Professional Documents
Culture Documents
Kelompok 4
Kelompok 4
Uploaded by
TaraaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kelompok 4
Kelompok 4
Uploaded by
TaraaCopyright:
Available Formats
TYPE Original Research
PUBLISHED 13 November 2023
DOI 10.3389/fphar.2023.1291896
Safety profile of intravenous
OPEN ACCESS digoxin in Chinese patients with
EDITED BY
Piero Pollesello,
Orion Corporation, Finland
acute heart failure with reduced
REVIEWED BY
Jouko Levijoki,
ejection fraction: a small-scale
Orion Corporation, Finland
Antonio Lax,
University of Murcia, Spain
prospective cohort study
*CORRESPONDENCE
Gangcheng Zhang, Xintian Liu 1,2†, Haojie Zhang 1†, Wenlin Cheng 2, Qingkun Fan 3,
zgc-wh@outlook.com
Xuan Zheng,
Zhibing Lu 2, Xuan Zheng 1* and Gangcheng Zhang 1*
xuanzheng@whu.edu.cn 1
Center of Structural Heart Disease, Zhongnan Hospital of Wuhan University, Wuhan, China, 2Department
†
These authors have contributed equally of Cardiology, Zhongnan Hospital of Wuhan University, Wuhan, China, 3Laboratory Medicine, Wuhan Asia
to this work Heart Hospital, Wuhan University of Science and Technology, Wuhan, China
RECEIVED 10 September 2023
ACCEPTED 25 October 2023
PUBLISHED 13 November 2023
CITATION
Background: Adverse effects of intravenous digoxin vary from patients and
Liu X, Zhang H, Cheng W, Fan Q, Lu Z, disease status, which should be closely monitored.
Zheng X and Zhang G (2023), Safety
profile of intravenous digoxin in Chinese Aims: To explore the safety profile of intravenous digoxin in acute heart failure with
patients with acute heart failure with reduced ejection fraction (HFrEF) among Chinese patients.
reduced ejection fraction: a small-scale
prospective cohort study. Methods: A clinical prospective, single-center, single-arm, open-label exploratory
Front. Pharmacol. 14:1291896.
doi: 10.3389/fphar.2023.1291896
clinical trial was performed in patients with acute HFrEF at Wuhan Asia Heart
Hospital. A fixed dose of 0.5 mg digoxin was used intravenously once per day for
COPYRIGHT
© 2023 Liu, Zhang, Cheng, Fan, Lu, Zheng 3 days. The normalized dosage of digoxin (NDD), toxic serum digoxin
and Zhang. This is an open-access article concentration (SDC), and adverse reactions of intravenous digoxin were recorded.
distributed under the terms of the
Creative Commons Attribution License Results: A total of 40 patients were recruited in the study. The SDC increased from
(CC BY). The use, distribution or 1.03 ± 0.34 ng/mL to 1.95 ± 0.52 ng/mL during treatment. 50% (20/40) patients
reproduction in other forums is
permitted, provided the original author(s) reached a toxic SDC of 2.0 ng/mL, and toxic effects were seen in 30% (12/40)
and the copyright owner(s) are credited patients. Estimated glomerular filtration rate (eGFR) < 60 mL/min [HR: 5.269; 95%
and that the original publication in this CI: 1.905–14.575, p = 0.001], NDD ≥7 μg/kg [HR: 3.028; 95% CI: 1.119–8.194, p =
journal is cited, in accordance with
accepted academic practice. No use, 0.029], and ischemic cardiomyopathy [HR: 2.658; 95% CI: 1.025–6.894, p =
distribution or reproduction is permitted 0.044] were independent risk factors for toxic SDC. Toxic SDC was effectively
which does not comply with these terms. identified [area under the receiver operating characteristic (ROC) curve = 0.85, p <
0.001] using this model, and patients would have a higher risk of toxicity with more
risk factors.
Conclusion: Intravenous digoxin of 0.5 mg was safe and effective for initial dose
but not suitable for maintenance treatment in Chinese patients with acute HFrEF.
Patients who had lower eGFR, received higher NDD, and had ischemic
cardiomyopathy should be closely monitored to avoid digoxin toxicity.
KEYWORDS
acute heart failure with reduced ejection fraction, intravenous digoxin, digoxin toxicity,
serum digoxin concentration (SDC), safety evaluation
Frontiers in Pharmacology 01 frontiersin.org
Liu et al. 10.3389/fphar.2023.1291896
Introduction Research protocol
Digoxin has been known as the only inotropic medicine that This was a clinical prospective, single-center, single-arm, open-
slows the heart rate while strengthening cardiac contractility for label exploratory clinical trial. The half-life of digoxin was 36 h, and
patients with heart failure (Digitalis Investigation Group, 1997). the concentration gradually increased during daily application.
However, the broad spectrum of toxicity effects from mild sight Therefore, we adopted a continuously daily intravenous fixed-
change to fatal arrhythmias raises concerns during clinical dose (0.5 mg) 3-day treatment approach given on day 0, day
application (Adams et al., 2002; Flory et al., 2012; Grześk et al., 1 and day 2. The intravenous digoxin (Southwest Pharmaceutical
2018; Kapelios et al., 2022). The pharmacokinetics of digoxin is Co., Ltd) of 0.5 mg was diluted to 10 mL with normal saline and
affected by multiple factors such as age, gender, renal function, and pumping at a rate of 1 mL/min. Digoxin levels were measured before
complications. Therefore, debates on digoxin safety and effects the dose of intravenous digoxin were given on day 0, day 1 and day
regarding the narrow therapeutic window, serum digoxin 2 as well as measured on day 3 around 24 h after the last dose was
concentration (SDC) of 0.8–2.0 ng/mL, are held in different given. SDC >2.0 ng/mL was set as a cut-off value of toxic SDC to
subgroups (Gona et al., 2023). stop the subsequent administration due to the increasing chance of
Many drugs have shown different pharmacokinetics in Chinese digoxin toxicity at maximum therapeutic concentration. Other
patients because of their different clinical characteristics including treatments were applied in accordance with illness conditions
low body weight and many complications. Intravenous digoxin is and guidelines. Toxicity effects were defined as follows: (I)
more often used in patients with acute heart failure because of its fast arrhythmia: atrioventricular blockade, bradycardia, ventricular
working, which also increases the risk of having toxicity effects. arrhythmias; (II) gastrointestinal symptoms: anorexia, nausea,
Since Chinese patients started intravenous digoxin treatment since vomiting, diarrhea, abdominal pain; (III) visual abnormality:
late of 2019, neither optimal therapeutic SDC range nor toxic SDC is blurred vision, yellow vision, green vision; and (IV) nervous
well studied. Whether the current dose recommendations and safety system symptoms: headache, dizziness, insomnia, lethargy,
evaluations can be applied among Chinese patients remains unclear. delirium. Severe adverse effects were defined as follows: persistent
Furthermore, acute heart failure with reduced ejection fraction ventricular tachycardia, ventricular fibrillation, severe bradycardia
(HFrEF) is critical and often accompanied by multiple-organ (heart rate <40 beats/min), and the use of temporary pacemakers.
dysfunction. The issue of how to use digoxin safely and reduce
the occurrence of digoxin toxicity among Chinese patients with
acute HFrEF is particularly important. Data collection
Here, we sought to investigate the optimal intravenous digoxin
dose as well as the safety profile in the setting of acute HFrEF among Baseline clinical characteristics of the enrolled patients were
Chinese patients. We also explore the underlying risk factors collected, including age, sex, weight, atrial fibrillation, HFrEF
predicting toxic SDC of digoxin. etiology, New York Heart Association (NYHA) functional class,
vital signs on admission, echocardiography, renal function, and
N-terminal pro B-type natriuretic peptide (NT-proBNP).
Methods Medicines related to heart failure, and non-pharmaceutical
therapies, including percutaneous coronary intervention, non-
Subjects invasive positive pressure ventilation, intra-aortic balloon pump,
radiofrequency catheter ablation for atrial fibrillation, implantable
Patients with acute HFrEF at the Critical Care Center (CCU) of cardioverter defibrillator, as well as cardiac resynchronization
Wuhan Asia Heart Hospital were consecutively enrolled in this therapy, were also collected on admission. SDC, electrolytes
study from July to October 2022. To be eligible for inclusion, the (potassium, sodium, magnesium, and chlorine),
patients had to meet the following criteria: (I) aged between 18 and electrocardiogram (heart rate, PR interval, QRS duration, and
90 years; (II) with body weight ≥50 kg; (III) presenting with acute QTc interval), and adverse effects were monitored daily during
HFrEF; (IV) estimated glomerular filtration rate (eGFR) ≥ 30 mL/ the study.
min; and (V) baseline SDC <0.5 ng/mL. Patients were excluded if
they met any of the following criteria: (I) having a contraindication
for digoxin, such as abnormal blood potassium level, hypertrophic Statistical analysis
cardiomyopathy, aortic stenosis, intracardiac thrombosis, pre-
excitation syndrome, acute myocardial infarction, The normally distributed data are expressed as the mean ±
bradyarrhythmias, ventricular arrhythmia, or thyroid dysfunction; standard deviation. The non-normally distributed data are
(II) receiving invasive mechanical ventilation; (III) with cardiogenic expressed as the median [interquartile range (IQR): Q1, Q3]. The
shock; and/or (IV) having oliguria, anuria, or receiving renal count data are expressed as the number of cases (percentage). Data
replacement therapy. were compared with Student’s t-test or Wilcoxon signed-rank test
This study was approved by the Ethics Committee of Wuhan for continuous variables depending on the normality of their
Asia Heart Hospital (No. 2023-YXKY-P004) and was conducted in distributions. Cox regression analysis was performed to
accordance with the principles described in the Declaration of investigate the association between relevant risk factors and toxic
Helsinki. Written informed consent was obtained from all SDC. The Kaplan-Meier survival curve was used to illustrate the
participants. dynamic change of SDC in patients with different numbers of
Frontiers in Pharmacology 02 frontiersin.org
Liu et al. 10.3389/fphar.2023.1291896
independent risk factors. The statistical analysis was performed TABLE 1 Baseline characteristics of Chinese patients with acute HFrEF enrolled
in this study (n = 40).
using GraphPad Prism 9.0 (GraphPad, La Jolla, CA,
United States). A p-value <0.05 was considered to be statistically Index Results
significant.
Age (years) 64.1 ± 13.6
Sex, n (%)
Results Male 27 (67.5)
Characteristics of the enrolled patients Female 13 (32.5)
Weight (kg) 68.2 ± 9.6
The baseline characteristics of the 40 patients with acute HFrEF
Atrial fibrillation, n (%) 25 (62.5)
are shown in Table 1. The mean age of patients was 64.1 ± 13.6 years,
67.5% of whom were male. 62.5% of the patients presented with The cause of HFrEF, n (%)
atrial fibrillation on admission. 75% had severe impairment on heart
Dilated cardiomyopathy 20 (50.0)
function at admission, as evident by elevated heart rate, increased
left ventricular diameter, reduced ejection fraction, and elevated NT- Ischemic cardiomyopathy 20 (50.0)
proBNP. Notably, the eGFR in more than 90% of patients NYHA functional class, n (%)
was <90 mL/min (37/40, 92.5%), and nearly half of these patients
Level III 10 (25.0)
had an eGFR <60 mL/min.
Level IV 30 (75.0)
Vital signs on admission
SDC trends
Heart rate (counts per minute) 102.2 ± 29.2
The normalized digoxin dose (NDD) was used to assess the Systolic pressure (mmHg) 132.2 ± 26.9
intravenous dosage, which was calculated as the intravenous
Diastolic blood pressure (mmHg) 81.5 ± 16.6
digoxin application dose divided by body weight. With the
application of 0.5 mg intravenous digoxin, mean NDD was Echocardiogram
7.2 ± 1.5 μg/kg (range: 4.2–9.8 μg/kg). The baseline SDC was
Left ventricular end-diastolic diameter (cm) 6.5 ± 0.7
0.27 ± 0.11 ng/mL. The SDC continuously increased as the daily
administration of fixed-dose intravenous digoxin (Figure 1A). Six EF (%) 27.1 ± 6.4
(15%) patients had a SDC >2.0 ng/mL on the second day, thus the Albumin (g/L) 37.8 ± 3.3
subsequent third dosage was not administered. The remaining
eGFR (mL/min) 63.1 ± 19.4
patients (34/40, 85%) continued their treatment, and their SDC
reached 1.96 ± 0.52 ng/mL on the third day. 41.7% (14/34) of eGFR grouping, n (%)
patients who completed 3-day treatment had a SDC >2.0 ng/ml. As
30–59 mL/min 18 (45.0)
shown in Figure 1B, a total of 20 patients had toxic SDC (>2.0 ng/
mL). However, all toxic SDC were reduced to below 2.0 ng/mL 60–89 mL/min 19 (47.5)
after drug withdrawal for 24 h. ≥90 mL/min 2 (5.0)
≥120 mL/min 1 (2.5)
Risk factors for toxic SDC NT-proBNP (pg/mL) 5,445 (2,227–7,561)
The data are expressed as the mean ± standard deviation, quantity (percentage), or median
Table 2 showed Cox analysis of risk factors for toxic SDC which (interquartile range). HFrEF, heart failure with reduced ejection fraction; NYHA, new york
heart association; eGFR, estimation of glomerular filtration rate; EF, ejection fraction; NT-
was defined as SDC >2.0 ng/mL in our study. Among the factors,
proBNP, amino-terminal brain natriuretic peptide precursor.
body weight was a protective factor to reduce the risk of reaching
toxic SDC. In the multivariate analysis, ischemic cardiomyopathy, a
NDD ≥7 μg/kg, and an eGFR <60 mL/min significantly increased Toxicity effects and outcomes
the risk of accumulation of SDC by 2 to 5 folds separately (Figures
2A–C). Using this multi-factor model, toxic SDC would be A total of 22 adverse reactions in 12 patients were observed
effectively identified [area under the receiver operating during the study, including 5 nausea and vomiting, 2 abdominal
characteristic (ROC) curve = 0.85, p < 0.001, Figure 2D]. pain, 2 delirium, 4 frequent premature ventricular beats, 4 short
Furthermore, the K-M curve showed that the risk for toxic SDC ventricular tachycardia, 4 bradycardia, 1 rash. No severe adverse
increased gradually as the number of independent risk factors effects such as persistent ventricular tachycardia, ventricular
increased (Figure 3A). Patients with 3 risk factors had nearly fibrillation, severe bradycardia, and the use of temporary
5 folds higher risk of reaching toxic SDC in the third day of pacemakers were recorded.
application (Figure 3B, log-rank = 18.23, p < 0.001). Patients showed significantly improvement at the end of the
Interestingly, the first dosage of intravenous digoxin would not study. The heart rates reduced from 98 ± 23 to 78 ± 18 beats/min
introduce toxic SDC regardless of their baselines. (p < 0.001). The trends of electrocardiogram parameters (heart rates,
Frontiers in Pharmacology 03 frontiersin.org
Liu et al. 10.3389/fphar.2023.1291896
FIGURE 1
The SDC change and accumulative percent of toxic SDC. (A) The SDC in the patients treated with digoxin at an intravenous dose of 0.5 mg daily at
the indicated time (0, 1, and 2 days). The cut-off line (dash line) indicated for SDC >2.0 ng/mL. (B) The accumulative percentage of toxic SDC. SDC, serum
digoxin concentration.
TABLE 2 Risk factors of toxic SDC (Cox regression analysis).
Variables Univariate Multivariate
HR 95% CI P HR 95% CI P
Age (years) 1.046 1.005–1.088 0.026
Sex
Female 3.937 1.618–9.582 0.003
Male 1.000
Weight (kg) 0.965 0.939–0.998 0.047
HFrEF etiology
Ischemic cardiomyopathy 2.018 1.005–5.059 0.034 2.658 1.025–6.894 0.044
Dilated cardiomyopathy 1.000
eGFR
<60 mL/min 3.478 1.335–9.065 0.001 5.269 1.905–14.575 0.001
≥60 mL/min 1.000
NT-proBNP(10 (Flory et al., 2012) pg/mL) 1.084 1.028–1.114 0.003
Normalized digoxin dose
≥7 μg/kg 2.201 1.045–5.732 0.016 3.028 1.119–8.194 0.029
<7 μg/kg 1.000
Normalized digoxin dose was calculated by digoxin application dose divided by body weight. SDC, serum digoxin concentration; HFrEF, heart failure with reduced ejection fraction; eGFR,
estimation of glomerular filtration rate; NT-proBNP, amino-terminal brain natriuretic peptide precursor; HR, hazards ratio; CI, confidence interval.
PR interval, QRS duration, and QTc interval) and parameters in the Discussion
electrolytes were listed in Supplementary Figures S1, S2, respectively.
NT-proBNP was significantly lower than those at the baseline [5,445 The current study demonstrated the following important
(2,277–7,561) vs 2,193 (854–5,108) pg/mL, p < 0.001]. The median findings: (I) after the administration of the fixed dosage of
length of hospitalization for the enrolled patients was 9 [6–12] days. intravenous digoxin (0.5 mg/day) for 3 consecutive days, the SDC
The major treatments except digoxin based on clinical condition of the Chinese patients with acute HFrEF gradually increased from
were listed in Supplementary Table S1. 1.02 to 1.96 ng/mL. The percentage of patients in whom the
Frontiers in Pharmacology 04 frontiersin.org
Liu et al. 10.3389/fphar.2023.1291896
FIGURE 2
Dynamic changes of SDC with different risk factors. (A) The SDC in patients with an eGFR over or below 60 mL/min; (B) the SDC in patients received
digoxin at a dose over or below 7 μg/kg; (C) the SDC in patients diagnosed with dilated cardiomyopathy or ischemic cardiomyopathy; (D) the ROC curve
of toxic SDC predicted by the number of independent risk factors. The area under the ROC curve was 0.85, p < 0.001. *, p < 0.05. SDC, serum digoxin
concentration; eGFR, estimation of glomerular filtration rate; ROC curve, receiver operating characteristic curve.
SDC >2.0 ng/mL increased with time; (II) the eGFR, NDD, and HFrEF to avoid toxicity while achieving the possible therapeutic
ischemic cardiomyopathy were the 3 important independent risk level for heart failure management.
factors that associated with toxic SDC. The hazard ratios of the toxic A maintenance dosage of 0.125–0.5 mg regardless of individual
SDC in the patients with an eGFR <60 mL/min, NDD ≥7 μg/kg, and differences is suggested to achieve the treatment effects while
ischemic cardiomyopathy were 5.269, 3.028, and 2.658, respectively; avoiding digoxin toxicity. Our study showed that 50% of patients
and (III) the risk of toxic SDC was higher in those whom with more had relatively safe SDC while the others had a toxic SDC during
risk factors as SDC increased rapidly. digoxin administration. To investigate the underlying factors
In previous studies and guidelines, the loading digoxin dose of causing this phenomenon, a Cox regression analysis was
10 μg/kg is recommended and can be added up to 1.0 mg or even performed, and the results showed that an eGFR <60 mL/min,
1.5 mg in total (Adams et al., 2002; McDonagh et al., 2021). NDD ≥7 μg/kg, and ischemic cardiomyopathy were independent
However, 15% or 50% patients reached toxic SDC with the risk factors associated with toxic SDC.
accumulation of 1.0 or 1.5 mg in total after treating for 2 or It is well documented that renal insufficiency affects digoxin
3 days in our study. We also found the SDC was maintained concentration (Flory et al., 2012; Pawlosky et al., 2013; Sc et al., 2017;
under 2.0 ng/mL when using 0.5 mg of intravenous digoxin as Bavendiek et al., 2023). In the current study, more than 90% of the
loading dose. In fact, the recommended digoxin level for patients with acute HFrEF had an eGFR <90 mL/min, and nearly
management of chronic heart failure was 0.5–1.0 ng/mL (Hunt half of the patients had an eGFR <60 mL/min. Thus, attention needs
et al., 2009), and in the present study about 1.0 ng/mL can be to be paid to renal function to prevent the administration of
achieved by one single loading dose of intravenous 0.5 mg digoxin. excessive doses of digoxin. Myocardial ischemia is another reason
Therefore, a lower loading dose of intravenous digoxin, 0.5 mg in affecting SDC. Myocardial ischemia inhibits activation of Na+-K+
our study, would be suggested for Chinese patients with acute ATPase in the cell membrane, which promotes the accumulation of
Frontiers in Pharmacology 05 frontiersin.org
Liu et al. 10.3389/fphar.2023.1291896
FIGURE 3
The positive association between the risk factors and SDC. (A) The change of SDC with different number of risk factors. The dashed line parallel to the
horizontal axis (2.0 ng/mL) indicated for toxic SDC; (B) the risk of toxic SDC based on different number of risk factors. Overall difference between groups
log-rank = 18.23, p < 0.001. SDC, serum digoxin concentration.
digoxin in myocardial cells and causes toxicity (Rogers et al., 2010; effects (Gona et al., 2023). Although we observed the highest SDC in
Ambrosy et al., 2018; McDonagh et al., 2021). Our study showed our study was 2.01 ± 0.52 ng/mL, it is unnecessary to maintain such
that the chance of SDC accumulation and the risk of reaching toxic a high concentration of digoxin in daily clinical practice.
SDC increased significantly as the number of independent risk There are some limitations in our study. First, because of the
factors increased. The SDC was maintained at a safe level for small sample size, these factors appear to be a little too large to be
those who had no risk factors, even when the accumulative included in the regression analysis (Vittinghoff and McCulloch,
intravenous digoxin reached 1.5 mg after 3-day application. 2007), so the statistical results may not be robust and will need to be
Conversely, all patients with 3 independent risk factors reached supported by a larger sample in the future. Second, the target
toxic SDC after 2 or 3-day application. These results suggest that the population of this study were patients with acute heart failure
more independent risk factors a patient has, the less of digoxin dose with dilated hearts and reduced ejection fraction. It is unclear
should be applied on the basis of the loading dose. Otherwise, the whether the results would also be applicable to patients with
intravenous digoxin could be administered every other day and other types of heart failure. Other types of heart failure should be
adjusted according to the SDC to avoid the risk of digoxin toxicity. included in further study. Third, the following patients were
Notably, we used a fixed-dose application in the present study to excluded from the study: elderly patients aged ≥90 years old,
explore the safety profile of intravenous digoxin. As the results from patients with a low body weight of <50 kg, patients with severe
our study, an intravenous digoxin of 0.5 mg would be suggested as renal failure (i.e., an eGFR <30 mL/min, oliguria, anuria, or renal
the loading dose for similar patients, and the maintenance doses replacement therapy), and critically ill patients (i.e., those in
should be adjusted regarding their risk factors and the SDC cardiogenic shock or those that required invasive mechanical
monitoring results. In this way, the SDC range can be effectively ventilation). Thus, the administration of digoxin in these patients
controlled for even a longer-term therapy, and the risk of digoxin requires further research and digoxin should be administered with
toxicity can be greatly reduced while maintaining the therapeutic caution.
concentration of digoxin.
The application of intravenous digoxin was relatively safe in this
study. The maximum SDC was only 3.06 ng/mL, and the SDC in all Conclusion
the patients in whom having toxic SDC decreased to <2.0 ng/mL
after 24 h of treatment termination. Only a few patients suffered The study shows that intravenous digoxin is safe for clinical
from mild toxicity effects, and no persistent ventricular tachycardia administration under close monitoring. The loading dose of
and severe bradycardia were observed like previous studies reported intravenous digoxin for Chinese patients with acute HFrHF is
(Hornestam et al., 1999; Hood et al., 2004). These findings suggest suggested at 0.5 mg, NDD of 4.2–9.8 μg/kg. The application of
that it is very important to monitor the SDC closely during the digoxin should be with caution in vulnerable patients, who are
administration of intravenous digoxin and observe the clinical female, the elderly, frail, malnourish, hypo- or hyper-kalaemic, renal
manifestations of patients during treatment. It has been dysfunction, and deteriorated cardiac function. Further
recommended to maintain a SDC no more than 1.2 ng/mL consideration should be paid on the NDD, eGFR, and heart
during digoxin application to minimize the incidence of toxicity failure etiology to avoid toxic SDC.
Frontiers in Pharmacology 06 frontiersin.org
Liu et al. 10.3389/fphar.2023.1291896
Data availability statement was supported by grants from Wuhan Municipal Health
Commission Medical Research Project (No. WX21B37).
The raw data supporting the conclusion of this article will be
made available by the authors, without undue reservation.
Acknowledgments
Ethics statement We appreciates all colleagues in Zhongnan hospital of Wuhan
University and Wuhan Asia Heart hospital for their assistance.
The studies involving humans were approved by Ethics
Committee of Wuhan Asia Heart Hospital. The studies were
conducted in accordance with the local legislation and Conflict of interest
institutional requirements. The participants provided their
written informed consent to participate in this study. The authors declare that the research was conducted in the
absence of any commercial or financial relationships that could be
construed as a potential conflict of interest.
Author contributions
XL: Data curation, Formal Analysis, Investigation, Writing–original Publisher’s note
draft. HZ: Data curation, Investigation, Methodology, WC: Investigation,
Methodology, Writing–original draft. QF: Funding acquisition, All claims expressed in this article are solely those of the authors
Investigation, Writing–original draft. ZL: Supervision, Validation, and do not necessarily represent those of their affiliated
Writing–review and editing. XZ: Data curation, Formal Analysis, organizations, or those of the publisher, the editors and the
Investigation, Methodology, Supervision, Validation, Writing–original reviewers. Any product that may be evaluated in this article, or
draft, Writing–review and editing. GZ: Conceptualization, Data claim that may be made by its manufacturer, is not guaranteed or
curation, Formal Analysis, Investigation, Methodology, Project endorsed by the publisher.
administration, Supervision, Validation, Writing–review and editing.
Supplementary material
Funding
The Supplementary Material for this article can be found online
The author(s) declare financial support was received for the at: https://www.frontiersin.org/articles/10.3389/fphar.2023.1291896/
research, authorship, and/or publication of this article. This work full#supplementary-material
References
Adams, K. F., Jr, Gheorghiade, M., Uretsky, B. F., Patterson, J. H., Schwartz, T. A., and controlled study. Digitalis in Acute Atrial Fibrillation (DAAF) Trial Group. Clin.
Young, J. B. (2002). Clinical benefits of low serum digoxin concentrations in heart Cardiol. 22, 96–102. doi:10.1002/clc.4960220208
failure. J. Am. Coll. Cardiol. 39, 946–953. doi:10.1016/s0735-1097(02)01708-4
Hunt, S. A., Abraham, W. T., Chin, M. H., Feldman, A. M., Francis, G. S., Ganiats,
Ambrosy, A. P., Bhatt, A. S., Stebbins, A. L., Wruck, L. M., Fudim, M., Greene, S. J., et al. T. G., et al. (2009). 2009 focused update incorporated into the ACC/AHA
(2018). Prevalent digoxin use and subsequent risk of death or hospitalization in ambulatory 2005 guidelines for the diagnosis and management of heart failure in adults A
heart failure patients with a reduced ejection fraction-Findings from the Heart Failure: a report of the American college of cardiology foundation/American heart association
Controlled Trial Investigating Outcomes of Exercise Training (HF-ACTION) randomized task force on practice guidelines developed in collaboration with the international
controlled trial. Am. Heart J. 199, 97–104. doi:10.1016/j.ahj.2018.02.004 society for heart and lung transplantation. J. Am. Coll. Cardiol. 53, e1–e90. doi:10.
1016/j.jacc.2008.11.013
Bavendiek, U., Großhennig, A., Schwab, J., Berliner, D., Liu, X., Maier, L., et al. (2023).
Simple and safe digitoxin dosing in heart failure based on data from the DIGIT-HF trial. Kapelios, C. J., Lund, L. H., Benson, L., Dahlström, U., Rosano, G. M. C., Hauptman,
Clin. Res. Cardiol. 112 (8), 1096–1107. doi:10.1007/s00392-023-02199-z P. J., et al. (2022). Digoxin use in contemporary heart failure with reduced ejection
fraction: an analysis from the Swedish Heart Failure Registry. Eur. Heart J. Cardiovasc
Digitalis Investigation Group (1997). The effect of digoxin on mortality and
Pharmacother. 8, 756–767. doi:10.1093/ehjcvp/pvab079
morbidity in patients with heart failure. N. Engl. J. Med. 336, 525–533. doi:10.1056/
NEJM199702203360801 McDonagh, T. A., Metra, M., Adamo, M., Gardner, R. S., Baumbach, A., Böhm, M.,
et al. (2021). 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic
Flory, J. H., Ky, B., Haynes, K., M Brunelli, S., Munson, J., Rowan, C., et al. (2012).
heart failure. Eur. Heart J. 42 (36), 3599–3726. doi:10.1093/eurheartj/ehab368
Observational cohort study of the safety of digoxin use in women with heart failure.
BMJ Open 2, e000888. doi:10.1136/bmjopen-2012-000888 Pawlosky, N., Macdonald, E., Patel, R., and Kanji, S. (2013). Evaluation of digoxin
concentration after loading dose in patients with renal dysfunction. Can.
Gona, S. R., Rosenberg, J., Fyffe-Freil, R. C., Kozakiewicz, J. M., and Money, M. E.
J. Hosp. Pharm. 66, 104–109. doi:10.4212/cjhp.v66i2.1232
(2023). Review: failure of current digoxin monitoring for toxicity: new monitoring
recommendations to maintain therapeutic levels for efficacy. Front. Cardiovasc Med. 10, Rogers, N. M., Jones, T. E., and Morris, R. G. (2010). Frequently discordant results
1179892. doi:10.3389/fcvm.2023.1179892 from therapeutic drug monitoring for digoxin: clinical confusion for the prescriber.
Intern. Med. J. 40, 52–56. doi:10.1111/j.1445-5994.2008.01847.x
Grześk, G., Stolarek, W., Kasprzak, M., Krzyżanowski, M., Szadujkis-Szadurska, K.,
Wiciński, M., et al. (2018). Therapeutic drug monitoring of digoxin-20 years of Scotcher, D., Jones, C. R., Galetin, A., and Rostami-Hodjegan, A. (2017). Delineating
experience. Pharmacol. Rep. 70, 184–189. doi:10.1016/j.pharep.2017.08.014 the role of various factors in renal disposition of digoxin through application of
physiologically based kidney model to renal impairment populations. J. Pharmacol.
Hood, W. B., Jr, Dans, A. L., Guyatt, G. H., Jaeschke, R., and McMurray, J. J. V. (2004).
Exp. Ther. 360, 484–495. doi:10.1124/jpet.116.237438
Digitalis for treatment of congestive heart failure in patients in sinus rhythm: a systematic
review and meta-analysis. J. Card. Fail 10, 155–164. doi:10.1016/j.cardfail.2003.12.005 Vittinghoff, E., and McCulloch, C. E. (2007). Relaxing the rule of ten events per
variable in logistic and Cox regression. Am. J. Epidemiol. 165, 710–718. doi:10.1093/aje/
Hornestam, B., Held, P., and Edvardsson, N. (1999). Effects of digoxin on
kwk052
electrocardiogram in patients with acute atrial fibrillation--a randomized, placebo-
Frontiers in Pharmacology 07 frontiersin.org
You might also like
- Taste of Paradise Chapter 2Document16 pagesTaste of Paradise Chapter 2Gisele Ferreira33% (6)
- TK3723+Data+Sheet+v0 23Document89 pagesTK3723+Data+Sheet+v0 23Phong LêNo ratings yet
- Commentary: Digoxin in Chronic Heart Failure: Possibility of A Second Chance?Document3 pagesCommentary: Digoxin in Chronic Heart Failure: Possibility of A Second Chance?Della Puspita SariNo ratings yet
- Intermittent Low Dose Digoxin May Be Effective and Safe in Patients With Chronic Heart Failure Undergoing Maintenance HemodialysisDocument6 pagesIntermittent Low Dose Digoxin May Be Effective and Safe in Patients With Chronic Heart Failure Undergoing Maintenance Hemodialysisdella psNo ratings yet
- Taking The Wrong Medication of Digoxin TabletsDocument3 pagesTaking The Wrong Medication of Digoxin TabletsMarfu'ah Mar'ahNo ratings yet
- Digoxin, MortalityDocument12 pagesDigoxin, MortalityKenWin NguyễnNo ratings yet
- Sethi 2018Document31 pagesSethi 2018Dina saniasihNo ratings yet
- 4 DigoxinDocument9 pages4 DigoxinThảo VươngNo ratings yet
- Dibacakan Oleh:: Achmad Nur Affendick Adriana Wulandari Dionisia I. Madin Ineke Lani Dimara Lis AmitasariDocument39 pagesDibacakan Oleh:: Achmad Nur Affendick Adriana Wulandari Dionisia I. Madin Ineke Lani Dimara Lis AmitasariMc'onethree BrownNo ratings yet
- 5 Ijca - 3 (2) - 316-323Document8 pages5 Ijca - 3 (2) - 316-323Mythology KingdomNo ratings yet
- Use of Digoxin For Heart Failure and Atrial FibrillationDocument9 pagesUse of Digoxin For Heart Failure and Atrial FibrillationeeleeNo ratings yet
- Effectiveness and Outcomes of H-Isdn in Addition To Conventional Therapy in Acute Heart Failure Patients With Renal ImpairmentDocument10 pagesEffectiveness and Outcomes of H-Isdn in Addition To Conventional Therapy in Acute Heart Failure Patients With Renal ImpairmentIJAR JOURNALNo ratings yet
- Use of Dexmedetomidine As A Sedative and Analgesic Agent in Critically Ill Adult Patients: A Meta-AnalysisDocument14 pagesUse of Dexmedetomidine As A Sedative and Analgesic Agent in Critically Ill Adult Patients: A Meta-AnalysisPatty Alarcón ParraNo ratings yet
- Acute Subdural Hematoma in Patients On OralDocument17 pagesAcute Subdural Hematoma in Patients On OralCinDy Advenia SiarNo ratings yet
- Journal Homepage: - : IntroductionDocument9 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- 1 s2.0 S105307702300784X MainDocument7 pages1 s2.0 S105307702300784X MainalfintonNo ratings yet
- Jiang 2022Document9 pagesJiang 2022Olivia LimNo ratings yet
- Bo-Jie Wang, Chun-Jing Li, Jian Hu, Huai-Jin Li, Chao Guo, Zhen-Han Wang, Qiao-Chu Zhang, Dong-Liang Mu, Dong-Xin WangDocument6 pagesBo-Jie Wang, Chun-Jing Li, Jian Hu, Huai-Jin Li, Chao Guo, Zhen-Han Wang, Qiao-Chu Zhang, Dong-Liang Mu, Dong-Xin WangferrevNo ratings yet
- PDFDocument14 pagesPDFJardee DatsimaNo ratings yet
- EBPG Guideline On Haemodynamic InstabilityDocument23 pagesEBPG Guideline On Haemodynamic InstabilityJevon JavierNo ratings yet
- Haloperidol RX Delirium Metaanalysis July 2023Document9 pagesHaloperidol RX Delirium Metaanalysis July 2023Jonty ArputhemNo ratings yet
- Digoxin: The Art and Science: ReviewDocument3 pagesDigoxin: The Art and Science: ReviewVisco Da GamaNo ratings yet
- Jaicm MS Id 555727Document7 pagesJaicm MS Id 555727Mita KerjapyNo ratings yet
- Brain and Behavior - 2020 - Feng - Reduced Thiamine Is A Predictor For Cognitive Impairment of Cerebral InfarctionDocument8 pagesBrain and Behavior - 2020 - Feng - Reduced Thiamine Is A Predictor For Cognitive Impairment of Cerebral InfarctionJasna BuhariNo ratings yet
- Anesth Analg 2019 129 6 1504-11Document8 pagesAnesth Analg 2019 129 6 1504-11Fernando SousaNo ratings yet
- Dex Review 2007Document11 pagesDex Review 2007Jackelyne VilelaNo ratings yet
- Pone 0168582Document22 pagesPone 0168582Hening Tirta KusumawardaniNo ratings yet
- Intranasal Midazolam Versus Intravenous Diazepam For The Treatment of Acute Seizures in Paediatric PatientsDocument5 pagesIntranasal Midazolam Versus Intravenous Diazepam For The Treatment of Acute Seizures in Paediatric PatientsArif KusumawidjayaNo ratings yet
- Digoxin Toxicity: Crucial To Diagnose: International Journal of Basic & Clinical PharmacologyDocument2 pagesDigoxin Toxicity: Crucial To Diagnose: International Journal of Basic & Clinical PharmacologyGima Amezia SariNo ratings yet
- Impact of Postoperative Dexmedetomidine Infusion On Incidence of Delirium in Elderly Patients Undergoing Major Elective Noncardiac Surgery2019Document12 pagesImpact of Postoperative Dexmedetomidine Infusion On Incidence of Delirium in Elderly Patients Undergoing Major Elective Noncardiac Surgery2019Cláudia Regina FernandesNo ratings yet
- Sio Jurnal Pertemuan 1Document9 pagesSio Jurnal Pertemuan 1raudatul jannahNo ratings yet
- Hayashi 2015Document5 pagesHayashi 2015Nur Syamsiah MNo ratings yet
- JurnalDocument8 pagesJurnalzefri suhendarNo ratings yet
- Nihms 666087Document24 pagesNihms 666087SouleymaneNo ratings yet
- Guideline For Stress Ulcer Prophylaxis in The Intensive Care UnitDocument4 pagesGuideline For Stress Ulcer Prophylaxis in The Intensive Care Unitannisa edwarNo ratings yet
- Meyfroidt-Smith2019 Article FocusOnDeliriumSedationAndNeurDocument3 pagesMeyfroidt-Smith2019 Article FocusOnDeliriumSedationAndNeurmedicnanaNo ratings yet
- Monitoreo de DigoxinaDocument13 pagesMonitoreo de DigoxinaWalter ReyesNo ratings yet
- Mechanism Underlying Linezolid-Induced Peripheral Neuropathy in Multidrug-Resistant Tuberculosis 2022Document12 pagesMechanism Underlying Linezolid-Induced Peripheral Neuropathy in Multidrug-Resistant Tuberculosis 2022awaluddin andyNo ratings yet
- Impact of Nitrate Use On Survival in Acute Heart Failure: A Propensity-Matched AnalysisDocument12 pagesImpact of Nitrate Use On Survival in Acute Heart Failure: A Propensity-Matched Analysisagung putraNo ratings yet
- Segunda Entrega InvestigacionDocument2 pagesSegunda Entrega InvestigacionDel Rio LauraNo ratings yet
- Surve Rohini 2016Document7 pagesSurve Rohini 2016Amro MahmoudNo ratings yet
- JurnalDocument10 pagesJurnalZaoldyeck PutriNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument10 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Journal Medicine: The New EnglandDocument9 pagesJournal Medicine: The New Englanddigocivil77No ratings yet
- Harmful Effects of Nsaids Among Patients With Hypertension and Coronary Artery DiseaseDocument7 pagesHarmful Effects of Nsaids Among Patients With Hypertension and Coronary Artery DiseaseFuchsia ZeinNo ratings yet
- Traa 144Document9 pagesTraa 144RashifNo ratings yet
- Evaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryDocument8 pagesEvaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryAudra Firthi Dea NoorafiattyNo ratings yet
- Recognize and Treatment of Digitalis Intoxication: Case ReportDocument6 pagesRecognize and Treatment of Digitalis Intoxication: Case ReportKilroy Vincent SterlingNo ratings yet
- Pathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaDocument7 pagesPathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaIJAR JOURNALNo ratings yet
- JURDING InternaDocument11 pagesJURDING Internadysha hasyaNo ratings yet
- Indian J PharaDocument7 pagesIndian J PharaprabaNo ratings yet
- Dexmedetomidine: An Updated Review: Annals of Pharmacotherapy March 2007Document11 pagesDexmedetomidine: An Updated Review: Annals of Pharmacotherapy March 2007eriza amalia zainNo ratings yet
- Dexmedetomidine: An Updated Review: Annals of Pharmacotherapy March 2007Document11 pagesDexmedetomidine: An Updated Review: Annals of Pharmacotherapy March 2007eriza amalia zainNo ratings yet
- DDDT 14 4695Document7 pagesDDDT 14 4695IvanGómezNo ratings yet
- MeduriDocument4 pagesMeduriSilvia Leticia BrunoNo ratings yet
- Medi 99 E11005Document6 pagesMedi 99 E11005maninagaNo ratings yet
- Jamaneurology - Meinel - 2023 Intravenous Thrombolysis in Patients With Ischemic Stroke and Recent Ingestion of Direct Oral AnticoagulantsDocument11 pagesJamaneurology - Meinel - 2023 Intravenous Thrombolysis in Patients With Ischemic Stroke and Recent Ingestion of Direct Oral AnticoagulantsAna Margarida J. - PsicólogaNo ratings yet
- Rathore SS. Digoxin in Treatment of Heart FailureDocument8 pagesRathore SS. Digoxin in Treatment of Heart FailureDinhLinhNo ratings yet
- DM - Thiazolidinedione Use, Fluid Retention, and Congestive Heart FailureDocument8 pagesDM - Thiazolidinedione Use, Fluid Retention, and Congestive Heart FailureIntan Siti HulaimaNo ratings yet
- Positive Inotropic Drugs and Drugs Used in DysrhythmiasDocument30 pagesPositive Inotropic Drugs and Drugs Used in DysrhythmiasBurnley JenifferNo ratings yet
- Delirium 5Document5 pagesDelirium 5Raja Friska YulandaNo ratings yet
- Infusion Therapy: For Pain, Headache and Related ConditionsFrom EverandInfusion Therapy: For Pain, Headache and Related ConditionsAlaa Abd-ElsayedNo ratings yet
- Swahili LanguageDocument14 pagesSwahili LanguagenedNo ratings yet
- Lesson 3. The Relationship of Percent Composition and Chemical FormulaDocument4 pagesLesson 3. The Relationship of Percent Composition and Chemical FormulaRandel MontielNo ratings yet
- Avascular Necrosis of The Fibular SesamoidDocument7 pagesAvascular Necrosis of The Fibular SesamoidAlex Yvan Escobedo HinostrozaNo ratings yet
- Bersa Arms 2011 CatalogDocument16 pagesBersa Arms 2011 CatalogAmmoLand Shooting Sports News100% (1)
- European Standard Norme Européenne Europäische Norm: Final Draft Fpren 15316-4-5Document30 pagesEuropean Standard Norme Européenne Europäische Norm: Final Draft Fpren 15316-4-5raduvlasaNo ratings yet
- Poultry Anatomy and PhysiologyDocument40 pagesPoultry Anatomy and PhysiologyMamtaNo ratings yet
- KRTB LFLP71.32Document31 pagesKRTB LFLP71.32Ranadheer BNo ratings yet
- Fundamentals of Breathing The Right Way UpdatedDocument25 pagesFundamentals of Breathing The Right Way UpdatedJohnNo ratings yet
- Test Certificate For Vista Superplast Hs 400 Consignee: Dhariwal Buildtech Ltd. Quantity: 22.022 MT Date: 14-12-2022 Batch No.: VK/2022-23/228Document1 pageTest Certificate For Vista Superplast Hs 400 Consignee: Dhariwal Buildtech Ltd. Quantity: 22.022 MT Date: 14-12-2022 Batch No.: VK/2022-23/228Deepak PachauriaNo ratings yet
- Extended Sample Invoice 0001Document1 pageExtended Sample Invoice 0001importvalleNo ratings yet
- Good and Evil of Moby Dick and Captain AhabDocument4 pagesGood and Evil of Moby Dick and Captain AhabCismaru ElenaNo ratings yet
- Exposure: The PhotoreactionDocument16 pagesExposure: The PhotoreactionGeetha ThiruvengadamNo ratings yet
- Si47 1971 Frenic Lift Loader Im WebDocument128 pagesSi47 1971 Frenic Lift Loader Im WebLogic EngineeringNo ratings yet
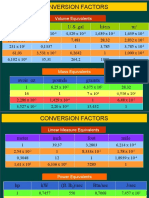
- Conversion Factors: in FT U.S. Gal Liters MDocument8 pagesConversion Factors: in FT U.S. Gal Liters MSamuel MahendraNo ratings yet
- Qualitative Analysis For Active Sulfur Species in Fuels and Solvents (Doctor Test)Document2 pagesQualitative Analysis For Active Sulfur Species in Fuels and Solvents (Doctor Test)Mikael Salamanca100% (1)
- Perfume & Makeup Sale 15.7Document15 pagesPerfume & Makeup Sale 15.7Shane PentonyNo ratings yet
- Surgicals RFQ Fy 2024-25Document225 pagesSurgicals RFQ Fy 2024-25Keshav KumarNo ratings yet
- Avinash Mathematics Project-1 (Edited)Document20 pagesAvinash Mathematics Project-1 (Edited)Harsh SharmaNo ratings yet
- Theology Finals - Grade 11Document7 pagesTheology Finals - Grade 11Sophia BiancaNo ratings yet
- Green Productivity PDFDocument341 pagesGreen Productivity PDFSisca Wiryawan100% (1)
- GY 112 Lecture NotesDocument13 pagesGY 112 Lecture NotesSyed Jabed Miadad AliNo ratings yet
- Bridge Axi AhbDocument22 pagesBridge Axi Ahbkrishnaav100% (1)
- Airport 170923125652Document46 pagesAirport 170923125652Raj GuptaNo ratings yet
- Samsung SH09xWH SH12xWH SERVICE MANUALDocument46 pagesSamsung SH09xWH SH12xWH SERVICE MANUALIoannis Perperis100% (1)
- Practice Test 1: (Code: B1T1)Document16 pagesPractice Test 1: (Code: B1T1)Sách Pháp Hiếu NhânNo ratings yet
- Daniel Dennett-Philosophy Has A Big Role To Play, "If Only It Will Play It" (Prospect)Document3 pagesDaniel Dennett-Philosophy Has A Big Role To Play, "If Only It Will Play It" (Prospect)AidanNo ratings yet
- Heiser - Temperature Charts For Induction and Constant Temperature HeatingDocument10 pagesHeiser - Temperature Charts For Induction and Constant Temperature Heatingsharkdude1134No ratings yet
- Pressurised Mud Cap Drilling Paper (Spe-125311-By Dany)Document7 pagesPressurised Mud Cap Drilling Paper (Spe-125311-By Dany)Hammad KhalidNo ratings yet