Professional Documents
Culture Documents
Perioperative Management of The Obese Patient
Perioperative Management of The Obese Patient
Uploaded by
АнастасияПлешкоOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perioperative Management of The Obese Patient
Perioperative Management of The Obese Patient
Uploaded by
АнастасияПлешкоCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/14728694
Perioperative management of the obese patient
Article in BJA British Journal of Anaesthesia · April 1993
DOI: 10.1093/bja/70.3.349 · Source: PubMed
CITATIONS READS
273 824
3 authors, including:
Jay Brodsky
Stanford University
199 PUBLICATIONS 5,184 CITATIONS
SEE PROFILE
All content following this page was uploaded by Jay Brodsky on 12 March 2018.
The user has requested enhancement of the downloaded file.
medigraphic Artemisa
en línea
Anestesiología
O DE A N ES T E
AN
Mexicana de M
EX
IC SI O
L
Revista
O
IO
GÍ
C
EG
AA
COL
.C.
ANT
GÍA
ES
LO
SO
IO
CI
ED ES
AD ST
MEXI NE
CANA DE A
CONFERENCIAS MAGISTRALES
Vol. 31. Supl. 1, Abril-Junio 2008
pp S85-S89
Perioperative management of the obese patient
Jay B. Brodsky, MD*
* Professor, Department of Anesthesia. Stanford University School of Medicine. Stanford, CA, 94305. Jbrodsky@stanford.edu
Obesity has become a world-wide epidemic in both indus- statistically associated with maximum life expectancy. For
trial and developing nations. The precursors of obesity in- men and women IBW can be calculated as 22 x height (m2).
clude gender, genetics, environment, ethnicity, education Normal weight ranges between ± 10% of IBW.
and socioeconomic status. Obesity related medical condi- Two general types of obesity are described. In “central-
tions are reversible following surgical weight loss. Laparos- android” obesity (more common in men) fat is located in the
copy is the preferred operative approach since it is associat- abdomen and upper body. In “peripheral-gynecoid” obesi-
ed with less postoperative pain, earlier recovery and reduced ty (more common in women) fat is located primarily in the
risk of postoperative pulmonary complications. Surgical hips, buttocks and thighs. Central-obesity is associated with
options currently include either strictly restrictive proce- the “metabolic syndrome” with an increased risk of cardio-
dures (vertical banded gastroplasty, adjustable gastric band- vascular disease.
ing) that limit stomach capacity, or operations that combine Body mass index (BMI), an indirect measure of obesity,
gastric restriction and malabsorption (Roux-en-Y gastric is calculated by dividing weight in kilograms (kg) by square
bypass, biliary-pancreatic diversion, duodenal switch). of height in meters (m2). BMI does not consider gender or
other contributing factors (water, muscle) as causes of in-
Fat
Non-Obese Obese
Fat creased TBW. A BMI of 20-25 kg/m2 is defined as normal
20.0% 38.4% weight, and BMI of 26 - 29 kg/m2 is “overweight”. BMI >
Body 70 kg 105 kg
weight
30 kg/m2 is “obese”. “Morbid obesity” describes obesity
that, if untreated, will significantly shorten the patient’s life.
LMB
kg % kg %
LMB A BMI > 40 kg/m2 is “morbid obesity”. A patient with a
80.0% Fat 14.0 20.0 40.3 38.4 61.6% BMI > 36 kg/m2 and multiple medical co-morbidities is
*LBM 56.0 80.0 64.7 61.6
considered a candidate for bariatric surgery.
70.0 100.0 105.0 100.0 Metabolic Syndrome (Central Obesity)
Three or more of the following must be present:
*LMB
Water 41.0 58.6 47.4 45.1
Protein 11.5 16.4 13.2 12.6 • Waist circumference > 102 cm (men), > 88 cm (women)
Glycogen 0.5 0.7 0.5 0.5 • Serum triglycerides > 150 mg/dL
Mineral 3.0 4.3 3.6 3.4 • HDL cholesterol < 40 mg/dL (men), < 50 mg/dL (women)
56.0 80.0 64.7 61.6 • Systolic blood pressure > 130 mmHg and/or diastolic
> 85 mmHg, or, on treatment for
www.medigraphic.com
Total body weight (TBW) is composed of lean body mass
(LBM = muscles, bones, tendons, ligaments and body wa- PREOPERATIVE EVALUATION
ter) and fat weight (FW). LBW should be about 80% of TBW
for males and 75% of for females. Obesity is present when Morbidity and mortality doubles with a BMI > 35 kg/m2
FW > 30% TBW. Ideal body weight (IBW) is a measure and rises exponentially with increasing BMI. Obesity is as-
initially derived from life insurance studies to describe weight sociated with many chronic medical conditions that must
Volumen 31, Suplemento 1, abril-junio 2008 S85
Brodsky JB. Perioperative management of the obese patient
be recognized and optimized before surgery. Endocrine con- load, after-load, mean pulmonary artery pressure (PAP), and
ditions such as Cushing’s disease, hypothyroidism and poly- an elevation in right and left ventricular stroke work. These
cystic ovary syndrome are also associated with obesity. A patients are often not physically active and may appear as-
patient scheduled for any surgery following previous bari- ymptomatic even with significant cardiovascular disease.
atric surgery should be evaluated for metabolic changes, Signs of pulmonary hypertension (exertional dyspnea, fa-
including protein, vitamin, iron and calcium deficiencies. tigue, syncope) should be sought and trans-esophageal
echocardiography (TEE) obtained in symptomatic patients.
Preoperative diagnostic testing Right heart failure is common in older patients.
Pulmonary system: Adipose is metabolically active and
Routine tests O2 consumption and CO2 production rise with increasing
weight. The work of breathing is increased since more ener-
Thyroid function gy must be expended to carry additional body mass, while
Lipid profile respiratory muscle performance is impaired. The fatty chest
Glucose
and abdominal walls reduce chest wall compliance. Mass
Liver function tests
Creatinine loading of the thoracic and abdominal chest walls causes
ECG abnormalities in lung volumes and gas exchange. Functional
Special tests residual capacity (FRC) is significantly reduced due to a
decrease in expiratory reserve volume (ERV), so total lung
Dexamethasone suppression test capacity (TLC) is reduced. Airways close during normal
Testosterone level ventilation. Continued perfusion of non-ventilated alveoli
RUQ ultrasound results in a PaO2 that is lower than predicted for similar aged
Sleep studies non obese patients. All these changes are directly propor-
ECHO (h/o heart disease or Fen/Phen)
tional to increasing BMI. Younger obese patients have an
Cardiac stress test
Pulmonary functions tests increased ventilatory response to hypoxia. An arterial blood
sample usually shows alveolar hyperventilation (PaCO2 30-
35 mmHg) and relative hypoxemia (PaO2 70-90 mmHg) on
Medications: All recent medications, including non-pre- room air. With increasing age sensitivity to CO2 decreases,
scription diet drugs must be identified since many have PaCO2 rises and PaO2 falls.
important implications for anesthesia. The combination of
phentermine and fenfluramine (“Phen-Fen”) is no longer
prescribed, but phentermine is still used world-wide. An as-
sociation between Phen-Fen and heart and lung problems
has been clearly established. These medications must be
stopped 2 weeks before surgery and a complete cardiac eval-
uation obtained. Sibutramine works in the brain by inhibit-
ing reuptake of nor-epinephrine, serotonin and dopamine,
producing a feeling of “anorexia” limiting food intake. It
can cause arrhythmias and hypertension. Orlistat blocks FRC
CC
absorption of dietary fat causing deficiencies in fat-soluble
RV
vitamins (A, D, E, K). Reduced vitamin K level can increase
the anticoagulation effects of coumadin. Nonobese Obese Obese Obese
Cardiovascular system: Cardiac output rises about 0.1 upright supine trendelenburg
liter/min for each 1 kg addition in weight. Stroke volume is
elevated since total blood volume increases to perfuse the Many patients maintain normal PaCO2 during the day
added body fat. Increased cardiac output combined with but have CO2-retention, sleep disturbances, intermittent air-
www.medigraphic.com
normal peripheral vascular resistance leads to systemic hy-
pertension. A 3-4 mmHg increase in systolic pressure and a
way obstruction with hypoxemia, pulmonary hypertension
and cardiac arrhythmia’s at night. Obstructive sleep apnea
2 mmHg increase in diastolic arterial pressure can be ex- (OSA) syndrome is characterized by frequent episodes of
pected for every 10 kg of weight gained. Increases in blood apnea (> 10 sec cessation of airflow despite continuous res-
volume and cardiac output eventually produce dilational piratory effort against a closed airway) and hypopnea (50%
cardiac hypertrophy. Left ventricular dysfunction is often reduction in airflow or reduction associated with a decrease
presents. Even normotensive patients have increased pre- of SpO2 > 4%). Patients may not be aware of these symp-
S86 Revista Mexicana de Anestesiología
Brodsky JB. Perioperative management of the obese patient
toms, so it is important to interview their spouses. A defini-
tive diagnosis can only be confirmed by polysomnography
in a sleep laboratory. Because of fragmented sleep patterns,
patients may complain of daytime sleepiness and headaches.
Chronic OSA leads to secondary polycythemia, hypoxemia,
and hypercapnia; all increase the risk of cardiac and cere-
bral vascular disease. OSA patients can be difficult to mask
ventilate, and their tracheas can be difficult to intubate. OSA
patients requiring nasal continuous positive airway pres-
sure (N-CPAP) at home should bring it to the hospital to use
in the PACU.
A few patients experience the “obesity hypoventilation
syndrome” characterized by somnolence, cardiac enlarge-
ment, polycythemia, hypoxemia and hypercapnia. Hypoven-
tilation is central and independent of intrinsic lung disease,
and is probably due to progressive desensitization of the
respiratory center to CO2 from nocturnal sleep disturbances.
Its most severe form, “Pickwickian Syndrome”, is character-
ized by marked obesity, hypersomnolence, hypoxia, hyper-
capnia, pulmonary hypertension, right ventricular enlarge-
ment and hypervolemia. Patients rely on a hypoxic gery. Prophylaxis with antibiotics for wound infection, and
ventilatory drive and may hypoventilate or become apneic heparin against deep venous thrombosis (DVT) are admin-
during emergence from general anesthesia when given O2. istered prior to surgery. If concerned about risk of acid aspi-
Gastrointestinal and urinary systems: It was once be- ration, H2-receptor antagonists or a proton pump inhibitor
lieved that obese patients were at greater risk for acid aspira- can be given.
tion because of increased intra-abdominal pressure, high Positioning: When possible, we have the unpremedicat-
incidence of GERD and hiatus hernia, and increased gastric ed patient climb off the gurney and position themselves on
volume with low gastric fluid pH. Recent work has chal- the OR table. All pressure points are carefully padded to
lenged this belief. There were no differences in gastric vol- avoid pressure sores, neurologic injury, and rhabdomyoly-
ume or pH between lean and moderately obese surgical pa- sis. In the supine position FRC is markedly reduced causing
tients. Obese patients without symptoms of GERD have ventilation/perfusion (V/Q) mismatch, and significant in-
relatively normal gastro-esophageal sphincter tone and may creases in O2 consumption, cardiac output, and PAP. The
have faster gastric emptying time. Patients at particular risk reverse Trendelenburg position (RTP) or a “head-elevated”
for gastric aspiration may be those with diabetes and gastro- position are best tolerated since the diaphragm is “unload-
paresis. Non-alcoholic steatohepatitis (NASH), with or with- ed” (Figure). Trendelenburg (TP) and lithotomy positions
out liver dysfunction, is extremely common with histologic decrease lung volumes. In properly positioned prone pa-
abnormalities present in the livers of as many as 90% of tient ventilation is actually improved. The lateral decubitus
patients. Preoperative liver function tests may not reflect position is tolerated if the panniculus is displaced off the
the actual severity of liver disease. Obesity is associated abdomen.
with increased renal blood flow and increased glomerular Monitoring: For laparoscopy only standard monitors are
filtration rate. applied. Non-invasive cuff pressure may be inaccurate if the
wrong size cuff is used. If the anatomy of the upper arm doesn’t
OPERATIVE CONSIDERATIONS allow proper fit, cuff pressures are obtained from the wrist or
ankle. For laparotomy a radial artery is cannulated. Central
Premedication: Preoperative sedation is avoided. If fiberop- lines (CVP, PA) can be useful for major abdominal and tho-
www.medigraphic.com
tic bronchoscopic (FOB) intubation is planned an anti-cho-
linergic is given. Medications for chronic hypertension are
racic procedures. Since venous access is often limited a cen-
tral line may be required for postoperative needs. A nerve
continued; except ACE-inhibitors, which should be stopped stimulator is used to assess neuromuscular blockade. Excess
preoperatively since their presence can lead to profound fat may make surface electrodes inaccurate. A BIS monitor or
hypotension during anesthesia. Diabetic medications are another “depth of anesthesia” device can be useful.
usually withheld on the morning of surgery, but blood sug- Pharmacologic considerations: Physiologic changes in
ar must be closely monitored before, during, and after sur- obesity affect distribution, binding and elimination of the
Volumen 31, Suplemento 1, abril-junio 2008 S87
Brodsky JB. Perioperative management of the obese patient
various anesthetic agents. In routine practice on normal Induction agents: Large doses of propofol or thiopental
weight patients drugs are usually administered on the basis of are needed due to increases in fat content, blood volume,
dose per actual unit body weight. This assumes that clearanc- and cardiac output. In theory dosing should be based on
es and distribution volumes are proportional to weight, which actual weight. However cardiovascular effects of large dos-
may not be valid in the obese patient. Obese patients have a es limit the absolute amount that can be given. Induction
smaller than normal fraction of total body water, increased dosing is based on LBW.
blood volume and cardiac output, greater than normal fat Opioids: Opioids are highly lipophilic, and in theory
content, increased LBW and changed tissue protein binding loading doses should be based on TBW. There is no clinical
from increased concentrations of free fatty acids, triglycer- evidence that lipophilic opioids last longer in morbidly
ides, lipoproteins, cholesterol and other serum constituents. obese patients. Generous use of long-acting opioids (mor-
In addition, renal blood flow and GFR are increased while phine, demerol, hydromorphone) can be dangerous since
cardiopulmonary function may not be optimal. Hepatic clear- respiratory depression must be avoided. The Vd of remifen-
ance is usually normal or even increased despite NASH. Highly tanyl in obese patients is less than expected, probably be-
lipophilic medications (barbiturates, benzodiazepines) have cause of hydrolysis by blood and tissue esterases. Dosing is
a significant increase in volume of distribution (Vd) and load- based on IBW.
ing dose of these drugs is usually increased. Since elimina- Muscle relaxants: Since pseudocholinesterase levels and
tion half-lives are longer, maintenance dosing should reflect extracellular fluid space are increased in obesity high doses
IBW. Non- or weakly lipophilic drugs are given based on of succinylcholine (1.0 mg/kg TBW) are used for induction.
LBW. LBW is + 20-30% of IBW. Systemic absorption of oral Complete paralysis is especially important during laparos-
medications is not significantly affected by obesity. copy to facilitate ventilation and to provide adequate space
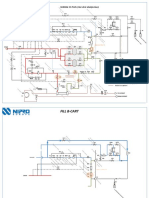
Inhalational agents: There is the misconception that re- for visualization and maneuvering of surgical equipment.
lease of volatile agents from the adipose tissue results in a Loss of pneumoperitoneum may indicate incomplete paral-
prolonged emergence from anesthesia. Sevoflurane and des- ysis. Since muscle relaxants are hydrophilic there is limited
flurane have lower lipid solubility than isoflurane. Although distribution in the added fat. There are no clinical advan-
reduced blood flow to adipose tissue may limit delivery of tages between any of the non-depolarizing relaxants. Neu-
volatile agent to the fat and liver, and inhalational anesthet- ro-muscular recovery time is similar in obese and non-obese
ics are stored in the fat long after completion of surgery, all patients with atracurium, vecuronium or rocuronium. Mus-
inhalational anesthetics are rapidly eliminated from the well- cle relaxants are administered in incremental doses based
perfused brain and lungs once the anesthetic is discontin- on IBW.
ued. Despite claims that one agent is superior to another for Fluids: Intraoperative fluid requirements are usually
bariatric operations, with proper timing, recovery from gen- greater than would be anticipated for laparoscopy. We in-
eral anesthesia is similar with any inhalation agent (Figure) fuse 40 ml/kg IBW of crystalloid.
or TIVA technique. Airway management: Patients cannot breathe adequate-
ly in the supine or lithotomy positions, and they may be at
Emergence end points risk for gastric aspiration. So tracheal intubation and assist-
10 ed or controlled ventilation should be considered for even
Desflurane Sevoflurane short procedures. Potential airway management problems
(fat face and cheeks, limited range of motion of the head,
8 neck and jaw, small mouth and large tongue, excessive pal-
atal and pharyngeal tissue, short large neck, high Mallam-
pati (III or IV) score) should all be evaluated preoperatively.
6 Mallampati score and large neck circumference are the most
Time to: reliable predictors of potential difficulties. If problems are
(min) anticipated FOB intubation is recommended. Increasing
4 weight or BMI is not a risk factor for difficult laryngoscopy.
www.medigraphic.com Positioning with the head, neck and shoulders elevated in
the head elevated laryngoscopy position (“HELP”) facili-
2 tates direct laryngoscopy. FOB-assisted tracheal intubation
is seldom necessary.
Despite conflicting evidence that patients are at greater
0 risk for acid aspiration it remains prudent to establish a se-
Response to verbal command Extubation cure airway as quickly and as safely as possible. Patients
S88 Revista Mexicana de Anestesiología
Brodsky JB. Perioperative management of the obese patient
Table II. Desaturation and recovery times of groups. laparoscopy without serious impairment of respiratory me-
chanics. Although absorption of insufflated CO2 can wors-
en hypercarbia and produce acidosis, changes are tempo-
rary and are usually well tolerated, and need not be corrected.
The surgical pneumoperitoneum can displace the diaphragm
cephalad causing endotracheal tube position to change, with
Safe apnea 178 ± 55 123 ± 24 153 ± 63
the tip entering a bronchus. Tube displacement should al-
Period (seconds) (1 vs 3:p < 0.05)
ways be considered in the differential diagnosis of hypox-
Recovery time 80 ± 30 206 ± 64 97 ± 41
emia developing during laparoscopic bariatric surgery.
(seconds) (2 vs 1:P < 0.001) (2 vs 3:P < 0.001)
Lowest SaO2(%) 83 ± 4 82 ± 5 83 ± 4
Hemodynamic changes: Pulmonary capillary wedge and
PAP pressures may be elevated secondary to increased pul-
Data is Mean ± Standard Deviation. monary blood volume and chronic hypoxemia. The RTP
will improve oxygenation but may also cause pooling of
should be pre-oxygenated in the reverse Trendelenburg blood and hypotension.
position (RTP) (Figure) until their SpO2 is 100% for several Regional anesthesia: Regional blocks can be technical-
mins. An apneic patient’s hemoglobin will desaturate very ly challenging. Special long epidural and spinal needles
quickly since FRC is reduced and O2 reserves are limited. may be needed. Insulated needles and a nerve stimulator
An i.v. induction with propofol and succinylcholine and can be used to identify the appropriate nerves for peripheral
cricoid pressure is the best way to establish an airway. A nerve blocks. Neuraxial spread of local anesthetics is direct-
second individual experienced with airway management, ly related to BMI. Increased abdominal pressure shifts blood
preferably another anesthesiologist, must always be present from the inferior vena cava into the epidural venous system
to assist if difficulty is encountered with mask ventilation decreasing the volume of the epidural and subarachnoid
or tracheal intubation. Aids for difficult intubation must be spaces. Epidural fat further reduces the capacity of the epi-
readily available, including a short laryngoscope handle dural space. For epidural and spinal blocks local anesthetic
and a variety of laryngoscope blades and a gum elastic dose requirements are reduced by 20-25%.
bougie. A laryngeal mask airway (LMA) can serve as a Anesthetic technique: For laparotomy and thoracotomy,
‘bridge’ until an endotracheal tube is placed. a combination of general anesthesia with epidural analge-
Ventilation: Obese patients should be mechanically ven- sia produces a lower incidence of postoperative respiratory
tilated with at least 50% O2 and a tidal volume (Vt) 12-15 complications and shorter hospital stays. Postoperative epi-
mL/kg IBW, preferably in the RTP. With mechanical venti- dural opioid analgesia, with or without local anesthetics, is
ESTE DOCUMENTO
lation, especially duringES ELABORADO
laparoscopy, POR MEDI-
peak ventilatory pres- recommended. General anesthesia is maintained with an
GRAPHIC
sures and end-tidal CO2 levels will increase. PEEP superim- inhalational anesthetic. Long-acting opioids are used with
posed upon a large Vt can worsen hypoxemia by depressing caution or avoided completely to decrease the risk of post-
cardiac output, which in turn will reduce O2 delivery to the operative respiratory depression. For laparoscopy we use a
tissues. Placement of sub-diaphragmatic packs or retractors short-acting opioid infusion (remifentanyl) with small
or changing to lithotomy or TP will also worsen hypox- amounts of i.v. fentanyl. The patient is ventilated with an
emia. Obese patients tolerate abdominal insufflation during inhalational anesthetic agent and 100% O2.
REFERENCES
1. Morbid Obesity - Peri-operative Management. Alvarez A (ed). 5. Gaszynski T, et al. Post-anesthesia recovery after infusion of
Cambridge University Press, 2004. propofol with remifentanyl or alfentanyl or fentanyl in morbidly
obese patients. Obes Surg 2004;14:1-7.
2. Brodsky JB. Positioning the morbidly obese patient for anesthe-
6. Jense HG, et al. Effects of obesity on safe duration of apnea in
sia. Obes Surg 2002;12:751-8. anesthetized humans. Anesth Analg 1991;72:89-93.
3. Brodsky JB, et al. Morbid obesity and tracheal intubation. Anesth 7. Lemmens HJM, et al. Estimating ideal body weight – a new
4.
Analg 2003;94:732-6. www.medigraphic.com
Collins JS, et al. Laryngoscopy and morbid obesity: a compari-
8.
formula. Obesity Surgery 2005;15:1082-3.
Lemmens HJM, et al. Estimating blood volume in obese and
morbidly obese patients. Obesity Surgery 2006;16:773-6.
son of the “sniff” and “ramped” positions. Obesity Surgery 9. Lemmens HJM, et al. The dose of succinylcholine in morbid
2004;14:1171-5. obesity. Anesthesia & Analgesia 2006;102:438-42.
Volumen 31, Suplemento 1, abril-junio 2008 S89
View publication stats
You might also like
- Musical Acoustics PDFDocument26 pagesMusical Acoustics PDFGino Mendoza0% (1)
- Renaissance Woman: Fat Loss, Muscle Growth & Performance Through Scientific EatingDocument20 pagesRenaissance Woman: Fat Loss, Muscle Growth & Performance Through Scientific EatingBenedict Ray Andhika33% (3)
- Least Mastered Competencies (Grade 6)Document14 pagesLeast Mastered Competencies (Grade 6)Renge Taña91% (33)
- Les ZOOM'sDocument242 pagesLes ZOOM'sHamza El Missouab86% (7)
- Professional Practice Session 1Document23 pagesProfessional Practice Session 1Dina HawashNo ratings yet
- Harrier Posner (2016) Marketing de La Moda 2da Edicion GGModaDocument225 pagesHarrier Posner (2016) Marketing de La Moda 2da Edicion GGModaPola Vanesa100% (1)
- List of Documents NBA PfilesDocument48 pagesList of Documents NBA PfilesDr. A. Pathanjali Sastri100% (1)
- 4 1 PDFDocument10 pages4 1 PDFNengLukmanNo ratings yet
- A Brief History of Clinical Airway ManagementDocument4 pagesA Brief History of Clinical Airway ManagementJames Lemuel Bato AquinoNo ratings yet
- Volume1 Fullreport PressPackDocument100 pagesVolume1 Fullreport PressPackEricusSolariusNo ratings yet
- SITE DEVELOPMENT PLAN Layout2Document1 pageSITE DEVELOPMENT PLAN Layout2V- irusNo ratings yet
- Sailing Directions For South AmericaDocument471 pagesSailing Directions For South AmericaCélio VelascoNo ratings yet
- ROADMAP 2050: Technical Analysis Executive SummaryDocument24 pagesROADMAP 2050: Technical Analysis Executive Summarybfly754151No ratings yet
- RETROACTIVO 2021 Incerpaz Playas REVISADO AdmDocument9 pagesRETROACTIVO 2021 Incerpaz Playas REVISADO AdmGersy paul Rodriguez AraujoNo ratings yet
- Halo Decorative Lighting: Area 1: Empo & LMPDocument19 pagesHalo Decorative Lighting: Area 1: Empo & LMPBucky Lasek27No ratings yet
- DENAH GEREJA IMANUEL BAUTASIK-ModelDocument1 pageDENAH GEREJA IMANUEL BAUTASIK-ModelVia YunusNo ratings yet
- Isometric View 2/F Water Supply System B: DN Exit DNDocument1 pageIsometric View 2/F Water Supply System B: DN Exit DNJesson Diaz VicenteNo ratings yet
- Outbreak To Recovery: C O V I D - 1 9 2 0 2 0Document2 pagesOutbreak To Recovery: C O V I D - 1 9 2 0 2 0Jeff MorrisNo ratings yet
- Rizal Street: Vicinity Map PerspectiveDocument1 pageRizal Street: Vicinity Map PerspectiveLenon RugayanNo ratings yet
- Bil. Nama Murid: I I& K ES IH AT AN LDocument57 pagesBil. Nama Murid: I I& K ES IH AT AN LROHINAH BT YULO KPM-GuruNo ratings yet
- Lkfbbworld Cm2020 RevDocument2 pagesLkfbbworld Cm2020 RevAfrizal FakhmyNo ratings yet
- Fatty AcidsDocument1 pageFatty AcidsMouddyNo ratings yet
- Placement 2009Document62 pagesPlacement 2009vipul_patel100% (12)
- Plano Base Santa Fe 2017Document1 pagePlano Base Santa Fe 2017Ale VillaNo ratings yet
- KKKKKDocument17 pagesKKKKKkukoyigbemigaNo ratings yet
- Ground Floor Plan: Waterbody WaterbodyDocument1 pageGround Floor Plan: Waterbody WaterbodyHB ARCHITECTNo ratings yet
- Preoperative Pain Neurophysiology Education For Lumbar Radiculopathy. A Randomized-Controlled TrialDocument8 pagesPreoperative Pain Neurophysiology Education For Lumbar Radiculopathy. A Randomized-Controlled TrialJesusNavarrete97No ratings yet
- Horarios Victoria Capilla Del SenorDocument1 pageHorarios Victoria Capilla Del SenorRamon Alejandro QuinterosNo ratings yet
- Cen-Cenelec WP 2020 enDocument104 pagesCen-Cenelec WP 2020 enSabri GünaydınNo ratings yet
- 12 Pearl WiDocument10 pages12 Pearl Wijecelyn mae BaluroNo ratings yet
- Site Development PlanDocument1 pageSite Development PlanMark Anthony De GuzmanNo ratings yet
- Consolidation Clean & GreenDocument2 pagesConsolidation Clean & GreenBhebe EuropaNo ratings yet
- AMAZONASDocument1 pageAMAZONASJUAN CARLOS DEL PINO VERANNo ratings yet
- Copper Testing - Quick Reference Guide 1-5Document4 pagesCopper Testing - Quick Reference Guide 1-5Daniel PiresNo ratings yet
- Cobro Playas Julio Incerpaz 2021Document3 pagesCobro Playas Julio Incerpaz 2021Gersy paul Rodriguez AraujoNo ratings yet
- 2022 10 13AustralianMotorcycleNewsDocument117 pages2022 10 13AustralianMotorcycleNewscivalNo ratings yet
- Summary of Grades 2016 - 2017 Six-AguinaldoDocument11 pagesSummary of Grades 2016 - 2017 Six-Aguinaldonorvel_19No ratings yet
- Procedimientos y Cirugía en ORL ZurdosDocument1 pageProcedimientos y Cirugía en ORL ZurdosMarco Antonio FigueroaNo ratings yet
- Rio Grande Flood Control Levee in The Upper Valley ProjectDocument1 pageRio Grande Flood Control Levee in The Upper Valley ProjectThe National DeskNo ratings yet
- BP Fragrance Journal PagesDocument1 pageBP Fragrance Journal PagesConstance FenskeNo ratings yet
- So 1Document1 pageSo 1MOHAMMED NEHALNo ratings yet
- MNKNDocument1 pageMNKNreyquidong03No ratings yet
- Arts Culture and The Latino Audience1Document20 pagesArts Culture and The Latino Audience1Pamela LopezNo ratings yet
- Col. Adalberto Tejeda Col. Zona Centro: Registro Federal de ElectoresDocument1 pageCol. Adalberto Tejeda Col. Zona Centro: Registro Federal de Electoresnoe emilio gonzalez riveraNo ratings yet
- OLI Electic VibratorsDocument2 pagesOLI Electic VibratorsSergio VLNo ratings yet
- Readiness Assessment Tools - CAVITE PROVINCE 2023 MR SIA - (PHO CHO MHO RHU HC BHSDocument186 pagesReadiness Assessment Tools - CAVITE PROVINCE 2023 MR SIA - (PHO CHO MHO RHU HC BHSChristean Val Bayani ValezaNo ratings yet
- Para Fotoshop ModelDocument1 pagePara Fotoshop ModelELSERES VILLALOBOS VILLANUEVANo ratings yet
- Lam in As Fund A Mentos RedesDocument48 pagesLam in As Fund A Mentos Redeshasse777No ratings yet
- City of Santa Barbara: Westside Bike Boulevard Gap ClosureDocument7 pagesCity of Santa Barbara: Westside Bike Boulevard Gap ClosureAnonymous kXVDRZMNo ratings yet
- TCS SessionDocument1 pageTCS Sessionpranshu171299No ratings yet
- English For Journ Certificate PDFDocument1 pageEnglish For Journ Certificate PDFIsaandra Miguel100% (1)
- Certificate Data Scientist IntroductionDocument1 pageCertificate Data Scientist IntroductionYoel Dwi Putra GultomNo ratings yet
- Who Owns Whom 1uk5c6sjkPeCf2Qt15ulWwqLjjfCHHAZYNi5juh5Document1 pageWho Owns Whom 1uk5c6sjkPeCf2Qt15ulWwqLjjfCHHAZYNi5juh5Mohammed MouftiNo ratings yet
- Who Owns WhomDocument1 pageWho Owns WhomHerbert WeigeltNo ratings yet
- FILIPO CompressedDocument1 pageFILIPO CompressedCarolina CarrascoNo ratings yet
- Short Term (Without Rotary)Document1 pageShort Term (Without Rotary)jitu2968No ratings yet
- Creating Videos With Confidence WorkbookDocument29 pagesCreating Videos With Confidence Workbookvero baudensNo ratings yet
- Plano Topografico-A1Document1 pagePlano Topografico-A1HomeroEdwinNo ratings yet
- 17041aa108 DWG PDF-modeldDocument1 page17041aa108 DWG PDF-modeldVishnu ThipparthiNo ratings yet
- Medicinal MushroomsDocument3 pagesMedicinal MushroomsEllice O. MonizNo ratings yet
- Cuenca HuancapiDocument1 pageCuenca HuancapiPia Camila Cabrera DelgadoNo ratings yet
- Flowchart Surdial 55 Plus 1.0 (With Hot Citric Option)Document4 pagesFlowchart Surdial 55 Plus 1.0 (With Hot Citric Option)Hyacinthe KOSSINo ratings yet
- Regional Immigration DataDocument1 pageRegional Immigration Dataapi-300259745No ratings yet
- The Rough Guide to Beijing (Travel Guide eBook)From EverandThe Rough Guide to Beijing (Travel Guide eBook)Rating: 2 out of 5 stars2/5 (1)
- Referee Report TemplateDocument2 pagesReferee Report TemplateAna Jufriani100% (1)
- Not in His Image (15th Anniversary Edition) - Preface and IntroDocument17 pagesNot in His Image (15th Anniversary Edition) - Preface and IntroChelsea Green PublishingNo ratings yet
- Unit 14 - Unemployment and Fiscal Policy - 1.0Document41 pagesUnit 14 - Unemployment and Fiscal Policy - 1.0Georgius Yeremia CandraNo ratings yet
- Mindanao Geothermal v. CIRDocument22 pagesMindanao Geothermal v. CIRMarchini Sandro Cañizares KongNo ratings yet
- Legal Reasoning For Seminal U S Texts Constitutional PrinciplesDocument13 pagesLegal Reasoning For Seminal U S Texts Constitutional PrinciplesOlga IgnatyukNo ratings yet
- PDFDocument86 pagesPDFAnonymous GuMUWwGMNo ratings yet
- Major Landforms of The Earth NotesDocument3 pagesMajor Landforms of The Earth NotesSIMMA SAI PRASANNANo ratings yet
- Case Study of A Condemned Boiler & Methods To Re-Establish ItDocument43 pagesCase Study of A Condemned Boiler & Methods To Re-Establish Its sivaNo ratings yet
- CONSTITUTIONAL - CHANGES - TO - BE - MADE - pdf-SOME IMPORTANT CHANGES TO BE MADE IN THE LANKAN PDFDocument32 pagesCONSTITUTIONAL - CHANGES - TO - BE - MADE - pdf-SOME IMPORTANT CHANGES TO BE MADE IN THE LANKAN PDFThavam RatnaNo ratings yet
- Intro To ForsciDocument16 pagesIntro To ForsciChloe MaciasNo ratings yet
- Power Point Skripsi UmarDocument12 pagesPower Point Skripsi UmarMuchamad Umar Chatab NasserieNo ratings yet
- GLS-LS40GW Specification 20200902Document5 pagesGLS-LS40GW Specification 20200902houyamelkandoussiNo ratings yet
- T-Systems CPNI Policy Statement - Final 022717 PDFDocument2 pagesT-Systems CPNI Policy Statement - Final 022717 PDFFederal Communications Commission (FCC)No ratings yet
- Whyte Human Rights and The Collateral Damage oDocument16 pagesWhyte Human Rights and The Collateral Damage ojswhy1No ratings yet
- Ordinary People Summary ChartDocument2 pagesOrdinary People Summary Chartangela_cristiniNo ratings yet
- Schedule CDocument273 pagesSchedule CAzi PaybarahNo ratings yet
- British Baker Top Bakery Trends 2023Document15 pagesBritish Baker Top Bakery Trends 2023kiagus artaNo ratings yet
- Frs Whatsapp Chat NotesDocument72 pagesFrs Whatsapp Chat NotesFarai NyaniNo ratings yet
- Process of Concept Formation: ReferencesDocument1 pageProcess of Concept Formation: ReferencesRamani SwarnaNo ratings yet
- APPLICATION FOR REGISTRATION/ACCREDITATION AS AN ECOZONE SERVICE ENTERPRISE (For Customs Broker, Freight Forwarder/Trucker and Security Agency)Document7 pagesAPPLICATION FOR REGISTRATION/ACCREDITATION AS AN ECOZONE SERVICE ENTERPRISE (For Customs Broker, Freight Forwarder/Trucker and Security Agency)Albert YsegNo ratings yet
- SG Unit5progresscheckfrq 5e815f88c4fb70Document9 pagesSG Unit5progresscheckfrq 5e815f88c4fb70api-485795043No ratings yet
- Fped 07 00310Document6 pagesFped 07 00310Fariz HidayatNo ratings yet
- Answer KeyDocument21 pagesAnswer KeyJunem S. Beli-otNo ratings yet
- Tata 207 Di LHD Cat.Document253 pagesTata 207 Di LHD Cat.Harneak Singh Gujral100% (4)
- Computer Awareness Topic Wise - TerminologiesDocument15 pagesComputer Awareness Topic Wise - TerminologiesdhirajNo ratings yet