Professional Documents
Culture Documents
Harrington 2015
Harrington 2015
Uploaded by
Geoffroy De VilmarestOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Harrington 2015
Harrington 2015
Uploaded by
Geoffroy De VilmarestCopyright:
Available Formats
Published Ahead of Print on November 2, 2015 as 10.1200/JCO.2015.61.
4370
The latest version is at http://jco.ascopubs.org/cgi/doi/10.1200/JCO.2015.61.4370
JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Postoperative Adjuvant Lapatinib and Concurrent
Chemoradiotherapy Followed by Maintenance Lapatinib
Monotherapy in High-Risk Patients With Resected
Squamous Cell Carcinoma of the Head and Neck: A Phase
III, Randomized, Double-Blind, Placebo-Controlled Study
Kevin Harrington, Stephane Temam, Hisham Mehanna, Anil D’Cruz, Minish Jain, Ida D’Onofrio,
Georgy Manikhas, Zsuzsanna Horvath, Yan Sun, Stefan Dietzsch, Pavol Dubinsky, Petra Holeckova,
Iman El-Hariry, Natalie Franklin, Nigel Biswas-Baldwin, Philippe Legenne, Paul Wissel, Thelma Netherway,
John Farrell, Catherine Ellis, Jing Wang-Silvanto, Mayur Amonkar, Nazma Ahmed, Sergio Santillana,
and Jean Bourhis
Author affiliations appear at the end of
this article. A B S T R A C T
Published online ahead of print at Purpose
www.jco.org on November 2, 2015. This multicenter phase III study evaluated the efficacy and safety of lapatinib, an epidermal growth
Supported by GlaxoSmithKline. K.H. factor receptor/ErbB2 inhibitor, administered concomitantly with chemoradiotherapy and as
acknowledges support from the Royal
maintenance monotherapy in patients with high-risk surgically treated squamous cell carcinoma of
Marsden Hospital/Institute of Cancer
Research National Institute for Health
the head and neck (SCCHN).
Research Biomedical Research Centre.
Patients and Methods
GlaxoSmithKline and Novartis funded
Patients with resected stage II to IVA SCCHN, with a surgical margin ⱕ 5 mm and/or extracapsular
editorial support.
extension, were randomly assigned to chemoradiotherapy (66 Gy total radiation dose and cisplatin
K.H. and S.T. contributed equally to this
100 mg/m2 per day administered on days 1, 22, and 43) plus placebo or lapatinib (1,500 mg per
work.
day) before and during chemoradiotherapy, followed by 12 months of maintenance monotherapy.
Presented, in part, at the 50th Annual
Meeting of the American Society of Results
Clinical Oncology, Chicago, IL, May Six hundred eighty-eight patients were enrolled (lapatinib, n ⫽ 346; placebo, n ⫽ 342). With a
30-June 3, 2014. median follow-up time of 35.3 months, the study ended early because of the apparent plateauing
Authors’ disclosures of potential of disease-free survival (DFS) events. Median DFS assessed by an independent review committee
conflicts of interest are found in the was 53.6 months and not reached for lapatinib and placebo, respectively (hazard ratio, 1.10; 95%
article online at www.jco.org. Author CI, 0.85 to 1.43). Investigator-assessed results confirmed the independent review committee
contributions are found at the end of
assessment. No significant differences in DFS by human papillomavirus status or overall survival
this article.
were observed between treatment arms. Similar numbers of patients in both treatment arms
Clinical trial information: NCT00424255. experienced adverse events (AEs), with more patients in the lapatinib arm than the placebo arm
Corresponding author: Jean Bourhis, experiencing serious AEs (48% v 40%, respectively). The most commonly observed treatment-
MD, PhD, University Hospital Centre, related AEs were diarrhea and rash, both predominantly in the lapatinib arm.
Bugnon 46, Vaud, Switzerland; e-mail:
jean.bourhis@chuv.ch. Conclusion
© 2015 by American Society of Clinical Addition of lapatinib to chemoradiotherapy and its use as long-term maintenance therapy does not
Oncology offer any efficacy benefits and had additional toxicity compared with placebo in patients with
0732-183X/15/3399-1/$20.00
surgically treated high-risk SCCHN.
DOI: 10.1200/JCO.2015.61.4370
J Clin Oncol 33. © 2015 by American Society of Clinical Oncology
ity.1 Generally, postoperative radiotherapy is needed
INTRODUCTION
in patients with locally advanced disease treated with
Locally advanced squamous cell carcinoma of the primary surgery. In addition, in high-risk patients
head and neck (SCCHN) remains a therapeutic (with positive resection margins or nodal extracapsular
challenge and is frequently treated with surgery extension [ECE]), postoperative radiotherapy com-
and/or radiotherapy. Long-term remission can be bined with concomitant chemotherapy is indicated.
obtained, but disease recurrence is seen in 15% to The potential benefit of adding chemotherapy
30% of patients at 3 years, depending on factors such to radiotherapy has been demonstrated in an up-
as tumor site and stage, nodal stage, and resectabil- dated meta-analysis of individual data from more
© 2015 by American Society of Clinical Oncology 1
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Copyright 2015 by American Society of Clinical Oncology
Harrington et al
than 16,000 patients with SCCHN in randomized trials that showed 50 Gy to the low-risk planning target volume 1; Appendix, online only) and
that concomitant chemotherapy added significant benefits in 5-year lapatinib (1,500 mg taken orally once per day) or placebo. This was followed by
event-free survival and overall survival (OS).2 Addition of chemother- administration of lapatinib monotherapy (1,500 mg orally once per day) or
placebo for 1 year in the maintenance phase or until disease relapse. Carbopla-
apy to postoperative radiotherapy has also been tested in two large
tin was allowed if cisplatin could not be given after the first or second cycle
phase III randomized studies in high-risk patients with locally ad- because of nephrotoxicity. Dose reductions or delays in randomly assigned
vanced SCCHN. Both studies reported improved disease-free survival treatment were permitted in case of grade 3, 4, or unacceptable adverse events
(DFS) or progression-free survival, although only one study reported (AEs) or AEs consistently associated with lapatinib. An independent program
improved OS.1,3 Long-term results of one of these trials, Radiation of quality assurance and analysis of radiotherapy plans (Radiotherapy Quality
Therapy Oncology Group 95-01, showed relatively high locoregional Assurance) was implemented (EqualEstro, Paris, France), with the aim of
failure rates and poor DFS (⬍ 30% in both arms), suggesting the need ensuring standardized delivery of radiotherapy across treatment arms.
At the time of completion or early discontinuation of study treatment,
for more effective adjuvant therapy in patients with operable SCCHN patients were observed for recurrence every 4 months for 2 years and then
at high risk of relapse.4 every 6 months until withdrawal from the study or death. After disease recur-
Although previous reports suggested that epidermal growth fac- rence, patients were monitored remotely every 6 months for survival outcome.
tor receptor (EGFR, c-ErbB1) is overexpressed in up to 90% of All patients gave written informed consent; the study was performed in accor-
SCCHN tumors, recent data from the Cancer Genome Atlas Network dance with good clinical practice guidelines and the Declaration of Helsinki
suggest that this is a significant overestimate.5 Even so, EGFR-targeted and approved by local ethics committees.
therapies are potentially beneficial for treating SCCHN,6 and this Patient Population
approach has been validated in a phase III trial that established a new Eligible patients had a histologically confirmed diagnosis of SCCHN at
standard of care for locally advanced SCCHN using the chimeric the oral cavity, oropharynx, hypopharynx, or larynx; pathologic stage II, III, or
anti-EGFR antibody cetuximab combined with radiotherapy.7 Cetux- IVA cancer and ECE of nodal disease and/or positive resection margin of ⱕ 5
imab, as monotherapy or in combination with cisplatin, has also been mm but with no evidence of gross residual disease; primary surgery with a
associated with clinical efficacy in patients with platinum-refractory curative intent completed within 4 to 6 weeks (no later than 8 weeks) before
random assignment; and complete recovery from the surgical procedure.
SCCHN.8,9
Details of exclusion criteria are included in the Appendix.
Heterodimerization and functional cross-talk between members
of the EGFR/ErbB family suggest that combining chemoradiotherapy Study End Points and Assessments
with multitargeted small-molecule tyrosine kinase inhibitors may The primary end point was DFS (time from random assignment to the
be a successful approach for the treatment of SCCHN. To date, earliest date of disease recurrence or death as a result of any cause) based on
EGFR-targeted agents such as humanized monoclonal antibodies10 or radiologic and/or clinical assessment of electronic case report form data by an
independent review committee. DFS was also assessed by the investigator
tyrosine kinase inhibitors,11,12 tested concomitantly with (chemo)ra-
(based on scans, endoscopies, or positive biopsy results).
diotherapy, have failed to demonstrate significant benefits in random- Secondary efficacy end points included OS (time from random assign-
ized trials, emphasizing the need for alternative EGFR-targeting ment until death as a result of any cause); disease-specific survival; time to
agents. One such agent is lapatinib, a small-molecule inhibitor of locoregional control; time to distant relapse; incidence of second primary
EGFR and human epidermal growth factor receptor 2 (HER2, ErbB2). tumor; and clinical outcome with biomarkers including DFS by human pap-
The combination of lapatinib and chemoradiotherapy was well toler- illomavirus (HPV) status15 and EGFR status. Medical resource utilization
ated and showed single-agent activity in a small number of patients (collected via the electronic case report form) and health-related quality of life
(HRQoL) were also evaluated. HRQoL was assessed using the Functional
with locally advanced SCCHN in phase I and II trials.13,14 Therefore, a Assessment of Cancer Therapy–Head and Neck and EQ-5D questionnaires
randomized, placebo-controlled, phase III study was designed to eval- (further details are provided in the Appendix). Other post hoc analyses
uate the efficacy and safety of lapatinib administered concomitantly included DFS in patients with or without ECE and with different
with chemoradiotherapy, followed by maintenance monotherapy for surgical margins.
1 year, in patients with resected SCCHN at high risk of relapse. Exposure to chemoradiotherapy was reported descriptively. Compliance
was assessed by tablet count. Safety end points included toxicities (including
late radiation morbidity), measured by recording the incidence and grading of
PATIENTS AND METHODS AEs and serious AEs (SAEs).
Tumor EGFR protein expression levels were evaluated by IHC. HPV
status was determined by evaluating the intratumoral expression levels of
Study Design and Treatment CDKN2A (p16) by IHC and the presence of DNA from high-risk HPV geno-
This was a randomized, double-blind, placebo-controlled, multicenter, types (HPV16 and HPV18) by chromogenic in situ hybridization (Appendix
phase III study (ClinicalTrials.gov identifier: NCT00424255; GlaxoSmithKline Table A1, online only). Samples that were p16 positive/HPV negative were
protocol number: EGF102988), conducted between December 2006 and re-examined by consensus high-risk HPV polymerase chain reaction for the
November 2013. Patients with resected high-risk SCCHN (defined as ECE of detection of HPV DNA. Samples that were p16 positive/HPV positive were
nodal disease or positive resection margin [ⱕ 5 mm]) were randomly assigned defined as harboring biologically relevant oncogenic HPV infection. Further
in a 1:1 ratio to lapatinib or placebo arms using a GlaxoSmithKline internal details are provided in the Appendix.
random assignment system, stratifying by nodal stage (N0 or N1 v N2), Clinical safety and tolerability were assessed in the safety population
primary tumor site, geographical region, and EGFR expression (immunohis- (comprising all patients who took at least one dose of study medication). AEs
tochemistry [IHC] EGFR3⫹ v non-EGFR3⫹). were graded according to the National Cancer Institute Common Terminol-
At the start of the treatment phase, randomly assigned treatment (lapa- ogy Criteria for Adverse Events (version 3) and coded using the Medical
tinib or placebo) was administered once daily for 3 to 7 days before commenc- Dictionary for Regulatory Activities (version 15.1).
ing the 6- to 7-week combined therapy phase, where patients received
postoperative adjuvant concurrent chemoradiotherapy (intravenous cisplatin Statistical Analysis
100 mg/m2 per day on days 1, 22, and 43 plus 2 Gy of radiation per day, 5 days The planned sample size was 680 patients (340 patients per arm). To
per week, for a total of 66 Gy to the high-risk planning target volume 2 and detect a hazard ratio (HR) of 0.7206 with 80% power, approximately 298
2 © 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
independently assessed events (disease recurrences or deaths as a result of any treatment arms had radiotherapy plans that were approved by the
cause) would be required for the final analysis. The expected accrual rate was independent quality assurance group.
15 patients per month for 45 months. Median follow-up time (with 95% CI)
was calculated using the reverse censoring method.16,17 Further details on the
statistical properties of the trial design are provided in the Appendix. Efficacy
All efficacy analyses were conducted on the intent-to-treat (ITT) popu- According to the study design, approximately 298 independently
lation, which comprised all patients randomly assigned to study treatment, assessed DFS events (disease recurrence or death) would be required
regardless of whether they received study medication. DFS and OS were for the final analysis. However, because of apparent plateauing of
summarized using Kaplan-Meier curves (all P values are two-sided unless investigator-reported events (and having reached a median follow-up
otherwise stated). Further details are provided in the Appendix. time of 35.3 months), it was decided to report the study using data
collected up to a clinical cutoff of March 29, 2013. At this time, there
RESULTS were 232 independently assessed DFS events.
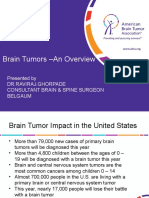
Study Population Characteristics Primary End Point: Independently Assessed DFS
Patients were enrolled from 84 sites in 21 countries (Appendix). DFS events were observed in 110 patients (32%) in the placebo
Overall, 930 patients were screened for study eligibility, and 688 arm compared with 122 patients (35%) in the lapatinib arm (HR, 1.10;
patients were randomly assigned to the ITT population (placebo, 95% CI, 0.85 to 1.43; P ⫽ .45). The median DFS was 53.6 months in
n ⫽ 342; lapatinib, n ⫽ 346; Fig 1). Patient demographics and char- the lapatinib arm but was not reached in the placebo arm (Fig 2A). On
acteristics were balanced between treatment arms (Table 1). The most the basis of Kaplan-Meier estimates from the DFS curves, the percent-
common primary tumor site was the oral cavity (41% of patients). The age of patients disease free at 36 months was 62.2% (95% CI, 56.1% to
hypopharynx was the primary site of disease in 33 patients (10%) in 67.7%) and 61.1% (95% CI, 55.0% to 66.7%) for placebo and lapa-
the placebo arm versus 53 patients (15%) in the lapatinib arm. Disease tinib, respectively; at 60 months, the values were 57.1% (95% CI,
characteristics at initial diagnosis were also balanced between treat- 49.5% to 64.0%) and 42.9% (95% CI, 32.3% to 53.1%) for placebo
ment arms within subgroups for overall HPV status (HPV positive, and lapatinib, respectively (numbers at risk at this time were low).
n ⫽ 44; HPV negative, n ⫽ 560). In HPV/p16-positive patients, the
oropharynx was the predominant primary tumor type (86% of pa- Secondary End Points
tients), and the proportion of patients with primary TNM stage T2 Investigator-assessed DFS events were observed in 39% to 40% of
tumors was higher in this group compared with the overall ITT pop- patients in both arms; no statistically significant difference was ob-
ulation (50% v 30%, respectively). Overall, 95% patients in both served between the two arms (HR, 1.03; 95% CI, 0.81 to 1.30; P ⫽ .82).
Assessed for eligibility
(N = 930)
Excluded or withdrew from study
(n = 242)
Randomly assigned to ITT population
(n = 688)
Assigned to placebo Assigned to lapatinib
(n = 342) (n = 346)
Analyzed in efficacy population Analyzed in efficacy population
(n = 342) (n = 346)
Analyzed in safety population Analyzed in safety population (n = 349)
(n = 336) Given lapatinib in error (n = 3)
Died (n = 110; 32%) Died (n = 105; 30%)
Ongoing (follow-up) (n = 169; 49%) Ongoing (follow-up) (n = 179; 52%)
Withdrew from study (n = 63; 18%) Withdrew from study (n = 62; 18%)
Patient’s decision (n = 33; 10%) Patient’s decision (n = 36; 10%)
Lost to follow-up (n = 24; 7%) Lost to follow-up (n = 18; 5%)
Investigator decision (n = 3; < 1%) Investigator decision (n = 6; 2%)
Other (n = 3; < 1%) Protocol violation (n = 1; < 1%)
Other (n = 3; < 1%)
Fig 1. Patient flow. ITT, intent to treat.
www.jco.org © 2015 by American Society of Clinical Oncology 3
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
(33% to 37% across treatments; Appendix Fig A1, online only). No
Table 1. Patient Demographic and Clinical Characteristics (including
stratification factors)
treatment effect was observed for DFS by HPV and EGFR status (Fig
3). No significant differences were observed between treatment arms
No. of Patients (%)
in DFS assessed in other subgroups (Fig 3).
Placebo Arm Lapatinib Arm Median OS was not reached in either treatment arm. Overall, 110
Characteristic (n ⫽ 342) (n ⫽ 346)
patients (32%) died in the placebo arm, compared with 105 patients
Age, years
(30%) in the lapatinib arm (Fig 4). On the basis of Kaplan-Meier
Median 55.0 54.0
Range 24-74 27-74
estimates from the OS curves, the percentage of patients alive at 36
Male sex 287 (84) 286 (83) months was 66.2% (95% CI, 60.4% to 71.4%) and 67.9% (95% CI,
Race category 62.1% to 73.0%) for placebo and lapatinib, respectively; at 60 months,
White 220 (64) 222 (64) the values were 57.3% (95% CI, 50.0% to 63.9%) and 56.6% (95% CI,
Black 1 (⬍ 1) 0 47.3% to 64.8%) for placebo and lapatinib, respectively.
Asian 121 (35) 123 (36) Results from analyses of additional secondary efficacy vari-
Other 0 1 (⬍ 1)
ables (disease-specific survival, time to locoregional recurrence,
Clinical stage
I 4 (1) 4 (1)
time to distant relapse, and incidence of second primary tumor)
II 31 (9) 34 (10) were consistent with the primary efficacy analyses; no difference
III 77 (23) 90 (26) between the two treatment arms was observed (Appendix Table 2,
IVa 230 (67) 216 (62) online only).
Missing 0 2 (⬍ 1) In HRQoL assessments using Functional Assessment of Cancer
p16 status Therapy–Head and Neck and EQ-5D questionnaires, similar trends
Positive 42 (12) 48 (14)
were observed in both treatment arms. Clinically meaningful de-
Negative 282 (82) 271 (78)
Unknown 18 (5) 7 (8)
creases from baseline were observed in all HRQoL scores at the end of
Overall HPV statusⴱ chemotherapy, indicating worsening of HRQoL (Appendix; Appen-
Positive 21 (6) 23 (7) dix Figs A2 and A3, online only). The decrease was significantly greater
Negative 284 (83) 276 (80) for patients on lapatinib than placebo. During the maintenance phase,
Unknown 37 (11) 47 (14) average scores returned to baseline values on most scales by mainte-
Stratification factors
nance week 8 and remained unchanged throughout this phase. How-
N stage
N0, N1 135 (39) 135 (39)
ever, patients receiving lapatinib had lower mean scores than those
N2 207 (61) 211 (61) receiving placebo. Both groups displayed clinically meaningful de-
Primary site of disease creases in HRQoL at the point of early withdrawal of treatment.
Oral cavity 145 (42) 140 (40) Overall, the amount of reported unscheduled medical resource utili-
Larynx 80 (23) 77 (22) zation was low and similar across treatment arms and corresponded to
Oropharynx 68 (20) 65 (19) the time points at which the greatest declines in HRQoL were observed
Hypopharynx 33 (10) 53 (15)
(Appendix Table A3, online only).
Multiple sites 16 (5) 11 (3)
Region†
Western 217 (63) 219 (63) Safety
Non-Western 125 (37) 127 (37) There were no significant differences between treatment arms in
EGFR expression exposure to placebo/lapatinib (Table 2), chemotherapy (Appendix
Non-3⫹ 99 (29) 104 (30) Table A4, online only), or radiotherapy (Appendix Table A5, online
3⫹ 243 (71) 242 (70) only). Overall, compliance was high in both treatment arms; 83% and
Abbreviation: EGFR, epidermal growth factor receptor. 76% of patients in the placebo and lapatinib arms, respectively, were
ⴱ
Defined by results of p16 expression (immunohistochemistry) and human
papillomavirus (HPV) DNA detection (chromogenic in situ hybridization);
ⱖ 80% compliant.
polymerase chain reaction was performed in certain cases to adjudicate A similar number of patients in both treatment arms experienced
discordant p16 and HPV results. AEs (Table 3). The most commonly observed AEs in both treatment
†Western region contains Canada, the United States, Austria, Croatia, Czech
Republic, Estonia, France, Germany, Greece, Hungary, Italy, Russia, Slovak arms were mucosal inflammation and nausea. In total, 224 patients
Republic, Spain, and the United Kingdom. Non-Western region contains (67%) in the placebo arm experienced grade 3 or 4 AEs compared with
Argentina, China, Hong Kong, India, Philippines, and Thailand.
263 patients (75%) in the lapatinib arm. The most common grade 3 or
4 AEs were lymphopenia and mucosal inflammation.
Overall, 204 patients (61%) and 228 patients (65%) in the pla-
Median DFS was 59.0 months in the placebo arm compared with 51.5 cebo and lapatinib arms, respectively, experienced AEs considered
months in the lapatinib arm (Fig 2B). On the basis of Kaplan-Meier related to study treatment. The most commonly observed treatment-
estimates from the DFS curves, the percentage of patients disease free related AEs were diarrhea (placebo [n ⫽ 25; 7%] v lapatinib [n ⫽ 96;
at 36 months was 57.7% (95% CI, 51.8% to 63.2%) and 56.9% (95% 28%], P ⬍ .001) and rash (placebo [n ⫽ 27; 8%] v lapatinib [n ⫽ 84;
CI, 50.8% to 62.5%) for placebo and lapatinib, respectively; at 60 24%], P ⬍ .001). Nausea was experienced by 75 patients (22%) and 82
months, the values were 49.3% (95% CI, 39.8% to 58.1%) and 41.8% patients (23%) in the placebo and lapatinib arms, respectively (P ⫽
(95% CI, 32.0% to 51.4%) for placebo and lapatinib, respectively. .75); vomiting was experienced by 58 patients (17%) and 76 patients
Fewer HPV/p16-positive patients (14% to 22% across treat- (22%) in the placebo and lapatinib arms, respectively (P ⫽ .19). SAEs
ments) had a DFS event compared with HPV/p16-negative patients were experienced by 133 patients (40%) and 166 patients (48%) in the
4 © 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
A 1.0
B 1.0
CRT + lapatinib CRT + lapatinib
CRT + placebo CRT + placebo
Disease-Free Survival
Disease-Free Survival
0.8 0.8
(probability)
(probability)
0.6 0.6
Placebo arm Lapatinib arm Placebo arm Lapatinib arm
0.4 0.4
n 342 346 n 342 346
Events: progression 110 (32) 122 (35) Events: disease recurrence 132 (39) 139 (40)
or death, n (%) or death, n (%)
0.2 Median DFS (95% CI) NR (54.6 to NR) 53.6 (45.8 to NR) 0.2 Median DFS (95% CI) 59.0 (38.0 to NR) 51.5 (38.9 to 61.2)
Hazard ratio (95% CI) 1.10 (0.85 to 1.43) Hazard ratio (95% CI) 1.03 (0.81 to 1.30)
Two-sided P .45 Two-sided P .82
0 10 20 30 40 50 60 70 0 10 20 30 40 50 60 70
Time Since Random Assignment (months) Time Since Random Assignment (months)
No. at risk No. at risk
Lapatinib 346 215 177 130 88 42 11 1 Lapatinib 346 237 188 135 90 44 11 1
Placebo 342 209 172 127 89 45 8 Placebo 342 224 183 131 91 47 11
Fig 2. Kaplan-Meier estimates of disease-free survival (DFS) in intent-to-treat population: (A) independently assessed and (B) investigator assessed. CRT,
chemoradiotherapy; NR, not reached.
placebo and lapatinib arms, respectively. Lymphopenia (5% of pa- occurrence of late radiation morbidity events was similar between
tients in both arms) and mucosal inflammation (nine patients [3%] the placebo and lapatinib arms (20% and 16% of patients,
and 17 patients [5%] in the placebo and lapatinib arms, respectively), respectively), and grade ⱖ 3 events occurred in 4% of patients in
were the most commonly experienced SAEs. both arms.
Sixteen patients (5%) and 25 patients (7%) experienced fatal AEs
in the placebo and lapatinib arm, respectively. Sepsis and pneumonia
were the most common known reasons for fatal SAEs (ⱕ 1% of DISCUSSION
patients in each arm). Two patients (⬍ 1%) in the placebo arm and
three patients (⬍ 1%) in the lapatinib arm had fatal AEs that were Despite a strong scientific rationale and supportive data from earlier
considered related to study medication by the investigator. The phase I and II studies, this phase III trial of lapatinib in combination
Subgroup n Hazard ratio (95% CI) P
All 688 .45
HPV status (HPV/p16)
Positive 44 .70
Negative 560 .29
Unknown 84 .56
ECE
Status 1: positive 320 .30
Status 1: negative 363 .81
Status 2: positive and surgical 471 .91
margins > 5 mm or negative
Status 2: positive and surgical 110 .91
margins ≤ 5 mm
Status 3: negative and surgical 527 .26
margins ≥ 1 mm or positive
Status 3: negative and surgical 42 .71
margins < 1 mm
Any involved surgical margin < 1 mm 209 .58
ECE positive and any involved 91 .91
surgical margins < 1 mm
Baseline EGFR IHC status
Non 3+ 203 .24
3+ 485 .92
0 1 2 3 4 5
Favors Lapatinib Favors Placebo
Fig 3. Forest plot summarizing disease-free survival (DFS) subgroup analyses (intent-to-treat population). DFS was independently assessed; all P values were
two-sided. ECE, extracapsular extension; EGFR, epidermal growth factor receptor; HPV, human papillomavirus; IHC, immunohistochemistry.
www.jco.org © 2015 by American Society of Clinical Oncology 5
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
1.0 CRT + lapatinib Table 3. Summary of On-Therapy and Follow-Up Overall Incidence of
CRT + placebo Adverse Events Occurring in ⱖ 15% of Patients in Either Treatment Arm
(overall and by grade [safety population])
0.8
No. of Patients (%)
Overall Survival
(probability)
0.6 All Gradesⴱ Grades 3 and 4†
Placebo Lapatinib Placebo Lapatinib
Arm Arm Arm Arm
0.4
Adverse Event (n ⫽ 336) (n ⫽ 349) (n ⫽ 336) (n ⫽ 349)
Placebo arm Lapatinib arm
n 342 346 Any event 328 (98) 344 (99) 224 (67)‡ 263 (75)
0.2 Events: deaths, n (%) 110 (32) 105 (30) Mucosal inflammation 214 (64) 229 (66) 57 (17)§ 84 (24)
Median OS (95% CI) NR (NR to NR) NR (58.8 to NR)
Hazard ratio (95% CI) 0.96 (0.73 to 1.25) Nausea 152 (45) 184 (53) 4 (1) 14 (4)
Rash 101 (30) 170 (49) 14 (4) 20 (6)
0 10 20 30 40 50 60 70 Vomiting 118 (35) 160 (46) 13 (4) 23 (7)
Dry mouth 130 (39) 148 (42) 10 (3) 16 (5)
Time Since Random Assignment (months)
Diarrhea 41 (12) 148 (42) 4 (1)㛳 20 (6)
No. at risk
Lapatinib 346 266 226 178 115 67 20 3 Dysphagia 115 (34) 128 (37) 39 (12) 56 (16)
Placebo 342 274 221 164 114 75 24 Lymphopenia 88 (26) 99 (28) 70 (21) 80 (23)
Weight decreased 65 (19) 92 (26) 9 (3) 12 (3)
Fig 4. Kaplan-Meier estimate of overall survival (OS; intent-to-treat population). Leukopenia 102 (30) 85 (24) 43 (13) 40 (11)
CRT, chemoradiotherapy; NR, not reached.
Anemia 60 (18) 77 (22) 7 (2) 16 (5)
Neutropenia 82 (24) 73 (21) 36 (11) 49 (14)
Pyrexia 64 (19) 66 (19) 0 4 (1)
with platinum-based chemoradiotherapy in patients with surgically Decreased appetite 71 (21) 65 (19) 9 (3) 11 (3)
treated high-risk SCCHN failed to meet its primary end point of DFS Constipation 73 (22) 58 (17) 2 (⬍ 1) 0
by independent review committee. In addition, no statistically signif- Asthenia 47 (14) 58 (17) 5 (1) 7 (2)
icant differences were seen in secondary end points, such as Radiation skin injury 78 (23) 54 (15) 7 (2) 5 (1)
Stomatitis 55 (16) 52 (15) 16 (5) 25 (7)
investigator-assessed DFS or OS. Exploratory analyses of the DFS data
Oropharyngeal pain 67 (20) 45 (13) 2 (⬍ 1) 2 (⬍ 1)
did not identify any patient subgroup that derived benefit (or experi-
enced detriment) from the addition of lapatinib to chemoradiother- NOTE. Only P values indicating statistically significant differences between
placebo and lapatinib are indicated.
apy. These results should be interpreted in light of the fact that ⴱ
Any event row contains patients with at least one adverse event regardless
lapatinib had a 0% response rate in a phase II study of EGFR inhibitor– of relationship to study treatment.
†Any event row contains patients with at least one adverse event with
naive or –refractory relapsed/metastatic SCCHN.18 Certainly, these maximum overall toxicity of grade 3 or 4 regardless of relationship to study
findings should serve as a note of caution on the risks of initiating large treatment.
‡P ⫽ .019.
phase III studies (of this and other drugs) with insufficient evidence of §P ⫽ .04.
single-agent activity. Although the results of this study are consistent 㛳P ⫽ .022.
with recently published trials that have combined EGFR-targeted
antibody therapies (cetuximab or panitumumab) with chemora-
diotherapy,10,19 the findings do not preclude the possibility that
small molecules with greater activity than lapatinib against EGFR
Table 2. Study Drug Exposure and Dose Delays (safety population) (eg, gefitinib, afatinib) may have a role in this context. Lapatinib
No. of Patients (%) has established efficacy in HER2-positive metastatic breast can-
Drug Exposure and Placebo Lapatinib
cer20; however, results of randomized studies in other EGFR-
Dose Delays (n ⫽ 336) (n ⫽ 349) driven cancers have been disappointing,21,22 suggesting that
Daily dose, mgⴱ lapatinib is more effective as an HER2 inhibitor than as an EGFR
Median 1,500 1,500 inhibitor in the clinic.
Range 782-1,500 750-1,500 When planning this study, projections of likely DFS and OS
Time on study treatment, weeks rates were based on data from practice-changing historical studies,
Mean 45.5 45.1 notably Radiation Therapy Oncology Group 95-01.1 However, the
SD 23.04 23.94
rates of reported DFS and OS events in the current study were
Median 62.9 62.9
Range 0-69 0-72
much lower than the projected rates, such that the required num-
Patients in maintenance phase ber of DFS events was not reached. In retrospect, it may have been
ⱖ 9 months 196 (58) 209 (60) more appropriate to base DFS and OS projections on the chemo-
No. of dose delays per patient radiotherapy arm of the European Organisation for Research and
0 219 (65) 192 (55) Treatment of Cancer 22931 study, given that most patients in this
1 55 (16) 76 (22)
study were recruited in non-US sites and the inclusion criteria
ⱖ2 62 (18) 81 (23)
Patients with dose reductions 27 (8) 47 (13)
included patients with close (⬍ 5 mm) margins.3 Although there
are caveats to cross-trial comparison of outcome data, the chemo-
Abbreviation: SD, standard deviation.
ⴱ
Daily dose was the cumulative dose divided by the duration of exposure.
radiotherapy arms of the current study and the European Organi-
sation for Research and Treatment of Cancer 22931 study seem to
6 © 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
be similar, suggesting that the control arm in our study performed
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
as would have been expected. This observation lends further
strength to the conclusion that the addition of lapatinib to chemo- Disclosures provided by the authors are available with this article at
radiotherapy adds no benefit in managing patients with high-risk www.jco.org.
postoperative SCCHN.
Exposure to the study medication was balanced, and compliance AUTHOR CONTRIBUTIONS
was high in both treatment arms. Although similar rates of tolerability
Conception and design: Kevin Harrington, Stephane Temam, Hisham
were observed, diarrhea and rash were observed more frequently in
Mehanna, Iman El-Hariry, Nigel Biswas-Baldwin, Philippe Legenne, Paul
the lapatinib arm, consistent with the known toxicities of this drug. In Wissel, Mayur Amonkar, Jean Bourhis
addition, there were more grade 3 or 4 AEs and deaths in the lapatinib Provision of study materials or patients: Kevin Harrington, Stephane
arm. Despite the additional toxicity, there was no evidence that Temam, Pavol Dubinsky, Jean Bourhis
lapatinib had a significant effect on HRQoL over and above che- Collection and assembly of data: Kevin Harrington, Stephane Temam,
Hisham Mehanna, Anil D’Cruz, Minish Jain, Ida D’Onofrio, Georgy
moradiotherapy, in part likely as a result of the high symptom
Manikhas, Zsuzsanna Horvath, Yan Sun, Stefan Dietzsch, Pavol
burden these patients already experience. Because the HRQoL Dubinsky, Petra Holeckova, Natalie Franklin, Nigel Biswas-Baldwin,
values returned to baseline during the adjuvant phase, this study Paul Wissel, John Farrell, Catherine Ellis, Nazma Ahmed, Sergio
adds to the existing literature that lapatinib is well tolerated as Santillana, Jean Bourhis
maintenance monotherapy. In conclusion, in patients with surgi- Data analysis and interpretation: Kevin Harrington, Stephane Temam,
cally treated high-risk SCCHN, the addition of lapatinib to chemo- Hisham Mehanna, Natalie Franklin, Nigel Biswas-Baldwin, Philippe
Legenne, Paul Wissel, Thelma Netherway, Catherine Ellis, Jing
radiotherapy and its use as long-term maintenance therapy offered Wang-Silvanto, Mayur Amonkar, Sergio Santillana, Jean Bourhis
no benefit in efficacy and had additional toxicity compared with Manuscript writing: All authors
chemotherapy alone. Final approval of manuscript: All authors
single agent in patients with recurrent and/or meta- neck: Rationale for future randomised trials in hu-
REFERENCES static squamous cell carcinoma of the head and man papilloma virus-negative disease. Eur J Cancer
neck who failed to respond to platinum-based ther- 49:1609-1618, 2013
1. Cooper JS, Pajak TF, Forastiere AA, et al: apy. J Clin Oncol 25:2171-2177, 2007 15. Ritchie JM, Smith EM, Summersgill KF, et al:
Postoperative concurrent radiotherapy and chemo- 9. Baselga J, Trigo JM, Bourhis J, et al: Phase II Human papillomavirus infection as a prognostic fac-
therapy for high-risk squamous-cell carcinoma of the multicenter study of the antiepidermal growth factor tor in carcinomas of the oral cavity and oropharynx.
head and neck. N Engl J Med 350:1937-1944, 2004 receptor monoclonal antibody cetuximab in combi- Int J Cancer 104:336-344, 2003
2. Pignon JP, le Maître A, Maillard E, et al: nation with platinum-based chemotherapy in pa- 16. Shuster JJ: Median follow-up in clinical trials.
Meta-analysis of chemotherapy in head and neck tients with platinum-refractory metastatic and/or J Clin Oncol 9:191-192, 1991
cancer (MACH-NC): An update on 93 randomised recurrent squamous cell carcinoma of the head and 17. Schemper M, Smith TL: A note on quantifying
trials and 17,346 patients. Radiother Oncol 92:4-14, neck. J Clin Oncol 23:5568-5577, 2005 follow-up in studies of failure time. Control Clin
2009 10. Mesía R, Henke M, Fortin A, et al: Chemora- Trials 17:343-346, 1996
3. Bernier J, Domenge C, Ozsahin M, et al: diotherapy with or without panitumumab in patients 18. de Souza JA, Davis DW, Zhang Y, et al: A
Postoperative irradiation with or without concomi- with unresected, locally advanced squamous-cell
phase II study of lapatinib in recurrent/metastatic
tant chemotherapy for locally advanced head and carcinoma of the head and neck (CONCERT-1): A
squamous cell carcinoma of the head and neck. Clin
neck cancer. N Engl J Med 350:1945-1952, 2004 randomised, controlled, open-label phase 2 trial.
Cancer Res 18:2336-2343, 2012
4. Cooper JS, Zhang Q, Pajak TF, et al: Long- Lancet Oncol 16:208-220, 2015
19. Ang KK, Zhang Q, Rosenthal DI, et al: Ran-
term follow-up of the RTOG 9501/intergroup phase 11. Gregoire V, Hamoir M, Chen C, et al: Gefitinib
domized phase III trial of concurrent accelerated
III trial: Postoperative concurrent radiation therapy plus cisplatin and radiotherapy in previously un-
radiation plus cisplatin with or without cetuximab for
and chemotherapy in high-risk squamous cell carci- treated head and neck squamous cell carcinoma:
stage III to IV head and neck carcinoma: RTOG
noma of the head and neck. Int J Radiat Oncol Biol A phase II, randomized, double-blind, placebo-
0522. J Clin Oncol 32:2940-2950, 2014
Phys 84:1198-1205, 2012 controlled study. Radiother Oncol 100:62-69, 2011
5. Cancer Genome Atlas Network: Comprehen- 12. Martins RG, Parvathaneni U, Bauman JE, et 20. Cameron D, Casey M, Oliva C, et al: Lapatinib
sive genomic characterization of head and neck al: Cisplatin and radiotherapy with or without erlo- plus capecitabine in women with HER-2-positive
squamous cell carcinomas. Nature 517:576-582, tinib in locally advanced squamous cell carcinoma of advanced breast cancer: Final survival analysis of a
2015 the head and neck: A randomized phase II trial. J Clin phase III randomized trial. Oncologist 15:924-934,
6. Kalyankrishna S, Grandis JR: Epidermal Oncol 31:1415-1421, 2013. 2010
growth factor receptor biology in head and neck 13. Harrington KJ, El-Hariry IA, Holford CS, et al: 21. Ravaud A, Hawkins R, Gardner JP, et al:
cancer. J Clin Oncol 24:2666-2672, 2006 Phase I study of lapatinib in combination with Lapatinib versus hormone therapy in patients with
7. Bonner JA, Harari PM, Giralt J, et al: Radio- chemoradiation in patients with locally advanced advanced renal cell carcinoma: A randomized phase
therapy plus cetuximab for squamous-cell carci- squamous cell carcinoma of the head and neck. J III clinical trial. J Clin Oncol 26:2285-2291, 2008
noma of the head and neck. N Engl J Med 354: Clin Oncol 27:1100-1107, 2009 22. Wülfing C, Machiels JP, Richel DJ, et al: A
567-578, 2006 14. Harrington K, Berrier A, Robinson M, et al: single-arm, multicenter, open-label phase 2 study of
8. Vermorken JB, Trigo J, Hitt R, et al: Open- Randomised phase II study of oral lapatinib com- lapatinib as the second-line treatment of patients
label, uncontrolled, multicenter phase II study to bined with chemoradiotherapy in patients with ad- with locally advanced or metastatic transitional cell
evaluate the efficacy and toxicity of cetuximab as a vanced squamous cell carcinoma of the head and carcinoma. Cancer 115:2881-2890, 2009
Affiliations
Kevin Harrington, Institute of Cancer Research and Royal Marsden Hospital, London; Hisham Mehanna, Institute of Head and Neck
Studies and Education, University of Birmingham, Birmingham; Natalie Franklin and John Farrell, GlaxoSmithKline, Uxbridge, United
Kingdom; Stephane Temam and Jean Bourhis, Institut Gustave- Roussy, Villejuif; Ida D’Onofrio, Hôpital Forcilles, Paris, France; Anil
D’Cruz, Tata Memorial Hospital, Mumbai; Minish Jain, Ruby Hall Clinic–Cancer Centre, Pune, India; Georgy Manikhas, St Petersburg City
Oncology Dispensary, St Petersburg, Russia; Zsuzsanna Horvath, Szent Imre University Teaching Hospital Budapest, Budapest, Hungary; Yan
www.jco.org © 2015 by American Society of Clinical Oncology 7
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
Sun, Beijing Cancer Hospital, Beijing, China; Stefan Dietzsch, Hospital and Policlinic for Radiation Therapy and Radio-oncology, Leipzig,
Germany; Pavol Dubinsky, East Slovakia Cancer Institute, Kosice, Slovakia; Petra Holeckova, Institute of Radiation Oncology, Hospital Na
Bulovce, and 1st Medical Faculty of Charles University, Prague, Czech Republic; Iman El-Hariry, Synta Pharmaceutical, Lexington, MA; Paul
Wissel and Mayur Amonkar, Novartis Pharmaceuticals, East Hanover, NJ; Catherine Ellis and Sergio Santillana, GlaxoSmithKline,
Philadelphia, PA; and Nigel Biswas-Baldwin, Philippe Legenne, Thelma Netherway, Jing Wang-Silvanto, and Nazma Ahmed, Novartis
Pharma AG, Basel, Switzerland.
■ ■ ■
8 © 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Postoperative Adjuvant Lapatinib and Concurrent Chemoradiotherapy Followed by Maintenance Lapatinib Monotherapy in High-Risk Patients
With Resected Squamous Cell Carcinoma of the Head and Neck: A Phase III, Randomized, Double-Blind, Placebo-Controlled Study
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are
self-held unless noted. I ⫽ Immediate Family Member, Inst ⫽ My Institution. Relationships may not relate to the subject matter of this manuscript. For more
information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Kevin Harrington No relationship to disclose
Honoraria: Merck Sharp & Dohme, Amgen, Oncos Therapeutics,
Cellgene Iman El-Hariry
Consulting or Advisory Role: Merck Sharp & Dohme, Amgen (Inst), No relationship to disclose
Viralytics Inc (Inst), Lytix Natalie Franklin
Speakers’ Bureau: Merck Sharp & Dohme, Amgen Employment: GlaxoSmithKline, Roche
Research Funding: Oncolytics Biotech (Inst), Genelux (Inst), Viralytics Stock or Other Ownership: GlaxoSmithKline
(Inst), AstraZeneca (Inst)
Nigel Biswas-Baldwin
Stephane Temam Employment: GlaxoSmithKline
No relationship to disclose Stock or Other Ownership: GlaxoSmithKline
Hisham Mehanna Philippe Legenne
Employment: Warwickshire Head Neck Clinic Employment: GlaxoSmithKline
Leadership: Warwickshire Head neck Clinic, Warwickshire Head Neck
Stock or Other Ownership: GlaxoSmithKline
Clinic (I)
Stock or Other Ownership: Warwickshire Head Neck Clinic Paul Wissel
Honoraria: AstraZeneca Employment: GlaxoSmithKline
Speakers’ Bureau: Merck Sharp & Dohme, Sanofi Pasteur, Merck Stock or Other Ownership: GlaxoSmithKline
Research Funding: GlaxoSmithKline (Inst), Merck Sharp & Dohme
(Inst), Sanofi Pasteur (Inst), Silence Therapeutics (Inst), Thelma Netherway
GlaxoSmithKline Biologicals (Inst) Employment: GlaxoSmithKline, Novartis
Travel, Accommodations, Expenses: Sanofi Pasteur, Merck Sharp & Stock or Other Ownership: GlaxoSmithKline, Novartis
Dohme, Merck Travel, Accommodations, Expenses: GlaxoSmithKline, Novartis
Anil D’Cruz John Farrell
Honoraria: Merck Serono Employment: GlaxoSmithKline
Travel, Accommodations, Expenses: Merck Serono Stock or Other Ownership: GlaxoSmithKline
Minish Jain Catherine Ellis
No relationship to disclose Employment: GlaxoSmithKline
Stock or Other Ownership: GlaxoSmithKline
Ida D’Onofrio
No relationship to disclose Jing Wang-Silvanto
Employment: GlaxoSmithKline
Georgy Manikhas Stock or Other Ownership: GlaxoSmithKline
No relationship to disclose
Mayur Amonkar
Zsuzsanna Horvath Employment: Novartis Pharmaceuticals
No relationship to disclose
Stock or Other Ownership: GlaxoSmithKline, Novartis Pharmaceuticals
Yan Sun
Nazma Ahmed
No relationship to disclose
No relationship to disclose
Stefan Dietzsch
Sergio Santillana
No relationship to disclose
Employment: GlaxoSmithKline Oncology, Takeda Pharmaceuticals
Pavol Dubinsky Stock or Other Ownership: GlaxoSmithKline Oncology, Takeda
Honoraria: Merck, Merck Sharp & Dohme, Amgen Pharmaceuticals
Research Funding: Quintiles, Merck
Jean Bourhis
Petra Holeckova Consulting or Advisory Role: Merck Serono
www.jco.org © 2015 by American Society of Clinical Oncology
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
Acknowledgment
We thank all patients and their families, investigators, and study staff; the independent data monitoring committee; and the BioClinica
(independent review committee), EqualEstro (Radiotherapy Quality Assurance), and PAREXEL (independent statistics) teams. The authors also
thank Jen Carver, Jhangir Irani, Sejal Patel, Zuheb Ali, and all members of the GlaxoSmithKline central and monitoring team. Lapatinib is an asset
of Novartis AG as of March 2, 2015. Editorial support was provided by Karen Yee, PhD, of Fishawack Indicia, funded by GlaxoSmithKline and
Novartis Pharmaceuticals Corporation.
Appendix
Methods
Radiation treatment. A detailed description of radiation target volumes and dose prescription is provided in the Radiation Therapy
Protocol Guidelines (Data Supplement). Patients in both arms of this study received a conventionally fractionated course of radiotherapy.
Irradiation was planned using either a standard two-dimensional technique or a three-dimensional conformal technique. The use of
intensity-modulated radiation therapy was not allowed. The selection of technique was left to the discretion of each center. Only linear
accelerator– based treatments (photon energy ⱖ 4 MV or electrons) were allowed.
Exclusion criteria. Patients were excluded if they had tumors of the nasopharynx, paranasal sinuses, or nasal cavity or tumors with
histology other than squamous cell carcinomas; evidence of distant metastases, gross postoperative residual disease, or second primary
tumor; any prior or concurrent anticancer treatment or concurrent treatment with an investigational agent; or history of another
malignancy within the last 5 years (excluding resected basal or squamous skin cancers).
Health-related quality of life (HRQoL) assessment. Functional Assessment of Cancer Therapy–Head and Neck (FACT-H&N,
comprising Functional Assessment of Cancer Therapy–General [FACT-G] and a head and neck subscale) and EQ-5D questionnaires
were completed at day 1 (before dose), at the end of chemotherapy, every 8 weeks during the first year of follow-up, and at discontinuation
of randomly assigned therapy. During the next 2 years of follow-up, patients were asked to complete the questionnaire every 4 months.
A minimal clinically important difference (ie, a clinically meaningful change) is defined as ⫹6 (improvement) and ⫺12 (worsening)
for the FACT-H&N total score, ⫹4 (improvement) and ⫺8 (worsening) for the FACT-G score, and ⫹3 (improvement) and ⫺3
(worsening) for the head and neck subscale score and Trial Outcome Index (TOI; Ringash J, et al: Qual Life Res 13:725-733, 2004); 0.08
for the EQ-5D utility score; and 7 for the EQ-5D thermometer score (Pickard AS, et al: Health Qual Life Outcomes 5:70, 2007).
Tissue samples. Tissue sections (4 m) and/or tissue blocks of the formalin-fixed and paraffin-embedded (FFPE) diagnostic biopsies
or resection specimens were collected. For the analysis, where only tissue sections were available, these were used. Where tissue blocks were
available, tissue microarrays (TMAs) were constructed. Briefly, hematoxylin and eosin–stained sections were prepared from the blocks to
confirm the presence of tumor, and the slides were annotated by a pathologist to guide TMA core selection. Up to four 0.6-mm diameter
tumor cores per block were transferred from the donor block to the recipient TMA block. A hematoxylin and eosin–stained section of the
prepared TMA was examined to assess adequate tumor sampling. Thick tissue curls (10 m) were taken from available blocks for DNA
extraction and downstream polymerase chain reaction (PCR) analysis.
HPV analysis protocol. All samples were analyzed for p16 expression by immunohistochemistry (IHC). Samples were assessed for
high-risk (HR) HPV DNA using a protocol based on that described and validated by Smeets et al (Int J Cancer 121:2465-2472, 2007).
Samples were assessed by HPV in situ hybridization (ISH). For samples that were found to be p16 positive/HPV negative by ISH using
TMAs, whole tissue sections were tested to reduce misclassification as a consequence of possible sampling limitations inherent to TMA
analysis. If the sample remained p16 positive/HPV negative by ISH on the whole tissue section, the sample was then examined by
consensus HR-HPV PCR to control for the suboptimal sensitivity of HPV ISH compared with target amplification techniques (Smeets SJ,
et al: Int J Cancer 121:2465-2472, 2007). This latter protocol has been previously validated and proven to have the same accuracy as using
p16 and HPV-PCR (Thavaraj S, et al: J Clin Pathol 64:308-312, 2011). For all samples in this study, samples that showed evidence of HPV
DNA (either by ISH or consensus PCR) and showed high p16 expression (HPV positive/p16 positive) were defined as harboring
biologically relevant oncogenic HPV infection (Smeets SJ, et al: Int J Cancer 121:2465-2472, 2007).
HPV and p16 testing methods. p16 IHC was carried out using a proprietary kit (CINtec Histology; MTM Laboratories AG,
Heidelberg, Germany) on a Benchmark Autostainer (Ventana Medical Systems, Tucson, AZ). Tissue from an oropharyngeal squamous
cell carcinoma with high p16 expression was used as a positive control. The primary antibody was omitted from negative controls. A binary
(positive and negative) scoring system was adopted, and p16 IHC was scored as positive if there was strong and diffuse nuclear and
cytoplasmic staining present in more than 70% of the malignant cells (Singhi AD, et al: Cancer 116:2166-2173, 2010). All other staining
patterns were scored as negative.
HR-HPV ISH was carried out using proprietary reagents (Inform HPV III Family 16 Probe [B]; Ventana) on a Benchmark
Autostainer (Ventana). The Inform HPV III Family 16 Probe (B) detects HR genotypes 16, 18, 31, 33, 35, 39, 51, 52, 56, 58, and 66. The
following three control samples were used: FFPE CaSki cells (HPV-16 positive; 600 copies per cell), HeLa cells (HPV-18 positive; 10 to 50
copies per cell), and C-33A (HPV-negative cell line; Ventana). A binary scoring system was used. The HR-HPV ISH test was scored as
positive if there was a blue reaction product that colocalized with the nuclei of malignant cells. Diffuse staining of tumor and stromal
© 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
tissues, considered to represent nonspecific chromogen precipitate, was scored as negative. Pale staining limited to the nucleoli of cells and
staining of occasional leukocytes and stromal cells were also disregarded, in line with the manufacturer’s instructions (Ventana).
For consensus PCR for oncogenic HPV, DNA was extracted from tissue curls using the Qiagen (Hilden, Germany) FFPE kit (without
xylene washes). The yield of DNA was quantified using nanodrop spectrophotometry. DNA adequacy was assessed by amplification of the
human -globin gene. HPV typing was performed using the GP5⫹/6⫹ primer set (Jacobs MV, et al: Clin Microbiol 35:791-795, 1997).
Samples were tested by PCR enzyme immunoassay using a cocktail of probes for 14 HR-HPV types and separately with a cocktail of probes
for six low-risk types. Samples testing positive for ab HR-HPV type were subject to second PCR and assayed with each of the 14 HR probes
independently of each other. A sample was defined as HR-HPV DNA positive if it tested positive in the HR-HPV cocktail reaction and an
HR-HPV genotype was identified in the second PCR reaction.
Scoring methods. The criteria used to score the p16 expression and HR-HPV ISH were defined before commencing the study. Two
pathologists analyzed the test results independently. Before commencing the study, a training set of 45 tonsil squamous cell carcinomas
was used to calibrate the two scorers, obtaining greater than 95% concordance (data not shown). The p16 IHC and HR-HPV ISH tests
were assessed separately alongside corresponding hematoxylin and eosin–stained sections, and the scores were collated by the study
coordinator. Any discordant scores (5%) between the pathologists were resolved at a meeting between the pathologists to establish a
consensus. In addition, all samples scored as p16 negative/HPV positive and p16 positive/HPV negative were reviewed by the two
pathologists together to ensure correct categorization.
Hypotheses. The study was designed to provide evidence to either support the null hypothesis (H0: ⱖ 1) or reject it in favor of the
alternative hypothesis (HA: ⬍ 1), where is the hazard ratio (HR) for disease-free survival (DFS; lapatinib/placebo). Assuming the DFS
curves are consistent with proportional hazards, then the null hypothesis represents equality of the median DFS in the two treatment arms,
or a lower median DFS in the lapatinib arm, and the alternative hypothesis represents a higher median DFS in the lapatinib arm.
Sample size assumptions. The following assumptions were made in the estimation of the required sample size: exponential distribu-
tions of DFS; an HR of 0.7206, which originates from estimated DFS rates at 2 years after random assignment of 65% in the lapatinib arm
and 55% in the placebo arm (an absolute increase of 10%), resulting in an approximate median DFS of 39 and 28 months in the lapatinib
arm and placebo arm, respectively; a 1:1 random assignment scheme, with a total of approximately 680 patients, 340 patients per arm (on
the basis of observed cure rates in the studies reported by Bernier et al3 and Cooper et al,4 it was anticipated that a portion of patients
entered onto the study may never reach an end point of recurrence of disease; therefore, more patients were recruited to allow for this); a
2.5% risk of erroneously claiming superiority of lapatinib in the presence of no true underlying difference (one-sided type I error); an 80%
chance of successfully detecting am HR of 0.7206, which equates to detecting a 39% increase in median DFS in patients who receive
lapatinib (39 months; HR, 0.0179) relative to placebo (28 months; HR, 0.0249); and an average constant accrual rate of 15 patients per
month for 45 months.
Efficacy end points. Greenwood’s formula was used to calculate the SE of the Kaplan-Meier curve estimates. The Pike estimator of the
HR and associated 95% CIs were also presented. DFS was compared between treatment arms using a nonstratified log-rank test. Cox
regression models were used to explore the effect of prognostic factors, including stratification factors and HPV status. The adjusted HR,
95% CI, and two-sided Wald 2 P values were presented.
HRQoL. For HRQoL analyses, data collected from FACT-H&N and EQ-5D questionnaires were summarized descriptively and
listed to show FACT-H&N responses for subscale, total, FACT-G, and TOI scores, and EQ-5D domain scores, thermometer values, and
derived utility scores. Changes from baseline were also summarized for each treatment arm with an analysis of covariance performed to
compare differences between study arms in FACT-G scores, TOI scores, EQ-5D utility scores, and thermometer scores.
Quality-of-life responder analyses were also performed to indicate scores that were clinically meaningful. Patients with missing
baseline assessments for FACT-H&N were excluded from analysis.
Results
Secondary end point: HRQoL. For HRQoL, at the end of chemoradiotherapy, clinically meaningful decreases from baseline were
observed in both arms in all HRQoL measures, as follows: FACT-H&N total (lapatinib, ⫺17.9; placebo, ⫺13.5), FACT-G (lapatinib,
⫺11.1; placebo, ⫺7.8), TOI (lapatinib, ⫺16.0; placebo, ⫺12.2), head and neck subscale (lapatinib, ⫺7.0; placebo, ⫺5.6), EQ-5D utility
(lapatinib, ⫺0.14; placebo, ⫺0.12), and EQ-5D thermometer (lapatinib, ⫺8.4; placebo, ⫺7.7) scores. All of these declines (except both
scores of EQ-5D) were found to be significantly worse (P ⬍ .05) for the patients on lapatinib than those on placebo. Results for FACT-G
and EQ-5D utility are illustrated in Appendix Figures A1 and A2 (showing changes in scores from baseline across all the treatment phases
in the study).
During the maintenance period, no clinically meaningful decreases from baseline were observed in both arms of all HRQoL measures
except TOI scores at maintenance week 8 (lapatinib, ⫺8.5; placebo, ⫺5.0). However, patients receiving lapatinib had significantly less
favorable changes (P ⬍ .05) than patients given placebo in FACT-H&N total score, FACT-G score (Fig A2), and TOI at multiple time
points throughout the maintenance period.
On treatment withdrawal, both groups displayed clinically meaningful declines in FACT-H&N total (lapatinib, ⫺14.9; placebo,
⫺16.2), FACT-G (lapatinib, ⫺10.1; placebo, ⫺12.2; Fig A1), TOI (lapatinib, ⫺11.9; placebo, ⫺12.5), head and neck subscale (lapatinib,
⫺4.9; placebo, ⫺4.1), EQ-5D utility (lapatinib, ⫺0.11; placebo, ⫺0.23), and EQ-5D thermometer scores (lapatinib, ⫺3.3; placebo,
www.jco.org © 2015 by American Society of Clinical Oncology
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
⫺11.4). However, the differences between treatment arms was not statistically significant (P ⬎ .05) except for EQ-5D, with both scores
significantly in favor of lapatinib compared with placebo (P ⬍ .05; Appendix Fig 3A).
Overall responder analyses showed that HRQoL worsened in more lapatinib-treated patients than patients taking placebo (P ⬍ .05)
according to FACT-H&N total scores and FACT-G scores, but the differences were not significant in TOI and head and neck subscale
scores (P ⬎ .05; Appendix Table A6).
EGF102988 Study Sites and Investigators
Sites in order of patient recruitment numbers were as follows: India (n ⫽ 119), France (n ⫽ 116), China (n ⫽ 80), Germany (n ⫽ 51),
Hungary (n ⫽ 41), the Russian Federation (n ⫽ 40), Spain (n ⫽ 36), the Czech Republic (n ⫽ 29), Slovakia (n ⫽ 24), Thailand (n ⫽ 22),
United Kingdom (n ⫽ 21), Greece (n ⫽ 21), Croatia (n ⫽ 18), Italy (n ⫽ 17), Austria (n ⫽ 15), the Philippines (n ⫽ 14), Argentina (n ⫽
9), Hong Kong (n ⫽ 8), United States of America (n ⫽ 3), Canada (n ⫽ 3), and Estonia (n ⫽ 1).
Argentina (n ⫽ 3): Blajman, Cesar R., MD; Campos, Claudio A., MD; Fein, Luis E., MD.
Austria (n ⫽ 3): Greil, Richard, MD; Kornek, Gabriela, MD; Scholtz, Arne-Wulf, MD.
Canada (n ⫽ 2): Jha, Naresh, MD, FRCPC, MBBS; Nabid, Abdenour, MD.
China (n ⫽ 7): Gao, Li, MD; Hu, Chaosu, MD; Hu, Guoqing, MD; Pan, Jianji, PhD; Sun, Yan, MD; Wu, Shao Xiong, MD; Yuan,
Zhiyong, MD.
Croatia (n ⫽ 2): Prgomet, Drago, MD; Virag, Mîso Mihajlo, MD.
Czech Republic (n ⫽ 4): Cervena, Renata, MD; Cincibuch, Jan, MD; Feltl, David, MD, PhD; Holeckova, Petra, MD.
Estonia (n ⫽ 1): Kuddu, Maire, MD.
France (n ⫽ 15): Babin, Emmanuel, MD; Banal, Alain, MD; Borel, Christian, MD; Cupissol, Didier, MD, PhD; Degardin, Marian,
MD; Delalande, Cecile, MD; Delord, Jean-Pierre, MD; D’Onofrio, Ida, MD; Duparc, Angelique, MD; Jadaud, Eric, MD; Lacau Saint
Guily, Jean, MD; Prevost, Alain, MD; Racadot, Séverine, MD; Temam, Stephane, MD; Zawadi, Ayman, MD.
Germany (n ⫽ 6): Classen, Johannes, Dr Med; Debus, Juergen P, Dr Med; Kortmann, Rolf-Dieter, Dr Med; Lang, Stephan, MD, PhD;
Schreiber, Andreas, Dr Med, MRCP; Vordermark, Dirk, Dr Med, PhD.
Greece (n ⫽ 4): Antonadou, Theodosia, MD; Maroudias, Nikolaos, MD; Psyrri, Amanda, MD; Skarlos, Dimosthenis, MD, PhD.
Hong Kong (n ⫽ 2): Au, Kwok Hung, MBBS; Chan, Yu Wai, Jimmy, MBBS.
Hungary (n ⫽ 3): Csejtei, András, MD; Horvai, Géza, MD; Remenár, Éva, MD.
India (n ⫽ 5): Almel, Sachin, MD; D’Cruz, Anil K., MBBS, MS; Iyer, Subramania, MS, MCh, FRCS; Jain, Minish M, MD; Kumar, R.
Rejnish, MD.
Italy (n ⫽ 5): Bacigalupo, Almalina, MD; Bianco, Roberto, MD; Caponigro, Francesco, MD; Nolè, Franco, MD; Villa, Eugenio, MD.
Philippines (n ⫽ 1): Pontejos, Alfredo Q., Jr, MD.
Russia (n ⫽ 3): Biakhov, Mikhail, MD, DSc; Manikhas, Georgy M., MD, PhD; Romanov, Ilya S., MD, PhD.
Slovakia (n ⫽ 1): Dubinsky, Pavol, MD.
Spain (n ⫽ 11): Ales, Jose E., MD; Ballester Navarro, Inmaculada, MD; Del Campo, Jose Maria, MD; Espinosa Arranz, Enrique, MD;
García Sáenz, Jose Angel, MD; Iglesias Docampo, Lara; Lavernia, Javier, MD; López, Rafael, MD; Martínez Galán, Joaquina, MD; Morales
Murillo, Serafin, MD; Rubio, Jordi, MD.
Thailand (n ⫽ 2): Chitapanarux, Imjai, MD; Eursritanakorn, Sirima.
United Kingdom (n ⫽ 7): Goodchild, Kathleen, BSc (Hons), MBBS, MRCP, FRCR; Guerrero Urbano, Maria Teresa, PhD, FRCR;
Harrington, Kevin J., BSc, MBBS, MRCP (United Kingdom); Junor, Elizabeth, MRCP, MD, FRCR; Kelly, Charles G., MB ChB, MSc,
FRCP; Robinson, Martin H., MD, MRCP; Simcock, Richard, MBBS, MRCP, FRCR.
United States (n ⫽ 2): Cordero, Joehassin, MD; Reimers, Hans J. Joachim, MD, PhD.
Table A1. Derivation of Overall HPV Status Based on Separate HPV/p16 Results
p16
Result HPV ISH Result HPV PCR Result Overall Status for Analysis
Positive Positive Not tested Positive
Positive Negative Positive Positive
Positive Negative Negative Negative
Positive Negative Not tested/unknown Unknown
Positive Unknown Not tested Unknown
Negative Negative Not tested Negative
Negative Positive Not tested Negative
Negative Unknown Not tested Negative
Unknown Any Not tested Unknown
Abbreviations: HPV, human papillomavirus; ISH, in situ hybridization; PCR, polymerase chain reaction.
© 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
Table A2. Additional Secondary End Points (intent-to-treat population)
Parameter (95% CI)
End Point Placebo Arm (n ⫽ 342) Lapatinib Arm (n ⫽ 346)
Disease-specific survival
Died as a result of head and neck cancer (events)
No. 89 79
% 26 23
Median cumulative incidence estimate of time to death as a result of head and neck cancer,
months NR (NR to NR) NR (NR to NR)
Nonstratified HR 0.89 (0.66 to 1.21)
Patients who died as a result of head and neck cancer at 36 months, % 27.3 (22.3 to 32.6) 24.6 (19.7 to 29.7)
Patients who died as a result of head and neck cancer at 60 months, % 35.0 (28.4 to 41.8) 33.1 (25.2 to 41.1)
Time to locoregional control
Patients with independently assessed locoregional recurrence
No. 49 40
% 14 12
Median cumulative incidence estimate of time to locoregional control, months NR (NR to NR) NR (NR to NR)
Nonstratified HR 0.81 (0.54 to 1.23)
Patients with independently assessed locoregional recurrence at 36 months, % 17.0 (12.9 to 21.7) 13.0 (9.3 to 17.2)
Patients with independently assessed locoregional recurrence at 60 months, % 17.7 (13.4 to 22.5) 17.5 (12.0 to 23.8)
Time to distant relapse
Patients with independently assessed distant recurrence
No. 51 63
% 15 18
Cumulative incidence estimate of time to distant recurrence (months), median (95% CI) NR (NR to NR) NR (NR to NR)
Nonstratified HR 1.23 (0.85 to 1.78)
Patients with independently assessed distant recurrence at 36 months, % 18.0 (13.7, 22.8) 21.5 (16.9 to 26.6)
Patients with independently assessed distant recurrence at 36 months, % 18.9 (14.3 to 23.9) 25.7 (19.3 to 32.4)
Incidence of second primary tumor
Independently assessed second primary malignancy incidence rate
No. 5 9
% 1.5 2.6
95% CI, % 0.5 to 3.4 1.2 to 4.9
Difference in incidence rate 1.1 (⫺1.2 to 3.6)
OR for incidence rate 1.80 (0.53 to 6.91)
Abbreviations: HR, hazard ratio; NR, not reached; OR, odds ratio.
Table A3. Unscheduled Medical Resource Use: Time Points at Which the Highest Proportion of Patients Reported Use, by Item, Through the Maintenance
Period and the Withdrawal From Treatment Visit
Lapatinib (n ⫽ 346) Placebo (n ⫽ 342)
Category and Type of Resource No. (%) Reported at No. (%) Reported at
Medical office visits
Primary care physician visits 22 (6) MW8 22 (6) MW8
Medical specialist visit 38 (11) MW16 39 (11) MW8
Nurse practitioner, physician’s assistant, or nurse visits 3 (1) End of CRT, MW8 4 (1) End of CRT, MW8, MW16
Telephone calls 3 (1) MW8 4 (1) End of CRT, MW8
Laboratory tests/radiology procedures
Nonstudy laboratory visits 11 (3) End of CRT, MW8 13 (4) MW8
Nonstudy radiology visits 10 (3) End of CRT 11 (3) MW16
Other nonstudy visits 6 (2) MW8 11 (3) WD
Home health care: home health care visits 2 (1) MW8 2 (1) WD
Hospital extended care
Days in general ward 19 (5) End of CRT 12 (4) End of CRT
Days in intensive care 2 (1) WD 2 (1) MW16, WD
Days in extended care facility 1 (⬍ 1) MW56, WD 1 (⬍ 1) WD
Urgent care: emergency room visits 5 (1) End of CRT 7 (2) End of CRT, MW8
Abbreviations: CRT, chemoradiotherapy; MW, maintenance week; WD, withdrawal.
www.jco.org © 2015 by American Society of Clinical Oncology
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
Table A4. Summary of Exposure to Chemotherapy (safety population)
Variable Placebo (n ⫽ 336) Lapatinib (n ⫽ 349)
ⴱ
No. of cycles of cisplatin received, No. (%)
0 11 (3) 9 (3)
1 19 (6) 28 (8)
2 92 (27) 106 (30)
3 214 (64) 205 (59)
4 0 0
5 0 1 (⬍ 1)†
Total actual dose of cisplatin, mg/m2
No. of patients 325 340
Mean (SD) 251.46 (60.143) 243.25 (63.324)
Median (range) 280.00 (37.6-300.0) 266.52 (56.7-300.0)
Total actual dose of cisplatin, mg
No. of patients 325 340
Mean (SD) 436.75 (115.786) 420.13 (118.187)
Median (range) 458.00 (50.0-655.8) 437.50 (80.0-692.0)
Total duration of cisplatin, days
No. of patients 325 340
Mean (SD) 36.30 (12.766) 34.84 (13.636)
Median (range) 43.00 (1.0-59.0) 43.00 (1.0-59.0)
Switch from cisplatin to carboplatin, No. (%) 328 344
Cisplatin only 316 (96) 334 (97)
Carboplatin only 3 (⬍ 1) 4 (1)
Switched 10 (3) 6 (2)
No. of chemotherapy cycles received,‡, No. (%)
0 8 (2) 5 (1)
1 11 (3) 25 (7)
2 96 (29) 104 (30)
3 218 (65) 208 (60)
4 1 (⬍ 1) 2 (⬍ 1)
5 1 (⬍ 1) 3 (⬍ 1)
6 0 0
7 1 (⬍ 1) 2 (⬍ 1)
Abbreviation: SD, standard deviation.
ⴱ
Any dose in the electronic case report form was considered a cycle, regardless of regimen (13 patients had ⱕ14 days between doses).
†After the second cisplatin dose of an every-3-week regimen, one patient switched to a weekly regimen and received three additional doses, resulting in a total
of five cisplatin cycles.
‡Includes both cisplatin and carboplatin. Some patients were on a weekly cisplatin/carboplatin regimen.
Table A5. Summary of Exposure to Radiotherapy (safety population)
Radiotherapy Variable Placebo (n ⫽ 336) Lapatinib (n ⫽ 349)
Actual cumulative dose, Gy
No. of patients 328 345
Mean (SD) 64.65 (7.331) 63.47 (11.238)
Median (range) 66.00 (4.0-76.0) 66.00 (8.0-86.0)
Actual cumulative dose, fractions
No. of patients 328 345
Mean (SD) 32.32 (3.666) 31.72 (5.620)
Median (range) 33.00 (2.0-38.0) 33.00 (4.0-43.0)
Duration of treatment phase (days)
No. of patients 328 345
Mean (SD) 47.41 (6.905) 46.43 (9.261)
Median (range) 47.00 (2.0-76.0) 47.00 (4.0-70.0)
Abbreviation: SD, standard deviation.
© 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Lapatinib and Chemoradiotherapy in SCCHN
Table A6. Overall Quality-of-Life Responder Status Based on FACT Scores
% Change
Scale and Type
of Change Lapatinib (n ⫽ 307) Placebo (n ⫽ 306) P
FACT H&N subscale .082
Improvement 19 25
Stable 4 5
Worsening 78 70
FACT TOI .098
Improvement 18 22
Stable ⬍1 2
Worsening 82 76
FACT-G .038
Improvement 30 39
Stable 3 4
Worsening 66 57
FACT-H&N total .007
Improvement 24 33
Stable 4 7
Worsening 72 60
NOTE. Overall responder status determined at the first visit that showed a clinically relevant improvement or worsening. Percentages may not add to 100% as a
result of rounding.
Abbreviations: FACT, Functional Assessment of Cancer Therapy; FACT-G, Functional Assessment of Cancer Therapy–General; FACT-H&N, Functional Assessment
of Cancer Therapy–Head and Neck; TOI, Trial Outcome Index.
1.0 HPV−/placebo
HPV−/lapatinib
Disease-Free Survival
HPV+/placebo
0.8 HPV+/lapatinib
(probability)
0.6
0.4
HPV/p16− HPV/p16+
0.2 Placebo arm Lapatinib arm Placebo arm Lapatinib arm
n 284 276 21 23
Events: disease recurrence 93 (33) 102 (37) 3 (14) 5 (22)
or death, n (%)
0 Median DFS (95% CI) NR (54.6 to NR) 51.5 (42.6 to 61.2) NR (NR to NR) NR (NR to NR)
Hazard ratio (95% CI) 1.16 (0.88 to 1.54) 1.32 (0.33 to 5.33)
Two-sided P .29 .70
0 10 20 30 40 50 60 70
Time Since Random Assignment (months)
No. at risk
HPV−/placebo 284 173 142 107 74 36 6
HPV−/lapatinib 276 164 134 102 71 34 10 1
HPV+/placebo 21 15 12 8 6 4 1
HPV+/lapatinib 23 18 18 13 7 2 1
Fig A1. Kaplan-Meier estimates of disease-free survival (DFS; intent-to-treat population) independently assessed by human papillomavirus (HPV) status (HPV and
p16). NR, not reached.
www.jco.org © 2015 by American Society of Clinical Oncology
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
Harrington et al
Adjusted Mean Change
From Baseline (95% CI)
4
2
0
−2
−4
−6
−8
−10
−12 Lapatinib
−14 Placebo
−16
8* 16* 24* 32* 40* 48 56*
e
py -
en al
ra mo
lin
tm w
Maintenance Weeks
*
t
ea ra
se
he e
ot ch
tr hd
Ba
di f
it
ra d o
om W
En
fr
Scheduled Assessments
Fig A2. Adjusted mean change from baseline in the Functional Assessment of Cancer Therapy–General score. (*) Denotes a statistically significant (P ⬍ .05)
difference versus placebo. Estimates that fall outside of the shaded region can be interpreted as a clinically meaningful change based on Ringash et al (Qual Life Res
13:725-733, 2004).
0.08
Adjusted Mean Change
From Baseline (95% CI)
−0.08
−0.16
−0.24 Lapatinib
Placebo
−0.32
8 16* 24 32 40 48 56
e
py -
en al
ra mo
lin
tm w
Maintenance Weeks
*
t
ea ra
se
he e
ot ch
tr hd
Ba
di f
it
ra o
om W
d
En
fr
Scheduled Assessments
Fig A3. Adjusted mean change from baseline in the EQ-5D utility index score. (*) Denotes a statistically significant (P ⬍ .05) difference versus placebo. Estimates
that fall outside of the shaded region can be interpreted as a clinically meaningful change based on Pickard et al (Health Qual Life Outcomes 5:70, 2007).
© 2015 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at University of Ca San Diego on November 3, 2015 from
Copyright © 2015 American Society of Clinical Oncology. All rights reserved.
132.239.1.230
You might also like
- Maxillofacial Rehabilitation - Prosthodontic and Surgical Considerations - John Beumer III, Thomas A. Curtis, Mark T. Marunick - 2nd Edition (1996) PDFDocument526 pagesMaxillofacial Rehabilitation - Prosthodontic and Surgical Considerations - John Beumer III, Thomas A. Curtis, Mark T. Marunick - 2nd Edition (1996) PDFVyoma83% (6)
- Atlas of Head & Neck Surgery-Vol 2 Lore & Medina PDFDocument848 pagesAtlas of Head & Neck Surgery-Vol 2 Lore & Medina PDFroata cristian100% (3)
- Vivas For The Oral and Maxillofacial Surgery FRCS-WDocument241 pagesVivas For The Oral and Maxillofacial Surgery FRCS-Warisnicole588% (8)
- MeduloblastomaDocument7 pagesMeduloblastomasilvia erfanNo ratings yet
- NPCDocument8 pagesNPCArsy Mira PertiwiNo ratings yet
- Curran 2011Document9 pagesCurran 2011Nguyễn Hoàng PhúcNo ratings yet
- JCO 2003 Lin 631 7Document7 pagesJCO 2003 Lin 631 7Adhika Manggala DharmaNo ratings yet
- 1 4918218693336367165 PDFDocument14 pages1 4918218693336367165 PDFjorgeaznarNo ratings yet
- 9 Randomized Phase III Evaluation of Cisplatin PlusDocument6 pages9 Randomized Phase III Evaluation of Cisplatin Plustrifamonika23No ratings yet
- 559 FullDocument5 pages559 FullSukhvinder Singh RanaNo ratings yet
- Impact On Survival On Interval Between Surgery andDocument10 pagesImpact On Survival On Interval Between Surgery andZamekile LukheleNo ratings yet
- Background: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckDocument10 pagesBackground: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckjoitNo ratings yet
- SouthAsianJCancer6115-2517942 065939Document5 pagesSouthAsianJCancer6115-2517942 065939Gibi SupitNo ratings yet
- Gynecology and Minimally Invasive Therapy: Case ReportDocument5 pagesGynecology and Minimally Invasive Therapy: Case ReportMetharisaNo ratings yet
- Annonc mdw587.026Document1 pageAnnonc mdw587.026Aaron Paul BernasNo ratings yet
- CapeOX ChronicleDocument22 pagesCapeOX ChronicleOttofianus Hewick KalangiNo ratings yet
- Nej Mo A 1905287Document12 pagesNej Mo A 1905287Ari KurniawanNo ratings yet
- Cisplatin-Based Chemoradiation Plus Cetuximab in Head and Neck Cancer Ann Oncol-2010-Merlano-annonc - mdq412Document6 pagesCisplatin-Based Chemoradiation Plus Cetuximab in Head and Neck Cancer Ann Oncol-2010-Merlano-annonc - mdq412ZuriNo ratings yet
- Ournal of Linical Ncology: PurposeDocument7 pagesOurnal of Linical Ncology: PurposeFadhillah ArafahNo ratings yet
- Car T LymphomaDocument14 pagesCar T LymphomaMuneer KhalamNo ratings yet
- Neoadjuvant Chemoradiotherapy Followed by Surgery VersusDocument15 pagesNeoadjuvant Chemoradiotherapy Followed by Surgery VersusRaul Matute MartinNo ratings yet
- FLOT 3 QuimioterapiaDocument8 pagesFLOT 3 Quimioterapiaerica corral corralNo ratings yet
- Wenzel 2005Document8 pagesWenzel 2005cikox21848No ratings yet
- P ('t':'3', 'I':'176969959') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document8 pagesP ('t':'3', 'I':'176969959') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Cecep Saeful HudaNo ratings yet
- Cisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerDocument10 pagesCisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerSouvik SahaNo ratings yet
- 551 PDFDocument5 pages551 PDFfaidgustisyarifNo ratings yet
- Sciencedirect: Original ResearchDocument10 pagesSciencedirect: Original ResearchchubyXDNo ratings yet
- 10 Anos Cross Trial Jco2021Document11 pages10 Anos Cross Trial Jco2021alomeletyNo ratings yet
- Contemporary Management of Advanced Laryngeal CancDocument3 pagesContemporary Management of Advanced Laryngeal Cancandre halimNo ratings yet
- Journal of Clinical Oncology Volume 32 Number 19 July 2014Document10 pagesJournal of Clinical Oncology Volume 32 Number 19 July 2014ivssonNo ratings yet
- Fonc 11 693386Document9 pagesFonc 11 693386Luana FerreiraNo ratings yet
- s13014 015 0495 4Document6 pagess13014 015 0495 4produxing 101No ratings yet
- FriquitinibDocument11 pagesFriquitinibMr. LNo ratings yet
- International Seminars in Surgical OncologyDocument8 pagesInternational Seminars in Surgical OncologyAhmad ShafiqNo ratings yet
- Esofago Carvical Valmasoni 2018Document9 pagesEsofago Carvical Valmasoni 2018Carlos N. Rojas PuyolNo ratings yet
- Survival With Cemiplimab in Recurrent Cervical CancerDocument12 pagesSurvival With Cemiplimab in Recurrent Cervical CancerKassem HijazyNo ratings yet
- Heymach-2022-Design and Rationale For A Phase1Document5 pagesHeymach-2022-Design and Rationale For A Phase1Luca BertolacciniNo ratings yet
- Nimotuzumab With Induction Chemotherapy and Chemo-Radiation in Patients With Advanced Head and Neck CancerDocument8 pagesNimotuzumab With Induction Chemotherapy and Chemo-Radiation in Patients With Advanced Head and Neck Cancerdewi ratnasariNo ratings yet
- Ipilimumab For Patients With Relapse After Allogeneic TransplantationDocument11 pagesIpilimumab For Patients With Relapse After Allogeneic TransplantationMhmd KorosNo ratings yet
- PIIS014067361261900XDocument10 pagesPIIS014067361261900X呂鍇東No ratings yet
- Glandula SalivarDocument8 pagesGlandula SalivarporsanimedNo ratings yet
- Analysis of Compliance, Toxicity and Survival WeeklyDocument11 pagesAnalysis of Compliance, Toxicity and Survival Weeklydanu20No ratings yet
- Ournal of Linical Ncology: PurposeDocument7 pagesOurnal of Linical Ncology: PurposeIvor Wiguna Hartanto WilopoNo ratings yet
- 166440996249740030Document10 pages166440996249740030111No ratings yet
- Articles: BackgroundDocument12 pagesArticles: BackgroundHalizah DamayNo ratings yet
- Tca 12 2161Document9 pagesTca 12 2161hafidisara05No ratings yet
- No Está Claro Dar RT A Lo Bestia Sino Se CuraDocument7 pagesNo Está Claro Dar RT A Lo Bestia Sino Se Curaouf81No ratings yet
- Improved Outcome by Adding Concurrent Chemotherapy ToDocument9 pagesImproved Outcome by Adding Concurrent Chemotherapy ToRaul Matute MartinNo ratings yet
- Advanced Colorectal Cancer: ESMO Clinical Practice Guidelines For TreatmentDocument5 pagesAdvanced Colorectal Cancer: ESMO Clinical Practice Guidelines For TreatmentMohamed OsamaNo ratings yet
- Head NeckDocument8 pagesHead NeckerandolphsavageNo ratings yet
- Jco 2007 11 4991Document7 pagesJco 2007 11 4991brasilianaraNo ratings yet
- Renal Cell Carcinoma A Case Series With Integrative Treatment 2329 6771 S1 002Document5 pagesRenal Cell Carcinoma A Case Series With Integrative Treatment 2329 6771 S1 002VanroNo ratings yet
- Eddy 2007Document8 pagesEddy 2007Mimsy Quiñones TafurNo ratings yet
- Annotated BibDocument16 pagesAnnotated Bibapi-542958465No ratings yet
- Baumann 2013Document8 pagesBaumann 2013nimaelhajjiNo ratings yet
- Hemdan 2014Document6 pagesHemdan 2014DavorIvanićNo ratings yet
- Post-Remission Therapy For Acute Myeloid Leukemia: Department of Internal Medicine III, University Hospital Ulm, GermanyDocument8 pagesPost-Remission Therapy For Acute Myeloid Leukemia: Department of Internal Medicine III, University Hospital Ulm, GermanyMini Bekti NingsihNo ratings yet
- Nejmp 038171Document3 pagesNejmp 038171Rifki Effendi SuyonoNo ratings yet
- First-Line Crizotinib Versus Chemotherapy in ALK-Positive Lung CancerDocument11 pagesFirst-Line Crizotinib Versus Chemotherapy in ALK-Positive Lung CancerRitam JoarderNo ratings yet
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocument12 pagesClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieNo ratings yet
- JR Kemo TitaDocument21 pagesJR Kemo TitaTitaPuspitasariNo ratings yet
- 2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumDocument8 pages2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumJad DegheiliNo ratings yet
- Cancer Regional Therapy: HAI, HIPEC, HILP, ILI, PIPAC and BeyondFrom EverandCancer Regional Therapy: HAI, HIPEC, HILP, ILI, PIPAC and BeyondNo ratings yet
- Differential Diagnosis of Head and SwellingDocument41 pagesDifferential Diagnosis of Head and Swellingmachine318No ratings yet
- (Ajomr)Document10 pages(Ajomr)MuhasbirNo ratings yet
- Oral Cavity CancerDocument16 pagesOral Cavity CancerIlma Kurnia SariNo ratings yet
- Human Pathology: Case Reports: Farid M., Protts F., Michael P. TDocument2 pagesHuman Pathology: Case Reports: Farid M., Protts F., Michael P. TInes Camilla PutriNo ratings yet
- Fhno Course Curriculum PDFDocument5 pagesFhno Course Curriculum PDFHarsha VardhanNo ratings yet
- Treatment MaligannciesDocument11 pagesTreatment MaligannciesannaNo ratings yet
- Dental Management of Pediatric Patients Receiving Immunosuppressive Therapy and or Head and Neck RadiationDocument10 pagesDental Management of Pediatric Patients Receiving Immunosuppressive Therapy and or Head and Neck RadiationمعتزباللهNo ratings yet
- CNS TumorsDocument32 pagesCNS TumorsjaveriaNo ratings yet
- Brain Tumors - An Overview: Presented by DR - Raviraj.Ghorpade Consultant Brain & Spine Surgeon BelgaumDocument33 pagesBrain Tumors - An Overview: Presented by DR - Raviraj.Ghorpade Consultant Brain & Spine Surgeon BelgaumRAVIRAJ GHORPADE BELGAUM ADVANCED NEUROSURGERYNo ratings yet
- Neoplasma Lecture For FKG''Document62 pagesNeoplasma Lecture For FKG''ginulNo ratings yet
- 681 FullDocument6 pages681 FullKurnia AnharNo ratings yet
- Carmignani 2018Document9 pagesCarmignani 2018Khumaira SantaNo ratings yet
- 2021 MO Laser CCEODocument8 pages2021 MO Laser CCEOAndressa A.No ratings yet
- A Systematic Review of Dysgeusia Induced by Cancer TherapiesDocument7 pagesA Systematic Review of Dysgeusia Induced by Cancer TherapiesWamberto AlmeidaNo ratings yet
- OSCEs For DentistryDocument3 pagesOSCEs For DentistryDame rohana50% (2)
- Liu - Ijos 2017Document11 pagesLiu - Ijos 2017Rohan BhagatNo ratings yet
- Genot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaDocument8 pagesGenot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaLarisssaa FerreiraNo ratings yet
- Detailed Lesson Plan in Mapeh 8 JoanneDocument9 pagesDetailed Lesson Plan in Mapeh 8 JoanneLANI JOY TABAMONo ratings yet
- Malignant Melanoma of The External EarDocument4 pagesMalignant Melanoma of The External EarNur Aisyah Soedarmin IieychaNo ratings yet
- Masa CervicalDocument9 pagesMasa CervicalMdacNo ratings yet
- RadiotherapyProtocols 2010V2 0Document86 pagesRadiotherapyProtocols 2010V2 0Diana MaicanNo ratings yet
- Study of Cancer Investigatory ProjectDocument19 pagesStudy of Cancer Investigatory ProjectShivam Shankar AnandNo ratings yet
- Full Chapter Nonlinear Fiber Optics 5Th Edition Govind P Agrawal PDFDocument53 pagesFull Chapter Nonlinear Fiber Optics 5Th Edition Govind P Agrawal PDFphyllis.hopson820100% (3)
- Gambaran Makroskopik Dan Mikroskopik Neoplasma Sistem Saraf PusatDocument7 pagesGambaran Makroskopik Dan Mikroskopik Neoplasma Sistem Saraf PusatIngrid NataschaNo ratings yet
- Basic Oncology RadiationDocument30 pagesBasic Oncology Radiationnugra raturandangNo ratings yet
- Brockstein - Head and Neck CancerDocument387 pagesBrockstein - Head and Neck CancerDr. Christian Dimitrov100% (1)
- J Oraloncology 2015 03 012Document8 pagesJ Oraloncology 2015 03 012Vitória LeiteNo ratings yet