Professional Documents
Culture Documents
Vitamina C
Vitamina C
Uploaded by
VICKYOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vitamina C
Vitamina C
Uploaded by
VICKYCopyright:
Available Formats
ARTICLE
Vitamin C Status of US Adults Assessed as Part
of the National Health and Nutrition
Examination Survey Remained Unchanged
between 2003–2006 and 2017–2018
Carissa D. Powers,a Maya R. Sternberg,a Sweta B. Patel,b Christine M. Pfeiffer,a
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
Renee J. Storandt,c and Rosemary L. Schleicher a,*
Background: We compared serum vitamin C (VIC) status of the adult (≥20 y) US population in the National Health
and Nutrition Examination Survey (NHANES) 2017–2018 with combined data from 2003–2004 and 2005–2006.
Methods: VIC was measured using HPLC with electrochemical detection. Mean data were stratified by age, sex,
race/Hispanic origin, income, body mass index, dietary intake, supplement use, and smoking status. Prevalence
of VIC deficiency (<11.4 μmol/L) was calculated.
Results: In NHANES 2017–2018, the mean VIC was 8 μmol/L higher in people ≥60 y compared with those 20–59 y
of age, 10 μmol/L lower in men vs women, 8 μmol/L lower in low vs high income, 11 μmol/L lower in obese vs
healthy weight, and 15 μmol/L lower in smokers vs nonsmokers. Differences in mean VIC across race/Hispanic
origin groups ranged from 2 to 7 μmol/L. Mean VIC was 27 μmol/L higher with vitamin C-containing supplement
use and positively associated (Spearman ρ = 0.33; P < 0.0001) with increasing dietary intake. The associations
between mean VIC and the investigated covariates were generally consistent and the prevalence of deficiency
was not significantly different between survey periods (6.8% vs 7.0%; P = 0.83). However, a few subgroups had
double the risk. We found no significant survey differences in mean VIC (51.2 vs 54.0 μmol/L; P = 0.09).
Conclusions: Overall VIC status of the US adult population has remained stable since last assessed in the NHANES
2005–2006 survey. Vitamin C deficiency remained high for those with low dietary intake and who smoke.
INTRODUCTION (1). Consuming only 5 varied servings of fruits
and vegetables a day can provide >200 mg of vita
Vitamin C is an essential nutrient that comes min C (2), a level more than twice the current
from fruits, vegetables, fortified foods, and supple 90 mg Daily Value (3). As an indicator of serum vita
ments. The main sources of vitamin C in the US min C (VIC) status, stabilized serum or plasma con
diet are citrus, tomato products, and potatoes centrations are measured. VIC concentrations
a
Centers for Disease Control and Prevention, National Center for Environmental Health, Atlanta, GA; bOak Ridge Institute for Science and
Education, Oak Ridge, TN; cCenters for Disease Control and Prevention, National Center for Health Statistics, Hyattsville, MD.
*Address correspondence to this author at: National Center for Environmental Health, Division of Laboratory Sciences, Nutritional Biomarkers Branch,
Atlanta, GA 30341. E-mail rschleicher@cdc.gov.
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for
Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.
Received May 17, 2022; accepted August 19, 2022.
https://doi.org/10.1093/jalm/jfac093
Published by Oxford University Press on behalf of American Association for Clinical Chemistry 2023.
This work is written by (a) US Government employee(s) and is in the public domain in the US.
272 JALM | 272–284 | 08:02 | March 2023
Vitamin C Status of US Adults ARTICLE
IMPACT STATEMENT
The VIC status of the US adult population was reassessed using NHANES 2017–2018 data. The overall mean
and prevalence of deficiency were essentially unchanged compared with NHANES 2003–2006. Smoking sta
tus, obesity, low socioeconomic status, low dietary intake, or not using supplements were confirmed to still be
associated with low VIC. Additionally, younger people, non-Hispanic Black people, and men had low VIC com
pared to their counterparts.
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
<11.4 μmol/L define prevalence of VIC deficiency. among adults increased by approximately 9%
Within 1 month of little to no vitamin C intake, from 2003–2006 to 2017–2018 (8).
signs and symptoms of vitamin C deficiency can Although VIC is the preferred vitamin C status in
occur (2). These may include fatigue, loss of appe dicator, 24-h dietary recall is more commonly used
tite, easy bruising, dry skin, and bleeding gums. such as in the 2013 Philippine National Nutrition
Ascorbic acid (10 mg/day) will cure or prevent Survey and 2008–2012 Korean NHANES (9, 10).
scurvy, the severest form of vitamin C deficiency Among the few recent surveys that measured ser
(4). um or plasma vitamin C are the UK National Diet
There is only one US population survey that Survey (2008–2010) and the Canadian Health
uses biological specimens to study the health Measures Survey (2012–2013) (11, 12). VIC was
and nutritional status of the noninstitutionalized last measured in the US population during the
civilian population. The National Health and 2005–2006 NHANES. Because not all nutritional
Nutrition Examination Survey (NHANES) is a biomarkers can be monitored continuously
2-year nationally representative study using ques throughout NHANES, it is important to periodically
tionnaires combined with physical examinations assess and document whether changes in the US
and biochemical measurements. The CDC labora population occurred over time. The aim of this
tory measures VIC for NHANES. Additional study was to update the information on the VIC
NHANES data include demographic factors such status in the US population.
as age, sex, and race/Hispanic origin, and lifestyle
factors such as dietary intake and supplement
use. Based on NHANES data, vitamin C dietary in MATERIALS AND METHODS
take in US adults decreased by approximately
13% from 2003 to 2018 (5). From the literature, Study Design and Participants
overall dietary supplement use increased by ap Since 1999, NHANES has been a continuous sur
proximately 4% from 2007–2008 to 2017–2018 vey with public use data released in 2-year survey
(6). As has been shown previously, smoking and periods. The two-year weights released as part of
obesity were associated with lower mean VIC the public use data provide nationally representative
and increased deficiency (7). The percentage of estimates for the US civilian noninstitutionalized
adults who smoked declined by approximately population. Through 2006 the NHANES sampling
10% from 2003–2006 to 2017–2018 (unpublished domains included oversampling of Mexican–
observations). However, the prevalence of obesity American people, adolescents aged 12–19 years,
March 2023 | 08:02 | 272–284 | JALM 273
ARTICLE
older people aged ≥60 years, and a supplemental categories. Poverty income ratio (PIR), which is the
sample of pregnant women. Starting in 2007, ratio of family income to poverty guidelines specif
NHANES no longer oversampled adolescents and ic to family size, was defined as low (0–1.85), mid
pregnant women, oversampled the entire Hispanic dle (1.86–3.5), or high (>3.5). Body mass index
population (compared to only the Mexican– (BMI) was defined as healthy weight (18.5–
American population), non-Hispanic Black people, 24.99 kg/m2), overweight (25–29.99 kg/m2), or
low-income non-Hispanic White people and other obesity (≥30 kg/m2). Self-reported 24-hour total
people, and non-Hispanic White people and other dietary vitamin C intake recorded at the mobile
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
people aged ≥80 years. In 2011, NHANES began examination center (MEC) as reliable, was stratified
also oversampling Asian–American people. More de in quartiles as: 0–<20, 20–<50, 50–<110, and
tails on the NHANES sampling designs can be found ≥110 mg/day. Any vitamin C-containing supple
elsewhere (13–15). Overall response rates for the ment use in the previous 30 days was assessed.
examined sample in 2003–2004, 2005–2006, and Serum cotinine concentrations were used to deter
2017–2018 were 76%, 77%, and 49%. Complete mine smoking status: non-smokers (≤10 ng/mL)
interview and examination response rates for each and smokers (>10 ng/mL).
survey period are publicly available on the For all surveys, serum was obtained within
NHANES website (16). The current study compared 30 minutes of blood clotting. One part serum was
NHANES 2017–2018 with the combined data from mixed with 4 parts 6% metaphosphoric acid to
NHANES 2003–2004 and 2005–2006. There was stabilize ascorbic acid. The metaphosphoric acid-
no evidence of a statistically significant difference stabilized sera were shipped frozen. In our labora
of average serum vitamin C levels between tory, samples were stored at −70 °C until analysis.
NHANES 2003–2004 and 2005–2006, 53.9 µmol/L
(95% CI [51.2, 56.6]) compared to 54.0 µmol/L Laboratory Method
(95% CI [52.6, 55.1]), respectively (P = 0.92). A sensitive chromatographic method with electro
Therefore, the cycles were combined to increase chemical detection was used for quantitating VIC in
sample size and improve statistical precision (17). NHANES 2003–2004, 2005–2006, and 2017–2018
Of the 14 780 people 20 years and older who were (7, 18). For NHANES 2003–2006 VIC (oxidized and re
interviewed and examined, 13 824 (93%) had serum duced) was measured as described by McCoy et al.
vitamin C measurements. Participants were categor with the following equipment and/or setting changes
ized by age (overall ≥20 years, 20–39 years, 40– for NHANES 2017–2018 (19). A 4-μL injection was se
59 years, or ≥60 years), sex (men or women), race/ parated using a Waters Acquity UPLC HSS T3 column
Hispanic origin (Mexican American, non-Hispanic (1.8 µm particle size [100Å]; 150 mm × 2.1 mm [in
Asian, non-Hispanic Black, or non-Hispanic White). ner diameter]) at a flow rate of 0.4 mL/min. All
Participants self-reported race and Hispanic origin. chromatographic peaks eluted within 8 min and
Although non-Hispanic Asian people have been VIC was detected on a Waters 2465 electrochemical
oversampled since NHANES 2011–2012, NHANES detector set at +450 mV with a 2 mm glassy carbon
2017–2018 was the first-time representative data working electrode and in situ Ag/AgCl (ISAAC) refer
for non-Hispanic Asian people were available for ence electrode. For NHANES 2017–2018, the analyt
VIC. Individuals whose race/Hispanic origin was re ical measurement range was 7.3–146 μmol/L. Limit
corded as “other Hispanic” or “other race,” includ of detection was 1.7 μmol/L. Bench QC pool means
ing people who report multiple races, were too (3 pools measured in each analytical run in duplicate)
small to reliably report separately but included in ranged from 15.8–118 μmol/L with an overall CV of
the overall and all other demographic and lifestyle 4%. Blind QC pool means (6 different pools with
274 JALM | 272–284 | 08:02 | March 2023
Vitamin C Status of US Adults ARTICLE
one pool per 20 samples) ranged from 11.2– the historical comparisons, weighted arithmetic
98.6 μmol/L with an overall CV of 6%. See means were computed from combined NHANES
Supplemental Table 1 in the online Data 2003–2004 and 2005–2006 cycles to provide esti
Supplement for QC pool statistic details. Bench QC mates with greater statistical precision. Four-year
were evaluated using a SAS Institute Incorporated weights for 2003–2006 were calculated using the
(Cary, NC) QC program (20). Blind QC results were original 2-year MEC weights (original weight/2).
evaluated against 3 SD of the characterization P values to compare either the weighted means
means (20 runs per pool). Two levels of National or weighted prevalences across multiple categor
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
Institute of Standards and Technology ies were based on an overall Wald F-test. If the
(Gaithersburg, MD) NIST standard reference mater null hypothesis of equality among the means or
ial (SRM) 970 were obtained for NHANES surveys. prevalences across the categories was rejected
They were used during NHANES 2003–2006 (ap at 0.05 significance level, pairwise tests were per
proximately 18 runs) and in 2017–2018 (approxi formed applying the Bonferroni method to control
mately 22 runs) average differences from targets for multiple comparisons using a t-statistic with 15
ranged from −0.3% to 0.4%. The laboratory methods df. Estimated mean differences between 2017–
for measuring VIC are thoroughly documented on 2018 and 2003–2006 along with 95% confidence
the National Center for Health Statistics (NCHS) web intervals are presented to assess whether there
site (21–23). have been any changes. P values for the pairwise
differences between the 2 survey periods for
Statistical Analysis each category were assessed using a t-statistic
We performed statistical analyses using SAS with 45 df. Multiple linear regression modeling
(v.9.4) and SAS-callable SUDAAN (v.11.0.3, RTI, was used to explore correlates of VIC concentra
Research Triangle Park, NC), to account for the tions. The a priori modeling plan was to enter all
complex sample design. Variance estimation was preselected variables into a regression model
based on Taylor Series Linearization and the (25). The preselected variables were: age, sex,
MEC weights were used to account for unequal race/Hispanic origin, PIR, BMI, dietary vitamin C
probabilities of selection, nonresponse, and non intake, vitamin C-supplement use, and smoking
coverage. Degrees of freedom (df) were calculated status. A 0.05 significance level to stay was evalu
based on the total number of primary sampling ated against Satterthwaite adjusted F P values in
units minus the number of strata defined by the combination with whether the covariable was a
survey design. Weighted arithmetic means for potential confounder regardless of statistical sig
VIC concentrations and weighted prevalences of nificance. The final step was to investigate all pair
VIC deficiency are shown for selected variables, wise interactions between variables in the model.
for NHANES 2017–2018. Prevalence estimates In the interest of parsimony, the beta coefficients
were suppressed if they did not meet the statistic for significant interactions were not presented in
al reliability criteria (24). Spearman correlation was the final regression model. However, to demon
used to assess the association between VIC and strate that these interactions did not appreciably
selected variables (25). Further, bivariate associa change the pattern of the associations between
tions for each nutritional biomarker and categoric the variables and VIC, the conditional marginal
al variables were based on geometric means (or means from the final model with the interactions
arithmetic means where appropriate) and 95% included are presented for the statistically signifi
confidence intervals across the categories. For cant pairwise interactions.
March 2023 | 08:02 | 272–284 | JALM 275
ARTICLE
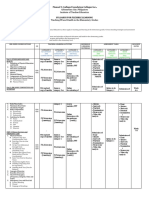
Table 1. For the US population 20 years and older, weighted prevalence (in percent) of vitamin C
deficiency (serum vitamin C <11.4 µmol/L) and weighted mean serum vitamin C concentrations,
National Health and Nutrition Examination Survey, 2017–2018.
Prevalence Mean
(95% CI)a Wald F (95% CI)a Wald F
Variables Variable categories n (%) P valueb (µmol/L) P valueb
Age Overall ≥20 4932 6.8 0.69 51.2 0.0005
(years) (5.0, 9.0) (48.3, 54.1)
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
20–39 1463 6.2 48.4
(4.1, 9.3) (45.3, 51.6)d
40–59 1563 7.0 49.4
(5.1, 9.5) (46.3, 52.5)d
≥60 1906 7.2 56.8
(5.1, 9.9) (53.0, 60.6)e
Sex Men 2377 7.7 0.10 46.1 <0.0001
(5.5, 10.6) (43.2, 48.9)d
Women 2555 5.9 56.0
(4.3, 8.1) (52.8, 59.3)e
Race/Hispanic origin Mexican–American 675 4.5 0.0313 49.7 0.0085
(2.6, 7.7)d,e (45.0, 54.4)d,e
Non-Hispanic Asian 693 3.0 54.6
(2.2, 4.1)e (51.6, 57.6)e
Non-Hispanic Black 1117 6.0 47.4
(3.5, 10.0)d,e (44.0, 50.8)d
Non-Hispanic White 1728 7.7 52.2
(5.5, 10.6)d (48.8, 55.6)d,e
PIR Low (0–1.85) 1893 9.8 0.002 46.3 0.0004
(6.9, 13.6)d (42.5, 50.1)d
Middle (1.86–3.5) 1095 6.7 52.1
(4.5, 10.0)d,e (47.9, 56.4)e
High (>3.5) 1304 4.6 54.2
(3.0, 6.8)e (50.6, 57.8)e
BMIc Healthy (18.5–24.99) 1173 7.6 0.0154 56.1 <0.0001
(kg/m2) (5.2, 11.1)d,e (51.7, 60.5)d
Overweight (25–29.99) 1563 4.4 55.9
(3.0, 6.4)d (53.4, 58.3)d
Obesity (≥30) 2049 7.7 45.4
(5.5, 10.5)e (42.3, 48.5)e
Dietary intake quartiles (0–<20) 1163 13.9 <0.0001 41.2 <0.0001
(mg/day) (10.5, 18.3)d (37.3, 45.0)d
(20–<50) 1139 7.4 45.5
(5.2, 10.4)e (41.9, 49.2)e
(50–<110) 1095 2.9 56.2
(1.9, 4.6)f (53.4, 59.0)f
≥110 1085 2.2 63.3
(1.1, 4.2)f (59.8, 66.7)g
(continued)
276 JALM | 272–284 | 08:02 | March 2023
Vitamin C Status of US Adults ARTICLE
Table 1. Continued
Prevalence Mean
(95% CI)a Wald F (95% CI)a Wald F
Variables Variable categories n (%) P valueb (µmol/L) P valueb
Vitamin C-containing supplement use Yes 1133 0.5 <0.0001 70.6 <0.0001
(0.2, 1.5)d (67.5, 73.7)d
No 3336 9.2 43.5
(6.9, 12.1)e (40.9, 46.2)e
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
Smoking status Nonsmokers 3751 4.4 0.0002 54.7 <0.0001
(3.2, 5.9)d (51.6, 57.7)d
Smokers 1162 14.6 39.9
(10.6, 19.8)e (36.8, 43.1)e
a
Compact letter display (d–g) is used to show statistically significant differences between pairwise comparisons after Bonferroni adjustment.
Categories sharing one or more letters were not significantly different. Pairwise comparisons were only assessed if the null hypothesis of
equality among the prevalences across the categories was rejected at the 0.05 significance level.
b
P value based on the Wald F-test, which tests whether at least one of the prevalences or means across the categories were significantly different.
c
Relative CI width for underweight was >130%. Estimate was suppressed (23).
RESULTS lowest risk, a difference of 11.8% (95% CI [8.4%,
15.2%]). Likewise, those whose intake was be
Prevalence in NHANES 2017–2018 tween 50–110 mg/day had a difference of 11.0%
The prevalence of VIC deficiency in 2017–2018 is (95% CI [7.3%, 14.7%]) compared to those with
shown in Table 1. We assessed absolute differ the lowest intake (<20 mg/day). Prevalence of VIC
ences between categories. There were no signifi deficiency was significantly lower in vitamin
cant differences in prevalence of VIC deficiency C-containing supplement users compared to
among age subgroups or sex. Among race/ nonusers, a difference of 9.0% (95% CI [6.0%,
Hispanic origin groups the only significant differ 11.9%]). Nonsmokers had significantly lower
ence in prevalence was between non-Hispanic prevalence of VIC deficiency compared to smo
White people and non-Hispanic Asian people kers, a difference of 10.2% (95% CI [6.2%, 14.3%]).
with non-Hispanic Asian people having lower
prevalence by 4.7% (95% CI [2.0%, 7.4%]). High in Mean Concentrations in NHANES 2017–2018
come was associated with significantly lower Mean VIC concentrations stratified by demo
prevalence of VIC deficiency compared to low in graphic or lifestyle factors for NHANES 2017–2018
come, a difference of 5.2% (95% CI [2.7%, 7.8%]). are shown in Table 1. Based on age, 60+ year-old
Although the healthy weight and obesity VIC defi adults had significantly higher mean VIC than other
ciency prevalences are similar (approximately age groups ranging 7.4–8.4 µmol/L. Women had
0.1% different), the only significant difference in significantly higher VIC than men by 10.0 µmol/L
BMI categories was between those with obesity (95% CI [7.7, 12.3]). Among race/Hispanic origin
compared to overweight adults, a difference of groups, the only significant difference was between
3.2% (95% CI [1.2%, 5.3%]). Low (<20 mg/day) vita non-Hispanic Black people and non-Hispanic Asian
min C dietary intake was associated with the people with non-Hispanic Asian people higher by
highest risk of VIC deficiency whereas high 7.2 µmol/L (95% CI [3.4, 11.0]). Mean VIC was
(≥110 mg/day) intake was associated with the 5.9–7.9 µmol/L higher in the middle and high PIR
March 2023 | 08:02 | 272–284 | JALM 277
ARTICLE
Table 2. Multiple linear regression resultsa for serum vitamin C concentrations in the US population 20
years and older, National Health and Nutrition Examination Survey, 2017–2018.
Beta coefficient
Variablesb Variable categories Reference category (95% CI) P valuec
Age Interceptd ≥60 50.4 <0.0001
(years) (45.2, 55.7)
20–39 −3.1 0.07
(−6.6, 0.4)
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
40–59 −5.3 0.0019
(−8.3, −2.3)
Sex Men Women −5.7 0.0017
(−8.9, −2.5)
Race/Hispanic origin Mexican–American Non-Hispanic White −0.8 0.52
(−3.3, 1.8)
Non-Hispanic Asian −1.6 0.28
(−4.6, 1.4)
Non-Hispanic Black −0.4 0.82
(−4.1, 3.3)
PIR Low (0–1.85) High (>3.5) −1.4 0.30
(−4.2, 1.4)
Middle (1.86–3.5) 0.2 0.91
(−4.0, 4.4)
BMI Healthy (18.5–24.99) Obesity (≥30) 8.3 0.0002
(kg/m2) (4.6, 12.0)
Overweight (25–29.99) 9.3 <0.0001
(6.6, 12.0)
Dietary intake (0–<20) ≥110 −17.5 <0.0001
quartiles (−21.2, −13.9)
(mg/day)
(20–<50) −14.7 <0.0001
(−18.4, −11.0)
(50–<110) −7.5 0.0001
(−10.5, −4.5)
Vitamin C-containing supplement use Yes No 19.2 <0.0001
(16.7, 21.6)
Smoking status Nonsmokers Smokers 8.6 <0.0001
(5.9, 11.3)
a 2
R = 29.4%.
b
Data were adjusted for the following variables: age, sex, race/Hispanic origin, PIR, BMI, dietary intake quartiles, vitamin C-containing supplement
use, and smoking status.
c
Student’s t-statistic with 15 df.
d
The regression intercept is the average vitamin C level when all model covariates are set to the reference level.
groups compared to low PIR. Adults of healthy weight ascending dietary intake quartile ranging 4.3–
or who were overweight had 10.5–10.7 µmol/L sig 22.1 µmol/L compared to the lowest (<20 mg/day).
nificantly higher vitamin C than adults with obesity. Mean VIC concentrations were significantly higher
VIC concentrations were significantly higher in each by 22.3 µmol/L (95% CI [19.5, 25.1]) in those taking
278 JALM | 272–284 | 08:02 | March 2023
Vitamin C Status of US Adults ARTICLE
vitamin C-containing supplements. Nonsmokers Nonsmokers had 8.6 µmol/L (95% CI [5.9, 11.3])
had significantly higher mean VIC than smokers by higher VIC concentrations than smokers. After
14.8 µmol/L (95% CI [11.7, 17.8]). examining all the pairwise interactions from the
model, there were 3 statistically significant interac
Regression Model tions: age and sex (P = 0.0243), age and vitamin
After adjusting for all covariates, there were no C-containing supplement use (P = 0.0001), and sex
longer any significant differences among race/ and smoking status (P = 0.0247). Selected estimated
Hispanic origin groups or PIR seen in 2017–2018 conditional marginal means from the model pre
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
(Table 2). But differences in mean VIC concentra sented in Table 2 plus the 3 significant interactions
tions by age, sex, BMI, dietary vitamin C intake, vita are shown in Fig. 1 to demonstrate the interpretation
min C-containing supplement use, and smoking of the significant interactions. Figure 1A demon
status continued to be statistically significant. strates a larger significant difference in VIC between
Namely, adults 40–59 years of age had 5.3 µmol/L men and women ≥60 years of age (12.2 μmol/L;
(95% CI [2.3, 8.3]) lower VIC concentrations than P < 0.0001) compared to those 20–39 years
those ≥60 years. VIC concentrations in women (7.4 μmol/L; P = 0.0005). Figure 1B demonstrates
were higher than men by 5.7 µmol/L (95% CI [2.5, that differences in VIC among supplement users
8.9]). Adults with healthy weight or overweight compared to nonusers were larger among those
had 8.3–9.3 µmol/L higher VIC concentrations. ≥60 years (28.5 µmol/L; P < 0.0001) than for peo
Those in the highest quartile of dietary intake had ple 20–39 years of age (11.7 µmol/L; P < 0.0001).
17.5 µmol/L (95% CI [13.9, 21.2]) higher VIC than Figure 1C demonstrates a significant difference in
those in the lowest quartile while those who VIC between nonsmoking women and non
consumed vitamin C-containing supplements smoking men (9.62 µmol/L; P < 0.0001) but not
had 19.2 µmol/L (95% CI [16.7, 21.6]) higher VIC between smoking women and smoking men
concentrations than those who did not. (3.4 µmol/L; P = 0.20).
A Sex B Vitamin C-containing C Smoking status
supplement use
70 70
Conditional marginal mean mmol/L
Conditional marginal mean mmol/L
80
Conditional marginal mean mmol/L
60 60
70
50 60 50
40 50
40
30 40
30 30
20
20
20
10 10
0 0 10
20-39 40-59 ≥60 20-39 40-59 ≥60
0
Age (years) Age (years)
Nonsmokers Smokers
Women Men Yes No Women Men
Fig. 1. NHANES 2017–2018 conditional marginal means and 95% confidence intervals derived from a
multiple linear regression with interactions for age and sex, age and vitamin C-containing supplement
use, and smoking status and sex.
March 2023 | 08:02 | 272–284 | JALM 279
ARTICLE
Survey Period Comparisons representative survey (51.2 vs 54.0 μmol/L; P =
Comparing both survey periods, the overall 0.09). These data are similar to UK National Diet
prevalence of VIC deficiency was similar in 2017– Survey (2008–2012) and the Canadian Health
2018 (Table 1) vs 2003–2006 (Table 3) with a differ Measures Survey (2012–2013) that produced
ence of 0.2% (95% CI [−2.0%, 2.5%], P = 0.83). means of 51.3 μmol/L and 53 μmol/L, respectively
Additionally, after adjusting for all covariates the (11, 12). Although the VIC concentration data were
difference remained not significant (P = 0.65) (un similar to the US, the prevalence of deficiencies
published observations). was lower; US 7%, Canadian 3%, and UK 2%. In
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
The overall mean VIC concentrations were not both NHANES survey periods, vitamin
significantly different between the 2 survey peri C-containing supplement users had mean VIC
ods (unadjusted difference 2003–2006 minus concentrations 30% higher than nonusers. In
2017–2018 was 2.74 µmol/L (95% CI [−0.41, NHANES 2017–2018, multivitamins were the
5.89], P = 0.09) as shown in Table 3. After adjusting most commonly used dietary supplements (6).
for all covariates this difference remained non Multivitamins typically contain vitamin C (26) with
significant (P = 0.52) (unpublished observations). the most popular vitamin C doses ranging from
Nevertheless, there were a few significantly lower 60–180 mg. Thirty-seven percent (95% CI [34.3,
VIC concentrations in 2017–2018 compared with 40.3]) of adults were taking vitamin C-containing
2003–2006, namely 60+ years of age, men, and supplements and among them only 0.5% were de
nonsmokers. ficient compared with 9% of those not taking vita
min C-containing supplements, demonstrating
risk reduction with supplement intake (Table 1).
DISCUSSION Serum or plasma vitamin C <5 μmol/L is a concen
tration consistent with signs and symptoms of
Overall population prevalence for VIC defi scurvy (27–30). There are relatively few scurvy
ciency has remained unchanged (approximately cases in the literature but in NHANES 2017–
7%) from 2003–2006 to 2017–2018, however, 2018, about 1% of US adults had VIC <5 µmol/L.
some covariates were associated with higher Consuming 5 varied servings of fruits and vegeta
prevalence of deficiency. For instance, low diet bles a day can provide >200 mg of vitamin C (2);
ary intake was associated with double the preva 8% of adults fell into this intake category with
lence of deficiency compared to the overall mean VIC of 65.6 μmol/L (95% CI [61.9, 69.3]),
population (Table 1). We divided 24-hour dietary which is 28% higher than the overall mean. As
intake into quartiles with the lowest quartile be noted in some other surveys but not all, low socio
tween 0 and 20 mg/day. It is known that signs economic status and high BMI were also asso
of vitamin C deficiency can appear within ciated with lower VIC (7, 11, 31, 32). Carr et al.
1 month of little or no vitamin C intake (below showed body weight dependency between daily
10 mg/day). In NHANES 2017–2018, 14% of vitamin C intake and steady state plasma vitamin
adults were consuming <10 mg/day (unpub C. They found that those with higher body weight
lished observations). Smoking, the other lifestyle require additional intake of vitamin C to increase
factor associated with increased risk of low VIC, their VIC. This important observation will require
had 3 times the prevalence of VIC deficiency com confirmation.
pared to not smoking. The pairwise interactions deepen our under
Mean VIC was essentially unchanged in US standing about the impact of multiple variables on
adults since last assessed in a nationally mean VIC (Fig. 1, A–C). The interactions between
280 JALM | 272–284 | 08:02 | March 2023
Vitamin C Status of US Adults ARTICLE
Table 3. For the US population 20 years and older: weighted prevalence (in percent) of vitamin C
deficiency (serum vitamin C <11.4 µmol/L) and weighted mean serum vitamin C concentrations,
National Health and Nutrition Examination Survey, 2003–2006, along with the estimated mean
difference between the National Health and Nutrition Examination Survey 2017–2018 and 2003–2006.
Mean difference
2003–06 2003–06 2017–18 minus
Prevalence Mean 2003–06
Variable (95% CI) (95% CI) (95% CI) P value of mean
Variables categories na (%) (µmol/L) (µmol/L) differencesb
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
Age Overall ≥20 8892 7.0 54.0 −2.74 0.09
(years) (5.7, 8.5) (52.4, (−5.89, 0.41)
55.5)
20–39 3233 6.9 51.0 −2.55 0.17
(5.4, 8.9) (48.8, (−6.24, 1.14)
53.2)
40–59 2635 8.1 51.6 −2.19 0.21
(6.3, 10.5) (49.7, (−5.66, 1.28)
53.4)
≥60 3024 5.1 63.0 −6.23 0.0023
(3.8, 6.8) (61.5, (−10.1, −2.35)
64.6)
Sex Men 4296 8.7 49.4 −3.31 0.0415
(7.0, 10.7) (47.7, (−6.48, −0.13)
51.0)
Women 4596 5.4 58.3 −2.23 0.21
(4.3, 6.8) (56.5, (−5.77, 1.30)
60.0)
Race/Hispanic origin Mexican– 1799 3.9 51.3 −1.61 0.51
American (2.6, 5.8) (48.9, (−6.53, 3.32)
53.8)
Non-Hispanic 1840 5.7 50.3 −2.87 0.13
Black (4.3, 7.6) (48.3, (−6.59, 0.86)
52.2)
Non-Hispanic 4616 8.0 54.9 −2.15 0.15
White (6.5, 9.8) (52.9, (−6.64, 2.34)
56.9)
PIR Low (0–1.85) 3455 9.7 49.2 –2.94 0.15
(8.0, 11.6) (47.4, (–6.99, 1.11)
51.1)
Middle (1.86–3.5) 2246 7.6 53.6 −1.46 0.51
(5.9, 9.8) (51.6, (−5.91, 2.99)
55.6)
High (>3.5) 2749 4.7 57.6 −3.41 0.08
(3.6, 6.1) (55.9, (−7.21, 0.39)
59.3)
BMIc Healthy (18.5– 2552 6.2 59.6 −3.50 0.13
(kg/m2) 24.99) (4.9, 7.9) (57.6, (−8.12, 1.12)
61.7)
Overweight (25– 3053 5.8 55.4 0.43 0.76
29.99) (4.7, 7.3) (53.7, (−2.45, 3.32)
57.2)
(continued)
March 2023 | 08:02 | 272–284 | JALM 281
ARTICLE
Table 3. Continued
Mean difference
2003–06 2003–06 2017–18 minus
Prevalence Mean 2003–06
Variable (95% CI) (95% CI) (95% CI) P value of mean
Variables categories na (%) (µmol/L) (µmol/L) differencesb
Obesity (≥30) 2996 8.5 47.4 −1.97 0.24
(6.6, 10.8) (45.7, (−5.32, 1.39)
49)
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
Dietary intake quartiles (0–<20) 1775 14.2 43.2 −2.01 0.37
(mg/day) (11.6, 17.2) (40.7, (−6.43, 2.42)
45.7)
(20–<50) 2068 9.0 48.2 −2.63 0.19
(7.2, 11.1) (46.1, (−6.62, 1.35)
50.2)
(50–<110) 2084 4.2 57.2 −1.03 0.50
(3.0, 5.8) (55.7, (−4.06, 2.00)
58.7)
≥110 2551 1.7 65.8 −2.54 0.17
(1.1, 2.6) (64.1, (−6.22, 1.13)
67.5)
Vitamin C-containing Yes 3603 1.7 66.7 −0.39 0.79
supplement use (1.3, 2.3) (65.4, (−3.29, 2.51)
68.1)
No 5176 11.2 43.8 −1.32 0.41
(9.2, 13.6) (41.9, (−4.52, 1.88)
45.8)
Smoking status Nonsmokers 6562 3.6 58.8 −4.07 0.0122
(2.8, 4.6) (57.5, (−7.21, −0.93)
60.0)
Smokers 2324 15.4 42.1 −2.19 0.22
(13.1, 18.0) (40.2, (−5.72, 1.34)
44.1)
a
n refers to the sample size in NHANES 2003–2006.
b
Student’s t-statistic with 45 df.
c
Relative CI width for underweight was >130%. Estimate was suppressed (23).
age and sex and age and supplement use were pri apart. The precision of the laboratory method was
marily among those ≥60 years. These differences in excellent with bench QC CVs ranging from 1.7% to
VIC (men vs women and supplement users vs nonu 7.6% (2003–2004), 3.7% to 5.7% (2005–2006), and
sers) were approximately twice the size of the other 3.6% to 4.1% (2017–2018). Although we did not par
age groups. Regarding smoking, the mean VIC dif ticipate in external quality assurance programs such
ference between men and women is only significant as INSTAND (Düsseldorf, Germany) and The Royal
in nonsmokers. College of Pathologists of Australasia (New South
A major strength of this study is that essentially Wales, Australia), and a direct method comparison
the same analytical method has been used to com between the old and new methods could not be
pare data over 2 time periods more than a decade done because the old instrument was no longer
282 JALM | 272–284 | 08:02 | March 2023
Vitamin C Status of US Adults ARTICLE
available, nevertheless we used 2 NIST standard ref CONCLUSION
erence materials, which showed minimal bias (<1%)
in both survey periods. The sample size for the VIC VIC status of the US adult population was essen
measurements was close to 5000 participants per tially the same in 2017–2018 since last assessed in
survey period providing a large sample to assess na 2003–2006. Prevalence of vitamin C deficiency re
tionally representative VIC status data. Smoking was mained high for smokers or those with low vitamin
assessed using a state-of-the-art tandem mass C intake.
spectrometry method to measure the biomarker
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
cotinine. A limitation of the survey was that only
44 women scored positive on the pregnancy test SUPPLEMENTARY MATERIAL
during 2017–2018 and therefore were not included
in our assessment; thus, our findings do not extend Supplementary material is available at
to pregnant women. The Journal of Applied Laboratory Medicine online.
Nonstandard Abbreviations: VIC, serum vitamin C; NHANES, National Health and Nutrition Examination Survey; BMI, body
mass index; PIR, poverty income ratio; MEC, mobile examination center; NCHS, National Center for Health Statistics.
Author Contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the follow
ing 4 requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of data;
(b) drafting or revising the article for intellectual content; (c) final approval of the published article; and (d) agreement to be accountable
for all aspects of the article thus ensuring that questions related to the accuracy or integrity of any part of the article are appropriately
investigated and resolved.
Authors’ Disclosures or Potential Conflicts of Interest: No authors declared any potential conflicts of interest.
Role of Sponsor: No sponsor was declared.
REFERENCES
1. Institute of Medicine. Dietary reference intakes for United States: 2003–2004 National Health and Nutrition
Vitamin C, Vitamin E, selenium, and carotenoids. Examination Survey (NHANES). Am J Clin Nutr 2009;90:
Washington (DC): The National Academies Press; 2000. 1252–63.
p. 154. 8. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of
2. Levine M, Rumsey SC, Daruwala R, Park JB, Wang Y. obesity and severe obesity among adults: United States,
Criteria and recommendations for vitamin C intake. J Am 2017–2018. NCHS data brief, no 360. Hyattsville (MD):
Med Assoc 1999;281:1415–23. National Center for Health Statistics; 2020.
3. FDA. Daily value on the new nutrition and 9. Angeles-Agdeppa I, Sun Y, Denney L, Tanda KV, Octavio
supplement facts labels. https://www.fda.gov/food/ RD, Carriquiry A, Capanzana MV. Food sources, energy
new-nutrition-facts-label/daily-value-new-nutrition- and nutrient intakes of adults: 2013 Philippines National
and-supplement-facts-labels (Accessed April 2022). Nutrition Survey. Nutr J 2019;18:59.
4. Levine M. New concepts in the biology and biochemistry 10. Kim J, Choi Y-H. Physical activity, dietary vitamin C, and
of ascorbic acid. N Engl J Med 1986;314:892–902. metabolic syndrome in the Korean adults: The Korea
5. USDA. What we eat in America nutrient intake data tables National Health and Nutrition Examination Survey 2008
2003–2004 and 2017–2018. https://www.ars.usda.gov/ to 2012. Public Health 2016;135:30–7.
northeast-area/beltsville-md-bhnrc/beltsville-human- 11. UK Government. National diet and nutrition survey
nutrition-research-center/food-surveys-research-group/ results from years 1, 2, 3, and 4 (combined) of the rolling
docs/wweia-data-tables/ (Accessed April 2022). programme (2008/2009–2011–2012). https://www.gov.
6. Mishra S, Stierman B, Gahche JJ, Potischman N. Dietary uk/government/statistics/national-diet-and-nutrition-
supplement use among adults: United States, 2017– survey-results-from-years-1-to-4-combined-of-the-
2018. NCHS data brief, no 399. Hyattsville (MD): National rolling-programme-for-2008-and-2009-to-2011-and-
Center for Health Statistics; 2021. 2012 (Accessed April 2022).
7. Schleicher RL, Carroll MD, Ford ES, Lacher DA. Serum 12. Langlois K, Cooper M, Colapinto CK. Vitamin C status of
vitamin C and the prevalence of vitamin C deficiency in the Canadian adults: findings from the 2012/2013 Canadian
March 2023 | 08:02 | 272–284 | JALM 283
ARTICLE
Health Measures Survey. Statistics Canada Health 22. CDC. National Health and Nutrition Examination Survey
Reports 2016;27:3–10. 2005–2006 Vitamin C. https://wwwn.cdc.gov/nchs/data/
13. Curtin LR, Mohadjer LK, Dohrmann SM, Montaquila JM, nhanes/2005-2006/labmethods/vic_d_met.pdf (Accessed
Kruszon-Moran D, Mirel LB, et al. The National Health and July 2022).
Nutrition Examination Survey: sample design, 1999– 23. CDC. National Health and Nutrition Examination Survey
2006. Vital Health Stat 2 2012;155:1–39. 2017–2018 Vitamin C. https://wwwn.cdc.gov/nchs/data/
14. Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, nhanes/2017-2018/labmethods/VIC-J-MET-508.pdf
Mirel LB, Carroll MD, et al. National Health and Nutrition (Accessed July 2022).
Examination Survey: sample design, 2007–2010. Vital 24. Parker JD, Talih M, Malec DJ, Beresovsky V, Carroll M,
Health Stat 2 2013;160:1–23. Gonzalez JF, et al. National Center for Health Statistics data
15. Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. presentation standards for proportions. National Center
National Health and Nutrition Examination Survey: for Health Statistics. Vital Health Stat 2017;2:175.
Downloaded from https://academic.oup.com/jalm/article/8/2/272/6967020 by guest on 25 November 2023
sample design, 2011–2014. Vital Health Stat 2 2014; 162: 25. Sternberg MR, Schleicher RL, Pfeiffer CM. Regression
1–33. modeling plan for 29 biochemical indicators of diet and
16. US Centers for Disease Control and Prevention, National nutrition measured in NHANES 2003–2006. J Nutr 2013;
Center for Health Statistics. Response rates & CPS 143:948S–56S.
population totals, National Health and Nutrition 26. NIH. Vitamin C fact sheet for health professionals. https://
Examination Survey. https://wwwn.cdc.gov/nchs/nhanes/ ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
ResponseRates.aspx (Accessed April 2022). (Accessed April 2022).
17. US Centers for Disease Control and Prevention, National 27. Angeli AM, Megna B, Mazepa M, Ivy ZK, Sultan S, Sloan JA.
Center for Health Statistics. National Health and Nutrition Transfusion-dependent anemia secondary to Vitamin C
Examination Survey: analytic guidelines, 2011–2014 and deficiency. Am J Hematol 2022;97:E166–88.
2015–2016. https://wwwn.cdc.gov/nchs/data/nhanes/ 28. Berry CT, Berry KG, Abbott J, Jiang AJ, Ronner L, Mollanazar
analyticguidelines/11-16-analytic-guidelines.pdf NK, et al. Resolution of acquired palmoplantar
(Accessed June 2022). keratoderma and scurvy after treatment of multivitamin
18. US Centers for Disease Control and Prevention. Second deficiencies. JAAD Case Rep 2022;22:27–30.
national report on biochemical indicators of diet and 29. Nastro A, Rosenwasser N, Daniels SP, Magnani J, Endo Y,
nutrition in the US population 2012. Atlanta (GA): National Hampton E, et al. Scurvy due to selective diet in a
Center for Environmental Health; 2012. p.72–84. seemingly healthy 4-year-old boy. Pediatrics 2019;144:
19. McCoy LF, Bowen MB, Xu M, Chen H, Schleicher RL. e20182824.
Improved HPLC assay for measuring serum vitamin C with 30. Eissen F, Jacocks C, Matthew C. Sailing the ship of life:
1-methyluric acid used as an electrochemically active scurvy and autoimmunity. Ther Adv Chronic Dis 2022;13:
internal standard. Clin Chem 2005;51:1062–4. 1–3.
20. Caudill SP, Schleicher RL, Pirkle JL. Multi-rule quality 31. Crook J, Horgas A, Yoon S-J, Grundmann O,
control for the age-related eye disease study. Stat Med Johnson-Mallard V. Insufficient vitamin C levels among
2008;27:4094–106. adults in the United States: results from the NHANES
21. CDC. National Health and Nutrition Examination Survey surveys, 2003–2006. Nutrients 2021;13:3910–21.
2003–2004 Vitamin C. https://wwwn.cdc.gov/nchs/data/ 32. Carr AC, Block G, Lykkesfeldt J. Estimation of vitamin C
nhanes/2003-2004/labmethods/l06_c_met_vitamin-c.pdf intake requirements based on body weight: implications
(Accessed July 2022). for obesity. Nutrients 2022;14:1460–7.
284 JALM | 272–284 | 08:02 | March 2023
You might also like
- DepED PFT Score CardDocument1 pageDepED PFT Score CardFelix Llamera81% (31)
- Nutrition and Diet Therapy Laboratory Manual - Docx?lmsauth 0a8fa5e7Document67 pagesNutrition and Diet Therapy Laboratory Manual - Docx?lmsauth 0a8fa5e7Davina Militar100% (3)
- Syllabus in Teaching Pe and HealthDocument5 pagesSyllabus in Teaching Pe and Healthjessica cacho100% (7)
- Inbody 720 Results InterpretationDocument33 pagesInbody 720 Results InterpretationRicardo Wallace Das Chagas LucasNo ratings yet
- BM I Chart GirlsDocument1 pageBM I Chart GirlscjgeronimoNo ratings yet
- 4.nutritional-Metabolic PatternDocument12 pages4.nutritional-Metabolic PatternLúcia Costa50% (2)
- Vitamin CDocument12 pagesVitamin CJefry WahyudiNo ratings yet
- 2016-Determinants of Anemia Among School-Aged Children in Mexico The United States and ColombiaDocument15 pages2016-Determinants of Anemia Among School-Aged Children in Mexico The United States and ColombiaElizabethNo ratings yet
- Vitamin D: Fat-Soluble Vitamins & MicronutrientsDocument6 pagesVitamin D: Fat-Soluble Vitamins & MicronutrientsMehak SharmaNo ratings yet
- EnglishDocument9 pagesEnglishapi-245723352No ratings yet
- Developing Suitable Methods of Nutritional Status Assessment: A Continuous ChallengeDocument9 pagesDeveloping Suitable Methods of Nutritional Status Assessment: A Continuous Challengeparampam21No ratings yet
- 9 FullDocument7 pages9 FullSaudah Sii SipitNo ratings yet
- Hs A220 (Us & Alaskan Health Indicators)Document8 pagesHs A220 (Us & Alaskan Health Indicators)teddzquizzerNo ratings yet
- Weight and Skin Colour As Predictors of Vitamin D Status: Results of An Epidemiological Investigation Using Nationally Representative DataDocument8 pagesWeight and Skin Colour As Predictors of Vitamin D Status: Results of An Epidemiological Investigation Using Nationally Representative Datatihemex618No ratings yet
- Consumul de ZaharDocument10 pagesConsumul de Zaharpaul_preda_bvNo ratings yet
- Frequency and Determinants of Vitamin A Deficiency in Children Under 5 Years of Age With PneumoniaDocument6 pagesFrequency and Determinants of Vitamin A Deficiency in Children Under 5 Years of Age With Pneumoniayuni020670No ratings yet
- Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation - United States, 2007-2009Document36 pagesPrevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation - United States, 2007-2009worksheetbookNo ratings yet
- Metabolic Syndrome in The Elderly Living in Marginal Peri-Urban Communities in Quito, EcuadorDocument10 pagesMetabolic Syndrome in The Elderly Living in Marginal Peri-Urban Communities in Quito, EcuadorDiana TorresNo ratings yet
- Chapter 1Document7 pagesChapter 1takumikurodaNo ratings yet
- Materi 4 Practice Paper of The Academy of Nutrition and Dietetics - Nutrition Intervention and Human Immunodeficiency Virus InfectionDocument13 pagesMateri 4 Practice Paper of The Academy of Nutrition and Dietetics - Nutrition Intervention and Human Immunodeficiency Virus InfectionGhania Agung RahmaniarNo ratings yet
- McLean 2008Document14 pagesMcLean 2008Maria PeppaNo ratings yet
- Nutrición Hospitalaria: Trabajo OriginalDocument7 pagesNutrición Hospitalaria: Trabajo OriginalJose J.No ratings yet
- Sebastian 2007Document11 pagesSebastian 2007ratvaNo ratings yet
- Morbidity and Mortality Weekly ReportDocument32 pagesMorbidity and Mortality Weekly Reporthimanshu7188No ratings yet
- Hci 540 DatabaseDocument11 pagesHci 540 Databaseapi-575725863No ratings yet
- The Frequency of Radiology Reporting of Childhood ObesityDocument4 pagesThe Frequency of Radiology Reporting of Childhood ObesityReza PramayudhaNo ratings yet
- 121 Short Stature or at Risk of Short StatureDocument3 pages121 Short Stature or at Risk of Short Statureramadhanu100% (1)
- Ingles Datos de Aumento de Cancer en Niños y Adolescentes EeuuDocument11 pagesIngles Datos de Aumento de Cancer en Niños y Adolescentes EeuuMildred RiofrioNo ratings yet
- Study That Uses Food Attitudes QuestionnaireDocument14 pagesStudy That Uses Food Attitudes QuestionnaireEd BotNo ratings yet
- FolatosDocument6 pagesFolatosBlackbeetleNo ratings yet
- Rationale HLTH 640Document5 pagesRationale HLTH 640api-535492370No ratings yet
- Diet Quality of US Adolescents During The Transition To Adulthood: Changes and PredictorsDocument9 pagesDiet Quality of US Adolescents During The Transition To Adulthood: Changes and PredictorsmiraandrianiNo ratings yet
- Diet Lifestyle and BRCA - Related Breast PDFDocument10 pagesDiet Lifestyle and BRCA - Related Breast PDFwasistoNo ratings yet
- Diantara Dingin Malam Kau Kembali Hiasi Temaram Dengan Air Mata Remuk Redam Kau Khawatir Kisah Kita Suram Kau Dan Aku Hampir Menyerah Melepas HarapDocument5 pagesDiantara Dingin Malam Kau Kembali Hiasi Temaram Dengan Air Mata Remuk Redam Kau Khawatir Kisah Kita Suram Kau Dan Aku Hampir Menyerah Melepas HarapYosie Yulanda PutraNo ratings yet
- Low-Fat or Low-Carb Diet: Does It Make A Difference?Document17 pagesLow-Fat or Low-Carb Diet: Does It Make A Difference?lapistoleroNo ratings yet
- Prevalence of Underweight Among Children and Adolescents: United States, 2007-2008Document3 pagesPrevalence of Underweight Among Children and Adolescents: United States, 2007-2008Daniel ChristoNo ratings yet
- Dissertation Vitamin D 2015Document4 pagesDissertation Vitamin D 2015BuyResumePaperFortCollins100% (1)
- Results in Relation To Other StudiesDocument3 pagesResults in Relation To Other StudiesBadseba TiweryNo ratings yet
- 17 - Prevalencia Anemia en Latino AmericaDocument10 pages17 - Prevalencia Anemia en Latino AmericaFernandoVignoloNo ratings yet
- F Is For Fat: How Obesity Threatens America's FutureDocument124 pagesF Is For Fat: How Obesity Threatens America's FutureDaniel J. SchneiderNo ratings yet
- Nutritional Assessment of Older Adults With Diabetes MellitusDocument8 pagesNutritional Assessment of Older Adults With Diabetes MellitusCarlo EspadinNo ratings yet
- Practice of Epidemiology Practice of EpidemiologyDocument11 pagesPractice of Epidemiology Practice of EpidemiologyDinda AyuuNo ratings yet
- DASH Diet 2020Document7 pagesDASH Diet 2020musyayyadahNo ratings yet
- 1 s2.0 S0749379722004299 MainDocument8 pages1 s2.0 S0749379722004299 MainJ GuimarãesNo ratings yet
- Intake Trends of Red Meat, Alcohol, and Fruits and Vegetables As Cancer-Related Dietary Factors From 1998 To 2009Document10 pagesIntake Trends of Red Meat, Alcohol, and Fruits and Vegetables As Cancer-Related Dietary Factors From 1998 To 2009Isa AguilarNo ratings yet
- JAMA EEUU Prvalencia Obesidad InfantilDocument8 pagesJAMA EEUU Prvalencia Obesidad InfantilAnonymous 0iU1pPeQNo ratings yet
- Physical Activity and Good Nutrition - Essential Elements To Prevent Chronic Diseases and ObesityDocument4 pagesPhysical Activity and Good Nutrition - Essential Elements To Prevent Chronic Diseases and ObesityccciiipppNo ratings yet
- The 2Nd Dr. Conrado R. Pascual Memorial LectureDocument6 pagesThe 2Nd Dr. Conrado R. Pascual Memorial LectureIris ÇhAppyøe EyyendhNo ratings yet
- NRSG 780 - Health Promotion and Population Health: Module 5: Health Disparities / Cultural CompetenceDocument24 pagesNRSG 780 - Health Promotion and Population Health: Module 5: Health Disparities / Cultural CompetencejustdoyourNo ratings yet
- Nutrients: Micronutrient Status in 153 Patients With Anorexia NervosaDocument10 pagesNutrients: Micronutrient Status in 153 Patients With Anorexia NervosaReza Yusna HanastaNo ratings yet
- Relation of Body Fat Indexes To Vitamin D Status and Deficiency Among Obese AdolescentsDocument9 pagesRelation of Body Fat Indexes To Vitamin D Status and Deficiency Among Obese AdolescentsJill R SendowNo ratings yet
- 1 s2.0 S2161831322003556 MainDocument8 pages1 s2.0 S2161831322003556 MainabuhudzaifNo ratings yet
- Buah Sayur5Document27 pagesBuah Sayur5AviasiNo ratings yet
- Trabajo Original Pediatria PDFDocument7 pagesTrabajo Original Pediatria PDFMirley MarinNo ratings yet
- Yaw Needs AssessmentDocument20 pagesYaw Needs Assessmentapi-644291804No ratings yet
- EvansDocument7 pagesEvansNur SyafiraNo ratings yet
- Nguyen2011 Article RelationshipBetweenObesityAndDDocument5 pagesNguyen2011 Article RelationshipBetweenObesityAndDdesytrilistyoatiNo ratings yet
- ProQuestDocuments 2023 11 13Document4 pagesProQuestDocuments 2023 11 13caylynncreatesNo ratings yet
- Dietary Quality Indices PHN 2013Document12 pagesDietary Quality Indices PHN 2013Xochitl PonceNo ratings yet
- New England Journal of Medicine Ranking 37th - Measuring The Performance of The U.S. Health Care SystemDocument2 pagesNew England Journal of Medicine Ranking 37th - Measuring The Performance of The U.S. Health Care SystemPaul JohnsonNo ratings yet
- Does Education Modify The Effect of Ethnicity in The Expression of Ideal Cardiovascular Health? The Baptist Health South Florida Employee StudyDocument8 pagesDoes Education Modify The Effect of Ethnicity in The Expression of Ideal Cardiovascular Health? The Baptist Health South Florida Employee Studysankalp dasNo ratings yet
- Ayesha Ishtiaq BS HND 2021-033 (M) Section BDocument13 pagesAyesha Ishtiaq BS HND 2021-033 (M) Section BAyesha IshtiaqNo ratings yet
- Infant and Young Child Feeding Practices in Urban Philippines and Their Associations With Stunting, Anemia, and Deficiencies of Iron and Vitamin ADocument18 pagesInfant and Young Child Feeding Practices in Urban Philippines and Their Associations With Stunting, Anemia, and Deficiencies of Iron and Vitamin AwidyarosatiNo ratings yet
- GuiaDocument3 pagesGuiaapi-421098116No ratings yet
- Micronutrient DeficiencyDocument15 pagesMicronutrient DeficiencyBaby Ruth BalderamaNo ratings yet
- Unit 9: Global Epidemic: Causes of ObesityDocument3 pagesUnit 9: Global Epidemic: Causes of ObesityNguyen Hoai ThuongNo ratings yet
- Nutritional AssessmentDocument6 pagesNutritional AssessmentReyna Mee Ahiyas100% (1)
- Adolescent Eating Habits - UpToDateDocument33 pagesAdolescent Eating Habits - UpToDateDaniela Herrera LozanoNo ratings yet
- Final Draft The Epidemic of Child Obesity in America 112514Document14 pagesFinal Draft The Epidemic of Child Obesity in America 112514api-269040739No ratings yet
- 1000 MCDP Phase 2Document118 pages1000 MCDP Phase 2Glory ShanunguNo ratings yet
- PE 1 MODULE 1 and 2Document17 pagesPE 1 MODULE 1 and 2Ks QueenNo ratings yet
- Manu Et Al-2015-Acta Psychiatrica ScandinavicaDocument12 pagesManu Et Al-2015-Acta Psychiatrica ScandinavicamerianaNo ratings yet
- Lizz ReportDocument29 pagesLizz Reportlizdorcus263No ratings yet
- Maths in Focus - Margaret Grove - ch3Document42 pagesMaths in Focus - Margaret Grove - ch3Sam Scheding100% (2)
- Grade 4-Nutritional Status (BMI)Document22 pagesGrade 4-Nutritional Status (BMI)larie_kayne5608No ratings yet
- MedicineDocument5 pagesMedicinepriyanka hermawanNo ratings yet
- Managing Stress Through Dance: LessonDocument21 pagesManaging Stress Through Dance: LessonGen HugoNo ratings yet
- RISK STRATIFICATION Effective Use of ACSM.8Document7 pagesRISK STRATIFICATION Effective Use of ACSM.8Doraisy SHNo ratings yet
- Nutrition For TeensDocument64 pagesNutrition For TeensGuia Theelena DeLa RosaNo ratings yet
- Frankenfield 2005 PDFDocument15 pagesFrankenfield 2005 PDFIván OsunaNo ratings yet
- Dietary Counseling in Dental Practice: Prevention - 5 Class Lect 17Document6 pagesDietary Counseling in Dental Practice: Prevention - 5 Class Lect 17Hassan MohamedNo ratings yet
- His Mind & Body Weight Loss PlannerDocument35 pagesHis Mind & Body Weight Loss PlannerHer Mind & BodyNo ratings yet
- Pe & Health Module 3 Week 6: Health-Related Components of FitnessDocument9 pagesPe & Health Module 3 Week 6: Health-Related Components of FitnessEXO'nflower luvNo ratings yet
- Obesity in ChildrenDocument15 pagesObesity in ChildrenJohn ConnorNo ratings yet
- Grade 8 Learning Module (Week 3)Document51 pagesGrade 8 Learning Module (Week 3)Mai Jane Gonzales BaezNo ratings yet
- Nursing Informatics Note - d1Document65 pagesNursing Informatics Note - d1georginaodamiNo ratings yet
- Community Nutrition Program Plan PowerpointDocument20 pagesCommunity Nutrition Program Plan Powerpointapi-523266509No ratings yet
- PE1 Lesson 1Document23 pagesPE1 Lesson 1cedrickNo ratings yet
- Bischoff 2019 - Obesity TherapyDocument10 pagesBischoff 2019 - Obesity TherapyEvania Astella SetiawanNo ratings yet