH inhibitors ivosidenib (IDH1) [105] phagocytosis of patient-derived AML stem cells and clearance of
and enasidenib (IDH2) [106] have proven to be safe and active in leukemia [117]. These exciting findings led to the clinical
adults. Due to the rarity of these mutations in children with AML, development of magrolimab, the first anti-CD47 antibody to enter
safety has not yet been established. Investigators from the COG clinical trials [118]. Initial studies of magrolimab given as a single
are currently testing enasidenib in patients with R/R IDH2-mutated agent to patients with AML or MDS were disappointing, possibly
AML (NCT04203316). because optimal activity will require blocking the CD47-mediated
Many FLT3 inhibitors are commercially available and are anti-phagocytic signal with anti-CD47 antibodies and enhancing
considered standard of care for newly diagnosed and relapsed pro-phagocytic signals with other agents. Preclinical studies
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1957
demonstrating synergy between magrolimab and azacitidine or Palliative care
other chemotherapeutic agents support this hypothesis and have Finally, we should emphasize the critical importance of palliative
led to several ongoing clinical trials in adults with AML or MDS and supportive care to preserve quality of life for children and
[119, 120]. The preliminary results of a trial of azacitidine, adolescents with relapsed AML [134]. The promise of emerging
venetoclax, and magrolimab in older or unfit adults with AML or therapeutics should be balanced with the provision of symptom
in adults with R/R AML (NCT04435691) were recently reported alleviation, compassionate and truthful communication, psycho-
(Daver et al., ASH 2021). Among 16 evaluable patients with newly social support, and if necessary, end-of-life planning and hospice
diagnosed AML, 15 (94%) achieved CR/CRi, with 7 patients care. As we move forward with early and advanced phase clinical
becoming MRD negative. The CR/CRi rates were 5 of 8 among trials, integration of quality of life metrics and patient reported
venetoclax-naive relapsed/refractory patients and 3 of 13 in outcome measures can provide powerful adjunctive understand-
patients who had failed prior venetoclax-based therapy. Overall, ing of the impact of these therapies on patient quality of life [135].
the therapy was well-tolerated, with no early mortality in the Furthermore, the opportunity to expand clinical trials to multi-
cohort of newly diagnosed patients. A pediatric development plan center settings with broad geographic distribution can benefit
for magrolimab is being developed. patients by limiting travel.
WT1
Wilms Tumor 1 (WT1) is a transcription factor which had limited CONCLUSION
expression in normal tissue but is commonly overexpressed in Relapsed pediatric AML poses a significant therapeutic challenge
AML. It has not been shown to have independent prognostic with suboptimal outcomes from conventional chemotherapy
significance in pediatric AML; however, it co-occurs with other salvage regimens. Currently, many biologically rational therapeu-
high-risk mutations such as FLT3-ITD [121] and is enriched in tics are under development that leverage our enhanced under-
patients with chemo-refractory disease [122]. WT1 is an intracel- standing of the underpinnings of AML relapse. Overarching goals
lular protein making it challenging to target using traditional cell- of emerging relapse therapy include targeting of LSCs, therapeutic
surface directed antibody therapy. For this reason, therapies have reprogramming of epigenetic, metabolic, and cell survival path-
been developed that recognize portions of the intracellular ways co-opted by leukemic blasts, and selective immunother-
peptides in the context of HLA, including CAR T cells [123], apeutic targeting LSCs and AML blasts while sparing normal HSCs.
genetically modified EBV specific T cells [124], and bispecific The pace of pediatric drug development is slow compared to that
antibodies [125]. in adults and can attributed to the low absolute numbers of
pediatric patients to enroll in randomized clinical trials, safety
CLL-1 concerns in pediatric patients despite their overall better
C-type lectin-like molecule 1 (CLL-1) is expressed on LSCs and AML functional status and organ function compared to adults, and
blasts, but not on normal HSCs, making it a potential target in often the requirement to test drugs in monotherapy, which is
AML. CAR T-cell therapy targeting CLL-1 is being studied in a unattractive in relapsed AML that can rapidly outpace a
phase I/II trial, in which three of the first four patients achieved CR monotherapy approach. With increased interest and resources
[126]. being put toward international collaborative clinical trials of
biologically rational therapies, there is the promise of increased
CD70 clinical trial participation with optimism for improved outcomes.
AML blasts and LSCs express CD70, a type 2 transmembrane
protein [127]. Cusatuzumab, at CD70 monoclonal antibody, has
been tested in a phase I study and shown to be tolerated and REFERENCES
eliminate LSCs [128]. CD70-specific CAR T cells have been 1. Rasche M, Zimmermann M, Steidel E, Alonzo T, Aplenc R, Bourquin JP, et al.
developed and shown preclinically to have potent activity against Survival following relapse in children with acute myeloid leukemia: a report
AML, sparing normal hematopoiesis [129]. from AML-BFM and COG. Cancers. 2021;13:2336. https://doi.org/10.3390/
cancers13102336
Preclinical testing of several other potential targets, including
2. Alexander TB, Bhakta N, Kolb EA, Rubnitz JE. Opportunities for expanding clinical
CD7, CD13, TIM3, NKG2D, CD64, mesothelin, and GRP78, has trial enrollment for relapsed and refractory pediatric acute myeloid leukemia in
yielded promising results [130]. It is possible that targeting more the United States and Canada. Pediatr Blood Cancer. 2017;64:e26632.
than a single tumor antigen is necessary. It was observed that 3. Hoffman AE, Schoonmade LJ, Kaspers GJ. Pediatric relapsed acute myeloid
CD33/CLEC12A are highly upregulated targets on pediatric AML leukemia: a systematic review. Expert Rev Anticancer Ther. 2021;21:45–52.
and can be preferentially targeted together [131]. It was also 4. Kaspers GJ, Zimmermann M, Reinhardt D, Gibson BE, Tamminga RY, Aleinikova
noted that CD33/FLT3 are immunotargets specific to KMT2A- O, et al. Improved outcome in pediatric relapsed acute myeloid leukemia: results
mutated infant AML suggesting that combinatorial targeting may of a randomized trial on liposomal daunorubicin by the International BFM Study
be effective in this group [131]. Checkpoint inhibition is being Group. J Clin Oncol. 2013;31:599–607.
5. Testa JR, Mintz U, Rowley JD, Vardiman JW, Golomb HM. Evolution of karyotypes
trialed by the TACL Consortium in a phase I/II study of nivolumab
in acute nonlymphocytic leukemia. Cancer Res. 1979;39:3619–27.
in combination with azacytidine in childhood relapsed AML 6. Ding L, Ley TJ, Larson DE, Miller CA, Koboldt DC, Welch JS, et al. Clonal evolution
(NCT03825367). in relapsed acute myeloid leukaemia revealed by whole-genome sequencing.
HCT has long been a mainstay in treatment of relapsed AML Nature. 2012;481:506–10.
with novel donor selection and graft manipulation being a major 7. Vago L, Perna SK, Zanussi M, Mazzi B, Barlassina C, Stanghellini MT, et al. Loss of
area of research that is outside the scope of this review. Donor mismatched HLA in leukemia after stem-cell transplantation. N Engl J Med.
lymphocyte infusions have been used for relapse after HCT in an 2009;361:478–88.
effort to enhance graft-versus-leukemia effect but have limited 8. Welch JS, Ley TJ, Link DC, Miller CA, Larson DE, Koboldt DC, et al. The origin and
success and can often come with a cost of graft-versus-host evolution of mutations in acute myeloid leukemia. Cell. 2012;150:264–78.
9. Jan M, Leventhal MJ, Morgan EA, Wengrod JC, Nag A, Drinan SD, et al. Recurrent
disease (GVHD). Allogeneic NK cells have been given to children
genetic HLA loss in AML relapsed after matched unrelated allogeneic hema-
with AML safely without causing GVHD [132]. Bednarski et al. topoietic cell transplantation. Blood Adv. 2019;3:2199–204.
recently completed a phase I trial using donor derived NK cells to 10. Klein K, Beverloo HB, Zimmermann M, Raimondi SC, von Neuhoff C, de Haas V,
treat pediatric AML that relapsed after HCT. They showed that et al. Prognostic significance of chromosomal abnormalities at relapse in chil-
donor derived NK cells persisted up to 6 months and maintain dren with relapsed acute myeloid leukemia: a retrospective cohort study of the
anti-leukemia activity highlighting the potential role for adoptive Relapsed AML 2001/01 Study. Pediatr Blood Cancer. 2022:69;e29341. https://doi.
NK cell immunotherapy in treating AML [133]. org/10.1002/pbc.29341
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1958
11. Farrar JE, Schuback HL, Ries RE, Wai D, Hampton OA, Trevino LR, et al. Genomic current treatment strategies and outcome of the AML-BFM Study Group. Can-
profiling of pediatric acute myeloid leukemia reveals a changing mutational cers. 2021;13:789. https://doi.org/10.3390/cancers13040789
landscape from disease diagnosis to relapse. Cancer Res. 2016;76:2197–205. 34. White T, Kaspers G, Abrahamsson J, Arad-Cohen N, Cianci D, Fernandez J, et al.
12. Umeda M, Ma J, Huang BJ, Hagiwara K, Westover T, Abdelhamed S, et al. Clinical outcomes of second relapsed and refractory first relapsed paediatric
Integrated genomic analysis identifies UBTF tandem duplications as a recurrent AML: a retrospective study within the NOPHO-DB SHIP consortium. Br J Hae-
lesion in pediatric acute myeloid leukemia. Blood Cancer Discov. matol. 2022. https://doi.org/10.1111/bjh.18039
2022;3:194–207. https://doi.org/10.1158/2643-3230.BCD-21-0160 35. Sharma A, Li Y, Huang S, Talleur AC, Suliman A, Qudeimat A, et al. Outcomes of
13. Balgobind BV, Zwaan CM, Pieters R, Van den Heuvel-Eibrink MM. The hetero- pediatric patients who relapse after first HCT for acute leukemia or MDS. Bone
geneity of pediatric MLL-rearranged acute myeloid leukemia. Leukemia. Marrow Transpl. 2021;56:1866–75.
2011;25:1239–48. 36. Wells RJ, Adams MT, Alonzo TA, Arceci RJ, Buckley J, Buxton AB, et al. Mitox-
14. Michmerhuizen NL, Klco JM, Mullighan CG. Mechanistic insights and potential antrone and cytarabine induction, high-dose cytarabine, and etoposide inten-
therapeutic approaches for NUP98-rearranged hematologic malignancies. sification for pediatric patients with relapsed or refractory acute myeloid
Blood. 2020;136:2275–89. leukemia: Children’s Cancer Group Study 2951. J Clin Oncol. 2003;21:2940–7.
15. Gruber TA, Larson Gedman A, Zhang J, Koss CS, Marada S, Ta HQ, et al. An Inv 37. Jeha S, Razzouk B, Rytting M, Rheingold S, Albano E, Kadota R, et al. Phase II
(16)(p13.3q24.3)-encoded CBFA2T3-GLIS2 fusion protein defines an aggressive study of clofarabine in pediatric patients with refractory or relapsed acute
subtype of pediatric acute megakaryoblastic leukemia. Cancer Cell. myeloid leukemia. J Clin Oncol. 2009;27:4392–7.
2012;22:683–97. 38. Cooper TM, Alonzo TA, Gerbing RB, Perentesis JP, Whitlock JA, Taub JW, et al.
16. Forgione MO, McClure BJ, Yeung DT, Eadie LN, White DL. MLLT10 rearranged AAML0523: a report from the Children’s Oncology Group on the efficacy of
acute leukemia: Incidence, prognosis, and possible therapeutic strategies. Genes clofarabine in combination with cytarabine in pediatric patients with recurrent
Chromosomes Cancer. 2020. https://doi.org/10.1002/gcc.22887 acute myeloid leukemia. Cancer. 2014;120:2482–9.
17. Sotoca AM, Prange KH, Reijnders B, Mandoli A, Nguyen LN, Stunnenberg HG, 39. van Eijkelenburg NKA, Rasche M, Ghazaly E, Dworzak MN, Klingebiel T, Rossig C,
et al. The oncofusion protein FUS-ERG targets key hematopoietic regulators and et al. Clofarabine, high-dose cytarabine and liposomal daunorubicin in pediatric
modulates the all-trans retinoic acid signaling pathway in t(16;21) acute myeloid relapsed/refractory acute myeloid leukemia: a phase IB study. Haematologica.
leukemia. Oncogene. 2016;35:1965–76. 2018;103:1484–92.
18. Diaz-Beya M, Labopin M, Maertens J, Aljurf M, Passweg J, Dietrich B, et al. 40. Messinger Y, Boklan J, Goldberg J, DuBois SG, Oesterheld J, Abla O, et al.
Allogeneic stem cell transplantation in AML with t(6;9)(p23;q34);DEK- Combination of clofarabine, cyclophosphamide, and etoposide for relapsed or
NUP214 shows a favourable outcome when performed in first complete refractory childhood and adolescent acute myeloid leukemia. Pediatr Hematol
remission. Br J Haematol. 2020;189:920–5. Oncol. 2017;34:187–98.
19. Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy 41. Shukla N, Kobos R, Renaud T, Steinherz LJ, Steinherz PG. Phase II trial of clo-
that originates from a primitive hematopoietic cell. Nat Med. 1997;3:730–7. farabine with topotecan, vinorelbine, and thiotepa in pediatric patients with
20. Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-Cortes J, et al. A cell relapsed or refractory acute leukemia. Pediatr Blood Cancer. 2014;61:431–5.
initiating human acute myeloid leukaemia after transplantation into SCID mice. 42. Inaba H, Stewart CF, Crews KR, Yang S, Pounds S, Pui CH, et al. Combination of
Nature. 1994;367:645–8. cladribine plus topotecan for recurrent or refractory pediatric acute myeloid
21. Thomas D, Majeti R. Biology and relevance of human acute myeloid leukemia leukemia. Cancer. 2010;116:98–105.
stem cells. Blood. 2017;129:1577–85. 43. Kolb EA, Steinherz PG. A new multidrug reinduction protocol with topotecan,
22. Duployez N, Marceau-Renaut A, Villenet C, Petit A, Rousseau A, Ng SWK, et al. vinorelbine, thiotepa, dexamethasone, and gemcitabine for relapsed or refrac-
The stem cell-associated gene expression signature allows risk stratification in tory acute leukemia. Leukemia. 2003;17:1967–72.
pediatric acute myeloid leukemia. Leukemia. 2019;33:348–57. 44. Cooper TM, Absalon MJ, Alonzo TA, Gerbing RB, Leger KJ, Hirsch BA, et al. Phase
23. Ng SW, Mitchell A, Kennedy JA, Chen WC, McLeod J, Ibrahimova N, et al. A 17- I/II study of CPX-351 followed by fludarabine, cytarabine, and granulocyte-
gene stemness score for rapid determination of risk in acute leukaemia. Nature. colony stimulating factor for children with relapsed acute myeloid leukemia: a
2016;540:433–7. report from the Children’s Oncology Group. J Clin Oncol. 2020;38:2170–7.
24. Elsayed AH, Rafiee R, Cao X, Raimondi S, Downing JR, Ribeiro R, et al. A six-gene 45. O’Brien MM, Lacayo NJ, Lum BL, Kshirsagar S, Buck S, Ravindranath Y, et al.
leukemic stem cell score identifies high risk pediatric acute myeloid leukemia. Phase I study of valspodar (PSC-833) with mitoxantrone and etoposide in
Leukemia. 2020;34:735–45. refractory and relapsed pediatric acute leukemia: a report from the Children’s
25. Angenendt L, Woste M, Mikesch JH, Arteaga MF, Angenendt A, Sandmann S, Oncology Group. Pediatr Blood Cancer. 2010;54:694–702.
et al. Calcitonin receptor-like (CALCRL) is a marker of stemness and an inde- 46. O’Brien MM, Alonzo TA, Cooper TM, Levine JE, Brown PA, Slone T, et al. Results
pendent predictor of outcome in pediatric AML. Blood Adv. 2021;5:4413–21. of a phase 2, multicenter, single-arm, open-label study of lenalidomide in
26. Jones L, McCarthy P, Bond J. Epigenetics of paediatric acute myeloid leukaemia. pediatric patients with relapsed or refractory acute myeloid leukemia. Pediatr
Br J Haematol. 2020;188:63–76. Blood Cancer. 2021;68:e28946.
27. Aladjidi N, Auvrignon A, Leblanc T, Perel Y, Benard A, Bordigoni P, et al. Out- 47. Horton TM, Perentesis JP, Gamis AS, Alonzo TA, Gerbing RB, Ballard J, et al. A
come in children with relapsed acute myeloid leukemia after initial treatment Phase 2 study of bortezomib combined with either idarubicin/cytarabine or
with the French Leucemie Aique Myeloide Enfant (LAME) 89/91 protocol of the cytarabine/etoposide in children with relapsed, refractory or secondary acute
French Society of Pediatric Hematology and Immunology. J Clin Oncol. myeloid leukemia: a report from the Children’s Oncology Group. Pediatr Blood
2003;21:4377–85. Cancer. 2014;61:1754–60.
28. Sander A, Zimmermann M, Dworzak M, Fleischhack G, von Neuhoff C, Reinhardt 48. Cooper TM, Sison EAR, Baker SD, Li L, Ahmed A, Trippett T, et al. A phase 1 study
D, et al. Consequent and intensified relapse therapy improved survival in of the CXCR4 antagonist plerixafor in combination with high-dose cytarabine
pediatric AML: results of relapse treatment in 379 patients of three consecutive and etoposide in children with relapsed or refractory acute leukemias or mye-
AML-BFM trials. Leukemia. 2010;24:1422–8. lodysplastic syndrome: A Pediatric Oncology Experimental Therapeutics Inves-
29. Gorman MF, Ji L, Ko RH, Barnette P, Bostrom B, Hutchinson R, et al. Outcome for tigators’ Consortium study (POE 10-03). Pediatr Blood Cancer. 2017;64:10.1002/
children treated for relapsed or refractory acute myelogenous leukemia (rAML): pbc.26414. https://doi.org/10.1002/pbc.26414
a Therapeutic Advances in Childhood Leukemia (TACL) Consortium study. 49. Alexander TB, Lacayo NJ, Choi JK, Ribeiro RC, Pui CH, Rubnitz JE. Phase I study of
Pediatr Blood Cancer. 2010;55:421–9. selinexor, a selective inhibitor of nuclear export, in combination with fludar-
30. Nakayama H, Tabuchi K, Tawa A, Tsukimoto I, Tsuchida M, Morimoto A, et al. abine and cytarabine, in pediatric relapsed or refractory acute leukemia. J Clin
Outcome of children with relapsed acute myeloid leukemia following initial Oncol. 2016;34:4094–101.
therapy under the AML99 protocol. Int J Hematol. 2014;100:171–9. 50. Karol SE, Cooper TM, Mead PE, Crews KR, Panetta JC, Alexander TB, et al. Safety,
31. Moritake H, Tanaka S, Miyamura T, Nakayama H, Shiba N, Shimada A, et al. The pharmacokinetics, and pharmacodynamics of panobinostat in children, ado-
outcomes of relapsed acute myeloid leukemia in children: results from the lescents, and young adults with relapsed acute myeloid leukemia. Cancer.
Japanese Pediatric Leukemia/Lymphoma Study Group AML-05R study. Pediatr 2020;126:4800–5.
Blood Cancer. 2021;68:e28736. 51. Sun W, Triche T Jr, Malvar J, Gaynon P, Sposto R, Yang X, et al. A phase 1 study of
32. Karlsson L, Forestier E, Hasle H, Jahnukainen K, Jonsson OG, Lausen B, et al. azacitidine combined with chemotherapy in childhood leukemia: a report from
Outcome after intensive reinduction therapy and allogeneic stem cell transplant the TACL consortium. Blood. 2018;131:1145–8.
in paediatric relapsed acute myeloid leukaemia. Br J Haematol. 52. Karol SE, Alexander TB, Budhraja A, Pounds SB, Canavera K, Wang L, et al.
2017;178:592–602. Venetoclax in combination with cytarabine with or without idarubicin in chil-
33. Rasche M, Steidel E, Zimmermann M, Bourquin JP, Boztug H, Janotova I, et al. dren with relapsed or refractory acute myeloid leukaemia: a phase 1, dose-
Second relapse of pediatric patients with acute myeloid leukemia: a report on escalation study. Lancet Oncol. 2020;21:551–60.
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1959
53. Pommert L, Schafer ES, Malvar J, Gossai N, Florendo E, Pulakanti K, et al. Deci- 75. Nechiporuk T, Kurtz SE, Nikolova O, Liu T, Jones CL, D’Alessandro A, et al. The
tabine and vorinostat with FLAG chemotherapy in pediatric relapsed/refractory TP53 apoptotic network is a primary mediator of resistance to BCL2 inhibition in
AML: report from the therapeutic advances in childhood leukemia and lym- AML cells. Cancer Disco. 2019;9:910–25.
phoma (TACL) consortium. Am J Hematol. 2022;97:613–22. https://doi.org/ 76. Pan R, Ruvolo V, Mu H, Leverson JD, Nichols G, Reed JC, et al. Synthetic lethality
10.1002/ajh.26510 of combined Bcl-2 inhibition and p53 activation in AML: mechanisms and
54. Konopleva M, Letai A. BCL-2 inhibition in AML: an unexpected bonus? Blood. superior antileukemic efficacy. Cancer Cell. 2017;32:748–60.e746.
2018;132:1007–12. 77. DiNardo CD, Tiong IS, Quaglieri A, MacRaild S, Loghavi S, Brown FC, et al.
55. Konopleva M, Pollyea DA, Potluri J, Chyla B, Hogdal L, Busman T, et al. Efficacy Molecular patterns of response and treatment failure after frontline venetoclax
and biological correlates of response in a phase II study of venetoclax mono- combinations in older patients with AML. Blood. 2020;135:791–803.
therapy in patients with acute myelogenous leukemia. Cancer Disco. 78. Stahl M, Menghrajani K, Derkach A, Chan A, Xiao W, Glass J, et al. Clinical and
2016;6:1106–17. molecular predictors of response and survival following venetoclax therapy in
56. Pan R, Hogdal LJ, Benito JM, Bucci D, Han L, Borthakur G, et al. Selective BCL-2 relapsed/refractory AML. Blood Adv. 2021;5:1552–64.
inhibition by ABT-199 causes on-target cell death in acute myeloid leukemia. 79. Yokoyama A, Somervaille TC, Smith KS, Rozenblatt-Rosen O, Meyerson M, Cleary
Cancer Disco. 2014;4:362–75. ML. The menin tumor suppressor protein is an essential oncogenic cofactor for
57. DiNardo CD, Pratz KW, Letai A, Jonas BA, Wei AH, Thirman M, et al. Safety and MLL-associated leukemogenesis. Cell. 2005;123:207–18.
preliminary efficacy of venetoclax with decitabine or azacitidine in elderly 80. Chen CW, Armstrong SA. Targeting DOT1L and HOX gene expression in MLL-
patients with previously untreated acute myeloid leukaemia: a non-randomised, rearranged leukemia and beyond. Exp Hematol. 2015;43:673–84.
open-label, phase 1b study. Lancet Oncol. 2018;19:216–28. 81. Stein EM, Garcia-Manero G, Rizzieri DA, Tibes R, Berdeja JG, Savona MR, et al. The
58. Wei AH, Strickland SA Jr, Hou JZ, Fiedler W, Lin TL, Walter RB, et al. Venetoclax DOT1L inhibitor pinometostat reduces H3K79 methylation and has modest
combined with low-dose cytarabine for previously untreated patients with clinical activity in adult acute leukemia. Blood. 2018;131:2661–9.
acute myeloid leukemia: results from a phase Ib/II study. J Clin Oncol. 82. Borkin D, He S, Miao H, Kempinska K, Pollock J, Chase J, et al. Pharmacologic
2019;37:1277–84. inhibition of the Menin-MLL interaction blocks progression of MLL leukemia
59. DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azaci- in vivo. Cancer Cell. 2015;27:589–602.
tidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J 83. Klossowski S, Miao H, Kempinska K, Wu T, Purohit T, Kim E, et al. Menin inhibitor
Med. 2020;383:617–29. MI-3454 induces remission in MLL1-rearranged and NPM1-mutated models of
60. Pearson ADJ, Zwaan CM, Kolb EA, Karres D, Guillot J, Kim SY, et al. Paediatric leukemia. J Clin Invest. 2020;130:981–97.
Strategy Forum for medicinal product development for acute myeloid leukae- 84. Krivtsov AV, Evans K, Gadrey JY, Eschle BK, Hatton C, Uckelmann HJ, et al. A
mia in children and adolescents: ACCELERATE in collaboration with the Eur- Menin-MLL inhibitor induces specific chromatin changes and eradicates disease
opean Medicines Agency with participation of the Food and Drug in models of MLL-rearranged leukemia. Cancer Cell. 2019;36:660–73.e611.
Administration. Eur J Cancer. 2020;136:116–29. 85. Uckelmann HJ, Kim SM, Wong EM, Hatton C, Giovinazzo H, Gadrey JY, et al.
61. Bhatt S, Pioso MS, Olesinski EA, Yilma B, Ryan JA, Mashaka T, et al. Reduced Therapeutic targeting of preleukemia cells in a mouse model of NPM1 mutant
mitochondrial apoptotic priming drives resistance to BH3 mimetics in acute acute myeloid leukemia. Science. 2020;367:586–90.
myeloid leukemia. Cancer Cell. 2020;38:872–90.e876. 86. Heikamp EB, Henrich JA, Perner F, Wong EM, Hatton C, Wen Y, et al. The Menin-
62. Chen X, Glytsou C, Zhou H, Narang S, Reyna DE, Lopez A, et al. Targeting MLL1 interaction is a molecular dependency in NUP98-rearranged AML. Blood.
mitochondrial structure sensitizes acute myeloid leukemia to venetoclax treat- 2022;139:894–906. https://doi.org/10.1182/blood.2021012806
ment. Cancer Disco. 2019;9:890–909. 87. Issa GC, Ravandi F, DiNardo CD, Jabbour E, Kantarjian HM, Andreeff M. Ther-
63. Guieze R, Liu VM, Rosebrock D, Jourdain AA, Hernandez-Sanchez M, Martinez apeutic implications of menin inhibition in acute leukemias. Leukemia.
Zurita A, et al. Mitochondrial reprogramming underlies resistance to BCL-2 2021;35:2482–95.
inhibition in lymphoid malignancies. Cancer Cell. 2019;36:369–84.e313. 88. Hahn CK, Berchuck JE, Ross KN, Kakoza RM, Clauser K, Schinzel AC, et al. Pro-
64. Roberts AW, Wei AH, Huang DCS. BCL2 and MCL1 inhibitors for hematologic teomic and genetic approaches identify Syk as an AML target. Cancer Cell.
malignancies. Blood. 2021;138:1120–36. 2009;16:281–94.
65. Pullarkat VA, Lacayo NJ, Jabbour E, Rubnitz JE, Bajel A, Laetsch TW, et al. 89. Tyner JW, Tognon CE, Bottomly D, Wilmot B, Kurtz SE, Savage SL, et al. Func-
Venetoclax and navitoclax in combination with chemotherapy in patients with tional genomic landscape of acute myeloid leukaemia. Nature. 2018;562:526–31.
relapsed or refractory acute lymphoblastic leukemia and lymphoblastic lym- 90. Walker AR, Byrd JC, Blachly JS, Bhatnagar B, Mims AS, Orwick S, et al. Entos-
phoma. Cancer Disco. 2021;11:1440–53. pletinib in combination with induction chemotherapy in previously untreated
66. Ramsey HE, Fischer MA, Lee T, Gorska AE, Arrate MP, Fuller L, et al. A novel MCL1 acute myeloid leukemia: response and predictive significance of HOXA9 and
inhibitor combined with venetoclax rescues venetoclax-resistant acute myelo- MEIS1 expression. Clin Cancer Res. 2020;26:5852–9.
genous leukemia. Cancer Disco. 2018;8:1566–81. 91. Sprussel A, Schulte JH, Weber S, Necke M, Handschke K, Thor T, et al. Lysine-
67. Caenepeel S, Brown SP, Belmontes B, Moody G, Keegan KS, Chui D, et al. AMG specific demethylase 1 restricts hematopoietic progenitor proliferation and is
176, a selective MCL1 inhibitor, is effective in hematologic cancer models essential for terminal differentiation. Leukemia. 2012;26:2039–51.
alone and in combination with established therapies. Cancer Disco. 92. Harris WJ, Huang X, Lynch JT, Spencer GJ, Hitchin JR, Li Y, et al. The histone
2018;8:1582–97. demethylase KDM1A sustains the oncogenic potential of MLL-AF9 leukemia
68. Kotschy A, Szlavik Z, Murray J, Davidson J, Maragno AL, Le Toumelin-Braizat G, stem cells. Cancer Cell. 2012;21:473–87.
et al. The MCL1 inhibitor S63845 is tolerable and effective in diverse cancer 93. Salamero O, Montesinos P, Willekens C, Perez-Simon JA, Pigneux A, Recher C,
models. Nature. 2016;538:477–82. et al. First-in-human phase I study of iadademstat (ORY-1001): a first-in-class
69. Luedtke DA, Su Y, Liu S, Edwards H, Wang Y, Lin H, et al. Inhibition of XPO1 lysine-specific histone demethylase 1A inhibitor, in relapsed or refractory acute
enhances cell death induced by ABT-199 in acute myeloid leukaemia via Mcl-1. J myeloid leukemia. J Clin Oncol. 2020;38:4260–73.
Cell Mol Med. 2018;22:6099–111. 94. Soucy TA, Smith PG, Milhollen MA, Berger AJ, Gavin JM, Adhikari S, et al. An
70. Fischer MA, Friedlander SY, Arrate MP, Chang H, Gorska AE, Fuller LD, et al. inhibitor of NEDD8-activating enzyme as a new approach to treat cancer. Nat-
Venetoclax response is enhanced by selective inhibitor of nuclear export ure. 2009;458:732–6.
compounds in hematologic malignancies. Blood Adv. 2020;4:586–98. 95. Kontandreopoulou CN, Diamantopoulos PT, Tiblalexi D, Giannakopoulou N,
71. Niu X, Zhao J, Ma J, Xie C, Edwards H, Wang G, et al. Binding of released Bim to Viniou NA. PARP1 as a therapeutic target in acute myeloid leukemia and
Mcl-1 is a mechanism of intrinsic resistance to ABT-199 which can be overcome myelodysplastic syndrome. Blood Adv. 2021;5:4794–805.
by combination with daunorubicin or cytarabine in AML cells. Clin Cancer Res. 96. Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, et al. Specific
2016;22:4440–51. killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) poly-
72. Teh TC, Nguyen NY, Moujalled DM, Segal D, Pomilio G, Rijal S, et al. Enhancing merase. Nature. 2005;434:913–7.
venetoclax activity in acute myeloid leukemia by co-targeting MCL1. Leukemia. 97. Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, et al. Tar-
2018;32:303–12. geting the DNA repair defect in BRCA mutant cells as a therapeutic strategy.
73. Luedtke DA, Su Y, Ma J, Li X, Buck SA, Edwards H, et al. Inhibition of CDK9 by Nature. 2005;434:917–21.
voruciclib synergistically enhances cell death induced by the Bcl-2 selective 98. Maifrede S, Martinez E, Nieborowska-Skorska M, Di Marcantonio D, Hulse M, Le
inhibitor venetoclax in preclinical models of acute myeloid leukemia. Signal BV, et al. MLL-AF9 leukemias are sensitive to PARP1 inhibitors combined with
Transduct Target Ther. 2020;5:17. cytotoxic drugs. Blood Adv. 2017;1:1467–72.
74. Phillips DC, Jin S, Gregory GP, Zhang Q, Xue J, Zhao X, et al. A novel CDK9 99. Barbier V, Erbani J, Fiveash C, Davies JM, Tay J, Tallack MR, et al. Endothelial
inhibitor increases the efficacy of venetoclax (ABT-199) in multiple models of E-selectin inhibition improves acute myeloid leukaemia therapy by disrupting
hematologic malignancies. Leukemia. 2020;34:1646–57. vascular niche-mediated chemoresistance. Nat Commun. 2020;11:2042.
Leukemia (2022) 36:1951 – 1960
S. Zarnegar-Lumley et al.
1960
100. DeAngelo DJ, Jonas BA, Liesveld JL, Bixby DL, Advani AS, Marlton P, et al. Phase 122. McNeer NA, Philip J, Geiger H, Ries RE, Lavallee VP, Walsh M, et al. Genetic
1/2 study of uproleselan added to chemotherapy in patients with relapsed or mechanisms of primary chemotherapy resistance in pediatric acute myeloid
refractory acute myeloid leukemia. Blood. 2022;139:1135–46. https://doi.org/ leukemia. Leukemia. 2019;33:1934–43.
10.1182/blood.2021010721 123. Rafiq S, Purdon TJ, Daniyan AF, Koneru M, Dao T, Liu C, et al. Optimized T-cell
101. Kent A, Vasu S, Schatz D, Monson N, Devine S, Smith C, et al. Glasdegib as receptor-mimic chimeric antigen receptor T cells directed toward the intracel-
maintenance therapy for patients with AML and MDS patients at high risk for lular Wilms Tumor 1 antigen. Leukemia. 2017;31:1788–97.
postallogeneic stem cell transplant relapse. Blood Adv. 2020;4:3102–8. 124. Chapuis AG, Egan DN, Bar M, Schmitt TM, McAfee MS, Paulson KG, et al. T cell
102. Schmoellerl J, Barbosa IAM, Eder T, Brandstoetter T, Schmidt L, Maurer B, et al. receptor gene therapy targeting WT1 prevents acute myeloid leukemia relapse
CDK6 is an essential direct target of NUP98 fusion proteins in acute myeloid post-transplant. Nat Med. 2019;25:1064–72.
leukemia. Blood. 2020;136:387–400. 125. Augsberger C, Hanel G, Xu W, Pulko V, Hanisch LJ, Augustin A, et al. Targeting
103. Pikman Y, Tasian SK, Sulis ML, Stevenson K, Blonquist TM, Apsel Winger B, et al. intracellular WT1 in AML with a novel RMF-peptide-MHC-specific T-cell bispecific
Matched targeted therapy for pediatric patients with relapsed, refractory, or antibody. Blood. 2021;138:2655–69.
high-risk leukemias: a report from the LEAP Consortium. Cancer Disco. 126. Zhang H, Wang P, Li Z, He Y, Gan W, Jiang H. Anti-CLL1 chimeric antigen
2021;11:1424–39. receptor T-cell therapy in children with relapsed/refractory acute myeloid leu-
104. Borthakur G, Popplewell L, Boyiadzis M, Foran J, Platzbecker U, Vey N, et al. kemia. Clin Cancer Res. 2021;27:3549–55.
Activity of the oral mitogen-activated protein kinase kinase inhibitor trametinib 127. Riether C, Schurch CM, Buhrer ED, Hinterbrandner M, Huguenin AL, Hoepner S,
in RAS-mutant relapsed or refractory myeloid malignancies. Cancer. et al. CD70/CD27 signaling promotes blast stemness and is a viable therapeutic
2016;122:1871–9. target in acute myeloid leukemia. J Exp Med. 2017;214:359–80.
105. DiNardo CD, Stein EM, de Botton S, Roboz GJ, Altman JK, Mims AS, et al. Durable 128. Riether C, Pabst T, Hopner S, Bacher U, Hinterbrandner M, Banz Y, et al. Tar-
remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N Engl J geting CD70 with cusatuzumab eliminates acute myeloid leukemia stem cells in
Med. 2018;378:2386–98. patients treated with hypomethylating agents. Nat Med. 2020;26:1459–67.
106. Stein EM, Fathi AT, DiNardo CD, Pollyea DA, Roboz GJ, Collins R, et al. Enasidenib 129. Sauer T, Parikh K, Sharma S, Omer B, Sedloev D, Chen Q, et al. CD70-specific CAR
in patients with mutant IDH2 myelodysplastic syndromes: a phase 1 subgroup T cells have potent activity against acute myeloid leukemia without HSC toxicity.
analysis of the multicentre, AG221-C-001 trial. Lancet Haematol. 2020;7:e309–19. Blood. 2021;138:318–30.
107. Levis M, Perl AE. Gilteritinib: potent targeting of FLT3 mutations in AML. Blood 130. Sun X, Wang G, Zuo S, Niu Q, Chen X, Feng X. Preclinical evaluation of CD64 as a
Adv. 2020;4:1178–91. potential target for CAR-T-cell therapy for acute myeloid leukemia. J Immun-
108. Lamble AJ, Tasian SK. Opportunities for immunotherapy in childhood acute other. 2022;45:67–77. https://doi.org/10.1097/CJI.0000000000000406
myeloid leukemia. Blood Adv. 2019;3:3750–8. 131. Willier S, Rothamel P, Hastreiter M, Wilhelm J, Stenger D, Blaeschke F, et al.
109. Lamble AJ, Eidenschink Brodersen L, Alonzo TA, Wang J, Pardo L, Sung L, et al. CLEC12A and CD33 coexpression as a preferential target for pediatric AML
CD123 expression is associated with high-risk disease characteristics in child- combinatorial immunotherapy. Blood. 2021;137:1037–49.
hood acute myeloid leukemia: a report from the Children’s Oncology Group. J 132. Rubnitz JE, Inaba H, Ribeiro RC, Pounds S, Rooney B, Bell T, et al. NKAML: a pilot
Clin Oncol. 2022;40:252–61. study to determine the safety and feasibility of haploidentical natural killer cell
110. Vadakekolathu J, Lai C, Reeder S, Church SE, Hood T, Lourdusamy A, et al. TP53 transplantation in childhood acute myeloid leukemia. J Clin Oncol.
abnormalities correlate with immune infiltration and associate with response to 2010;28:955–9.
flotetuzumab immunotherapy in AML. Blood Adv. 2020;4:5011–24. 133. Bednarski JJ, Zimmerman C, Berrien-Elliott MM, Foltz JA, Becker-Hapak M, Neal
111. Uy GL, Aldoss I, Foster MC, Sayre PH, Wieduwilt MJ, Advani AS, et al. Flotetu- CC, et al. Donor memory-like NK cells persist and induce remissions in pediatric
zumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood. patients with relapsed AML after transplant. Blood. 2022;139:1670–83.
2021;137:751–62. 134. Weaver MS, Heinze KE, Kelly KP, Wiener L, Casey RL, Bell CJ, et al. Palliative care
112. Angelova E, Audette C, Kovtun Y, Daver N, Wang SA, Pierce S, et al. CD123 as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62:
expression patterns and selective targeting with a CD123-targeted antibody- S829–33.
drug conjugate (IMGN632) in acute lymphoblastic leukemia. Haematologica. 135. Snaman J, McCarthy S, Wiener L, Wolfe J. Pediatric palliative care in oncology. J
2019;104:749–55. Clin Oncol. 2020;38:954–62.
113. Pemmaraju N, Lane AA, Sweet KL, Stein AS, Vasu S, Blum W, et al. Tagraxofusp in
blastic plasmacytoid dendritic-cell neoplasm. N Engl J Med. 2019;380:1628–37.
114. Pollard JA, Loken M, Gerbing RB, Raimondi SC, Hirsch BA, Aplenc R, et al. CD33 AUTHOR CONTRIBUTIONS
expression and its association with gemtuzumab ozogamicin response: results SZ-L, KJC, and JER contributed to the preparation of the manuscript and reviewed
from the randomized phase III Children’s Oncology Group Trial AAML0531. J Clin and approved the final manuscript.
Oncol. 2016;34:747–55.
115. Hoseini SS, Guo H, Wu Z, Hatano MN, Cheung NV. A potent tetravalent T-cell-
engaging bispecific antibody against CD33 in acute myeloid leukemia. Blood
Adv. 2018;2:1250–8. FUNDING
116. Jaiswal S, Jamieson CH, Pang WW, Park CY, Chao MP, Majeti R, et al. CD47 is JER was supported by American Lebanese Syrian Associated Charities and National
upregulated on circulating hematopoietic stem cells and leukemia cells to avoid Institutes of Health CA21765.
phagocytosis. Cell. 2009;138:271–85.
117. Majeti R, Chao MP, Alizadeh AA, Pang WW, Jaiswal S, Gibbs KD Jr, et al. CD47 is
an adverse prognostic factor and therapeutic antibody target on human acute COMPETING INTERESTS
myeloid leukemia stem cells. Cell. 2009;138:286–99. The authors declare no competing interests.
118. Sikic BI, Lakhani N, Patnaik A, Shah SA, Chandana SR, Rasco D, et al. First-in-
human, first-in-class phase I trial of the anti-CD47 antibody Hu5F9-G4 in patients
with advanced cancers. J Clin Oncol. 2019;37:946–53. ADDITIONAL INFORMATION
119. Chao MP, Takimoto CH, Feng DD, McKenna K, Gip P, Liu J, et al. Therapeutic Correspondence and requests for materials should be addressed to Jeffrey E.
targeting of the macrophage immune checkpoint CD47 in myeloid malig- Rubnitz.
nancies. Front Oncol. 2019;9:1380.
120. Wang C, Sallman DA. Targeting the cluster of differentiation 47/signal-reg- Reprints and permission information is available at http://www.nature.com/
ulatory protein alpha axis in myeloid malignancies. Curr Opin Hematol. reprints
2022;29:44–52.
121. Ho PA, Zeng R, Alonzo TA, Gerbing RB, Miller KL, Pollard JA, et al. Prevalence and Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims
prognostic implications of WT1 mutations in pediatric acute myeloid leukemia in published maps and institutional affiliations.
(AML): a report from the Children’s Oncology Group. Blood. 2010;116:702–10.
Leukemia (2022) 36:1951 – 1960
You might also like
- Guideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementDocument26 pagesGuideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementYo Me100% (1)
- 00130478-202105000-00006 Serial Neurologic Assessment in Pediatrics (SNAP) : A New Tool For Bedside Neurologic Assessment of Critically Ill ChildrenDocument13 pages00130478-202105000-00006 Serial Neurologic Assessment in Pediatrics (SNAP) : A New Tool For Bedside Neurologic Assessment of Critically Ill ChildrenYo MeNo ratings yet
- Introduction To Psychiatric NursingDocument11 pagesIntroduction To Psychiatric NursingjoycechicagoNo ratings yet
- NBME 7 Answers KathyDocument6 pagesNBME 7 Answers KathySubash Ghimire88% (17)
- Injection Overmolding For Aesthetics and Strength Part 1Document4 pagesInjection Overmolding For Aesthetics and Strength Part 1The Bioclear ClinicNo ratings yet
- Recent Advances in Managing Acute Lymphoblastic LeukemiaDocument13 pagesRecent Advances in Managing Acute Lymphoblastic LeukemiaAndra GeorgianaNo ratings yet
- Acute Myeloid Leukemia...Document20 pagesAcute Myeloid Leukemia...hemendre0% (1)
- Treatment of Infant Leukemias Challenge and PromiseDocument5 pagesTreatment of Infant Leukemias Challenge and PromiseSyifa SariNo ratings yet
- Pi Is 1083879110001576Document9 pagesPi Is 1083879110001576cyntmeirelessNo ratings yet
- Leucemia GenomicaDocument14 pagesLeucemia GenomicaNathalie Soler BarreraNo ratings yet
- Acute Myeloid Leukemia in Children 2016Document10 pagesAcute Myeloid Leukemia in Children 2016Jorge Eduardo Espinoza RiosNo ratings yet
- 2019 Molecular Approaches To Treating Pediatric LeukemiasDocument12 pages2019 Molecular Approaches To Treating Pediatric LeukemiasIverson LewisNo ratings yet
- AmlDocument29 pagesAmlSari HestiyariniNo ratings yet
- How I Treat Pediatri CacutemyeloidleukemiaDocument10 pagesHow I Treat Pediatri CacutemyeloidleukemiaValeria FuentesNo ratings yet
- Res Medica: Journal of The Royal Medical SocietyDocument11 pagesRes Medica: Journal of The Royal Medical SocietyDwika AudiyanandaNo ratings yet
- AYASDocument11 pagesAYASXimena GarcíaNo ratings yet
- Treatment of Acute Lymphoblastic Leukemia: Review ArticleDocument13 pagesTreatment of Acute Lymphoblastic Leukemia: Review ArticlehoshihopeNo ratings yet
- Current and Emerging Therapies For Acute Myeloid LeukemiaDocument22 pagesCurrent and Emerging Therapies For Acute Myeloid LeukemiaRutuja KuhikarNo ratings yet
- General Introduction and Outline of This ThesisDocument28 pagesGeneral Introduction and Outline of This Thesisali99No ratings yet
- From The Experts: How I Treat Older Patients With Acute Myeloid LeukemiaDocument12 pagesFrom The Experts: How I Treat Older Patients With Acute Myeloid LeukemiaWillyPeñaNo ratings yet
- Jurnal HemaDocument9 pagesJurnal Hematrisna amijayaNo ratings yet
- Acute Lymphoblastic Leukemia: John Han-Chih Chang Matthew M. Poppe Chia-Ho Hua Karen J. Marcus Natia EsiashviliDocument7 pagesAcute Lymphoblastic Leukemia: John Han-Chih Chang Matthew M. Poppe Chia-Ho Hua Karen J. Marcus Natia EsiashviliErvanda ZilmiNo ratings yet
- Mantle Cell Lymphoma ThesisDocument7 pagesMantle Cell Lymphoma Thesisgjdpj4jq100% (1)
- Acute Lymphoblastic Leukemia in Children and Adolescents: Prognostic Factors and Analysis of SurvivalDocument7 pagesAcute Lymphoblastic Leukemia in Children and Adolescents: Prognostic Factors and Analysis of SurvivalAbdurrahman HasanuddinNo ratings yet
- Blood Research and DisordersDocument7 pagesBlood Research and DisordersDea ArdiyatiNo ratings yet
- Acute Lymphoblastic Leukemia Research PaperDocument6 pagesAcute Lymphoblastic Leukemia Research Paperafeavbrpd100% (1)
- Acute Myeloid LeukemiaDocument11 pagesAcute Myeloid Leukemiafitra azraNo ratings yet
- Acute Lymphoblastic Leukaemia 2024Document28 pagesAcute Lymphoblastic Leukaemia 2024XRobert17No ratings yet
- Prognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergDocument11 pagesPrognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergStephania SandovalNo ratings yet
- Regimen Calgb 8811Document14 pagesRegimen Calgb 8811ricardo_cheNo ratings yet
- Pediatric Blood Cancer - 2023 - Abstracts From The 39th Annual Meeting of The Histiocyte SocietyDocument64 pagesPediatric Blood Cancer - 2023 - Abstracts From The 39th Annual Meeting of The Histiocyte SocietySeham GoharNo ratings yet
- Biol Blood Marrow Transplant 21 (2015) 653e660Document8 pagesBiol Blood Marrow Transplant 21 (2015) 653e660Rhinaldy DanaraNo ratings yet
- Reviews: Chronic Lymphocytic Leukaemia: From Genetics To TreatmentDocument18 pagesReviews: Chronic Lymphocytic Leukaemia: From Genetics To Treatmentlengers poworNo ratings yet
- Bosch2019 PDFDocument18 pagesBosch2019 PDFlengers poworNo ratings yet
- Article 2Document5 pagesArticle 2Mahadev HaraniNo ratings yet
- Tratamento HodgkinDocument15 pagesTratamento HodgkinIsabella Claudino FernandesNo ratings yet
- Case StudyDocument10 pagesCase Studysabrown109No ratings yet
- Biomedicine & Pharmacotherapy: ReviewDocument8 pagesBiomedicine & Pharmacotherapy: ReviewAsfahani LatiefahNo ratings yet
- Background: Pediatric Acute Lymphoblastic LeukemiaDocument3 pagesBackground: Pediatric Acute Lymphoblastic LeukemiaNitin KumarNo ratings yet
- Nejme 1200409Document2 pagesNejme 1200409Arie Krisnayanti Ida AyuNo ratings yet
- Gribben, 2011 AlemtDocument7 pagesGribben, 2011 AlemtveraffulNo ratings yet
- Megan Wiese, MS, PA-C Naval Daver, MDDocument11 pagesMegan Wiese, MS, PA-C Naval Daver, MDFathiyya SalsabilaNo ratings yet
- Leukemia, Lymphoma Children PDFDocument31 pagesLeukemia, Lymphoma Children PDFPartha GanesanNo ratings yet
- Mixed Phenotype Acute LeukemiaDocument10 pagesMixed Phenotype Acute LeukemiaMarco Aurélio SartoriNo ratings yet
- Acute Lymphoblastic Leukaemia: SeminarDocument13 pagesAcute Lymphoblastic Leukaemia: Seminarklinik kf 275No ratings yet
- Successful Management of Granulocytic Sarcoma With Co - 2016 - Pediatric HematolDocument2 pagesSuccessful Management of Granulocytic Sarcoma With Co - 2016 - Pediatric HematolHawin NurdianaNo ratings yet
- Leukemia Research Paper Thesis StatementDocument9 pagesLeukemia Research Paper Thesis Statementaparnaharrisonstamford100% (1)
- Biology of Blood and Marrow Transplantation: Cellular TherapyDocument8 pagesBiology of Blood and Marrow Transplantation: Cellular TherapyFrankenstein MelancholyNo ratings yet
- Cancer Stem Cells From Concept To CureDocument9 pagesCancer Stem Cells From Concept To CurePrateek JoshiNo ratings yet
- Acute Myeloid Leukemia ThesisDocument5 pagesAcute Myeloid Leukemia ThesisBuyCheapEssayOmaha100% (2)
- Novel Immunotherapeutics in B-Cell Precursor ALLDocument23 pagesNovel Immunotherapeutics in B-Cell Precursor ALLqcywh2000No ratings yet
- Biology of Blood and Marrow TransplantationDocument6 pagesBiology of Blood and Marrow TransplantationFrankenstein MelancholyNo ratings yet
- How I Treat Acute Myeloid LeukemiaDocument10 pagesHow I Treat Acute Myeloid LeukemiaSutiara Prihatining TyasNo ratings yet
- Pediatrik LeukemiasDocument14 pagesPediatrik LeukemiasLefrina GusrianiiNo ratings yet
- 1548 FullDocument13 pages1548 FullsabarinaramNo ratings yet
- Pui 2006Document13 pagesPui 2006Eva ArdianahNo ratings yet
- JCM 08 01175 v2 PDFDocument28 pagesJCM 08 01175 v2 PDFAs'har AnwarNo ratings yet
- BR J Haematol - 2014 - Fuente - Managing Children With Chronic Myeloid Leukaemia CMLDocument15 pagesBR J Haematol - 2014 - Fuente - Managing Children With Chronic Myeloid Leukaemia CMLLissaberti AmaliahNo ratings yet
- Article Ang3Document9 pagesArticle Ang3Ayoub HajjarNo ratings yet
- Nejmoa1708566 PDFDocument10 pagesNejmoa1708566 PDFAhmad SahidNo ratings yet
- Original PapersDocument6 pagesOriginal PapersfxkryxieNo ratings yet
- American J Hematol - 2018 - Cortes - Glasdegib in Combination With Cytarabine and Daunorubicin in Patients With AML orDocument11 pagesAmerican J Hematol - 2018 - Cortes - Glasdegib in Combination With Cytarabine and Daunorubicin in Patients With AML orjayshethNo ratings yet
- HIT LLA Recaida en Pediatria 2020Document34 pagesHIT LLA Recaida en Pediatria 2020Nathalie Soler BarreraNo ratings yet
- Advances in The Treatment of Sickle CellDocument15 pagesAdvances in The Treatment of Sickle CellMayuri P KNo ratings yet
- Nejmra 2216691Document15 pagesNejmra 2216691Yo MeNo ratings yet
- Atypical Manifestations of Acute Coronary Syndrome - Throat Discomfort: A Multi-Center Observational StudyDocument8 pagesAtypical Manifestations of Acute Coronary Syndrome - Throat Discomfort: A Multi-Center Observational StudyYo MeNo ratings yet
- Acutekidneyinjuryin Cardiacsurgery: Christina Massoth,, Alexander Zarbock,, Melanie MeerschDocument12 pagesAcutekidneyinjuryin Cardiacsurgery: Christina Massoth,, Alexander Zarbock,, Melanie MeerschYo MeNo ratings yet
- LUTS - 2012 - PETERS - Effect of Sacral Neuromodulation Rate On Overactive Bladder Symptoms A Randomized CrossoverDocument5 pagesLUTS - 2012 - PETERS - Effect of Sacral Neuromodulation Rate On Overactive Bladder Symptoms A Randomized CrossoverYo MeNo ratings yet
- 2008 Psicologiadela Motivacionyla Emocion MC GrawDocument7 pages2008 Psicologiadela Motivacionyla Emocion MC GrawYo MeNo ratings yet
- New insights into β-cell failure, regeneration and replacementDocument2 pagesNew insights into β-cell failure, regeneration and replacementYo MeNo ratings yet
- Nejmra 2215289Document13 pagesNejmra 2215289Yo Me100% (1)
- Ensteins Anomaly of The Left-Sides Trucispid ValveDocument5 pagesEnsteins Anomaly of The Left-Sides Trucispid ValveYo MeNo ratings yet
- Thehealthscienceslibrarynetworkfor IndiaDocument30 pagesThehealthscienceslibrarynetworkfor IndiaYo MeNo ratings yet
- Identification of Circular Rnas AsDocument58 pagesIdentification of Circular Rnas AsYo MeNo ratings yet
- 430-Article Text-970-1-10-20181105Document4 pages430-Article Text-970-1-10-20181105Yo MeNo ratings yet
- Intensive & Critical Care NursingDocument5 pagesIntensive & Critical Care NursingYo MeNo ratings yet
- A National Study of Patient Safety Culture And.14Document7 pagesA National Study of Patient Safety Culture And.14Yo MeNo ratings yet
- Networking of Medical Libraries in Andhra Pradesh: A ProposalDocument13 pagesNetworking of Medical Libraries in Andhra Pradesh: A ProposalYo MeNo ratings yet
- Renal Outcomes Following Intravenous Contrast Administration in Patients With Acute Kidney Injury: A Multi-Site Retrospective Propensity-Adjusted AnalysisDocument11 pagesRenal Outcomes Following Intravenous Contrast Administration in Patients With Acute Kidney Injury: A Multi-Site Retrospective Propensity-Adjusted AnalysisYo Me100% (1)
- Out (1) Spinal AnesthesiaDocument5 pagesOut (1) Spinal AnesthesiaYo MeNo ratings yet
- Combined Spinal and Epidural ADocument5 pagesCombined Spinal and Epidural AYo MeNo ratings yet
- Tranexamic Acid Current Knowns and Unknowns.4Document1 pageTranexamic Acid Current Knowns and Unknowns.4Yo MeNo ratings yet
- BMJ p332 FullDocument1 pageBMJ p332 FullYo MeNo ratings yet
- Flexible Bioelectronics With Power Autonomous Sensing and Data AnalyticsDocument187 pagesFlexible Bioelectronics With Power Autonomous Sensing and Data AnalyticsYo MeNo ratings yet
- Stac2055 Classification of Cosmic Structures For Galaxies With Deep Learning: Connecting Cosmological Simulations With ObservationDocument17 pagesStac2055 Classification of Cosmic Structures For Galaxies With Deep Learning: Connecting Cosmological Simulations With ObservationYo MeNo ratings yet
- Leaf Letuce Lactuca Sativa L L 121 Growth in Hydroponics With Different Nutrient Solutions Used To Generate Ultrafine BubblesDocument13 pagesLeaf Letuce Lactuca Sativa L L 121 Growth in Hydroponics With Different Nutrient Solutions Used To Generate Ultrafine BubblesYo MeNo ratings yet
- Jama Ruopp 2022 RV 220007 1662040577.72953Document13 pagesJama Ruopp 2022 RV 220007 1662040577.72953Yo MeNo ratings yet
- 1-S2.0-S1878875022005460-Main Filum Terminale: A Comprehensive Review With Anatomical, Pathological, and Surgical ConsiderationDocument10 pages1-S2.0-S1878875022005460-Main Filum Terminale: A Comprehensive Review With Anatomical, Pathological, and Surgical ConsiderationYo MeNo ratings yet
- Bmj-2021-069211.full Reduce Unnecessary Use of Proton Pump InhibitorsDocument7 pagesBmj-2021-069211.full Reduce Unnecessary Use of Proton Pump InhibitorsYo MeNo ratings yet
- 00130478-202105000-00013 Improving "Neuro Checks" in Neonatal ICU and PICU Is A Serial Neurologic Assessment in PediatricsDocument3 pages00130478-202105000-00013 Improving "Neuro Checks" in Neonatal ICU and PICU Is A Serial Neurologic Assessment in PediatricsYo MeNo ratings yet
- The Role of Biased Data in Computerized Gender DiscriminationDocument6 pagesThe Role of Biased Data in Computerized Gender DiscriminationYo MeNo ratings yet
- Jama Samsky 2021 RV 210015 1636669111.74911Document11 pagesJama Samsky 2021 RV 210015 1636669111.74911Yo MeNo ratings yet
- Hepatitis C Education Class - 2009Document64 pagesHepatitis C Education Class - 2009BENNo ratings yet
- 6 - Immune Deficiency Diseases 2Document8 pages6 - Immune Deficiency Diseases 2Belle Galao GepteNo ratings yet
- English For Nursing Giving Direction in The HospitalDocument3 pagesEnglish For Nursing Giving Direction in The HospitalBrave First100% (1)
- Suz 183Document29 pagesSuz 183Benny Chris TantoNo ratings yet
- Gastrointestinal System Review QuestionsDocument10 pagesGastrointestinal System Review QuestionsSiena PlacinoNo ratings yet
- Anestesi Pada Pasien Gangguan GinjalDocument28 pagesAnestesi Pada Pasien Gangguan GinjallovianettesherryNo ratings yet
- Crack Powerpoint 3Document21 pagesCrack Powerpoint 3api-2851237360% (1)
- EstradiolDocument1 pageEstradiol3S - JOCSON, DENESE NICOLE LEE M.No ratings yet
- Parte 2 Complete Reflexology For Live (Inglés) Autor Barbara y Kevin Kunz-262-289Document28 pagesParte 2 Complete Reflexology For Live (Inglés) Autor Barbara y Kevin Kunz-262-289Hombres Alto ValorNo ratings yet
- Clinical Teaching ON Geriatric AssessmentDocument9 pagesClinical Teaching ON Geriatric AssessmentANITTA SNo ratings yet
- Weight ManagementDocument36 pagesWeight ManagementAbdur RehmanNo ratings yet
- EXPERTS AGAINST LOCKDOWN - Open Letter To An Taoiseach and Minister For HealthDocument6 pagesEXPERTS AGAINST LOCKDOWN - Open Letter To An Taoiseach and Minister For HealthPeterNo ratings yet
- Rinhs Science 8 4th Catch Up Activity 2 Digestive System Crossword PuzzleDocument2 pagesRinhs Science 8 4th Catch Up Activity 2 Digestive System Crossword PuzzleRyan BersaminNo ratings yet
- Gynaecology - Riley HarrisonDocument45 pagesGynaecology - Riley HarrisonFiras AliNo ratings yet
- A A A A C C C C A A A A D D D D Eeee M M M M IIII C C C C S S S S C C C C IIII Eeee N N N N C C C C Eeee S S S SDocument3 pagesA A A A C C C C A A A A D D D D Eeee M M M M IIII C C C C S S S S C C C C IIII Eeee N N N N C C C C Eeee S S S SnelisaNo ratings yet
- IGCSE Biology Text DDocument8 pagesIGCSE Biology Text DBlackphanthomNo ratings yet
- Use of Peripheral Nerve Stimulator To MonitorDocument4 pagesUse of Peripheral Nerve Stimulator To MonitorTurlough LynchNo ratings yet
- Clinical Aspects of IVHDocument11 pagesClinical Aspects of IVHsteffiwpNo ratings yet
- Fall2010 Pdfpage76Document99 pagesFall2010 Pdfpage76stro desuNo ratings yet
- Transtracheal Jet Ventilation: Learning ObjectivesDocument5 pagesTranstracheal Jet Ventilation: Learning ObjectivesRicardoNo ratings yet
- R01 Revitalife Drip Protocol - UPDATED 9-19-2018Document10 pagesR01 Revitalife Drip Protocol - UPDATED 9-19-2018Eking InNo ratings yet
- 2015 02 12 - Clinical LOINC TutorialDocument36 pages2015 02 12 - Clinical LOINC TutorialDaniel Vreeman100% (1)
- RH NegativeDocument4 pagesRH NegativeMitch LeeNo ratings yet
- Nhs Covid Pass - Vaccinated: Covid-19 Vaccine Astrazeneca Covid-19 Vaccine AstrazenecaDocument1 pageNhs Covid Pass - Vaccinated: Covid-19 Vaccine Astrazeneca Covid-19 Vaccine AstrazenecaSuzanne MurphyNo ratings yet
- Responsible Parenthood: Role of Father & Mother in The FamilyDocument7 pagesResponsible Parenthood: Role of Father & Mother in The FamilyBhenjo Hernandez BaronaNo ratings yet
- Nursing Care of The Family During PregnancyDocument23 pagesNursing Care of The Family During PregnancyGladys YaresNo ratings yet
- Ulcirex CapsuleDocument3 pagesUlcirex Capsulehk_scribdNo ratings yet