Professional Documents
Culture Documents
NursingCarePlanGroup4 Revised
NursingCarePlanGroup4 Revised
Uploaded by
jae jaeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NursingCarePlanGroup4 Revised
NursingCarePlanGroup4 Revised
Uploaded by
jae jaeCopyright:
Available Formats
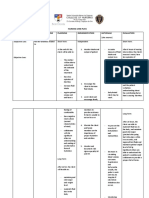
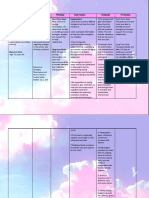
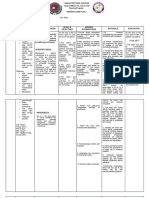
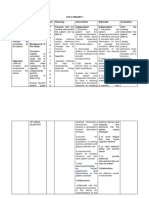
Case Scenario:
Mrs. RCS, a 78 year old female residing at Rafaela Subdivision, Makinabang, baliuag Bulacan has been admitted to your floor for rehabilitation from massive stroke. Mrs. RCS is
very slow in speech but is able to give appropriate answers. You received the patient from a local medical center. Before Mrs. RCS had this stroke, she was able to take complete
care of herself and lived by herself, according to her and her family.
Mrs. RCS now has complete paralysis on the right side of her body. Her dominant hand is her right hand. Mrs. RCS is unable to do the following for herself: feed herself, provide
hygiene, dress, use the bathroom, or simply write her name. She states she wants to get better but states she doesn't know if it will ever happen.
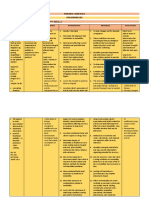
Assessment Nursing Diagnosis Nursing Objectives Nursing Interventions Rationale Evaluation
After 8 hours of
Subjective: Self-care deficit After 8 hours of Independent: 1. This encourage a tight and healthy
implementing nursing
related to loss of independent and relationship between nurse and
1. Establish rapport with the client. intervention, goals are
Client states she gross and fine collaborative nursing client. nurse will gain the trust of
the patient thus, allowing the client met as evidence by:
wants to get better motor skill on the intervention, the client 2. Discuss specific pathology and
but states she right side of the will: individual potentials. to communicate effectively with the
doesn't know if it body secondary to nurse.
will ever happen stroke as evidenced - verbalize knowledge 3. Educate the client and family - verbalized
members about the importance of 2. Establishing realistic expectations understanding about
by inability to feed about hemiplegia
Objective: self-management. and promotes an understanding of hemiplegia
herself, inability to - verbalize a more the current situation and needs.
do proper hygiene, rational overview on - verbalized a more
Right hemiplegia 4. Assess the level of independence
inability to dress, performing ADLs and 3. To improve self-management and rational overview on
or complete using functional independence
inability to use the future possibilities. foster transition from hospital to performing ADLs
paralysis on the measure (FIM).
bathroom, inability - demonstrate community. and future
right half of the to write, and independent feeding 5. Encourage the client to give out possibilities.
body. speech problem. 4. This aids in planning for meeting
by handling utensils maximum participation in planning - demonstrated
her treatment care plan. individual needs. It also helps in
Slow in speech (spoon), determining the capability and independent feeding
(broca’s aphasia) - demonstrate picking 6. Assist with ADLs, such as feeding, capacity of the client to perform by handling utensils
up of cup and glass grooming, bathing, and dressing. ADLs (spoon),
Conscious and Encourage independence in ADLs - demonstrated
with 8 fluid ounces of
oriented (Has the when possible. 5. Involvement provides the client picking up of cup
water,
capacity to give with an ongoing sense of control, and glass with 8
appropriate - demonstrate ingestion 7. Provide self-help devices: extensions improves coping skills, and can fluid ounces of
answers) of food safely and in with hooks for picking things up enhance cooperation with the
a socially acceptable water,
from the floor, toilet risers, long-
manner - demonstrated
Unable to - demonstrate proper handled brushes, drinking straw, and therapeutic regimen. ingestion of food
independently shower chairs.
hand washing 6. This is to maintain self-esteem and safely and in a
perform activities
of daily living such - demonstrate drying 8. Assist with movement and Range of promote recovery, the client needs socially acceptable
as: feed, provide herself using a towel Motion exercises using unaffected to do as much as possible for manner
hygiene, dress, use - demonstrate proper extremities to support and move the themselves. - demonstrated proper
the bathroom, and maneuver of putting weaker side. hand washing
7. Enable the client to manage for self,
write since the on necessary items of 9. Maintain a supportive, firm attitude. enhance independence and self- - demonstrated drying
dominant hand is clothing Allow the client sufficient time to esteem, reduce reliance on others herself using a towel
the right hand. - demonstrate proper carry out self-tasks to the best of for meeting own needs, and enable - demonstrated proper
maneuver on taking their abilities. the client to be more socially active. maneuver of putting
off necessary items of on necessary items
clothing 10. Present positive reinforcement for 8. Encourage improvements in range of clothing
- demonstrate proper all activities attempted; note partial of motion, strength and provides - demonstrated proper
achievements. neuroplasticity
maneuver on maneuver on taking
manipulation of 11. Provide adequate rest periods, 9. Clients need empathy and to know off necessary items
clothing for toileting ensure safety and comfort of the caregivers will be consistent in their of clothing
- demonstrate proper client. assistance - demonstrated proper
maneuver of sitting maneuver on
12. Instruct the client, family, or 10. This enhances the sense of self-
on and rising from manipulation of
caregiver in energy conservation worth, promotes independence, and
toilet or commode techniques. encourages the client to continue clothing for
endeavors. toileting
- demonstrated proper
11. To prevent further stress, fatigue maneuver of sitting
Collaborative: and injury. on and rising from
13. Refer the client to a physical and 12. This enhances performance while toilet or commode
occupational therapist. conserving limited energy and
preventing an increase in the level
of fatigue.
13. Rehabilitation helps to relearn skills
that are lost when part of the brain
is damaged.
Group 4 - BSN 1B
Belas, Juliet
Cruz, Darylle
Enciso, Leika Jade
Juliano, Jaelah Faith
Santos, Faith Stephanie
Orogan, Kim Saena
You might also like
- How To Get A Woman To Pay You Volume 2 (Guy Blaze) (Z-Library)Document54 pagesHow To Get A Woman To Pay You Volume 2 (Guy Blaze) (Z-Library)neverlosetime8952No ratings yet
- NCP LymphedemaDocument1 pageNCP Lymphedemayasira50% (2)
- Nursing Care PlanDocument2 pagesNursing Care Planrexale riaNo ratings yet
- Self Care Deficit NCP Alzheimer's DiseaseDocument4 pagesSelf Care Deficit NCP Alzheimer's DiseaseHanna Se75% (4)
- NCP Ineffective CopingDocument3 pagesNCP Ineffective CopingAqua RentoNo ratings yet
- ABAP FULL MaterialDocument128 pagesABAP FULL Materialanon_417818412100% (2)
- NCP Actual 1Document2 pagesNCP Actual 1Paolo Vittorio Perdigueros GonzalesNo ratings yet
- 203 Module 2 - NCP - GestaDocument3 pages203 Module 2 - NCP - Gestahaxa yzaNo ratings yet
- Cues Objectives Interventions Rationale EvaluationDocument4 pagesCues Objectives Interventions Rationale EvaluationEdgel QuidolesNo ratings yet
- Nursing Problem Explanation Goal Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Problem Explanation Goal Intervention Rationale Evaluation SubjectiveZed P. EstalillaNo ratings yet
- NCP Disturbed Body ImageDocument5 pagesNCP Disturbed Body ImageEricka Munsayac100% (1)
- NCP Final OutputDocument13 pagesNCP Final OutputBern NerquitNo ratings yet
- Needs/ Problems/Cues Nursing Diagnosis Scientific Basis Objectives of Care Nursing Actions RationaleDocument1 pageNeeds/ Problems/Cues Nursing Diagnosis Scientific Basis Objectives of Care Nursing Actions RationaleHarold PeranduzNo ratings yet
- Nursing Care Plan On Depression - Docx - 20231228 - 232453 - 0000Document3 pagesNursing Care Plan On Depression - Docx - 20231228 - 232453 - 0000Abdul SamadNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument1 pageAssessment Diagnosis Planning Intervention Rationale EvaluationALIANA KIMBERLY MALQUESTONo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationALIANA KIMBERLY MALQUESTONo ratings yet
- Assessment Diagnosis Planning Intervention EvaluationDocument5 pagesAssessment Diagnosis Planning Intervention EvaluationBianx SarmentaNo ratings yet
- Focus Action ResponseDocument3 pagesFocus Action ResponseJesselyn CampitNo ratings yet
- NCP 1Document2 pagesNCP 1Alyanna Alcazar CapateNo ratings yet
- NCP - Self Care Deficit Neuromuscular Impairment Secondary To CVADocument1 pageNCP - Self Care Deficit Neuromuscular Impairment Secondary To CVAHannah BatallonesNo ratings yet
- ANGEL-NCP - CaseloadDocument7 pagesANGEL-NCP - CaseloadNik Rose ElNo ratings yet
- NCPDocument2 pagesNCPsallylaserna100% (1)
- Midterm 3021Document9 pagesMidterm 3021api-283170120No ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanBelleNo ratings yet
- NCP001 IsolationDocument2 pagesNCP001 IsolationJoyh LasutaNo ratings yet
- Self-Care Deficit R/T Cerebrovascular Accident As Evidenced by Hemiplegia / Poor Personal HygieneDocument1 pageSelf-Care Deficit R/T Cerebrovascular Accident As Evidenced by Hemiplegia / Poor Personal HygieneScarlet PachecoNo ratings yet
- Yori Nicole Martine T. Cuyos: Care-Deficit-Nursing-Diagnosis-Care-PlanDocument4 pagesYori Nicole Martine T. Cuyos: Care-Deficit-Nursing-Diagnosis-Care-PlanYori Nicole Martine CuyosNo ratings yet
- Top 2 PriorityDocument6 pagesTop 2 PriorityRonel ResurricionNo ratings yet
- NCP TemplateDocument4 pagesNCP TemplateIRISH CACAYANNo ratings yet
- Advance in Ncm..Document3 pagesAdvance in Ncm..Ellaine SuapengcoNo ratings yet
- NCM 114 NCP ModuleDocument4 pagesNCM 114 NCP ModuleHelen GonzalesNo ratings yet
- NCP DementiaDocument6 pagesNCP Dementiamikee jane sabilloNo ratings yet
- Essentials of Psychiatric Mental Health Nursing Concepts of CareDocument1 pageEssentials of Psychiatric Mental Health Nursing Concepts of CareEno AlNo ratings yet
- Clinical Instructor: Mrs. Ramon A. Galicia, RN: Krystlle Lyre G. Cordero 4Bcn San Beda College Nursing Care PlanDocument4 pagesClinical Instructor: Mrs. Ramon A. Galicia, RN: Krystlle Lyre G. Cordero 4Bcn San Beda College Nursing Care Planstarcordero100% (2)
- Top 2 PriorityDocument3 pagesTop 2 PriorityRonel ResurricionNo ratings yet
- NCP Breast CancerDocument2 pagesNCP Breast CancerErika Mae MananganNo ratings yet
- LarideDocument3 pagesLaridelouie john abilaNo ratings yet
- Nursing Care Plan BalnkDocument2 pagesNursing Care Plan BalnkKateLayaogNo ratings yet
- NCP For SchizoDocument6 pagesNCP For SchizoGILIANNE MARIE JIMENEANo ratings yet
- TFN Finals ReviewerrDocument3 pagesTFN Finals ReviewerrEIRAM ROSE AMPARADONo ratings yet
- Cefi NCPDocument4 pagesCefi NCPIRISH CACAYANNo ratings yet
- Faye Glenn AbdellahDocument1 pageFaye Glenn Abdellahliza bNo ratings yet
- Date Cues Nsg. DX Scientific Basis Goal of Care NSG Intervention Rationale EvaluationDocument4 pagesDate Cues Nsg. DX Scientific Basis Goal of Care NSG Intervention Rationale EvaluationWenalyn Grace Abella LlavanNo ratings yet
- Professionalism in Physical Therapy: Core Values Bod P05-04-02-03 (Amended BodDocument6 pagesProfessionalism in Physical Therapy: Core Values Bod P05-04-02-03 (Amended BodJay PatelNo ratings yet
- Margaret Newman NCPDocument4 pagesMargaret Newman NCPRoshin TejeroNo ratings yet
- Client-Centered TheoryDocument19 pagesClient-Centered TheoryJoe-Liane AntonioNo ratings yet
- Nursing DiagnosisDocument11 pagesNursing Diagnosisseife slassieNo ratings yet
- NCP - PoliomyelitisDocument4 pagesNCP - PoliomyelitisCassey CuregNo ratings yet
- Risk For Injury Related To Extreme Hyperac Tivity/ph Ysical Agitatio NDocument2 pagesRisk For Injury Related To Extreme Hyperac Tivity/ph Ysical Agitatio NCindy BelmesNo ratings yet
- NCP Final WardDocument5 pagesNCP Final WardEloisa Joy MaquidatoNo ratings yet
- Nursing Care Plan For Depression PDFDocument3 pagesNursing Care Plan For Depression PDFtanmai nooluNo ratings yet
- Dewi Kurniawati 2014901057 - NERS REGULER (Deficit Self Care)Document3 pagesDewi Kurniawati 2014901057 - NERS REGULER (Deficit Self Care)Alri LestariNo ratings yet
- Marco Ray Vela NCPDocument2 pagesMarco Ray Vela NCPMarco VelaNo ratings yet
- Nueva Ecija University of Science and Technology: O V A ADocument16 pagesNueva Ecija University of Science and Technology: O V A AKym RonquilloNo ratings yet
- NCP-self Care DeficitDocument2 pagesNCP-self Care DeficitJoyh Lasuta74% (19)
- Nursing Care Plan - BeDocument6 pagesNursing Care Plan - BeMart UrsuNo ratings yet
- NURSING CARE PLAN (For Case Study)Document2 pagesNURSING CARE PLAN (For Case Study)Kathleen Martinez100% (1)
- Nursing Care Plan: Assessment Nursing Diagnosis Inference Planning Intervention Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Nursing Diagnosis Inference Planning Intervention Rationale EvaluationIrish LigayaNo ratings yet
- Ill-Discipline Is Destructive: A Hand Book on Social Policy, Social Care, Parenting, & Discipline:From EverandIll-Discipline Is Destructive: A Hand Book on Social Policy, Social Care, Parenting, & Discipline:No ratings yet
- Hyper Discord I ADocument86 pagesHyper Discord I ATimothy BowenNo ratings yet
- Ahsan's CVDocument2 pagesAhsan's CVAhsan DilshadNo ratings yet
- GNLD Carotenoid Complex BrochureDocument2 pagesGNLD Carotenoid Complex BrochureNishit KotakNo ratings yet
- Geometry CH 1 Test Review BDocument8 pagesGeometry CH 1 Test Review Balex montemayoresNo ratings yet
- Mental ManipulationDocument2 pagesMental ManipulationSunčica Nisam100% (2)
- Tertullian The African An Anthropological ReadingDocument236 pagesTertullian The African An Anthropological Readingz100% (3)
- Departmental Interpretation and Practice NotesDocument19 pagesDepartmental Interpretation and Practice NotesDifanny KooNo ratings yet
- Receita Sol Amigurumi - ENGDocument1 pageReceita Sol Amigurumi - ENGMaría de VeraNo ratings yet
- Amazing Race GuidelinesDocument10 pagesAmazing Race GuidelinesVince Nicole LomocsoNo ratings yet
- South Indian RecipesDocument7 pagesSouth Indian RecipesJagannath AcharyaNo ratings yet
- The Global City-Wps OfficeDocument10 pagesThe Global City-Wps OfficeJunel Dumandan LabradorNo ratings yet
- Wireless Communication Systems & NetworksDocument2 pagesWireless Communication Systems & NetworksNaresh KumarNo ratings yet
- Ketlie Augustin, A097 199 166 (BIA March 17, 2017)Document2 pagesKetlie Augustin, A097 199 166 (BIA March 17, 2017)Immigrant & Refugee Appellate Center, LLC0% (1)
- Somaliland Electoral Laws HandbookDocument0 pagesSomaliland Electoral Laws HandbookGaryaqaan Muuse YuusufNo ratings yet
- AaaDocument45 pagesAaaPriya NairNo ratings yet
- Negras in Brazil Chapter 1Document26 pagesNegras in Brazil Chapter 1Juliana GóesNo ratings yet
- Turn Your Lights Down Low: Bob MarleyDocument5 pagesTurn Your Lights Down Low: Bob MarleyIvan ChicaneNo ratings yet
- 16 Legacy B1 - P1 Quiz 8BDocument2 pages16 Legacy B1 - P1 Quiz 8BKremena Mihova100% (2)
- NI Tutorial 8473 enDocument2 pagesNI Tutorial 8473 enGabriel CostaNo ratings yet
- Acts Adopted Under The EC Treaty/Euratom Treaty Whose Publication Is ObligatoryDocument24 pagesActs Adopted Under The EC Treaty/Euratom Treaty Whose Publication Is ObligatoryivanmjwNo ratings yet
- The Grand IllusionDocument46 pagesThe Grand Illusionconnect2rahul4204100% (2)
- (Download PDF) Digital Media Steganography Principles Algorithms and Advances 1St Edition Mahmoud Hassaballah Editor Online Ebook All Chapter PDFDocument43 pages(Download PDF) Digital Media Steganography Principles Algorithms and Advances 1St Edition Mahmoud Hassaballah Editor Online Ebook All Chapter PDFdorothy.parkhurst152100% (15)
- Agreement Copy From Parties - Azzurra Pharmaconutrition PVT - Ltd...............Document4 pagesAgreement Copy From Parties - Azzurra Pharmaconutrition PVT - Ltd...............PUSHKAR PHARMANo ratings yet
- Thank-You For Downloading The SW Tool IQ-OQ-PQ Template!Document14 pagesThank-You For Downloading The SW Tool IQ-OQ-PQ Template!MichelleNo ratings yet
- Hyundai R290Lc 7 Hydraulic Excavator: Brazo Opción Boom/Stick Option (HEX) 1Document3 pagesHyundai R290Lc 7 Hydraulic Excavator: Brazo Opción Boom/Stick Option (HEX) 1Beatriz PinedoNo ratings yet
- Ozone Mag #59 - Sep 2007Document100 pagesOzone Mag #59 - Sep 2007Ozone MagazineNo ratings yet
- Pa CourseworkDocument5 pagesPa Courseworkafjwoamzdxwmct100% (2)
- Group 1 - OfW RemittancesDocument22 pagesGroup 1 - OfW RemittancesFLORENCE MAY SUMINDOLNo ratings yet