Professional Documents
Culture Documents
PROTOZOA
PROTOZOA
Uploaded by
miti.pongos.swu0 ratings0% found this document useful (0 votes)
6 views6 pagesProtozoa are classified as pathogenic, commensal, or opportunistic based on their interactions with humans. Pathogenic protozoa like Entamoeba histolytica exist in the human body and cause harm, while commensal protozoa like E. coli exist without harming their host. Opportunistic protozoa typically do not affect healthy individuals but can severely infect immunocompromised people. Protozoa are also classified by their location in the intestines, urogenital tract, blood, or tissues. E. histolytica is a pathogenic intestinal protozoan that can cause amoebic colitis and liver abscesses through ingestion of cysts or person-to-
Original Description:
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentProtozoa are classified as pathogenic, commensal, or opportunistic based on their interactions with humans. Pathogenic protozoa like Entamoeba histolytica exist in the human body and cause harm, while commensal protozoa like E. coli exist without harming their host. Opportunistic protozoa typically do not affect healthy individuals but can severely infect immunocompromised people. Protozoa are also classified by their location in the intestines, urogenital tract, blood, or tissues. E. histolytica is a pathogenic intestinal protozoan that can cause amoebic colitis and liver abscesses through ingestion of cysts or person-to-
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
6 views6 pagesPROTOZOA
PROTOZOA
Uploaded by
miti.pongos.swuProtozoa are classified as pathogenic, commensal, or opportunistic based on their interactions with humans. Pathogenic protozoa like Entamoeba histolytica exist in the human body and cause harm, while commensal protozoa like E. coli exist without harming their host. Opportunistic protozoa typically do not affect healthy individuals but can severely infect immunocompromised people. Protozoa are also classified by their location in the intestines, urogenital tract, blood, or tissues. E. histolytica is a pathogenic intestinal protozoan that can cause amoebic colitis and liver abscesses through ingestion of cysts or person-to-
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 6
Pre cyst stage
PROTOZOA
- 10-60 X 15-30u average (15-20u)
PATHOGENIC PROTOZOA - Round or oval with a blunt pseudopodia
- Protozoa that exist in human body and cause harm to - Absent cyst wall
infected human (E. histolytica, G. lamblia, B. coli) - Single nucleus present.
COMMENSAL PROTOZOA Cyst stage
- Protozoa that exist human body but does not cause harm
- 10-20u average (15u)
to infected human ( e.g. E. coli, E. dispar, E. hartmanni) -Responsible for - Four nuclei are present in mature
food storage
quadrinucleated cyst
OPPORTUNISTIC PROTOZOA
-Disappears - Glycogen mass & chromatoid bodies are present
- weak protozoa that cause minimal effect to infected during
in immature cysts –disappear in mature ones.
healthy man but has severe effect on infected excystation
immunocompromised man ( e.g. Cryptosporidium parvum) LIFE CYCLE (CHRONOLOGICAL ORDER)
POTENTIALLY PATHOGENIC FREE-LIVING PROTOZOA - Pre-cyst
- Free-living in nature away from man but some of them - Uninucleate cells
may cause disease if they enter the human body by certain - Binucleate cells
route. - Quadrinucleate cells
- - Trophozoites
CLASSIFFIED ACCORDING TO ITS LOCATION:
Pathogenesis
INTESTINES:
- Depends on the:
Amoeba : Entamoeba Virulence
Flagellates : Giardia Host resistance
Sporozoa : Cryptosporidium Condition of the Intestinal tract
Ciliates : Balantidium coli - How will E. histolytica burrow the intestinal
lumen?
UROGENITAL Answer: Due to the presence of
histolytic enzyme that is used to
Trichomonas
destroy the intestinal mucosa leading
BLOOD AND TISSUES to the formation of flask-shaped ulcer.
Trypanosoma Factors Determining Pathogenicity
Leishmania (Flagellates)
- Strain
Plasmodium
E. dispar similar to E. histolytica only
Toxoplasma
that E. dispar is non-invasive.
- Virulence
TROPHOZOITE CYST - Host Factors
Active / Vegetative Dormant Immunity
Feeding stage Infectious Stage Nutrition
Sensitive Highly resistant Drugs
Causes symptoms of the body Debilitating state
Intestine
- Followed by:
INTESTINAL PROTOZOAS (AMOEBA) Proliferation of connective tissue
Intensive Ulcerations
Entamoeba histolytica Extra-intestinal invasion to brain, liver,
- Pathogenic lung or skin.
- Ingests RBC
- Pseudopod forming non-flagellated protozoan Since the parasite’s habitat is the caecum area, there will
parasite be chances where during the burrowing of the
- Most invasive of the Entamoeba parasites trophozoites, it would affect the liver area since it is
- The only member of the family to cause COLITIS closest to the region. The patient will then have the extra-
and LIVER ABSCESS. intestinal amoebiasis.
- Habitat: Caecum and Sigmoidorectal region
Clinical Pictures
(Large Intestine)
- Infective stage: Quadrinucleate cyst 2 forms: Asymptomatic and Symptomatic
- Mode of reproduction: Binary Fission
- Mode of Infection: - Asymptomatic – are cyst carriers only. They are
Eating raw vegetables non-infective to the parasites. (More than 75%
Drinking water of our asymptomatic cases are healthy cyst
Flies and food handlers (cyst passer) passers)
Faeco oral (autoinfection) - Symptomatic
Acute Intestinal Amoebiasis – (gradual
Morphology of Trophozoite onset), fever (low grade), diarrhea,
dysentery, abdominal pain, localized
- 10-60 X 15-30u average (20-25 u)
abdominal tenderness, tenesmus &
- Cytoplasm is clearly differentiated into:
strain, painful spasm of anal sphincter
ECTOPLASM: is clear with well-
Chronic Intestinal Amoebiasis -
developed pseudopodia.
Recurrent attacks of dysentery with
ENDOPLASM: dense & fine granular
intervening periods of constipation,
enclosing:
abdominal distension & Flatulence,
- NUCLEUS: spherical containing centrally located
weight loss and cachexia.
karyosome & peripheral evenly distributed small
Extra Intestinal Amoebiasis - Amoebic
chromatin dots.
hepatitis or amoebic abscess, lung
- FOOD VACUOLES: contain leukocytes/RBC
abscess, brain abscess or skin abscess.
Complications Very effective in killing amoebas in the
wall of the intestine, in blood, and in
- Amoeboma (localized granulomatous mass liver abscesses.
misdiagnosed with carcinoma) - Luminal Amoebicide
- Hemorrhage Used if the infection is mild
- Perforation of Ulcer (secondary peritonitis - rare
Diluxanide furoate
but fatal)
- Stricture of colon
- Asymptomatic patients: are given luminal
- Appendicitis
amoebicide as Diluxanide furoate.
Diagnosis (Intestinal Amoebiasis) - Symptomatic patients: are given tissue
amoebicide as Metronidazole followed by
- Clinically presents with Dysentery luminal amoebicide as Diluxanide furoate.
Painful frequent evacuation of small - Percutaneous drainage of liver abscess is
quantities of stool containing mucus indicated for patients who do not respond to
tinged with blood. metronidazole.
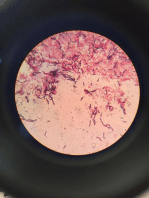
- Laboratory Preparation: Direct Stool Examination
Wet Preparation Epidemiology
Iodine Stained - Cyst passers are the main source of infection.
Permanent stain with iron - Cysts remain viable in faeces for few days, in
haematoxylin or trichrome. water for longer periods.
Stain used for the - Cysts are killed by dryness, heat (over 55ºC) and
visualization of E. histolytica by chlorine.
Trophozoites are found in diarrhoeic
stool Control
Cysts are found in formed stool.
- Treatment of patients.
- Concentration Techniques for cysts
- Examination and treatment of food handlers.
- Environmental sanitation.
Typical Amoebic Dysentery Stool Typical Bacillary Dysentery Stool - Personal prophylaxis.
Bulky Scanty - Human faeces should not be used as fertilizers.
Acidic Alkaline
Scanty Exudate Massive Exudate
Pus Cells + Pus +++ CHECH FOR UNDERSTANDING!
Blood + Blood + Multiple choices
Presence of Charcot-Leyden Absence of Charcot-Leyden
Crystals Crystals 1. Entamoeba histolytica trophozoites are found in:
Presence of Amoebae Absence of Amoebae a) Duodenum of infected human.
Trophozoites Trophozoites b) Jejunum of infected human.
c) Caecum of infected human.
d) All of the above.
- Indirect Diagnosis
Serological tests in chronic
2. Infection with Entamoeba histolytica occurs through eating
amoebiasis.
green salad contaminated with:
Detection of copro-antigen using
a) Trophozoites of Entamoeba histolytica.
monoclonal antibodies.
b) Cysts of Entamoeba histolytica.
Copro-antigen is a specific
c) Both trophozoites and cysts of Entamoeba
antigen found in the stool.
histolytica.
- Molecular techniques
Polymerase Chain Reaction (PCR)
3. Pathogenicity of Entamoeba histolytica depends on:
- Radiological Examination using Barium Enema
a) Parasite virulence.
For the visualization of the Large
b) Host resistance.
Intestine
c) Condition of intestinal tract.
- Sigmoidoscopy
d) All of the above.
To visualize the ulcer, scrap, aspirate or
take biopsy to see the trophozoites.
4. Patients with chronic intestinal amoebiasis suffer from:
Diagnosis (Extra-intestinal Amoebiasis) a) Dysentery, tenesmus with painful spasm of anal
sphincter.
- Clinical: according to the organ affected. b) Recurrent attacks of dysentery alternating with
- Laboratory: constipation.
Examination of aspirate from lung or c) Fever, diarrhea and tenesmus.
liver abscesses for trophozoites. d) None of the above.
Color of liver abscess:
Anchovy sauce 5. The following findings in stool suggest amoebic not
Liver scanning bacillary dysentery infection:
Radiology of diaphragm level and a) Acidic pH and presence of Charcot Leyden
pulmonary lesions. Crystals.
Serology b) Alkaline pH and presence of Charcot Leyden
Leukocytosis due to 2ry bacterial Crystals.
infection. c) Massive exudate with presence of many pus
- Amebic liver abscess is the most common extra- cells.
intestinal form of amebiasis
True or False
Treatment
1. Cyst passers are the main source of Entamoeba histolytica
- Tissue Amoebicide infection.
Used if the infection is severe and 2. Trophozoites of Entamoeba histolytica produce ulcers with
already has luminal destruction. indurated margin in intestinal mucosa.
Metronidazole, Tinidazole. 3. Examination and treatment of food handlers is very
important to control Entamoeba histolytica infection.
4. Infection with Entamoeba histolytica is totally localized to Usually spherical
the gastrointestinal tract. mature cyst: 4-8 nuclei, sometimes 16
5. Both trophozoites and cysts of Entamoeba histolytica are Immature cyst: 2 or more nuclei
infective to man. Karyosome is large, may/may not be
compact and/or eccentric
BONUS QUESTION:
- Cytoplasm: coarsely granular chromatoidal
bodies: Splinter-shaped or broom-shaped with
rough, pointed end
Rounded quadrinucleate cysts (20μ) seen in stool of patients should
be reported:
Entamoeba gingivalis
a) Entamoeba histolytica cyst - a common inhabitant of the mouth of man
a) Entamoeba dispar cyst - lives on the surface of teeth and gums, in gum
b) Entamoeba histolytica / dispar cyst pockets and sometimes in the tonsillar crypts
c) Entamoeba coli cyst - Organisms are more common in persons with
pyorrhea (gum disease) but they are not the
cause of the condition
- Hosts: Humans, other primates, dogs and cats
Entamoeba dispar
- Prevalence is from 50 to 95%
- formerly designated as non-pathogenic E.
- Mode of transmission:
histolytica
Kissing
- 9x more prevalent than E. histolytica
Droplet spray
- Morphologically identical with E. histolytica
Sharing of utensils
- their DNA and ribosomal RNA are different
- No cyst stage
- Diagnosis: negative serologic tests
Trophozoites have no ingested RBCs Morphology of Trophozoites
Entamoeba hartmanni - 10-20μm
- Morphologically indistinguishable from E. - Moves quickly
histolytica/E. dispar - Non pathogenic
- Has numerous blunt pseudopodia
Morphology of Trophozoite - Has numerous food vacuoles that contain
cellular debris and bacteria
- similar to E. histolytica except that it is much - has ingested leukocytes
smaller (5-12 μm)
- ingest bacteria but does not ingest RBCs
Endolimax nana
- 1 nucleus w/ small and compact, central
- Second most common endo commensal of
karyosome
humans
- more sluggish, non-progressive motility
- worldwide distribution 30%
Morphology of Cysts - Lives in the large intestine mainly near the
cecum
- 5-10μm, spherical in shape - feed on bacteria
- Mature: 4 nucleus with a coarse cytoplasm - non pathogenic
- immature cysts - Usually have chromatoidal bars - Outstanding feature:
- (short with tapered ends, or thin and bar-like) larger karyosome than those of the
genus Entamoeba
Entamoeba coli absent peripheral chromatin
- most common endo-commensal of humans
- has a worldwide distribution Morphology of Trophozoites
- Feeds on bacteria and any other cells available to
- small size of 6 to 15 μm
it
- Cytoplasm is granular and vacuolated
- does not invade tissues
- nucleus exhibits a large irregularly shaped
- common inhabitant of the lumen of the cecum
karyosome
and colon of man and other animals
- (may appear “blot-like”) with no peripheral
- Has the typical Entamoeba nucleus
chromatin
Morphology of Trophozoites - on the nuclear membrane
- Pseudopodia are blunt and hyaline
- Usually 15-25 μm in diameter (range 10-50 μm) - Sluggish, non-progressive motility
- Cytoplasm:
More vacuolated or granular Morphology of Cysts
endoplasm with bacteria and debris - Spherical or ovoid in shape
but no RBCs - Mature cyst:
Dirty-looking or honeycomb 5 – 14 μm in diameter
appearance
4 nuclei when mature
Narrower, less differentiated
A refractile cyst wall present
ectoplasm
Chromatoidal bodies are not usually
- Pseudopodia: Broader and Blunter
found
function more to ingest food
sluggish, non-directional motility
Iodameba butschlii
- Nucleus
- Not very common endocommensal in people
1 nucleus
- non-pathogenic
Thicker, irregular, coarsely granular
- Lives in the large intestine, predominantly in the
peripheral chromatin with a large
cecal areas
eccentric karyosome (not compact,
- Has a very high prevalence in pigs
may/may not be eccentric.
50% of pigs are infected with this
Morphology of Cysts ameba in France and Egypt
pigs are probably its normal host
- size: 10-35 μm
- Nucleus
Morphology of Trophozoites
Morphology of Trophozoites
- Usually 9-14 μm long (range 6-20 μm) - Average size 15 X 8 μ
- Single large vesicular nucleus with large - Pear shaped (broad anteriorly –tapering
chromatin- rich karyosome, surrounded by a posteriorly)
layer of achromatic granules globules and - Convex dorsally –flat ventrally with bi-lobed
anchored to nuclear membrane by achromatic anterior concavity (sucking discs) for attachment
fibrils (described as “basket nuclei”) - Motility by 4 pairs of flagellae (similar to a falling
- Cytoplasm appears granular, containing vacuoles leaf)
with ingested bacteria and debris - Two oval nuclei with central karyosome.
- Hyaline pseudopodia with sluggish progressive - Two axostyle traversing the body
motility - Two rod-shaped parabasal bodies across the
Morphology of Cysts axostyle
- 5-20 μm , oval-round in shape Morphology of Cyst
- uninucleated “basket nuclei” - Average size 12 X 7 μ
- Prominent characteristic: large glycogen vacuole - Oval with well-defined cyst wall
- which stains deeply w/ iodine - Four nuclei present usually at one pole.
- Includes: axostyle – parabasal bodies – remnants
Diantamoeba fragilis of flagella
- LIFE CYCLE - it does not form cysts and
trophozoites cannot survive passage through the Pathogenesis
small intestine. - Determined by:
- Humans probably get infected by this Strain Virulence
endocommensal when they ingest pinworm Host susceptibility
eggs! (Enterobius vermicularis) - Predisposing factors- determines the disease
severity.
Hypogammaglobulinaemia – Low
antibodies
Achlorhydria – No Hydrochloric acid
(ph 1-3)
- Pathogenicity is directly related to the
attachment of Trophozoite and surface area
affected.
- Mechanism of disease development
Mechanical Irritation
Enterotoxin
Blunting of brush border
Malabsorption syndrome
Pathogenesis and Clinical pictures
- Trophozoites feed on mucus = NO SYMPTOMS
- Trophozoites cause hyperaemia and
inflammation of duodenal wall (Duodenitis).
Symptoms include:
Epigastric pain
digestive disturbances
Steatorrhoea (fatty diarrhea- Stool is
light-colored and greasy)
Flatulence
- In patients with impaired immunity as:
Hypogammaglobulinaemia.
Diminished secretory IgA in small
intestine.
Diminished gastric acidity or
achlorohydria; severe symptoms will
occur such as:
Persistent diarrhea
Steatorrhoea,
INTESTINAL PROTOZOAS (FLAGELLATES) Malabsorption
Anemia.
Giardia lamblia Hypoproteinemia
Fat-soluble vitamin
- Causes Giardiasis in man, especially children deficiency.
- Geographic distribution: Cosmopolitan Jaundice and biliary colic.
- Habitat: duodenum, upper part of small
intestine, bile ducts and gall bladder as Diagnosis
trophozoites attached to the mucosa. - Direct Fecal Smear (DFS)
- Definitive Host: Man - If negative stool samples is strongly suspected
- Reservoir Host: Animals (excretion is irregular), the test must me
- Infective Stage: Cyst repeated.
- No flagella on the cyst stage - String Test
- Mode of infection: - Serological tests: for copro antigen detection
Contaminated food or water
Flies and food handlers Treatment
(Heteroinfection) - Metronidazole or Tinidazole, recently
Faeco oral (Autoinfection) Albendazole
- 8 - 10 μ
INTESTINAL OPPURTUNISTIC PROTOZOAS - Geographic distribution: worldwide
- Takes the shape of oocyst containing sporozoites
(SPOROZOA) - Infective stage: Sporulated oocyst
- AUTOINFECTION DOES NOT OCCUR
- HABITAT: Microvilli of the small intestine
- Unsporulated oocyst is excreted in the stool of
- Complains of mostly infected humans is watery the patient.
diarrhea - Same life cycle with Cryptosporidium but instead
- THE ONLY PROTOZOA CAPABLE OF SEXUAL OR of thick or thin walled oocyst, it produces
ASEXUAL REPRODUCTION unsporulated oocysts.
- Commonly associated from raspberries, basils.
OOCYST CYST - Oocyst sporulation happens in the environment
CASING (THICK SHELL) WITH PART OF THE NATURAL LIFE CYCLE specifically in the soil.
SPOROCYSTS INSIDE - Mode of infection: Ingestion of sporulated
oocysts in contaminated food or drink.
Cryptosporidium parvum
- Causes cryptosporidiosis Isospora belli (Cytoisospora belli)
- 4-6μ - Causes isosporiasis
- Only sporozoa with no sporocyst inside oocyst, - 30 X 12 μ
only sporozoite - Geographic distribution: worldwide
- Geographic distribution: worldwide - Takes the shape of oocyst containing sporozoites
- Takes the shape of oocyst containing sporozoites - Infective stage: Sporulated oocyst
- Resistant to chlorine - Same process with Cyclospora cayetanensis
- Infective stage: Sporulated oocyst - Same life cycle with Cryptosporidium but instead
- Mode of infection: of thick or thin walled oocyst, it produces
Ingestion of thick-walled oocyst unsporulated and sporulated oocysts.
Contaminated food and water (hetero - AUTOINFECTION MAY OCCUR
infection) - Mode of infection: Ingestion of sporulated
Faeco oral route in already infected oocysts in contaminated food or drink.
patient (external autoinfection)
Diagnosis of Cyclospora and Isospora
Thin-walled oocysts in intestinal lumen
- Stool examination to detect unstained oocysts
of already infected patient cause
- Stained oocyst by Modified Ziehl Neelsen (MZN)
internal autoinfection.
Development in human body PATHOGENESIS OF INTESTINAL PROTOZOA (SPOROZOA)
- For sexual reproduction, zygote can either - Intestinal villi show:
become thick-walled or thin-walled oocyst. Inflammatory changes
Thick-walled oocyst – External Atrophy
autoinfection
Crypt hyperplasia
Infective to man
- In immunosuppressed patients:
Thin-walled oocyst – Internal
Dissemination of the parasite to:
autoinfection
Esophagus
- Sporozoite attack brush borders of the epithelial
gall bladder
cells.
respiratory tract
- LIFE CYCLE
urinary bladder
Oocyst
Sporocyst
CLINICAL PICTURE OF INTESTINAL PROTOZOA (SPOROZOA)
Trophozoite
Type I Meront - In immunocompetent subject
Merozoite Mild self-limited diarrhea for 2 weeks
If ASEXUAL REPRODUCTION, - In children
Merozoites can develop Abdominal discomfort
again into Trophozoites. Diarrhea
If SEXUAL REPRODUCTION, Anorexia
Merozoites can be fever
differentiated into male and nausea
female gametocytes. Both weight loss
gender then merges, - In immunocompromised patients
producing a zygote. Sever life-threatening diarrhea
- Thin wall oocyst is formed(endogenous Dehydration
autoinfection) Malabsorption
- Thick walled oocysts are excreted in stool
TREATMENT OF INTESTINAL PROTOZOA (SPOROZOA)
Diagnosis - For immunocompetent:
- Clinical Picture: diarrhea
Self-limited
- Stool analysis
- For immunocompromised:
Direct Fecal Smear (DFS)
Concentration method using Paromomycin (for Cryptosporidium)
Shaether’s sugar floatation technique. Trimethoprim + Sulphamethoxazole
Oocysts are seen by: (for Cyclospora and Isospora)
Staining stool smear with Fluid and Electrolyte replacement
modified Ziehl Neelsen stain.
Immunofluorescence assay. EPIDEMIOLOGY AND CONTROL
- Intestinal Biopsy – to detect meronts and - Cryptosporidiosis is a zoonotic disease
gamonts - Oocysts are highly resistant to chemicals
- Faeco-oral infection occurs (external
Cyclospora cayetanensis autoinfection)
- Proper washing of green vegetables
- Causes cyclosporiasis
- Pure water supply c. Disseminated Cut
Haemoflagellates (Blood flagellates) Leishmaniasis (L. aethiopica)
d. Chronic (Recidivan) Relapsing
General characteristics: Cut Leishmaniasis (L. tropica)
Present in blood and tissues B. New World Cutaneous leishmaniasis
Move by flagellum (mastigote) then invade their host (N.W.C.L.)
Transmitted to man through arthropod bites a. Relapsing skin lesion
Require vector (blood sucking insect) for transmission (Chiclero’s Ulcer) – (L.
Alternate cycles and acquire 2 interchangeable stages in mexicana)
host and vector
Multiply by simple binary fission - Mucocutaneous Leishmaniasis “ESPUNDIA”
a. L. braziliensis
T. gambiense T. rhodesiense - Visceral Leishmaniasis “Kala-azar”
a. L. donovani
T. brucei b. L. infantum
Trypanosoma c. L. chagasi
Flagellates Haemoflagellates T. cruzi
Leishmania
Sporozoa Blood Sporozoa Plasmodium spp.
(P. falciparum, P. ovale, P.vivax, P.
malariae)
GEOGRAPHICAL DISTRIBUTION
- Usually, disease Leishmania (Old World) is in the
Middle East and Africa. South America cases
Leishmania spp. possess the Leishmania species (New World)
- Disease caused by Leishmania spp. is - Leishmania attacks the Human Viscera (Soft
Leishminiasis which is divided into: organs of the body)
Cutaneous - Mode of infection: Through the bite of FEMALE
Mucocutaneous sandflies
Visceral Lesions (most severe) - Rarely, Leishmaniasis is spread from a pregnant
- Leishmania established everywhere in Forest, woman to her baby
desert, mountains, towns, countries
PATHOGENESIS AND CLINICAL PICTURE OF CUTANEOUS
- Leishmania spp. are strictly obligatory
LEISHMANIASIS
intracellular parasite of macrophages/monocyte
series (Histiocytes – Epitheloid cells – Kupfer - Causes BLACK FEVER
cells – R.E.Cs) - NODULE forms at the site of bite due to
- Multiply by binary fission within macrophages of: multiplication of Leishmania in skin macrophages
SKIN – RETICULOENDOTHELIAL SYSTEM & other and granulomatous reaction around them.
VISCERA - ULCER
- Acquire interchangeable stages: - Healing occurs leaving a DISFIGURING SCAR
Amastigotes (Diagnostic stage): in - THE PATIENT DEVELOPS SOLID IMMUNITY
Man- Dogs –Rodents. - Morphology of wound: somewhat like a volcano
Promastigotes (Infective stage): in with a raised edge and central crater
vector & culture
- Transmission of the disease is seasonal – mainly LESIHMANIA SPECIES CAUSING ULCER IN THE NEW WORLD
zoonotic. Exceptions are L. donovani in india & L.
SPECIES DISEASE LOCATION
tropica….. Whereas man is the only source of
L. peruviana Dry Ulcer (Uta) Peru, and
maintaining infection (Anthroponotic) Brazil
- Ca be transmitted through contaminated L. pifanoi Diffuse lesion and resembles Brazil
syringes lepromatous leprosy (does not
- Vector of transmission is SANDFLY under the heal or ulcerate)
genus of “Phlebotomus” (Old world) L. braziliensis Spread along lymphatics to Guyana, and
(Espundia) mucous membrane producing Brazil
erosion of nasal septum, palate,
DISEASES
and larynx
L. mexicana Chiclero’s ulcer or Bay sore Mexico, Belize,
- Cutaneous Leishmaniasis (Oriental Sore)
Single ulcer affects the ear Guatemala,
A. Old World Cutaneous Leishmaniasis causing destruction of the Panama,
(O.W.C.L.) cartilage Honduras, etc.
a. Single Dry Non-Exudative
Lesion (L. tropica)
b. Multiple Wet Exudative Trypanosoma
Lesion (L. major) -
You might also like
- Miller and Herlay Book Mcqs Complete-1 PDFDocument195 pagesMiller and Herlay Book Mcqs Complete-1 PDFAmeer hamza76% (82)
- Parasitology and Clinical MicrosDocument16 pagesParasitology and Clinical MicrosErvette May Niño MahinayNo ratings yet
- Special Stains in Histopathology KEM Hospital MumbaiDocument46 pagesSpecial Stains in Histopathology KEM Hospital Mumbaiimranandu1086% (7)
- Reviewer in MicrobiologyDocument15 pagesReviewer in MicrobiologyRonel ResurricionNo ratings yet
- PARASITOLOGY (Quizlet)Document9 pagesPARASITOLOGY (Quizlet)Allyssa AniNo ratings yet
- Para Lect Prelims (Reviewer) : Lumbricoides Is An Example of A/anDocument17 pagesPara Lect Prelims (Reviewer) : Lumbricoides Is An Example of A/anJ Pao Bayro - LacanilaoNo ratings yet
- Suggested ResponsesDocument3 pagesSuggested ResponsesVrutika PatelNo ratings yet
- Sas Hes032 15Document9 pagesSas Hes032 15Jacob GarcesNo ratings yet
- Unit 8Document6 pagesUnit 8Tresha MadroñalNo ratings yet
- Birao Sas 15 Microbiology and ParasitologyDocument8 pagesBirao Sas 15 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesNo ratings yet
- TOPNOTCH Parasitology-Supertable-by-Yns-Pereyra-Cocoy-Calderon-Troy-Soberano-UPDATED-NOVEMBER-2017Document25 pagesTOPNOTCH Parasitology-Supertable-by-Yns-Pereyra-Cocoy-Calderon-Troy-Soberano-UPDATED-NOVEMBER-2017Waiwit KritayakiranaNo ratings yet
- 1MicrobioTrans - EukaryotesDocument9 pages1MicrobioTrans - EukaryotesJeztin Faye Del RosarioNo ratings yet
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocument14 pages1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaNo ratings yet
- Infection and Immunity Exam 1: Study GuideDocument9 pagesInfection and Immunity Exam 1: Study GuideDavid Miguel LandryNo ratings yet
- PROTOZOA (Sarcodina) : ProtozoologyDocument7 pagesPROTOZOA (Sarcodina) : ProtozoologyReyven Niña DyNo ratings yet
- CHAPTER 5 ParasitologyyDocument35 pagesCHAPTER 5 ParasitologyyMerlpa May AlcardeNo ratings yet
- Mod 7 NotesDocument35 pagesMod 7 Notesadneeniqbal259No ratings yet
- Intestinal and Commensal AmoebaDocument9 pagesIntestinal and Commensal AmoebaFuture TrekingNo ratings yet
- Microbio Act 05 10 2022Document2 pagesMicrobio Act 05 10 2022Janna Niña ElementoNo ratings yet
- CHAPTER 5 ParasitologyDocument57 pagesCHAPTER 5 ParasitologyKreizel FajaNo ratings yet
- Disease Causing OrganismsDocument4 pagesDisease Causing OrganismsANKITA GAYENNo ratings yet
- CHAPTER 5 ParasitologyDocument29 pagesCHAPTER 5 ParasitologyMerlpa May AlcardeNo ratings yet
- Group 4 Pharma ReportingDocument79 pagesGroup 4 Pharma ReportingIver Bryant JapsonNo ratings yet
- BZ Lab 4.0Document7 pagesBZ Lab 4.0Alexa Jean D. HonrejasNo ratings yet
- Parasitology Lesson 2Document4 pagesParasitology Lesson 2John Henry G. Gabriel IVNo ratings yet
- Trematodes: Intestinal SpeciesDocument7 pagesTrematodes: Intestinal SpeciesMica BernardoNo ratings yet
- Para Lec TransesDocument5 pagesPara Lec Transeslewistulio004No ratings yet
- 2 Parasitology Parasitic AmoebasDocument8 pages2 Parasitology Parasitic AmoebasknkjnNo ratings yet
- Parasitology (Lect #3) TransDocument6 pagesParasitology (Lect #3) TransSherlyn Giban InditaNo ratings yet
- Balantidum Coli: EBON, SISON - 2017Document5 pagesBalantidum Coli: EBON, SISON - 2017Abcd ReyesNo ratings yet
- Amoeba Notes 2015Document6 pagesAmoeba Notes 2015Ivy FlorentinoNo ratings yet
- Entamoeba and Entamoeba HistolyticaDocument9 pagesEntamoeba and Entamoeba HistolyticaKei Ml100% (1)
- Parasitology Table ProtozoaDocument10 pagesParasitology Table ProtozoaMae Rose Charlene MendozaNo ratings yet
- Adobe Scan 02 Nov 2023Document23 pagesAdobe Scan 02 Nov 2023aashiquezainmuhammedNo ratings yet
- Jurnal Toksoplasma GondiiDocument6 pagesJurnal Toksoplasma GondiiFina Rachma DestafanyNo ratings yet
- CHAPTER 5 ParasitologyDocument35 pagesCHAPTER 5 ParasitologyMerlpa May AlcardeNo ratings yet
- Entamoeba HistolyticaDocument7 pagesEntamoeba HistolyticaAarthyshree ManikandanNo ratings yet
- 6.2 2021para ReviewlocalwactsDocument35 pages6.2 2021para ReviewlocalwactsHeyzel joy FabianNo ratings yet
- Para Lec Midterms MergedDocument77 pagesPara Lec Midterms MergedMVSNo ratings yet
- Balantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansDocument2 pagesBalantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansMichael Vincent P.No ratings yet
- Las 9 Pcol2 Antiprotozoal DrugsDocument64 pagesLas 9 Pcol2 Antiprotozoal Drugsjenet soleilNo ratings yet
- Week 15 16 Protozoa Other Systemic InfectionsDocument6 pagesWeek 15 16 Protozoa Other Systemic InfectionsJASMINE ROSE ESPINASNo ratings yet
- ProtozoaDocument25 pagesProtozoanupur.kmcNo ratings yet
- Module 6.4 ParasitesDocument6 pagesModule 6.4 ParasitesPNo ratings yet
- 2 & 3 Protozoa and MalariaDocument22 pages2 & 3 Protozoa and Malariaمصطفي خندقاويNo ratings yet
- Amoeba: Ms. Helga SyDocument7 pagesAmoeba: Ms. Helga Syanti romantic txtNo ratings yet
- Amoeba paraDocument9 pagesAmoeba paraHANNA CASANDRA GARCIANo ratings yet
- The Intestinal ProtozoaDocument15 pagesThe Intestinal ProtozoaKHURT MICHAEL ANGELO TIUNo ratings yet
- 5 Chemotherapy of Parasitic DiseaseDocument86 pages5 Chemotherapy of Parasitic DiseaseWovelyNo ratings yet
- Parasitology Table: ProtozoaDocument10 pagesParasitology Table: ProtozoaKate Alyssa CatonNo ratings yet
- Parasitology Ciliates FlagellatesDocument4 pagesParasitology Ciliates FlagellatesarvinkennethdelacruzNo ratings yet
- Entamoeba Histolytica PDFDocument5 pagesEntamoeba Histolytica PDFViand NugrohoNo ratings yet
- Parasitology 1Document18 pagesParasitology 1christine delgado100% (2)
- IntProt PDFDocument15 pagesIntProt PDFWasilla MahdaNo ratings yet
- Introduction To Medical ParasitologyDocument50 pagesIntroduction To Medical ParasitologyKAYISIRE EMERYNo ratings yet
- Parasitology ReviewerDocument17 pagesParasitology Reviewerlouie100% (1)
- Plasm OdiumDocument12 pagesPlasm OdiumtqurroNo ratings yet
- Microbiology - 20Document6 pagesMicrobiology - 20karmylle andradeNo ratings yet
- (PARA) 1.5 - Blood and Tissue FlagellatesDocument6 pages(PARA) 1.5 - Blood and Tissue FlagellatesGuia De GuzmanNo ratings yet
- Week 4 Medical and Public Health ParasitologyDocument36 pagesWeek 4 Medical and Public Health Parasitologylewistulio004No ratings yet
- Kingdoms Shortlisting PDFDocument28 pagesKingdoms Shortlisting PDFNoman KhanNo ratings yet
- In-Vitro Toxicity Assessment of Antimalarial Drugs On Cultured Embryonic Rat Neurons, Macrophage (RAW 264.7), and Kidney Cells (VERO - CCl-81)Document1 pageIn-Vitro Toxicity Assessment of Antimalarial Drugs On Cultured Embryonic Rat Neurons, Macrophage (RAW 264.7), and Kidney Cells (VERO - CCl-81)WUSA9 TVNo ratings yet
- XII Biology Chromosomes and DNA TestDocument3 pagesXII Biology Chromosomes and DNA TestSamina AftabNo ratings yet
- Experiment 6 (Lab Periods 5 and 6) Restriction Enzymes and Restriction FragmentsDocument4 pagesExperiment 6 (Lab Periods 5 and 6) Restriction Enzymes and Restriction FragmentsLloaana 12No ratings yet
- Human Anatomy and Physiology Laboratory Manual Fetal Pig Version Update 10Th Edition Marieb Test Bank Full Chapter PDFDocument33 pagesHuman Anatomy and Physiology Laboratory Manual Fetal Pig Version Update 10Th Edition Marieb Test Bank Full Chapter PDFAlexandraPerrymzyd100% (13)
- Second Thoughts About Viruses Vaccines and The HIV Part 2 Robert.O.YoungDocument5 pagesSecond Thoughts About Viruses Vaccines and The HIV Part 2 Robert.O.YoungDavidNo ratings yet
- Types of VaccinesDocument21 pagesTypes of VaccinesAtoillah IsvandiaryNo ratings yet
- Developmental Psychology Lecture 1 MidtermsDocument3 pagesDevelopmental Psychology Lecture 1 MidtermsAngelo SumaoyNo ratings yet
- Chromosomal MutationDocument3 pagesChromosomal MutationChristian jayr BalcitaNo ratings yet
- AkapulkoDocument4 pagesAkapulkoH Tecson PereyraNo ratings yet
- Genetics Questions - MCQDocument4 pagesGenetics Questions - MCQManisanthosh KumarNo ratings yet
- Coronavirus (COVID-19) Research Compilation (JPM)Document32 pagesCoronavirus (COVID-19) Research Compilation (JPM)lunar100% (1)
- ENDOCRINE SYSTEM - REVIEWERDocument9 pagesENDOCRINE SYSTEM - REVIEWERVanya YeleniaNo ratings yet
- Plant Pathogens Principles of Plant PathologyDocument376 pagesPlant Pathogens Principles of Plant PathologyChirag Gupta100% (1)
- Out PDFDocument12 pagesOut PDFMaria RenjaanNo ratings yet
- Jipmer 2015 Solved QPDocument67 pagesJipmer 2015 Solved QPS Balagopal Sivaprakasam67% (3)
- Floppy BabyDocument13 pagesFloppy BabyJorge JhgNo ratings yet
- Krok 2 2002-2003 PediatricsDocument19 pagesKrok 2 2002-2003 PediatricsAli Zeeshan100% (1)
- Chorus BroşürDocument2 pagesChorus BroşürBilgi KurumsalNo ratings yet
- Case Pres Drug StudyDocument3 pagesCase Pres Drug StudyMark Teofilo Dela PeñaNo ratings yet
- Sistem Saraf PeriferDocument5 pagesSistem Saraf PeriferFitri SukmawatiNo ratings yet
- Huda Munir McqsDocument21 pagesHuda Munir McqsAngelo P. VeluzNo ratings yet
- 1st Periodical Test Grade 9Document7 pages1st Periodical Test Grade 9Jay Ronnie PranadaNo ratings yet
- CollagenaseDocument3 pagesCollagenaseThivia RajNo ratings yet
- DP1 BioSL - Topic 1 - Revision WorksheetDocument19 pagesDP1 BioSL - Topic 1 - Revision WorksheetlesedimamareganeNo ratings yet
- BIO G10 Q3 W5 D1 RevDocument4 pagesBIO G10 Q3 W5 D1 RevGu Jun PyoNo ratings yet
- Agglutination Reaction JMHFHSDocument50 pagesAgglutination Reaction JMHFHSRajkishor YadavNo ratings yet
- Test Rate List 2017 NewDocument17 pagesTest Rate List 2017 NewParakram BhattNo ratings yet
- Crozet Et Al. - 2018 - Birth of A Photosynthetic Chassis A MoClo ToolkitDocument13 pagesCrozet Et Al. - 2018 - Birth of A Photosynthetic Chassis A MoClo ToolkitFélix de CarpentierNo ratings yet