Professional Documents
Culture Documents
Floppy Infant
Floppy Infant
Uploaded by
Rajesh pooniaCopyright:
Available Formats
You might also like
- AES - FluidChart 2020Document1 pageAES - FluidChart 2020Christian De Leon100% (1)
- Health AssessmentttDocument64 pagesHealth AssessmentttAudreySalvador100% (4)
- HypotoniaDocument8 pagesHypotoniavania oktavianiNo ratings yet
- The Floppy Infant:: Evaluation of HypotoniaDocument13 pagesThe Floppy Infant:: Evaluation of HypotoniaminipredatorNo ratings yet
- Floppy BabyDocument13 pagesFloppy BabyJorge JhgNo ratings yet
- Cerebral Palsy An Overview 2018Document11 pagesCerebral Palsy An Overview 2018Yhuliana AcostaNo ratings yet
- Positional Plagiocephaly From Structure To Function Clinic - 2020 - Early HumanDocument6 pagesPositional Plagiocephaly From Structure To Function Clinic - 2020 - Early HumanmireliNo ratings yet
- Neonatal HypotoniaDocument8 pagesNeonatal Hypotoniazulfiqar aliNo ratings yet
- Benign and Severe Early Life Seizures A Round in The First Year of LifeDocument11 pagesBenign and Severe Early Life Seizures A Round in The First Year of LifeClemente PonceNo ratings yet
- The Floppy Newborn-2013Document3 pagesThe Floppy Newborn-2013nikos.alexandrNo ratings yet
- Trastornos Del Movimiento Articulo 2Document7 pagesTrastornos Del Movimiento Articulo 2cfernandfuNo ratings yet
- Hypotonia: A Clinical Sign, Different Etiologies: Keywords: Infant Newborn Muscle Hypotonia/etiologyDocument6 pagesHypotonia: A Clinical Sign, Different Etiologies: Keywords: Infant Newborn Muscle Hypotonia/etiologyAna SopaNo ratings yet
- Impact of Cerebral Palsy Outline: A Research Review: Sharath Hullumani VDocument5 pagesImpact of Cerebral Palsy Outline: A Research Review: Sharath Hullumani VSharath Hullumani VNo ratings yet
- Graham 2016Document25 pagesGraham 2016Constanzza Arellano LeivaNo ratings yet
- The Floppy Infant Contribution of Genetic and MetaDocument21 pagesThe Floppy Infant Contribution of Genetic and MetaMagdaLena02No ratings yet
- Cerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006Document11 pagesCerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006andreas kevinNo ratings yet
- Cerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006Document11 pagesCerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006andreas kevinNo ratings yet
- Neurology History and ExaminationDocument35 pagesNeurology History and ExaminationPhilemon ChizororoNo ratings yet
- Long-Term Follow-Up of Newborns at Neurological Risk: Research Open AccessDocument8 pagesLong-Term Follow-Up of Newborns at Neurological Risk: Research Open Accessleivaherre10No ratings yet
- Development RegessionDocument7 pagesDevelopment RegessionGayanNo ratings yet
- Prenatal Ischemia Deteriorates White Matter, Brain Organization, and FunctionDocument10 pagesPrenatal Ischemia Deteriorates White Matter, Brain Organization, and FunctionJakssuel AlvesNo ratings yet
- Neurogenic BladderDocument8 pagesNeurogenic BladderrafendyfendyNo ratings yet
- Spinal DisDocument32 pagesSpinal DisAkmal Niam FirdausiNo ratings yet
- The Role of Oxytocin in Abnormal Brain DevelopmentDocument31 pagesThe Role of Oxytocin in Abnormal Brain DevelopmentZeljko LekovicNo ratings yet
- Review: Impact of Nutrition On Brain Development and Its Neuroprotective Implications Following Preterm BirthDocument8 pagesReview: Impact of Nutrition On Brain Development and Its Neuroprotective Implications Following Preterm BirthOlivia RamadhaniNo ratings yet
- Approach To The Diagnosis of Congenital Myopathies PIIS0960896613009942Document20 pagesApproach To The Diagnosis of Congenital Myopathies PIIS0960896613009942ElcklymNo ratings yet
- An Approach To A Child With ArthritisDocument9 pagesAn Approach To A Child With Arthritispadamati govardhan reddy reddyNo ratings yet
- Cranial Ultrasound Findings in Late Preterm Infants and Correlation With Perinatal Risk FactorsDocument7 pagesCranial Ultrasound Findings in Late Preterm Infants and Correlation With Perinatal Risk FactorsM Ibnu Rahman SyahNo ratings yet
- Recent Advances in Cerebral PalsyDocument16 pagesRecent Advances in Cerebral PalsyTasyaNo ratings yet
- Evaluation and Management of The Dizzy PatientDocument9 pagesEvaluation and Management of The Dizzy Patientsara mohamedNo ratings yet
- Biomedical Journal: SciencedirectDocument11 pagesBiomedical Journal: SciencedirectTahir AlyasNo ratings yet
- Crum Rine 2001Document12 pagesCrum Rine 2001FabsscribNo ratings yet
- Approach To The Child With ComaDocument10 pagesApproach To The Child With Comapradeepgullipalli.1089No ratings yet
- Bahan Ajar Iv Spina BifidaDocument7 pagesBahan Ajar Iv Spina Bifidaanon_800290919No ratings yet
- CNS ST 6 CDocument13 pagesCNS ST 6 CEuiJinMoonNo ratings yet
- Neonatal Hypoxic Ischemic Encephalopathy: An Update On Disease Pathogenesis and TreatmentDocument12 pagesNeonatal Hypoxic Ischemic Encephalopathy: An Update On Disease Pathogenesis and TreatmentJavier Miranda MalleaNo ratings yet
- Cerebral Palsy Etiology, Evaluation, and Management of The Most Common Cause For Pediatric DisabilityDocument14 pagesCerebral Palsy Etiology, Evaluation, and Management of The Most Common Cause For Pediatric DisabilityDavid ParraNo ratings yet
- Palsy Etiology, Pathophysiology and Therapeutic InterventionsDocument43 pagesPalsy Etiology, Pathophysiology and Therapeutic InterventionsJakssuel AlvesNo ratings yet
- Management of Neonatal Seizures: AIIMS-NICU Protocols 2010Document18 pagesManagement of Neonatal Seizures: AIIMS-NICU Protocols 2010gitphillipNo ratings yet
- Neurodesarrollo en El NICUDocument11 pagesNeurodesarrollo en El NICUvaleria tabares sanchezNo ratings yet
- Floppy Infant Syndrome: Overview: Jaspreet Kaur, Sonu PuniaDocument10 pagesFloppy Infant Syndrome: Overview: Jaspreet Kaur, Sonu PuniaSrishti MannNo ratings yet
- Newborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersDocument11 pagesNewborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- Classification Systems in Cerebral PalsyDocument11 pagesClassification Systems in Cerebral PalsyLizza Mora RNo ratings yet
- Congenital Hypotonia - Is There An Algorithm-2004Document5 pagesCongenital Hypotonia - Is There An Algorithm-2004nikos.alexandrNo ratings yet
- 1 s2.0 S2255482312702126 MainDocument9 pages1 s2.0 S2255482312702126 MainsarinovitapratiwiNo ratings yet
- Biomedicines 10 00965 v2Document25 pagesBiomedicines 10 00965 v2Nia AvellanedaNo ratings yet
- Medico Legal Aspects of Severe Traumatic Brain InjuryDocument17 pagesMedico Legal Aspects of Severe Traumatic Brain InjuryIrv CantorNo ratings yet
- Upadhyay 2020Document11 pagesUpadhyay 2020DellNo ratings yet
- Neurologic Clinics Pediatric Neurology Part IDocument296 pagesNeurologic Clinics Pediatric Neurology Part IPirokunNo ratings yet
- Hypoxic Ischemic Neonatal Encephalopathy - Emerging Therapeutic Strategies Based On Pathophysiological Phases of The Lesion.Document9 pagesHypoxic Ischemic Neonatal Encephalopathy - Emerging Therapeutic Strategies Based On Pathophysiological Phases of The Lesion.Fernando ArancibiaNo ratings yet
- 884-Article Text-4451-1-10-20210212 PDFDocument6 pages884-Article Text-4451-1-10-20210212 PDFNdamale NicholasNo ratings yet
- First Seizure ApproachDocument8 pagesFirst Seizure ApproachPrankur PandeyNo ratings yet
- Ataxia in ChildrenDocument9 pagesAtaxia in ChildrenMuhammad Irvan AvandiNo ratings yet
- Hercules Baby - A Rare Case Presentation of Congenital MyopathyDocument4 pagesHercules Baby - A Rare Case Presentation of Congenital MyopathyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 10.1007@s00381 020 04746 9Document12 pages10.1007@s00381 020 04746 9Alvaro Perez HenriquezNo ratings yet
- Approach To Floppy InfantDocument7 pagesApproach To Floppy InfantLee Chiang ShengNo ratings yet
- Cerebral PalsyDocument8 pagesCerebral PalsyAlin CiubotaruNo ratings yet
- Unit Nursing Care of Children With Central Nervous System Disowe RsDocument32 pagesUnit Nursing Care of Children With Central Nervous System Disowe RsalaineaNo ratings yet
- Evaluation and Management of The Dizzy Patient: L M LuxonDocument8 pagesEvaluation and Management of The Dizzy Patient: L M LuxonCarolina Sepulveda RojasNo ratings yet
- Si Ewert SenDocument12 pagesSi Ewert SenErsya MuslihNo ratings yet
- DialoguesClinNeurosci 20 301Document26 pagesDialoguesClinNeurosci 20 301Erick HernandezNo ratings yet
- Allergic Reaction To Hyaluronidase Use After Hyaluronic Acid Filler InjectionDocument4 pagesAllergic Reaction To Hyaluronidase Use After Hyaluronic Acid Filler InjectionJennifer Villarroel CarrascoNo ratings yet
- Microbiology 200 PointsDocument11 pagesMicrobiology 200 PointsHassan Ahmad100% (1)
- Nurse CpdprogramDocument104 pagesNurse CpdprogramPRC Board100% (1)
- UveitisDocument90 pagesUveitisfranceseyemd89% (9)
- In Vitro Callus Induction of Saffron (Crocus Sativus L.)Document5 pagesIn Vitro Callus Induction of Saffron (Crocus Sativus L.)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Should I Ask My Friends If They AreDocument3 pagesShould I Ask My Friends If They AreMike ReyesNo ratings yet
- Aphasia AssessmentDocument6 pagesAphasia Assessment蔡季霖No ratings yet
- ScleritisDocument3 pagesScleritisPangala NitaNo ratings yet
- Prof Djoko - Autoimmune Kidney Disease v2 ENGDocument35 pagesProf Djoko - Autoimmune Kidney Disease v2 ENGlaboratorium spektrumNo ratings yet
- Deferasirox-An Oral Agent For Chronic Iron Overload: New Drug DevelopmentsDocument8 pagesDeferasirox-An Oral Agent For Chronic Iron Overload: New Drug DevelopmentsTriska Maharani Manoppo100% (1)
- Lana21831enc 002Document235 pagesLana21831enc 00226desemberNo ratings yet
- STELLAR Study (Rosuvastatina)Document44 pagesSTELLAR Study (Rosuvastatina)ijido_sc100% (1)
- Benjamin CarsonDocument84 pagesBenjamin CarsonElena FlorentinaNo ratings yet
- How To Speak So People Really Listen Sample ChapterDocument25 pagesHow To Speak So People Really Listen Sample ChapterCapstone PublishingNo ratings yet
- Multiple Choice Questions: Control of Body MovementDocument20 pagesMultiple Choice Questions: Control of Body MovementwanderagroNo ratings yet
- Local Flap Reconstruction of Large Scalp DefectsDocument5 pagesLocal Flap Reconstruction of Large Scalp DefectsPalwasha MalikNo ratings yet
- Barrie Trower Confidential Report On TETRA 2001Document65 pagesBarrie Trower Confidential Report On TETRA 2001MA-DocNo ratings yet
- Hydrophobic Zeolite ManuscriptDocument27 pagesHydrophobic Zeolite ManuscriptKayla Cshane Dela CruzNo ratings yet
- The Fentanyl Story: Theodore H. StanleyDocument12 pagesThe Fentanyl Story: Theodore H. StanleyRafael GaytanNo ratings yet
- Traditional Herbal Drugs of Southern Uganda, II - Literature Analysis and Antimicrobial AssaysDocument22 pagesTraditional Herbal Drugs of Southern Uganda, II - Literature Analysis and Antimicrobial AssaysMinyty LeNo ratings yet
- Various Kinds of Leave Admissible To Tamil Nadu Government ServantsDocument16 pagesVarious Kinds of Leave Admissible To Tamil Nadu Government Servantssankkitha100% (1)
- Trematodes MidtermsDocument20 pagesTrematodes MidtermsThea GonzalesNo ratings yet
- 5-1 Organoleptic SpoilageDocument5 pages5-1 Organoleptic SpoilageMichaela ZacharovovaNo ratings yet
- Functional FoodsDocument52 pagesFunctional FoodsMade DesmantaNo ratings yet
- Gridrasi HDocument92 pagesGridrasi HramNo ratings yet
- Effect of Urea On Plants GrowthDocument20 pagesEffect of Urea On Plants GrowthPallavi RajNo ratings yet
- CertificateDocument1 pageCertificateamit singhNo ratings yet
- Thesun 2009-10-09 Page02 Isa Review Govt To Study Laws in 18 CountriesDocument1 pageThesun 2009-10-09 Page02 Isa Review Govt To Study Laws in 18 CountriesImpulsive collectorNo ratings yet
Floppy Infant
Floppy Infant
Uploaded by
Rajesh pooniaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Floppy Infant
Floppy Infant
Uploaded by
Rajesh pooniaCopyright:
Available Formats
[Downloaded free from http://www.pediatricneurosciences.com on Saturday, March 14, 2020, IP: 103.207.14.
204]
Review Article
A structured approach to the assessment of a
floppy neonate
Molla Imaduddin Ahmed, Mehtab Iqbal, Nahin Hussain
Department of Paediatrics, Leicester Royal Infirmary, University Hospitals of Leicester, Leicester, United Kingdom
Address for correspondence: Dr. Molla Imaduddin Ahmed, Leicester Royal Infirmary, University Hospitals of Leicester, Infirmary Square,
Leicester, LE1 5WW, United Kingdom. E‑mail: drahmed38@gmail.com
ABSTRACT
Hypotonia in a newborn presents a diagnostic challenge for clinicians. It is an important clinical feature that
may indicate an underlying systemic illness or neurological problem at the level of the central or peripheral
nervous system. It is important to know the different presentations of hypotonia and to have the knowledge of
the diagnostic work up which requires multidisciplinary assessment and input and the prognostic implications of
these disorders. This review article presents a structured approach highlighting initial assessment, examination,
and management of a neonate with generalized hypotonia.
Key words: Floppy neonate, hypotonia, structured approach
Introduction Important Aspects in History and
Hypotonia in a newborn poses a diagnostic challenge
Examination
for neonatologists and pediatricians, as it is a clinical
sign suggestive of both benign and serious conditions. Prenatal, neonatal, and perinatal history
The differential diagnosis for neonatal hypotonia is The list of differential diagnosis of hypotonia in neonates is long,
extensive and a methodical approach helps in localizing but a good history will narrow the possibilities. A detailed family
the problem to a specific region of the nervous system history may be very helpful: A family history of neuromuscular
and formulating a differential diagnosis. Most of these disease needs to be elicited; a history of repeated abortions
neonates need prolonged mechanical ventilation, and may suggest a variety of disorders with prenatal onset,
diagnosing the underlying cause helps plan the management developmental delay (a chromosomal abnormality), delayed
and inform the parents about the prognosis. This review motor milestones (a congenital myopathy), and premature
article presents a structured approach highlighting initial death (metabolic or muscle disease).[1]
assessment, examination, and management of a neonate
with generalized hypotonia. Details of pregnancy, delivery, and postnatal period are
important. Prenatal risk factors include parental age,
Access this article online This is an open access article distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows
Quick Response Code:
others to remix, tweak, and build upon the work non‑commercially, as long as the
Website:
author is credited and the new creations are licensed under the identical terms.
www.pediatricneurosciences.com
For reprints contact: reprints@medknow.com
DOI:
10.4103/1817-1745.181250 Cite this article as: Ahmed MI, Iqbal M, Hussain N. A structured approach
to the assessment of a floppy neonate. J Pediatr Neurosci 2016;11:2-6.
2 / © 2016 Journal of Pediatric Neurosciences | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.pediatricneurosciences.com on Saturday, March 14, 2020, IP: 103.207.14.204]
Ahmed, et al.: Assessment of a floppy neonate
consanguinity, a history of drug or teratogen exposure, hypotonia and examining mother may reveal the features of
maternal diseases (diabetes/epilepsy), reduced fetal myotonia. Likewise, neonatal myasthenia may be suspected
movements, polyhydramnios, and breech presentation. if mother displays fatigability of eyelids on upward gaze and
History of congenital infections ‑ toxoplasmosis, rubella, fatigability of arms with sustained forward extension.[1]
cytomegalovirus, herpes simplex, and any history of pre‑ or
post‑natal insult increase the likelihood of central nervous The major task in the evaluation of a hypotonic neonate is
system (CNS) dysfunction as the underlying cause of to determine the anatomic level of the pathology; whether
hypotonia.[2] It is also important to evaluate the mother for it is central or peripheral in origin. The pattern of weakness
muscle weakness and myotonia.[3] and muscle involvement may help to localize the involved
region in the nervous system [Table 1].
Meticulous documentation of any delivery complications,
perinatal birth trauma, low Apgar scores, and time of onset
of the hypotonia should be done. A detailed history regarding Clinical Features of Central Hypotonia
the degree of weakness and its progression should be recorded.
These hypotonic neonates show signs of abnormal
An abnormal fetal presentation and a shortened umbilical consciousness, seizures, apneas, abnormal posturing, and
cord indicate poor fetal movement and may point toward feeding difficulties. Muscle power is relatively preserved and
neuromuscular disorder.[2] Neonates who need mechanical axial weakness is a significant clinical feature. The tendon
ventilation soon after birth have significant muscle weakness. reflexes are normal or hyperactive, and there is no evidence
Inborn error of metabolism should be considered in neonates of muscle fasciculations.[10] Diminished or absent tendon
who are born with normal pregnancy and delivery who later reflexes point toward lower motor neuron lesion and brisk
on develop hypotonia after a period of normality.[4] reflexes indicate CNS dysfunctions.[1]
Tight fisting of the hands, which do not open spontaneously,
Clinical examination and in which the thumbs are enclosed by the other fingers
Clinical examination is the key in narrowing the differential or adducted across the palmar surface, and adduction of
diagnosis. The physical examination should include the the thighs such that the legs are crossed when the infant is
assessment of relevant clinical signs including a detailed held in vertical suspension (scissoring) may be evidence of
neurologic evaluation and an assessment for dysmorphic spasticity.[11]
features.[5,6] The presence of congenital malformations in
other organ systems and dysmorphic features indicates a Postural reflexes are generally preserved in infants with cerebral
possible syndromic diagnosis. Important conditions to rule hypotonia despite a paucity of spontaneous movements. In
out are trisomy 21 where hypotonia is associated with short some acute encephalopathies, the Moro reflex may be
stature,[7] characteristic facies and cardiac anomalies,[8] and exaggerated.[11]
Prader–Willi syndrome where hypotonia is associated with
characteristic facial features, reduced deep tendon reflexes,
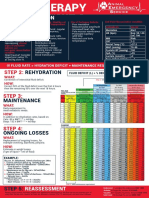
Table 1: Differentiating the features of a floppy
feeding difficulties, and hypogonadism.[9] neonate according to the site of involvement[2,11]
Site of Clinical features Differential diagnoses
It is important to determine whether the baby has low tone involvement
with or without weakness. Tone is defined as resistance of Central Central hypotonia Brain malformations
muscle to stretch, therefore babies with hypotonia have Brisk or normal tendon Perinatal asphyxia
decreased resistance on passive stretching.[5] On the other reflexes Chromosomal disorders
hand, weakness is decreased muscle strength or power.[6] Lack Preserved neonatal Inborn errors of
reflexes metabolism
of spontaneous movement in a baby suggests weakness. Most Abnormal brain function
hypotonic neonates demonstrate a characteristic frog‑legged Anterior horn Generalized weakness Spinomuscular atrophy
posture‑full abduction and external rotation of the legs as well cell and absent deep
as a flaccid extension of the arms.[1] Other signs of hypotonia tendon reflexes
include head lag, slip‑through on vertical suspension, and Nerve Distal muscle weakness Peripheral neuropathy
and wasting
draping on ventral suspension. Decreased tendon
reflexes
Weakness can be assessed by the cry, facial expressions, Neuromuscular Involvement of facial Myasthenia gravis
sucking and Moro’s reflex, antigravity movements, and junction muscles with or without botulism
respiratory effort. It is important to evaluate the distribution generalized weakness
Muscle Weakness Congenital muscular
and progression of weakness in differentiating the causes of Decreased tendon dystrophy
neonatal hypotonia. reflexes Congenital myotonic
Fasciculations joint dystrophy
Physical examination of parents may also provide useful cues contractures Congenital and
as babies with congenital myotonic dystrophy have severe metabolic myopathy
2016 / Jan-Mar / Volume 11 / Journal of Pediatric Neurosciences / 3
[Downloaded free from http://www.pediatricneurosciences.com on Saturday, March 14, 2020, IP: 103.207.14.204]
Ahmed, et al.: Assessment of a floppy neonate
Clinical Features of Peripheral congenital muscular dystrophies, metabolic myopathies,
and some forms of the congenital myopathies. The blood
Hypotonia for CK measurement should be obtained before performing
the electromyography or muscle biopsy, as these procedures
Babies with anterior horn cell disease usually have sparing of may cause false elevation of CK levels. The CK and
extra‑ocular muscles while the disorders of neuromuscular iso‑enzyme levels may be increased 10‑fold for up to 1 week
junctions may have ptosis and extra‑ocular muscle following normal vaginal delivery (presumably due to muscle
weakness.[6] These infants appear more alert in comparison trauma). The CK may be even higher in the context of
to those with CNS involvement. There is weakness in acidosis (e.g., severely asphyxiated newborns). [11] Other
the antigravity limb muscles along with diminished or biochemical investigations (e.g., serum lactate and carnitine
absent reflexes. They can have deformities of bones or levels) may be required in specific circumstances.
joints (arthrogryposis).[2] Fasciculations, often observed in
the tongue, are often very difficult to distinguish from normal
random tongue movements. Postural reflexes are absent or Chest X‑ray
diminished, and limbs that lack voluntary movement also A chest radiograph may demonstrate enlarged cardiac
cannot move reflexively. shadows indicating cardiomyopathy or thin ribs, related to
reduced fetal respiratory movements. The latter observation
is a useful clue to antenatal onset of neuromuscular disease.
Investigations An enlarged heart on chest X‑ray may suggest Pompe disease.
Appropriate use of investigations is necessary to establish a
specific etiologic diagnosis and should be guided by the history Lumbar puncture
and physical examination. We suggest a systematic approach Cerebrospinal fluid (CSF) analysis is important to rule out
based on the tests currently utilized in the evaluation of infants neuroinfections. Markedly, increased protein concentration
with hypotonia. Clinical details and relevant diagnostic tests in CSF may indicate peripheral neuropathy or specific
are discussed in conjunction with specific disorders. degenerative conditions.
Here is a list of investigations for neonates with hypotonia Screening for inborn errors of metabolism
(a schematic approach to the diagnosis of neonatal hypotonia
is shown in Figure 1). If the clinical picture suggests multisystem involvement,
screening should be done for inborn errors of metabolism.[4]
Neuroimaging
Electrophysiological studies
In babies with features of central hypotonia, neuroimaging is
a valuable tool for diagnosis. Cranial and spinal neuroimaging Nerve conduction and electromyogram studies are useful
(computed tomography/magnetic resonance imaging) studies in the assessment of disorders affecting the lower motor
are helpful in the identification of structural malformations, unit. Electromyography[15] is very helpful in establishing
neuronal migration defects, brain stem and cerebellar the diagnosis of SMA and disorders of the neuromuscular
abnormalities, and can identify features suggestive of junction (botulism and congenital forms of myasthenia
mitochondrial abnormalities and metabolic diseases. gravis).
Nerve conduction studies are consistent and reliable after
Genetic studies 32 weeks of gestation. [11] Nerve conduction velocities
These tests should be chosen according to the clinical may be very slow or unrecordable in congenital peripheral
presentation of the infants. The karyotype will disclose any neuropathies. Nerve conduction studies and electromyography
genetic defects such as chromosomal duplications, deletions, are also useful in diagnosing hereditary motor sensory
trisomies such as Down syndrome (Trisomy 21), and disorders neuropathies and in differentiating axonal disorders from
of genetic imprinting such as Prader Willi syndrome. demyelinating conditions. [16,17] Slow nerve conduction
Molecular genetic tests may also help in the diagnosis of spinal velocity and conduction block favor peripheral nerve
muscular atrophy (SMA) (deletion of SMN gene)[12,13] and involvement.
myotonic dystrophy (trinucleotide repeats).[14]
Muscle and nerve biopsies
Blood investigations These investigations should be considered, even if the
Blood investigations including full blood count, electrolytes, electrophysiological studies are normal.[18] Muscle biopsy
and inflammatory markers are important to rule out with immunohistochemical staining and electron microscopy
systemic disorders causing hypotonia including sepsis and is the method of choice for differentiating myopathies and
dyselectrolytemias. Muscle enzymes (creatine kinase [CK] muscular dystrophies, although it is more invasive. If biopsy
assay) are helpful in diagnosing muscle disorders such as shows specific abnormalities, it can be an essential part of the
4 / Journal of Pediatric Neurosciences / Volume 11 / Jan-Mar / 2016
[Downloaded free from http://www.pediatricneurosciences.com on Saturday, March 14, 2020, IP: 103.207.14.204]
Ahmed, et al.: Assessment of a floppy neonate
Floppy neonate
History and physical examination
Hypotonia with abnormal consciousness, seizures, Hypotonia, weakness, alert look, fasciculations,
apnea, abnormal posturing, and feeding difficulties absent or reduced tendon reflexes
Muscle weakness in mother
CT/MRI, Screening for IEM, Septic screen,
CSF analysis, Karyotype
Yes
No Maternal myotonia
Perinatal asphyxia, cerebral malformations, IEM,
sepsis, chromosomal disorders
Yes No
Myotonic History of
Creatine kinase dystrophy myasthenia
in mother
High Normal
Congenital DNA testing for spinal
muscular muscular atrophy (SMN) Yes SMA
dystrophy Transient
Negative myasthenia
gravis – AchR
Ab and
EMG and NCS edrophonium
test
Myopathic Neuropathic Neuromuscular transmission defect
NCV
Congenital Transient myasthenia gravis,
myopathies Reduced congenital myasthenia syndromes
Normal
Peripheral
Neuropathy
Confirm by SMA
muscle biopsy
Confirm by
nerve biopsy
Figure 1: Evaluation of a neonate with generalized hypotonia.[2,5,10,19] CT: Computed tomography, MRI: Magnetic resonance imaging, IEM: Inborn errors of
metabolism, CSF: Cerebrospinal fluid, NCV: Nerve conduction velocity, SMA: Spinal muscular atrophy, NCS: Nerve conduction study
diagnostic evaluation in the newborn to guide subsequent neonates need prolonged mechanical ventilation. Regular
DNA molecular diagnostic studies. physiotherapy is needed to aid the clearance of respiratory
secretions and will prevent limb contractures. It is vital to
aggressively treat any respiratory infections. Feeding should
What is the Management of this Clinical be initiated by nasogastric tube and gastrostomy may be
Presentation? needed for few babies. Weight should be closely monitored as
excessive weight gain can worsen existing muscle weakness.
Hypotonia is an important clinical presentation at birth or in
the first few days of life. A specific diagnosis can help tailor Children with neuromuscular disorders need attention if they
the management and explain the prognosis to parents. require anesthesia. Muscle relaxants should only be used
if necessary as they have a more prolonged effect in these
It is very important to continue supportive care with children. They are also susceptible to malignant hyperthermia
regards to feeding and respiration. Most of these hypotonic and implicating agents should be avoided.[20]
2016 / Jan-Mar / Volume 11 / Journal of Pediatric Neurosciences / 5
[Downloaded free from http://www.pediatricneurosciences.com on Saturday, March 14, 2020, IP: 103.207.14.204]
Ahmed, et al.: Assessment of a floppy neonate
It is important to ensure multidisciplinary follow‑up for 2. Prasad AN, Prasad C. The floppy infant: Contribution of genetic and
neonates with neuromuscular disorders. Follow‑up should metabolic disorders. Brain Dev 2003;25:457‑76.
be arranged with neurologist and respiratory team, and an 3. Dubowitz V, editor. The floppy infant syndrome. In: Muscle Disorders in
Childhood. 2nd ed. London: WB Saunders Company; 1995. p. 457‑72.
appointment with the geneticist for genetic counseling should
4. Tein I. Neonatal metabolic myopathies. Semin Perinatol 1999;23:125‑51.
be offered. 5. Fenichel GM, editor. The hypotonic infant. In: Clinical Pediatric
Neurology: A Signs and Symptoms Approach. 4th ed. Philadelphia:
If there are symptoms and signs of severe neuromuscular WB Saunders Company; 2001. p. 149‑69.
involvement at birth (with respiratory insufficiency, lack 6. Crawford TO. Clinical evaluation of the floppy infant. Pediatr Ann
of swallowing, cough, and tendon reflexes), the prognosis 1992;21:348‑54.
is very poor. Such a presentation should lead to timely 7. Morris AF, Vaughan SE, Vaccaro P. Measurements of neuromuscular
ethical discussions as well as parental counseling and to the tone and strength in Down’s syndrome children. J Ment Defic Res
1982;26(Pt 1):41‑6.
consideration of early extubation. In babies with hypotonia
8. Rogers PT, Coleman M. Medical Care in Down Syndrome. New York:
who survive the neonatal period, it is important to have Dekker; 1992.
detailed discussions sensitively with parents regarding the 9. Cassidy SB, Schwartz S, Miller JL, Driscoll DJ. Prader‑Willi syndrome.
appropriateness of cardiopulmonary resuscitation in the event Genet Med 2012;14:10‑26.
of cardiac arrest or acute respiratory failure. 10. Paro‑Panjan D, Neubauer D. Congenital hypotonia: Is there an
algorithm? J Child Neurol 2004;19:439‑42.
11. Hill A. Neonatal hypotonia. In: Maria BL, editor. Current Management
Conclusion in Child Neurology. 3rd ed. Hamilton: B C Decker Inc.; 2005. p. 529‑34.
12. Vitali T, Sossi V, Tiziano F, Zappata S, Giuli A, Paravatou‑Petsotas M,
The list of differential diagnoses for floppiness in the neonatal et al. Detection of the survival motor neuron (SMN) genes by FISH:
Further evidence for a role for SMN2 in the modulation of disease
age group is extensive. However, most of these neonates
severity in SMA patients. Hum Mol Genet 1999;8:2525‑32.
have distinctive features in their family history, history at 13. Lefebvre S, Bürglen L, Frézal J, Munnich A, Melki J. The role of the
presentation, and their physical examination that can help SMN gene in proximal spinal muscular atrophy. Hum Mol Genet
differentiate them into central and peripheral disorders, and 1998;7:1531‑6.
sometimes can lead to specific diagnoses within these groups. 14. Kamsteeg EJ, Kress W, Catalli C, Hertz JM, Witsch‑Baumgartner M,
As there are frequent implications for future pregnancies, and Buckley MF, et al. Best practice guidelines and recommendations on the
specific treatments are available in a few disorders, we should molecular diagnosis of myotonic dystrophy types 1 and 2. Eur J Hum
strive for an accurate diagnosis in these neonates. Genet 2012;20:1203‑8.
15. David WS, Jones HR Jr. Electromyography and biopsy correlation with
suggested protocol for evaluation of the floppy infant. Muscle Nerve
Financial support and sponsorship 1994;17:424‑30.
16. Renault F. The role of electrodiagnostic studies in the diagnosis of
Nil.
hypotonia in infancy. Rev Med Liege 2004;59 Suppl 1:190‑7.
17. Russell JW, Afifi AK, Ross MA. Predictive value of electromyography
Conflicts of interest in diagnosis and prognosis of the hypotonic infant. J Child Neurol
1992;7:387‑91.
There are no conflicts of interest. 18. Richer LP, Shevell MI, Miller SP. Diagnostic profile of neonatal
hypotonia: An 11‑year study. Pediatr Neurol 2001;25:32‑7.
19. Hahn JS, Henry M, Hudgins L, Madan A. Congenital hypomyelination
References neuropathy in a newborn infant: Unusual cause of diaphragmatic and
vocal cord paralyses. Pediatrics 2001;108:E95.
1. Leyenaar J, Camfield P, Camfield C. A schematic approach to hypotonia 20. Wedel DJ. Malignant hyperthermia and neuromuscular disease.
in infancy. Paediatr Child Health 2005;10:397‑400. Neuromuscul Disord 1992;2:157‑64.
6 / Journal of Pediatric Neurosciences / Volume 11 / Jan-Mar / 2016
You might also like
- AES - FluidChart 2020Document1 pageAES - FluidChart 2020Christian De Leon100% (1)
- Health AssessmentttDocument64 pagesHealth AssessmentttAudreySalvador100% (4)
- HypotoniaDocument8 pagesHypotoniavania oktavianiNo ratings yet
- The Floppy Infant:: Evaluation of HypotoniaDocument13 pagesThe Floppy Infant:: Evaluation of HypotoniaminipredatorNo ratings yet
- Floppy BabyDocument13 pagesFloppy BabyJorge JhgNo ratings yet
- Cerebral Palsy An Overview 2018Document11 pagesCerebral Palsy An Overview 2018Yhuliana AcostaNo ratings yet
- Positional Plagiocephaly From Structure To Function Clinic - 2020 - Early HumanDocument6 pagesPositional Plagiocephaly From Structure To Function Clinic - 2020 - Early HumanmireliNo ratings yet
- Neonatal HypotoniaDocument8 pagesNeonatal Hypotoniazulfiqar aliNo ratings yet
- Benign and Severe Early Life Seizures A Round in The First Year of LifeDocument11 pagesBenign and Severe Early Life Seizures A Round in The First Year of LifeClemente PonceNo ratings yet
- The Floppy Newborn-2013Document3 pagesThe Floppy Newborn-2013nikos.alexandrNo ratings yet
- Trastornos Del Movimiento Articulo 2Document7 pagesTrastornos Del Movimiento Articulo 2cfernandfuNo ratings yet
- Hypotonia: A Clinical Sign, Different Etiologies: Keywords: Infant Newborn Muscle Hypotonia/etiologyDocument6 pagesHypotonia: A Clinical Sign, Different Etiologies: Keywords: Infant Newborn Muscle Hypotonia/etiologyAna SopaNo ratings yet
- Impact of Cerebral Palsy Outline: A Research Review: Sharath Hullumani VDocument5 pagesImpact of Cerebral Palsy Outline: A Research Review: Sharath Hullumani VSharath Hullumani VNo ratings yet
- Graham 2016Document25 pagesGraham 2016Constanzza Arellano LeivaNo ratings yet
- The Floppy Infant Contribution of Genetic and MetaDocument21 pagesThe Floppy Infant Contribution of Genetic and MetaMagdaLena02No ratings yet
- Cerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006Document11 pagesCerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006andreas kevinNo ratings yet
- Cerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006Document11 pagesCerebral Palsy: Comprehensive Review and Update: Annals of Saudi Medicine March 2006andreas kevinNo ratings yet
- Neurology History and ExaminationDocument35 pagesNeurology History and ExaminationPhilemon ChizororoNo ratings yet
- Long-Term Follow-Up of Newborns at Neurological Risk: Research Open AccessDocument8 pagesLong-Term Follow-Up of Newborns at Neurological Risk: Research Open Accessleivaherre10No ratings yet
- Development RegessionDocument7 pagesDevelopment RegessionGayanNo ratings yet
- Prenatal Ischemia Deteriorates White Matter, Brain Organization, and FunctionDocument10 pagesPrenatal Ischemia Deteriorates White Matter, Brain Organization, and FunctionJakssuel AlvesNo ratings yet
- Neurogenic BladderDocument8 pagesNeurogenic BladderrafendyfendyNo ratings yet
- Spinal DisDocument32 pagesSpinal DisAkmal Niam FirdausiNo ratings yet
- The Role of Oxytocin in Abnormal Brain DevelopmentDocument31 pagesThe Role of Oxytocin in Abnormal Brain DevelopmentZeljko LekovicNo ratings yet
- Review: Impact of Nutrition On Brain Development and Its Neuroprotective Implications Following Preterm BirthDocument8 pagesReview: Impact of Nutrition On Brain Development and Its Neuroprotective Implications Following Preterm BirthOlivia RamadhaniNo ratings yet
- Approach To The Diagnosis of Congenital Myopathies PIIS0960896613009942Document20 pagesApproach To The Diagnosis of Congenital Myopathies PIIS0960896613009942ElcklymNo ratings yet
- An Approach To A Child With ArthritisDocument9 pagesAn Approach To A Child With Arthritispadamati govardhan reddy reddyNo ratings yet
- Cranial Ultrasound Findings in Late Preterm Infants and Correlation With Perinatal Risk FactorsDocument7 pagesCranial Ultrasound Findings in Late Preterm Infants and Correlation With Perinatal Risk FactorsM Ibnu Rahman SyahNo ratings yet
- Recent Advances in Cerebral PalsyDocument16 pagesRecent Advances in Cerebral PalsyTasyaNo ratings yet
- Evaluation and Management of The Dizzy PatientDocument9 pagesEvaluation and Management of The Dizzy Patientsara mohamedNo ratings yet
- Biomedical Journal: SciencedirectDocument11 pagesBiomedical Journal: SciencedirectTahir AlyasNo ratings yet
- Crum Rine 2001Document12 pagesCrum Rine 2001FabsscribNo ratings yet
- Approach To The Child With ComaDocument10 pagesApproach To The Child With Comapradeepgullipalli.1089No ratings yet
- Bahan Ajar Iv Spina BifidaDocument7 pagesBahan Ajar Iv Spina Bifidaanon_800290919No ratings yet
- CNS ST 6 CDocument13 pagesCNS ST 6 CEuiJinMoonNo ratings yet
- Neonatal Hypoxic Ischemic Encephalopathy: An Update On Disease Pathogenesis and TreatmentDocument12 pagesNeonatal Hypoxic Ischemic Encephalopathy: An Update On Disease Pathogenesis and TreatmentJavier Miranda MalleaNo ratings yet
- Cerebral Palsy Etiology, Evaluation, and Management of The Most Common Cause For Pediatric DisabilityDocument14 pagesCerebral Palsy Etiology, Evaluation, and Management of The Most Common Cause For Pediatric DisabilityDavid ParraNo ratings yet
- Palsy Etiology, Pathophysiology and Therapeutic InterventionsDocument43 pagesPalsy Etiology, Pathophysiology and Therapeutic InterventionsJakssuel AlvesNo ratings yet
- Management of Neonatal Seizures: AIIMS-NICU Protocols 2010Document18 pagesManagement of Neonatal Seizures: AIIMS-NICU Protocols 2010gitphillipNo ratings yet
- Neurodesarrollo en El NICUDocument11 pagesNeurodesarrollo en El NICUvaleria tabares sanchezNo ratings yet
- Floppy Infant Syndrome: Overview: Jaspreet Kaur, Sonu PuniaDocument10 pagesFloppy Infant Syndrome: Overview: Jaspreet Kaur, Sonu PuniaSrishti MannNo ratings yet
- Newborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersDocument11 pagesNewborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- Classification Systems in Cerebral PalsyDocument11 pagesClassification Systems in Cerebral PalsyLizza Mora RNo ratings yet
- Congenital Hypotonia - Is There An Algorithm-2004Document5 pagesCongenital Hypotonia - Is There An Algorithm-2004nikos.alexandrNo ratings yet
- 1 s2.0 S2255482312702126 MainDocument9 pages1 s2.0 S2255482312702126 MainsarinovitapratiwiNo ratings yet
- Biomedicines 10 00965 v2Document25 pagesBiomedicines 10 00965 v2Nia AvellanedaNo ratings yet
- Medico Legal Aspects of Severe Traumatic Brain InjuryDocument17 pagesMedico Legal Aspects of Severe Traumatic Brain InjuryIrv CantorNo ratings yet
- Upadhyay 2020Document11 pagesUpadhyay 2020DellNo ratings yet
- Neurologic Clinics Pediatric Neurology Part IDocument296 pagesNeurologic Clinics Pediatric Neurology Part IPirokunNo ratings yet
- Hypoxic Ischemic Neonatal Encephalopathy - Emerging Therapeutic Strategies Based On Pathophysiological Phases of The Lesion.Document9 pagesHypoxic Ischemic Neonatal Encephalopathy - Emerging Therapeutic Strategies Based On Pathophysiological Phases of The Lesion.Fernando ArancibiaNo ratings yet
- 884-Article Text-4451-1-10-20210212 PDFDocument6 pages884-Article Text-4451-1-10-20210212 PDFNdamale NicholasNo ratings yet
- First Seizure ApproachDocument8 pagesFirst Seizure ApproachPrankur PandeyNo ratings yet
- Ataxia in ChildrenDocument9 pagesAtaxia in ChildrenMuhammad Irvan AvandiNo ratings yet
- Hercules Baby - A Rare Case Presentation of Congenital MyopathyDocument4 pagesHercules Baby - A Rare Case Presentation of Congenital MyopathyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 10.1007@s00381 020 04746 9Document12 pages10.1007@s00381 020 04746 9Alvaro Perez HenriquezNo ratings yet
- Approach To Floppy InfantDocument7 pagesApproach To Floppy InfantLee Chiang ShengNo ratings yet
- Cerebral PalsyDocument8 pagesCerebral PalsyAlin CiubotaruNo ratings yet
- Unit Nursing Care of Children With Central Nervous System Disowe RsDocument32 pagesUnit Nursing Care of Children With Central Nervous System Disowe RsalaineaNo ratings yet
- Evaluation and Management of The Dizzy Patient: L M LuxonDocument8 pagesEvaluation and Management of The Dizzy Patient: L M LuxonCarolina Sepulveda RojasNo ratings yet
- Si Ewert SenDocument12 pagesSi Ewert SenErsya MuslihNo ratings yet
- DialoguesClinNeurosci 20 301Document26 pagesDialoguesClinNeurosci 20 301Erick HernandezNo ratings yet
- Allergic Reaction To Hyaluronidase Use After Hyaluronic Acid Filler InjectionDocument4 pagesAllergic Reaction To Hyaluronidase Use After Hyaluronic Acid Filler InjectionJennifer Villarroel CarrascoNo ratings yet
- Microbiology 200 PointsDocument11 pagesMicrobiology 200 PointsHassan Ahmad100% (1)
- Nurse CpdprogramDocument104 pagesNurse CpdprogramPRC Board100% (1)
- UveitisDocument90 pagesUveitisfranceseyemd89% (9)
- In Vitro Callus Induction of Saffron (Crocus Sativus L.)Document5 pagesIn Vitro Callus Induction of Saffron (Crocus Sativus L.)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Should I Ask My Friends If They AreDocument3 pagesShould I Ask My Friends If They AreMike ReyesNo ratings yet
- Aphasia AssessmentDocument6 pagesAphasia Assessment蔡季霖No ratings yet
- ScleritisDocument3 pagesScleritisPangala NitaNo ratings yet
- Prof Djoko - Autoimmune Kidney Disease v2 ENGDocument35 pagesProf Djoko - Autoimmune Kidney Disease v2 ENGlaboratorium spektrumNo ratings yet
- Deferasirox-An Oral Agent For Chronic Iron Overload: New Drug DevelopmentsDocument8 pagesDeferasirox-An Oral Agent For Chronic Iron Overload: New Drug DevelopmentsTriska Maharani Manoppo100% (1)
- Lana21831enc 002Document235 pagesLana21831enc 00226desemberNo ratings yet
- STELLAR Study (Rosuvastatina)Document44 pagesSTELLAR Study (Rosuvastatina)ijido_sc100% (1)
- Benjamin CarsonDocument84 pagesBenjamin CarsonElena FlorentinaNo ratings yet
- How To Speak So People Really Listen Sample ChapterDocument25 pagesHow To Speak So People Really Listen Sample ChapterCapstone PublishingNo ratings yet
- Multiple Choice Questions: Control of Body MovementDocument20 pagesMultiple Choice Questions: Control of Body MovementwanderagroNo ratings yet
- Local Flap Reconstruction of Large Scalp DefectsDocument5 pagesLocal Flap Reconstruction of Large Scalp DefectsPalwasha MalikNo ratings yet
- Barrie Trower Confidential Report On TETRA 2001Document65 pagesBarrie Trower Confidential Report On TETRA 2001MA-DocNo ratings yet
- Hydrophobic Zeolite ManuscriptDocument27 pagesHydrophobic Zeolite ManuscriptKayla Cshane Dela CruzNo ratings yet
- The Fentanyl Story: Theodore H. StanleyDocument12 pagesThe Fentanyl Story: Theodore H. StanleyRafael GaytanNo ratings yet
- Traditional Herbal Drugs of Southern Uganda, II - Literature Analysis and Antimicrobial AssaysDocument22 pagesTraditional Herbal Drugs of Southern Uganda, II - Literature Analysis and Antimicrobial AssaysMinyty LeNo ratings yet
- Various Kinds of Leave Admissible To Tamil Nadu Government ServantsDocument16 pagesVarious Kinds of Leave Admissible To Tamil Nadu Government Servantssankkitha100% (1)
- Trematodes MidtermsDocument20 pagesTrematodes MidtermsThea GonzalesNo ratings yet
- 5-1 Organoleptic SpoilageDocument5 pages5-1 Organoleptic SpoilageMichaela ZacharovovaNo ratings yet
- Functional FoodsDocument52 pagesFunctional FoodsMade DesmantaNo ratings yet
- Gridrasi HDocument92 pagesGridrasi HramNo ratings yet
- Effect of Urea On Plants GrowthDocument20 pagesEffect of Urea On Plants GrowthPallavi RajNo ratings yet
- CertificateDocument1 pageCertificateamit singhNo ratings yet
- Thesun 2009-10-09 Page02 Isa Review Govt To Study Laws in 18 CountriesDocument1 pageThesun 2009-10-09 Page02 Isa Review Govt To Study Laws in 18 CountriesImpulsive collectorNo ratings yet