Professional Documents
Culture Documents
Korraa 2022
Korraa 2022
Uploaded by
AhmedCopyright:
Available Formats
You might also like
- Cure Black Magic & Evil Eye by Ruqya Ash-Sharya (Islamic Method)Document163 pagesCure Black Magic & Evil Eye by Ruqya Ash-Sharya (Islamic Method)Roohani786100% (9)
- J of Inher Metab Disea 2023 Spiekerkoetter Genomic Newborn Screening Are We Entering A New Era of ScreeningDocument18 pagesJ of Inher Metab Disea 2023 Spiekerkoetter Genomic Newborn Screening Are We Entering A New Era of ScreeningMarianne Angela CortezNo ratings yet
- 11 - Infant NutritionDocument33 pages11 - Infant NutritionEmad MashaalNo ratings yet
- PICU Protocol FINALDocument120 pagesPICU Protocol FINALwalaa mousaNo ratings yet
- Guidelines For Treatment of Septic Shock in ResourDocument21 pagesGuidelines For Treatment of Septic Shock in ResourdintaboiceNo ratings yet
- Neonatal JaundiceDocument3 pagesNeonatal JaundiceMohola Tebello GriffithNo ratings yet
- Hidrosefalus KongenitalDocument8 pagesHidrosefalus KongenitalSebastiano SegaNo ratings yet
- BMC Pediatrics: Management of Neonatal Hyperbilirubinemia: Pediatricians' Practices and Educational NeedsDocument7 pagesBMC Pediatrics: Management of Neonatal Hyperbilirubinemia: Pediatricians' Practices and Educational Needsmaya maeNo ratings yet
- Mechanical Ventilation Guidelines SNSDocument8 pagesMechanical Ventilation Guidelines SNSClaudia KosztelnikNo ratings yet
- Egyptian Neonatology Protocol 1st Ed 2022Document124 pagesEgyptian Neonatology Protocol 1st Ed 2022sherif ghazyNo ratings yet
- Ozdamire 2017organismesDocument7 pagesOzdamire 2017organismesFatma ElzaytNo ratings yet
- Original Research Article: ISSN: 2230-9926Document7 pagesOriginal Research Article: ISSN: 2230-9926Fatma ElzaytNo ratings yet
- The Diagnosis of Scabies by Non-Expert Examiners: A Study of Diagnostic AccuracyDocument13 pagesThe Diagnosis of Scabies by Non-Expert Examiners: A Study of Diagnostic AccuracyAnisa Rifkia ZSNo ratings yet
- Technology-Dependent Children: International Journal of Pediatrics and Adolescent MedicineDocument6 pagesTechnology-Dependent Children: International Journal of Pediatrics and Adolescent MedicinecharoleNo ratings yet
- Developing A Neonatal Unit Ventilation Protocol For The Preterm BabyDocument6 pagesDeveloping A Neonatal Unit Ventilation Protocol For The Preterm BabyMALIK MANASRAHNo ratings yet
- Ihz 009Document9 pagesIhz 009Abie SultanNo ratings yet
- COVID-19 Vaccine Uptake and Hesitancy Among Pregnant and Lactating Women in Saudi ArabiaDocument17 pagesCOVID-19 Vaccine Uptake and Hesitancy Among Pregnant and Lactating Women in Saudi ArabiaNormanNo ratings yet
- Bedside (Pediatrics)Document289 pagesBedside (Pediatrics)tajfaiz779No ratings yet
- JFamCommunityMed262113-1349692 034456Document5 pagesJFamCommunityMed262113-1349692 034456Putri Zatalini SabilaNo ratings yet
- Ihac 077Document7 pagesIhac 077CONSTANTIUS AUGUSTONo ratings yet
- Guidiline SdraDocument19 pagesGuidiline SdraLariza CostaNo ratings yet
- Nac y AntibióticosDocument7 pagesNac y AntibióticosRoberto MorenoNo ratings yet
- Jurnal d2d 1bDocument9 pagesJurnal d2d 1bTephii DoankkzzNo ratings yet
- Peritonitis in Children On Peritoneal Dialysis: 12 Years of Tertiary Center ExperienceDocument7 pagesPeritonitis in Children On Peritoneal Dialysis: 12 Years of Tertiary Center ExperienceMarselya GaniNo ratings yet
- FasdfyDocument8 pagesFasdfyzuliamNo ratings yet
- Experiences With Neonatal Jaundice Management in Hospitals and The Community: Interviews With Australian Health ProfessionalsDocument9 pagesExperiences With Neonatal Jaundice Management in Hospitals and The Community: Interviews With Australian Health Professionalsstardust.m002No ratings yet
- Jaundice 20 PDFDocument54 pagesJaundice 20 PDFHaziq KamardinNo ratings yet
- Consenso de Sindroe de Dificultad Respiratoria en NeonataosDocument19 pagesConsenso de Sindroe de Dificultad Respiratoria en NeonataosSayonara Mordagon ChoqueticllaNo ratings yet
- JurnalDocument7 pagesJurnalskocabzzNo ratings yet
- Outcomes of Single-Dose Empirical Antibiotic Treatment in Children With Suspected Sepsis Implemented in The Emergency DepartmentDocument5 pagesOutcomes of Single-Dose Empirical Antibiotic Treatment in Children With Suspected Sepsis Implemented in The Emergency Departmentaldo saadot garcia ortizNo ratings yet
- Management Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaDocument4 pagesManagement Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Study of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreDocument11 pagesStudy of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jurnal Hiperbilirubin 2Document3 pagesJurnal Hiperbilirubin 2Seni safitriNo ratings yet
- Pharmaceutics 13 00140Document20 pagesPharmaceutics 13 00140bhavanaparabNo ratings yet
- Zahrotunisa Yuwana (Kritik Jurnal)Document10 pagesZahrotunisa Yuwana (Kritik Jurnal)ZahroNo ratings yet
- Clinical Profile of Fungal Sepsis in New Born: A Tertiary Centre Experience From BangladeshDocument4 pagesClinical Profile of Fungal Sepsis in New Born: A Tertiary Centre Experience From BangladeshPhilippe Ceasar C. BascoNo ratings yet
- Inter-Grader Agreement in The Diabetic Retinopathy Screening Program in Palestine-IJMBS-2018.Document6 pagesInter-Grader Agreement in The Diabetic Retinopathy Screening Program in Palestine-IJMBS-2018.Riyad BanayotNo ratings yet
- 219neonatal ExaminationDocument6 pages219neonatal Examinationsam2000samNo ratings yet
- Israeli Et Al 2021 Clinical Efficacy of Topical Nasal Pomegranate Fruit Extract For Chronic Rhinitis and ChronicDocument10 pagesIsraeli Et Al 2021 Clinical Efficacy of Topical Nasal Pomegranate Fruit Extract For Chronic Rhinitis and ChronicShelin AmandaNo ratings yet
- Efficacy of Table Salt As A Treatment Option For Umbilical Granuloma in InfantsDocument5 pagesEfficacy of Table Salt As A Treatment Option For Umbilical Granuloma in InfantsajmrdNo ratings yet
- 1 s2.0 S2666535220300057 MainDocument8 pages1 s2.0 S2666535220300057 MainSensi Tresna AdilahNo ratings yet
- Part 5: Neonatal ResuscitationDocument30 pagesPart 5: Neonatal ResuscitationAngela Giselle Garcia RuizNo ratings yet
- Journal Pediatric Shock BaruDocument6 pagesJournal Pediatric Shock BaruHhhNo ratings yet
- Health Science Reports - 2022 - SeyedAlinaghi - Impact of COVID 19 Pandemic On Routine Vaccination Coverage of Children andDocument12 pagesHealth Science Reports - 2022 - SeyedAlinaghi - Impact of COVID 19 Pandemic On Routine Vaccination Coverage of Children andArumm88No ratings yet
- Factors Associated With Complicated Pneumonia in ChildrenDocument19 pagesFactors Associated With Complicated Pneumonia in ChildrenJHONATAN MATA ARANDANo ratings yet
- 2018 Year in Review in Critical CareDocument5 pages2018 Year in Review in Critical CareRs ArNo ratings yet
- Immunization Manual For Medical and Nursing Students - Final Smaller PDFDocument296 pagesImmunization Manual For Medical and Nursing Students - Final Smaller PDFamit100% (3)
- NAC en NiñosDocument14 pagesNAC en NiñosAnonymous DxJyWJwtNo ratings yet
- CAP in Children - IDSADocument52 pagesCAP in Children - IDSAlala liliNo ratings yet
- Neonatal Jaundice RDocument19 pagesNeonatal Jaundice REssam HassanNo ratings yet
- Assessment of The Awareness, Perception, Attitudes, and Preparedness of Health-Care Professionals Potentially Exposed To COVID-19 in The United Arab EmiratesDocument12 pagesAssessment of The Awareness, Perception, Attitudes, and Preparedness of Health-Care Professionals Potentially Exposed To COVID-19 in The United Arab EmiratesSarah SanadNo ratings yet
- Disease KnowledgeDocument6 pagesDisease KnowledgeJaved IqbalNo ratings yet
- Urinary Tract Infection in Children - A Narrative Review of Clinical Practice GuidelinesDocument20 pagesUrinary Tract Infection in Children - A Narrative Review of Clinical Practice GuidelinesJad DegheiliNo ratings yet
- Bharath A PDocument103 pagesBharath A PSuman MondalNo ratings yet
- Antimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaDocument9 pagesAntimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaBima RizkiNo ratings yet
- Part 5: Neonatal ResuscitationDocument30 pagesPart 5: Neonatal ResuscitationFandoko ChaniagoNo ratings yet
- Aynalem 2020@journal - Pone.0235544Document14 pagesAynalem 2020@journal - Pone.0235544Huệ MinhNo ratings yet
- Pneumonia in Infants and ChildrenDocument52 pagesPneumonia in Infants and ChildrenMikeyNo ratings yet
- Fpubh 10 881296Document12 pagesFpubh 10 881296Bekalu EndaleNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- Advances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and DiagnosticsFrom EverandAdvances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and DiagnosticsSidharth Kumar SethiNo ratings yet
- Chapter IiDocument3 pagesChapter IiTupas Alpiche Lyka SheherezadeNo ratings yet
- Mountains Beyond Mountains EssayDocument7 pagesMountains Beyond Mountains EssayKaliyah MartinNo ratings yet
- Requirements Before Issuance of Sanitary Permit: For Food EstablishmentsDocument4 pagesRequirements Before Issuance of Sanitary Permit: For Food EstablishmentsSheryl MH-PradaNo ratings yet
- Weekly Activity Report: Number of AttendeesDocument7 pagesWeekly Activity Report: Number of AttendeestabilinNo ratings yet
- Disease PredictionDocument111 pagesDisease PredictionSahabaj AlamNo ratings yet
- VAC Form 1Document1 pageVAC Form 1Angela TabudlongNo ratings yet
- EnterobiasisDocument5 pagesEnterobiasiszairaconcoNo ratings yet
- Textbook Ebook Textbook of Small Animal Emergency Medicine 1St Edition PDF All Chapter PDFDocument43 pagesTextbook Ebook Textbook of Small Animal Emergency Medicine 1St Edition PDF All Chapter PDFlue.ring158100% (6)
- Ungs 2050Document2 pagesUngs 2050Fazdrul AkiffNo ratings yet
- Argumentative EssayDocument7 pagesArgumentative EssaynemoviNo ratings yet
- Palmoplantar Hyperhidrosis: A Therapeutic ChallengeDocument4 pagesPalmoplantar Hyperhidrosis: A Therapeutic ChallengeWesley DornelasNo ratings yet
- Psychedelics, Technology, Psychedelics: Bernard S. Aaronson and Humphrey OsmondDocument8 pagesPsychedelics, Technology, Psychedelics: Bernard S. Aaronson and Humphrey OsmondJuan ScuroNo ratings yet
- A Feasibility Randomised Control Trial of Individual Cognitive Stimulation Therapy For Dementia Impact On Cognition Quality of Life and PositiveDocument10 pagesA Feasibility Randomised Control Trial of Individual Cognitive Stimulation Therapy For Dementia Impact On Cognition Quality of Life and Positivemadalena limaNo ratings yet
- ACCREDITED PROFESSIONAL ORGANIZATIONS (APOs) and ACCREDITED INTEGRATED PROFESSIONAL ORGANIZATIONS (AIPOs) As of March 4 2021Document7 pagesACCREDITED PROFESSIONAL ORGANIZATIONS (APOs) and ACCREDITED INTEGRATED PROFESSIONAL ORGANIZATIONS (AIPOs) As of March 4 2021ChinoNo ratings yet
- Prevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDDocument7 pagesPrevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDMusainah FeisalNo ratings yet
- Anglican Girls Letter March 30 2021Document4 pagesAnglican Girls Letter March 30 2021Ebele AbrahamNo ratings yet
- 5 (Jeremy Stranks) Health and Safety Pocket BookDocument10 pages5 (Jeremy Stranks) Health and Safety Pocket BookTuralNo ratings yet
- Mindfulness For Exams by Ashley LodgeDocument2 pagesMindfulness For Exams by Ashley Lodgepetit_19794618No ratings yet
- ProstataDocument26 pagesProstatasidney souzaNo ratings yet
- The Question of Sex Education in SchoolsDocument2 pagesThe Question of Sex Education in SchoolsPhoebe FranciscoNo ratings yet
- 50K Training PlanDocument2 pages50K Training PlanStephen RoemerNo ratings yet
- Risk Assessment MatrixDocument2 pagesRisk Assessment MatrixjulcemarfelipeNo ratings yet
- NCP Spiritual DistressDocument3 pagesNCP Spiritual DistressAngelo ArabejoNo ratings yet
- Binge Anxiety Killer Cheat Sheet: InstructionsDocument4 pagesBinge Anxiety Killer Cheat Sheet: Instructionsdoppler_No ratings yet
- Ensuring Patient Comfort and Clinical Accuracy During Impression Taking 3Document11 pagesEnsuring Patient Comfort and Clinical Accuracy During Impression Taking 3Raul HernandezNo ratings yet
- Activity Checklist Lecture 240307 110843Document76 pagesActivity Checklist Lecture 240307 110843ALI-A ALINo ratings yet
- Understanding Communication and ConsentDocument24 pagesUnderstanding Communication and ConsentCHRIS FLYNNNo ratings yet
- Summary Barang Masuk Dan Keluar: Nama Item Kategori Item Kode ItemDocument204 pagesSummary Barang Masuk Dan Keluar: Nama Item Kategori Item Kode ItemTitha RahmiNo ratings yet
- Larvicidal Activity of Anacardium Occidental Against Aedes Aegypti FINALDocument5 pagesLarvicidal Activity of Anacardium Occidental Against Aedes Aegypti FINALVernice OrtegaNo ratings yet
Korraa 2022
Korraa 2022
Uploaded by
AhmedOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Korraa 2022
Korraa 2022
Uploaded by
AhmedCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/362285329
Severe Hyperbilirubinemia in Term and Late Preterm Newborns: An Evidence-
Based Clinical Practice Guideline Adapted for The Use in Egypt Based on The
‘Adapted ADAPTE’ Methodology
Article in Annals of Neonatology Journal · July 2022
DOI: 10.21608/anj.2022.121921.1055
CITATION READS
1 88
24 authors, including:
Afaf Korraa Hisham Awad
إن Ain Shams University
10 PUBLICATIONS 62 CITATIONS 48 PUBLICATIONS 437 CITATIONS
SEE PROFILE SEE PROFILE
Dina Rabie Mohamed Salah Eldin Abdel Kader
Ain Shams University Misr University for Science & Technology
12 PUBLICATIONS 9 CITATIONS 13 PUBLICATIONS 146 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Yasser Sami H. Abdel Dayem Amer on 09 March 2023.
The user has requested enhancement of the downloaded file.
Annals of Neonatology Journal OPEN ACCESS
ISSN: 2636-3596
Original Article
Severe Hyperbilirubinemia in Term and Late Preterm Newborns: An Evidence-Based
Clinical Practice Guideline Adapted for The Use in Egypt Based on The ‘Adapted
ADAPTE’ Methodology
Afaf Korraa1*, Mossallam M. Nasser2, Ahmed Youssef 3, Hesham Awad 4, Safaa Emam4 ,Ghada Gad 4 ,
Dina Rabie4, Effat Assar5, Eman Almorsy1, Suzan S. Gad 6, Sameh Tawfik 7, Nefeisa Refat8, Hala
Fouad9, Mohamed S. Abdelkader9, Osama El Fikey5, Walaa A Abuelhamd10, Zahraa Ez El-Din10,
Mohammed Abdelshafy11, Nouran B AbdAlla6, Nesreen Kamal12, Iman F. Iskander10
Methodology Group: Ashraf Abdelbaky13, Tarek E.I.Omar14, Yasser S. Amer15
DOI: 10.21608/anj.2022.121921.1055
*
Correspondence: Pediatric Department, Faculty of medicine for girls, Al-Azhar University, Egypt
Email: afafkorraa@gmail.com
Full list of author information is available at the end of the article.
Abstract
Background: The presented evidence-based clinical practice guideline (CPG) is proposed as a National
CPG using an evidence-based and formal CPG adaptation methodology. The purpose of this study was
to adapt the international CPGs’ recommendations for term and late preterm neonates with severe
hyperbilirubinemia to suit the healthcare system in the Egyptian context. This CPG provides a
framework for prediction, prevention and management of severe hyperbilirubinemia in newborn infants
of 35 or more weeks of gestation. The quality of evidence and strength of recommendations are
indicated. The guideline adaptation group was chosen from various Egyptian Universities. There was an
active involvement of a Multidisciplinary Review Committee following a standardized process. The
Neonatology Guideline Adaptation Group (NGAG) was assigned individual health questions to cover
the different sections of the required CPG. A literature search for source CPGs was carried out. The
NGAG studied several guidelines. Critical appraisal was done by AGREE II (Appraisal of Guidelines
for Research and Evaluation) Instrument to rate and select the appropriate guidelines. Results: The
NGAG decided to adapt mainly the American Academy of Pediatrics Guideline (2004, 2009 & 2011)
and for the questions which were not answered; the best and most relevant evidence available was used.
Implementation tools were sought for to facilitate the application of the adapted CPG. Conclusion: The
finalized CPG offers healthcare providers with applicable evidence-based guidance for severe neonatal
hyperbilirubinemia in the Egyptian context. The Adapted ADAPTE method emphasized the value of
collaborative clinical and methodological expert groups’ efforts for adaptation of national guidelines.
Key words: Guidelines; bilirubin; hyperbilirubinemia; kernicterus, newborn
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Introduction death. The incidence of severe neonatal
Neonatal jaundice refers to yellow hyperbilirubinemia per 10,000 live births
discoloration of the skin and sclera of was found to be highest in the African
newborn babies [1]. It is generally region at 667.8, compared to 4.4/10, 000
considered a benign self-limiting in the Americans [5].
condition, affecting more than 60% of In Egypt, the numbers are not known;
healthy term and 80% of preterm infants however in a recent study on 4000 well
[2,3] . However, in some cases, severe full-term newborns screened for
neonatal hyperbilirubinemia (SNH) can jaundice, 1.9% had bilirubin levels in the
lead to irreversible brain damage and high-risk zone on the Bhutani
kernicterus [4]. Surviving infants may nomogram. This means that, in a
acquire long-term neuro-developmental population with 2.5 million new births
sequelae such as chorioathetoid cerebral per year a large group could be at risk for
palsy, sensorineural hearing loss, and severe hyperbilirubinemia and its
growth and developmental delays. Acute sequelae [6].
bilirubin encephalopathy (ABE) and In the neonatal intensive care of Cairo
chronic bilirubin encephalopathy (CBE) university Children’s hospital, in 2011,
are largely preventable if severe 44/249 admitted jaundiced newborns not
hyperbilirubinemia is identified early and only had extreme hyperbilirubinemia, but
treated promptly with effective presented with moderate to severe
phototherapy or, when indicated, bilirubin encephalopathy and in a
exchange transfusion. In a recent recently published follow up study in the
systematic review in which severe same Neonatal Intensive Care Unit
neonatal hyperbilirubinemia was defined (NICU), 23/202 babies admitted with
as that associated with acute bilirubin severe hyperbilirubinemia had abnormal
encephalopathy, exchange transfusion or
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
neurological examination at follow up [7, evidence and assessment of the benefit
8]. versus the harm of various care options
The root causes for these shocking resulting in statements that optimize
numbers within the Egyptian community patient's care [11]. The production of
include parental ignorance of the risk of clinical practice guidelines using this
severe jaundice, absence of timely follow approach is both costly and time
up for jaundiced newborns, as well as consuming. Adaptation of CPG is a valid
delay in proper intervention [9]. and efficient alternative to de novo
While tactics to prevent and treat severe development especially in resource-
neonatal hyperbilirubinemia must be limited countries. It also provides a
sensitive to cultural and resource means to expedite the process and has
variations, the universality of root causes been acknowledged by the World Health
suggest that a common strategy should Organization (WHO) to advance
be applied to make kernicterus a very guideline production. To date in Egypt
rare event throughout the world. A there does not exist a standardized
systematic approach should be developed national CPG for the prediction,
in Egypt whereby newborn infants are prevention and management of severe
monitored for risk of hyperbilirubinemia neonatal hyperbilirubinemia.
and prompt interventions followed to The aim of this work was to use the
prevent acute bilirubin encephalopathy Adapted ADAPTE method of Alexandria
and kernicterus [9]. University to provide an evidence-based
Clinical Practice Guidelines (CPGs) are CPG tailored to the needs of the Egyptian
tools for improving the quality and safety healthcare context that can be applied at
of healthcare services using a all healthcare levels from outpatients to
standardized process [10]. They are NICU settings, in order to prevent long-
produced by a systematic review of the
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
term morbidity and mortality from severe consisting of sensory neural hearing
neonatal hyperbilirubinemia. loss or auditory dys-synchrony, (3)
Definitions used in this Guideline: oculomotor impairments especially
Kernicterus: is the pathological impairment of up-gaze, but also
finding of deep-yellow staining of lateral gaze impairments including
neurons and neuronal necrosis of the strabismus, and (4) dental enamel
basal ganglia and brainstem nuclei; hypoplasia of the deciduous teeth
and clinically associated with chronic [12].
bilirubin encephalopathy [12]. Severe neonatal hyperbilirubinemia
Acute bilirubin encephalopathy (SNH): a total serum bilirubin (TSB)
(ABE): a clinical syndrome, that concentration greater than 20 mg/dL
occurs in the presence of severe in the first 72 hours of life [12].
hyperbilirubinemia, presenting with Critical or extreme
various combinations of decreased hyperbilirubinemia: a TSB
feeding, lethargy, hypotonia and/or concentration greater than 25 mg/dL
hypertonia, high-pitched cry, during the first 28 days of life [12].
retrocollis, opisthotonus, setting sun Methods
sign, fever, seizures, and death [12]. This study is part of a major project by
Chronic bilirubin encephalopathy the Egyptian Pediatric Clinical Practice
(CBE): a clinical tetrad that occurs Guidelines Committee (EPG) which was
after the history of severe formulated by members of the
hyperbilirubinemia consisting of (1) a Departments of Pediatrics from multiple
movement disorder consisting not Egyptian Universities. EPG is currently
only of athetosis and dystonia, but affiliated to the Supreme Council of the
may also include spasticity and Egyptian University Hospitals
hypotonia, (2) auditory dysfunction (http://epg.edu.eg). The committee is
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
guided by a formal CPG adaptation countries. The patient population
methodology: The “Adapted ADAPTE” included in this CPG was late preterm
[13]. and term newborns diagnosed with
This CPG is prepared using the Adapted indirect hyperbilirubinemia or at risk for
ADAPTE method of Alexandria severe hyperbilirubinemia meeting the
University that was based on the following criteria; age ≤ 28 days, weight
ADAPTE Manual and Resource Tool Kit ≥ 2.5 kg and GA ≥35 weeks. Preterm
version 2.0, released by the ADAPTE neonates and neonates with cholestasis
Collaboration in 2009 [13-15]. This were excluded from this CPG. This
formal CPG adaptation process consists adapted CPG is intended for use by
of three phases (i.e., set-up, adaptation, neonatologists, pediatricians, family
and finalization) and 24 steps with physicians, physician assistants,
modifications in the steps and tools to advanced practice nurses in outpatient,
suit the local healthcare context in health home visits, inpatient, and NICU
systems with limited resources like settings.
Egypt. The guideline adaptation group was
Guidelines adaptation methodology chosen from multiple Egyptian
Phase 1 (Set Up): universities. There was active
The topic of severe neonatal involvement of a Multidisciplinary
hyperbilirubinemia was chosen as a Review Committee including clinicians
priority because it has been proven that (academic faculty staff and consultant
with implementation of CPG in the pediatricians and neonatologists) and
western world the incidence of chronic CPG methodologists.
bilirubin encephalopathy has declined Phase 2 (Adaptation):
dramatically compared to the numbers The NGAG included 23 Professors of
seen in low- and middle income Neonatology in addition to Professors of
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Pediatrics and a general pediatrician who (2010 [20] , 2016 [21] CPGs, the
are experts in evidence-based CPG Australian (Queensland, 2017) [22] CPG
adaptation methodologies. Clinical as well as Canadian Pediatric Association
questions are identified, using the PIPOH (2018) [23] CPG were considered. The
model, including questions for risk first draft of the adapted CPG marks the
factors, prevention, prediction, diagnosis, last step of this phase.
and treatment (Table 1). The PIPOH Phase 3 (Finalization phase): In phase
model includes the target patient 3, the first draft of the adapted CPG is
population (P), intervention(s) (I), finalized after assessing whether it is
professionals and clinical specialties (P), acceptable and applicable to the Egyptian
outcomes (O), and healthcare settings or healthcare context. The draft was then
context (H). The literature search was disseminated to a panel of external
conducted using MEDLINE/PubMed and reviewers of topic experts. Afterwards,
Google Scholar portals. The Appraisal of the feedback of reviewers was revised
Guidelines for Research and Evaluation and discussed within the NGAG with
Instrument (AGREE II) [16] was used to consideration of the national healthcare
appraise the eligible Source CPGs. context. The finalized version of the
AGREE II is considered the gold adapted CPG included relevant practical
standard for quality assessment of CPG. implementation tools and strategies.
It is a reliable tool that consists of 23 Ethical approval
items organized in six domains. The Ethics approval and consents: are not
neonatology guideline adaptation group applicable in this context.
(NGAG) studied several CPGs using the Results
criteria of the AGREE II. The American We identified 19 clinical questions using
Academy of Pediatrics (AAP) (2004 the PIPOH model. We studied several
[17], 2009[18], 2011 [19] CPGs, NICE source original CPGs for prediction,
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
prevention and management of severe These tools were developed and revised
neonatal hyperbilirubinemia. Based on by the NGAG group to be used by
the results of the AGREE II appraisal and healthcare providers and families of
in-depth content review, there was a neonates for education and awareness, so
consensus among the members of the that the tools would be effective in our
NGAG to adapt the AAP CPGs (2004, community. Implementation tools are
2009 & 2011) [18-20] to answer the 19 shown in Appendices 1-5. The most
clinical questions posted. For questions important of which were the summary of
not answered within the chosen source, recommendations, the discharge card for
the group searched for other most the parents that shows the possible risk
relevant evidence available providing its for developing severe jaundice in their
grading and reference. The AGREE II babies and the time of follow up. The
ratings of the AAP CPG were 96% algorithm for the management of a case
(domain 1: scope and purpose), 90.7% presenting with neonatal jaundice, the
(domain 2: stakeholder involvement), decision making graphs as well as how to
97.9% (domain 3: rigor of development), make phototherapy most effective.
98 (domain 4: clarity and presentation), Future updates to this adapted CPG will
72.2% (domain 5: applicability), 97.2% review and consider any evidence
(domain 6: editorial independence), 88.8 published after our cut-off date.
% (overall assessment 1), and the overall Key to Evidence: The evidence
assessment 2 showed that NGAG presented in this CPG is categorized
recommended its use in practice. The according to the categorization of the
summary recommendations of the AAP Steering Committee on Quality
adapted CPG are highlighted in Table 1. Improvement and Management [17]
A set of CPG implementation tools were
attached to the finalized adapted CPG.
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
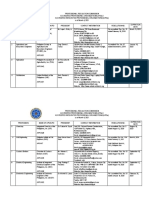
Table 1: Health Questions Question What is the schedule of follow up
Question How can SNH be prevented among 10 for the jaundiced newborn after
1 newborns with gestational age ≥ 35 leaving maternity?
weeks and ≥ 2.5 kilograms? Question When to order other investigations
Question What are the risk factors for SNH to 11 for neonatal jaundice? Which tests
2 be assessed in every newborn? to order?
Question What is the feeding counselling Question What are the different modalities of
3 required for mothers to decrease risk 12 treatment of neonatal
of severe neonatal hyperbilirubinemia?
hyperbilirubinemia? Question What is the best method of
Question How to monitor and assess babies 13 administering phototherapy?
4 for neonatal jaundice? Question When to discontinue phototherapy
Question What is the best method of 14 and how to monitor for rebound
5 predicting SNH among babies ≥ 35 hyperbilirubinemia?
weeks gestation and ≥ 2.5 kg (safe, Question When is exchange transfusion
cost effective)? 15 indicated? How is it performed?
Question When should TSB or TcB be How to avoid its complications?
6 measured? How a bilirubin level is Question Is there a role for IVIG use?
interpreted using the hour-specific 16
nomogram? Question Is there a role for other medicines in
Question What message should parents know 17 the treatment of neonatal
7 before discharge from maternity hyperbilirubinemia?
hospital? Question What information should be given to
Question What should be included in the 18 parents during hospitalization and
8 formal assessment of babies with before discharge?
gestational age ≥35 weeks and Question How to follow up the baby with
weight >2.5 kg presenting with 19 severe hyperbilirubinemia after
neonatal hyperbilirubinemia? discharge?
Question When and how to assess for ABE?
9
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Table 2: Key Recommendations water or dextrose water
CPG Source Recommendations Level is NOT recommended.
of 2 SECONDARY PREVENTION OF SNH:
Evide AAP All infants should be 4
nce 2004- routinely monitored for
PRIMARY PREVENTION of severe 2009- the development of
hyperbilirubinemia: 2011 jaundice, and all nurseries
o During antenatal care: should have established
AAP 2004- All pregnant women 2 protocols for the
2009-2011 should be tested for assessment of jaundice.
ABO and Rh (D) blood AAP If a mother has not had 2
types. An antibody titer 2004- prenatal blood grouping or
should be performed 2009- is Rh-negative, a direct
for mothers with 2011 antibody test (Coombs’
suspected test), blood type, and Rh
incompatibility. type on the infant’s (cord)
All mothers with Rh- blood are strongly
incompatibility should recommended.
receive Anti D AAP If the maternal blood is 3
prophylaxis 2004- group O, check the
o Following delivery: Support breast 2009- infant’s blood type and
feeding 2011 direct antibody test, unless
AAP 2004- Clinicians should 3 bilirubin measurement and
2009-2011 advise mothers to nurse risk assessment using
their infants at least 8 Bhutani nomogram is
to 12 times per day for done together with close
the first several days. follow-up.
AAP 2004- Routine 2
2009-2011 supplementation of
breastfed infants with
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
DIAGNOSIS of RISK for severe of the infant and the evolution
hyperbilirubinemia and use of Bhutani of hyperbilirubinemia.
nomogram (Appendix fig 1): GPP If repeat TSB shows a rate of 4
AAP Before discharge from 3 rise >0.2 mg/dL/hour, this
2004- maternity hospital, every baby should be considered
2009- newborn should be assessed high risk and persistent values
2011 for the risk of developing above this rate require urgent
hyperbilirubinemia, and all intervention.
nurseries should establish AAP A TcB and/or TSB 4
protocols for assessing this 2004- measurement should be
risk. Such assessment is 2009- performed if the jaundice
particularly important in 2011 appears excessive for the
infants who are discharged infant’s age or if there is any
before the age of 72 hours. doubt about the degree of
AAP Combining a pre-discharge 3 jaundice exists.
2004- measurement of TSB or TcB AAP Visual estimation of bilirubin 3
2009- with clinical risk factors 2004- levels from the degree of
2011 (gestational age/ Rh- or ABO 2009- jaundice can lead to errors,
incompatibility) will provide 2011 particularly in darkly
the most accurate risk pigmented infants
assessment for SNH. AAP All bilirubin levels should be 3
AAP A TSB measurement should 3 2004- interpreted according to the
2004- be performed on every infant 2009- infant’s age in hours (Figure
2009- who is jaundiced in the first 2011 1.).
2011 24 hours after birth (Figure
1). The need for and timing of
a repeat TSB measurement
will depend on the zone in
which the TSB falls on the
nomogram (Figure 1), the age
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Instructions to parents before discharge from AAP Follow-up should be provided 3
maternity hospital 2004- for some newborns discharged
AAP All maternity hospitals 4 2009- before 48 hours, 2 follow up
2004- should provide written 2011 visits may be required, the
2009- information for parents at the first visit between 24 and 72
2011 time of discharge, which hours and the second between
should include an explanation 72 and 120 hours. Clinical
about neonatal jaundice, the judgment should be used in
need to monitor infants for determining follow up. (It is
jaundice, and advice on how essential to ensure a protocol
monitoring should be done. for the assessment of jaundice
during these follow up visits
Follow up of a baby for jaundice after especially in rural Egypt).
discharge from maternity hospital ( appendix AAP Earlier or more frequent 3
Fig 4a,b,c): 2004- follow-up should be provided
AAP All infants should be 3 2009- for those who have risk factors
2004- examined by a qualified health 2011 for hyperbilirubinemia ,
2009- professional in the first few whereas those discharged with
2011 days after discharge to assess few or no risk factors can be
the infant’s wellbeing and the seen after longer intervals
presence or absence of AAP If appropriate follow-up 4
jaundice. 2004- cannot be ensured in the
The timing and location of 2009- presence of elevated risk for
this assessment is determined 2011 developing severe
by the length of stay in the hyperbilirubinemia, it may be
nursery, pre-discharge TcB or necessary to delay discharge
TSB, presence or absence of until appropriate follow-up
risk factors for severe can be ensured or the period
hyperbilirubinemia and risk of of greatest risk has passed (72-
other neonatal problems. 96 hours).
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
AAP Follow-up assessment should 3 explained by the history and
2004- include the infant’s weight physical examination.
2009- and percent change from birth AAP Infants who have an elevation 3
2011 weight, adequacy of intake, 2004- of direct reacting (or
pattern of voiding and 2009- conjugated) bilirubin should
stooling, and the presence or 2011 have a urine analysis and
absence of jaundice. culture. Additional laboratory
AAP Clinical judgment should be 3 evaluation for sepsis should
2004- used to determine the need for be performed if indicated by
2009- a bilirubin measurement. If history and physical
2011 there is any doubt about the examination.
degree of jaundice, the TSB or AAP If the direct reacting (or 4
TcB level should be measured. 2004- conjugated) bilirubin is
2009- elevated, additional
AAP Assessment for acute 4 2011 evaluation for the causes of
2004- bilirubin encephalopathy cholestasis is recommended.
2009- should be done in every AAP It is an option to measure the 4
2011 severely jaundiced baby or 2004- serum albumin level and
any jaundiced baby with risk 2009- consider an albumin level of
factors for neurotoxicity using 2011 less than 3.0 g/dL as a risk
modified BIND score factor for lowering the
(appendix table I) threshold for phototherapy
use.
Diagnosis of the cause of jaundice:
AAP The possible cause of 3
2004- jaundice should be sought in
2009- an infant requiring
2011 phototherapy or whose TSB
is rising rapidly (i.e., crossing
percentiles) and is not
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Treatment of neonatal hyperbilirubinemia: 2011 does not fall or continues to
AAP In using the guidelines for 4 rise despite intensive
2004- phototherapy and exchange phototherapy, it is likely that
2009- transfusion, the direct hemolysis is occurring.
2011 reacting (or conjugated) AAP In breastfed infants on 3
bilirubin level should NOT 2004- conventional phototherapy, it
be subtracted from the total. 2009- is recommended that, if
AAP If the TSB is at a level at 3 2011 possible, breastfeeding should
2004- which exchange transfusion is be continued while
2009- recommended or if the TSB withholding phototherapy for
2011 level is 25 mg/dL (428 the duration of the feed,
mol/L) or higher at any time, provided TSB is not rising.
it is a medical emergency and AAP In breastfed infants receiving 2
the infant should be admitted 2004- phototherapy,
immediately and directed to a 2009- supplementation with
hospital pediatric service for 2011 expressed breast milk or
intensive “crash-cart” formula is appropriate if the
Phototherapy, to avoid delay infant’s intake seems
in initiation of treatment. inadequate, weight loss is
excessive, or the infant is
dehydrated.
A) Phototherapy (appendix fig 2): AAP Routine intravenous fluids are 3
AAP All nurseries and NICUs 4 2004- NOT necessary for term or
2004- treating infants should have 2009- near term infants receiving
2009- the necessary equipment to 2011 phototherapy unless there is
2011 provide intensive evidence of dehydration.
phototherapy AAP Monitoring TSB for infants 3
AAP Recommendations for 3 2004- receiving intensive
2004- phototherapy treatment are 2009- phototherapy:
2009- given in Figure 2. If the TSB 2011 • If TSB ≥ 25 mg/dL, repeat
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
TSB within 2–3 hours. the need for exchange
• If TSB 20–25 mg/dL, repeat transfusion.
within 3–4 hours. AAP Immediate exchange transfusion 4
• If TSB <20mg/dL, repeat 2004- is recommended in any infant
within 4-6 hours. 2009- who is jaundiced and manifests
If TSB continue to fall. 2011 signs of intermediate to
Repeat in 8-12 hours. advanced stages of acute
Consider exchange bilirubin encephalopathy
transfusion if TSB is not (hypertonia, arching, retrocollis,
decreasing or is moving opisthotonus, fever, high pitched
closer to the level for cry) even if the TSB is falling.
exchange transfusion AAP Exchange transfusions should be 4
AAP When TSB is 13–14 mg/dL 3 2004- performed only by a team of
2004- discontinue phototherapy. 2009- trained personnel in a neonatal
2009- Depending on the cause of the 2011 intensive care unit with full
2011 hyperbilirubinemia, it is an monitoring and resuscitation
option to measure TSB 24 capabilities
hours after discharge to check GPP A double-volume exchange 4
for rebound unless there are transfusion should be performed
signs of hemolysis. to treat babies whose serum
bilirubin level indicates its
B) Exchange Transfusion (appendix fig 3): necessity and/or with clinical
Recommendations for exchange transfusion features and signs of acute
If an exchange transfusion is 4 bilirubin encephalopathy.
AAP
2004- being considered, the serum
2009- albumin level should be
2011 measured, and the bilirubin/
albumin ratio used in
conjunction with the TSB level
and other factors in determining
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
following medications for the
GPP Use the following medications 4 GPP treatment of
with caution in a baby with hyperbilirubinemia is NOT
hyperbilirubinaemia as they may indicated: (Phenobarbitone,
cause bilirubin to be displaced Agar, Clofibrate, albumin,
from albumin binding sites. charcoal, cholestyramine,
• Konakion Dpenicillamine, glycerine,
• Digoxin riboflavin, homeopathy,
• Diazepam • Salicylates metalloporphyrins).
• Diuretics (e.g., furosemide and
hydrochlorothiazide) • Parents information during hospitalization
Ceftriaxone • Ibuprofen •
Sulfamethoxazole such as in AAP Give parents or caregivers 3
trimethoprim/sulfamethoxazole 2004, information about treatment
(cotrimoxazole) 2009, for hyperbilirubinemia
• Indomethacin 2011 including:
• Free fatty acids (Intralipid) *Encourage mothers of
jaundiced breastfed babies to
C) Intravenous Immunoglobulins (IVIG) breastfeed frequently, and to
AAP In isoimmune hemolytic 2 wake the baby for feeds if
2004- disease, administration of necessary.
2009- IVIG (0.5-1 g/kg over 2 • Provide lactation/feeding
2011 hours) is recommended if the support to breastfeeding
TSB is rising despite intensive mothers whose baby is visibly
phototherapy or the TSB level jaundiced.
is within 2 to 3 mg/dL of the • Reassurance that
exchange level. If necessary, breastfeeding, nappy-
this dose can be repeated after changing can continue in most
12 hours. cases.
The use of any of the 4 • Offer parents or caregivers
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
verbal and written information hemoglobin measurement
on phototherapy or exchange should be performed at two
transfusion. weeks if it was low at
• Give information about discharge and at four weeks if
anticipated duration of it was normal.
treatment. GPP: Good Practice Point (based on the
expertise of the NGAG)
• Upon completion of therapy
give information about
Discussion
rebound and follow up
Jaundice is one of the most common
Follow up of newborns with severe conditions requiring medical attention in
hyperbilirubinemia: Egyptian newborn babies [6]. Because it
GPP Any infant with severe 4 is so common and usually benign, cases
neonatal hyperbilirubinemia
of SNH can easily be missed and
should receive a hearing
mistaken for simple physiological
screen including brainstem
auditory evoked potentials
jaundice which is known to occur in 60%
(ABR) for the early diagnosis of term and 80% of preterm babies in the
of auditory dys-synchrony or first week of life. The management of
sensory neural hearing loss neonatal jaundice is a particular
and timely intervention.
challenge to the neonatologist. He/she
GPP Infants who required 4
should learn to avoid over treatment of
exchange transfusion or those
who exhibit neurological
harmless cases specially with limited
abnormalities require regular resources but at the same time should
neurological follow up. never miss severe neonatal
GPP Infants with isoimmunization 4 hyperbilirubinemia which if left
are at risk of severe anemia
untreated can lead to permanent
after several weeks (up to 8-
bilirubin-induced neurological damage
12 weeks of age); a repeat
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
[24] . The importance of this work lies in practical framework for the prediction,
using the Adapted ADAPTE method [13] prevention and management of SHB
to expedite the production of this adapted through the use of this adapted CPG.
evidence-based CPG, for the use in the Testing the blood group and RH type of
Egyptian community, to prevent further the mother can identify risky blood
increase in the number of kernicterus groups; and health education at that point
cases by following the instructions in the antenatal care clinic can raise
provided to healthcare physicians and awareness of the mother to the possible
other medical personnel that deal with risks her baby may be exposed to if she
newborns. The presence of the Egyptian belongs to a risky blood group. Also,
pediatric guidelines committee has clear instructions regarding breast
provided support and has been a feeding support as well as date of follow
facilitator for this project and the up for jaundice are essential. Education
inclusion of representative professors of the mother for red flags her baby
from multiple universities all over Egypt might show that require urgent medical
has enriched the process bringing in advice can allow timely medical
different experiences that were essential intervention that would prevent acute
for the completion of this work. bilirubin encephalopathy which is the
The aim of this project was to produce consequence of neglected severe neonatal
an available evidence-based document hyperbilirubinemia.
that caters to the need and increases the Measuring a predischarge TSB or TcB
awareness of Egyptian physicians for newborn infants, and plotting it on
managing newborn babies regarding the the Bhutani hour-specific nomogram
risk of developing severe neonatal [25] provides an excellent guide for
hyperbilirubinemia and kernicterus and timely follow up and for predicting
to provide them with a standardized which infants are at increased risk for
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
developing severe hyperbilirubinemia and the risks of severe jaundice. Other
and its sequelae. Once baby is clinically tools, like the summary of
jaundiced, the CPG encourages mothers recommendations when printed on a
to seek medical advice and decision small card and made available in every
making should be guided according to nursery as well as the decision charts can
the clinical examination for signs of make the life of physicians much easier
acute bilirubin encephalopathy as well as and facilitate correct decision making.
plotting the serum bilirubin on specific Limitations: Although the achievement
graphs to decide whether phototherapy is of producing this adapted Egyptian CPG
sufficient or the baby requires exchange for the prediction, prevention and
transfusion. In the latter case, this management of SNH newborns is a huge
newborn should be managed as a medical one; there are limitations to its
emergency where intensive phototherapy effectiveness in reducing the number
is started while preparations for exchange kernicterus cases in our community.
transfusion are made using the crash cart These include the limited financial
approach. resources required for the wide
The preparation not only of the adapted dissemination of the CPG, and for the
CPG but also the attached continuous medical training and
implementation tools, though tedious is workshops essential for neonatal
essential. Implementation tools facilitate healthcare providers to be effective in its
the use of this adapted CPG. The Arabic application in Egypt. The difficult
explanation of jaundice and its sequelae collaboration with Obstetric colleagues
in a small flyer that parents can receive which is essential for educating the
on discharge, facilitates communication mothers during antenatal care regarding
with the parents and also increases risky blood groups and the seriousness of
awareness to the importance of follow up neglecting early neonatal jaundice and
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
the importance of close follow up after 3. Protocols for monitoring and assessment of
delivery. Also, resources are required for the risk for severe neonatal
hyperbilirubinemia using the bilirubin
providing points of care, bilirubin
nomogram should be present in all nurseries
measuring devices, affordable
including bilirubin measurement (TcB or
phototherapy and training personnel on TSB) and the risk factors for neurotoxicity.
how to make it more effective. 4. Blood group testing of mothers and infants
Conclusions as well as direct Coombs’ test should be
Using the Adapted ADAPTE method performed in every baby who appears
jaundiced in the first 24 hours of life. If
facilitated the production of an adapted
there is no mother-infant Rh or ABO
evidence-based CPG for the predication,
incompatibility and Coombs’ test is
prevention and management of severe negative, other causes of hemolysis should
neonatal hyperbilirubinemia in late be sought for (e.g. G6PD).
preterm and term newborns in prompt 5. Every infant jaundiced in the first 24 hours
time, and with the required should have total serum bilirubin (TSB)
measurement and be managed accordingly.
implementation tools. The effectiveness
6. If treatment is required, it should be based
of this CPG should be assessed by
on TSB (do NOT subtract the direct
monitoring the impact of the use of these fraction)
CPGs in the reduction of cases of 7. All bilirubin levels should be interpreted
kernicterus that still occur in our country. according to the infant’s age in hours using
Summary of Key Recommendations the bilirubin nomogram and an appropriate
1. Increase awareness of mothers, during follow-up date based on the time of
antenatal care, about the risks of severe discharge and the risk assessment; all should
neonatal jaundice especially if her blood be arranged and written in a follow-up card.
group is Rh-negative or O and/or her 8. Initiate phototherapy as soon as possible.
indirect Coombs’ test is positive. Avoid any delay.
2. Early promotion of successful frequent 9. In isoimmune hemolytic disease (ABO or
breastfeeding. Rh-incompatibility) administration of
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
intravenous immunoglobulin (IVIG, 0.5-1 Abbreviations
g/kg over 2 hours) is recommended if the AAP: American Academy of Pediatrics
TSB is rising despite intensive phototherapy ABE: Acute bilirubin encephalopathy
or if the TSB level is within 2 to 3 mg/dL of AGREE II: Appraisal of Guidelines for
the exchange level. If necessary, this dose Research and Evaluation Instrument
can be repeated after 12 hours. BIND score: Bilirubin induced neurological
10. Any baby presenting with severe neonatal damage score
jaundice should be examined using the CBE: chronic bilirubin encephalopathy
modified BIND score. CPG: clinical practice guideline
11. If there are signs of acute bilirubin EPG: Egyptian Pediatric Clinical Practice
encephalopathy or if TSB reaches exchange Guidelines Committee
transfusion level or if the TSB level ≥ 25 NGAG: Neonatal guideline adaptation group
mg/dL (428 mol/L), it is a MEDICAL NICU: Neonatal intensive care unit
EMERGENCY and the infant should be PIPOH model: population (P), intervention(s)
admitted immediately for intensive “crash- (I), professionals and clinical specialties (P),
cart” phototherapy, while preparing for outcomes (O), and healthcare settings or context
possible exchange to avoid delay in (H)
initiation of treatment. SNH: severe neonatal hyperbilirubinemia
12. The use of any of the following medications TSB: total serum bilirubin
for the treatment of hyperbilirubinemia in WHO: World health organization
healthy term or late preterm is NOT Acknowledgement
recommended (phenobarbitone, agar, The NGAG gratefully acknowledges the
clofibrate, charcoal, cholestyramine, D- American Academy of Pediatrics Subcommittee
penicillamine, glycerine, riboflavin). on Hyperbilirubinemia and the help of the
13.Follow up of any baby with severe professors who reviewed drafts of this Adapted
hyperbilirubinemia should include ABR, a CPG and provided valuable criticisms, as part of
neurological examination and follow up for the External Review Panel, whether at the
anemia. national level: Dr. Nahed Fahmy, Cairo
University; Dr. Mohamed Fathalla, Ain Shams
University; Dr. Aly Afia, Al-Azhar University;
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Dr. Hesham Abdel-Hady, Mansoura University financial funding throughout the development of
and Dr. Abdel Latif Abdel Moez, Assuit this work in terms of utilization of its facilities.
University; or at the international level : Dr. This work is not related to any pharmaceutical
Vinny Bhutani, Stanford University and Dr. company. The members of the NGAG and their
John Watchco, Pittsburgh University. universities volunteered their participation.
Author's contributions Funding
Members of the CPG adaptation group (Clinical The research was self-funded by the authors and
subgroup) (searching, screening, AGREE II no funding was received from any funding body
assessment): Iman Iskander, Mossallam or organization.
Mohamed Nasser, Afaf Korraa, Ahmed Availability of Materials
Youssef, Dina Rabie, Ghada Gad, Effat Assar Any relevant material in addition to future
, Eman Almorsy, Mohammed Abdelshafy , revisions and updates will be made available
Mohamed Abdel Kader, Nouran AbdAllah, and downloadable from the official website of
Safaa Shafik, Suzan Gad. the Egyptian Pediatrics Clinical Practice
Methodology Group: Ashraf Abdelbaky, Tarek Guidelines Committee (http://epg.edu.eg).
Omar and Yasser Amer. Author's details
1
Iman F. Iskander was the Chair of the NGAG. Pediatric Department, Faculty of medicine for
Afaf A. Korraa, Iman Iskander and Mossallam girls, Al-Azhar University, Egypt
2
Nasser have written the first draft of the Pediatric Department, Faculty of medicine for
manuscript. Ashraf Abdelbaky and Tarek E. boys, Al-Azhar University, Egypt
3
Omar conceptualized and designed the study. Pediatric Department, Armed Forced College
Yasser S. Amer reviewed the methodology, of Medicine, Egypt
4
drafts and the final version of this manuscript. Pediatric Department, Ain Shams University,
All authors contributed to the data collection, Egypt
5
critical appraisal of guidelines and approved the Pediatric Department, Benha University, Egypt
6
final version of the manuscript. Pediatric Department, Suez Canal University,
Conflict of interest Egypt
7
The Armed Forces College of Medicine Pediatric Department, Military Medical
(AFCM) and The Neonatology Guideline Academy, Egypt
8
Adaptation Group (NGAG) provided non- Pediatric Department, Assuit University, Egypt
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
9
Pediatric Department, Misr University for 3- Maisels MJ. Epidemiology of neonatal
Science and Technology, Egypt jaundice. In: Maisels MJ, Watchko JF,
10
Pediatric Department, Cairo University, Egypt editors. Neonatal jaundice. Amsterdam:
11
Pediatric Department, Benha Children’s Harwood Academic Publishers; 2000. p. 37–
Hospital, Egypt 49.
12
Public health Department, Cairo University, 4- Ebbesen F, Andersson C, Verder H, Grytter
Egypt C, Pedersen-Bjergaard L, Petersen JR, et al.
13
Pediatric Department, Allergy, Immunology & Extreme hyperbilirubinaemia in term and
Rheumatology unit, Ain Shams University, near-term infants in Denmark. Acta
Egypt, Chair of EPG. paediatrica. 2005;94(1):59-64.
14
Pediatric Department, Pediatric Neurology, 5- Slusher TM, Zamora TG, Appiah D, Stanke
Alexandria University, Egypt. JU, Strand MA, Lee BW, et al. Burden of
15
Pediatrics Department and Clinical Practice severe neonatal jaundice: a systematic
Guidelines and Quality Research Unit-Quality. review and meta-analysis. BMJ paediatrics
Management Department, King Saud University open. 2017;1(1):e000105.
Medical City, Riyadh, Saudi Arabia.
6- Basheer H, Makhlouf M, El Halawany F,
Fahmy N, Iskander I. Screening for neonatal
Date received: 24th April 2021, accepted 17th
jaundice in El Galaa Teaching Hospital: A
July 2021
Egyptian Maternity Hospital – Can
References the model be replicated? Journal of Clinical
1- Ayyappan S, Philip S, Bharathy N, Ramesh Neonatology. 2017;6(2):128-33.
V, Kumar CN, Swathi S, et al. Antioxidant 7- Gamaleldin R, Iskander I, Seoud I, Aboraya
status in neonatal jaundice before and after H, Aravkin A, Sampson PD, et al. Risk
phototherapy. Journal of pharmacy & factors for neurotoxicity in newborns with
bioallied sciences. 2015; 7(Suppl 1):S16-2 severe neonatal hyperbilirubinemia.
2- Bhutani VK, Johnson LH, Keren R. Pediatrics. 2011;128(4):e925-31.
Diagnosis and management of 8- El Houchi SZ, Iskander I, Gamaleldin R, El
hyperbilirubinemia in the term neonate: for a Shenawy A, Seoud I, Abou-Youssef H, et al.
safer first week. Pediatric clinics of North Prediction of 3- to 5-Month Outcomes from
America. 2004;51(4):843-61, vii. Signs of Acute Bilirubin Toxicity in
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Newborn Infants. The Journal of Pediatrics. 1, 2022, 1-6. doi: 10.21608/anj.2022.
2017;183:51-5. 114062.1044
9- Iskander I, Gamaleldin R, Kabbani M. Root 15- Amer YS, Elzalabany MM, Omar TI,
causes for late presentation of severe Ibrahim AG, Dowidar NL. The ADAPTE
neonatal hyperbilirubinaemia in Egypt. Collaboration The ADAPTE Process:
Eastern Mediterranean health Journal Resource Toolkit versions for Guideline
2012;18(8):882-7. Adaptation. Version 2.0 (2009). Available
10- Fervers B, Burgers JS, Voellinger R, from: https://www.g-i-n.net/ .
Brouwers M, Browman GP, Graham ID et al 16- Brouwers M, Kho ME, Browman GP,
Guideline adaptation: an approach to Burgers JS, Cluzeau F, Feder G, Fervers B,
enhance efficiency in guideline development Graham ID, Grimshaw J, Hanna S,
and improve utilisation. BMJ Qual Saf Littlejohns P, Makarski J, Zitzelsberger L
(2011); 20(3):228–236. for the AGREE Next Steps Consortium.
11- Glasziou P, Ogrinc G, Goodman S. Can AGREE II: Advancing guideline
evidence-based medicine and clinical quality development, reporting and evaluation in
improvement learn from each other? BMJ healthcare. Can Med Assoc
Qual Saf (2011); 20 (Suppl 1):i13–i17. J. 2010. Available online July 5,
12- Shapiro SM. Definition of the clinical 2010. doi:10.1503/cmaj.090449
spectrum of kernicterus and bilirubin- 17- American Academy of Pediatrics
induced neurologic dysfunction (BIND). Subcommittee on Hyperbilirubinemia.
Journal of perinatology : official journal of Management of hyperbilirubinemia in the
the California Perinatal Association. newborn infant 35 or more weeks of
2005;25(1):54-9. gestation. Pediatrics. 2004;114(1):297-316
13- The ADAPTE Collaboration. The 18- Maisels MJ, Bhutani VK, Bogen D,
ADAPTE process: resource Toolkit versions Newman TB, Stark AR, Watchko JF.
for Guideline Adaptation Version 2.0 Hyperbilirubinemia in the newborn infant >
Available from :http://www.g.i-n-net/ 2009. or =35 weeks' gestation: an update with
14- Abdel-Azeem M. El-Mazary. "Egyptian clarifications.Pediatrics.2009;124(4):1193-8.
Pediatric Guidelines are Available Now 19- American Academy of Pediatrics.
Online.". Annals of Neonatology Journal, 4, Technical Report: Phototherapy to Prevent
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
severe Neonatal Hyperbilirubinemia in the Society: Canadian Paediatric Society; 2018
Newborn Infant 35 or More Weeks of [updated 28/2/2018; cited 2018 15/6/2018].
Gestation.Pediatrics,2011;128:e1046-e1052. 24- Maisels MJ. Managing the jaundiced
http://pediatrics.aappublications.org/content/ newborn: a persistent challenge. Canadian
128/4/e1046.full.pdf+html Medical Association Journal 2015;
20- National Institute for Health and Clinical 187(5):335-43.
Excellence. Neonatal jaundice.: NICE 25- Bhutani VK, Johnson L, Sivieri EM.
guideline [CG98]; 2010. Predictive ability of a predischarge hour-
21- National Institute for Health and Care specific serum bilirubin for subsequent
Excellence. Jaundice in newborn babies significant hyperbilirubinemia in healthy
under 28 days.: NICE guideline [CG98]; term and near-term newborns. Pediatrics.
2016. 1999 Jan;103(1):6-14.
22- Queensland Clinical Guidelines.
Neonatal jaundice. State of Queensland
Queensland Health; 2018.
23- Barrington KJ, Sankaran K, Canadian
Paediatric Society, Fetus and Newborn
Committee. Guidelines for detection,
management and prevention of
hyperbilirubinemia in term and late preterm
newborn infants | Canadian Paediatric
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Appendix 1
Figure (1): Bilirubin nomogram (BN) [25]
BN shows 3 risk zones by the percentile tracks, high-risk zone, Intermediate-risk zone, and Low
risk zone. The purpose of the BN is to predict which newborn is at high, intermediate, or low risk
to develop severe hyperbilirubinemia after discharge from the hospital.
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Appendix 2
Fig (2): Guidelines for phototherapy in infants ≥ 35 weeks gestation [17]
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Appendix 3
Fig (3). Guidelines for exchange transfusion in infants ≥35 weeks’ gestation [17]
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Appendix 4
Table I: Clinical assessment of neurotoxicity using the Modified (bilirubin induced neurologic dysfunction
(BIND) score
CLINICAL SIGN SCORE SEVERITY
MENTAL STATUS Date/Time
Normal 0 None
Sleepy but arousable
1 Mild
Decreased feeding
Lethargy
Poor suck and/or 2 Moderate
Irritable/jittery with short-term strong suck
Semi-coma
Apnea
3 Severe
Seizures
Coma
Total / 3
MUSCLE TONE
Normal 0 None
Persistent mild hypotonia 1 Mild
Moderate hypotonia
Moderate hypertonia
Increasing arching of neck and trunk on 2 Moderate
stimulation without spasms of arms and legs
and without trismus
Persistent retrocollis
Opisthotonus
Crossing or scissoring of arms or legs but 3 Severe
without spasms of arms and legs and without
trismus
Total / 3
CRY PATTERN
Normal 0 None
High pitched 1 Mild
Shrill 2 Moderate
Inconsolable crying or
Cry weak or absent in child with previous 3 Severe
history of high pitched or shrill cry
Total / 3
OCCULOMOTOR OR EYE MOVEMENTS
Normal 0 None, Mild
Sun-setting
3 Severe
Paralysis of Upward Gaze
Total / 3
Total ABE Score / 12
Final score out of 12 (zero: Normal, 1-4: mild encephalopathy, 5-6: moderate encephalopathy, 7-12: severe
encephalopathy) [12]
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Appendix 5
Figure 4 (A): Algorithm for management and follow-up according to pre-discharge bilirubin, gestation, and risk
factors [17]
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Figure 4 (B): Algorithm for management and follow-up according to pre-discharge bilirubin, gestation, and risk
factors [17]
Annals of Neonatology Journal 2022; 4(2): 67-97
Korraa et al., 2022." Severe Hyperbilirubinemia in Term and Late Preterm Newborns: ….
Figure 4 (c): Algorithm for management and follow-up according to pre-discharge bilirubin, gestation, and risk
factors [17]
Submit your next manuscript to Annals of
Neonatology Journal and take full advantage of:
• Convenient online submission
• Thorough and rapid peer review
• No space constraints or color figure
charges
• Immediate publication on acceptance
• No limit as regards tables or figures.
• Open Access research freely available for
redistribution
Submit your manuscript at:
www.anj.journals.ekb.eg
Citation: Afaf Korraa; Mossallam M Nasser; Ahmed Youssef; Dina Rabie; Effat Assar; Eman Almorsy;
Tarek Omar; Suzan S Gad; Sameh Tawfik; Nefeisa Refat; Ghada Gad; Hala Fouad; Osama El Fikey;
Safaa Emam; Walaa A Abuelhamd; Zahraa Ez El Din; Mohammed Abdelshafy; Hesham Awad; Nouran
B AbdAlla; Mohamed Abdelkader; Ashraf Abdelbaky; Nesreen Kamal; Yasser S. Amer; Eman F.
Iskander. "Severe Hyperbilirubinemia in Term and Late Preterm Newborns: An Evidence-Based
Clinical Practice Guideline Adapted for The Use in Egypt Based on The ‘Adapted ADAPTE’
Methodology". Annals of Neonatology Journal 2022; 4(2):67-97 doi: 10.21608/anj.2022.121921.1055
Copyright: Korraa et al., 2022. This article is an open access article distributed under
the terms and conditions of the Creative Commons Attribution (CC-BY) license (4).
Annals of Neonatology Journal 2022; 4(2): 67-97
View publication stats
You might also like
- Cure Black Magic & Evil Eye by Ruqya Ash-Sharya (Islamic Method)Document163 pagesCure Black Magic & Evil Eye by Ruqya Ash-Sharya (Islamic Method)Roohani786100% (9)
- J of Inher Metab Disea 2023 Spiekerkoetter Genomic Newborn Screening Are We Entering A New Era of ScreeningDocument18 pagesJ of Inher Metab Disea 2023 Spiekerkoetter Genomic Newborn Screening Are We Entering A New Era of ScreeningMarianne Angela CortezNo ratings yet
- 11 - Infant NutritionDocument33 pages11 - Infant NutritionEmad MashaalNo ratings yet
- PICU Protocol FINALDocument120 pagesPICU Protocol FINALwalaa mousaNo ratings yet
- Guidelines For Treatment of Septic Shock in ResourDocument21 pagesGuidelines For Treatment of Septic Shock in ResourdintaboiceNo ratings yet
- Neonatal JaundiceDocument3 pagesNeonatal JaundiceMohola Tebello GriffithNo ratings yet
- Hidrosefalus KongenitalDocument8 pagesHidrosefalus KongenitalSebastiano SegaNo ratings yet
- BMC Pediatrics: Management of Neonatal Hyperbilirubinemia: Pediatricians' Practices and Educational NeedsDocument7 pagesBMC Pediatrics: Management of Neonatal Hyperbilirubinemia: Pediatricians' Practices and Educational Needsmaya maeNo ratings yet
- Mechanical Ventilation Guidelines SNSDocument8 pagesMechanical Ventilation Guidelines SNSClaudia KosztelnikNo ratings yet
- Egyptian Neonatology Protocol 1st Ed 2022Document124 pagesEgyptian Neonatology Protocol 1st Ed 2022sherif ghazyNo ratings yet
- Ozdamire 2017organismesDocument7 pagesOzdamire 2017organismesFatma ElzaytNo ratings yet
- Original Research Article: ISSN: 2230-9926Document7 pagesOriginal Research Article: ISSN: 2230-9926Fatma ElzaytNo ratings yet
- The Diagnosis of Scabies by Non-Expert Examiners: A Study of Diagnostic AccuracyDocument13 pagesThe Diagnosis of Scabies by Non-Expert Examiners: A Study of Diagnostic AccuracyAnisa Rifkia ZSNo ratings yet
- Technology-Dependent Children: International Journal of Pediatrics and Adolescent MedicineDocument6 pagesTechnology-Dependent Children: International Journal of Pediatrics and Adolescent MedicinecharoleNo ratings yet
- Developing A Neonatal Unit Ventilation Protocol For The Preterm BabyDocument6 pagesDeveloping A Neonatal Unit Ventilation Protocol For The Preterm BabyMALIK MANASRAHNo ratings yet
- Ihz 009Document9 pagesIhz 009Abie SultanNo ratings yet
- COVID-19 Vaccine Uptake and Hesitancy Among Pregnant and Lactating Women in Saudi ArabiaDocument17 pagesCOVID-19 Vaccine Uptake and Hesitancy Among Pregnant and Lactating Women in Saudi ArabiaNormanNo ratings yet
- Bedside (Pediatrics)Document289 pagesBedside (Pediatrics)tajfaiz779No ratings yet
- JFamCommunityMed262113-1349692 034456Document5 pagesJFamCommunityMed262113-1349692 034456Putri Zatalini SabilaNo ratings yet
- Ihac 077Document7 pagesIhac 077CONSTANTIUS AUGUSTONo ratings yet
- Guidiline SdraDocument19 pagesGuidiline SdraLariza CostaNo ratings yet
- Nac y AntibióticosDocument7 pagesNac y AntibióticosRoberto MorenoNo ratings yet
- Jurnal d2d 1bDocument9 pagesJurnal d2d 1bTephii DoankkzzNo ratings yet
- Peritonitis in Children On Peritoneal Dialysis: 12 Years of Tertiary Center ExperienceDocument7 pagesPeritonitis in Children On Peritoneal Dialysis: 12 Years of Tertiary Center ExperienceMarselya GaniNo ratings yet
- FasdfyDocument8 pagesFasdfyzuliamNo ratings yet
- Experiences With Neonatal Jaundice Management in Hospitals and The Community: Interviews With Australian Health ProfessionalsDocument9 pagesExperiences With Neonatal Jaundice Management in Hospitals and The Community: Interviews With Australian Health Professionalsstardust.m002No ratings yet
- Jaundice 20 PDFDocument54 pagesJaundice 20 PDFHaziq KamardinNo ratings yet
- Consenso de Sindroe de Dificultad Respiratoria en NeonataosDocument19 pagesConsenso de Sindroe de Dificultad Respiratoria en NeonataosSayonara Mordagon ChoqueticllaNo ratings yet
- JurnalDocument7 pagesJurnalskocabzzNo ratings yet
- Outcomes of Single-Dose Empirical Antibiotic Treatment in Children With Suspected Sepsis Implemented in The Emergency DepartmentDocument5 pagesOutcomes of Single-Dose Empirical Antibiotic Treatment in Children With Suspected Sepsis Implemented in The Emergency Departmentaldo saadot garcia ortizNo ratings yet
- Management Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaDocument4 pagesManagement Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Study of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreDocument11 pagesStudy of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jurnal Hiperbilirubin 2Document3 pagesJurnal Hiperbilirubin 2Seni safitriNo ratings yet
- Pharmaceutics 13 00140Document20 pagesPharmaceutics 13 00140bhavanaparabNo ratings yet
- Zahrotunisa Yuwana (Kritik Jurnal)Document10 pagesZahrotunisa Yuwana (Kritik Jurnal)ZahroNo ratings yet
- Clinical Profile of Fungal Sepsis in New Born: A Tertiary Centre Experience From BangladeshDocument4 pagesClinical Profile of Fungal Sepsis in New Born: A Tertiary Centre Experience From BangladeshPhilippe Ceasar C. BascoNo ratings yet
- Inter-Grader Agreement in The Diabetic Retinopathy Screening Program in Palestine-IJMBS-2018.Document6 pagesInter-Grader Agreement in The Diabetic Retinopathy Screening Program in Palestine-IJMBS-2018.Riyad BanayotNo ratings yet
- 219neonatal ExaminationDocument6 pages219neonatal Examinationsam2000samNo ratings yet
- Israeli Et Al 2021 Clinical Efficacy of Topical Nasal Pomegranate Fruit Extract For Chronic Rhinitis and ChronicDocument10 pagesIsraeli Et Al 2021 Clinical Efficacy of Topical Nasal Pomegranate Fruit Extract For Chronic Rhinitis and ChronicShelin AmandaNo ratings yet
- Efficacy of Table Salt As A Treatment Option For Umbilical Granuloma in InfantsDocument5 pagesEfficacy of Table Salt As A Treatment Option For Umbilical Granuloma in InfantsajmrdNo ratings yet
- 1 s2.0 S2666535220300057 MainDocument8 pages1 s2.0 S2666535220300057 MainSensi Tresna AdilahNo ratings yet
- Part 5: Neonatal ResuscitationDocument30 pagesPart 5: Neonatal ResuscitationAngela Giselle Garcia RuizNo ratings yet
- Journal Pediatric Shock BaruDocument6 pagesJournal Pediatric Shock BaruHhhNo ratings yet
- Health Science Reports - 2022 - SeyedAlinaghi - Impact of COVID 19 Pandemic On Routine Vaccination Coverage of Children andDocument12 pagesHealth Science Reports - 2022 - SeyedAlinaghi - Impact of COVID 19 Pandemic On Routine Vaccination Coverage of Children andArumm88No ratings yet
- Factors Associated With Complicated Pneumonia in ChildrenDocument19 pagesFactors Associated With Complicated Pneumonia in ChildrenJHONATAN MATA ARANDANo ratings yet
- 2018 Year in Review in Critical CareDocument5 pages2018 Year in Review in Critical CareRs ArNo ratings yet
- Immunization Manual For Medical and Nursing Students - Final Smaller PDFDocument296 pagesImmunization Manual For Medical and Nursing Students - Final Smaller PDFamit100% (3)
- NAC en NiñosDocument14 pagesNAC en NiñosAnonymous DxJyWJwtNo ratings yet
- CAP in Children - IDSADocument52 pagesCAP in Children - IDSAlala liliNo ratings yet
- Neonatal Jaundice RDocument19 pagesNeonatal Jaundice REssam HassanNo ratings yet
- Assessment of The Awareness, Perception, Attitudes, and Preparedness of Health-Care Professionals Potentially Exposed To COVID-19 in The United Arab EmiratesDocument12 pagesAssessment of The Awareness, Perception, Attitudes, and Preparedness of Health-Care Professionals Potentially Exposed To COVID-19 in The United Arab EmiratesSarah SanadNo ratings yet
- Disease KnowledgeDocument6 pagesDisease KnowledgeJaved IqbalNo ratings yet
- Urinary Tract Infection in Children - A Narrative Review of Clinical Practice GuidelinesDocument20 pagesUrinary Tract Infection in Children - A Narrative Review of Clinical Practice GuidelinesJad DegheiliNo ratings yet
- Bharath A PDocument103 pagesBharath A PSuman MondalNo ratings yet
- Antimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaDocument9 pagesAntimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaBima RizkiNo ratings yet
- Part 5: Neonatal ResuscitationDocument30 pagesPart 5: Neonatal ResuscitationFandoko ChaniagoNo ratings yet
- Aynalem 2020@journal - Pone.0235544Document14 pagesAynalem 2020@journal - Pone.0235544Huệ MinhNo ratings yet
- Pneumonia in Infants and ChildrenDocument52 pagesPneumonia in Infants and ChildrenMikeyNo ratings yet
- Fpubh 10 881296Document12 pagesFpubh 10 881296Bekalu EndaleNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- Advances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and DiagnosticsFrom EverandAdvances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and DiagnosticsSidharth Kumar SethiNo ratings yet
- Chapter IiDocument3 pagesChapter IiTupas Alpiche Lyka SheherezadeNo ratings yet
- Mountains Beyond Mountains EssayDocument7 pagesMountains Beyond Mountains EssayKaliyah MartinNo ratings yet
- Requirements Before Issuance of Sanitary Permit: For Food EstablishmentsDocument4 pagesRequirements Before Issuance of Sanitary Permit: For Food EstablishmentsSheryl MH-PradaNo ratings yet
- Weekly Activity Report: Number of AttendeesDocument7 pagesWeekly Activity Report: Number of AttendeestabilinNo ratings yet
- Disease PredictionDocument111 pagesDisease PredictionSahabaj AlamNo ratings yet
- VAC Form 1Document1 pageVAC Form 1Angela TabudlongNo ratings yet
- EnterobiasisDocument5 pagesEnterobiasiszairaconcoNo ratings yet
- Textbook Ebook Textbook of Small Animal Emergency Medicine 1St Edition PDF All Chapter PDFDocument43 pagesTextbook Ebook Textbook of Small Animal Emergency Medicine 1St Edition PDF All Chapter PDFlue.ring158100% (6)
- Ungs 2050Document2 pagesUngs 2050Fazdrul AkiffNo ratings yet
- Argumentative EssayDocument7 pagesArgumentative EssaynemoviNo ratings yet
- Palmoplantar Hyperhidrosis: A Therapeutic ChallengeDocument4 pagesPalmoplantar Hyperhidrosis: A Therapeutic ChallengeWesley DornelasNo ratings yet
- Psychedelics, Technology, Psychedelics: Bernard S. Aaronson and Humphrey OsmondDocument8 pagesPsychedelics, Technology, Psychedelics: Bernard S. Aaronson and Humphrey OsmondJuan ScuroNo ratings yet
- A Feasibility Randomised Control Trial of Individual Cognitive Stimulation Therapy For Dementia Impact On Cognition Quality of Life and PositiveDocument10 pagesA Feasibility Randomised Control Trial of Individual Cognitive Stimulation Therapy For Dementia Impact On Cognition Quality of Life and Positivemadalena limaNo ratings yet
- ACCREDITED PROFESSIONAL ORGANIZATIONS (APOs) and ACCREDITED INTEGRATED PROFESSIONAL ORGANIZATIONS (AIPOs) As of March 4 2021Document7 pagesACCREDITED PROFESSIONAL ORGANIZATIONS (APOs) and ACCREDITED INTEGRATED PROFESSIONAL ORGANIZATIONS (AIPOs) As of March 4 2021ChinoNo ratings yet
- Prevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDDocument7 pagesPrevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDMusainah FeisalNo ratings yet
- Anglican Girls Letter March 30 2021Document4 pagesAnglican Girls Letter March 30 2021Ebele AbrahamNo ratings yet
- 5 (Jeremy Stranks) Health and Safety Pocket BookDocument10 pages5 (Jeremy Stranks) Health and Safety Pocket BookTuralNo ratings yet
- Mindfulness For Exams by Ashley LodgeDocument2 pagesMindfulness For Exams by Ashley Lodgepetit_19794618No ratings yet
- ProstataDocument26 pagesProstatasidney souzaNo ratings yet
- The Question of Sex Education in SchoolsDocument2 pagesThe Question of Sex Education in SchoolsPhoebe FranciscoNo ratings yet
- 50K Training PlanDocument2 pages50K Training PlanStephen RoemerNo ratings yet
- Risk Assessment MatrixDocument2 pagesRisk Assessment MatrixjulcemarfelipeNo ratings yet
- NCP Spiritual DistressDocument3 pagesNCP Spiritual DistressAngelo ArabejoNo ratings yet
- Binge Anxiety Killer Cheat Sheet: InstructionsDocument4 pagesBinge Anxiety Killer Cheat Sheet: Instructionsdoppler_No ratings yet
- Ensuring Patient Comfort and Clinical Accuracy During Impression Taking 3Document11 pagesEnsuring Patient Comfort and Clinical Accuracy During Impression Taking 3Raul HernandezNo ratings yet
- Activity Checklist Lecture 240307 110843Document76 pagesActivity Checklist Lecture 240307 110843ALI-A ALINo ratings yet
- Understanding Communication and ConsentDocument24 pagesUnderstanding Communication and ConsentCHRIS FLYNNNo ratings yet
- Summary Barang Masuk Dan Keluar: Nama Item Kategori Item Kode ItemDocument204 pagesSummary Barang Masuk Dan Keluar: Nama Item Kategori Item Kode ItemTitha RahmiNo ratings yet
- Larvicidal Activity of Anacardium Occidental Against Aedes Aegypti FINALDocument5 pagesLarvicidal Activity of Anacardium Occidental Against Aedes Aegypti FINALVernice OrtegaNo ratings yet