Professional Documents
Culture Documents
Journal Pone 0284911
Journal Pone 0284911
Uploaded by
SIVAMATHIVANAN P 22MTL129Copyright:
Available Formats
You might also like
- CHCECE030 - Student Assessment Task 1 - QuestioningDocument16 pagesCHCECE030 - Student Assessment Task 1 - QuestioningIlhami Nur Rahmat50% (2)
- 3.02 Groundwater Lab ReportDocument2 pages3.02 Groundwater Lab Reportisland67% (3)
- User Manual Infusion Pump S100-200-300Document79 pagesUser Manual Infusion Pump S100-200-300Nicolae Arpentii100% (1)
- Scientific Principles of Strength TrainingDocument38 pagesScientific Principles of Strength Trainingarkko5585% (13)
- Sketchy Pharm (Benzo) ReviewDocument2 pagesSketchy Pharm (Benzo) ReviewMitz JuneNo ratings yet
- Methodology of Surface Electromyography in Gait Analysis: Review of The LiteratureDocument8 pagesMethodology of Surface Electromyography in Gait Analysis: Review of The LiteraturemaketoNo ratings yet
- Urtnasan2018 Article AutomatedDetectionOfObstructivDocument8 pagesUrtnasan2018 Article AutomatedDetectionOfObstructivRayana VieiraNo ratings yet
- HINT - High Level Inferencing Tool: An Expert System For The Interpretation of Neurophysiological StudiesDocument18 pagesHINT - High Level Inferencing Tool: An Expert System For The Interpretation of Neurophysiological StudiesRama BayuNo ratings yet
- TIM.2020 A Sleep Apnea Detection Method Based On Unsupervised Feature Learning and Single-Lead ElectrocardiogramDocument12 pagesTIM.2020 A Sleep Apnea Detection Method Based On Unsupervised Feature Learning and Single-Lead ElectrocardiogramYasrub SiddiquiNo ratings yet
- A Long Short-Term Memory Ensemble Approach For Improving The Output Prediction in ICUDocument11 pagesA Long Short-Term Memory Ensemble Approach For Improving The Output Prediction in ICUIdris RabiuNo ratings yet
- Automatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDocument15 pagesAutomatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDayana VieiraNo ratings yet
- 2019 - Ers - Ai LFTDocument11 pages2019 - Ers - Ai LFTJohn BlackbNo ratings yet
- Aittokallio, Virkki, Polo - 2009 - Understanding Sleep-Disordered Breathing Through Mathematical ModellingDocument11 pagesAittokallio, Virkki, Polo - 2009 - Understanding Sleep-Disordered Breathing Through Mathematical ModellingFGR2711No ratings yet
- Automatic Home-Based Screening of Obstructive Sleep Apnea Using Single Channel Electrocardiogram and Spo2 SignalsDocument17 pagesAutomatic Home-Based Screening of Obstructive Sleep Apnea Using Single Channel Electrocardiogram and Spo2 SignalsAdam HansenNo ratings yet
- Fmed 10 1174631Document7 pagesFmed 10 1174631Natansa Adi SukmaNo ratings yet
- Research Paper 2017-3Document11 pagesResearch Paper 2017-3Vikas KaushikNo ratings yet
- Casale Chi 2019Document10 pagesCasale Chi 2019Ketlin CastroNo ratings yet
- Autonomic Effects of Spinal Manipulative Therapie Systematic ReviewDocument12 pagesAutonomic Effects of Spinal Manipulative Therapie Systematic ReviewbesombespierreNo ratings yet
- Bio Marcadores en Sarcopenia Calvani2017Document6 pagesBio Marcadores en Sarcopenia Calvani2017JAVIER VELASQUEZ100% (1)
- 3413ijcsa05 PDFDocument13 pages3413ijcsa05 PDFVanathi AndiranNo ratings yet
- Neurofilaments in Progressive Multiple Sclerosis: A Systematic ReviewDocument11 pagesNeurofilaments in Progressive Multiple Sclerosis: A Systematic ReviewAlin CiubotaruNo ratings yet
- The Classification of EEG-based Winking Signals: A Transfer Learning and Random Forest ApproachDocument7 pagesThe Classification of EEG-based Winking Signals: A Transfer Learning and Random Forest ApproachDhruv TNo ratings yet
- Lung Function Parameters of Healthy, Non-Smoking Young People and Employees at Shaqra University, ShaqraDocument6 pagesLung Function Parameters of Healthy, Non-Smoking Young People and Employees at Shaqra University, ShaqrahimayatullahNo ratings yet
- Driver Drowsiness Classification Using Fuzzy Wavelet-Packet-Based Feature-Extraction AlgorithmDocument11 pagesDriver Drowsiness Classification Using Fuzzy Wavelet-Packet-Based Feature-Extraction AlgorithmAlex WongNo ratings yet
- Final SynopsisDocument15 pagesFinal SynopsisgauravchauNo ratings yet
- Ppaer 1Document5 pagesPpaer 1Piyash ApexNo ratings yet
- 10 1002@jcp 28839Document11 pages10 1002@jcp 28839Ahmed SaifNo ratings yet
- Ann ArticleDocument12 pagesAnn ArticleSABARISH VNo ratings yet
- Review Article: Magnetoencephalography: Fundamentals and Established and Emerging Clinical Applications in RadiologyDocument19 pagesReview Article: Magnetoencephalography: Fundamentals and Established and Emerging Clinical Applications in RadiologyThe StreetNo ratings yet
- New Seep Apnea AIDocument15 pagesNew Seep Apnea AIgauravchauNo ratings yet
- Applied Sciences: Special Issue: "Research On Biomedical Signal Processing"Document3 pagesApplied Sciences: Special Issue: "Research On Biomedical Signal Processing"prabhatNo ratings yet
- ERS Statement On Standardisation of Cardiopulmonary Exercise Testing in Chronic Lung DiseasesDocument25 pagesERS Statement On Standardisation of Cardiopulmonary Exercise Testing in Chronic Lung Diseasesnatalia cunha varellaNo ratings yet
- Predicción Longitudinal de La Aptitud Cardiorrespiratoria A Través de Dispositivos Portátiles en Entornos de Vida LibreDocument11 pagesPredicción Longitudinal de La Aptitud Cardiorrespiratoria A Través de Dispositivos Portátiles en Entornos de Vida Libremariojosehurtado3955No ratings yet
- 3 ArticleDocument59 pages3 ArticleAlbert PierssonNo ratings yet
- Osteoarthritis Year in Review 2014: Mechanics e Basic and Clinical Studies in OsteoarthritisDocument14 pagesOsteoarthritis Year in Review 2014: Mechanics e Basic and Clinical Studies in OsteoarthritisFrenkky AlexaNo ratings yet
- SV2021112102Document12 pagesSV2021112102pashaNo ratings yet
- 18iommodelpolicy TRDocument37 pages18iommodelpolicy TRkaysa3No ratings yet
- Whole Body Magnetic Resonance Imaging in InflammatDocument14 pagesWhole Body Magnetic Resonance Imaging in InflammateugeniaNo ratings yet
- UltrassonografiaDocument6 pagesUltrassonografiaLenir LuzNo ratings yet
- PE Como Predictores de Discapacidad en EM - 2012Document5 pagesPE Como Predictores de Discapacidad en EM - 20122j5f2y76g2No ratings yet
- Dario Farina, Luigi Fattorini, Francesco Felici and Giancarlo FilligoiDocument12 pagesDario Farina, Luigi Fattorini, Francesco Felici and Giancarlo FilligoiJen PassilanNo ratings yet
- Impact of Mild To Moderate Exacerbations On OutcomDocument4 pagesImpact of Mild To Moderate Exacerbations On OutcomlalopotNo ratings yet
- Effect of Action Observation Therapy inDocument33 pagesEffect of Action Observation Therapy inseroxat2005No ratings yet
- Detection of Borderline Mental Disorder On Electrocardiosignals Using EMDDocument4 pagesDetection of Borderline Mental Disorder On Electrocardiosignals Using EMDJohnsonNo ratings yet
- The Global Lung Function Initiative - Dispelling Some Myths of Lung Function Test InterpretationDocument13 pagesThe Global Lung Function Initiative - Dispelling Some Myths of Lung Function Test InterpretationUriel ChavarriaNo ratings yet
- JCM 11 03739 v2Document19 pagesJCM 11 03739 v2Edher Benitez PliegoNo ratings yet
- Ijms 13 13894Document17 pagesIjms 13 13894osama mosaNo ratings yet
- Sensors: Physiological Sensor Signals Classification For Healthcare Using Sensor Data Fusion and Case-Based ReasoningDocument16 pagesSensors: Physiological Sensor Signals Classification For Healthcare Using Sensor Data Fusion and Case-Based ReasoningbengheniaNo ratings yet
- Mann Assessment of Swallowing AbilityDocument9 pagesMann Assessment of Swallowing Abilityluca bastianiNo ratings yet
- 10.1007@s00405 016 4015 4Document10 pages10.1007@s00405 016 4015 4Lorena PaulaNo ratings yet
- Position Paper of The EACVI and EANM On Artificial Intelligence Applications in Multimodality Cardiovascular Imaging Using SPECTCT, PETCT, and Cardiac CTDocument15 pagesPosition Paper of The EACVI and EANM On Artificial Intelligence Applications in Multimodality Cardiovascular Imaging Using SPECTCT, PETCT, and Cardiac CTKotolNo ratings yet
- 1 s2.0 S1746809423006924 MainDocument11 pages1 s2.0 S1746809423006924 MainAshish NehraNo ratings yet
- 167 2016 Article 4272Document18 pages167 2016 Article 4272asmaNo ratings yet
- Eus 310Document9 pagesEus 310Fahreza CaesarioNo ratings yet
- Bioinformatics 2021 15Document7 pagesBioinformatics 2021 15AhdiatShinigamiNo ratings yet
- Pruebas de Función Pulmonar en Distrofia Muscular TiposDocument10 pagesPruebas de Función Pulmonar en Distrofia Muscular TiposEzeBorjesNo ratings yet
- Pamj 39 140Document20 pagesPamj 39 140Karen CruzNo ratings yet
- A Mettre Zotero 8Document9 pagesA Mettre Zotero 8Clara ScemamaNo ratings yet
- Ferrario 2006Document7 pagesFerrario 2006yenni anggrainiNo ratings yet
- Cattaneo 2019Document11 pagesCattaneo 2019Rolando Huaman BravoNo ratings yet
- Speech Based Parkinson's Disease Detection Using Machine LearningDocument7 pagesSpeech Based Parkinson's Disease Detection Using Machine LearningIJRASETPublicationsNo ratings yet
- Wearable Sensors For Clinical Applications in Epilepsy, Parkinson's Disease, and Stroke: A Mixed Methods Systematic ReviewDocument13 pagesWearable Sensors For Clinical Applications in Epilepsy, Parkinson's Disease, and Stroke: A Mixed Methods Systematic ReviewMANIMEGALAI M. ECENo ratings yet
- Computer Methods and Programs in Biomedicine: Reza Boostani, Foroozan Karimzadeh, Mohammad NamiDocument15 pagesComputer Methods and Programs in Biomedicine: Reza Boostani, Foroozan Karimzadeh, Mohammad NamiAlanCarrilloNo ratings yet
- Electroestimulacion Funcional INGLESDocument9 pagesElectroestimulacion Funcional INGLESLeticia RiveraNo ratings yet
- 2023 EAACI - Guidelines - Diagnosis - IgE-mediated - Food - AllergyDocument56 pages2023 EAACI - Guidelines - Diagnosis - IgE-mediated - Food - AllergyOlga CîrsteaNo ratings yet
- Urologic ExaminationDocument4 pagesUrologic ExaminationTansanee MalivalayaNo ratings yet
- Sim Tanwar IccDocument1 pageSim Tanwar IccManoj MauryaNo ratings yet
- Deep Breathing Exercises: Procedure AssessmentDocument3 pagesDeep Breathing Exercises: Procedure AssessmentJelly Jia100% (1)
- CASE STUDY - LeadershipDocument3 pagesCASE STUDY - LeadershipJino GamerNo ratings yet
- PE-ZR-DAS-NT-TR-02209: Comments Resolution SheetDocument81 pagesPE-ZR-DAS-NT-TR-02209: Comments Resolution SheetSheik BenasudeenNo ratings yet
- 7Th Grade Persuasive Essay TopicsDocument8 pages7Th Grade Persuasive Essay TopicsapgsrfnbfNo ratings yet
- 2.3 Sources of Health ReportingDocument5 pages2.3 Sources of Health ReportingPela KqbcgrlaNo ratings yet
- A Comparison of Test Retest Reliability and Random Measurement Error of BI and MBI in Patients With Chronic StrokeDocument6 pagesA Comparison of Test Retest Reliability and Random Measurement Error of BI and MBI in Patients With Chronic Strokelolocy LNo ratings yet
- Psikoedukasi Seks Mengenai LGBT Di Sma Muhammadiyah 1 PekanbaruDocument5 pagesPsikoedukasi Seks Mengenai LGBT Di Sma Muhammadiyah 1 PekanbaruAjeng Safitri -No ratings yet
- Grammar Plus - Unit 5Document4 pagesGrammar Plus - Unit 5Franklin Asencio0% (1)
- Method of Statement For Soil Replacement and BackfillingDocument7 pagesMethod of Statement For Soil Replacement and Backfillingmartina magedNo ratings yet
- Hayes.P Et - Al, 2012 - Foot Strike Patterns and Ground Contact Times During High-Calibre Middle-Distance RacesDocument10 pagesHayes.P Et - Al, 2012 - Foot Strike Patterns and Ground Contact Times During High-Calibre Middle-Distance Racesok okNo ratings yet
- Programa de Investigación FormativaDocument28 pagesPrograma de Investigación FormativaYESSAMEN ESTHER COLLANTES TORRESNo ratings yet
- Delta Green - Need To Know (Player Version)Document38 pagesDelta Green - Need To Know (Player Version)Jesse BerenfeldNo ratings yet
- HypospadiasDocument57 pagesHypospadiasTilahun SaolNo ratings yet
- Adha Standards08Document16 pagesAdha Standards08anasofiakNo ratings yet
- Developmental Olympic Lifting CycleDocument16 pagesDevelopmental Olympic Lifting Cyclehanus.milannseznam.czNo ratings yet
- Psychometric Properties of Senior Fitness TestDocument1 pagePsychometric Properties of Senior Fitness TestSrilatha GirishNo ratings yet
- Paper Presentation PDFDocument18 pagesPaper Presentation PDFramneekNo ratings yet
- Mental HelthDocument19 pagesMental Helthjayvee dacubaNo ratings yet
- Bibliotherapy - Definitions, Uses, and Studies by Lindeman & KLing (1968)Document6 pagesBibliotherapy - Definitions, Uses, and Studies by Lindeman & KLing (1968)Fourani HASP0% (1)
- Homeroom Guidance SampleDocument7 pagesHomeroom Guidance SampleAngelyn Lingatong100% (2)
- Double ComparisonDocument3 pagesDouble ComparisonMai PhuongNo ratings yet
- Seizure Case Study Answers 1Document3 pagesSeizure Case Study Answers 1Maica LectanaNo ratings yet
Journal Pone 0284911
Journal Pone 0284911
Uploaded by
SIVAMATHIVANAN P 22MTL129Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal Pone 0284911
Journal Pone 0284911
Uploaded by
SIVAMATHIVANAN P 22MTL129Copyright:
Available Formats
PLOS ONE
RESEARCH ARTICLE
Surface electromyography signal processing
and evaluation on respiratory muscles of
critically ill patients: A systematic review
Emanuel Fernandes Ferreira da Silva Junior ID1, Shirley Lima Campos2, Wagner
Souza Leite3, Pedro Vanderlei de Sousa Melo2, Rômulo Aquino Coelho Lins2, Maria das
Graças Rodrigues de Araújo2, Marcelo Renato Guerino ID1,2*
1 Translational Health Graduate Program, Federal University of Pernambuco—UFPE, Recife, Pernambuco,
Brazil, 2 Department of Physiotherapy, Federal University of Pernambuco—UFPE, Recife, Pernambuco,
a1111111111 Brazil, 3 Health-applied Biology Graduate Program, Federal University of Pernambuco—UFPE,
a1111111111 Pernambuco, Brazil
a1111111111
a1111111111 * marcelo.guerino@ufpe.br
a1111111111
Abstract
OPEN ACCESS
Background
Citation: Silva Junior EFFd, Campos SL, Leite WS,
Melo PVdS, Lins RAC, Araújo MdGRd, et al. (2023) Surface Electromyography (sEMG) has been used to monitor respiratory muscle function
Surface electromyography signal processing and and contractility in several clinical situations, however there is the lack of standardization for
evaluation on respiratory muscles of critically ill the analysis and processing of the signals.
patients: A systematic review. PLoS ONE 18(4):
e0284911. https://doi.org/10.1371/journal.
pone.0284911 Objective
Editor: Gustavo Plaza-Manzano, Complutense To summarize the respiratory muscles most assessed by sEMG in the critical care setting
University of Madrid: Universidad Complutense de and the assessment procedure details employed on those muscles regarding electrode
Madrid, SPAIN placement, signal acquisition, and data analysis.
Received: January 20, 2023
Accepted: April 12, 2023 Methods
Published: April 27, 2023 A systematic review of observational studies was registered on PROSPERO (number
CRD42022354469). The databases included PubMed; SCOPUS; CINAHL, Web of Science
Copyright: © 2023 Silva Junior et al. This is an
open access article distributed under the terms of and ScienceDirect. Two independent reviewers ran the quality assessment of the studies
the Creative Commons Attribution License, which using the Newcastle-Ottawa Scale and Downs & Black checklists.
permits unrestricted use, distribution, and
reproduction in any medium, provided the original
author and source are credited.
Results
Data Availability Statement: All relevant data are
A total of 311 participants were involved across the 16 studies, from which 62.5% (10)
within the manuscript and its Supporting assessed the diaphragm muscle and 50% (8) assessed the parasternal muscle with similar
Information files. electrode placement in both of them. We did not identify common patterns for the location of
Funding: SLC, 001, The Prorectorate for Graduate the electrodes in the sternocleidomastoid and anterior scalene muscles. 12/16 reported
Studies (PROPG) da Federal University of sample rate, 10/16 reported band-pass and 9/16 reported one method of cardiac-interfer-
Pernambuco – UFPE Coordination for the
ence filtering technique. 15/16 reported Root Mean Square (RMS) or derivatives as sEMG-
Improvement of Higher Education Personnel
(CAPES); APQ-0249-4.08/20, Foundation for obtained variables. The main applicabilities were the description of muscle activation in dif-
Science and Technology Support from ferent settings (6/16), testing of reliability and correlation to other respiratory muscles
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 1 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Pernambuco (FACEPE) and 403341/2020-5, assessment techniques (7/16), and assessment of therapy response (3/16). They found
National Council for Scientific and Technological sEMG feasible and useful for prognosis purposes (2/16), treatment guidance (6/16), reliable
Development – CNPq / Ministry of Science,
Technology, Innovation and Communications /
monitoring under stable conditions (3/16), and as a surrogate measure (5/16) in mechani-
Ministry of Health of Brazil – MoH MRG, 001, The cally ventilated patients in elective or emergency invasive procedures (5/16) or in acute
Prorectorate for Graduate Studies (PROPG) da health conditions (11/16).
Federal University of Pernambuco – UFPE
Coordination for the Improvement of Higher
Education Personnel (CAPES).
Conclusions
The diaphragm and parasternal muscles were the main muscles studied in the critical care set-
Competing interests: The authors have declared
that no competing interests exist. ting, and with similar electrodes placement. However, several different methods were observed
for other muscles electrodes placement, sEMG signals acquisition and data analysis.
1. Introduction
Surface Electromyography (sEMG) signals have been recognized as a technological instrument
for capturing respiratory myoelectric signals, and have been highlighted for the evaluation of
respiratory neuromuscular function. In 2002, the American Thoracic Society/European Respi-
ratory Society issued guidelines validating the use of sEMG signals as a method for analyzing
respiratory neural triggering [1].
Respiratory muscle dysfunction is common in critically ill patients, and can lead to acute
respiratory failure, also associated with increased hospital mortality, morbidity and hospital
stay [2]. Therefore, it is crucial to assess respiratory functions, including the activity of the dia-
phragm and other respiratory muscles. Surface electromyography (sEMG) is a useful non-
invasive asset that provides valuable information for monitoring the activity of these muscles
[3] during breathing in critically ill patients.
sEMG signals can be employed to identify patients who are at risk for respiratory failure,
monitoring the response to therapy, and guiding the timing of interventions [4,5]. Further-
more, they can offer insight into the patient’s level of effort during breathing [6], facilitate the
assessment of the effectiveness of various ventilation strategies [6,7] and thus contribute to
improving outcomes by allowing for earlier identification and intervention.
Despite the wide range of functionalities and benefits, the lack of standardization in sEMG
can create issues, such as data inconsistency [8], due to non-standardized procedures for elec-
trode placement, signal acquisition, and data analysis. This can lead to inaccurate diagnoses
and ineffective treatments resulting from potential misinterpretation of data and respective
errors. Moreover, limited comparability and replicability of sEMG protocols [9], which may
hinder evidence-based practices and jeopardize progress in the field.
In 1999, the Surface EMG for Non-Invasive Assessment of Muscle (SENIAM) project
aimed to integrate basic and applied research on sEMG for European cooperation. The project
resulted in recommendations for sensor placement procedures and signal processing for 27
muscle segments, however, respiratory muscles were not included [10]. Thus, bringing the
need for scientific evidence regarding the optimal sEMG procedures and analysis for respira-
tory muscles [11,12].
Based on the considerations presented, we conducted a systematic review of surface electro-
myography to address the following research questions:
1. What were the main respiratory muscles assessed through sEMG in the critical care setting?
2. What sEMG procedure details are described, regarding electrode placement, signal acquisi-
tion, and data analysis?
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 2 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
2. Methods
2.1 Design
This study was conducted as a systematic review, adhering to the PRISMA (2020) guidelines
for reporting of systematic reviews and meta-Analysis [13] S4 Table. Details of the protocol for
this review were registered on PROSPERO (number CRD42022354469).
2.2 Data sources and search strategy
Five databases were searched for this review, including Medical Literature Analysis and
Retrieval System Online (Medline) of the United States National Library of Medicine
(PubMed), SCOPUS, Cumulative Index to Nursing and Allied Health Literature (CINAHL),
Web of Science and ScienceDirect. The bibliographic survey was conducted until August 11,
2022 with no restrictions on language or year of publication. The search terms were formu-
lated using adaptation to the PICO framework, and indexed terms from the Medical Subject
Headings (MeSH) metadata system were combined with and keywords, “surface electromyog-
raphy”; “respiratory muscles” and “intensive care unit”, to create a comprehensive search strat-
egy tailored to each database’s particularities, as described in S1 Appendix.
2.3 Eligibility criteria
The inclusion criteria for this study were as follows: (1) study design—observational studies,
including retrospective, prospective cohort, case-control, and cross-sectional; (2) assessment
instrument—respiratory assessment using sEMG; (3) population–adults aged 18 years or
older; (4) Condition: admitted to an intensive care unit. Studies that applied other methods of
muscle electrical activity assessment aside from sEMG, such as needle EMG, were excluded, as
well as those focusing solely on burn patients or patients requiring neuromuscular blockers, or
missing information of sEMG parameter configuration or signal processing.
2.4 Screening and data extraction
First, the eligible studies had their title and abstract screened using the Systematic Review-Ray-
yan [14] synthesis software by two independent reviewers (E. F. F. S. J. and W. S. L.). Secondly,
full-text screening was performed on the selected studies, and in cases of disagreement
between the pair of reviewers, a third assessor was consulted to resolve discrepancies. Finally,
the data extracted comprised: author, year, country, study objectives, study design, sample
characteristics, and sEMG data-related variables, such as respiratory muscles assessed, elec-
trode placement, signal acquisition, and data analysis. The flowchart of included and excluded
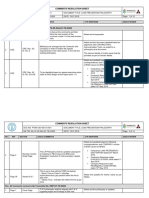
localized literature is represented using terms described in (Fig 1).
2.5 Quality assessment
The quality appraisal of observational studies was conducted using two checklists: Newcastle-
Ottawa [15] and Downs & Black scales [16]. The Newcastle-Ottawa scale comprises three
domains: selection, comparability, and exposure receiving scores from zero to nine. The result-
ing interval scores are used to qualify the studies into Good (7–9 points), Satisfactory (5–6
points), or Poor (0–4 points) quality [15]. The scale presents a slight difference in the scoring
system for case-control and cross-sectional studies.
The Downs & Black scale comprises a questionnaire consisting of 27 items categorized into
five domains: reporting (10 items), external validity (3 items), study bias (7 items), confound-
ing factors (6 items), and study power (1 item). The final items are scored as yes or no
responses. The final scores assigned to studies are used to determine their methodological
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 3 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Fig 1. Identification of studies through databases according to Preferred Reporting Items for Systematic Reviews and Meta-
analyses (PRISMA).
https://doi.org/10.1371/journal.pone.0284911.g001
quality with scores categorized as: Excellent (26–28); Good (20–25); Righteous (15–19); and
Poor (�14) points [16].
3. Results
The total of 36,901 articles were initially screened, then reduced to 36,341 after excluding 560
duplicates. An additional 36,317 articles were excluded based on their failure to meet the inclu-
sion criteria after the title/abstract screening and further 8 articles were excluded due to miss-
ing information of sEMG parameter configuration or signal processing. As a result of this
screening process, 16 articles were included in this review (Fig 1).
3.1 Quality assessment
15 studies (93.75%) were scored as cross-sectional design and one study (6.25%) were scored
as case-control design. By using the Newcastle-Ottawa scale, 11 studies (68.75%) were rated as
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 4 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Table 1. Quality assessment of the included studies.
Author, year, Country Study design Methodological quality (Score)
Newcastle-Ottawa Scale Downs & black Scale
Pozzi et al. (2022) [17], Cross-sectional 6 15
Italy (Satisfactory) (Fair)
Graßhoff et al. (2021) [18], Germany Cross-sectional 6 15
(Satisfactory) (Fair)
Bureau et al. (2021) [19], France Cross-sectional 7 15
(Good) (Fair)
Lokin et al. (2020) [20], Netherlands Cross-sectional 7 15
(Good) (Fair)
Roesthuis et al. (2020) [21], Netherlands Cross-sectional 7 16
(Good) (Fair)
Souza Costa et al. (2020) [22], Brazil Cross-sectional 7 15
(Good) (Fair)
Bellani et al. (2018) [6], Cross-sectional 5 15
Italy (Satisfactory) (Fair)
Duarte et al. (2017) [23], Cross-sectional 5 15
Brazil (Satisfactory) (Fair)
Sánchez et al. (2017) [24], Colombia Case-control 7 15
(Good) (Fair)
Ortega et al. (2017) [25], Colombia Cross-sectional 6 15
(Satisfactory) (Fair)
Walterspache et al. (2017) [26], Germany Cross-sectional 6 16
(Satisfactory) (Fair)
Cecchini et al. 2014 [27], Cross-sectional 6 15
France (Satisfactory) (Fair)
Schmidt et al. 2013 [28], Cross-sectional 5 17
France (Satisfactory) (Fair)
Tassaux et al. 2005 [29], Switzerland Cross-sectional 5 14
(Satisfactory) (Poor)
Tassaux et al. (2002) [30], Switzerland Cross-sectional 6 14
(Satisfactory) (Poor)
Imsand et al. 1994 [31], Switzerland Cross-sectional 5 12
(Satisfactory) (Poor)
https://doi.org/10.1371/journal.pone.0284911.t001
having “satisfactory” quality, while five studies (31.25%) were classified as “good” Table 1.
None of the studies were considered to be of poor methodological quality, as detailed in S1
and S2 Tables. Meanwhile, using the Downs & Black scale, 13 studies (81.25%) were classified
as having fair methodological quality, while three studies (18.75%) were considered to be of
“poor” quality, as outlined in S3 Table.
3.2 Outcome: sEMG processing variables for respiratory muscles
Table 2 shows the processing data for the sEMG analysis. Sampling rate was mentioned in
twelve studies (75%) obtaining variations between 500 and 10,000 Hz [6,17–19,21,23–
27,29,30], Bandpass filters were reported in 10 studies (62.5%) with variations between
0–1,000 Hz [6,17,19,21,22,24–27,31]. Only one study (6.25%) reported high-pass and low-pass
filters for EMG signal processing details [26].
Regarding cardiac-interference filtering techniques to prevent EMG noise contamination,
nine studies (50%) have reported a number of techniques, including gating [6,17,18,20,31], or
some sort of adaptive filter [21,25,30] or even visual inspection [26]. Amplifier gain is one of
the settings for high quality EMG signals with low noise. This setting is defined as the ratio
between the voltage that enters and exits the amplifier, should suit the characteristics of the
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 5 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Table 2. Summary of respiratory muscle sEMG processing variables.
Author/Year Respiratory muscle sEMG processing data
Sample rate LPF HPF Band-pass CIF technique Amplifier Data acquisition Unit Measures Software
(Hz) (Hz) (Hz) (Hz) Gain duration
Pozzi et al. (2022) [17] 500 NR NR 0–200 Gating NR 180s μV RMS LabChat
Graßhoff et al. (2021) 1.000 NR NR NR Gating NR NR μV RMS NR
[18]
Bureau et al. (2021) 10.000 NR NR 40–500 NR NR 600s NR EMGMAX/ LabChart
[19] EMGAUC
Lokin et al. (2020) NR NR NR NR Gating NR 900s μV RMS MATLAB
[20] R2016a
Roesthuis et al. (2020) 2.048 NR NR 25–500 Wavelet-based NR 300s % EMGPEAK; MATLAB
[21] adaptive filter EMGAUC/min R2014b
Souza Costa et al. NR NR NR 20–500 NR NR 60s μV RMS NR
(2020) [22]
Bellani et al. (2018) 500 NR NR 0–200 Gating 20 NR μV RMS Dipha Software
[6]
Duarte et al. (2017) 500 NR NR NR NR NR NR NR RMS NR
[23]
Sánchez et al. (2017) 1.024 NR NR 20–500 NR NR 1.200s NR RMS NR
[24]
Ortega et al. (2017) 1.024 NR NR 10–500 RLS adaptive 5th- NR 180s NR NR NR
[25] order filter
Walterspacher et al. 10.000 500 1.000 20–1.000 Visual inspection 1000 120s % RMS LabChat v.7.2
(2017) [26]
Cecchini et al. (2014) 2.000 NR NR 10–1.000 NR 500 180s % RMS NR
[27]
Schmidt et al. (2013) NR NR NR NR NR NR NR NR EMGMAX; NR
[28] EMGAUC
Tassaux et al. (2005) 1.000 NR NR NR NR NR 60s NR EMG signal NR
[29]
Tassaux et al. (2002) 2.000 NR NR NR 50-Hz filter NR 600s NR EMGAUC AcqKnowledge
[30]
Imsand et al. (1994) NR NR NR 15–1.000 Manual gating NR 60s % EMG signals NR
[31]
LPF: Low-pass filter; HPF: High-pass filter; CIF: Cardiac-interference filtering; NR: Not reported; RMS: Root mean square; EMG: Electromyogram; EMGAUC: Area
under the EMG signal curve; EMGmax: The difference between the maximum amplitude of RMS signal and its baseline; EMGpeak: Peak of muscle activity during
inspiration; EMGAUC/min: End of muscle activity per breath.
https://doi.org/10.1371/journal.pone.0284911.t002
experiment, the type of electrodes used, as well as the muscle studied, and not the adjusted to
exceed the voltage expected from the system [32]. Gain was mentioned in three studies
(18.75%) with variations between 20–1,000 times [6,26,27]. EMG data acquisition recording
reported by twelve studies (75%) varied from 60 through 1.200 seconds [17,19–22,24–27,29–
31] Table 2.
Regarding the sEMG signal units, five papers (31.25%) [6,17,18,20,22] presented them in
microvolts (μV), four studies (25%) [21,26,27,31] in percentages, and eight studies (50%) did
not inform any unit [19,23–25,28–31]. The obtained variables were presented as simple mean
RMS/EMG signal usually rectified or normalized [6,17–20,22–24,26,27,29] or integrated RMS/
EMG signals—the difference between the maximum amplitude of RMS signal and its baseline
(EMGMAX), area under the EMG signal curve (EMGAUC), peak of muscle activity during inspi-
ration (EMGPEAK), and end of muscle activity per breath (EMGAUC/min) [19,21,28,30,31]
Table 2.
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 6 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
For software dedicated to sEMG signal offline analysis, only seven (43.75%) reported which
one they used. Labchart was the most reported by three studies (18.75%) [17,19,26], followed
by two reporting Matlab (12.5%) [20,21] and two reporting Dinha (6.25%) [6], and Acqknow-
ledge (6.25%) [30] Table 2.
3.3 Outcomes: Characteristics of the studies, technical parameters of sEMG
of the respiratory muscles and clinical applicability
A total of 311 participants were involved across the 16 studies, with 15 studies (66.2%) report-
ing male participants as the majority. The average age of the participants ranged from
62.1 ± 10.56 years Table 3.
According to the objectives of the included studies, the applicability of sEMG used in
mechanically ventilated patients can be summarized to the following categories, description
muscles activation in different settings [17,21–23,28,31], testing of reliability and correlation
to other respiratory muscles assessment techniques [6,18,20,24–27] and assessment of therapy
response [19,29,30]. These studies have found that sEMG was feasible and resourceful tool for
prognosis purposes [17,22] treatment guidance [19,26,27,29–31], reliable monitoring under
stable conditions [20,23,28] and as surrogate measure [6,18,21,24,25] Table 3.
The mechanically ventilated patients’ scenarios for sEMG assessment employment were
either in the elective or emergency invasive procedures [18,20,23,25,26] or in acute health con-
ditions [6,17,19,21,22,24,27–30] Table 3.
Scalene muscles (ESC) were analyzed in four studies (25%) [21,22,27,28] however, informa-
tion related to electrode placement was described in only three studies (18.75%), guided by
ultrasound positioned in the lower region of the muscle third [21], positioned in the posterior
triangle of the neck, at the level of the cricoid cartilage [27] and in bilateral recordings, posi-
tioned in the posterior triangle of the neck at the level of the cricoid cartilage, between the ster-
nocleidomastoid muscle and the clavicle [28]. Some studies did not provide sufficient
information to determine placement [22] Table 3.
Sternocleidomastoid (SCM) muscle analysis was performed in seven studies (43.7%)
[6,17,21,22,24,30,31], therefore, information related to electrode placement was described in
only six studies (37.5%) rejecting each other, being its placement in the middle third, identified
by palpation on the right or left side, generally opposite to the medications due to the fixation
of the central venous catheter [6,17], guided by ultrasound in the lower third of the muscle
[21], 20% of the distance between the mastoid apophysis and the sternal furcula [39], posi-
tioned over the muscle “palpation” and the mastoid process [30] and fixed on the muscle body
[31]. The other studies did not provide information to determine the placement [22] Table 3.
The terminology referring to the parasternal has been characterized by the intercostal por-
tion parallel to the sternum, however, it may be linked to the intercostal muscles, referring to
the fibers parallel to the sternum [33–35]. The selected papers described and analyzed the para-
sternal muscles in eight studies (50%), under the positioning in the second intercostal space
[6,17–19,21,26,28], and electrodes placed in the fifth intercostal space in the posterior axillary
line2, however only [6,17,18,26] placed the electrodes bilaterally Table 3.
The positioning of the electrodes on the Diaphragm (DIA) was measured in ten studies
(62.5%), attached to the lower intercostal spaces in the midclavicular line
[6,17,18,20,22,24,25,29] that of these only three studies analyzed the right hemibody [22,24,25]
and positioning two electrodes in the paraxiphoid region, 5 cm below the xiphoid process, and
the other 2, in the bilateral costal margin region, with a distance of approximately 16 cm
between them [23,26]. Only one study (6.25%) reported analyzing the Rectus Abdominal mus-
cle with its positioning on the left midclavicular line, at the level of the umbilicus [17] Table 3.
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 7 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Table 3. Summary of sample characteristics, technical parameters of sEMG of the respiratory muscles, clinical use and respective studies’ findings.
Author, year, Objective Sample characteristics Body position, skin electrode
Country placement and muscles assessed Main findings
Pozzi et al. To describe respiratory muscle N. of participants: 37. Body position: Not reported. Respiratory muscles’ electrical
(2022) [17], Italy activation by sEMG during an Age: 56 (50–62). Reference electrode: Not reported. activity increased during
spontaneous breathing trial and to Sex: M: 27/ F: 10. Inter electrode distance: Not spontaneous breathing trial.
assess their electrical activity in Condition: COPD, Diabetes, reported. Recruitment of expiratory muscles
successful vs. failing weaning ARDS, atrial fibrillation, Diaphragm: Lower costal margin, quantified by sEMG is associated
patients. Septic shock. bilaterally on the midclavicular line. with this trial failure.
Inclusion criteria: Patients Parasternals: 2nd intercostal space,
who were on IMV for > 48 h bilaterally in the parasternal line.
eligible for spontaneous Sternocleidomastoid: In the middle
breathing trial. third of the sternocleidomastoid
muscle, on the right or left side
(usually opposite the central venous
line).
Rectus abdominis: On the left
midclavicular line, at the level of the
umbilicus.
Graßhoff et al. To investigate the estimation of the N. of participants: 43. Body position: Not reported. sEMG was well correlated with
(2021) [18], pressure-time product of Age: 64 ± 11. Reference electrode: Sternum. pressure-time product. sEMG can be
Germany inspiratory muscle pressure via Sex: M: 34/ F: 9. Inter electrode distance: Not used as a non-invasive alternative for
sEMG by identifying a patient- Condition: Patients scheduled reported. monitoring the patients’ inspiratory
specific conversion factor during for elective bronchoscopy. Diaphragm: Bilaterally at the lower effort under assisted mechanical
end-expiratory occlusions. Inclusion criteria: Intubated, costal margin on the midclavicular ventilation.
moderate/deep sedation level, line.
on assisted spontaneous Parasternals: Bilaterally in the 2˚
ventilation. intercostal space on the parasternal
line.
Bureau et al. To evaluate the respective impact of N. of participants: 34. Body position: Not reported. Parasternal intercostal muscles
(2021) [19], customized PAV and PSV settings Age: 66 (57–77). Reference electrode: Not reported. electrical activity and asynchrony
France on patient-ventilator asynchrony. Sex: M: 25 / F: 9. Inter electrode distance: 2 cm. index were lower with PAV and
Condition: Patients on PSV Parasternals: 2˚ intercostal space other PSV modes. Mechanical
under IMV for > 24 h, for lateral to the estrum. ventilation modes did not decrease
respiratory cause with Alae nasi muscles: Placed on the dyspnea and activity of muscles,
hypoxemia. lateral surfaces of the nose. even though PAV was able to reduce
Inclusion criteria: Sedated in asynchrony more effectively.
IMV.
Lokin et al. To compare the ability of N. of participants: 15. Body position: Not reported. sEMG was not reliable for breathing
(2020) [20], diaphragm activity detection Age: 62 (45–72). Reference electrode: Sternum. effort detection in subjects who were
Netherlands between surface electromyography Sex: M: 9 / F: 6. Inter electrode distance: Not invasively ventilated compared with
of the diaphragm and Condition: Adults with reported. transesophageal electromyography.
transesophageal electromyography clinical complications, Diaphragm: Bilaterally below the In stable recordings, however, both
of the diaphragm. elective and emergency front and lower dorsal ribs. of the methods had excellent
surgery. temporal correlation and good
Inclusion criteria: At least 48 agreement.
h of IMV in PSV.
Roesthuis et al. To investigate the effect of different N. of participants: 17. Body position: Not reported. Extradiaphragmatic inspiratory
(2020) [21], inspiratory support levels on the Age: 64 ± 8.2. Reference electrode Patient’s pulse. muscle activity increases in response
Netherlands recruitment pattern of Sex: M: 12 / F: 5. Inter electrode distance: Not to lower inspiratory support levels.
extradiaphragmatic inspiratory Condition: COPD, reported. However, there is a poor correlation
muscles and to evaluate agreement pneumonia, ARDS, Scalenes/Sternocleidomastoid: Lower and agreement with the change in
between activity of abdominal aortic aneurysm. third of the muscles. diaphragm activity.
extradiaphragmatic inspiratory Inclusion criteria: At least 3 Parasternals: 2nd intercostal space, 3
muscles and the diaphragm. days in IMV, light/some deep cm lateral to the sternum.
sedation. Alae nasi muscles: Placement of an
electrode in each nostril
Genioglossus: Below the chin and
above the hyoid bone.
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 8 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Table 3. (Continued)
Author, year, Objective Sample characteristics Body position, skin electrode
Country placement and muscles assessed Main findings
Souza Costa To analyze the respiratory muscle N. of participants: 46. Body position: 45˚. Subjects succeeding in a weaning
et al. (2020) [22], groups involved with the timed Age: 80 (71–87). Reference electrode: Not reported. trial had higher muscle strength. A
Brazil inspiratory index index utilizing the Sex: M: 26 / F: 20. Inter electrode distance: Not vigorous diaphragm with low fatigue
sEMG. Condition: Sepsis, acute reported. potential seems essential for
respiratory failure, stroke and Diaphragm: In the lower intercostal successful weaning.
heart failure. spaces on the right side of the body, in
Inclusion criteria: Patients the midclavicular line.
who were on IMV for > 24 h, Scalenes: Not reported.
clinically ready for the Sternocleidomastoid: Not reported.
weaning process. External intercostals: In the 5th
intercostal space on the posterior
axillary line.
Bellani et al. To assess the reliability of sEMG of N. of participants: 14. Body position: Not reported. Diaphragm activity can be reliably
(2018) [6], Italy the respiratory muscles for Age: 56 ± 12. Reference electrode: Not reported. monitored by both electrical activity
monitoring diaphragm electrical Sex: M: 12 / F:2. Inter electrode distance: Not measured by nasogastric tube with
activity and subject effort during Condition: Pneumonia, reported. electrodes and sEMG.
assisted ventilation. ARDS, sepsis, trauma. Sternocleidomastoid: Middle third of
Inclusion criteria: Patients the SCM muscle.
intubated or tracheostomized External intercostals: 2th intercostal
in PSV mode. space, bilaterally on the parasternal
line, for parasternal external
intercostal muscles.
Diaphragm: Inferior costal margin,
bilaterally in the midclavicular line,
for costal diaphragm.
Duarte et al. To evaluate the diaphragmatic N. of participants: 14. Body position: 35˚. There were significant differences
(2017) [23], surface electromyography of Age: 57 ± 7.1. Reference electrode: Not reported. between the root mean square of the
Brazil postoperative liver transplantation Sex: M: 10 / F:4. Inter electrode distance: 16 cm. diaphragm domes under mechanical
subjects. Condition: Liver Diaphragm: Two electrodes in the ventilation and after extubation,
transplantation. paraxiphoid region, 5 cm below the showing lower effectiveness of the
Inclusion criteria: Patients xiphoid process, and the other 2, in diaphragm muscle against
eligible for extubation in the region of the bilateral costal resistance.
PSV. margin, with approximately 16 cm
between them.
Sánchez et al. To assess the engagement of the Case group Body Position: Not reported. Engagement of respiratory muscles
(2017) [24], respiratory muscles as an index N. of participants: 23. Reference electrode: Not reported. index is a promising index to assess
Colombia during spontaneous breathing trial Age: 30.3 ± 10. Inter electrode distance: Not the level of participation of
and to associate the level of Sex: M: 14 / F:9. reported. respiratory muscle on spontaneous
engagement with the muscular Condition: Patients poisoned Diaphragm: Anterolateral portion of breathing test in patients poisoned,
weakness in poisoned patients. by organophosphate. the thorax, between the 6th and 8th which could improve the extubation
Inclusion criteria: Patients intercostal space, between the mid- prognosis for these patients.
who were on IMV during axillary line and the external clavicular
spontaneous breathing trial. line
Control group Sternocleidomastoid: 20% of the
N. of participants: 28. distance between the mastoid
Age: 27 ± 6.5. apophysis and the sternal notch.
Sex: M: 21/ F:7.
Condition: Healthy patients.
Inclusion criteria: Received
non-invasive ventilation for
900 second.
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 9 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Table 3. (Continued)
Author, year, Objective Sample characteristics Body position, skin electrode
Country placement and muscles assessed Main findings
Ortega et al. To evaluate the feasibility of sEMG N. of participants: 10. Body position: Not reported. The obtained indexes show a
(2017) [25], derived indexes in predicting Age: 63.14 ± 16.9. Reference electrode: Not reported. correlation between high
Colombia weaning outcomes among Sex: M: 10. Inter electrode distance: Not expenditure and weaning test failure.
mechanically ventilated subjects Condition: Postoperative reported. sEMG is becoming a promising
after cardiac surgery. cardiac surgery. Diaphragm: Between the 7th and 8th procedure for assessing the state of
Inclusion criteria: Clinically intercostal spaces between the mechanically ventilated patients.
stable ready for IMV midaxillary line and the external
weaning. clavicular line.
Walterspache To assess the acute effects on the N. of participants: 9. Body position: Supine (lying down), Diaphragm’s electrical activity
et al. (2017) [26], neural respiratory drive measured Age: 66 ± 18. semi-sitting at 30˚ and sitting at 80˚ in changed under spontaneous
Germany by sEMG and the diaphragm in Sex: M: 6 / F: 3. bed. breathing from supine to sitting and
different body positions during Condition: Lung Reference electrode: Not reported. between semirecumbent to sitting.
mechanical ventilation. transplantation and stroke. Inter electrode distance: 2cm. Body positioning influences
Inclusion criteria: Diaphragm: Bilaterally on the lower respiratory drive to the diaphragm
Tracheostomized patients costal margin, 16 cm lateral to the in tracheotomized patients during
hemodynamically stable in common electrode, placed 5 cm unassisted breathing.
spontaneous breathing trial. cranial to the xiphoid.
Parasternals: Bilaterally in the 2nd
intercostal space.
Cecchini et al. To compare electrical activity of N. of participants: 12. Body position: Not reported. NAVA and PSV both reduced
2014 [27], diaphragm, scalene, and alae nasi, Age: 68 ± 8. Reference electrode: Not reported. extradiaphragmatic inspiratory
France according to the ventilatory mode Sex: Not reported. Inter electrode distance: Not muscle activity, in proportion to the
and assist level. Condition: Patients with reported. level of assistance. NAVA resulted in
acute respiratory failure, Scalenes: In the posterior triangle of a predominant contribution of the
pneumonia, ARDS, the neck, at the level of the cricoid diaphragm to inspiratory effort.
pulmonary edema, septic and cartilage.
cardiogenic shock Alae nasi muscles: They were
Inclusion criteria: Adults in obtained by placing an electrode in
IMV capable of triggering each nostril.
PSV/NAVA.
Schmidt et al. To determine if sEMG of N. of participants: 12. Body position: Not reported. sEMG of extradiaphragmatic
2013 [28], extradiaphragmatic inspiratory Age: 60 ± 15. Reference electrode: Not reported. inspiratory muscles provides a
France muscles vary with PSV settings and Sex: M: 9 / F: 3. Inter electrode distance: Not reliable and non-invasive indicator
relate to the degree of discomfort Condition: Patients with reported. of respiratory muscle loading/
and the intensity of dyspnea in pneumonia, COPD and Scalenes: Bilateral registers, unloading in mechanically ventilated
acutely ill patients. septic shock. positioned in the posterior triangle of patients. It is strongly correlated to
Inclusion criteria: Patients the neck at the level of the cricoid the intensity of dyspnea, and could
intubated or tracheostomized cartilage, between the be used as a surrogate of respiratory
in IMV weaning process. sternocleidomastoid muscle and the sensations.
clavicle.
Parasternals: Bilateral records,
positioned in the 2nd intercostal
space, close to the sternum.
Alae nasi muscles: Placement of an
electrode in each nostril.
Tassaux et al. To test the hypothesis that N. of participants: 10. Body position: Not reported. Setting expiratory trigger at a higher
2005 [29], increasing the expiratory trigger set- Age: 68.7 ± 10. Reference electrode: Sternum. percentage of peak inspiratory flow
Switzerlan point could reduce the magnitude Sex: M: 7 / F: 3. Inter electrode distance: Not in patients with obstructive disease
of intrinsic PEEP, the number of Condition: Patients with reported. during pressure support improves
non triggering breaths, the level of acute respiratory failure with Diaphragm: Bilaterally on the costal patient–ventilator synchrony and
inspiratory effort and triggering COPD Inclusion criteria: margin. reduces inspiratory muscle effort.
delay. Intubated patients in IMV
weaning phase.
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 10 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Table 3. (Continued)
Author, year, Objective Sample characteristics Body position, skin electrode
Country placement and muscles assessed Main findings
Tassaux et al. To compare the effects of ASV and N. of participants: 10. Body position: Not reported. ASV provided levels of minute
(2002) [30], SIMV-PS modes on patient- Age: 71 ± 9.6. Reference electrode: Not reported. ventilation comparable to those of
Switzerlan ventilator interactions in Sex: F: 6 / M: 4. Inter electrode distance: Not SIMV-PS. Central respiratory drive
mechanical ventilation. Condition: Patients with reported. and sternocleidomastoid activity
COPD exacerbation, acute Sternocleidomastoid: Placed over the were markedly reduced in ASV,
pneumonia, asthma and muscle (palpation) and the mastoid suggesting decreased inspiratory
sepsis. process. load and improved patient-ventilator
Inclusion criteria: Intubated interactions.
patients in weaning
procedure by SIMV-PS or
ASV mode.
Imsand et al. To assess quantitatively the effect of N. of participants: 5. Body position: 45˚. The durations of electrical activation
1994 [31], varying the level of machine Age: 58.6 ± 8. Reference electrode: Not reported. and the integrated electromyograms
Switzerland assistance on the electrical activity Sex: M: 1 / F: 4. Inter electrode distance: Not of diaphragm and
amplitude of inspiratory muscles. Condition: COPD reported. sternocleidomastoid were similar in
Inclusion criteria: intubated Sternocleidomastoid: Muscle body. successive spontaneous and assisted
patients, hemodinamically breaths, neither changed with
stable, conscious and not increasing level of machine
sedated. assistance.
ARDS: Acute respiratory distress syndrome; cm: Centimeters; COPD: Chronic obstructive pulmonary disease; sEMG: Surface electromyography; ICU: Intensive care
unit; IMV: Invasive mechanical ventilation; PEEP: Positive end-expiratory pressure; NAVA: Neurally adjusted ventilatory assist; PAV: Proportional assist ventilation;
PSV: Pressure support ventilation; ASV: Adaptive support ventilation; SIMV-PS: Synchronized intermittent mandatory ventilation plus pressure support, F: Female; M:
Male; mm: Millimeters; RMS: Root mean square.
https://doi.org/10.1371/journal.pone.0284911.t003
The alae nasi muscles were analyzed in only four studies (25%) [19,21,27,28] with its elec-
trodes for electromyographic capture placed in each nostril. The genioglossus muscle was ana-
lyzed in only one study (6.25%), reliably reporting its positioning, characterized below the
chin and above the hyoid bone [21]. In relation to the reference electrode, only four studies
(25%) reported its placement, three studies (18.75%) under the sternum [18,20,29], and one
study (6.25%) attached to the patient’s wrist [21].
The interelectrode distance affects the signal quality and determines the volume of muscle
fibers that will be measured, therefore, affecting the selectivity of recording. This parameter
was reported in three studies (18.75%) which reported its distance of 2 cm [19,26] and 16 cm
[23]. Four studies (25%) reported the angle positioning of patients: 35˚ [19], 45˚ [22,31] and in
three different body positions, supine at 0˚, semirecumbent at 30˚ and sitting at 80˚ on the bed
[26] Table 3.
4. Discussion
This review presents findings indicating that the diaphragm and parasternal muscles were the
most commonly used for assessing respiratory function through sEMG in critically ill patients
admitted to the ICU. To the best of our knowledge, this is the first systematic review to com-
prehensively summarize the methodological aspects of the evaluation protocols and sEMG sig-
nals processing of respiratory muscles in patients admitted to the ICU.
Upon analyzing the respiratory electromyographic data processing and analysis procedures
in the included studies, it was found a lack of standardization in the target respiratory muscles,
electrode placement and data acquisition details. Therefore, the studies could not be subjected
to quantitative analyses or meta-analyses. A wide range of significant variation in the anatomi-
cal sites for skin electrode placement, especially for muscles underlying other larger muscles.
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 11 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
This could be minimized by implementing other resources, such as ultrasound guidance, as
demonstrated by Roesthuis et al. [21], although Imsand et al. [31] presented some respiratory
muscles feasible to be tracked for electrode placement by palpating muscle body.
The diaphragm and parasternal muscles were the most common for sEMG assessment in
critically ill patients in the ICU, likely due to their crucial role in respiratory function. The dia-
phragm electromyogram provides a sensitive measure of neural respiratory drive with each
breath and reflects the imposed load on respiratory muscles [36]. Similarly, the parasternal
intercostal muscles are obligatory during respiration [37] and are the first external respiratory
muscles to respond to an increased demand. Electrodes for diaphragm sEMG are typically
placed in the 7th or 8th intercostal spaces along the midclavicular line, which is the zone of
apposition where the active diaphragm thickens with consequent lung volume increase during
breathing [38,39]. For the parasternal muscles, electrodes are typically placed in the 2nd or 3rd
intercostal spaces along the midclavicular line. However, the historical summary of different
locations has challenged the consistency and reliability of its sEMG signals, particularly with
the interference of the large pectoralis major muscle [38]. This site for sEMG of parasternal
has been studied through ultrasound imaging and it was found to be an area audible and visi-
ble for single motor unit activity with an acceptable signal-to-noise ratio [39].
The use of sEMG in critically ill patients undergoing invasive mechanical ventilation may
provide a reliable assessment tool, however, it must be used with caution as the ventilatory
modes can affect the observed results. For example, Roesthuis et al. [21], reported that the
activity of the extra diaphragmatic inspiratory muscles increases when they remain at lower
levels under support pressure. Furthermore, Cecchini et al. [27] showed that increasing levels
of ventilatory support pressure and Neurally Adjusted Ventilatory Assist (NAVA) reduced the
electrical activity of the diaphragm, scalene and alae nasal muscles. Nevertheless the study con-
ducted by Bellani et al. [6] reported that electrical activity of the diaphragm, evaluated using
sEMG, can be reliably used during ventilation with pressure support as it was analyzed and
correlated with esophageal electrical measures. Additionally, Imsand et al. [31] study demon-
strated that the duration of diaphragm and sternocleidomastoid electrical activities were simi-
lar with successive spontaneous and assisted breaths, except that the use of ventilation with
support pressure has been preventing diaphragmatic fatigue [40].
Regarding patient positions during sEMG analysis, only the study conducted by Walterspa-
cher et al. [26], revealed that the diaphragm muscle is the most active in supine and semi-sit-
ting positions, while having reduced activation in the sitting position. The authors explained
this phenomenon by attributing it to the compensation mechanism for changes in the length-
tension of the diaphragm by the changes of body position, which unloads the diaphragm.
Systematic reviews of sEMG protocols in healthy individuals [11] adults and the elderly
[12], were fundamental to research the evidence for sEMG in the ICU. A similar pattern was
noticed with the immense variability of sEMG protocols and analyzes. In the context of the
ICU, Abunurah et al. [5] performed a systematic review, not including details for processing
sEMG or placing surface electrodes on the respiratory muscles, as described in the present sys-
tematic review.
During breathing in the upright position, other muscles besides the diaphragm are
recruited, such as the scalenes and the parasternal intercostals. According to respiratory physi-
ology, when high requirements for increased lung ventilation are present, recruitment of
accessory respiratory muscles is required, characterized by the sternocleidomastoid and exter-
nal intercostal muscles [11,41,42]. Although sEMG is an easy-to-apply and sensitive tool for
capturing muscle activity, it has some disadvantages, such as susceptibility to interference
from activities in other muscle groups (cross-talk) and limited standardization for analysis and
processing of recorded sEMG signals [43].
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 12 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
This systematic review introduces some limitations that require careful consideration. The
inconsistency of methods and data reports in the included studies restricted the possibility of
conducting meta-analyses. For instance, some studies did not report any effect size measures
with EMG signals, leading to an incomplete data assessment. Another fact is that despite the
joint statement of ATS/ERS in 2002, which one of the goals was to promote standardization of
techniques for assessing respiratory muscle function, including electromyographic methods,
minimal adherence to this guideline was observed in the published studies.
Moreover, there is a lack of comparative evidence for different analysis techniques and
removal strategies of motion artifacts, resulting in uncertainty regarding the best approach for
reliable clinical inferences. Limited number of software is currently available to address the
detection and removal of motion artifacts, and even manual inspection for noises has been
reported. Once adequate signal processing is achieved, further research is needed to study the
incorporation strategies of sEMG into clinical practices, including ICU.
5. Conclusion
The diaphragm and parasternal muscles are the most studied muscles in the cited protocols in
the ICU setting, as well as their electrode placement patterns. There is significant variation in
the methods and tools used for analyzing and processing of respiratory sEMG signals. The use
of RMS appears to be essential in identifying muscle contractility behavior at different settings.
Although clinical studies have provided useful information about the positions and analyses of
respiratory sEMG in the ICU. Further studies are warranted to better explore the muscles
physiological aspects in such a vulnerable population and tailor strategies to increase their
chances of better outcomes.
Supporting information
S1 Appendix. Full search strategy.
(DOCX)
S1 Table. Results of the critical appraisal using the Newcastle-Ottawa scale adapted for
cross-sectional studies.
(DOCX)
S2 Table. Results of the critical appraisal using the The Newcastle-Ottawa scale (NOS) for
case-control study.
(DOCX)
S3 Table. Risk of bias assessment assessed by the Downs and Black.
(DOCX)
S4 Table. PRISMA checklist.
(PDF)
Author Contributions
Conceptualization: Emanuel Fernandes Ferreira da Silva Junior, Shirley Lima Campos, Wag-
ner Souza Leite.
Data curation: Emanuel Fernandes Ferreira da Silva Junior, Wagner Souza Leite.
Formal analysis: Emanuel Fernandes Ferreira da Silva Junior, Wagner Souza Leite, Pedro
Vanderlei de Sousa Melo, Rômulo Aquino Coelho Lins.
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 13 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Funding acquisition: Marcelo Renato Guerino.
Investigation: Emanuel Fernandes Ferreira da Silva Junior, Wagner Souza Leite.
Methodology: Emanuel Fernandes Ferreira da Silva Junior, Wagner Souza Leite.
Project administration: Emanuel Fernandes Ferreira da Silva Junior.
Resources: Emanuel Fernandes Ferreira da Silva Junior, Marcelo Renato Guerino.
Software: Emanuel Fernandes Ferreira da Silva Junior.
Supervision: Shirley Lima Campos, Maria das Graças Rodrigues de Araújo, Marcelo Renato
Guerino.
Validation: Emanuel Fernandes Ferreira da Silva Junior, Shirley Lima Campos, Wagner Souza
Leite, Marcelo Renato Guerino.
Visualization: Emanuel Fernandes Ferreira da Silva Junior, Shirley Lima Campos, Wagner
Souza Leite, Marcelo Renato Guerino.
Writing – original draft: Emanuel Fernandes Ferreira da Silva Junior, Shirley Lima Campos,
Wagner Souza Leite, Rômulo Aquino Coelho Lins.
Writing – review & editing: Emanuel Fernandes Ferreira da Silva Junior, Shirley Lima Cam-
pos, Wagner Souza Leite, Maria das Graças Rodrigues de Araújo, Marcelo Renato Guerino.
References
1. American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle
testing. Am J Respir Crit Care Med. 2002; 166: 518–624. https://doi.org/10.1164/rccm.166.4.518 PMID:
12186831
2. Lai C-C, Tseng K-L, Ho C-H, Chiang S-R, Chen C-M, Chan K-S, et al. Prognosis of patients with acute
respiratory failure and prolonged intensive care unit stay. J Thorac Dis. 2019; 11: 2051–2057. https://
doi.org/10.21037/jtd.2019.04.84 PMID: 31285898
3. Carteaux G, Lyazidi A, Cordoba-Izquierdo A, Vignaux L, Jolliet P, Thille AW, et al. Patient-ventilator
asynchrony during noninvasive ventilation: a bench and clinical study. Chest. 2012; 142: 367–376.
https://doi.org/10.1378/chest.11-2279 PMID: 22406958
4. Karaborklu Argut S, Celik D, Yasacı Z. Effectiveness of therapeutic electromyographic biofeedback
after orthopedic knee surgeries: a systematic review. Disabil Rehabil. 2022; 44: 3364–3372. https://doi.
org/10.1080/09638288.2020.1867904 PMID: 33417500
5. AbuNurah HY, Russell DW, Lowman JD. The validity of surface EMG of extra-diaphragmatic muscles
in assessing respiratory responses during mechanical ventilation: A systematic review. Pulmonology.
2020; 26: 378–385. https://doi.org/10.1016/j.pulmoe.2020.02.008 PMID: 32247711
6. Bellani G, Bronco A, Arrigoni Marocco S, Pozzi M, Sala V, Eronia N, et al. Measurement of Diaphrag-
matic Electrical Activity by Surface Electromyography in Intubated Subjects and Its Relationship With
Inspiratory Effort. Respir Care. 2018; 63: 1341–1349. https://doi.org/10.4187/respcare.06176 PMID:
30389829
7. Duiverman ML, Huberts AS, Bladder G, Wijkstra PJ. Surface respiratory EMG during different settings
of non-invasive ventilation in stable COPD. Eur Respir J. 2016;48. https://doi.org/10.1183/13993003.
congress-2016.OA3530
8. Hogrel J-Y. Clinical applications of surface electromyography in neuromuscular disorders. Neurophysiol
Clin Clin Neurophysiol. 2005; 35: 59–71. https://doi.org/10.1016/j.neucli.2005.03.001 PMID: 16087069
9. Campanini I, Disselhorst-Klug C, Rymer WZ, Merletti R. Surface EMG in Clinical Assessment and Neu-
rorehabilitation: Barriers Limiting Its Use. Front Neurol. 2020; 11. Available: https://www.frontiersin.org/
articles/10.3389/fneur.2020.00934. https://doi.org/10.3389/fneur.2020.00934 PMID: 32982942
10. Hermens HJ, Freriks B, Merletti R, Blok J, Rau G, Hägg G. et al. European recommendations for sur-
face electromyography. Roessingh research and development. 1999; 8: 13–54.
11. Cabral EEA, Fregonezi GAF, Melo L, Basoudan N, Mathur S, Reid WD. Surface electromyography
(sEMG) of extradiaphragm respiratory muscles in healthy subjects: A systematic review. J
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 14 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
Electromyogr Kinesiol Off J Int Soc Electrophysiol Kinesiol. 2018; 42: 123–135. https://doi.org/10.1016/
j.jelekin.2018.07.004 PMID: 30077087
12. Dos Reis IMM, Ohara DG, Januário LB, Basso-Vanelli RP, Oliveira AB, Jamami M. Surface electromy-
ography in inspiratory muscles in adults and elderly individuals: A systematic review. J Electromyogr
Kinesiol Off J Int Soc Electrophysiol Kinesiol. 2019; 44: 139–155. https://doi.org/10.1016/j.jelekin.2019.
01.002 PMID: 30658230
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020
statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372: n71. https://doi.org/
10.1136/bmj.n71 PMID: 33782057
14. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic
reviews. Syst Rev. 2016; 5: 210. https://doi.org/10.1186/s13643-016-0384-4 PMID: 27919275
15. Peterson J, Welch V, Losos M, Tugwell, PJOOHRI. The Newcastle-Ottawa scale (NOS) for assessing
the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute.
2011; 2(1):1–12.
16. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological
quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Com-
munity Health. 1998; 52: 377–384. https://doi.org/10.1136/jech.52.6.377 PMID: 9764259
17. Pozzi M, Rezoagli E, Bronco A, Rabboni F, Grasselli G, Foti G, et al. Accessory and Expiratory Muscles
Activation During Spontaneous Breathing Trial: A Physiological Study by Surface Electromyography.
Front Med. 2022;9. Available: https://www.frontiersin.org/articles/10.3389/fmed.2022.814219.
18. Graßhoff J, Petersen E, Farquharson F, Kustermann M, Kabitz H-J, Rostalski P, et al. Surface EMG-
based quantification of inspiratory effort: a quantitative comparison with Pes. Crit Care. 2021; 25: 441.
https://doi.org/10.1186/s13054-021-03833-w PMID: 34930396
19. Bureau C, Decavèle M, Campion S, Nierat M-C, Mayaux J, Morawiec E, et al. Proportional assist venti-
lation relieves clinically significant dyspnea in critically ill ventilated patients. Ann Intensive Care. 2021;
11: 177. https://doi.org/10.1186/s13613-021-00958-7 PMID: 34919178
20. Lokin JL, Dulger S, Glas GJ, Horn J. Transesophageal Versus Surface Electromyography of the Dia-
phragm in Ventilated Subjects. Respir Care. 2020; 65: 1309–1314. https://doi.org/10.4187/respcare.
07094 PMID: 32234771
21. Roesthuis LH, van der Hoeven JG, van Hees HWH, Schellekens W-JM, Doorduin J, Heunks LMA.
Recruitment pattern of the diaphragm and extradiaphragmatic inspiratory muscles in response to differ-
ent levels of pressure support. Ann Intensive Care. 2020; 10: 67. https://doi.org/10.1186/s13613-020-
00684-6 PMID: 32472272
22. Costa HLL de S, Souza LC de, Neto AE da S, Guimarães BL da S, Azeredo LM de, Godoy MDP, et al.
Involvement of Respiratory Muscles During the Timed Inspiratory Effort Index Measurement With Sur-
face Electromyography. Respir Care. 2020; 65: 1857–1863. https://doi.org/10.4187/respcare.07465
PMID: 32723857
23. Duarte RP, Sentanin AC, da Silva AMO, Tonella RM, Duarte GL, Ratti LSR, et al. Diaphragm Muscle
Surface Electromyography in Patients Submitted to Liver Transplant and Eligible for Extubation. Trans-
plant Proc. 2017; 49: 829–831. https://doi.org/10.1016/j.transproceed.2017.01.059 PMID: 28457405
24. Salazar Sánchez MB, Hernández Valdivieso AM, Mañanas Villanueva MÁ. Assessment of mechani-
cally ventilated patients intoxicated with organophosphates by a novel surface electromyographic
index. J Crit Care. 2017; 41: 260–267. https://doi.org/10.1016/j.jcrc.2017.05.022 PMID: 28599200
25. Ortega ICM, Valdivieso AMH, Lopez JFA, Villanueva MÁM, Lopez LHA. Assessment of weaning
indexes based on diaphragm activity in mechanically ventilated subjects after cardiovascular surgery. A
pilot study. Rev Bras Ter Intensiva. 2017; 29: 213–221. https://doi.org/10.5935/0103-507X.20170030
PMID: 28977261
26. Walterspacher S, Gückler J, Pietsch F, Walker DJ, Kabitz H-J, Dreher M. Activation of respiratory mus-
cles during weaning from mechanical ventilation. J Crit Care. 2017; 38: 202–208. https://doi.org/10.
1016/j.jcrc.2016.11.033 PMID: 27951475
27. Cecchini J, Schmidt M, Demoule A, Similowski T. Increased diaphragmatic contribution to inspiratory
effort during neurally adjusted ventilatory assistance versus pressure support: an electromyographic
study. Anesthesiology. 2014; 121: 1028–1036. https://doi.org/10.1097/ALN.0000000000000432 PMID:
25208082
28. Schmidt M, Kindler F, Gottfried SB, Raux M, Hug F, Similowski T, et al. Dyspnea and surface inspiratory
electromyograms in mechanically ventilated patients. Intensive Care Med. 2013; 39: 1368–1376.
https://doi.org/10.1007/s00134-013-2910-3 PMID: 23575612
29. Tassaux D, Gainnier M, Battisti A, Jolliet P. Impact of expiratory trigger setting on delayed cycling and
inspiratory muscle workload. Am J Respir Crit Care Med. 2005; 172: 1283–1289. https://doi.org/10.
1164/rccm.200407-880OC PMID: 16109983
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 15 / 16
PLOS ONE Surface electromyography of respiratory muscles in the critically ill
30. Tassaux D, Dalmas E, Gratadour P, Jolliet P. Patient-ventilator interactions during partial ventilatory
support: a preliminary study comparing the effects of adaptive support ventilation with synchronized
intermittent mandatory ventilation plus inspiratory pressure support. Crit Care Med. 2002; 30: 801–807.
https://doi.org/10.1097/00003246-200204000-00014 PMID: 11940749
31. Imsand C, Feihl F, Perret C, Fitting JW. Regulation of inspiratory neuromuscular output during synchro-
nized intermittent mechanical ventilation. Anesthesiology. 1994; 80: 13–22. https://doi.org/10.1097/
00000542-199401000-00006 PMID: 8291702
32. Acierno SP D’Ambrosia C, Solomonow M, Baratta RV, D’Ambrosia RD. Electromyography and biome-
chanics of a dynamic knee brace for anterior cruciate ligament deficiency. Orthopedics. 1995; 18:
1101–1107. https://doi.org/10.3928/0147-7447-19951101-11 PMID: 8559695
33. Mohammadi P, Akbari M, Sarrafzadeh J, Moradi Z. Comparison of respiratory muscles activity and
exercise capacity in patients with idiopathic scoliosis and healthy individuals. Physiother Theory Pract.
2014; 30: 552–556. https://doi.org/10.3109/09593985.2014.938382 PMID: 25051355
34. Katayama K, Suzuki Y, Hoshikawa M, Ohya T, Oriishi M, Itoh Y, et al. Hypoxia exaggerates inspiratory
accessory muscle deoxygenation during hyperpnoea. Respir Physiol Neurobiol. 2015; 211: 1–8. https://
doi.org/10.1016/j.resp.2015.02.005 PMID: 25747385
35. Guenette JA, Henderson WR, Dominelli PB, Querido JS, Brasher PM, Griesdale DEG, et al. Blood flow
index using near-infrared spectroscopy and indocyanine green as a minimally invasive tool to assess
respiratory muscle blood flow in humans. Am J Physiol Regul Integr Comp Physiol. 2011; 300: R984–
992. https://doi.org/10.1152/ajpregu.00739.2010 PMID: 21289237
36. Jolley CJ, Luo Y-M, Steier J, Reilly C, Seymour J, Lunt A, et al. Neural respiratory drive in healthy sub-
jects and in COPD. Eur Respir J. 2009; 33: 289–297. https://doi.org/10.1183/09031936.00093408
PMID: 18829678
37. De Troyer A, Legrand A, Gevenois PA, Wilson TA. Mechanical advantage of the human parasternal
intercostal and triangularis sterni muscles. J Physiol. 1998;513 (Pt 3): 915–925. https://doi.org/10.1111/
j.1469-7793.1998.915ba.x PMID: 9824728
38. Tagliabue G, Ji M, Suneby Jagers JV, Lee W, Dean D, Zuege DJ, et al. Limitations of surface EMG esti-
mate of parasternal intercostal to infer neural respiratory drive. Respir Physiol Neurobiol. 2021; 285:
103572. https://doi.org/10.1016/j.resp.2020.103572 PMID: 33161120
39. Gandevia SC, Hudson AL, Gorman RB, Butler JE, De Troyer A. Spatial distribution of inspiratory drive
to the parasternal intercostal muscles in humans. J Physiol. 2006; 573: 263–275. https://doi.org/10.
1113/jphysiol.2005.101915 PMID: 16556657
40. Brochard L, Harf A, Lorino H, Lemaire F. Inspiratory pressure support prevents diaphragmatic fatigue
during weaning from mechanical ventilation. Am Rev Respir Dis. 1989; 139: 513–521. https://doi.org/
10.1164/ajrccm/139.2.513 PMID: 2643905
41. De Troyer A, Estenne M. Functional anatomy of the respiratory muscles. Clin Chest Med. 1988; 9: 175–
193. PMID: 3292122
42. De Troyer A, Estenne M. Coordination between rib cage muscles and diaphragm during quiet breathing
in humans. J Appl Physiol. 1984; 57: 899–906. https://doi.org/10.1152/jappl.1984.57.3.899 PMID:
6238017
43. Caruso P, Albuquerque ALP de, Santana PV, Cardenas LZ, Ferreira JG, Prina E, et al. Diagnostic
methods to assess inspiratory and expiratory muscle strength. J Bras Pneumol. 2015; 41: 110–123.
https://doi.org/10.1590/S1806-37132015000004474 PMID: 25972965
PLOS ONE | https://doi.org/10.1371/journal.pone.0284911 April 27, 2023 16 / 16
You might also like
- CHCECE030 - Student Assessment Task 1 - QuestioningDocument16 pagesCHCECE030 - Student Assessment Task 1 - QuestioningIlhami Nur Rahmat50% (2)
- 3.02 Groundwater Lab ReportDocument2 pages3.02 Groundwater Lab Reportisland67% (3)
- User Manual Infusion Pump S100-200-300Document79 pagesUser Manual Infusion Pump S100-200-300Nicolae Arpentii100% (1)
- Scientific Principles of Strength TrainingDocument38 pagesScientific Principles of Strength Trainingarkko5585% (13)
- Sketchy Pharm (Benzo) ReviewDocument2 pagesSketchy Pharm (Benzo) ReviewMitz JuneNo ratings yet
- Methodology of Surface Electromyography in Gait Analysis: Review of The LiteratureDocument8 pagesMethodology of Surface Electromyography in Gait Analysis: Review of The LiteraturemaketoNo ratings yet
- Urtnasan2018 Article AutomatedDetectionOfObstructivDocument8 pagesUrtnasan2018 Article AutomatedDetectionOfObstructivRayana VieiraNo ratings yet
- HINT - High Level Inferencing Tool: An Expert System For The Interpretation of Neurophysiological StudiesDocument18 pagesHINT - High Level Inferencing Tool: An Expert System For The Interpretation of Neurophysiological StudiesRama BayuNo ratings yet
- TIM.2020 A Sleep Apnea Detection Method Based On Unsupervised Feature Learning and Single-Lead ElectrocardiogramDocument12 pagesTIM.2020 A Sleep Apnea Detection Method Based On Unsupervised Feature Learning and Single-Lead ElectrocardiogramYasrub SiddiquiNo ratings yet
- A Long Short-Term Memory Ensemble Approach For Improving The Output Prediction in ICUDocument11 pagesA Long Short-Term Memory Ensemble Approach For Improving The Output Prediction in ICUIdris RabiuNo ratings yet
- Automatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDocument15 pagesAutomatic Detection of Respiratory Arrests in OSA Patients Using PPG and Machine Learning TechniquesDayana VieiraNo ratings yet
- 2019 - Ers - Ai LFTDocument11 pages2019 - Ers - Ai LFTJohn BlackbNo ratings yet
- Aittokallio, Virkki, Polo - 2009 - Understanding Sleep-Disordered Breathing Through Mathematical ModellingDocument11 pagesAittokallio, Virkki, Polo - 2009 - Understanding Sleep-Disordered Breathing Through Mathematical ModellingFGR2711No ratings yet
- Automatic Home-Based Screening of Obstructive Sleep Apnea Using Single Channel Electrocardiogram and Spo2 SignalsDocument17 pagesAutomatic Home-Based Screening of Obstructive Sleep Apnea Using Single Channel Electrocardiogram and Spo2 SignalsAdam HansenNo ratings yet
- Fmed 10 1174631Document7 pagesFmed 10 1174631Natansa Adi SukmaNo ratings yet
- Research Paper 2017-3Document11 pagesResearch Paper 2017-3Vikas KaushikNo ratings yet
- Casale Chi 2019Document10 pagesCasale Chi 2019Ketlin CastroNo ratings yet
- Autonomic Effects of Spinal Manipulative Therapie Systematic ReviewDocument12 pagesAutonomic Effects of Spinal Manipulative Therapie Systematic ReviewbesombespierreNo ratings yet
- Bio Marcadores en Sarcopenia Calvani2017Document6 pagesBio Marcadores en Sarcopenia Calvani2017JAVIER VELASQUEZ100% (1)
- 3413ijcsa05 PDFDocument13 pages3413ijcsa05 PDFVanathi AndiranNo ratings yet
- Neurofilaments in Progressive Multiple Sclerosis: A Systematic ReviewDocument11 pagesNeurofilaments in Progressive Multiple Sclerosis: A Systematic ReviewAlin CiubotaruNo ratings yet
- The Classification of EEG-based Winking Signals: A Transfer Learning and Random Forest ApproachDocument7 pagesThe Classification of EEG-based Winking Signals: A Transfer Learning and Random Forest ApproachDhruv TNo ratings yet
- Lung Function Parameters of Healthy, Non-Smoking Young People and Employees at Shaqra University, ShaqraDocument6 pagesLung Function Parameters of Healthy, Non-Smoking Young People and Employees at Shaqra University, ShaqrahimayatullahNo ratings yet
- Driver Drowsiness Classification Using Fuzzy Wavelet-Packet-Based Feature-Extraction AlgorithmDocument11 pagesDriver Drowsiness Classification Using Fuzzy Wavelet-Packet-Based Feature-Extraction AlgorithmAlex WongNo ratings yet
- Final SynopsisDocument15 pagesFinal SynopsisgauravchauNo ratings yet
- Ppaer 1Document5 pagesPpaer 1Piyash ApexNo ratings yet
- 10 1002@jcp 28839Document11 pages10 1002@jcp 28839Ahmed SaifNo ratings yet
- Ann ArticleDocument12 pagesAnn ArticleSABARISH VNo ratings yet
- Review Article: Magnetoencephalography: Fundamentals and Established and Emerging Clinical Applications in RadiologyDocument19 pagesReview Article: Magnetoencephalography: Fundamentals and Established and Emerging Clinical Applications in RadiologyThe StreetNo ratings yet
- New Seep Apnea AIDocument15 pagesNew Seep Apnea AIgauravchauNo ratings yet
- Applied Sciences: Special Issue: "Research On Biomedical Signal Processing"Document3 pagesApplied Sciences: Special Issue: "Research On Biomedical Signal Processing"prabhatNo ratings yet
- ERS Statement On Standardisation of Cardiopulmonary Exercise Testing in Chronic Lung DiseasesDocument25 pagesERS Statement On Standardisation of Cardiopulmonary Exercise Testing in Chronic Lung Diseasesnatalia cunha varellaNo ratings yet
- Predicción Longitudinal de La Aptitud Cardiorrespiratoria A Través de Dispositivos Portátiles en Entornos de Vida LibreDocument11 pagesPredicción Longitudinal de La Aptitud Cardiorrespiratoria A Través de Dispositivos Portátiles en Entornos de Vida Libremariojosehurtado3955No ratings yet
- 3 ArticleDocument59 pages3 ArticleAlbert PierssonNo ratings yet
- Osteoarthritis Year in Review 2014: Mechanics e Basic and Clinical Studies in OsteoarthritisDocument14 pagesOsteoarthritis Year in Review 2014: Mechanics e Basic and Clinical Studies in OsteoarthritisFrenkky AlexaNo ratings yet
- SV2021112102Document12 pagesSV2021112102pashaNo ratings yet
- 18iommodelpolicy TRDocument37 pages18iommodelpolicy TRkaysa3No ratings yet
- Whole Body Magnetic Resonance Imaging in InflammatDocument14 pagesWhole Body Magnetic Resonance Imaging in InflammateugeniaNo ratings yet
- UltrassonografiaDocument6 pagesUltrassonografiaLenir LuzNo ratings yet
- PE Como Predictores de Discapacidad en EM - 2012Document5 pagesPE Como Predictores de Discapacidad en EM - 20122j5f2y76g2No ratings yet
- Dario Farina, Luigi Fattorini, Francesco Felici and Giancarlo FilligoiDocument12 pagesDario Farina, Luigi Fattorini, Francesco Felici and Giancarlo FilligoiJen PassilanNo ratings yet
- Impact of Mild To Moderate Exacerbations On OutcomDocument4 pagesImpact of Mild To Moderate Exacerbations On OutcomlalopotNo ratings yet
- Effect of Action Observation Therapy inDocument33 pagesEffect of Action Observation Therapy inseroxat2005No ratings yet
- Detection of Borderline Mental Disorder On Electrocardiosignals Using EMDDocument4 pagesDetection of Borderline Mental Disorder On Electrocardiosignals Using EMDJohnsonNo ratings yet
- The Global Lung Function Initiative - Dispelling Some Myths of Lung Function Test InterpretationDocument13 pagesThe Global Lung Function Initiative - Dispelling Some Myths of Lung Function Test InterpretationUriel ChavarriaNo ratings yet
- JCM 11 03739 v2Document19 pagesJCM 11 03739 v2Edher Benitez PliegoNo ratings yet
- Ijms 13 13894Document17 pagesIjms 13 13894osama mosaNo ratings yet
- Sensors: Physiological Sensor Signals Classification For Healthcare Using Sensor Data Fusion and Case-Based ReasoningDocument16 pagesSensors: Physiological Sensor Signals Classification For Healthcare Using Sensor Data Fusion and Case-Based ReasoningbengheniaNo ratings yet
- Mann Assessment of Swallowing AbilityDocument9 pagesMann Assessment of Swallowing Abilityluca bastianiNo ratings yet
- 10.1007@s00405 016 4015 4Document10 pages10.1007@s00405 016 4015 4Lorena PaulaNo ratings yet
- Position Paper of The EACVI and EANM On Artificial Intelligence Applications in Multimodality Cardiovascular Imaging Using SPECTCT, PETCT, and Cardiac CTDocument15 pagesPosition Paper of The EACVI and EANM On Artificial Intelligence Applications in Multimodality Cardiovascular Imaging Using SPECTCT, PETCT, and Cardiac CTKotolNo ratings yet
- 1 s2.0 S1746809423006924 MainDocument11 pages1 s2.0 S1746809423006924 MainAshish NehraNo ratings yet
- 167 2016 Article 4272Document18 pages167 2016 Article 4272asmaNo ratings yet
- Eus 310Document9 pagesEus 310Fahreza CaesarioNo ratings yet
- Bioinformatics 2021 15Document7 pagesBioinformatics 2021 15AhdiatShinigamiNo ratings yet
- Pruebas de Función Pulmonar en Distrofia Muscular TiposDocument10 pagesPruebas de Función Pulmonar en Distrofia Muscular TiposEzeBorjesNo ratings yet
- Pamj 39 140Document20 pagesPamj 39 140Karen CruzNo ratings yet
- A Mettre Zotero 8Document9 pagesA Mettre Zotero 8Clara ScemamaNo ratings yet
- Ferrario 2006Document7 pagesFerrario 2006yenni anggrainiNo ratings yet
- Cattaneo 2019Document11 pagesCattaneo 2019Rolando Huaman BravoNo ratings yet
- Speech Based Parkinson's Disease Detection Using Machine LearningDocument7 pagesSpeech Based Parkinson's Disease Detection Using Machine LearningIJRASETPublicationsNo ratings yet
- Wearable Sensors For Clinical Applications in Epilepsy, Parkinson's Disease, and Stroke: A Mixed Methods Systematic ReviewDocument13 pagesWearable Sensors For Clinical Applications in Epilepsy, Parkinson's Disease, and Stroke: A Mixed Methods Systematic ReviewMANIMEGALAI M. ECENo ratings yet
- Computer Methods and Programs in Biomedicine: Reza Boostani, Foroozan Karimzadeh, Mohammad NamiDocument15 pagesComputer Methods and Programs in Biomedicine: Reza Boostani, Foroozan Karimzadeh, Mohammad NamiAlanCarrilloNo ratings yet
- Electroestimulacion Funcional INGLESDocument9 pagesElectroestimulacion Funcional INGLESLeticia RiveraNo ratings yet
- 2023 EAACI - Guidelines - Diagnosis - IgE-mediated - Food - AllergyDocument56 pages2023 EAACI - Guidelines - Diagnosis - IgE-mediated - Food - AllergyOlga CîrsteaNo ratings yet
- Urologic ExaminationDocument4 pagesUrologic ExaminationTansanee MalivalayaNo ratings yet
- Sim Tanwar IccDocument1 pageSim Tanwar IccManoj MauryaNo ratings yet
- Deep Breathing Exercises: Procedure AssessmentDocument3 pagesDeep Breathing Exercises: Procedure AssessmentJelly Jia100% (1)
- CASE STUDY - LeadershipDocument3 pagesCASE STUDY - LeadershipJino GamerNo ratings yet
- PE-ZR-DAS-NT-TR-02209: Comments Resolution SheetDocument81 pagesPE-ZR-DAS-NT-TR-02209: Comments Resolution SheetSheik BenasudeenNo ratings yet
- 7Th Grade Persuasive Essay TopicsDocument8 pages7Th Grade Persuasive Essay TopicsapgsrfnbfNo ratings yet
- 2.3 Sources of Health ReportingDocument5 pages2.3 Sources of Health ReportingPela KqbcgrlaNo ratings yet
- A Comparison of Test Retest Reliability and Random Measurement Error of BI and MBI in Patients With Chronic StrokeDocument6 pagesA Comparison of Test Retest Reliability and Random Measurement Error of BI and MBI in Patients With Chronic Strokelolocy LNo ratings yet
- Psikoedukasi Seks Mengenai LGBT Di Sma Muhammadiyah 1 PekanbaruDocument5 pagesPsikoedukasi Seks Mengenai LGBT Di Sma Muhammadiyah 1 PekanbaruAjeng Safitri -No ratings yet
- Grammar Plus - Unit 5Document4 pagesGrammar Plus - Unit 5Franklin Asencio0% (1)
- Method of Statement For Soil Replacement and BackfillingDocument7 pagesMethod of Statement For Soil Replacement and Backfillingmartina magedNo ratings yet
- Hayes.P Et - Al, 2012 - Foot Strike Patterns and Ground Contact Times During High-Calibre Middle-Distance RacesDocument10 pagesHayes.P Et - Al, 2012 - Foot Strike Patterns and Ground Contact Times During High-Calibre Middle-Distance Racesok okNo ratings yet
- Programa de Investigación FormativaDocument28 pagesPrograma de Investigación FormativaYESSAMEN ESTHER COLLANTES TORRESNo ratings yet
- Delta Green - Need To Know (Player Version)Document38 pagesDelta Green - Need To Know (Player Version)Jesse BerenfeldNo ratings yet
- HypospadiasDocument57 pagesHypospadiasTilahun SaolNo ratings yet
- Adha Standards08Document16 pagesAdha Standards08anasofiakNo ratings yet
- Developmental Olympic Lifting CycleDocument16 pagesDevelopmental Olympic Lifting Cyclehanus.milannseznam.czNo ratings yet
- Psychometric Properties of Senior Fitness TestDocument1 pagePsychometric Properties of Senior Fitness TestSrilatha GirishNo ratings yet
- Paper Presentation PDFDocument18 pagesPaper Presentation PDFramneekNo ratings yet
- Mental HelthDocument19 pagesMental Helthjayvee dacubaNo ratings yet
- Bibliotherapy - Definitions, Uses, and Studies by Lindeman & KLing (1968)Document6 pagesBibliotherapy - Definitions, Uses, and Studies by Lindeman & KLing (1968)Fourani HASP0% (1)
- Homeroom Guidance SampleDocument7 pagesHomeroom Guidance SampleAngelyn Lingatong100% (2)
- Double ComparisonDocument3 pagesDouble ComparisonMai PhuongNo ratings yet
- Seizure Case Study Answers 1Document3 pagesSeizure Case Study Answers 1Maica LectanaNo ratings yet