Professional Documents
Culture Documents
Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation
Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation
Uploaded by
pamelaidea0 ratings0% found this document useful (0 votes)
18 views7 pagesOriginal Title
AGE
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
18 views7 pagesAssessment Nursing Diagnosis Planning Intervention Rationale Evaluation
Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation
Uploaded by
pamelaideaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 7
Patient Name: Sr.
Efleda Catipon
Dx: Acute Gastroenteritis
SN: Idea, Pamela A.
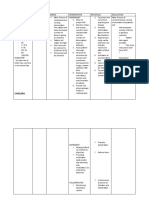
ASSESSMENT NURSING PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective Data: “Deficient Fluid Short Term Independent 1. Gain a good patient- After 8 hours shift,
“Malambot po yung Volume related to Planning: 1. Establish trust and nurse relationship. goal is partially met.
dumi niya at color fluid loss secondary rapport. 2. Establish baseline Patient are able to
yellow” as verbalized to Diarrhea as After 8 hours shift, 2. Assess the vital data observations. bring back his normal
by the patient’s evidenced by dry and the patient will be signs and compare 3. This will provide a pattern of fecal
guardian. flaky skin, poor skin able to achieve it with the normal data that could be elimination and
turgor, yellowish and normal pattern of pattern. used to evaluate the improved her
watery stool” fecal elimination and 3. Assess for the proper intervention hydration status.
exhibit signs of signs of that the client needs.
improvement in dehydration 4. To reduce dryness of
Objective Data: hydration status. including skin the mucosa and
Generalized turgor, oral mucosa, integumentary; and to
weakness etc. prevent dehydration.
Dry and flaky 4. Encourage the 5. To determine if IV fluid
skin client to increase and electrolyte For the long term goal
Pale nail Long Term the fluid intake. replacement are after days of therapy
beds Planning: 5. Monitor I & O and needed. patient are able to
Delayed After days of nursing IV fluids. 6. To promote bring back her
capillary refill intervention, the 6. Provide health awareness on related strength, gained back
Poor skin patient successfully teachings on factors. her normal stool
turgor able to prevent avoidance of 7. To give patient output, color and
Yellow and dehydration due to dehydration. comfort. characteristic. The
watery stool Diarrhea and 7. Provide patient patient is also able to
Impaired Bowel opportunity to rest maintain her hydration
VS Taken as Movements. and calm and safe as evidenced by good
follows 4pm: environment. skin turgor and moist
T: 36.1°C mucosa and skin.
PR: 83 Dependent
RR: 21 8. Based on the result
BP: 100/80 or fecalysis.
8pm: 9. Administer
T: 36.4°C medication
PR: 90 prescribed by the
RR: 22 physician.
BP: 100/80
ASSESSMENT NURSING PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective Data: “Gastrointestinal Short Term Planning: Independent 1. Gain a good After 8 hours shift, goal
“2 weeks na po siyang infection as related to 1. Establish trust patient-nurse is partially met. Patient
nag LBM bago po Diarrhea as evidenced After 8 hours shift, the and rapport. relationship. are able to reduce
maadmit dito by frequent watery patient will be able to 2. Assess the vital 2. Establish fecal elimination, but is
hanggang ngayon po stools” report reduction in signs and baseline data still yellowish in color
madalas pa din po ang frequency of stools. compare it with observations. and watery in
pagdumi niya” as the normal 3. To help characteristics.
verbalized by the pattern. differentiate
patient’s guardian. 3. Observe and individual
record stool disease and
frequency, assesses
characteristics, severity of
Long Term Planning: amount and episode.
After days of nursing precipitating 4. To give patient
Objective Data: intervention, the factors. comfort. After days of therapy,
Generalized patient successfully 4. Provide patient goal is fully met.
weakness able to prevent and opportunity to Patient are able to
Increased achieve normal pattern rest and calm bring back her normal
peristalsis of fecal elimination. and safe fecal elimination, stool
Frequent environment. normal color and
watery stools characteristics.
Dependent
5. Give 5. To gain
VS Taken as follows medications as nursing-patient
4pm: ordered by intervention
T: 36.1°C physician. with rapport to
PR: 83 6. Cooperate with care givers and
RR: 21 the family to to give hope for
BP: 100/80 serve foods better status of
8pm: that can help to health.
T: 36.4°C improve bowel 6. To facilitate
PR: 90 movements of balanced food.
RR: 22 patient.
BP: 100/80
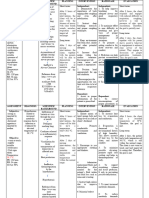
ASSESSMENT NURSING PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective Data: “Risk for Inflammatory Short Term Planning: Independent 1. Gain a good After 8 hours shift, goal
“Minsan nasakit tyan Bowel Disease 1. Establish trust patient-nurse is partially met. Patient
ko tapos minsan secondary to Diarrhea After 8 hours shift, the and rapport. relationship. are able to feel relief
pabalik balik lagnat ko as evidenced by patient will be able to 2. Assess the vital 2. Establish from pain and achieve
o ‘di kaya’y sinat” abdominal cramps” relieve abdominal pain signs and baseline data normal body
and will also be able to compare it with observations. temperature, but it still
return to her normal the normal 3. To give patient may occur.
body temperature. pattern. comfort.
3. Provide patient 4. To promote
opportunity to relaxation and
Objective Data: rest and calm pain reduction.
Generalized and safe
weakness environment.
Guarding 4. Teach patient in
behavior at Long Term Planning: diversionary After days of therapy,
abdomen After days of nursing activities in goal is fully met.
Warm to touch intervention, the easing pain. Patient are able to
patient successfully prevent episodes of
able to prevent abdominal pain and
abdominal pain. The Dependent intermittent fever.
patient will also be
able to prevent Administer and
frequent hyperthermia. prescribed
VS Taken as follows Paracetamol +
4pm: tramadol 1 cap TID
T: 36.4°C PRN x Pain,
PR: 87 Paracetamol 500mg
RR: 21 PRN x Fever
BP: 110/70
Patient
8pm: Name: Sr. Efleda Catipon
Dx:
T: Acute
37.9°C Gastroenteritis
PR: 101
SN: Idea, Pamela A.
RR: 21
BP: 110/70
ASSESSMENT NURSING PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective Data: “Gastrointestinal Short Term Independent 1. Gain a good patient- After 8 hours shift,
“2 weeks na po siyang infection as related to Planning: 1. Establish trust and nurse relationship. goal is partially met.
nag LBM bago po Diarrhea as rapport. 2. Establish baseline Patient are able to
maadmit dito evidenced by After 8 hours shift, 2. Assess the vital data observations. reduce fecal
hanggang ngayon po frequent watery the patient will be signs and compare 3. To help differentiate elimination, but is still
madalas pa din po stools and abdominal able to report it with the normal individual disease and yellowish in color and
ang pagdumi niya” as cramps” reduction in pattern. assesses severity of watery in
verbalized by the frequency of stools. 3. Observe and record episode. characteristics. The
patient’s guardian. The patient will be stool frequency, 4. To promote relaxation patient are also able
able to relieve characteristics, and pain reduction. to feel relief from pain
“Minsan nasakit tyan abdominal pain and amount and 5. To give patient and achieve normal
ko tapos minsan will also be able to precipitating comfort. body temperature, but
pabalik balik lagnat ko return to her normal factors. it still may occur.
o ‘di kaya’y sinat” body temperature. 4. Teach patient in
diversionary
activities in easing
pain.
Objective Data: Long Term 5. Provide patient For the long term goal
Generalized Planning: opportunity to rest after days of therapy
weakness After days of nursing and calm and safe patient are able to
Dry and flaky intervention, the environment. bring back her normal
skin patient successfully fecal elimination, stool
Pale nail beds able to prevent and Dependent normal color and
Delayed achieve normal 6. Cooperate with the 6. To gain nursing-patient characteristics. The
capillary refill pattern of fecal family to serve intervention with rapport to patient are also able
Poor skin elimination. The foods that can help care givers and to give hope to prevent episodes of
turgor patient will also be to improve bowel for better status of health. abdominal pain and
Yellow and able to prevent movements of 7. To facilitate balanced intermittent fever.
watery stool abdominal pain and patient. food.
frequent 7. Administer
VS Taken as follows hyperthermia. medication
4pm: prescribed by the
T: 36.1°C physician.
PR: 83
RR: 21 Administer and prescribed
BP: 100/80 Paracetamol + tramadol 1
8pm: cap TID PRN x Pain,
T: 36.4°C Paracetamol 500mg PRN x
PR: 90 Fever
RR: 22
BP: 100/80
You might also like
- NBME Family Medicine Form 1Document8 pagesNBME Family Medicine Form 1Anna100% (1)
- Childhood and Adolescence: Voyages in Development, 7e: Chapter 7: Infancy: Social andDocument60 pagesChildhood and Adolescence: Voyages in Development, 7e: Chapter 7: Infancy: Social andNUR HUMAIRA ROSLINo ratings yet
- Delivering Better Oral HealthDocument102 pagesDelivering Better Oral Healthsavrasx100% (1)
- Fluid Volume Deficit Related To Nausea and VomitDocument3 pagesFluid Volume Deficit Related To Nausea and VomitJakeNo ratings yet
- Risk NCP - PESCADERO 4CDocument1 pageRisk NCP - PESCADERO 4COrlando VillanuevaNo ratings yet
- JaundiceDocument4 pagesJaundicepamelaideaNo ratings yet
- NCP Deficit Fluid VolumeDocument4 pagesNCP Deficit Fluid VolumeKingJayson Pacman06No ratings yet
- Volume 1Document2 pagesVolume 1roxybiscanteNo ratings yet
- Gastroenteritis NCPDocument6 pagesGastroenteritis NCPKaguraNo ratings yet
- Deficient Fluid Volume (AGEDocument2 pagesDeficient Fluid Volume (AGENursesLabs.com83% (6)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermLorie May GuillangNo ratings yet
- Nursing Care PlansDocument31 pagesNursing Care PlansCyril Jane Caanyagan AcutNo ratings yet
- IndependentDocument2 pagesIndependentR Hornilla ArcegaNo ratings yet
- MS Soapie #1Document2 pagesMS Soapie #1Fatima KateNo ratings yet
- Ate Gabs Nyo Pagod NaDocument3 pagesAte Gabs Nyo Pagod NaGabrielle EvangelistaNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- Name: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralDocument2 pagesName: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralRainier IbarretaNo ratings yet
- Nursing Care Plan, DeficientDocument5 pagesNursing Care Plan, Deficientimee15No ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- HydroceleDocument10 pagesHydroceleRyan ReNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJobelyn TunayNo ratings yet
- Nursing Care Plan - BeDocument6 pagesNursing Care Plan - BeMart UrsuNo ratings yet
- Viernes, Jericho NCP CimcDocument2 pagesViernes, Jericho NCP CimcJayson Respicio jr.No ratings yet
- NCP PediatricDocument5 pagesNCP PediatricSL Hanna NebridaNo ratings yet
- Salva, R.D NCP & Drug Study (Isph - Gs Pediaward)Document7 pagesSalva, R.D NCP & Drug Study (Isph - Gs Pediaward)Rae Dominick Aquino SalvaNo ratings yet
- NCP JaundiceDocument3 pagesNCP JaundiceCamille Joy BaliliNo ratings yet
- Assessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Objective: Sto: DX StoDocument2 pagesAssessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Objective: Sto: DX StoBasema HashhashNo ratings yet
- Patient'S Intials: A.M.B Age: 19 Sex: Male PATIENT'S DIAGNOSIS: AGE (Acute Gastroenteritis)Document1 pagePatient'S Intials: A.M.B Age: 19 Sex: Male PATIENT'S DIAGNOSIS: AGE (Acute Gastroenteritis)Markus Tobias CarreonNo ratings yet
- Nursing Care PlanDocument12 pagesNursing Care Plankeishaaa29100% (6)
- Nursing Care Plan: Cues Nursing Diagnosi S Analysis GOAL and Objectives Intervention Rationale EvaluationDocument5 pagesNursing Care Plan: Cues Nursing Diagnosi S Analysis GOAL and Objectives Intervention Rationale EvaluationMark Allison BuenaventuraNo ratings yet
- NCP MeningitisDocument2 pagesNCP MeningitisARISNo ratings yet
- HYPONATREMIADocument3 pagesHYPONATREMIADienizs Labini TadenaNo ratings yet
- NCP-SUGATON-HYPERTHERMIA IndivdualDocument2 pagesNCP-SUGATON-HYPERTHERMIA IndivdualPrincess Faniega SugatonNo ratings yet
- College of Nursing: University of The EastDocument8 pagesCollege of Nursing: University of The EastroblesNo ratings yet
- Postpartal Discharge InstructionsDocument3 pagesPostpartal Discharge InstructionsDuchess Juliane Jose MirambelNo ratings yet
- Final Nursing Care PlanDocument7 pagesFinal Nursing Care PlanKatherine BellezaNo ratings yet
- JVJV NCP Risk For Fluid Volume DeficitDocument2 pagesJVJV NCP Risk For Fluid Volume DeficitvicenteturasNo ratings yet
- Diabetes Mellitus Nursing Care PlanDocument7 pagesDiabetes Mellitus Nursing Care PlanSheenaGuinoCullaNo ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPjsksNo ratings yet
- Fluid Volume Deficit R/T Diarrhea & VomitingDocument4 pagesFluid Volume Deficit R/T Diarrhea & Vomitingjisoo100% (3)
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- Prado NCPDocument4 pagesPrado NCPalleah pradoNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjective: IndependentDocument2 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjective: IndependentgeorgiaNo ratings yet
- NCP - AgeDocument5 pagesNCP - Ageunsp3akabl386% (7)
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- Facto NCPDocument3 pagesFacto NCPkkd nyleNo ratings yet
- Case Scenario: Dependent/ Independent/ Collaborative RationaleDocument3 pagesCase Scenario: Dependent/ Independent/ Collaborative RationaleRhos Antonette GuimbanNo ratings yet
- NCP 3rd ROTATIONDocument17 pagesNCP 3rd ROTATIONMarie Ashley CasiaNo ratings yet
- Electolyte ImbalanceDocument2 pagesElectolyte ImbalanceFouzia GillNo ratings yet
- Fluid Volume Deficit Related To Loose Watery Stool Diarrhea)Document2 pagesFluid Volume Deficit Related To Loose Watery Stool Diarrhea)Jesse James Advincula Edjec100% (15)
- Short Term: Short TermDocument3 pagesShort Term: Short TermreolalasmjNo ratings yet
- NCP&SOAPIEDocument4 pagesNCP&SOAPIEMica OmotsosircNo ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPJet Ray-Ann GaringanNo ratings yet
- Pedia NCPDocument6 pagesPedia NCPZel MartinezNo ratings yet
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocument11 pagesNursing Care Plan: Cues Objectives Interventions Rationale EvaluationKyla Mae JumaritoNo ratings yet
- NCP Deficient Fluid VolumeDocument3 pagesNCP Deficient Fluid VolumeDoneva Lyn MedinaNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 pagesSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNo ratings yet
- Feedings Down": Subjective Short Term Goal After DX Short Term GoalDocument2 pagesFeedings Down": Subjective Short Term Goal After DX Short Term GoalTeddCamilingNo ratings yet
- Intestinal Failure: Diagnosis, Management and TransplantationFrom EverandIntestinal Failure: Diagnosis, Management and TransplantationAlan LangnasNo ratings yet
- CI ReqDocument5 pagesCI ReqpamelaideaNo ratings yet
- What Is Viral EncephalitisDocument2 pagesWhat Is Viral EncephalitispamelaideaNo ratings yet
- JaundiceDocument4 pagesJaundicepamelaideaNo ratings yet
- Garcia NCPDocument3 pagesGarcia NCPpamelaideaNo ratings yet
- Mechanism of LaborDocument98 pagesMechanism of LaborLaarnee Sinsioco SantosNo ratings yet
- Santrock 0072990597 ch04Document29 pagesSantrock 0072990597 ch04Desi Purnamasari YanwarNo ratings yet
- Job Description: Cardiff and Vale University Health Board Job DetailsDocument9 pagesJob Description: Cardiff and Vale University Health Board Job DetailsmustakNo ratings yet
- Liberty (Art. 21) : ProtectionDocument15 pagesLiberty (Art. 21) : ProtectionA2 Sir Fan PageNo ratings yet
- Adhd Research Paper OutlineDocument8 pagesAdhd Research Paper Outlineh00sprt3100% (1)
- محاضرات تلوث بيئيDocument63 pagesمحاضرات تلوث بيئيمصطفى العباديNo ratings yet
- The Newborn ExaminationDocument132 pagesThe Newborn ExaminationdevilstNo ratings yet
- Employee WelfareDocument12 pagesEmployee WelfareADITYA KHEITAN100% (1)
- Lecture Note For The Course Compasinated Health Ca - 230420 - 003913Document26 pagesLecture Note For The Course Compasinated Health Ca - 230420 - 003913Mandla Hussen100% (4)
- Learning Library PDFDocument65 pagesLearning Library PDFBayu SaksonoNo ratings yet
- Drug Products Renewal of Marketing Authorization (MA) - GCC-1Document2 pagesDrug Products Renewal of Marketing Authorization (MA) - GCC-1harishsushilNo ratings yet
- Pediatric Helpful HintsDocument32 pagesPediatric Helpful Hintspainah sumodiharjoNo ratings yet
- Collaboration Roundtable Partnership ToolkitDocument134 pagesCollaboration Roundtable Partnership ToolkitShirley Saez SesbreñoNo ratings yet
- PEPA SummaryDocument6 pagesPEPA SummaryKhalid Masood GhaniNo ratings yet
- Examples of Blog WritingDocument7 pagesExamples of Blog WritingprimistartNo ratings yet
- Brewin, C. (2014) - Cognitive Foundations of Clinical Psychology PDFDocument229 pagesBrewin, C. (2014) - Cognitive Foundations of Clinical Psychology PDFMarcela Fernanda Guzmán SánchezNo ratings yet
- Requirement Status For Selected Person PATEL ROHITDocument5 pagesRequirement Status For Selected Person PATEL ROHITRohit PatelNo ratings yet
- Benefits of Cupping On Body HealthDocument15 pagesBenefits of Cupping On Body Healthviatul shuknaNo ratings yet
- The Effectiveness of Pre-Operative Deep BreathingDocument5 pagesThe Effectiveness of Pre-Operative Deep BreathingJulenda CintarinovaNo ratings yet
- Official: Á51Ñ Antimicrobial Effectiveness TestingDocument3 pagesOfficial: Á51Ñ Antimicrobial Effectiveness TestingKaren Rojas LópezNo ratings yet
- Branches of PsychologyDocument23 pagesBranches of PsychologyAnonymous g90fKyhP9k100% (1)
- Certified Pharmacovigilance Mohd SaifDocument1 pageCertified Pharmacovigilance Mohd SaifsaifNo ratings yet
- What? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanDocument45 pagesWhat? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanM Rizky Assilmy LubisNo ratings yet
- Human Rights Policy Poster English UsDocument1 pageHuman Rights Policy Poster English UsLahiruNo ratings yet
- Critical Thinking 9-16Document17 pagesCritical Thinking 9-16chelseeNo ratings yet
- Material Safety Data SheetDocument7 pagesMaterial Safety Data SheetSincler Neyra RamosNo ratings yet
- Hygienia EnglishDocument40 pagesHygienia EnglishAsanga MalNo ratings yet