Professional Documents
Culture Documents
Comparative Chart Front
Comparative Chart Front
Uploaded by
bella friscaamaliaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comparative Chart Front
Comparative Chart Front
Uploaded by
bella friscaamaliaCopyright:
Available Formats
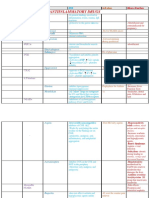
Comparison Chart of Systemic Autoinflammatory Diseases (SAID)
Cryopyrin-Associated Periodic Syndromes (CAPS) Pyrin Protein Folding Mevalonate Kinase Deficiencies Inflammatory Bone Diseases Pyogenic Diseases Granulomatous Monarch-1 Proteasome Idiopathic Macrophage Activation Diseases PLCG2-associated SLC29A3 related ADA2 deficiency
Familial Cold Muckle-Wells Neonatal-Onset Schnitzler Familial Tumour Necrosis Hyperimmuno- Mevalonate Deficiency of Majeed Syndrome Chronic Recurrent Deficiency of Familial Psoriasis Pyogenic Sterile Juvenile Systemic NLRP12-Associat- Chronic Atypical Behçets Disease Periodic Fever, Systemic-Onset Adult-Onset (Primary) Familial PLCG2-associated Autoinflammation SLC29A3 Spectrum Deficiency of Ad-
Autoinflammatory Syndrome* Multisystem Syndrome Mediterranean Factor (TNF)- globulinemia D Aciduria (MA) Interleukin-1ß –aka Chronic Recur- Multifocal Interleukin-36-Re- (PSORS2)–aka Arthritis, Granulomatosis ed Periodic Fever Neutrophilic Aphthous Stoma- Juvenile Idiopathic Stills Disease–aka Hemophagocytic Antibody Defi- & PLCG2-asso- Disorder–aka H. enosine Deami-
Syndrome* Autoinflammatory Fever* Associated with Periodic (IL-1ß) Receptor rent Multifocal Osteo- Osteomyelitis–aka ceptor Antagonist CARD14-Mediated Pyoderma –aka Blau syndrome, Syndrome–aka Dermatosis w/ titis, Pharyngitis, Arthritis–aka Still’s, Adult Still’s, Wissler- Lymphohistiocy- ciency & Immune ciated Antibody syndrome; Pigmented nase 2 (DADA2)
Hypertrichosis w/IDDM;
Disease–aka Chronic Periodic Sydrome Fever Syndrome (Mevalonate Kinase Antagonist (DIRA) myelitis, Congenital Synovitis, Acne, (DITRA)–aka Pustular Psoriasis Gangrenosum, & Pediatric Granuloma- Familal Cold Autoin- Lipodystrophy & & Cervical Ad- Systemic Juvenile Fanconi Syndrome tosis–aka Familial Dysregulation, Deficiency & Faisalabad Histiocytosis
–aka Fever w/Early
Infantile Neurological –aka Familial Hiber- (HIDS)* Deficiencies, such as –aka Osteomyelitis, Dyserythropoietic Pustulosis, Hyperosto- Generalized Pustular Acne Syndrome tous Arthritis (PGA), flammatory Syndrome Elevated Temper- enitis (PFAPA) Idiopathic Arthritis Erythrophagocytic (PLAID)–aka Familial Immune Dysregu- & Sinus Histiocytosis Onset Stroke (FEOS)
HIDS & MA are also Anemia, & Neutro- sis, Osteitis Syndrome Early Onset Sarcoido- 2, or Guadaloupe
Cutaneous Articular nian Fever* Sterile Multifocal Psoriasis (GPP) ature–aka Nakajo- –aka Marshall Lymphohistiocytosis Atypical Cold Urticaria lation (APLAID) w/Massive Lymphade-
referred to as MKD) philic Dermatosis sis, or Jabs Syndrome Periodic Fever nopathy
Syndrome (CINCA)* w/Periostitis Pustulosis Nishimura Syndrome Syndrome (FACU) or FCAS3
ACRONYM FCAS MWS NOMID/CINCA SCHNITZLER FMF TRAPS HIDS MA DIRA/OMPP MAJEED CRMO/SAPHO DITRA/PSORP CAMPS/PSORS2 PAPA BLAU/PGA/EOS NLRP12/FCAS2 CANDLE/PRAAS BEHÇETS/BD PFAPA soJIA/sJIA AOSD 1° HLH/ FHL PLAID/FCAS3 APLAID SLC29A3 DADA2
GENE NLRP3 NLRP3 NLRP3 Currently unknown. MEFV TNFRSF1A MVK MVK IL1RN LPIN2 Currently unknown. IL36RN CARD14 PSTPIP1 NOD2 NLRP12 PSMB8; also ERAP1 (with HLA-B51); Currently unknown. Currently unknown. Currently unknown. PRF1, STX11, STXBP2, Heterozygous genomic PLCG2 mutation SLC29A3 CECR1
(Some pts. w/somatic PSMB4, PSMB9, also variants near: CCR1, HLA-DRB1 in some pts. MUNC13-4 , RAB27A deletions within the
NLRP3 mutations.)76 PSMA3, POMP 59 KLRC4, STAT4 42 w/European ancestry57 X link: SH2D1A, BIRC4 PLCG2 gene64
INHERITANCE Autosomal Dominant.
Large familial groups,
Autosomal Dominant. Autosomal Dominant.
Spontaneous mutations, Spontaneous mutations,
Unknown. Autosomal Recessive.
Some cases are gene-
Autosomal Dominant.
Spontaneous mutations,
Autosomal recessive.
Some cases w/only one
Autosomal recessive. Autosomal recessive. Autosomal recessive. Currently unknown. Autosomal recessive. Autosomal Dominant.
Spontaneous mutations,
Autosomal Dominant.
Spontaneous mutations,
Autosomal Dominant. Autosomal Dominant.
Spontaneous mutations,
Autosomal recessive. Complex. Currently unknown. Complex. Currently unknown. Autosomal recessive,
but if X-linked: inheri-
Autosomal Dominant. Autosomal Dominant. Autosomal recessive. Autosomal recessive.
some spontaneous some familial groups.1 few familial cases.1 dosage-dependent some familial groups.1 mutation found.33 some familial groups.23 some familial groups.29,30 some familial groups.29,30 tance is dominant.
mutations.1 autosomal dominant.10
ETHNICITY Affects all races, but
many are of European
Affects all races, but
many are of European
Any–present in all
races.1
Affects all races, but
most cases are in
Turk, Armenian, Arab,
Sephardic Jew, Italian.1
Affects all races. 2nd
most common inherited
Mostly of Dutch descent, Mostly of Dutch
or Northern European.1 descent, or Northern
Carriers in 0.2% population
of Newfoundland & 1.3%
Currently, the only
documented cases are
Affects all races, but the
majority of patients have
May affect all races. Pts.
w/Caucasian, Spanish,
Most w/European or
Asian ancestry. Pts. in US,
Currently, the only docu- Affects all races.
mented cases are from
Unknown. Cases in Gua- Unknown. Caucasian,
deloupe, US, Martinique, Hispanic, Japanese
Rare in the USA. More
common in the Middle
Affects all races.40 Affects all races.
soJIA accounts for 10%
Rare. Affects all races.44 Affects all races. 80% of Unknown. Most reported Unknown.
African Americans, & 20% cases w/European
Unknown. Many pts. w/ Unknown.
Middle Eastern ancestry.
descent.1 descent.1 Europe.13 More men than Most common inherited SAID (after FMF.)1 European.1 in Puerto Rico. Also Dutch of Middle Eastern European ancestry; more Asian, African, Algerian EU, Canada (Newfound- Europe, New Zealand & France, Italy, & Armenia. pts. & one case in East, Asia & Japan. of all JIA.45 of pts. w/European decent ancestry. Some from India, Paki-
women are affected. periodic fever syndrome. Brazilian & Lebanese pts.16 ancestry.18 female pts. than males.21,22 & Tunisian ancestry.58,75,77 land), Haiti, & Taiwan.23 the USA.30 38,39,75
South Africa.27,60 (Silk Road Route.)42,43 have PRF1 mutations.47,48 stan, Spain, Bulgaria.70
FREQUENCY IN 1:1 million, or more. In
USA 300+ diagnosed–
1:1 million, maybe more.
Some large family
Estimated frequency
1:1 million, mostly due
Unknown. Over 150
known cases, mostly in
In specific ethnic
groups, the carrier
Unknown. TRAPS affects
0.01:10,000 people in the
Unknown, but very rare. Unknown, but very rare.
>200-300 known patients <100 known patients
Unknown, but very Unknown, but very rare.
rare. In some regions of Very few documented
Unknown, but rare. Unknown but rare. 1% of Unknown, but rare.
Sfax, Tunisians are car-
Unknown, but rare. Unknown, but rare. Unknown, but rare. Unknown, but rare. Prevalence is 80-
370:100,000 people in
Unknown. Most common Uncommon. 0.4–0.9
non-infectious recurrent cases per 100,000
France: estimated that 1° HLH affects 1:50,000
0.16:100,000 people have people worldwide.48
Unknown but rare. Unknown but rare. Unknown but rare. Unknown but rare.
THE WORLD most cases are from groups.5 Frequency of to spontaneous genetic Europe.13 frequency of MEFV vari- European Union.51 >1000 worldwide, (>300, when worldwide.11 Aricibo, Puerto Rico cases at this time.18,53 riers, w/ a 0.52% chance Turkey, 10:100,000 in fever disorder.40 people, per year.46 AOSD. AOSD affects
large family groups.2,5 CAPS in France is mutations.5 ants is up to 1:5 people.1 pts. worldwide.52 suspected cases are w/more DIRA carriers, of having the disease in Japan & 0.6:100,000 in more women than men.44
1:360,000.55 also included.)12 DIRA may occur 1:6300.16 this population.58 Yorkshire, UK.3
TIMING OF 12-24 hours, or longer.
Onset of fever & flares
Often lasts 2-3 days.
Random onset–flares of
Continuous w/increased
symptoms & fever
12-36 hours. Rash is
present first. Intermit-
12-72 hours.1,9 Days to weeks.
Recurrent fever & flares Average flare is 3
3-7 days. Recurrent bouts
of fever & flares every
4-5 days. Recurrent
flares & fever every 2-3
Continuous inflamma-
tion from birth/fetal
Flares last for a few
days, w/1-4 exacerba-
At least 6 months
w/chronic or relapsing
Flares last days–weeks.
Some w/chronic symp-
Continuous chronic
pustular or plaque
Early-onset, destructive,
recurrent inflamma-
Intermittent-persistent
daily fevers, rash &
1-3, to up to 7-15 days of
fevers 39–40°C, rash &
Frequent fevers w/dis-
ease flares. Inflammatory
Mouth ulcers are pres-
ent in almost all patients
Periodic fevers & symp-
toms lasting 3-6 days,
Fevers often > 39°C 1-2
times/day for >2 weeks,
High fevers > 39°C that
last for <4 hours,
Fevers often > 39°C 1-2
times/day for >2 weeks,
Onset <5 minutes after
exposure to cold air
Recurrent skin lesions,
chronic inflammation,
Fever 39°C w/flares that
last 7-10 days w/joint &
Intermittent, recurrent
fevers, livedo reticularis
SYMPTOMS is often 1-3 hours after fever & symptoms are during flares.1 Chronic tent fevers, that often can occur weekly, or weeks.1,9 2-12 weeks.1,9 Some weeks. Patients have development. Untreated tions a month of high symptoms. Often 7-25 toms. Most flare w/infec- psoriasis, triggered by tion of the joints, skin & arthritis. pain. Onset after expo- flares & symptoms are during flares, for around recurring every 21-28 most often occuring in recurring more than most often occurring in (evaporative cooling).64 & progressive eye abdominal pain; peri- rash, vasculopathy, &
exposure to cold or often triggered by cold inflammation noted occur separately from only a few times a year. flares occur after vac- chronic inflammation DIRA can lead to death fevers, severe pain, & yrs. of symptoms. Many tions, stress, medication inflammatory stimuli. muscle. Flares often sure to cold or cooling often present before the 10 days w/inflammation days. Pts. are symptom- the evening w/arthralgia,once a week, w/ a the evening w/arthralgia, Frequent sinus/lung complications from this carditis & sometimes high risk for early-onset
OR ATTACKS cooling temperatures.1 or cooling temperature.1 between flares. the rash.13 cines.9 noted between flares.11 in infancy–childhood.16 joint swelling.18,53 bone lesions heal changes, during preg- Some cases w/psoriatic occur after mild injury, temperatures.38,39 age of 6 months.26,27 in the eye, & arthritis.42,43 free between flares.40 rash & other symptoms. maculopapular rash & rash & other symp- infections. Concurrent disease.66,67,68 diarrhea. Flares occur lacunar stroke.73,74
completely.19,22 nancy or menstruation.58 arthritis.23,24 or injections.29 45,46
arthralgia.44 toms.47,48 autoimmune diseases.64,65 once every 2-3 months.70
AGE OF ONSET Infancy, but a few pres- Infancy, but a few Neonatal/early infancy. Most cases start in Infancy, to under 20 Most first attacks by 3 >90% present w/symp- Most present w/symp- Most have symptoms at Most present w/symp- Mostly affects children– Variable age of onset. Variable age of onset First symptoms of Rash often develops by Neonatal/early infancy. Onset at birth or in Most show symptoms Early childhood, usually Onset before the age of First onset of symptoms Onset <1yr: often by 6 Onset in infancy-under 6 Onset in infancy Onset in infancy-starts Onset of symptoms in
ent w/symptoms later present w/symptoms Rash, symptoms, & middle age, over 35-50 years of age for the first yrs, & almost all begin by toms in infancy.9 toms at birth, or in early birth, or as a neonate: toms in infancy to early some adult onset. Peak Many have symptoms from infancy–childhood arthritis develop by 1-10 4 months of age, fevers Rash, fevers, symptoms, infancy. Progressive in early adulthood between 2-5 years of 16–most often by 2 years occurs between 16-35 months–early childhood. months of age. Lifelong w/recurrent skin lesions, w/recurrent fevers infancy–early childhood.
in childhood or adoles- later in childhood or abnormal labs are often yrs. Youngest pt. was 13 symptoms.9 20 yrs. of age; a few start infancy. Most have facial pustular rash, bone pain, childhood, between 3 incidence of flares is starting in childhood. to adulthood w/pustular yrs old, & skin lesions and other symptoms may be present at damage from chronic (20’s-30’s) but the onset age. A few adult-onset of age, or between 0-5 yrs. of age. Affects all Some in utero or late symptoms, but some arthralgia, eye inflamma- & flares. Chronic & w/recurrent fevers,
cence.1 adolescence.1 present at birth.1,6 yrs old. Symptoms start later in life.9 features noted at birth.11 swollen joints, & oral weeks to 2 years of age.18 around 10 years of age.22 Some have symptoms psoriasis.23,24 develop during adoles- present by 4 yrs. of age.34 birth.38,39 inflammation noted as can be in childhood, or cases. Many teens yrs. of age.46 ages.44 childhood. A few adult- find the symptoms less tion, & infections. Some progressive systemic livedo reticularis rash, &
w/the rash.13 ulcers.16 beginning in adulthood.58 cence.29,32 the child grows.26,27 any age.42,43 outgrow it.40 onset cases.47,48,49 severe in adulthood.64,65 w/ intestinal symptoms.68 symptoms develop.69,70,71 vasculopathy.73,74
SYSTEMIC FINDINGS:
SKIN/ Cold induced urticaria-
like rash w/increased
Urticaria-like rash
w/increased neutrophils
Ever-present1 Urticaria-
like rash w/increased
Maculopapular rash,
& plaques (sometimes
Erysipeloid erythema
on the ankle–foot–be-
Migrating rash w/deep
pain under rash areas.
Diffuse maculopapular
rash. Some w/petechiae
Diffuse maculopapular
or morbilliform rash.
Epidermal neutrophilic
pustules at hair folicles.
Most patients have
inflammatory dermatosis,
Some patients have
acne, &/or pustulosis
Recurrent, generalized
pustular psoriasis & high
Generalized pustular
psoriasis (can be
Pathergy. Pyoderma
gangrenosum ulcerative
First symptom: scaly
plaques. The rash often
Present during flares:
Cold-induced urticarial
Annular cutaneous
plaques w/residual
Pathergy. Pseudofol-
liculitis, erythema
Some have a rash with
flares. Aphthous stoma-
Rash: Fleeting, evanes-
cent, migratory, bright
Evanescent, salmon-
pink, mildly pruritic
40% w/transient
maculopapular, nodular
Cold urticaria, erythema
& itching post cold expo-
Erythematous plaques &
vesiculopustular blister-
Hyperpigmentation
w/hypertrichosis.69,70 ,71,72
Livedo reticularis rash,
few w/polyarteritis nodo-
CUTANEOUS neutrophils at the ec- at the eccrine coils.4 neutrophils at the itchy) on the chest low knee region–lasts Severe pain follows the or purpura present. A Some w/petechiae or Oral ulcers, pathergy, Sweet’s syndrome, on the palms &/or soles fevers after erythema- severe), &/or plaque lesions, &/or severe starts on the face, then or malar rash39 noted in purpura. Lipodsystrophy: nodosum-like &/or titis, & pharygitis w/ salmon-pink, morbilli- maculopapular rash on or purpuric skin rashes sure (air, wet skin, cold ing rash that intensifies Some w/notable varicose sa. Diffuse vasculopathy,
crine coils.4 Almost daily Most w/daily rash that eccrine coils. Rash & limbs. Dermis has 2-3 days during flares rash path from the trunk few w/apthous ulcers.1,9 purpura present. A few hyperkeratosis, acan- pustular skin lesions, of their extremities (w/ tous rash. Some w/acral psoriasis. Sometimes cystic acne. Affected on the torso. Biopsies w/ some pts. Some with first on face & around acneiform nodules. 98% exudate, (but no form, macular rash often the proximal limbs & during bouts of high food). Some w/angioede- w/heat & sun exposure. veins on the legs.69 w/impaired endothelial
rash that increases increases w/flares.1 increases w/flares.4 neutrophillic infiltrate. of symptoms.1 out to the limbs.9 w/apthous ulcers.1,9,11 thosis; high neutrophil psoriasis. Intra-epidermal SAPHO). 23% w/psoria- pustules & nail damage, nails are affected w/ tissues w/high neutrophil non-caseating granu- buccal aphthosis.38,39 joints. Lips swell w/flares. w/mouth ulcers, & 65% infection) is a classic presents w/onset of trunk.44 fever. Jaundice.47,48 ma; chronic granulomata. Cellulitis often develops integrity & endothelial
w/flares.1 Dermographism.13 infiltrate of dermis.16,26 neutrophils.18,53 sis.19,22,54 or chronic plaques.58,61 psoriasis.23, 24 infiltration.29 lomatous dermatitis.34 Purple-red eyelids.26,27 have genital ulcers.43 finding.40,41 fevers.45,46 Ice cube test negative.64 w/rashes.66,67 cellular activation.73,74
NEUROLOGIC Some have headaches,
fatigue w/fever after
Some have headaches,
fatigue w/fever & flares.
Headaches, fever,
fatigue, chronic aseptic
Intermittent fevers can
rise > 40°C. Chills are
Fevers. Acute aseptic
meningitis is rare & can
Fevers lasting >3 days at
over 38°C w/flares.
Headaches & fevers
w/flares of symptoms
Fevers w/flares. Micro-
cephaly, dolichoceph-
High fevers are not
common, or noted in
High fevers last for a few
days w/flares & severe
Fevers affect a number
of patients during flares
Sudden onset high fever Not seen.23, 24
>40°C w/chills. Some pts.
Fevers can accompany
flares of joint inflam-
Intermittent-persistent
daily fevers. Some have-
Fevers 39–40°C myalgia,
headaches w/flares.
Aseptic meningitis &
systemic inflammation.
20-40% have Neuro-
Behçets w/headaches,
High fevers for 3-6 days,
w/chills & malaise.
High fevers >39°C 1-2
times/day for >2 weeks.
>95% have high, spiking
fevers, fatigue and
High fevers. Increased
CSF protein. High ICP.
Not noted.64,65 Not noted.66,67,68
No fevers noted w/cold- No fevers noted as a part
Fever 39°C w/flares
lasting over a week.69,70
Recurrent fevers & early-
onset lacunar strokes.
cold exposure. Uncommon to have meningitis, & high CNS uncommon. Fatigue & occur during flares, but Some have headaches are common.1,9 More aly, mental retardation, the neonatal period. pain. Other neurological of CRMO. Other neuro- have a headache w/the mation and pain. Other cranial neuropathies. Other neurological symp- Growth delays–low aseptic meningitis or Some patients have Other neurological myalgia w/flares. Multifocal inflammation induced urticaria.64,65 of this disease (but fevers Psychomotor delays, Possible adult stroke
Unknown if there are many other CNS pressure (ICP). Many headaches are common is never chronic.1 Other w/flares of symptoms.1,9 severe neurological developmental delays, Neurological complica- symptoms are not noted. logical symptoms are not onset of the rash & fever, neurological symptoms 80% have vision damage toms are not noted.31 height & weight. Devel- meningoencephalitis, headaches w/flares. symptoms are rare. A Other neurological of the gray & white may be present w/infec- dysmorphic facial risk. Brain biopsies:
notable CNS affects at symptoms.1 A few pts. with mental &/or cogni- w/fevers. Temperature neurological involve- symptoms are rarely cerebellar ataxia, tions are not common. Growth delays in height, noted. Some w/impaired plus muscle weakness & are not noted.31 & joint deformities if opmental delays.26,27 seizures, hemiplegia, or Other neurological few cases w/seizures, symptoms are very rarely matter, intracranial tions).66,67,68 features noted.69,70 diffuse vasculopathy,
this time.1 have MWS/NOMID tive impairments. Papille- changes, stress & exer- ment is very rarely seen present in HIDS.9 cerebellar atrophy & A few cases of cerebral & chronic pain are com- bone growth, or overall elevated heart rate. 58,,61 untreated. Some cases cranial nerve palsies. symptoms are meningismus, irritabil- seen.44 bleeding, generalized w/impaired endothelial
crossover of symptoms. dema is common.6 cise can trigger flares.13 in FMF. epilepsy often develop vasculitis noted.16,26 mon.18,53 impaired growth.19,22,54 have peripheral nerves Cerebral venous throm- not noted.41 ity & decreased level of atrophy or brain edema, integrity & endothelial
over time.11 affected.34 bosis w/high ICP noted.43 consciousness.46 seizures &/or coma.47 cellular activation.73,74
AUDITORY Some pts have mild
hearing loss–not cur-
Many have increased
sensorineural hearing
Many have increased
sensorineural hearing
Uncommon.13 Uncommon–not be- Uncommon–not believed Uncommon–not be-
lieved to be caused by a to be caused by TRAPS.1 lieved to be caused by
Uncommon–not believed Not noted.15,16
to be caused by MA.1,9,11
Not noted.18,53 Not noted.19,21,22,54 Not noted.58,61,62 Not seen.23, 24 Not noted.29,30,31 Not noted.34 Many have increased
sensorineural hearing
Some have frequent
otitis &/or recurrent
Not noted.42,43 Not noted.40,41 Not noted to be from
soJIA.45,46
Not noted.44 Not noted.47,48,49 Not noted.64,65 Not noted.66 Sensorineural hearing
loss, from early infancy/
Unknown.73,74
rently known if it‘s from loss, starting in adoles- loss, from infancy/child- FMF disorder.1 HIDS.1,9 loss.38,39 sinusitis.27 childhood.69,70
CAPS inflammation.1 cence.1 hood.1,6
OPHTHALMIC Conjunctivitis
(non-infectious) during
Conjunctivitis
(non-infectious) during
Papilledema, uveitis,
iritis, conjunctivitis.
Not noted.13 Very rare to uncommon.1 Conjunctivitis, & peri-
orbital edema during
Very rare to uncommon.9 Uveitis, central cataracts,
blue sclerae & tape-
Eye issues are rare.
Non-infectious conjunc-
Not noted.18,53 Some cases of uveitis.19 Not noted.58,61,62 Not seen.23, 24 Not noted.29,30,31 Uveitis (some w/blind-
ness) 50% w/cataracts,
Not noted.38,39 Nodular episcleritis (in-
flammation on the eye.)
Frequent anterior &/or
posterior uveitis. Cata-
Not noted.40,41 Uveitis can be a compli-
cation from soJIA.46
Not noted.44 Blindness due to CNS
inflammation.48
Uncommon.66 Many develop corneal
erosions, blisters,
Uveitis. Blindness can
occur from anterior
Unknown.73,74
Strokes have the poten-
flares.1 flares,1 or corneal haze.26 Some w/retinal scarring, flares.1,9 toretinal degeneration tivitis can be caused by 1:3 pts. get 2° glaucoma, Conjunctivitis. Keratitis. ract, retinal vasculitis ulcerations, intraocular uveitis & glaucoma. Pto- tial to cause blindness.
MWS/NOMID crossover corneal haze or vision are often present, even DIRA.15,16 inflamed conjunctiva, Periorbital edema. <30% risk for blindness. hypertension, &/or sis, eyelid swelling from
pts. may have more eye loss.6,26 in less severe cases.11 lacrimal glands, retina & Purple-red eyelids.26,27 Papilledema w/CNS cataracts.66,67,68 histiocytic deposits.69,70,71
involvement. optic nerves.34 involvement.43
CARDIO- Not noted.1 Rare.1 Some have clubbing of
fingers. Some cases of
Not noted.13 45% have pleuritis, pain- Common, including
ful respiration, w/flares. pleurisy.1
Rare.1 Some pts. have
developed severe respi-
Rare.1,11 Some w/resp. distress.
1 case: Pulmonary hemo-
Not noted.18,53 Not common–some pa-
Elevated heart rate. Elec- Not noted.23, 24
tients also have ANCA+
trolyte imbalances during
Not noted.29,30,31 Some have atrial hyper- Not noted.38,39
tension &/or pericarditis.
Clubbing of the fingers
&/or toes. At risk for
Myocarditis, endocarditis
w/aortic or mitral insuffi-
Flares of fevers, stoma-
Serositis (especially
titis & pharygitis are not
pericarditis) is often
<25% have pleuritis,
pericarditis (a few
High risk for respiratory
infections triggering
44% w/recurrent sinus
&/or respiratory infec-
Mild humoral immune
deficiency w/increased
Pericarditis w/flares.
Cardiac defects noted:
Unknown.73,74
PULMONARY pericardial effusions, or Some w/pericarditis.1 ratory infections. Higher siderosis & progressive Vasculitis that can
fever & onset of pustular Some cases with lung cardiac arrythmias & ciency, arterial aneurysm, associated w/respiratory
seen. Pleuritis, pleural w/tamponade.) Some fevers, systemic inflam- tions, >50% w/allergies, frequency of sinus &/or ASD, VSD, PDA, mitral
pericarditis.1 risk for issues w/S. interstitial fibrosis.15,16,17 affect the lungs.18,54
rash; Risk for cardiac ar- involvement.34,35 dilated cardiomyopa- pulmonary embolism.43 illness.40,41
effusions can occur. myocarditis, pleural mation & MAS. Edema.49 asthma &/or autoimmune respiratory infections or valve prolapse, cardio-
pneumoniae infections.78 rest, & septicemia.58,61 thy.26,27 Risk for MAS.46 effusions, ARDS.44 diseases.65 interstitial pneumonia.66,67 megaly & others.69,70
ABDOMINAL Uncommon.1 Some have abdominal
pain w/flares or other
Nausea, vomiting & GI symptoms are uncom- Sterile peritonitis, pain, Peritonitis, diarrhea, &
abdominal pain w/flares, mon. Enlarged liver &/or and/or constipation with constipation w/flares.1
Extreme pain, vomiting
& diarrhea w/flares.1,9
Enlarged liver &/or
spleen. Cholestatic liver
Rarely have GI issues. Enlarged liver & chole- Some patients also have Nausea during flares. At Not noted.23,24
Mouth ulcers, stomatitis, static jaundice in the inflammatory bowel risk for loss of appetite.58,60
Some patients also
have irritable bowel
Enlarged liver &/or Some patients have ab-
spleen. Some w/ GI pain, dominal pain w/flares.39
Loose bowels w/flares.
Enlarged liver & abdo-
Ulcers from mouth to Abdominal pain, diarrhea Peritonitis rarely occurs.
anus. Nausea, abdominal are often present w/ 50% have an enlarged
50-75% w/enlarged liver,
abnormal LFTs. 43%
Liver disease is common. Not noted. Some have
High risk of death from concurrent autoim-
Some w/bouts of
abdominal pain, bloody
Diabetes Mellitus. En-
larged liver/spleen. Abd.
Enlarged liver & spleen;
diffuse vasculopathy
gastrointestinal issues.1 or w/high CNS pressure.6 spleen is common.13 flares.1 Some w/enlarged liver/ disease. Pain, vomiting & failure to thrive are neonatal period, but it is diseases.19
Infant case w/failure to syndrome.29 higher risk for kidney &/ men. Delayed or slow pain, anorexia, diarrhea, flares.40,41 spleen, some w/an w/enlarged spleen. multi-organ failure in 2+ mune diseases that may diarrhea, enterocolitis, pain, diarrhea, failure to noted in the liver.73,74
spleen, other GI issues.78 & diarrhea w/flares.1,9,11 common.16 transient.18,53 thrive, diarrhea.63 or liver issues.34,35,36 growth.26,27 (may be bloody).43 enlarged liver.46 Renal disease is rare.44 months if untreated.49 involve other organs.65 or ulcerative colitis.67,68 thrive. Hypogonadism.69,70
LYMPHATIC Not noted.1 Rarely noted.1 Some pts. with enlarged
liver and/or spleen,
<20% w/lymphoma, IgM Enlarged spleen is
myeloma, or Walden- common, some have
Enlarged spleen is
common; some have
Enlarged cervical lymph Enlarged spleen, &/or
nodes w/flares.1 Few lymph nodes are
Enlarged liver and/or
spleen is common.
Neonates: enlarged liver Some cases of ANCA+ Risk for renal and liver
& neutropenia; anemia is Vasculitis that can affect impairment & systemic
Not seen.23, 24 Not noted.29,30,31 Enlarged liver &/or
spleen, enlarged lymph
Some patients with
adenopathy.39
Enlarged liver, with Some w/enlarged liver
elevated liver enzymes; &/or spleen; enlarged
Cervical adenopathy
during flares.40,41
Many w/generalized Lymphadenopathy is
lymphadenopathy. Some common. Many
Lymphoma. Hemophago-
cytosis–spleen/lymph
Not noted. Some need
IVIG for low immuno-
Not noted.67,68 Lymphadenopathy.
Rosai-Dorfman sinus
Not noted.73,74
many have enlarged ströms. >45% w/enlarged enlarged lymph nodes.1 enlarged lymph nodes.1 w/enlarged spleen.78 common.1,11 Risk of organ failure if common–can be severe.18 the kidneys.19 infection w/severe nodes.34,35,36 enlarged lymph nodes.26,27 lymph nodes.43 w/mesenteric adenitis.45,46 w/enlarged liver &/or nodes. Enlarged liver &/ globulins & frequent histiocytosis w/massive
lymph nodes.1 lymph nodes.13 untreated.16 flares.58,61 spleen.44 or spleen.49 infections. Few w/CVID.65 lymphadenopathy.69,70,71
JOINTS/BONES Arthralgias, stiffness &
swelling with flares.1
Arthralgias, recurrent
arthritis, stiffness &
Joint pain, knee valgus
or varus. Some w/frontal
80% have muscle, bone
&/or joint pain; arthri-
Mono/Polyarthritis,
oligoarthritis & clubbing
Intermittent or chronic
arthritis in large joints
Arthralgias common,
symmetric polyarthritis
Congenital defects are
often noted: micro-
Joint swelling, severe
bone pain. Bone biopsy
Periarticular tender soft
tissue swelling. Bone
Joint swelling, limp, Muscle weakness during
severe bone pain over af- fevers & flares. Risk for
Intermittent joint pain,
psoriatic arthritis. 30%
Episodic inflamma-
tory arthritis, often to
Symmetrical chronic
polyarthritis or oligoar-
Myalgia, arthralgia, fa-
tigue & malaise w/flares.
Joint Contractures,
muscle atrophy, pan-
45% have arthralgias
&/or arthritis–often the
Arthralgias, fatigue and
malaise. No permanent
Arthralgias may come
before the arthritis. 88%
Myalgias, arthralgias &/
or arthritis are common.
Hemophagocytosis in the
bone marrow. Delayed
Not noted.64,65
Some have concurrent
Not noted.67,68 Short stature. Arthralgias. Not noted.73,74
Dysmorphic facial
MUSCLES & swelling with flares.1 bossing, saddleback tis. Bone pain is most are common. Ankle w/muscle pain & swell- frequently noted.1 cephaly, dolichocephaly, shows no infection. biopsy shows no infec- fected bones (mostly long inflammatory arthritis.59,61 of affected patients in one joint at a time that thritis of the wrists, Permanent bone or joint niculitis induced knees &/or ankles, but joint or bone issues have polyarticular or Wrist changes after 6 closure of the bones of autoimmune diseases features: Triangular face,
nose, contractures, common in the iliac arthralgias are common. ing.1 wide irregular fontanels, Common: Balloon-like tion. Early-onset Chronic bones). 2-18 bone lesions one European family w/ doesn’t resolve on it’s knees, ankles w/ a boggy damage not noted.39 lipodystrophy, myositis, other joints can be noted, and patients are oligoarticular arthritis, months. 41% develop the skull in infants, bulg- that may involve the rotated ears, macrocrania,
CARTILAGE clubbing.1 <50% of and tibia. <40% have Severe arthritis of the low set and posteriorly widening of the ante- Recurrent Multifocal are commonly found. PSORS2 also had psori- own. Intermittent sterile appearance is usually fatigue and malaise. affected. May be the first symptom-free between most often in the wrists, intercarpal and carpo- ing fontanel often noted. joints, such as inflamma- exophtalmia. Pectus exca-
patients knees have bone lesions. Some w/ hip or ankle is rare.1 rotated ears, downslant- rior rib ends, periosteal Osteomyelitis (CRMO), Earlier age of onset & atic arthritis.24 pauciarticular, peripher- caused by an exuberant Inflammed nose & ear sign of Behçets. X ray is PFAPA flares.40,41 knees, &/or ankles. metacarpal joint space Neck stiffness, abnormal tory arthritis or undif- vatum, wide-set nipples,
bony overgrowth. Short osteocondensation & ed palpebral fissures. elevation along multiple periarticular tender soft many bone lesions=more al erosive arthritis. Joint tenosynovitis.34,35,36 cartilage (chondritis). normal but synovium of- Some w/cervical spine, narrowing a few yrs. muscle tone, impaired ferenciated connective widened ribs, long bone
stature, growth delays sclerotic bone mar- Hypotonia, myopathy, long bones, multifocal tissue swelling, short severe disease. Bone damage & destruction Growth delays–low ten has high neutrophils hip, temporomandibular after onset of AOSD–25% muscle coordination, tissue diseases.65 changes, short, square
failure to thrive, arthritis, row involvement in the & failure to thrive are osteolytic lesions. Other stature, delayed bone biopsy/cultures show no can often develop from height & weight.26,27 or mononuclear cells & joint arthritis or synovial then develop pericapitate paralysis.48,49 hands, sacrococcygal
& osteopenia noted.1,26 legs.13 common.11 bones affected.16 age, contractures.18 infection. 19,22 the arthritis.29,30,31,32,55 a vasculitis process.43 cysts.45,46 ankylosis.44 dimple, contractures.69,70
VASCULITIS Not noted.1 Not noted.1 Vasculitis rarely
develops.1
Vasculitis noted in 20%
of patients.13
HSP, polyarteritis
nodosa.1
HSP, lymphocytic
vasculitis.1
Cutaneous vasculitis
common, HSP is rare.1
Not noted.11 A few w/localized or
cerebral vasculitis.16
Not noted.18,53 Some w/Takayasu arteri- Not noted.59,60
tis, or ANCA+ Vasculitis.54
Not seen.23, 24 Not noted.29 Some w/vasculitis, leuko- Not noted.38,39
cytoclastic vasculitis.34
Not noted.26,27 Extensive vasculits. 30% Not noted.40,41
w/venous thrombosis.43
Not noted.45,46 Not noted.44 Not noted.47,48,49 Not noted.64,65 Not noted.67,68 Not noted. Some w/vari- Diffuse vasculopathy in
cose veins on legs.69 the skin, liver & brain.73,74
AMYLOIDOSIS Elevated serum amy-
loid (SAA). Secondary
Elevated SAA.
>25 % w/secondary
Elevated SAA. Second-
ary amyloidosis in <2%
A few patients have
developed secondary
Common >50% in
untreated patients, it
10-20% occurrence–
higher risk w/cysteine
<5-10%–uncommon.9 Not noted-unknown.9,11 Not noted.15,16,17 Not noted.18,53 Not noted.19,22 ,54 Not noted.59,60 Not noted.23, 24 Not noted.29 Not noted.34 Not noted.39 Not noted.26,27 Not noted.42,43 Not noted.40,41 Amyloidosis occurs in
7.4% of pts. in the USA,
Very rare.44 Not noted.47,48,49 Not noted.64,65 Not noted.67,68 Not noted.69,70,71,72 Not noted.73,74
amyloidosis in some amyloidosis.1,9 pts.1,6 amyloidosis.13 depends on genotype.9 mutation.9 and 16% in Turkey.46
patients.1,9
ABNORMAL High: ESR, CRP, SAA.
Leukocytosis with
High: ESR, CRP, SAA.
Leukocytosis,with
Chronically high: ESR,
CRP, SAA, anemia,
Monoclonal IgM &/or
IgG gammopathy. High:
High: ESR, CRP, SAA
between flares.
High: ESR, CRP, SAA.
Elevated PMNs,
High: ESR, CRP, SAA
w/flares. High IgD w/IgA
Anemia, leukocytosis, High: ESR, CRP, leukocy-
thrombocytopenia. High: tosis, chronic anemia.16,56
Congenital dyserythro-
poietic anemia (CDA).
Whole body MRI can
reveal multifocal bone
High during flares (most
pts.): ESR, CRP, neu-
Mildly elevated WBC,
CRP & ESR rarely
Cultures of bone & skin
are negative. Purulent
High CRP & ESR, ACE,
immunoglobulins.
Elevated CRP may be
noted during flares. But
Hypochromic or normo-
cytic anemia. High CRP,
Leukocytosis common.
Normal–rarely elevated
High: ESR, CRP, WBC
during flares–normal
High: ESR, CRP, WBC,
SAA, ferritin, aldolase.
High: ESR, CRP, LFTs,
ferritin. Low glycosy-
High: ESR, CRP, triglycer-
ides, LFTs, soluble CD25,
High IgE. Low serum IgA,
IgG, IgM. Decreased cir-
Low circulating IgA, IgM
antibodies, decreased
Chronically elevated,
but increase during
High: CRP, ESR w/flares.
Cytopenia. Blood: 10-fold
LABS flares.1 flares.1 granulocyte ESR, CRP. Leukocytosis. Fibrinogen, Leukocyto- polyclonal gammopathy, in 80% pts. Mevalonate ESR, CRP, SAA, CK, IgD, High ESR. WBC can be lesions.20 Normal or trophils, lactate levels, elevated–only during synovial fluid full of neu- Anemia, leukopenia, some pts. do not have ESR, triglycerides. Some ESR or CRP. Some cryo- levels when not flar- Elevated LFT’s. Leuko- lated ferritin. Leukocy- ferritin. Low: platelets, culating CD19+ B cells, class-switched memory flares: CRP, ESR, WBC. decrease in ADA2. Low
leukocytosis.1,6 Complement normal to sis present with flares.1 leukocytosis.1 aciduria noted during IgA. IgE; chronically high normal, or elevated– elevated WBC, ESR, Low: plasma albumin, flares of symptoms.56 trophils. High w/flares: eosinophilia, hematu- elevated CRP w/ flares.39 w/elevated platelets, globulinemia, elevated ing.40,41 cytosis, thrombocytosis tosis, anemia common fibrinogen. Low NK cell IgG+ & IgA+ memory B cells & NK T cells. High during flares: IgG, ADA2-specific adenosine
elevated. 50% w/inflam- flares.1 Mevalonate aciduria.1,11 neutropenia in infancy. CRP.19,22,54 calcium, zinc. Risk for CRP, ESR, WBC.29,30,32 ria, proteinuria, pyuria, TSH, &/or LDL.26,27 factor VIII, fibrinolysis.43 Anemia.45,46 w/flares. Prolonged PTT cytotoxic function, B cells, NK cells. >60% ANA negative.67,68 Ig A. Pts. can become deaminase activity: blood
matory anemia.13 Cultures negative.18 infections w/flares.59,60 abnormal LFTs (LF).34,36 (DIC risk.)44 neutropenia, anemia.49 +ANA. WBC normal.64,65 very anemic.69,70,71,72 & CD14+ monocytes.73,74
The rash can vary in size, The CAPS rash is often NOMID pt. w/rash, frontal Schnitzler syndrome: Urti- FMF: Erysipelas-like erythe- TRAPS rash on the chest HIDS: Maculopapular rash MA: 21 month old pt. w/ DIRA: Generalized pustulo- Sweet’s Syndrome is often Palmar pustulosis SAPHO 3 yr. old w/generalized Pustular psoriasis–seen w/ PAPA: Pyoderma gangreno- Blau syndrome: Reddish- Urticarial rash w/flares CANDLE: Child w/facial lip- Behçet’s Disease: Oral PFAPA: Aphthous stomatitis. soJIA: Salmon-pink rash AOSD: Salmon trunk erup- Generalized purpuric ma- Cold-induced urticarial APLAID vesiculopustular Pt. w/hyperpigmentation. Livedo reticularis type rash
& intensity in all forms of more pronounced during bossing, & saddleback carial skin rash on the arm. ma around the ankle. (Arthritis of a child. (Swiss Med Wkly. on the hand. (cri-net.com Auto facial dysmorphism. (Orphanet sis. (NOMID Alliance pt. image) present w/Majeed. (pbase. (CRMO). (cri-net.com SAPHO Syn- pustular psoriasis. (dermis.net/ CAMPS. (dermatlas.med.jhmi.edu/ sum. (dermatlas.med.jhmi.edu/image/ brown papules. (Dermatology after cold exposure. odystrophy, rash & swollen ulcers. (dermis.net/dermisroot/ (drpaulose.com; blog.timesunion.com/ on abdomen. (Joint Bone Spine, tion on a young adult pt. cules in Familial HLH. (Arch rash. (NOMID Alliance pt. image) rash. (sciencedirect.com/science/ (onlinelibrary.wiley.com/doi/10.1111/ is seen on DADA2 pts.
CAPS. (NOMID Alliance pt. image) flares. (NOMID Alliance pt. image) nose. (NOMID Alliance pt. image) (cri-net.com Schnitzler image 6) Research & Therapy 2009 11:212) 2012;142:w13602) Inflammatory Diseases image 23) Journal of Rare Diseases 2006 1:13) com/leobarco/image/69914524) drome image 29: Spondylarthropathies) dermisroot/en/32493/image.htm) image/pustular_psoriasis_1_061124) pyoderma_gangrenosum_1_020918) Online Journal 15 (12): 5) (NOMID Alliance pt. image) lips. (NOMID Alliance pt. image) en/17101/image.htm Behçet’s disease) mdtobe Mystery Monday 125) Volume 74, Issue 5, Pages 500-503) (cri-net.com AOSD image 1) Dermatol. 2002;138(9):1208-1212) article/pii/S0002929712004181) pde.12085/full#pde12085-fig-0001)
Main authors: Karen Durrant RN, BSN–President of The NOMID Alliance, & Dr Juan Ignacio Aróstegui MD–Immunologist at the CDB Hospital Clínic in Barcelona, Spain & Director of La Unidad de Enfermedades Autoinflamatorias (autoinflamatorias.com) List of abbreviations: All Cited References & Full Image Credits are Listed on the Back Side The NOMID Alliance is a 501(c)(3) non-profit
Acknowledgements: A special thanks to the many medical doctors who have helped to make voluntary suggestions in regards to this reference chart: Dr Juan Ignacio Aróstegui, Dr Hal Hoffman, Dr Raphaela Goldbach-Mansky, Dr Anna Simon, Dr Polly Ferguson, Dr Rebecca Marsh, Dr Daniel Kastner, Dr Luca Cantarini, Dr Véronique Hentgen, Dr Nico M. Wulffraat, Dr Kieron ACE: Angiotensin-converting enzyme (lab test) CRP: C-reactive protein (lab test); NK cells: Natural killer cells of this Chart. organization dedicated to improving aware-
Leslie & Dr Lori Broderick. Thank you Nathan Durrant for donating your graphic design services. Our deepest thanks to The NOMID Alliance Board of Directors, & to all the patients & families who have supplied images for this chart, & support for The NOMID Alliance. You are our greatest inspiration and strength! A special thanks to all of the doctors from the International ADA2: Adenosine deaminase 2 DIC: Disseminated intravascular coagulation PMNs: Polymorphonuclear leukocytes (on lab tests w/ WBC count) ness, care and treatment for patients with
ESR: Erythrocyte sedimentation rate (lab test); Westergren ESR pt.: abbreviation for the word “patient” This chart is an educational reference to increase awareness about CAPS or other autoinflammatory diseases.
Society of Systemic Auto-Inflammatory Diseases (ISSAID) for their research & dedication to patients with autoinflammatory diseases, plus the opportunity to present this chart in a poster session at the Autoinflammation 2013 Congress. Thanks for the inspiration for this chart also go to: The Translational Autoinflammatory Disease Section at the National Institute of Arthritis ANCA+ Vasculitis: Granulomatosis w/polyangiitis (GPA); Wegener’s
GI: Gastrointestinal (organs in the abdomen) PTT: Partial thromboplastin time (lab test) autoinflammatory diseases.
and Musculoskeletal and Skin Diseases (NIAMS) & The National Human Genome Research Institute at the National Institutes of Health (NIH); The Spanish Society of Pediatric Rheumatology (SERPE) & La Unidad de Enfermedades Autoinflamatorias; The French Centre de Référence des Maladies Auto-inflammatoires (CeRéMAI) & Le Club Rhumatismes et Inflamations; Der- ARDS: Acute Respiratory Distress Syndrome
P.O. Box 590354
matology Online Atlas. (DermIS Dermatology Information System), the Pediatric Rheumatology European Society (PReS), PRINTO, the EUROFEVER Project, EULAR, CARRA & the many other research centers and doctors around the world. Thanks to The American College of Rheumatology (ACR) for their efforts & for our non-profit rate booth at ACR 2013 Annual Meeting. CD14+ monocytes: Cluster of differentiation 14 positive monocytes HSP: Henoch–Schönlein purpura, anaphylactoid purpura SAA: Serum amyloid A protein (lab test) This document is not intended to replace professional medical care, diag- San Francisco, CA 94159
CD19: B-lymphocyte antigen CD19-aka Cluster of Differentiation 19 ICP: Intracranial pressure TSH: Thyroid-stimulating hormone (lab test); thyrotropin nosis and/or treatment by a qualified specialist. It is to be used only for 1-415-831-8782
Disclosure: All of the doctors involved in the authorship, review, editing and creation of this chart voluntarily donated their help for this educational reference, & received no financial compensation. Novartis Pharmaceuticals Canada Inc. provided The NOMID Alliance with an unrestricted grant in 2012 to help with the initial development & printing costs for this chart. A CD25: Soluble interleukin-2-receptor IDDM: Insulin-Dependent Diabetes Mellitus w/: abbreviation for the word “with” non-commercial, educational purposes. © 2013 The NOMID Alliance. karen.nomidalliance.org@gmail.com
generous unrestricted grant from Swedish Orphan Biovitrum AB (Sobi) in 2013 is currently supporting many projects, including: the printing of this chart for the ACR meeting, patient picnics in 2014, & an educational grant for our injection tips guide for families, and some other projects that will be developed in 2014. The NOMID Alliance has received a number of unrestricted CNS: Central Nervous System (involving the brain, spinal cord) LFTs: Liver function tests (lab test): AST, ALT, GGT, ALK Phos, Bilirubin WBC: White Blood Count (lab test)
grants at various times from Regeneron, Novartis & Sobi for grant-specific projects. Karen Durrant has received reimbursement for out-of-pocket travel costs from SOBI to attend a few meetings as a patient representative, but has received no personal financial compensation from any pharmaceutical company.
*These noted diseases are also referred to as “Classic” Hereditary Periodic Fever Syndromes (CAPS, FMF, HIDS, & TRAPS)
You might also like
- USMLE Step I Boards BuzzwordsDocument11 pagesUSMLE Step I Boards BuzzwordsnisreenNo ratings yet
- Anemia Hemolítica Autoinmune NEJMDocument13 pagesAnemia Hemolítica Autoinmune NEJMSMIBA Medicina100% (1)
- Bhalani 4Document86 pagesBhalani 4Vanessa Cavill100% (2)
- The Ischemic ElectrocardiogramDocument16 pagesThe Ischemic ElectrocardiogramAdiel OjedaNo ratings yet
- Immunology & Serology Review Notes George Vincent Gellena, RMT, Mls (Ascpi)Document9 pagesImmunology & Serology Review Notes George Vincent Gellena, RMT, Mls (Ascpi)Angelo Jude CobachaNo ratings yet
- Adult Infectious Diseases Over 200 Case Studies: Intended For: Medical Students, Ambulists, Hospitalists, Nurse Practitioners, Physician AssistantsFrom EverandAdult Infectious Diseases Over 200 Case Studies: Intended For: Medical Students, Ambulists, Hospitalists, Nurse Practitioners, Physician AssistantsRating: 4.5 out of 5 stars4.5/5 (7)
- Hiper IgD Syndrome (HIDS) Clinical and Genetic Features in Five PatientsDocument1 pageHiper IgD Syndrome (HIDS) Clinical and Genetic Features in Five PatientsDavids MarinNo ratings yet
- Kuruvilla2018 FiziopatDocument15 pagesKuruvilla2018 FiziopatFilip BanarescuNo ratings yet
- Group A StrepDocument2 pagesGroup A Strepspinedr07No ratings yet
- Guillain Barre Syndrome A ReviewDocument7 pagesGuillain Barre Syndrome A ReviewEditor IJTSRDNo ratings yet
- @acute Nephritic SyndromeDocument3 pages@acute Nephritic SyndromeMazlia FarzanaNo ratings yet
- Gems Opt Select Brochure 2021 v6 3Document2 pagesGems Opt Select Brochure 2021 v6 3Bongani West VuthaNo ratings yet
- Hyperpitutiarism & Pituitary Adenmoas: Pathogenesis MorphologyDocument2 pagesHyperpitutiarism & Pituitary Adenmoas: Pathogenesis MorphologyEna PaparićNo ratings yet
- Supervisor: Prof. Dr. Atan Baas Sinuhaji, Spa (K)Document35 pagesSupervisor: Prof. Dr. Atan Baas Sinuhaji, Spa (K)Ranap HadiyantoNo ratings yet
- Novel Treatments Paradigms: Membranous Nephropathy: Table 1Document13 pagesNovel Treatments Paradigms: Membranous Nephropathy: Table 1Jhair Murillo AparicioNo ratings yet
- Disease Cheat SheetDocument393 pagesDisease Cheat Sheetsurviving nursing school50% (2)
- Hydro CortisoneDocument3 pagesHydro Cortisonepaninay17No ratings yet
- How Common Infections Affect The Brain in Health and DiseaseDocument35 pagesHow Common Infections Affect The Brain in Health and DiseaseonthewightNo ratings yet
- Sindrome de Fiebre PeriodicaDocument10 pagesSindrome de Fiebre PeriodicaHakundusNo ratings yet
- Immuno SemisDocument8 pagesImmuno SemisFait HeeNo ratings yet
- Genome Poster 2009Document1 pageGenome Poster 2009ISAAC LEWNo ratings yet
- Pointers For Medically Important BacteriaDocument2 pagesPointers For Medically Important BacteriamerryNo ratings yet
- Sample Rezi Cu BrioDocument10 pagesSample Rezi Cu BrioMihai BurdujaNo ratings yet
- Lameness, ShoatsDocument35 pagesLameness, Shoatskennyrogers kawooyaNo ratings yet
- PLASMODIUMDocument5 pagesPLASMODIUMGhina RizwanNo ratings yet
- An Assignment On Autoimmunity: July 2012Document15 pagesAn Assignment On Autoimmunity: July 2012SudhakarNo ratings yet
- Asthma Drug StudyDocument2 pagesAsthma Drug StudySheril Sularte CasanesNo ratings yet
- Immuno-Sero Semi-Finals Immunoproliferative Disorders Multiple MyelomaDocument2 pagesImmuno-Sero Semi-Finals Immunoproliferative Disorders Multiple MyelomaFait HeeNo ratings yet
- DexamethasoneDocument3 pagesDexamethasoneGwyn RosalesNo ratings yet
- Trypanosoma-SppDocument4 pagesTrypanosoma-SppVE NI CENo ratings yet
- Case 10Document6 pagesCase 10Bhargav GohelNo ratings yet
- 4 Heredodegenerative DiseasesDocument10 pages4 Heredodegenerative DiseasesVan John MagallanesNo ratings yet
- Taxonomy: Family StaphylococcaceaeDocument40 pagesTaxonomy: Family StaphylococcaceaeMarissa Terrado SorianoNo ratings yet
- Biochemistry of AgingDocument2 pagesBiochemistry of AgingKaedehara KazuhaNo ratings yet
- Hypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesDocument1 pageHypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesmcwnotesNo ratings yet
- Parasites High YoieldDocument4 pagesParasites High Yoieldnreena aslamNo ratings yet
- Immuno-Sero Semi-Finals Immunoproliferative Disorders Multiple MyelomaDocument5 pagesImmuno-Sero Semi-Finals Immunoproliferative Disorders Multiple MyelomaFait HeeNo ratings yet
- Glomerular Disease and DiureticsDocument26 pagesGlomerular Disease and DiureticsDapot SianiparNo ratings yet
- Module 6.5 MycologyDocument4 pagesModule 6.5 MycologyPNo ratings yet
- Draft TPIDocument20 pagesDraft TPIElias VermNo ratings yet
- PW Lab 3Document26 pagesPW Lab 3Diana CentaurusNo ratings yet
- Year Ii Pharmacology Drugs ListDocument21 pagesYear Ii Pharmacology Drugs ListsaifuddinNo ratings yet
- SEM 2 (ImmunoSero - Part1&2)Document8 pagesSEM 2 (ImmunoSero - Part1&2)DayNo ratings yet
- Autoimmune Diseases: Central ToleranceDocument8 pagesAutoimmune Diseases: Central ToleranceMaria MikaelaNo ratings yet
- Diseases For The BoardsDocument2 pagesDiseases For The BoardsBrendan MillinerNo ratings yet
- Community in Tables AllTalabaDocument14 pagesCommunity in Tables AllTalabaAhmed MansourNo ratings yet
- Communicable Disease Nursing Epidemiology: Parade of DiseasesDocument2 pagesCommunicable Disease Nursing Epidemiology: Parade of DiseasesFranz Patrick Legria, CPAC - SNNo ratings yet
- Drug Study: Name of Drugs Mechanism of Action Contraindications Side Effects Adverse Effects Nursing ResponsibilitiesDocument2 pagesDrug Study: Name of Drugs Mechanism of Action Contraindications Side Effects Adverse Effects Nursing ResponsibilitiesCarissa Mae Tapec EstradaNo ratings yet
- Cellulitis (Pathophysio)Document3 pagesCellulitis (Pathophysio)Erald PaderangaNo ratings yet
- Drug Induced Hemolytic AnemiaDocument1 pageDrug Induced Hemolytic AnemiaArnao Maria Mikaela EuniceNo ratings yet
- Myositis Autoantibodies and Clinical Phenotypes 2104Document7 pagesMyositis Autoantibodies and Clinical Phenotypes 2104Mario SuarezNo ratings yet
- Drug Mechanism Clincal Use Side Effects Antifungal: Amphote Ricin BDocument30 pagesDrug Mechanism Clincal Use Side Effects Antifungal: Amphote Ricin BCess Lagera Ybanez0% (1)
- Drug StudyDocument10 pagesDrug StudyNine SaguiboNo ratings yet
- Nephrotic Syndrome PDF 2Document2 pagesNephrotic Syndrome PDF 2MNo ratings yet
- Braun Falco 2012Document7 pagesBraun Falco 2012Alexandra OpreaNo ratings yet
- Disease Signs and Symptoms Deficiency/Problem Notes AmyloidosisDocument14 pagesDisease Signs and Symptoms Deficiency/Problem Notes AmyloidosisSriKavya DevineniNo ratings yet
- Drug Sheet 2Document88 pagesDrug Sheet 2Umbe ChinakaNo ratings yet
- 2010 Pharmacologic Agents For Pediatric Neuroimmune DisordersDocument9 pages2010 Pharmacologic Agents For Pediatric Neuroimmune DisordersamallullaNo ratings yet
- Organism Description Drug of ChoiceDocument14 pagesOrganism Description Drug of ChoiceMary YongcoNo ratings yet
- AAD BF Inborn Errors of MetabolismDocument2 pagesAAD BF Inborn Errors of Metabolismkahkashanahmed065No ratings yet
- Non-inflammatory immunology: An introduction to the immune system and its pathologiesFrom EverandNon-inflammatory immunology: An introduction to the immune system and its pathologiesNo ratings yet
- Pediatric Immunology: A Case-Based Collection with MCQs, Volume 2From EverandPediatric Immunology: A Case-Based Collection with MCQs, Volume 2No ratings yet
- MD Anderson Handbook 2018Document197 pagesMD Anderson Handbook 2018Brent AllieNo ratings yet
- ORS + Anti DiarrhealsDocument25 pagesORS + Anti DiarrhealsThihansa GeminiNo ratings yet
- A Multilevel Primare CareDocument11 pagesA Multilevel Primare CareJaime BusquetNo ratings yet
- KA VaccinationDocument9 pagesKA VaccinationVictor GaborNo ratings yet
- Jurnal Biji AlpukatDocument16 pagesJurnal Biji AlpukatnaniNo ratings yet
- Health6 - q3 - Mod1 - Diseases and Disorders Caused by Poor Environmental Sanitation - v3Document17 pagesHealth6 - q3 - Mod1 - Diseases and Disorders Caused by Poor Environmental Sanitation - v3Aira Galang100% (1)
- Most Common Ophthalmic Diagnoses in Eye Emergency Departments: A Multicenter StudyDocument8 pagesMost Common Ophthalmic Diagnoses in Eye Emergency Departments: A Multicenter StudyAlba García MarcoNo ratings yet
- Understanding Homicide Causes Types and PreventionDocument1 pageUnderstanding Homicide Causes Types and PreventiondivyaNo ratings yet
- Surgery of The SkinDocument66 pagesSurgery of The SkinJess PeltraNo ratings yet
- Jurnal Diabetes (Nusdin)Document4 pagesJurnal Diabetes (Nusdin)nusdin fachriNo ratings yet
- Hepatitis B VaccineDocument3 pagesHepatitis B VaccineChoox PriiNo ratings yet
- Health Threats CHN G2Document28 pagesHealth Threats CHN G2Chriss Una PacamalanNo ratings yet
- 01 Hypertension 2023Document71 pages01 Hypertension 2023salnaimat7No ratings yet
- DownloadDocument10 pagesDownloadmandapatiNo ratings yet
- Psychiatric Mental Health Comprehensive Case StudyDocument12 pagesPsychiatric Mental Health Comprehensive Case Studyapi-662890978No ratings yet
- Peoria County Booking Sheet 03/07/14Document9 pagesPeoria County Booking Sheet 03/07/14Journal Star police documentsNo ratings yet
- HemoperitoneumDocument36 pagesHemoperitoneumnovitafitri123No ratings yet
- Cancer: Kendriya Vidyalaya AruvankaduDocument20 pagesCancer: Kendriya Vidyalaya AruvankaduGáMÍNG WÍTH ÁBHÍ GaMÍNG CHÁNNÉLNo ratings yet
- The Diabetes Handbook by DK - Parte3Document20 pagesThe Diabetes Handbook by DK - Parte3CarlosPutnamNo ratings yet
- Prime Centric Therapy Clinic: Special Topic Report March 23, 2023 I. Cerebrovascular Accident (CVA) II. ReferencesDocument19 pagesPrime Centric Therapy Clinic: Special Topic Report March 23, 2023 I. Cerebrovascular Accident (CVA) II. ReferencesKRYSTEL CAMILLE ESCANONo ratings yet
- Preprint Not Peer Reviewed: COVID-19 and Lockdown: A Study On The Impact On Mental HealthDocument13 pagesPreprint Not Peer Reviewed: COVID-19 and Lockdown: A Study On The Impact On Mental HealthloloasbNo ratings yet
- Quiz 5 NDocument16 pagesQuiz 5 NabezareljvenNo ratings yet
- SP CDQ PDFDocument3 pagesSP CDQ PDFsx rxNo ratings yet
- ABC - First Aid ManualDocument65 pagesABC - First Aid ManualDitend TeshNo ratings yet
- Parrish September 16Document9 pagesParrish September 16rohitNo ratings yet
- Blood Transfusion ReactionsDocument51 pagesBlood Transfusion ReactionsIgwe SolomonNo ratings yet
- School of Health and Allied Health Sciences Nursing DepartmentDocument5 pagesSchool of Health and Allied Health Sciences Nursing DepartmentAriadnejenn Pepito BerameNo ratings yet
- NCMB317 Lec MidtermDocument55 pagesNCMB317 Lec Midterm2 - GUEVARRA, KYLE JOSHUA M.No ratings yet