Professional Documents
Culture Documents
Nursing Care Plan
Nursing Care Plan
Uploaded by
Lura Xstilice B. GalinatoCopyright:
Available Formats
You might also like
- Nursing Diagnosis Diabetic KetoacidosisDocument11 pagesNursing Diagnosis Diabetic Ketoacidosismonisha50% (4)
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرة100% (2)
- Nursing Care PlanDocument37 pagesNursing Care Planpia lestrange100% (6)
- Chak de India Management Perspective ProjectDocument21 pagesChak de India Management Perspective ProjectMr. Umang PanchalNo ratings yet
- Nursing Care Plan For "Diabetes Mellitus - Diabetic Ketoacidosis"Document17 pagesNursing Care Plan For "Diabetes Mellitus - Diabetic Ketoacidosis"jhonroks97% (36)
- Coronary Artery Disease Care PlanDocument2 pagesCoronary Artery Disease Care PlanDanelle Harrison, RN100% (2)
- Diabetes Mellitus Nursing Care PlanDocument7 pagesDiabetes Mellitus Nursing Care PlanjamieboyRN91% (32)
- HypertensionDocument13 pagesHypertensionkennedy1434450% (4)
- 3 Nursing Care Plan Diabetes MellitusDocument5 pages3 Nursing Care Plan Diabetes MellitusAnnisa Silvera II50% (2)
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonNo ratings yet
- Nursing Care Plan For A Patient With Pleural EffusionDocument5 pagesNursing Care Plan For A Patient With Pleural Effusionmac042250% (4)
- 6 Diabetes Mellitus Nursing Care PlansDocument14 pages6 Diabetes Mellitus Nursing Care PlansMerlyn Rivera PelecinNo ratings yet
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرةNo ratings yet
- Nursing Care PlanDocument10 pagesNursing Care PlanZerica Andaca83% (6)
- Sodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyDocument5 pagesSodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyMorgan Mitchell100% (10)
- 314Document65 pages314dim4erema100% (3)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel100% (2)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- NCP For DM1Document2 pagesNCP For DM1Pau Hipol MadriagaNo ratings yet
- NCPDocument7 pagesNCPChris Denver BancaleNo ratings yet
- ACTIVITY 1: Nursing Care PlanDocument4 pagesACTIVITY 1: Nursing Care PlanChelsea JardelezaNo ratings yet
- Nursing Care Plan For "DYSRHYTHMIAS"Document12 pagesNursing Care Plan For "DYSRHYTHMIAS"jhonroks79% (14)
- Nursing Care Plan "Diabetes"Document8 pagesNursing Care Plan "Diabetes"Senor Senior100% (1)
- NCP FVDDocument2 pagesNCP FVDMarlon AnryNo ratings yet
- Pregnancy Induced Hypertension Nursing Diagnosis NANDADocument9 pagesPregnancy Induced Hypertension Nursing Diagnosis NANDASanal S SalimNo ratings yet
- NCP Heart BlockDocument3 pagesNCP Heart BlockEköw Santiago Javier33% (3)
- Assessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGDocument11 pagesAssessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGGrape JuiceNo ratings yet
- NCPDocument15 pagesNCPCamille PinedaNo ratings yet
- Nursing Diagnosis For TonsillitisDocument3 pagesNursing Diagnosis For TonsillitisVaneca Go67% (9)
- Nursing Care Plan For DM PatientDocument10 pagesNursing Care Plan For DM PatientRainier Rhett Concha100% (5)
- Risk For Fluid ImbalanceDocument8 pagesRisk For Fluid Imbalanceapi-277522722100% (1)
- Nursing Care in Patient With Diabetes MellitusDocument24 pagesNursing Care in Patient With Diabetes Mellitusmira utami ningsih83% (6)
- Nursing Care PlanDocument28 pagesNursing Care PlanChristine Karen Ang Suarez67% (3)
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionStephanie Louisse Gallega Hisole100% (2)
- Nursing Care Plans For UTIDocument2 pagesNursing Care Plans For UTIHannah Pin67% (3)
- Diabetic KetoacidosisDocument5 pagesDiabetic KetoacidosisJill Catherine Cabana100% (3)
- Nursing Care Plan For HypoglycemiaDocument3 pagesNursing Care Plan For HypoglycemiaPuteri AzmanNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanRhitzle Ann100% (1)
- Septic ShockDocument1 pageSeptic ShockShaine Wolfe100% (1)
- Velez College of Nursing F. Ramos Street, Cebu CityDocument57 pagesVelez College of Nursing F. Ramos Street, Cebu Cityinah krizia lagueNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care Planjnx_anonymousNo ratings yet
- Nursing Care Plan Infection)Document4 pagesNursing Care Plan Infection)Kez Domine100% (1)
- CP Intestinal Obstruction Nursing Care PlanDocument7 pagesCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaNo ratings yet
- Nursing Care Plans All PresentationsDocument23 pagesNursing Care Plans All PresentationsKaren Joyce Costales Magtanong100% (3)
- NCP - DM - FatigueDocument12 pagesNCP - DM - FatigueJisel-Apple BulanNo ratings yet
- Nursing Care Plans For Activity IntoleranceDocument3 pagesNursing Care Plans For Activity Intoleranceravenshadow100% (2)
- Nursing Care Plan DiabetesDocument2 pagesNursing Care Plan DiabetesJen Faye Orpilla100% (9)
- Hyperkalemia: Ateneo de Naga University College of Nursing Nursing Care PlanDocument1 pageHyperkalemia: Ateneo de Naga University College of Nursing Nursing Care PlanRenie Serrano100% (1)
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalNo ratings yet
- Heart Failure Care PlanDocument2 pagesHeart Failure Care PlanJonathon100% (1)
- A Renal Failure (NCP)Document2 pagesA Renal Failure (NCP)Julie Aranda Hapin100% (1)
- CRF Fluid Volume Excess NCPDocument3 pagesCRF Fluid Volume Excess NCPchubbielitaNo ratings yet
- Heart Failure Care PlanDocument6 pagesHeart Failure Care PlanOlivia Winkler StuartNo ratings yet
- Myocardial InfarctionDocument20 pagesMyocardial Infarctionshmily_0810100% (2)
- Anemia NCPDocument20 pagesAnemia NCPNursidar Pascual Mukattil80% (5)
- Pleural Effusion NCPsDocument7 pagesPleural Effusion NCPsJaja Nagallo100% (2)
- Pre & Post Operative TracheostomyDocument2 pagesPre & Post Operative TracheostomyHantu Kak Limah100% (2)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)ghellersNo ratings yet
- DR HANY KHALIL Diabetes ComplicationsDocument54 pagesDR HANY KHALIL Diabetes ComplicationsEslam HamadaNo ratings yet
- DKADocument5 pagesDKAMariel BernabeNo ratings yet
- PLAN1Document3 pagesPLAN1Raya Ibarra LumogdangNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Ec6004 Satellite Communication r2013Document2 pagesEc6004 Satellite Communication r2013Anonymous JnvCyu85No ratings yet
- FBFP UserGuide 2 21Document88 pagesFBFP UserGuide 2 21Zlatko OžanićNo ratings yet
- Web Designing Am ItDocument25 pagesWeb Designing Am ItAmit VermaNo ratings yet
- D C A B: Installation Electronic Vessel Control D4, D6 EVC - CDocument2 pagesD C A B: Installation Electronic Vessel Control D4, D6 EVC - Csivan_sg1800No ratings yet
- Finding Solar Potential Using QGISDocument4 pagesFinding Solar Potential Using QGISJailly AceNo ratings yet
- Giant Water Heater Parts - DT016-172-BPS-EPS-EnDocument2 pagesGiant Water Heater Parts - DT016-172-BPS-EPS-EnFrancois TheriaultNo ratings yet
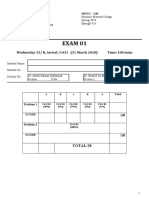
- Meng 310 Exam 01 Spring 2010Document4 pagesMeng 310 Exam 01 Spring 2010Abdulrahman AlzahraniNo ratings yet
- How To Analyse Non-Fictional Texts-1Document5 pagesHow To Analyse Non-Fictional Texts-1chaymaelmeknassi2No ratings yet
- Market SegmentationDocument30 pagesMarket Segmentationmldc2011No ratings yet
- English in The Middle AgesDocument216 pagesEnglish in The Middle AgesAna Basarte100% (2)
- Plete Collection Xvid (1) TorrentDocument1,297 pagesPlete Collection Xvid (1) TorrentShawn Fernandez25% (8)
- Psycosocial Activities Day 3Document40 pagesPsycosocial Activities Day 3John Briane CapiliNo ratings yet
- Judicial Review CSGDocument13 pagesJudicial Review CSGSushmaNo ratings yet
- Glaciers Notes Part 1Document6 pagesGlaciers Notes Part 1David ZhaoNo ratings yet
- Repair-Training Quotation: Dododo Medical Equipment Service Co.,LtdDocument1 pageRepair-Training Quotation: Dododo Medical Equipment Service Co.,LtdPhong DoNo ratings yet
- HDHR-242U: High Density PolyethyleneDocument1 pageHDHR-242U: High Density Polyethylenefrancisca ulloa riveraNo ratings yet
- 2014 Table Clinic InstructionsDocument19 pages2014 Table Clinic InstructionsMaria Mercedes LeivaNo ratings yet
- The Discriminant: Given A Quadratic Equation Use The Discriminant To Determine The Nature of The RootsDocument17 pagesThe Discriminant: Given A Quadratic Equation Use The Discriminant To Determine The Nature of The RootsdianneNo ratings yet
- Control System Kec 602Document2 pagesControl System Kec 602Nitya MishraNo ratings yet
- 01 eLMS Activity 1 Network TechnologyDocument2 pages01 eLMS Activity 1 Network Technologybasahara sengokuNo ratings yet
- DisabilityDocument34 pagesDisabilitymeghnaumNo ratings yet
- India 2020 - A Vision For The New MilleniumDocument13 pagesIndia 2020 - A Vision For The New MilleniumsanjeevNo ratings yet
- IMC 151 - PAIR AssignmentDocument37 pagesIMC 151 - PAIR Assignmentfarishaemylia40No ratings yet
- 1 SM PDFDocument12 pages1 SM PDFElan Patria NusadiNo ratings yet
- TS TR 0075 D PDFDocument2 pagesTS TR 0075 D PDFromanjcNo ratings yet
- Machine Learning in GeoscienceDocument22 pagesMachine Learning in GeoscienceAde PrayudaNo ratings yet
- Journaling PDFDocument1 pageJournaling PDFMargarita Maria Botero PerezNo ratings yet
- Sage Instant Accounts Uk Ed...Document3 pagesSage Instant Accounts Uk Ed...TPKratorNo ratings yet
Nursing Care Plan
Nursing Care Plan
Uploaded by
Lura Xstilice B. GalinatoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan
Nursing Care Plan
Uploaded by
Lura Xstilice B. GalinatoCopyright:
Available Formats
nursing Care Plan
Nursing Diagnosis Fluid Volume Deficit r/t active fluid loss (increased urine output) Long Term Goal: Patient will have adequate fluid balance
Short Term Goals / Outcomes: Patients will maintain urine output >30 ml/hr, BP > 90/60, HR 60-100 and glucose 70-200 mg/dl. Patient will demonstrate elastic skin turgor and moist, pink mucous membranes. Intervention Weigh patient daily. Rationale Changes in weight can provide information on fluid balance and the adequacy of volume replacement. 1lb = 2.2kg. Fluid volume deficit reduces glomerular filtration and renal blood flow causing oliguria. The patient in DKA may also be undergoing osmotic diuresis and have excessive outputs. Poor turgor, dry membranes and excessive thirst are all signs of dehydration. Compensatory mechanisms result in peripheral vasoconstriction with a weak thready pulse, drop in systolic blood pressure, orthostatic hypotension and reduced CVP. Evaluation Patient able to maintain weight.
Measure and record urine output hourly; report urine output less than 30ml for 2 consecutive hours. Assess skin turgor, mucous membranes and complaints of thirst. Measure vital signs, including CVP (central venous pressure).
Intake equal to output.
Membranes pink and moist, no tenting. BP 100/60, HR 80, RR 24, urine output >30ml/hr CVP 6.
Assess neurological status.
Alterations in mental status can omlur Awake, alert and oriented from severe volume depletion and altered X3. sodium levels, Patients are also at risk for seizures. Glucose has a high osmotic pull. Glucose levels needs to be reduced gradually for the fluid balance to omlur. A steady decline of 50 to 75 mg/hr is desirable. Insulin therapy needs to continue until ketoacidosis is resolved. Glucose decreased from 350 to 280 in first hour of treatment.
Monitor serum glucose every 30 to 60 minutes, then hourly as long as insulin infusion continues. Notify physician if glucose does not fall by 50 mg/dl in the initial hour. Monitor for
Because insulin therapy needs to continue No signs of hypoglycemia
hypoglycemia.
until ketoacidosis is resolved and the blood glucose improves faster than the acidosis, hypoglycemia can omlur. Osmotic diuresis causes increased excretion of potassium. Insulin therapy results in shifting of potassium intracellular. Both DKA and HHNS result in a total body deficit for potassium. Serum potassium may be elevated, normal, or low. Goal is to maintain levels between 3 and 4 mEq/L. With insulin therapy and as ketoacidosis resolves potassium levels can shift quickly. Hyperkalemia can develop.
noted.
Assess for signs of hypokalemia: fatigue, malaise, confusion, muscle weakness, cramping, shallow respirations and cardiac abnormalities. Assess for signs of hyperkalemia: irritability, weakness, EKG changes (tall peaked T waves, wide QRS, prolonged PR interval and flattened P wave). Assess for signs of hyponatremia: weakness, headache, malaise, confusion, poor skin turgor, weight loss, decreased CVP, nausea, abdominal cramps. Assess for signs of metabolic acidosis: drowsiness, Kussmaul respirations, nausea, confusion and fruity odor to the breath. Assess serum ketones / acetone levels.
No signs of hypokalemia present.
No signs of hyperkalemia present.
Hyperglycemia can cause water to be No signs of hyponatremia pulled from intracellular fluid and placed present. in the extracellular compartment, causing dilution of serum sodium. Osmotic diuresis contributes to hyponatremia.
Patients with DKA have metabolic acidosis due the build up of ketones in the blood stream.
Patient admitted with fruity breath and Kussmaul respirations, resolving with treatment.
Serum ketones are a more reliable measure than urine ketone tests. DKA is associated with elevated levels of ketone bodies in the blood. Patients with DKA have metabolic acidosis with a pH less than 7.3 and a bicarbonate less than 15 mEq/L. Normal ratio is 10:1 to 15:1. Ratios greater than 20:1 are associated with dehydration.
Serum ketone 3.0 on admission.
Assess arterial blood gases. Assess BUN/ creatine ratio.
pH 7.1 HCO3 18 metabolic acidosis. Ratio 12:1 after fluid replacement.
Assess for changes in hemoglobin, hemoatocrit and white blood cell count.
Elevations in white blood cell count may All levels WNL. indicate infection, a common precursor to DKA. All levels may be elevated due to hemoconcentration. Urine culture positive for UTI.
Assess for abnormalities Pneumonia and urinary tract infections in chest x-ray and are the most frequent infections causing urinalysis. DKA and HHNS.
Monitor for effects of IV Volume replacement is necessary to BP 100/60, HR 80, RR 24, therapy. provide adequate circulation, perfusion urine output >30ml/hr. and oxygenation of the tissues. Replacement is adequate when vital signs are back to baseline. Initiate and administer IV therapy:
0.9% NSS administered X2L. Initial goal is to correct circulatory volume deficit. Isotonic saline will rapidly expand extracellular fluid volume. The secondary goal, correction of water deficit, is usually amlomplished by a hypotonic solution. D5 NSS infusing at 65ml/hr. Vital signs normal, pulses +3, BGM 199, Urine output >30ml/hr.
Isotonic saline (0.9%) initially. Subsequent type of therapy depends, on the state of hydration, serum electrolyte levels and urinary output. Dextrose is added to IV fluids when blood glucose concentrations are less than 250 mg/dl in DKA or less than 300 mg/dl in HHS.
Dextrose is added to prevent hypoglycemia excessive decline in plasma osmolality the leads to cerebral edema.
Initiate and administer Insulin therapy:
IV bolus dose of regular insulin is followed by continuous infusion. Prime the line by
Insulin is necessary to correct the ketoacidosis. Injected forms are inconsistently absorbed when the patient is hypotensive and acidotic. Insulin has an affinity to the tubing. 50ml must be primed through the tubing, to allow the mixture to coat the tubing and make sure the patient is receiving the
Insulin infusing at 2units/hr. Serum positive for ketones.
wasting 50ml of the mixture. Administer potassium IV as ordered: typically 20 to 30 mEq/L. Administer bicarbonate as ordered.
true dose.
Potassium is added to Iv infusions once renal function has been established and serum potassium levels are below 5.5 mEq/L. This recommenced only in lifethreatening hyperkalemia, severe lactic acidosis and severe acidosis in adults with pH less than 6.9
K 3.0 20meq KCL administered over 1 hour.
pH 7.1 no bicarb needed.
Nursing Diagnosis Risk for Ineffective management of the Therapeutic Regimen related to complexity of the medical regimen
Long Term Goal: Patient will be able to selfmanage disease and prevent complications
Short Term Goals / Outcomes: Patient will verbalize dietary needs and restrictions. Patient will be compliant with pharmacological therapy. Hemoglobin A1c will be less than 6.5%. Patient will verbalize measures to prevent complications (i.e. skin/ foot care). Patient will verbalize sick day management. Intervention Determine the patients learning needs, selfmanagement skills and ability and willingness to learn. Teach signs of hyperglycemia: increased thirst, increased hunger, increased urination, fatigue, blurred vision and poor wound healing. Teach causes and prevention of hyperglycemia. Rationale An initial assessment must be done to determine what needs taught and how the patient best learns. Evaluation Patient states needs education on foot care and insulin. Learns best by demonstration. Patient able to state 3 signs of hyperglycemia.
Hyperglycemia results when inadequate insulin is present to use glucose. Excessive glucose results in an osmotic effect that causes the hallmark symptoms. Increased food intake, noncompliance with medications, infection, illness and stress will all elevate glucose levels and insulin needs. The best way to prevent hyperglycemia to be compliant with dietary restriction, medication regimen and blood glucose monitoring.
Patient states the importance of taking medications and proper diet.
Teach symptoms and causes of hypoglycemia.
Symptoms include trembling, shaking, sweating, tingling of extremities, blurred vision, slurred speech and fatigue. All causes are due to excess insulin available in relationship to nutrients. Common causes include missed or delayed meals, irregular carbohydrate content and taking medications at the wrong time.
Patient able to state 3 signs of hypoglycemia.
Teach treatment when hypoglycemia occurs:
Hypoglycemia is considered blood Patient states to drink 4-6 glucose less than 70 mg/dl. 10 to 15 ounces of juice if having grams of carbohydrate should raise the signs of hypoglycemia. 3-4 glucose tablets. glucose levels 30 to 45 mg/dl. Glucose containing products will produce faster 8-10 Lifesaver results. candies. 4-6 ounces of juice. HbA1c measures the blood glucose over the past 2-3 months, so it is a better indicator of the overall management. Noncompliance with dietary regulations can result in hyperglycemia. Regular excise reduces the risk of cardiovascular complications and has an insulin-like effect and helps lower blood glucose levels. Moderate weight loss has been shown to improve hyperglycemia and hypertension. Intensive glucose control should range between 80 and 120 mg/dl fasting. HbA1c should be below 7.0%. Patient should perform 30 minutes of moderate physical activity on most days of the week. HbA1c level 6.0%.
Monitor HbA1c levels.
Assess understanding of the diabetic diet. Assess pattern of physical exercise.
Patient states have trouble at times choosing the best foods. Patient exercises 3 times a week for 30 minutes.
Establish goals with the patient for weight loss, glucose levels, HbA1c levels and exercise regimen.
Patient and nurse agree the patient will attempt to lose 5 pounds, keep glucose between 80-120 and maintain exercise program.
Refer to registered An individualized meal plan should be dietician for individualized developed for each patient. diet instruction. Instruct to take oral hyperglycemia Hypoglycemia occurs less often with oral agents; however episodes of
Patient has appointment set up with dietician. Patient states when to take medications in relationship
medications as ordered. Instruct to take insulin as ordered. Instruct in the type, onset, peak and duration of action of specific insulin.
hypoglycemia can occur in patients who dont eat regularly. Insulin is required for individuals with type 1 diabetes and some with type 2 diabetes. Specific types of insulin vary in the onset, peak and duration. These characteristics of the specific insulin ordered determine when the injection should be administered. Inaccurate technique can result in an elevated glucose level.
to meals. Patient states when to rake insulin in relationship to meals. Patient states when to take insulin in relationship to meals.
Instruct the patient to prepare and administer insulin.
proper procedure rotation of injection sites storage of insulin mixing of insulin
Patient able to demonstrate appropriate technique, stated to rotate sites with Insulin injections should be given in the each injection. Will keep subcutaneous tissue. Injecting over the insulin in refrigerator. same site will result in reduced absorption. Insulin should be refrigerated. Unopened vials may be stored until expiration date. If the patient experiences irritation from the cold insulin, vials may be stored at room temperature for one month and then discarded. Patients should refer to the manufactures guidelines when mixing insulin. A specific routine should be individualized to each patient. In general routines should be 30 to 60 minutes in length 3-4 times a week for good glycemic control. Dehydration can hasten hypoglycemia, especially in a hot environment. Insulin requirements increase with infection. Allows the patient to guide therapy. Patient able to verbalize management during illness. Patient exercises 3 times a week for 30 minutes.
Assist patient to develop an exercise routine. Include methods to maintain hydration and prevent hypoglycemia when exercising. Instruct the patient on diabetes management during illness:
continue to take all diabetes medication self-monitor blood Provides for early detection of DKA. glucose every 2 to 4 hours
Test urine for ketones if blood glucose is consistently higher than 300 mg/dl or nausea or vomiting occur. Sufficient intake is needed to prevent Drink fluid and dehydration. simple carbohydrates: soup, pudding, etc Early treatment of hyperglycemia can prevent the occurrence of DKA or HHNS. Paten able to verbalize when extra insulin needs are necessary.
Instruct the patient to take additional short acting insulin as prescribed when:
blood glucose levels are greater than 300 mg/dl. vomiting for more than 2 to 4 hours. failure of urinary ketones to clear within 12 hours. symptoms of dehydration or developing DKA. Fungal infections in nails (thick, deformed, or ingrown) are a port of bacterial entry. general appearance Neuropathy leads to dryness, fissuring of the skin, muscle weakness and of the foot changes to the shape of the foot. status of nails Pressure over bony prominences leads abnormalities in to callus formation and skin shape of foot breakdown. callus or corn formation.
Assess skin integrity include:
Patient able to state what it is necessary to inspect the feet for.
Teach patients to inspect feet daily. Use a mirror if necessary to examine bottom of feet.
Palpate dorsalis pedis and posterior tibial pulses. Assess for edema.
Atherosclerosis results in gradual decrease in blood supply to the foot. Edema is a major predisposing factor for ulcerations. Neuropathy leads to swelling in the foot. Maceration between the toes can lead to infection. Soaking can cause maceration.
Pulses +3 bilaterally. No edema noted.
Instruct patient to wash feet daily in warm water using mild soap. Dry carefully and gently, especially between toes. Avoid soaking feet. Teach patient to report signs of infection immediately. Instruct in appropriate footwear:
Patient able to verbalize proper foot care.
Early treatment is essential to prevent amputation. To prevent injury to the foot sue to decreased sensation appropriate footwear is essentials. The widest part of the shoe must accommodate the widest part of the foot.
Patient able to verbalize signs of infection.
have foot size measured. inspect shoes daily by feeling for irregularities in lining or foreign objects in shoes. wear clean, wellfitting stockings of cotton, synthetic blend, or wool. never go barefoot.
Patient able to verbalize proper foot care.
Soft cotton or wool will absorb moisture from perspiration and discourage an environment for fungus.
Teach patient to:
Sue to loss of normal pain and temperature sensation from neuropathy test bath water with thermal injuries can occur. Patient able to verbalize wrist or elbow measure to prevent a avoid heating pads, thermal burn. hot water bottle, or electric blankets maintain safe distance form fireplace or space heater.
Instruct patient in nail care:
Avoid injury to the toes. Patient able to verbalize proper nail care.
trim straight across file sharp corners consult a podiatrist of unable to manage by self.
Teach patient to avoid over the counter selftreatment for foot problems. Teach patient to stop smoking.
Many over the counter agents contain Patient able to verbalize. salicylic acid that may cause ulceration in a diabetic foot. The vasoconstriction effects of smoking reduced the ability of the tissues to heal.
You might also like
- Nursing Diagnosis Diabetic KetoacidosisDocument11 pagesNursing Diagnosis Diabetic Ketoacidosismonisha50% (4)
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرة100% (2)
- Nursing Care PlanDocument37 pagesNursing Care Planpia lestrange100% (6)
- Chak de India Management Perspective ProjectDocument21 pagesChak de India Management Perspective ProjectMr. Umang PanchalNo ratings yet
- Nursing Care Plan For "Diabetes Mellitus - Diabetic Ketoacidosis"Document17 pagesNursing Care Plan For "Diabetes Mellitus - Diabetic Ketoacidosis"jhonroks97% (36)
- Coronary Artery Disease Care PlanDocument2 pagesCoronary Artery Disease Care PlanDanelle Harrison, RN100% (2)
- Diabetes Mellitus Nursing Care PlanDocument7 pagesDiabetes Mellitus Nursing Care PlanjamieboyRN91% (32)
- HypertensionDocument13 pagesHypertensionkennedy1434450% (4)
- 3 Nursing Care Plan Diabetes MellitusDocument5 pages3 Nursing Care Plan Diabetes MellitusAnnisa Silvera II50% (2)
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonNo ratings yet
- Nursing Care Plan For A Patient With Pleural EffusionDocument5 pagesNursing Care Plan For A Patient With Pleural Effusionmac042250% (4)
- 6 Diabetes Mellitus Nursing Care PlansDocument14 pages6 Diabetes Mellitus Nursing Care PlansMerlyn Rivera PelecinNo ratings yet
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرةNo ratings yet
- Nursing Care PlanDocument10 pagesNursing Care PlanZerica Andaca83% (6)
- Sodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyDocument5 pagesSodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyMorgan Mitchell100% (10)
- 314Document65 pages314dim4erema100% (3)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel100% (2)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- NCP For DM1Document2 pagesNCP For DM1Pau Hipol MadriagaNo ratings yet
- NCPDocument7 pagesNCPChris Denver BancaleNo ratings yet
- ACTIVITY 1: Nursing Care PlanDocument4 pagesACTIVITY 1: Nursing Care PlanChelsea JardelezaNo ratings yet
- Nursing Care Plan For "DYSRHYTHMIAS"Document12 pagesNursing Care Plan For "DYSRHYTHMIAS"jhonroks79% (14)
- Nursing Care Plan "Diabetes"Document8 pagesNursing Care Plan "Diabetes"Senor Senior100% (1)
- NCP FVDDocument2 pagesNCP FVDMarlon AnryNo ratings yet
- Pregnancy Induced Hypertension Nursing Diagnosis NANDADocument9 pagesPregnancy Induced Hypertension Nursing Diagnosis NANDASanal S SalimNo ratings yet
- NCP Heart BlockDocument3 pagesNCP Heart BlockEköw Santiago Javier33% (3)
- Assessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGDocument11 pagesAssessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGGrape JuiceNo ratings yet
- NCPDocument15 pagesNCPCamille PinedaNo ratings yet
- Nursing Diagnosis For TonsillitisDocument3 pagesNursing Diagnosis For TonsillitisVaneca Go67% (9)
- Nursing Care Plan For DM PatientDocument10 pagesNursing Care Plan For DM PatientRainier Rhett Concha100% (5)
- Risk For Fluid ImbalanceDocument8 pagesRisk For Fluid Imbalanceapi-277522722100% (1)
- Nursing Care in Patient With Diabetes MellitusDocument24 pagesNursing Care in Patient With Diabetes Mellitusmira utami ningsih83% (6)
- Nursing Care PlanDocument28 pagesNursing Care PlanChristine Karen Ang Suarez67% (3)
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionStephanie Louisse Gallega Hisole100% (2)
- Nursing Care Plans For UTIDocument2 pagesNursing Care Plans For UTIHannah Pin67% (3)
- Diabetic KetoacidosisDocument5 pagesDiabetic KetoacidosisJill Catherine Cabana100% (3)
- Nursing Care Plan For HypoglycemiaDocument3 pagesNursing Care Plan For HypoglycemiaPuteri AzmanNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanRhitzle Ann100% (1)
- Septic ShockDocument1 pageSeptic ShockShaine Wolfe100% (1)
- Velez College of Nursing F. Ramos Street, Cebu CityDocument57 pagesVelez College of Nursing F. Ramos Street, Cebu Cityinah krizia lagueNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care Planjnx_anonymousNo ratings yet
- Nursing Care Plan Infection)Document4 pagesNursing Care Plan Infection)Kez Domine100% (1)
- CP Intestinal Obstruction Nursing Care PlanDocument7 pagesCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaNo ratings yet
- Nursing Care Plans All PresentationsDocument23 pagesNursing Care Plans All PresentationsKaren Joyce Costales Magtanong100% (3)
- NCP - DM - FatigueDocument12 pagesNCP - DM - FatigueJisel-Apple BulanNo ratings yet
- Nursing Care Plans For Activity IntoleranceDocument3 pagesNursing Care Plans For Activity Intoleranceravenshadow100% (2)
- Nursing Care Plan DiabetesDocument2 pagesNursing Care Plan DiabetesJen Faye Orpilla100% (9)
- Hyperkalemia: Ateneo de Naga University College of Nursing Nursing Care PlanDocument1 pageHyperkalemia: Ateneo de Naga University College of Nursing Nursing Care PlanRenie Serrano100% (1)
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalNo ratings yet
- Heart Failure Care PlanDocument2 pagesHeart Failure Care PlanJonathon100% (1)
- A Renal Failure (NCP)Document2 pagesA Renal Failure (NCP)Julie Aranda Hapin100% (1)
- CRF Fluid Volume Excess NCPDocument3 pagesCRF Fluid Volume Excess NCPchubbielitaNo ratings yet
- Heart Failure Care PlanDocument6 pagesHeart Failure Care PlanOlivia Winkler StuartNo ratings yet
- Myocardial InfarctionDocument20 pagesMyocardial Infarctionshmily_0810100% (2)
- Anemia NCPDocument20 pagesAnemia NCPNursidar Pascual Mukattil80% (5)
- Pleural Effusion NCPsDocument7 pagesPleural Effusion NCPsJaja Nagallo100% (2)
- Pre & Post Operative TracheostomyDocument2 pagesPre & Post Operative TracheostomyHantu Kak Limah100% (2)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)ghellersNo ratings yet
- DR HANY KHALIL Diabetes ComplicationsDocument54 pagesDR HANY KHALIL Diabetes ComplicationsEslam HamadaNo ratings yet
- DKADocument5 pagesDKAMariel BernabeNo ratings yet
- PLAN1Document3 pagesPLAN1Raya Ibarra LumogdangNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Ec6004 Satellite Communication r2013Document2 pagesEc6004 Satellite Communication r2013Anonymous JnvCyu85No ratings yet
- FBFP UserGuide 2 21Document88 pagesFBFP UserGuide 2 21Zlatko OžanićNo ratings yet
- Web Designing Am ItDocument25 pagesWeb Designing Am ItAmit VermaNo ratings yet
- D C A B: Installation Electronic Vessel Control D4, D6 EVC - CDocument2 pagesD C A B: Installation Electronic Vessel Control D4, D6 EVC - Csivan_sg1800No ratings yet
- Finding Solar Potential Using QGISDocument4 pagesFinding Solar Potential Using QGISJailly AceNo ratings yet
- Giant Water Heater Parts - DT016-172-BPS-EPS-EnDocument2 pagesGiant Water Heater Parts - DT016-172-BPS-EPS-EnFrancois TheriaultNo ratings yet
- Meng 310 Exam 01 Spring 2010Document4 pagesMeng 310 Exam 01 Spring 2010Abdulrahman AlzahraniNo ratings yet
- How To Analyse Non-Fictional Texts-1Document5 pagesHow To Analyse Non-Fictional Texts-1chaymaelmeknassi2No ratings yet
- Market SegmentationDocument30 pagesMarket Segmentationmldc2011No ratings yet
- English in The Middle AgesDocument216 pagesEnglish in The Middle AgesAna Basarte100% (2)
- Plete Collection Xvid (1) TorrentDocument1,297 pagesPlete Collection Xvid (1) TorrentShawn Fernandez25% (8)
- Psycosocial Activities Day 3Document40 pagesPsycosocial Activities Day 3John Briane CapiliNo ratings yet
- Judicial Review CSGDocument13 pagesJudicial Review CSGSushmaNo ratings yet
- Glaciers Notes Part 1Document6 pagesGlaciers Notes Part 1David ZhaoNo ratings yet
- Repair-Training Quotation: Dododo Medical Equipment Service Co.,LtdDocument1 pageRepair-Training Quotation: Dododo Medical Equipment Service Co.,LtdPhong DoNo ratings yet
- HDHR-242U: High Density PolyethyleneDocument1 pageHDHR-242U: High Density Polyethylenefrancisca ulloa riveraNo ratings yet
- 2014 Table Clinic InstructionsDocument19 pages2014 Table Clinic InstructionsMaria Mercedes LeivaNo ratings yet
- The Discriminant: Given A Quadratic Equation Use The Discriminant To Determine The Nature of The RootsDocument17 pagesThe Discriminant: Given A Quadratic Equation Use The Discriminant To Determine The Nature of The RootsdianneNo ratings yet
- Control System Kec 602Document2 pagesControl System Kec 602Nitya MishraNo ratings yet
- 01 eLMS Activity 1 Network TechnologyDocument2 pages01 eLMS Activity 1 Network Technologybasahara sengokuNo ratings yet
- DisabilityDocument34 pagesDisabilitymeghnaumNo ratings yet
- India 2020 - A Vision For The New MilleniumDocument13 pagesIndia 2020 - A Vision For The New MilleniumsanjeevNo ratings yet
- IMC 151 - PAIR AssignmentDocument37 pagesIMC 151 - PAIR Assignmentfarishaemylia40No ratings yet
- 1 SM PDFDocument12 pages1 SM PDFElan Patria NusadiNo ratings yet
- TS TR 0075 D PDFDocument2 pagesTS TR 0075 D PDFromanjcNo ratings yet
- Machine Learning in GeoscienceDocument22 pagesMachine Learning in GeoscienceAde PrayudaNo ratings yet
- Journaling PDFDocument1 pageJournaling PDFMargarita Maria Botero PerezNo ratings yet
- Sage Instant Accounts Uk Ed...Document3 pagesSage Instant Accounts Uk Ed...TPKratorNo ratings yet