Professional Documents
Culture Documents
Final Practical Review
Final Practical Review
Uploaded by
Joelle DwekOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Final Practical Review
Final Practical Review
Uploaded by
Joelle DwekCopyright:
Available Formats
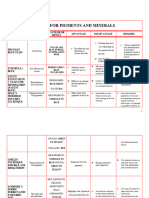
OSI N N- BLU-
. eosin methylene blue (EMB) agar ⇒ complex, selective and differential medium
⇒ contains gelatin, lactose, and the dyes eosin Y and methylene blue
⇒ gelatin = provides nitrogen and organic carbon (nutrient source)
⇒ lactose = fermented to acid-end products by E. coli and E. aerogenes
• eosin Y and methylene blue dyes purpose ⇒ to inhibit most' Gram + organism growth (exceptions: Enterococcus & Staphylococcus)
⇒ react with aggressive lactose fermenters whose end products turn dark purple or
black (typical of E. coli) and accompanied by green metallic sheen
- other scenarios ⇒ react with less aggressive lactose fermenters (Enterobacter or Klebsiella) that makes pink to dark purple colonies
⇒ lactose non-fermenters retain their normal color or take on the color of the medium (colorless)
• application ⇒ to isolate fecal coliform
◦ N EN =RIC AGAR.
- hekton enteric (HE) agar ⇒ complex, moderately selective and differential medium made to isolate Salmonella and Shigella species
- this isolation is based on the ability to ferment lactose, sucrose, or salicin to acid end-products and to reduce sulfur to hydrogen sulfide gas (Has)
- ferric ammonium citrate included as a source of oxidized iron to react with any Has produced to make black precipitate ferrous sulfide (Fes)
• bile salts included to prevent/inhibit Gram + growth
• bromothymol blue and acid fuchsin dyess added to indicate pH changes
- differentiation of media is a result of various colors produced in the colonies and agar
• enteries produce acid from fermentation ⇒ yellow to salmon-pink colonies
• Salmonella and Shigella species don't ferment any g the sugars, they break down animal tissue that raises pH of the medium and produces ⇒ blue-green color
• Salmonella species reduce sulfur to Has and colonies contain Fes ⇒ produces black color
• Results and Interpretations
↳ poor or no growth ⇒ inhibited by bile and/or dyes ⇒ Gram +
↳ good growth ⇒ not inhibited by bile and/or dyes ⇒ Gram-
↳ pink to orange growth ⇒ produces acid from lactose, sucrose, and/or salicin fermentation ⇒ not Shigella or Salmonella
↳ blue-green growth with black precipitate ⇒ doesn't ferment lactose, sucrose, or salicin, but reduces sulfur to hydrogen sulfide (Has) ⇒ probable Salmonella
↳ blue-green growth without black precipitate ⇒ doesn't ferment lactose, sucrose, or salicin,and doesn't reduce sulfur ⇒ probable Shigella or rarely Salmonella
- application ⇒ to isolate and differentiate Salmonella and Shigella species from other Gram- enteric organisms in a patient's stool sample
⇒ to identify fecal contamination of dairy and poultry products
I 1 SN IRON AGAR.
• lysine iron agar (1A)
L ⇒ a combination medium that detects bacterial ability to decarboxylate or deaminate lysine and to reduce sulfur
• ferric ammonium citrate ⇒ sulfur reduction indicator
. bromocresol purple ⇒ pH indicator
↳ purple at pH = 6.8
↳ yellow at or below pH = 5.2
• LIA prepared as a slant with deep butt (aerobic zone in slant and anaerobic zone in butt)
• if medium inoculated with lysine decarboxylase f) organism, acid production from glucose fermentation will induce decarboxylase enzyme production
• acidic pH will turn the medium yellow
- decarboxylation of lysine makes amine cadaverine and alkalinize the agar to turn it purple
• if organism produces lysine deaminase ⇒ produces compounds that react with ferric ammonium citrate and makes a red color
↳ deamination reactions require oxygen (slant)
. hydrogen sulfide (Has) produced in LIA by anaerobic reduction of thiosulfate
↳ ferric ions in medium react with Has to make black precipitate in butt of medium
• Results and Interpretations
↳ purple slant/purple butt ⇒ lysine deaminase-; lysine decarboxylase-1 ⇒ KIK
↳ purple slant/yellow butt ⇒ lysine deaminase-; lysine decarboxylase-; glucose fermentation ⇒ KIA
↳ red slant/yellow butt ⇒ lysine deaminase-;
l lysine decarboxylase-; glucose fermentation ⇒ RIA
↳ black precipitate ⇒ sulfur reduction ⇒ Has
- application ⇒ to differentiate enterics based on their ability to decarboxylate or deaminate lysine and produce hydrogen sulfide (HS)
⇒ used to identify members of Salmonella and Shigella
All O SAL AGAR
- differential media ⇒ used to visually distinguish microorganisms from one another
- selective media ⇒ used to grow/isolate specific types of microorganisms suppressing the growth of other microorganisms
- mannitol salt agar (USA) contains the carbohydrates mannitol, 7.5% sodium chloride (NaCl), and the pH indicator phenol red
- components
↳ phenol red indicate ⇒ yellow below pH = 6.8
⇒ red at pH = 7.4 - 8.4
⇒ pink at pH = 8.4 and above
↳ mannitol ⇒ gives substrate for fermentation and makes medium differential
↳ sodium chloride ⇒ makes medium selective since its concentration is high enough to dehydrate/kill most bacteria
• bacteria
↳ staphylococci thrive on this medium due to its adaptation to salty habitats such as human skin
↳ phenol red ⇒ indicates whether fermentation with an acid has taken place by changing color as the pH changes
↳ most staphylococci are able to grow on MSA, but do NOT ferment mannitol, showing growth as pink or red and the medium stays unchanged
↳ Staphylococcus aureus ferments mannitol, producing acids and lowers medium pH ⇒ bright yellow colonies form
• application ⇒ mannitol salt aga.r used for isolation and differentiation of Staphylococcus aureus from other StaphylococcuS species
BLOOD AGAR
• blood agar separates Gram + cocci that produces exotoxins called hemolysins
- hemolysins ⇒ lipids/proteins that break down red blood cells
• blood agar is made of 5% of blood (sheep blood) in a tryptic soy agar base
blood agar allows differentiation of bacteria based on their ability to hemolyze red blood cells
3 types of hemolysis
↳ beta-hemolysis ⇒ complete destruction of red blood cells and hemoglobin, resulting in a clearing of the medium around the colonies
↳ alpha-hemolysis ⇒ partial destruction of red blood cells and produces an olive-greenish discoloration of the agar around the colonies
in reflected light → converting heme in hemoglobin to methelglobin that cannot bind oxygen, appearing as green
↳ gamma-hemolysis ⇒ nonhemolysis, appearing as simple growth with no change to the medium
- hemolysins produced by streptococci ⇒ streptolysins
. 2 forms ⇒ Type O and Type S
↳ streptolysin 0 ⇒ oxygen sensitive, grows best under anaerobic conditions (in agar)
↳ streptolysin S ⇒ oxygen stable, grows in aerobic conditions surface of agar plate)
- streak stab technique ⇒ method to provide environment favorable for streptolySins
↳ blood agar plate streaked for isolation and then stabbed with a loop
↳ alpha-hemolysis on the surface but beta-hemolysis in the stab
BAA RACH SUSCEPT/BHi T St
. bacitracin ⇒ made by Bacillus licheniformis is a powerful peptide antibiotic that inhibits bacterial cell wall synthesis by
interfering with peptidoglycan transport across the cytoplasmic membrane → effective only to bacteria with cell walls
that are in the process of growing
• novobiocin ⇒ antibiotic produced by Streptomyces nivens →
interferes with ATPase activity associated with DNA gyrase
(enzyme needed for DNA replication)
- optochin ⇒ antibiotic derived from quinine that disrupts ATP synthase activity - reduced ATP production in susceptible bacteria
- bacitracin test is used to differentiate and identify ⇒ beta-hemolytic group A streptococci (Streptococcus pyogenes - bacitracin susceptible)
from other beta-hemolytic streptococci (bacitracin resistant)
UL RAVI T RADIATION DA AGE & R- PAR
• part of electromagnetic spectrum, with shorter and high energy wavelengths than visible light
- prolonged exposure ⇒ thymine dimers formed between pyrimidines (cytosine-cytosine, cytosine-thymine, or thymine-thymine)
• thymine molecules interfere with DNA replication
• bacteria have mechanisms to repair DNA damage
- DNA damage repair
↳ E. coli ⇒ performs light repair (photoreactivation)
⇒ DNA photolyase activated by visible light
↳ excision repair/dark repair
1. thymidine dimer distorts sugar-phosphate backbone but this is detected by MurABC endonuclease that breaks the dimer
2. DNA polymerase 1 inserts the complementary nucleotide 5' to 3' direction to make dsDNA
3.DNA ligase ⇒ closes gap between the last nucleotide of the new segment and the first nucleotide of the old DNA (completed repair)
* * mechanisms are only capable of repairing small amount of UV damage, NOT long/intense exposure
↳ application ⇒ with UN's lethal effect on bacterial cells, it can be used for decontamination
⇒ UV light can penetrate glass and plastic materials poorly
⇒ bacterial cells have natural mechanisms to repair UV damage
UREA DROLYSIS UR=ASE IEST
• urea production ⇒ by decarboxylation of certain amino acids
↳ primary nitrogenous waste in the urine of many mammals
- urea can be hydrolyzed to ammonia and carbon dioxide by bacteria having the enzyme called urease
↳ provides nitrogen in a usable form (ammonia) and acts as a virulence factor for pathogens such as Helicobacter pylori
- enteric bacteria possess ability to metabolize urea
• urease test used urea agar to differentiate enteric organisms capable of rapid urea hydrolysis
- pH indicator ⇒ used to track rising pH due to accumulation of ammonia
↳ rapid urease- positive organisms ⇒ + result within a day
↳
slower urease-positive organisms ⇒ may take several days to prom a readable result
• urea broth will be used in this lab because its only nutrient source other than urea is
trace amount of yeast extract
• pink ⇒ rapid urea hydrolysis 1
strong urease production → areae-positive
S organism
- orange or yellow ⇒ no urea hydrolysis, urease is absent or not produced in enough quantity to produce result
in 24 hours, organism cannot live in urease broth → urease-negative organism
• application ⇒ to differentiate organisms based on their ability to hydrolyze urea with the urease enzyme
↳ urinary tract pathogens distinguished from enteric bacteria
↳ identifying H. pylori (associated with gastric ulcers and stomach ulcers)
• Urea agar → fishtail inoculation on surface only
CATALASE TEST
- electron transport chains (ETC) of aerobic and facultative anaerobic bacteria have molecules that can
accept and donate electrons depending on the condition
- these molecules alternate between their oxidized and reduced forms, passing electrons down the chain to
oxygen (final electron acceptor)
• energy lost by electrons in this transfer is used to perform oxidative phosphorylation (ADP + P-ATP)
- most cases ⇒ electrons in aerobic ETC follow stepwise path to oxygen
: other cases ⇒ other paths can be followed and result in toxic form of oxygen production
• flavoprotein ⇒ this electron transport chain carrier molecule bypasses the next carrier in the chain to
directly transfer electrons to oxygen
⇒ produces hydrogen peroxide (Hao) = highly potent tox.
in
• reduced flavin adenine dinucleotide (FADH,) ⇒ capable of same reaction
- hydrogen peroxide and superoxide radical are TOXIC because they can oxidize proteins and render biochemicals nonfunctional
• protective enzymes
1. superoxide dismutase ⇒ enzyme that catalyzes conversion of superoxide radicals to hydrogen peroxide
(less lethal than superoxide)
2. catalase ⇒ enzyme that converts hydrogen peroxide into water and gaseous oxygen
* * the ability to synthesize these protective enzymes shows the organism's ability to live in the presence of oxygen
• application ⇒ this test identifies organisms that produce the enzyme catalase
⇒ this test differentiates anaerobic vs. aerobic bacteria by detecting the presence of the enzyme catalase, which
converts H2O into H2O and oxygen
⇒ catalase-positive culture = when Hao. is added, oxygen gas bubbles forms
⇒ catalase-negative culture = when no bubbles appear upon addition of H2O.
⇒ it is used to differentiate catalase-positive Micrococcus and Staphylococus
0 from the catalase-negative
Streptococcus, Enterococcus, and Lactococcus
EPIDE k $ ULATION
. epidemiology ⇒ study of the causes, occurrence, transmission, distribution, and prevention of disease in a population
• identification of pathogens happens first by discovering mode of transmission
• portal of entry ⇒ exact route where pathogen is introduced into a new host through ingestion, inhalation, direct skin
contact, open wounds, or blood transfusions)
⇒ infectious diseases can be transmitted by fomites (inanimate contaminated objects), biting insects (vectors),
or through sick people and animals, or healthy people (reservoir)
- common source epidemic ⇒ disease transmitted from an area such as a heating or cooling system of a building or from
contaminated water that infects many people at once
- propagated transmission ⇒ where pathogen is passed from person to person
• index case ⇒ first case of such a disease
• incidence rate ⇒ #of new cases of a disease reported in a defined population during a specific time period
- period prevalence ⇒ #of cases of a disease at a specific point in time in a defined population
• epidemiologists are tasked with identifying the source of a disease and establishing its transmission mode
- they then have to characterize the diseases quantitatively using measures such as incidence and prevalence
- incidence rate ⇒ indicates probability an individual will contract the disease in a specific time period
- prevalence ⇒ indicator of the disease's presence in the population
SLIDE AGGLUTINATION
. agglutination reactions ⇒ highly sensitive and used to detect either the presence of antigen or antibody in a sample
• antigen ⇒ structure (protein) that binds to antibodies and agglutinates form due to binding
- agglutinates ⇒ visible clumps of antibodies
• agglutination ⇒ evidence of antigen-antibody reaction and considered a positive test
- direct agglutination ⇒ relies on combination of antibodies and particulate antigens produced naturally
⇒ used to identify pathogens (like Salmonella and Streptococcus sp.) to determine if patient
was exposed to a certain pathogen based on the antibodies they have
• indirect (passive) agglutination ⇒ artificial construction of antigen and antibody
⇒ used in some pregnancy tests and also in diagnosing diseases such as
syphilis or Neisseria meningitidis
• positive agglutination result ⇒ agglutinate is visible
You might also like
- The ABC of Organic Agriculture Nuzie1 1 U1pcng 1 Dlfta9Document396 pagesThe ABC of Organic Agriculture Nuzie1 1 U1pcng 1 Dlfta9CUCULEAC STEFANNo ratings yet
- Selective, Differential, & Enriched Media Lab ChartDocument2 pagesSelective, Differential, & Enriched Media Lab ChartFrankiesgirl6yr100% (6)
- Microbio Lab 8Document4 pagesMicrobio Lab 8api-3743217100% (5)
- Special StainsDocument2 pagesSpecial StainsGheorghe-Emilian Olteanu100% (2)
- (Microbio) Enterobacteriaceae-Dr. Natividad (Mulan)Document11 pages(Microbio) Enterobacteriaceae-Dr. Natividad (Mulan)Lee Delos Santos100% (4)
- Media and StainingDocument6 pagesMedia and StainingJennifer O'DonnellNo ratings yet
- Bacte Gram NegativeDocument2 pagesBacte Gram NegativeDeisyleine RoldanNo ratings yet
- Activity in Biochemical TestDocument5 pagesActivity in Biochemical TestMaui Vecinal de GuzmanNo ratings yet
- Microbio Lab 7 (Leigh)Document8 pagesMicrobio Lab 7 (Leigh)api-3743217100% (6)
- Salmonella and Listeria 2Document11 pagesSalmonella and Listeria 2Gurpreet SinghNo ratings yet
- Veterinary Microbiology Lab FP DraftDocument23 pagesVeterinary Microbiology Lab FP DraftSɪʟᴇɴᴛ GᴀᴍɪɴɢNo ratings yet
- Biochemical Test (Enterobacteriaceae)Document1 pageBiochemical Test (Enterobacteriaceae)Renz BagasNo ratings yet
- Pcog Lec Midterms PDFDocument18 pagesPcog Lec Midterms PDFMikaela YumulNo ratings yet
- Technical Specification Sheet: Harlequin® Salmonella ABC Medium (NCM1003)Document2 pagesTechnical Specification Sheet: Harlequin® Salmonella ABC Medium (NCM1003)Carlos Zavaleta GuzmánNo ratings yet
- Special StainsDocument1 pageSpecial StainsGerald TejadaNo ratings yet
- EnterobacteriaceaeDocument3 pagesEnterobacteriaceaePark SunghoonNo ratings yet
- Important Media and Biochemical Tests For Diagnostic Microbiology 2023Document3 pagesImportant Media and Biochemical Tests For Diagnostic Microbiology 2023yn6q5fc5pzNo ratings yet
- Culture Media - FinalDocument39 pagesCulture Media - FinalMA. ELIZABETH P. BONGHANOYNo ratings yet
- Culture MediaDocument2 pagesCulture Mediarkenlaurenceorevor9No ratings yet
- Culture MediaDocument2 pagesCulture MediaJobelleNo ratings yet
- Microbiology Lab (Midterms) : November 2015 Dr. Mark CalbanDocument3 pagesMicrobiology Lab (Midterms) : November 2015 Dr. Mark Calbanrichmarkconag1No ratings yet
- MCB2010L Final Notes PDFDocument12 pagesMCB2010L Final Notes PDFTotalMeanGirlNo ratings yet
- Week 13 - Biochemical ID of GN BacteriaDocument8 pagesWeek 13 - Biochemical ID of GN BacteriaDax Liwell SalesNo ratings yet
- Components Positive Result Negative Result PrincipleDocument2 pagesComponents Positive Result Negative Result PrincipleAngeline TwoNo ratings yet
- EnterobacteriaceaeDocument8 pagesEnterobacteriaceaeWansun MaglangitNo ratings yet
- Microb Summary 3314Document28 pagesMicrob Summary 3314KPNo ratings yet
- Ncm0105 Ts En-UsDocument2 pagesNcm0105 Ts En-UsJonathan GodoyNo ratings yet
- Mannitol Salt AgarDocument1 pageMannitol Salt AgarJoelle DwekNo ratings yet
- Agars & TestsDocument73 pagesAgars & Testssana khanNo ratings yet
- HP - 5 - Mounting and Staining Version 2Document11 pagesHP - 5 - Mounting and Staining Version 2Klieden LobrigasNo ratings yet
- MICRO 2nd Sem FINAL Practical Exam All 2nd Sem Topics 1Document33 pagesMICRO 2nd Sem FINAL Practical Exam All 2nd Sem Topics 1RozeanneNo ratings yet
- Lab Group Disc Suzea and ErikaDocument14 pagesLab Group Disc Suzea and ErikaJaneNo ratings yet
- MicroTech Lec Reviewer FinalsDocument18 pagesMicroTech Lec Reviewer FinalsAzh Haezen Marithe TarlacNo ratings yet
- Color/ Char Organism Color/Cha R Organism: E. Coli S. Typhimurium Shigella Flexneri Proteus Mirabilis P. AeruginosaDocument8 pagesColor/ Char Organism Color/Cha R Organism: E. Coli S. Typhimurium Shigella Flexneri Proteus Mirabilis P. AeruginosaDOREEN NIZZA CAMIGLA FERRERNo ratings yet
- Part IIDocument15 pagesPart IIIan LapidezNo ratings yet
- Physical ContaminationDocument10 pagesPhysical ContaminationGlenn BanlaygasNo ratings yet
- Notes Regarding Additional Media Used in Lab 12Document5 pagesNotes Regarding Additional Media Used in Lab 12jlconnors941No ratings yet
- Matching TypeDocument4 pagesMatching TypeMary Jane Mondelo CabiltesNo ratings yet
- Biochemical Tests BacteriaDocument30 pagesBiochemical Tests BacteriaScribdTranslationsNo ratings yet
- Histopath - STAININGDocument2 pagesHistopath - STAININGvoreb84649No ratings yet
- Enterics Reviewer For MicrobiologyDocument8 pagesEnterics Reviewer For MicrobiologyGea MarieNo ratings yet
- Lab Report Microbe Prac 1Document5 pagesLab Report Microbe Prac 1domo- kunNo ratings yet
- 18.1-FAMILY ENTEROBACTERIACEAE and TESTSDocument2 pages18.1-FAMILY ENTEROBACTERIACEAE and TESTSJesette KhoNo ratings yet
- Exogenous and Endogenous Pigment.....Document30 pagesExogenous and Endogenous Pigment.....Mohan ChoudharyNo ratings yet
- Histopathologic Technique 2Document71 pagesHistopathologic Technique 2Kimberly AnnNo ratings yet
- Staining & CytopathologyDocument12 pagesStaining & CytopathologyStephanie Kate Arriola100% (1)
- Chapter 18 Enterobacteriaceae (1)Document11 pagesChapter 18 Enterobacteriaceae (1)Saldo SherlynNo ratings yet
- BACTERIOLOGY ENDORSEMENTDocument17 pagesBACTERIOLOGY ENDORSEMENTst.camilluslab23No ratings yet
- Bacte Lab - STAININGDocument4 pagesBacte Lab - STAININGbirdsdaisiesNo ratings yet
- GI BacteriaDocument1 pageGI Bacteriajingwei_xiongNo ratings yet
- L EmbDocument2 pagesL EmbJONATHAN BAUTISTA MARTINEZNo ratings yet
- BIOCHEMISTRY Lecture NotesDocument7 pagesBIOCHEMISTRY Lecture NotesFaye AquinoNo ratings yet
- Lysine Iron Agar L: Art. No. 01-094Document2 pagesLysine Iron Agar L: Art. No. 01-094LuluNo ratings yet
- StainDocument4 pagesStain2B SALVADOR Jamaica C.No ratings yet
- Day 2 OutputDocument9 pagesDay 2 OutputStephanie Kate ArriolaNo ratings yet
- Case Study 2 Nur Hazirah Amani Binti Halim (MLT07190003)Document4 pagesCase Study 2 Nur Hazirah Amani Binti Halim (MLT07190003)Nur Hazirah AmaniNo ratings yet
- Aubf - Chapter 4Document6 pagesAubf - Chapter 4Kristin SoquilloNo ratings yet
- Biochemical TestingDocument10 pagesBiochemical TestingKatrina Mae MedinaNo ratings yet
- A Critical Review On Martynia Annua LinnDocument9 pagesA Critical Review On Martynia Annua LinnNovy TanoNo ratings yet
- SDS - 181001 - Carbol Fuchsin Ziehl Neelsen Stain Sds - Rev3Document7 pagesSDS - 181001 - Carbol Fuchsin Ziehl Neelsen Stain Sds - Rev3dadi hartonoNo ratings yet
- Molecules of LifeDocument5 pagesMolecules of LifeEmmaNo ratings yet
- Diagram Based Questions With AnswersDocument10 pagesDiagram Based Questions With AnswersV P SomeshwarNo ratings yet
- Inorganic Nomenclature Worksheet 2Document7 pagesInorganic Nomenclature Worksheet 2Ji-Shawn PardassieNo ratings yet
- CAT 3904 en - Bearing - Units - Plastic - Housing - Series PDFDocument7 pagesCAT 3904 en - Bearing - Units - Plastic - Housing - Series PDFJesusNo ratings yet
- PROTOCOL - IRAP and REMAP For RetrotransposonDocument7 pagesPROTOCOL - IRAP and REMAP For RetrotransposonAngela JimenezNo ratings yet
- Chem ProjectDocument17 pagesChem ProjectNehaNo ratings yet
- MEDICINAL CHEMISTRY-I - Practicals PDFDocument25 pagesMEDICINAL CHEMISTRY-I - Practicals PDFAnit Dubey100% (1)
- Opportunities For Zambian MoringaDocument47 pagesOpportunities For Zambian MoringaSuresh KumarNo ratings yet
- Varjani2020 Article TreatmentOfWastewaterFromPetroDocument9 pagesVarjani2020 Article TreatmentOfWastewaterFromPetroKemuel MatthewNo ratings yet
- Ranjeet ShahiDocument529 pagesRanjeet Shahiयash ᴍᴀɴGalNo ratings yet
- Alkanes: Self-Attempt Questions 1 (I)Document7 pagesAlkanes: Self-Attempt Questions 1 (I)EdcademiaNo ratings yet
- G11 Bubalus EditedDocument28 pagesG11 Bubalus EditedA - CAYAGA, Kirby, C 12 - HermonNo ratings yet
- TIFC BrochureHigh ResDocument20 pagesTIFC BrochureHigh Resguven44100% (1)
- Rawat 2021Document9 pagesRawat 2021Melissa Yactayo YarangaNo ratings yet
- Pembuatan Biodiesel Biji Kepuh Dengan Proses TransesterifikasiDocument11 pagesPembuatan Biodiesel Biji Kepuh Dengan Proses TransesterifikasiIvandre Jonathan SianiparNo ratings yet
- Face Tonic MarantaDocument6 pagesFace Tonic MarantaVITA OKTAVIYANTI PUTRI 2018No ratings yet
- Chemical Equations - Practice SolutionsDocument2 pagesChemical Equations - Practice SolutionslolaNo ratings yet
- Review Article On BiofertilizersDocument17 pagesReview Article On Biofertilizersnet_set71% (7)
- Fragrance Mix Patient InfoDocument1 pageFragrance Mix Patient Infoᴇᴜʀᴇsɪᴀ ᴀsɪᴀɴNo ratings yet
- IMVIC TestDocument13 pagesIMVIC TestLaksilu Viduraga Peiris100% (5)
- LOCTITE Do It Right Guide v5 ApprovedDocument44 pagesLOCTITE Do It Right Guide v5 ApprovedvfrpilotNo ratings yet
- Bpo C Chapter 10Document55 pagesBpo C Chapter 10DewiSugiartiNo ratings yet
- Synthesis, Structure and Chemical Transformations of 4-AminobenzaldehydeDocument5 pagesSynthesis, Structure and Chemical Transformations of 4-AminobenzaldehydeBrem BalazsNo ratings yet
- Application of Nuclear Magnetic Resonance Spectroscopy To The Analysis of Organic Archaeological MaterialsDocument16 pagesApplication of Nuclear Magnetic Resonance Spectroscopy To The Analysis of Organic Archaeological Materialsian.godfrey303No ratings yet
- Plastic Waste ManagementDocument56 pagesPlastic Waste ManagementMaulik KotadiyaNo ratings yet
- Nutritive Value of Coconut Grating Residue For PigsDocument5 pagesNutritive Value of Coconut Grating Residue For PigsSubramanian SenthilmuruganNo ratings yet
- Industrial Crops & Products: Didem Sutay Kocabas, Merve Erkoç Akçelik, Erinç Bahçegül, Hatice Neval OzbekDocument13 pagesIndustrial Crops & Products: Didem Sutay Kocabas, Merve Erkoç Akçelik, Erinç Bahçegül, Hatice Neval Ozbekjans carlosNo ratings yet