Professional Documents
Culture Documents
PHND
PHND
Uploaded by
bagholderCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PHND
PHND
Uploaded by
bagholderCopyright:
Available Formats
Research
JAMA Surgery | Original Investigation
Association of Prehospital Needle Decompression With Mortality
Among Injured Patients Requiring Emergency Chest Decompression
Daniel Muchnok, NRP; Allison Vargo, BS; Andrew-Paul Deeb, MD, MSc; Francis X. Guyette, MD, MPH; Joshua B. Brown, MD, MSc
Invited Commentary
IMPORTANCE Prehospital needle decompression (PHND) is a rare but potentially life-saving Supplemental content
procedure. Prior studies on chest decompression in trauma patients have been small, limited
to single institutions or emergency medical services (EMS) agencies, and lacked appropriate
comparator groups, making the effectiveness of this intervention uncertain.
OBJECTIVE To determine the association of PHND with early mortality in patients requiring
emergent chest decompression.
DESIGN, SETTING, AND PARTICIPANTS This was a retrospective cohort study conducted from
January 1, 2000, to March 18, 2020, using the Pennsylvania Trauma Outcomes Study
database. Patients older than 15 years who were transported from the scene of injury were
included in the analysis. Data were analyzed between April 28, 2021, and September 18, 2021.
EXPOSURES Patients without PHND but undergoing tube thoracostomy within 15 minutes of
arrival at the trauma center were the comparison group that may have benefited from PHND.
MAIN OUTCOMES AND MEASURES Mixed-effect logistic regression was used to determine the
variability in PHND between patient and EMS agency factors, as well as the association
between risk-adjusted 24-hour mortality and PHND, accounting for clustering by center and
year. Propensity score matching, instrumental variable analysis using EMS agency-level PHND
proportion, and several sensitivity analyses were performed to address potential bias.
RESULTS A total of 8469 patients were included in this study; 1337 patients (11%) had PHND
(median [IQR] age, 37 [25-52] years; 1096 male patients [82.0%]), and 7132 patients (84.2%)
had emergent tube thoracostomy (median [IQR] age, 32 [23-48] years; 6083 male patients
[85.3%]). PHND rates were stable over the study period between 0.2% and 0.5%. Patient
factors accounted for 43% of the variation in PHND rates, whereas EMS agency accounted
for 57% of the variation. PHND was associated with a 25% decrease in odds of 24-hour
mortality (odds ratio [OR], 0.75; 95% CI, 0.61-0.94; P = .01). Similar results were found in
patients who survived their ED stay (OR, 0.68; 95% CI, 0.52-0.89; P < .01), excluding severe
traumatic brain injury (OR, 0.65; 95% CI, 0.45-0.95; P = .03), and restricted to patients with
severe chest injury (OR, 0.72; 95% CI, 0.55-0.93; P = .01). PHND was also associated with
lower odds of 24-hour mortality after propensity matching (OR, 0.79; 95% CI, 0.62-0.98;
P = .04) when restricting matches to the same EMS agency (OR, 0.74; 95% CI, 0.56-0.99;
P = .04) and in instrumental variable probit regression (coefficient, −0.60; 95% CI, –1.04 to
–0.16; P < .01).
CONCLUSIONS AND RELEVANCE In this cohort study, PHND was associated with lower 24-hour
mortality compared with emergent trauma center chest tube placement in trauma patients.
Although performed rarely, PHND can be a life-saving intervention and should be reinforced
in EMS education for appropriately selected trauma patients. Author Affiliations: Division of
General/Trauma Surgery, Department
of Surgery, University of Pittsburgh
Medical Center, Pittsburgh,
Pennsylvania (Muchnok, Vargo, Deeb,
Brown); Department of Emergency
Medicine, University of Pittsburgh
Medical Center, Pittsburgh,
Pennsylvania (Guyette).
Corresponding Author: Joshua B.
Brown, MD, MSc, Division of General/
Trauma Surgery, Department of
Surgery, University of Pittsburgh
Medical Center, PUH F1266.2, 200
JAMA Surg. doi:10.1001/jamasurg.2022.3552 Lothrop St, Pittsburgh, PA 15213
Published online August 17, 2022. (brownjb@upmc.edu).
(Reprinted) E1
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
Research Original Investigation Prehospital Needle Decompression and Mortality in Patients Requiring Chest Decompression
T
rauma is a leading cause of death in the US,1 with chest
trauma contributing to mortality in up to 60% of Key Points
cases.2 Prehospital needle decompression (PHND) is a
Question Is prehospital needle decompression (PHND)
life-saving intervention to temporarily treat tension pneu- associated with lower 24-hour mortality among trauma patients
mothorax by emergency medical services (EMS) clinicians. requiring emergent chest decompression?
Both Advanced Trauma Life Support and Prehospital
Findings In this cohort analysis of 8469 trauma patients, PHND was
Trauma Life Support courses advocate use of needle de-
associated with a statistically significant 25% decrease in the odds of
compression for the emergent management of tension 24-hour mortality when compared with tube thoracostomy
pneumothorax.3,4 placement within 15 minutes of arrival at the trauma center.
The effectiveness of PHND is debated, with concerns raised
Meaning PHND was associated with lower 24-hour mortality
about appropriate patient selection and procedural
among trauma patients requiring emergent chest decompression
technique.5-7 Prehospital needle decompression is rare; exist- and should be emphasized in appropriately selected patients.
ing literature on the procedure consists of small, descriptive
studies over short time periods.8,9 They typically include a
single EMS agency or destination facility, thereby limiting Treatment and Control Groups
generalizability.8-10 PHND is performed empirically based on Our treatment group was defined as patients undergoing PHND.
clinical findings in the field. Tension pneumothorax cannot be This was identified by International Classification of Diseases,
confirmed after PHND is performed, making retrospective re- Ninth Revision (ICD-9) and Tenth Revision (ICD-10) procedure
view challenging. Most prior work lacks a comparator group codes (eMethods in the Supplement) plus a location code in-
to evaluate outcomes between those who did or did not un- dication the prehospital setting.
dergo PHND. We defined our control group as patients not undergoing
This is important as several studies question the benefits PHND but treated with tube thoracostomy placement within
of prehospital procedures, some even suggesting harm, par- 15 minutes of arrival at the trauma center. As we cannot verify
ticularly in the urban penetrating population supporting a tension pneumothorax diagnosis in the field, we believe this
“scoop-and-run” approach.11,12 However, it remains unclear represents a group of patients who may have benefited from
whether these procedures were indicated in comparator groups PHND given the emergent need for tube thoracostomy after
and may simply be markers of more severe injury. arrival at the trauma center. Tube thoracostomy was simi-
These limitations underscore the need for robust evalua- larly identified using ICD-9 and ICD-10 procedure codes
tion of PHND and assessment of its potential effect on out- (eMethods in the Supplement), with the procedure time stamp
comes. Our objective was to determine the association of PHND and trauma center admission time stamp to calculate the place-
with early mortality among injured patients requiring emer- ment time frame.
gent chest decompression. We hypothesized that PHND would
be associated with a lower risk of 24-hour mortality com- Missing Data
pared with emergent tube thoracostomy placement at the To address missing data, multiple imputation was performed
trauma center. for prehospital and admission vital signs, including systolic
blood pressure (SBP), heart rate, respiratory rate (RR), and Glas-
gow Coma Scale (GCS), as well as emergency department (ED)
transfusion requirement. Missing data for patients ranged from
Methods 6.5% (555 of 8469) for ED transfusion requirement to 34.0%
Study Population (2876 of 8469) for prehospital SBP. Multiple imputation using
This study was approved by the institutional review board of iterative, fully conditional specification chained equations was
the University of Pittsburgh. Between January 1, 2000, and performed to add 5 imputed data sets.13 Outcome models were
March 18, 2020, we performed a retrospective cohort analy- performed using estimation techniques that combine model
sis of the Pennsylvania Trauma Outcome Study (PTOS) data- coefficients and SEs from each imputed data set while adjust-
base, a state-wide trauma registry from 44 trauma centers. Data ing for the variability between imputed data sets.14 A com-
submission is mandatory for trauma center accreditation in the plete case analysis demonstrated similar results, and thus, the
state of Pennsylvania. Patients were eligible for inclusion if they results of the imputed data set are presented.
were 16 years or older and transported from the scene. Pa-
tients were excluded if burn was the primary mechanism of Statistical Analysis
injury, or they were dead on arrival. Patient race and ethnic- We calculated the proportion of eligible trauma patients un-
ity data were not specifically gathered for this study owing to dergoing PHND on an annual basis over the study period. We
high rates of missingness in the PTOS data set and were not then evaluated the proportion of variation in PHND attribut-
planned as analysis variables. This study was determined to able to patient vs EMS agency factors using 2 mixed-effects lo-
be exempt from the need for informed consent by the Univer- gistic regression models. First, we constructed a model using
sity of Pittsburgh institutional review board, owing to the use PHND as the outcome and no covariates with a random effect
of deidentified patient data. The Strengthening the Report- for EMS agency. Next, we fit a similar model adjusting for pre-
ing of Observational Studies in Epidemiology (STROBE) hospital time, SBP, heart rate, RR, GCS, intubation, mecha-
reporting guidelines were followed. nism of injury, and EMS clinician level of care (advanced life
E2 JAMA Surgery Published online August 17, 2022 (Reprinted) jamasurgery.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
Prehospital Needle Decompression and Mortality in Patients Requiring Chest Decompression Original Investigation Research
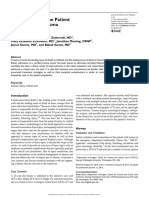
Figure 1. Annual Rate of Prehospital Needle Decompression Over the Study Period
50
45
Prehospital needle decompression, %
40
35
30
25
20
15
10
0
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 The solid line represents the overall
Year study rate, and shading represents
the 95% CI.
support [ALS] vs basic life support [BLS]) with a random ef- Sensitivity Analyses
fect for EMS agency. We then determined the relative de- To ensure the robustness of our results, we performed sev-
crease in the variance component of the EMS agency by in- eral sensitivity analyses. We excluded patients who died in
cluding patient-level covariates to estimate what proportion the ED to exclude patients presenting in extremis, periar-
of variation in PHND was associated with patient factors. rest, or cardiac arrest who may have received bilateral rapid
Our primary outcome was 24-hour mortality. For our pri- tube thoracostomy empirically and resulted in an increased
mary analysis, we performed mixed-effects logistic regres- mortality rate in the control group. We also excluded
sion to determine the association between 24-hour mortality patients with severe head injury (AIS ≥ 3) to exclude early
and PHND while adjusting for demographics, mechanism, in- death from traumatic brain injury in patients who would
jury severity score, prehospital time, prehospital and admis- not have benefited from PHND. We restricted patients to
sion vital signs, prehospital and ED blood transfusion, pre- those with severe chest injury (AIS ≥ 3) to exclude patients
hospital level of care (ALS vs BLS), transport mode (helicopter who may have undergone PHND or tube thoracostomy
vs ground ambulance), emergent surgery for hemorrhage con- empirically but did not actually need the procedure for a
trol, emergent craniotomy, and severe head, abdomen, or chest thoracic injury. Similarly, we restricted patients to those
injury defined as an abbreviated injury scale (AIS) score of 3 with documented pneumothorax to exclude patients who
or more in the respective body region. A 2-level nested ran- may not have benefited from PHND. We also evaluated the
dom effect was included to account for clustering of patients cohort including patients who were DOA to ensure that ex-
within trauma centers, as well as within year of admission given clusion did not bias our results with more deaths in the PHND
the long study period. group. We stratified our evaluation by transport mode to in-
Documented pneumothorax or hemothorax was cap- vestigate the association of differences in resources, training,
tured using ICD-9 and ICD-10 diagnosis codes. We assessed the and experience between EMS clinicians in ground and heli-
association of PHND with patient physiology as a proxy for po- copter transport.
tential benefit by evaluating the proportion of patients receiv- Finally, to evaluate the design thresholds that we
ing PHND with resolution of abnormal SBP, heart rate, and/or selected, we performed our primary analysis using 2-hour,
RR on trauma center arrival. Continuous data are presented 4-hour, and 6-hour mortality to corroborate the association of
as median (IQR). Continuous variables were compared using PHND with a spectrum of early mortality. We also compared
Wilcoxon rank sum tests, and categorical variables were com- patients undergoing PHND to those undergoing ED tube tho-
pared using χ2 tests. Adjusted odds ratios (aORs) with 95% CIs racostomy at more than 15 minutes from arrival at the trauma
are reported from regression models. A 2-sided P value ≤ .05 center to ensure appropriateness of the 15-minute threshold
was considered significant. Data analysis was conducted using to define emergent tube thoracostomy.
Stata, version 17MP (StataCorp). Data were analyzed between
April 28, 2021, and September 18, 2021.
Results
Causal Inference Approaches
To address potential bias for PHND, we used 2 causal infer- A total of 434 253 eligible trauma patients were identified. The
ence approaches. We performed propensity score matching rate of PHND among all eligible trauma patients was less than
using the entire study cohort and a separate analysis restrict- 1% annually and stable over the study period (Figure 1). In the
ing matches to patients treated by the same EMS agency. Sec- total eligible study population, patient factors accounted for
ond, we performed an instrumental variable analysis using the 43% of variation in PHND rates, whereas EMS agency ac-
EMS agency-level proportion of PHND. Details of these ap- counted for 57% of PHND variation. PHND rates were stable
proaches are in the eMethods in the Supplement. over the study period between 0.2% and 0.5%.
jamasurgery.com (Reprinted) JAMA Surgery Published online August 17, 2022 E3
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
Research Original Investigation Prehospital Needle Decompression and Mortality in Patients Requiring Chest Decompression
A total of 8469 patients were included in this study; 1337
Table 1. Characteristics of Treatment Groups
patients (11%) had PHND (median [IQR] age, 37 [25-52] years;
1096 male patients [82.0%]; 241 female patients [18.0%]), and Prehospital
Emergent tube needle
7132 patients (84.2%) had emergent tube thoracostomy (me- Characteristic thoracostomy decompression
dian [IQR] age, 32 [23-48] years; 6083 male patients [85.3%]; No. 7132 1337
1048 female patients [14.7%]). The majority of patients with Age, median (IQR), y 32 (23-48) 37 (25-52)
PHND (789 of 1337 [59.0%]) had pneumothorax diagnosed by Sex, No. (%)
ICD-9 or ICD-10 coding compared with half the patients re- Female 1048 (14.7) 241 (18.0)
Male 6083 (85.3) 1096 (82.0)
ceiving tube thoracostomy (3464 of 7132 [48.6%]), whereas
Mechanism, No. (%)
only 15.4% of patients who had PHND (206 of 1337) and 24.9%
Blunt 3272 (45.9) 956 (71.5)
of patients (1175 of 7132) who received tube thoracostomy were
Penetrating 3856 (54.1) 381 (28.5)
diagnosed with hemothorax only (Table 1). Ultimately, 90.9%
ISS, median (IQR) 25 (14-35) 26 (14-38)
of patients with PHND (1215 of 1337) received tube thoracos-
Prehospital
tomy. In the PHND and tube thoracostomy cohorts, patient fac-
Total time, median (IQR), min 33 (23-50) 46 (31-61)
tors accounted for only 12% of variation in PHND rates, whereas
Response time, median (IQR), min 7 (4-13) 9 (4-15)
EMS agency accounted for 88% of PHND variation. Scene time, median (IQR), min 13 (9-20) 17 (11-26)
Patients receiving PHND had resolution of hypotension in Transport time, median (IQR), min 13 (9-20) 15 (11-22)
37.9% (129 of 340), abnormal respiratory rate in 20.8% (89 of SBP, median (IQR), mm Hg 102 (75-128) 110 (80-137)
428), and abnormal heart rate in 16.8% (121 of 720). Overall, Hypotension, No. (%)a 2212 (30.9) 354 (32.6)
32.3% of patients (301 of 931) who received PHND had reso- Heart rate, median (IQR), 94 (66-117) 99 (72-120)
lution of at least 1 of the previously mentioned physiologic beats/min
Tachycardia, No. (%)b 3507 (44.0) 579 (46.1)
abnormalities baon arrival to the trauma center.
RR, median (IQR), 16 (6-23) 16 (4-24)
Regression analysis demonstrated that PHND was associ- respirations/min
ated with a 25% decrease in odds of 24-hour mortality after risk Abnormal RR, No. (%)c 2858 (38.0) 582 (52.8)
adjustment (odds ratio [OR], 0.75; 95% CI, 0.61-0.94; P = .01) GCS score, median (IQR) 8 (3-15) 3 (3-15)
(Table 2), with a risk-adjusted mortality of 28.1% vs 37.8% in pa- Intubation, No. (%) 1285 (18.0) 512 (38.3)
tients receiving tube thoracostomy. Similar results were found Admission
in patients who survived their ED stay (OR, 0.68; 95% CI, 0.52- SBP, median (IQR), mm Hg 90 (0-125) 110 (67-138)
0.89; P < .01), excluding severe traumatic brain injury (OR, 0.65; Heart rate, median (IQR), 88 (0-115) 94 (57-118)
beats/min
95% CI, 0.45-0.95; P = .03), and restricted to patients with se-
RR, median (IQR), 14 (0-22) 14 (0-22)
vere chest injury (OR, 0.72; 95% CI, 0.55-0.93; P = .01). For respirations/min
propensity score matching, 1236 patients who had PHND (92%) GCS score, median (IQR) 3 (3-15) 3 (3-14)
were matched to patients who received emergent tube thora- PRBC in ED, median (IQR) 0 (0-2) 0 (0-2)
costomy. The matching produced well-balanced groups Prehospital blood transfusion, 120 (1.7) 57 (4.3)
No. (%)
(Figure 2). In the matched cohort, PHND was associated with a Transport mode, No. (%)
21% decrease in the odds of 24-hour mortality (OR, 0.79; 95% Helicopter 1479 (26.1) 705 (52.8)
CI, 0.62-0.98; P = .04) (Table 2). When restricting matches to Ground 4181 (73.9) 629 (47.2)
within the same EMS agency, 968 patients who had PHND were Prehospital clinician level of care,
matched to control patients, with good balance of propensity No. (%)
BLS 151 (2.7) 4 (0.3)
score variables (OR, 0.74; 95% CI, 0.56-0.99; P = .04) (Figure 3).
ALS 5446 (97.3) 1325 (99.7)
Similarly, PHND was associated with a 26% reduction in the
Head AIS, median (IQR) 3 (2-4) 3 (2-5)
odds of 24-hour mortality (Table 2). Finally, instrumental vari-
Chest AIS, median (IQR) 3 (3-4) 3 (3-4)
able probit regression demonstrated that PHND was associ-
Abdomen AIS, median (IQR) 2 (2-4) 2 (1-4)
ated with lower 24-hour mortality (coefficient –0.60; 95% CI,
Pneumothorax diagnosis, No. (%) 3464 (48.6) 789 (59.0)
–1.04 to –0.16, P < .01). Results of the partial F test (F46, 2762
Hemothorax (only) diagnosis, 1175 (24.9) 206 (15.4)
(1−0.05) = 21.6; P < .01) and the Anderson-Rubin statistic con- No. (%)
fidence set (95% CI, –1.05 to –0.19 vs coefficient Wald 95% CI, 24-h Mortality, No. (%) 3261 (45.7) 471 (35.2)
–1.04 to –0.16) suggest that the instrument was not weak. In-hospital mortality, No. (%) 3679 (51.6) 583 (43.6)
In sensitivity analyses (Table 2), PHND was associated Abbreviations: AIS, abbreviated injury scale; ALS, advanced life support;
with lower odds of 24-hour mortality among patients that BLS, basic life support; ED, emergency department; GCS, Glasgow Coma Scale;
survived their ED stay, when excluding patients with severe ISS, injury severity score; PRBC, packed red blood cell; RR, respiratory rate;
SBP, systolic blood pressure.
head injury and when restricting to patients with severe a
Prehospital SBP less than 90 mm Hg.
chest injury. When including patients who were DOA, there b
Prehospital heart rate greater than 100 beats per minute.
were an additional 15 4 patients who had PHND and c
Prehospital RR less than 10 or greater than 29 respirations per minute.
102 patients who had tube thoracostomy, with PHND re-
maining associated with lower 24-hour mortality (Table 2).
The effect size of PHND on 24-hour mortality was greater transport (Table 2). PHND was also associated with lower
for helicopter transport but remained significant for ground 2-hour, 4-hour, and 6-hour mortality, whereas the 15-minute
E4 JAMA Surgery Published online August 17, 2022 (Reprinted) jamasurgery.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
Prehospital Needle Decompression and Mortality in Patients Requiring Chest Decompression Original Investigation Research
improvement after PHND and technical success rates of pleural
Table 2. Adjusted Odds Ratio (OR) of 24-Hour Mortality for Prehospital
Needle Decompression Compared With Tube Thoracostomy cavity decompression. Clinical improvement rates vary consid-
Within 15 Minutes of Arrival at the Trauma Center erably between studies, ranging from 5.7% to 53% after
PHND.7,10,16,18,19 Several studies reported that improvements in
Characteristic aOR (95%CI) P value
dyspnea and hypoxia were more common than improvement in
Primary analysis 0.75 (0.61-0.94) .01
hemodynamic parameters,7,10,18 although patients with hypo-
Propensity matched cohort 0.79 (0.62-0.98) .04
tension have a 3-fold higher odds of having improvement in
Propensity matched cohort within EMS agency 0.74 (0.56-0.99) .04
blood pressure than patients without hypotension before
Survived ED stay 0.68 (0.52-0.89) <.01
PHND.16 We found comparable rates of physiologic improve-
Excluded severe head injury 0.65 (0.45-0.95) .03
ment after PHND, with one-third of patients having at least 1
Severe chest injury 0.72 (0.55-0.93) .01
physiologic abnormality improving. Success of pleural decom-
Documented pneumothorax 0.68 (0.49-0.95) .02
pression is also highly variable, ranging from 5.9% to 100% with
Including patients DOA (n = 8725) 0.67 (0.45-0.98) .04 a bimodal distribution of mostly greater than 80% or less than
Helicopter transport 0.67 (0.52-0.86) <.01 25% success rates among studies.19 Complication rates of PHND
Ground transport 0.77 (0.60-0.98) .03 range from 2% to 13.7%, including iatrogenic pneumothorax or
Abbreviations: aOR, adjusted odds ratio; DOA, dead on arrival; ED, emergency hemothorax, subcutaneous hematoma, and dislodgement or
department; EMS, emergency medical services. kinking of the catheter, leading to hemodynamic compromise.7,17
Reported mortality rates after PHND range from 12% to 79% and
threshold for tube thoracostomy appears to be appropriate are universally lower in patients not presenting in traumatic
(eResults in the Supplement). arrest.9,19 Davis and colleagues18 found that an improvement in
systolic blood pressure after PHND was associated with im-
proved odds of survival, whereas Warner et al8 found 4 unex-
pected survivors who obtained return of spontaneous circula-
Discussion tion after PHND.
Results of this cohort study suggest that PHND is a rarely per- To facilitate outcome assessment for PHND, we chose our
formed procedure, with less than 1% of all trauma patients from comparison group to account for trauma patients with the per-
the study period receiving this intervention. When evaluating ceived need for emergent chest decompression who could have
rates of PHND in potentially eligible patients requiring emer- been candidates for PHND. We believe this comparison group
gent chest decompression, only 11% received decompression. represented patients who may have benefited from PHND and
After assessing variation in rates of PHND, we found that the ma- allowed us to assess the association of the PHND interven-
jority of variation was attributable to EMS agency factors. This tion with outcomes among trauma patients who required emer-
trend was more pronounced among patients requiring emer- gent chest decompression.
gent chest decompression. Overall, PHND was associated with Our data suggest that PHND was an effective procedure;
a 25% decrease in odds of mortality at 24 hours compared with however, only 11% of potentially eligible patients received this
emergent tube thoracostomy placement within 15 minutes of intervention. Although many factors may influence this and in-
patient arrival at the trauma center, and this finding persisted dications for decompression may have arisen late in transport
in several methodologic approaches and sensitivity analyses. or after arrival, EMS clinicians should have a high index of sus-
We also found a different association between PHND and mor- picion when considering tension pneumothorax in the setting
tality for patients transported by helicopter compared with of chest trauma and consider PHND. This is similar to a recom-
ground, which may be related to greater training and experi- mendation that was made by the 2018 Tactical Combat Casu-
ence for helicopter EMS clinicians, potentially translating to alty Care guidelines, which advocate for an aggressive ap-
differences in patient selection and/or procedural success; proach to suspecting and treating tension pneumothorax based
however, this requires further investigation. on mechanism of injury and respiratory distress.20 Patients who
Our rates of PHND were similar to those of prior work, rang- had PHND tended to have more severe presentations, but our
ing from 0.2% to 1.7% of trauma patients, depending on the analysis demonstrated that patients who had better prognostic
population studied.7,8,15,16 The presence of hypotension be- indicators still received emergent tube thoracostomy and likely
fore PHND varied widely from 7.9% to 86%7,17; however, most had tension pneumothorax. Prehospital procedures remain con-
studies report prehospital hypotension rates between 25% and troversial with several authors failing to find benefit.11,12 PHND
50%,8,10,18 more in line with the third of patients with prehos- is distinct from some prehospital procedures, such as intuba-
pital hypotension reported here. tion, which add time at the scene of the injury and can induce
One of the difficulties in studying PHND was the lack of a periprocedural harm from hypoxia and/or hypotension. PHND
comparison group, which hampered a robust assessment of the can be performed en route with lower risk of harm. Further, much
potential impact on outcomes. EMS clinicians empirically per- support of scoop-and-run approaches come from urban set-
form PHND for patients who present with signs and symptoms tings with penetrating trauma. Of note, more than 70% of the
of tension pneumothorax, but it is difficult to determine if these PHND cases in this study were performed in patients with blunt
patients actually have tension pneumothorax leading to abnor- mechanism of injury, which may affect the results seen here.
mal physiology. Thus, prior work is largely descriptive of pa- When considering the variation that we see in rates of
tients undergoing PHND. Many prior studies report on clinical PHND, there is area for improvement at the EMS agency level.
jamasurgery.com (Reprinted) JAMA Surgery Published online August 17, 2022 E5
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
Research Original Investigation Prehospital Needle Decompression and Mortality in Patients Requiring Chest Decompression
Figure 2. Absolute Standardized Differences Between Prehospital Needle Decompression Group
and Emergent Tube Thoracostomy Group Before and After Matching in Propensity Score Variables
Transport mode
Prehospital intubation
Mechanism
Prehospital SBP
Prehospital clinician level Before matching
Prehospital heart rate After matching
Prehospital time
Prehospital GCS score
Absolute standardized differences
Prehospital blood less than 0.1 (vertical dashed line) are
Prehospital RR considered to represent good
balance of covariates between
0 0.2 0.4 0.6 groups after matching. GCS indicates
Absolute standardized difference Glasgow Coma Scale; RR, respiratory
rate; SBP, systolic blood pressure.
Figure 3. Absolute Standardized Differences Between Prehospital Needle Decompression Group
and Emergent Tube Thoracostomy Group Before and After Matching in Propensity Score Variables
Within Emergency Medical Services Agency
Prehospital intubation
Mechanism
Prehospital SBP
Prehospital clinician level
Before matching
Prehospital heart rate
After matching
Prehospital time
Prehospital GCS score
Absolute standardized differences
Prehospital blood less than 0.1 (vertical dashed line) are
Prehospital RR considered to represent good
balance of covariates between
0 0.1 0.2 0.3 0.4 groups after matching. GCS indicates
Absolute standardized difference Glasgow Coma Scale; RR, respiratory
rate; SBP, systolic blood pressure.
This variation underscores the need for thorough education pneumothorax and distinction from hemothorax relies on ICD
and quality assurance and performance-improvement pro- coding and may undercode these diagnoses. There are also sev-
grams within EMS agencies along with timely follow-up on pa- eral assumptions that were made about the comparison group,
tient outcomes at the trauma center. Further, incorporating namely, the presence of tension pneumothorax. Some pa-
simulation or cadaver-based training for EMS clinicians may tients may have received tube thoracostomy as a proactive
facilitate successful placement more often than didactic train- measure at the trauma center before imaging, and we cannot
ing alone.21 Ultimately, a standardized approach to address- confirm that every patient had tension pneumothorax. Addi-
ing tension pneumothorax in the prehospital setting should tionally, these patients may have deteriorated just before or
be implemented to reduce variability and improve outcomes. on arrival to the trauma center and thus did not meet the in-
Recent advances in the type of catheter22-25 and anatomic po- dications for PHND by EMS clinicians at the trauma scene or
sition for PHND placement26-28 may improve success. The during transport. PTOS does not include data on indications
evolving role of prehospital point-of-care ultrasound may im- for PHND. We also did not have data on field hypoxia or dys-
prove patient selection for PHND.29 pnea. The timing of prehospital vital signs relative to PHND was
not available, thus, although only one-third of patients un-
Limitations dergoing PHND experienced hypotension, it is unclear whether
This study had several limitations. We cannot conclude cau- this SBP was taken before or after the procedure. Similarly, most
sation between PHND and 24-hour survival because of the patients who had PHND experienced an improvement in vital
retrospective observational nature of this study. We were un- signs by the time they arrived at the trauma center, but it re-
able to reliably determine laterality or if bilateral PHND was mains unclear if PHND was solely responsible. We also did not
performed based on ICD coding, as well as whether a subse- have qualitative data about respiratory effort or distress. Al-
quent chest tube was placed on the same side as the PHND. though we implemented various statistical measures to miti-
We were also unable to determine the anatomic site where gate for confounding and selection bias, the reduction in mor-
PHND was performed, and we do not have data on procedure- tality associated with PHND may be a proxy for more aggressive
specific complications. Similarly, identification of an actual prehospital trauma care overall. Our results matching pa-
E6 JAMA Surgery Published online August 17, 2022 (Reprinted) jamasurgery.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
Prehospital Needle Decompression and Mortality in Patients Requiring Chest Decompression Original Investigation Research
tients within EMS agency to remove agency-level variation trauma center chest tube placement at the scene of the acci-
engenders confidence in the results presented here. Despite dent in trauma patients. Although performed rarely, PHND
these limitations, our derivation of a comparison group of can be a life-saving intervention and should be reinforced in
patients requiring emergent chest decompression was a novel EMS education for appropriately selected trauma patients.
method to allow the assessment of outcomes and we believe EMS agencies should be proactive in conducting quality
adds to the literature surrounding PHND in trauma patients. assurance and performance improvement to reduce variation
in PHND practices. Future work should focus on the underly-
ing causes of variation among EMS agencies, appropriate
patient selection, and optimizing the technique of PHND.
Conclusions Implementing a standardized approach to considering PHND
Results of this cohort study suggest that PHND was associated can reduce variability in patient care and improve outcomes
with lower 24-hour mortality compared with emergent in trauma patients.
ARTICLE INFORMATION environment. Prehosp Emerg Care. 2008;12(2): 20. Butler FK Jr, Holcomb JB, Shackelford SA, et al.
Accepted for Publication: May 30, 2022. 162-168. doi:10.1080/10903120801907299 Management of suspected tension pneumothorax
9. Weichenthal L, Crane D, Rond L. Needle in tactical combat casualty care: TCCC guidelines
Published Online: August 17, 2022.
thoracostomy in the prehospital setting: change 17-02. J Spec Oper Med. 2018;18(2):19-35.
doi:10.1001/jamasurg.2022.3552
a retrospective observational study. Prehosp Emerg doi:10.55460/XB1Z-3BJU
Author Contributions: Dr Brown had full access to
Care. 2016;20(3):399-403. doi:10.3109/ 21. Grabo D, Inaba K, Hammer P, et al. Optimal
all of the data in the study and takes responsibility
10903127.2015.1102992 training for emergency needle thoracostomy
for the integrity of the data and the accuracy of the
10. Henry R, Ghafil C, Golden A, et al. Prehospital placement by prehospital personnel: didactic
data analysis.
needle decompression improves clinical outcomes teaching versus a cadaver-based training program.
Concept and design: Muchnok, Vargo, Deeb, Brown.
in helicopter evacuation patients with multisystem J Trauma Acute Care Surg. 2014;77(3)(suppl 2):
Acquisition, analysis, or interpretation of data:
trauma: a multicenter study. J Spec Oper Med. 2021; S109-S113. doi:10.1097/TA.0000000000000349
Muchnok, Guyette, Brown.
21(1):49-54. doi:10.55460/XDCK-IY9J 22. Aho JM, Thiels CA, El Khatib MM, et al. Needle
Drafting of the manuscript: Muchnok, Brown.
11. Seamon MJ, Fisher CA, Gaughan J, et al. thoracostomy: clinical effectiveness is improved
Critical revision of the manuscript for important
Prehospital procedures before emergency using a longer angiocatheter. J Trauma Acute Care
intellectual content: All authors.
department thoracotomy: “scoop and run” saves Surg. 2016;80(2):272-277. doi:10.1097/
Statistical analysis: Deeb, Brown.
lives. J Trauma. 2007;63(1):113-120. doi:10.1097/ TA.0000000000000889
Administrative, technical, or material support:
Vargo, Guyette, Brown. TA.0b013e31806842a1 23. Chang SJ, Ross SW, Kiefer DJ, et al. Evaluation
Supervision: Brown. 12. Taghavi S, Maher Z, Goldberg AJ, et al. An of 8.0-cm needle at the fourth anterior axillary line
Eastern Association for the Surgery of Trauma for needle chest decompression of tension
Conflict of Interest Disclosures: None reported.
multicenter trial examining prehospital procedures pneumothorax. J Trauma Acute Care Surg. 2014;76
Additional Information: These data were provided in penetrating trauma patients. J Trauma Acute Care (4):1029-1034. doi:10.1097/
by the Pennsylvania Trauma Systems Foundation, Surg. 2021;91(1):130-140. doi:10.1097/ TA.0000000000000158
Mechanicsburg, Pennsylvania. The Foundation TA.0000000000003151 24. Hecker M, Hegenscheid K, Völzke H, et al.
specifically disclaims responsibility for any analyses, 13. White IR, Royston P, Wood AM. Multiple Needle decompression of tension pneumothorax:
interpretations, or conclusions. imputation using chained equations: Issues and population-based epidemiologic approach to
REFERENCES guidance for practice. Stat Med. 2011;30(4):377-399. adequate needle length in healthy volunteers in
doi:10.1002/sim.4067 Northeast Germany. J Trauma Acute Care Surg.
1. Centers for Disease Control and Prevention.
14. Rubin DB. Multiple Imputation for Nonresponse 2016;80(1):119-124. doi:10.1097/
Underlying cause of death, 1999-2020. Accessed
in Surveys. John Wiley & Sons; 1987. doi:10.1002/ TA.0000000000000878
November 23, 2021. https://wonder.cdc.gov/ucd-
icd10.html 9780470316696 25. Zengerink I, Brink PR, Laupland KB, Raber EL,
15. Kaserer A, Stein P, Simmen HP, Spahn DR, Zygun D, Kortbeek JB. Needle thoracostomy in the
2. ATLS Subcommittee; American College of
Neuhaus V. Failure rate of prehospital chest treatment of a tension pneumothorax in trauma
Surgeons’ committee on Trauma; International
decompression after severe thoracic trauma. Am J patients: what size needle? J Trauma. 2008;64(1):
ATLS working group. Advanced Trauma Life
Emerg Med. 2017;35(3):469-474. doi:10.1016/ 111-114. doi:10.1097/01.ta.0000239241.59283.03
Support (ATLS): the ninth edition. J Trauma Acute
Care Surg. 2013;74(5):1363-1366. doi:10.1097/ j.ajem.2016.11.057 26. Inaba K, Branco BC, Eckstein M, et al. Optimal
TA.0b013e31828b82f5 16. Newton G, Reay G, Laing CM, King-Shier K. positioning for emergent needle thoracostomy:
Clinical characteristics of patients undergoing a cadaver-based study. J Trauma. 2011;71(5):1099-
3. McSwain NE Jr, Salomone J, Pons P, et al, eds.
needle thoracostomy in a Canadian helicopter 1103. doi:10.1097/TA.0b013e31822d9618
PHTLS:Prehospital Trauma Life Support. 7th ed.
Mosby/Jems; 2011. emergency medical service. Prehosp Emerg Care. 27. Inaba K, Karamanos E, Skiada D, et al. Cadaveric
2022;26(3):400-405. doi:10.1080/ comparison of the optimal site for needle
4. The Committee on Trauma. Advanced Trauma Life
10903127.2021.1912226 decompression of tension pneumothorax by
Support. 10th ed. American College of Surgeons; 2018.
17. Axtman BC, Stewart KE, Robbins JM, et al. prehospital care providers. J Trauma Acute Care Surg.
5. Bulger EM, Nathens AB, Rivara FP, MacKenzie E,
Prehospital needle thoracostomy: what are the 2015;79(6):1044-1048. doi:10.1097/
Sabath DR, Jurkovich GJ. National variability in
indications and is a post-trauma center arrival chest TA.0000000000000849
out-of-hospital treatment after traumatic injury.
tube required? Am J Surg. 2019;218(6):1138-1142. 28. Laan DV, Vu TDN, Thiels CA, et al. Chest wall
Ann Emerg Med. 2007;49(3):293-301. doi:10.1016/
doi:10.1016/j.amjsurg.2019.09.020 thickness and decompression failure: a systematic
j.annemergmed.2006.06.038
18. Davis DP, Pettit K, Rom CD, et al. The safety and review and meta-analysis comparing anatomic
6. Riwoe D, Poncia HDM. Subclavian artery
efficacy of prehospital needle and tube locations in needle thoracostomy. Injury. 2016;47
laceration: a serious complication of needle
thoracostomy by aeromedical personnel. Prehosp (4):797-804. doi:10.1016/j.injury.2015.11.045
decompression. Emerg Med Australas. 2011;23(5):
Emerg Care. 2005;9(2):191-197. doi:10.1080/ 29. El Zahran T, El Sayed MJ. Prehospital
651-653. doi:10.1111/j.1742-6723.2011.01466.x
10903120590924500 ultrasound in trauma: a review of current and
7. Eckstein M, Suyehara D. Needle thoracostomy in
19. Sharrock MK, Shannon B, Garcia Gonzalez C, potential future clinical applications. J Emerg
the prehospital setting. Prehosp Emerg Care. 1998;
et al. Prehospital paramedic pleural decompression: Trauma Shock. 2018;11(1):4-9. doi:10.4103/
2(2):132-135. doi:10.1080/10903129808958857
a systematic review. Injury. 2021;52(10):2778-2786. JETS.JETS_117_17
8. Warner KJ, Copass MK, Bulger EM. Paramedic
doi:10.1016/j.injury.2021.08.008
use of needle thoracostomy in the prehospital
jamasurgery.com (Reprinted) JAMA Surgery Published online August 17, 2022 E7
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a New York University User on 08/26/2022
You might also like
- Validating The Brain Injury GuidelinesDocument9 pagesValidating The Brain Injury GuidelinesMarcus CezilloNo ratings yet
- Rhetorical Analysis EssayDocument5 pagesRhetorical Analysis Essayapi-320095543No ratings yet
- Emergency Medical Services Intervals and Survival in Trauma Assessment of The Golden Hour in A North American Prospective CohortDocument27 pagesEmergency Medical Services Intervals and Survival in Trauma Assessment of The Golden Hour in A North American Prospective Cohortnageur2017No ratings yet
- Jamainternal Anderson 2023 Oi 230029 168798202879016Document9 pagesJamainternal Anderson 2023 Oi 230029 168798202879016vqm99d4kyrNo ratings yet
- Jamainternal Anderson 2023 Oi 230029 1687982028.79016Document9 pagesJamainternal Anderson 2023 Oi 230029 1687982028.79016lakshminivas PingaliNo ratings yet
- Comparision of 2 Techniques of TCF Closure Analysis of Outcomes and Health Care UseDocument6 pagesComparision of 2 Techniques of TCF Closure Analysis of Outcomes and Health Care Usehai1No ratings yet
- Jamainternal Del Pozo Cruz 2022 Oi 220055 1667324433.60094Document10 pagesJamainternal Del Pozo Cruz 2022 Oi 220055 1667324433.60094nikolaiNo ratings yet
- Variation in Preoperative and Postoperative Physical Therapist Management of Patients Opting For Elective Abdominal SurgeryDocument13 pagesVariation in Preoperative and Postoperative Physical Therapist Management of Patients Opting For Elective Abdominal Surgeryjimelsanmartin447No ratings yet
- Dang 2021Document10 pagesDang 2021Nurul AidaNo ratings yet
- Profilaxia de TEV em NCDocument9 pagesProfilaxia de TEV em NCSarah BernardesNo ratings yet
- Jama Subramaniam 2019 PC 190001Document11 pagesJama Subramaniam 2019 PC 190001Oihane Manterola LasaNo ratings yet
- 1 s2.0 S1053077022009168 MainDocument8 pages1 s2.0 S1053077022009168 MainOttofianus Alvedo Hewick KalangiNo ratings yet
- IPHMILitRev V5.2Document5 pagesIPHMILitRev V5.2miguel angel camachoNo ratings yet
- 8 28 PDFDocument8 pages8 28 PDFfirmansyahddsNo ratings yet
- Articles: BackgroundDocument8 pagesArticles: BackgroundfirmansyahddsNo ratings yet
- A Metaanalysis of Treatment Outcomes of Early.32Document8 pagesA Metaanalysis of Treatment Outcomes of Early.32khalid123No ratings yet
- 1 s2.0 S1053077021008405 MainDocument13 pages1 s2.0 S1053077021008405 Maindiogofc123No ratings yet
- Grosse-Sundrup2012 Score PredictifDocument2 pagesGrosse-Sundrup2012 Score PredictifZinar PehlivanNo ratings yet
- Damage Control Management y Polytrauma PatientDocument324 pagesDamage Control Management y Polytrauma PatientMauri ParadedaNo ratings yet
- Golden HourDocument28 pagesGolden HourYves BurckelNo ratings yet
- Flaherty 2016Document6 pagesFlaherty 2016Diornald MogiNo ratings yet
- Prognostic Factors For Spinal Chordomas and Chondrosarcomas Treated With Postoperative Pencil-Beam Scanning Proton Therapy - A Large, Single-Institution ExperienceDocument10 pagesPrognostic Factors For Spinal Chordomas and Chondrosarcomas Treated With Postoperative Pencil-Beam Scanning Proton Therapy - A Large, Single-Institution ExperienceAnnisa RahmaNo ratings yet
- Optimal Timing of An Invasive Strategy in Patients With Non-ST-elevation Acute Coronary Syndrome - A Meta-Analysis of Randomised TrialsDocument10 pagesOptimal Timing of An Invasive Strategy in Patients With Non-ST-elevation Acute Coronary Syndrome - A Meta-Analysis of Randomised TrialsRoberto López MataNo ratings yet
- Invasive Versus Non-Invasive Management of Older Patients With non-ST Elevation Myocardial Infarction (SENIOR-NSTEMI) : A Cohort Study Based On Routine Clinical DataDocument12 pagesInvasive Versus Non-Invasive Management of Older Patients With non-ST Elevation Myocardial Infarction (SENIOR-NSTEMI) : A Cohort Study Based On Routine Clinical DatasavitageraNo ratings yet
- 2012 Postarrest ResuscitationDocument12 pages2012 Postarrest ResuscitationAlma EscobarNo ratings yet
- The 10 Year Prognosis and Prevalence Of.13Document8 pagesThe 10 Year Prognosis and Prevalence Of.13Suryati HusinNo ratings yet
- Wang JiangDocument3 pagesWang Jiangmuhammad wajahatNo ratings yet
- Effect of Procalcitonin-Guided Antibiotic Treatment On Mortality in Acute Respiratory Infections: A Patient Level Meta-AnalysisDocument36 pagesEffect of Procalcitonin-Guided Antibiotic Treatment On Mortality in Acute Respiratory Infections: A Patient Level Meta-Analysisrista ria ariniNo ratings yet
- 2020 Terri Glioma PRODocument7 pages2020 Terri Glioma PRORimpa Basu AchariNo ratings yet
- Anesthesia Needs Large International Clinical Trials: Mcmaster University, Ontario, CanadaDocument4 pagesAnesthesia Needs Large International Clinical Trials: Mcmaster University, Ontario, Canadaserena7205No ratings yet
- Prognostic Value of Immunohistochemistry-Based Subtyping Before and After Neoadjuvant Chemotherapy in Patients With Triple-Negative Breast CancerDocument9 pagesPrognostic Value of Immunohistochemistry-Based Subtyping Before and After Neoadjuvant Chemotherapy in Patients With Triple-Negative Breast Cancerwilliam.cardales03No ratings yet
- Pro CalcDocument13 pagesPro CalcEdison QueirozNo ratings yet
- Nihms 462781Document21 pagesNihms 462781samuel anchondoNo ratings yet
- Haber 2017Document8 pagesHaber 2017Gisela M SilvaNo ratings yet
- Diagnosis and Management of Lumbar Spinal StenosisDocument12 pagesDiagnosis and Management of Lumbar Spinal StenosisMaíra CerqueiraNo ratings yet
- Journal Reading SarafDocument10 pagesJournal Reading SarafRifa RoazahNo ratings yet
- Epoc ExacerbadoDocument18 pagesEpoc ExacerbadoJuan David AlvarezNo ratings yet
- Surgical Vs Medical Treatments For Type 2 Diabetes Mellitus A Randomized Clinical TrialDocument9 pagesSurgical Vs Medical Treatments For Type 2 Diabetes Mellitus A Randomized Clinical TrialRofi MarhendraNo ratings yet
- Rasi Laine N 2020Document7 pagesRasi Laine N 2020core6406No ratings yet
- FCVM 10 1126888Document16 pagesFCVM 10 1126888Valeria ChongNo ratings yet
- Owen 2013Document9 pagesOwen 2013Yacine Tarik AizelNo ratings yet
- Critical Care For The Patient With Multiple TraumaDocument12 pagesCritical Care For The Patient With Multiple TraumaSyifa Aulia AzizNo ratings yet
- 0413 Massive Upper GI BleedingDocument12 pages0413 Massive Upper GI BleedingIsaura MendezNo ratings yet
- XlskdsladDocument9 pagesXlskdsladJoãoNo ratings yet
- Laparoscopy A Realistic Diagnostic and Theraputic Modality For Abdominal Trauma Our Experience of Laparoscopy in Abdominal Trauma A Prospective StudyDocument6 pagesLaparoscopy A Realistic Diagnostic and Theraputic Modality For Abdominal Trauma Our Experience of Laparoscopy in Abdominal Trauma A Prospective StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Print PDFDocument2 pagesPrint PDFpang_paangNo ratings yet
- Impact of Antiplatelet Therapy During Endovascular Therapy For Tandem OcclusionsDocument8 pagesImpact of Antiplatelet Therapy During Endovascular Therapy For Tandem Occlusionsrifki irsyadNo ratings yet
- Tracheotomy On Obese Patient PDFDocument5 pagesTracheotomy On Obese Patient PDFListya ParamitaNo ratings yet
- Balanced Crystalloids Versus Saline For Critically Ill Patients (BEST-Living)Document10 pagesBalanced Crystalloids Versus Saline For Critically Ill Patients (BEST-Living)vali.levo7No ratings yet
- Classifi Cation of Treatment-Related Mortality in Children WithDocument7 pagesClassifi Cation of Treatment-Related Mortality in Children WithIgnatia Rosalia KiranaNo ratings yet
- Comparision Between Provisional Diagnosis Made in Emergency Department VS Final Discharge Diagnosis at Ramkrishna Care Hospital, Raipur C.GDocument14 pagesComparision Between Provisional Diagnosis Made in Emergency Department VS Final Discharge Diagnosis at Ramkrishna Care Hospital, Raipur C.GIJAR JOURNALNo ratings yet
- Acute DizzinessDocument24 pagesAcute Dizzinesswiseman1405No ratings yet
- Schmidt2020 Article SynergisticEffectsOfForensicMeDocument12 pagesSchmidt2020 Article SynergisticEffectsOfForensicMeLanny Dwi ChandraNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundDita Putri DamayantiNo ratings yet
- Ooi 160066Document6 pagesOoi 160066bjro1986No ratings yet
- Wilcox2015 2 PDFDocument7 pagesWilcox2015 2 PDFAccel XtremeNo ratings yet
- Emergency Medical Services Intervals and Survival in Trauma: Assessment of The "Golden Hour" in A North American Prospective CohortDocument16 pagesEmergency Medical Services Intervals and Survival in Trauma: Assessment of The "Golden Hour" in A North American Prospective CohortrutnomleniNo ratings yet
- LatitudeDocument15 pagesLatitudeJulio MineraNo ratings yet
- Lewis 2016Document1 pageLewis 2016Adjhy Aji AchmadNo ratings yet
- Letter To The Editor Impact of Invasive Ventilation On Surviva - 2018 - RespiraDocument2 pagesLetter To The Editor Impact of Invasive Ventilation On Surviva - 2018 - RespiraArika EffiyanaNo ratings yet
- From Thoracic Surgery to Interventional Pulmonology: A Clinical GuideFrom EverandFrom Thoracic Surgery to Interventional Pulmonology: A Clinical GuideJ. Francis Turner, Jr.No ratings yet
- Nej MR A 1607714Document9 pagesNej MR A 1607714bagholderNo ratings yet
- Nej Mo A 2107051Document9 pagesNej Mo A 2107051bagholderNo ratings yet
- Nej MR A 1916801Document12 pagesNej MR A 1916801bagholderNo ratings yet
- Myocarditis CovidDocument7 pagesMyocarditis CovidbagholderNo ratings yet
- Jama Lipsky 2022 GM 220002 1645819318.31521Document2 pagesJama Lipsky 2022 GM 220002 1645819318.31521bagholderNo ratings yet
- Chinese Acupuncture and Moxibustion VideoDocument5 pagesChinese Acupuncture and Moxibustion VideoVirgil Anma100% (1)
- Language IIIDocument28 pagesLanguage IIIraquel395No ratings yet
- A Review of Free Range Duck Farming Systems in IndonesiaDocument105 pagesA Review of Free Range Duck Farming Systems in IndonesiaRofiqul AlaNo ratings yet
- Cycloplegic Effect of 0.5%tropicamide and 0.5%phenylephrine Mixed Eye Drops - Objective Assessment in Japanese Schoolchildren With MyopiaDocument5 pagesCycloplegic Effect of 0.5%tropicamide and 0.5%phenylephrine Mixed Eye Drops - Objective Assessment in Japanese Schoolchildren With Myopiaal_dhi_01No ratings yet
- A Risk Calculator For Bipolar Spectrum DisorderDocument2 pagesA Risk Calculator For Bipolar Spectrum DisorderDavidNo ratings yet
- Stepwise Provisional Versus Systematic Culotte For Stenting of True Coronary Bifurcation Lesions - Five-Year Follow-Up of The Multicentre Randomised EBC TWO Trial - EuroInterventionDocument9 pagesStepwise Provisional Versus Systematic Culotte For Stenting of True Coronary Bifurcation Lesions - Five-Year Follow-Up of The Multicentre Randomised EBC TWO Trial - EuroInterventionValentin CHIONCELNo ratings yet
- Seal of Good Local GovernanceDocument30 pagesSeal of Good Local GovernanceCatherine AmicanNo ratings yet
- 7 Day Intermittent Fasting Meal PlanDocument11 pages7 Day Intermittent Fasting Meal Plandietbykt.planshareNo ratings yet
- Safety Culture and Leadership FundamentalsDocument15 pagesSafety Culture and Leadership FundamentalsAurelio DutariNo ratings yet
- Avatar Identification and Problematic GamingDocument7 pagesAvatar Identification and Problematic GamingAndreaNo ratings yet
- Why You Should Quit Social Media 2Document6 pagesWhy You Should Quit Social Media 2api-650392913No ratings yet
- Chrome Galvanize - AerosolDocument1 pageChrome Galvanize - AerosolJodyNo ratings yet
- Gce Marking Scheme: Biology/Human Biology (New) AS/AdvancedDocument33 pagesGce Marking Scheme: Biology/Human Biology (New) AS/AdvancedRabea2222sweetandsouNo ratings yet
- 【加CE】出口 - 生化试剂 - N-乙酰-β-D-氨基葡萄糖苷酶试剂盒 NAG - 说明书 - 英文 - 1030316 - 2018.11.23Document3 pages【加CE】出口 - 生化试剂 - N-乙酰-β-D-氨基葡萄糖苷酶试剂盒 NAG - 说明书 - 英文 - 1030316 - 2018.11.23Abdul HameedNo ratings yet
- DianPutriAliyya (2000026031)Document5 pagesDianPutriAliyya (2000026031)annawageNo ratings yet
- Antimicrobial ResistanceDocument4 pagesAntimicrobial ResistanceDip Ayan MNo ratings yet
- Coursework For PsychiatristDocument7 pagesCoursework For Psychiatristafjwoamzdxwmct100% (2)
- Angelica Sanders ResumeDocument2 pagesAngelica Sanders Resumeapi-509815638No ratings yet
- Juvenile Justice Reform/Restoring Arkansas Families BillDocument12 pagesJuvenile Justice Reform/Restoring Arkansas Families BillMarine GlisovicNo ratings yet
- Mentorship Resume-2Document1 pageMentorship Resume-2api-550521804No ratings yet
- Updated Paternity and Maternity Leave W - ExerciseDocument20 pagesUpdated Paternity and Maternity Leave W - ExerciseNielle BautistaNo ratings yet
- Naveed Alam - Updated Curriculum Vitae 1Document4 pagesNaveed Alam - Updated Curriculum Vitae 1basharat121No ratings yet
- Crestone Updated Draft Operator AgreementDocument21 pagesCrestone Updated Draft Operator AgreementJulie BaxterNo ratings yet
- Acute Coronary Syndromes - M. Brizzio (Intech, 2012) WW PDFDocument224 pagesAcute Coronary Syndromes - M. Brizzio (Intech, 2012) WW PDFMihaela NițulescuNo ratings yet
- Nutrition of Blueberry 10-7-11 MO StrikDocument60 pagesNutrition of Blueberry 10-7-11 MO StrikJesús Miguel Maguiña EspinozaNo ratings yet
- Fasting For Fat LossDocument43 pagesFasting For Fat LossGordonReader8100% (2)
- Specification - ISOMALT LM - V007Document4 pagesSpecification - ISOMALT LM - V007Hakan ÇİÇEKNo ratings yet
- Iota AdnexDocument10 pagesIota Adnexlinh hoàngNo ratings yet
- First Aid BookletDocument37 pagesFirst Aid BookletLeNo ratings yet