Professional Documents
Culture Documents
โรคกระดูกพรุน (Osteoporosis)
โรคกระดูกพรุน (Osteoporosis)
Uploaded by
037 Onpreeya LansaiCopyright:
Available Formats
You might also like
- Anatomy ราม 2559 & ใบประกอบ 2558-9Document70 pagesAnatomy ราม 2559 & ใบประกอบ 2558-9Zatann Angel100% (1)
- แนวทางการดูแลรักษากลุ่มอาการสูงอายุ 2558Document142 pagesแนวทางการดูแลรักษากลุ่มอาการสูงอายุ 2558THATAPZ0% (1)
- ราชวิถี อาชีวเวชศาสตร์Document36 pagesราชวิถี อาชีวเวชศาสตร์Angela DuangchitNo ratings yet
- โรคมะเร็ง (Cancer)Document36 pagesโรคมะเร็ง (Cancer)HiiNo ratings yet
- หนังสือ คู่มือศึกษาความหลากหลาย เห็ด (Mushrooms) - compressedDocument160 pagesหนังสือ คู่มือศึกษาความหลากหลาย เห็ด (Mushrooms) - compressedAlpameawNo ratings yet
- อุ๋งอิ๋งDocument13 pagesอุ๋งอิ๋งChotika InbutNo ratings yet
- kinnaree chai,+วารสาร+ฉ.3+เรื่องที่+14Document17 pageskinnaree chai,+วารสาร+ฉ.3+เรื่องที่+14Mor OB-GYNNo ratings yet
- การผลิตภาชนะชีวภาพจากผักตบชวาDocument14 pagesการผลิตภาชนะชีวภาพจากผักตบชวาmercurybkkNo ratings yet
- คู่มือสำรวจแมลงDocument100 pagesคู่มือสำรวจแมลงnv5dhbtfcnNo ratings yet
- b7afca163d495614d310e0b9d2feeb6aDocument66 pagesb7afca163d495614d310e0b9d2feeb6aCenny EndearNo ratings yet
- GTE092Document5 pagesGTE092MaxMaximumNo ratings yet
- eauheritagestaff,+##default.groups.name.manager##,+10 วิวรณ์+วงศ์อรุณDocument13 pageseauheritagestaff,+##default.groups.name.manager##,+10 วิวรณ์+วงศ์อรุณsuriyaporn kamonthomNo ratings yet
- (2559) เขตปกครองพิเศษคลองเตยฯDocument34 pages(2559) เขตปกครองพิเศษคลองเตยฯArjin ThongyuukongNo ratings yet
- เล่มปรับพื้นฐานชีววิทยา 64 สมบูรณ์Document26 pagesเล่มปรับพื้นฐานชีววิทยา 64 สมบูรณ์Pigletpooh PoohNo ratings yet
- บ้านครอบครัวไทยร่วมสมัย 2 PDFDocument77 pagesบ้านครอบครัวไทยร่วมสมัย 2 PDFPlakaemNo ratings yet
- WNT Signaling CPEDocument14 pagesWNT Signaling CPEศักดิ์ชัย พูนศรีเจริญกุลNo ratings yet
- 213481911 ซักประวัติได อย างตรงประเด นในเวลาที จำกัดDocument36 pages213481911 ซักประวัติได อย างตรงประเด นในเวลาที จำกัดเกมกวี MedicalStudentNo ratings yet
- filesNameCONTENT1051935443083 PDFDocument8 pagesfilesNameCONTENT1051935443083 PDFfuyuck12345No ratings yet
- ข้อสอบโอเน็ตการงานปี2550Document46 pagesข้อสอบโอเน็ตการงานปี2550Arisara SasomNo ratings yet
- บ้านครอบครัวไทยร่วมสมัย 1Document66 pagesบ้านครอบครัวไทยร่วมสมัย 1PlakaemNo ratings yet
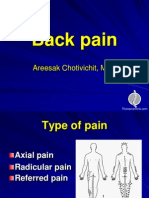
- Back PainDocument54 pagesBack PainthaispineclinicNo ratings yet
- Hip frac มชDocument43 pagesHip frac มชThanawat SimaNo ratings yet
- 2.Cell & Microscope - ของนักเรียน ปี 2566Document17 pages2.Cell & Microscope - ของนักเรียน ปี 2566พศิกาญจน์ ยางสูงNo ratings yet
- Guideline For Management of OA KneeDocument32 pagesGuideline For Management of OA KneeNattawara KampirapawongNo ratings yet
- สไลด์กระดูกพรุน PDFDocument16 pagesสไลด์กระดูกพรุน PDFTrithep PannawatsakunNo ratings yet
- 03 253377 Siravich v4n2Document8 pages03 253377 Siravich v4n2Rapeepan JutananNo ratings yet
- Hip FXDocument16 pagesHip FXVutthivong MnvNo ratings yet
- เฉลยใบงานเคมี 2Document142 pagesเฉลยใบงานเคมี 2ปุณ ปุณณวิชญ์ ก้อนนาคNo ratings yet
- ฟอนต์เส้นประ2แบบภาค3Document10 pagesฟอนต์เส้นประ2แบบภาค3ซาหริม อึนNo ratings yet
- คู่มือการดูแลโรคตาเบื้องต้นDocument54 pagesคู่มือการดูแลโรคตาเบื้องต้นSupalerk Kowinthanaphat50% (4)
- โรคข้อเสื่อมDocument45 pagesโรคข้อเสื่อมHom Jee WonNo ratings yet
- เอกสาร วิทยากรแผนการสอน 63Document34 pagesเอกสาร วิทยากรแผนการสอน 63Nunthawun KhoomthongNo ratings yet
- เอกสาร วิทยากรแผนการสอน 63Document34 pagesเอกสาร วิทยากรแผนการสอน 63Nunthawun KhoomthongNo ratings yet
- บ้านครอบครัวไทยร่วมสมัย 6 PDFDocument68 pagesบ้านครอบครัวไทยร่วมสมัย 6 PDFPlakaemNo ratings yet
- KnowDocument22 pagesKnowแก้มใส GahMzNo ratings yet
- สื่อระบบกระดูกDocument39 pagesสื่อระบบกระดูกSuwapit BoonrangkawNo ratings yet
- d47205cb605b4ba396c42aa52423d2e5Document16 pagesd47205cb605b4ba396c42aa52423d2e5Lala lola 757No ratings yet
- บ้านครอบครัวไทยร่วมสมัย 5 PDFDocument95 pagesบ้านครอบครัวไทยร่วมสมัย 5 PDFPlakaemNo ratings yet
- รพศรพทDocument3 pagesรพศรพทpondchoNo ratings yet
- กล้ามเนื้อ เกณฑ์วินิจฉัยโรคกระดูกกล้ามเนื้อและโครงร่าง PDFDocument34 pagesกล้ามเนื้อ เกณฑ์วินิจฉัยโรคกระดูกกล้ามเนื้อและโครงร่าง PDFNop KongNo ratings yet
- การทดสอบสมรรถภาพทางกายวัยผู้สูงอายุDocument9 pagesการทดสอบสมรรถภาพทางกายวัยผู้สูงอายุคนบางแคร์ แคร์บางคน0% (1)
- TDRG 633 VSup 11 Fin CDocument289 pagesTDRG 633 VSup 11 Fin CmintunlananobgynNo ratings yet
- แผนการออกกำลังกาย นายอดิศร คุตโคสาย Tme2n 623Document7 pagesแผนการออกกำลังกาย นายอดิศร คุตโคสาย Tme2n 623Adisron KhutkhoNo ratings yet
- Thai Guideline Osteoporosis 2021Document26 pagesThai Guideline Osteoporosis 2021Nattawara KampirapawongNo ratings yet
- ตารางสอน ตารางสอบ ตารางคลินิก ปีการศึกษา 2563Document9 pagesตารางสอน ตารางสอบ ตารางคลินิก ปีการศึกษา 2563wits joobNo ratings yet
- Japanese101HD 2022aoysensei (v2) PDFDocument35 pagesJapanese101HD 2022aoysensei (v2) PDFSirawit BumrungsriNo ratings yet
- เวทีเสวนา ร่วมพัฒนาระบบสุขภาพชุมชน ครั้งที่ 7 เรื่อง การจัดการโรคเรื้อรังในชุมชนDocument106 pagesเวทีเสวนา ร่วมพัฒนาระบบสุขภาพชุมชน ครั้งที่ 7 เรื่อง การจัดการโรคเรื้อรังในชุมชนadkittipong100% (1)
- ExampleDocument23 pagesExampleปกป้อง คับNo ratings yet
- ปทรูปสิทธิบาลีDocument492 pagesปทรูปสิทธิบาลีNabhadr BijjayeshbaipoolvangshaNo ratings yet
- ภาวะภูมิคุ้มกันไวเกินจากยาเคมีบำบัดกลุ่มแพลทินัมDocument9 pagesภาวะภูมิคุ้มกันไวเกินจากยาเคมีบำบัดกลุ่มแพลทินัมเด็กชายสมันตภัทร แฟนคลับอาจารย์กวงNo ratings yet
- TDRG 633 VSup 44 Fin CDocument276 pagesTDRG 633 VSup 44 Fin CmintunlananobgynNo ratings yet
- Sheet 2565-2-08-09Document18 pagesSheet 2565-2-08-09Watsana MahasinNo ratings yet
- แนวทางเวชปฏิบัติการดูแลรักษาผู้ป่วยท้องDocument90 pagesแนวทางเวชปฏิบัติการดูแลรักษาผู้ป่วยท้องPasut ChangeNo ratings yet
- คู่มือการปฏิบัติตามมาตรฐานจีเอพี มกษ.7436-2563 สำหรับฟาร์มเลี้ยงสัตว์น้ำเพื่อการบริโภคDocument12 pagesคู่มือการปฏิบัติตามมาตรฐานจีเอพี มกษ.7436-2563 สำหรับฟาร์มเลี้ยงสัตว์น้ำเพื่อการบริโภคStuart GlasfachbergNo ratings yet
- Md 306 สมถกัมมัฏฐาน 40 วิธีDocument156 pagesMd 306 สมถกัมมัฏฐาน 40 วิธีSutus AramrattanaNo ratings yet
- อจท แบบวัดฯคณิตศาสตร์ม 3Document24 pagesอจท แบบวัดฯคณิตศาสตร์ม 3PraeMaiSamart73% (11)
- ฟอมเคส Stady เลือกสรร22Document90 pagesฟอมเคส Stady เลือกสรร22ketsara95302No ratings yet
โรคกระดูกพรุน (Osteoporosis)
โรคกระดูกพรุน (Osteoporosis)
Uploaded by
037 Onpreeya LansaiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
โรคกระดูกพรุน (Osteoporosis)
โรคกระดูกพรุน (Osteoporosis)
Uploaded by
037 Onpreeya LansaiCopyright:
Available Formats
โรคกระดูกพรุน (Osteoporosis) 17-A
โรคกระดูกพรุน (Osteoporosis)
นพ.วีระ สถิรอังกูร
นพ.ชัยวัฒน ปยะสกุลแกว
นพ.ชวนนท สุมนะเศรษฐกุล
นพ.วิชาญ กาญจนถวัลย
นพ.ปฤศนัย พฤฒิกุล
17
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
โรคกระดูกพรุน (Osteoporosis) 17-1
โรคกระดูกพรุน (Osteoporosis)
นพ.วีระ สถิรอังกูร* นพ.ชัยวัฒน ปยะสกุลแกว*
นพ.ชวนนท สุมนะเศรษฐกุล* นพ.วิชาญ กาญจนถวัลย*
นพ.ปฤศนัย พฤฒิกุล*
ēøÙÖøąéĎÖóøčî ÙČĂ ēøÙìĊęöĊÙüćöĒ×ĘÜĒÖøŠÜ×ĂÜÖøąéĎÖ (bone strength) úéúÜ ÿŠÜñúĔĀšöĊÙüćöđÿĊę÷ÜêŠĂÖøąéĎÖĀĆÖ
ÿĎÜ×ċĚîêćöîĉ÷ćö×ĂÜ National Institute of Health ×ĂÜÿĀøĆåĂđöøĉÖć ĔîðŘ 25431 ÙüćöĒ×ĘÜĒÖøŠÜ×ĂÜÖøąéĎÖðøąÖĂïéšü÷
2 ÿŠüîĀúĆÖ ÙČĂ ÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ (bone density) ĒúąÙčèõćó×ĂÜÖøąéĎÖ (bone quality)2 ÿŠüîĂÜÙŤÖćøĂîćöĆ÷
ēúÖ3 ĕéšĔĀšÙĞćîĉ÷ćöĕüšüŠć “đðŨîēøÙÖøąéĎÖìĊęđÖĉé×ċĚîìĆęüøŠćÜÖć÷ (systemic skeletal disease) àċęÜöĊöüúÖøąéĎÖêęĞć (low bone
mass) øŠüöÖĆïÖćøđÿČęĂö×ĂÜēÙøÜÿćøøąéĆïÝčúõćó×ĂÜÖøąéĎÖ (micro architecture deterioration) ÿŠÜñúĔĀšÖøąéĎÖöĊÙüćö
đðøćąïćÜĒúąĀĆÖÜŠć÷” ĒúąĕéšÖĞćĀîéđÖèæŤĔîÖćøüĉîĉÝÞĆ÷ēé÷ĂćýĆ÷ÖćøêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖēé÷ĔĀšÖćøüĉîĉÝÞĆ÷ēøÙ
ÖøąéĎÖóøčîđöČęĂöĊÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖêęĞćÖüŠć -2.5 ×ĂÜÿŠüîđïĊę÷Üđïîöćêøåćî (T-score Œ -2.5) đöČęĂđðøĊ÷ïđìĊ÷ïÖĆï
ÙŠćđÞúĊę÷ĒúąÿŠüîđïĊę÷Üđïîöćêøåćî×ĂÜöüúÖøąéĎÖĔîüĆ÷ÿćüàċęÜëČĂüŠćđðŨîߊüÜìĊęöĊöüúÖøąéĎÖÿĎÜÿčé (êćøćÜìĊę 17.1)
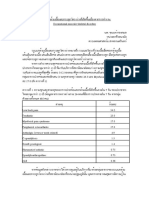
êćøćÜìĊę 17.1 ÖćøüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčîêćöÙüćöĀîćĒîŠîÖøąéĎÖ3
ðÖêĉ (normal) ÙüćöĀîćĒîŠîÖøąéĎÖĂ÷ĎŠĔîđÖèæŤðÖêĉ ÙČĂöĊÙŠćöćÖÖüŠćĀøČĂđìŠćÖĆï -1 ÿŠüîđïĊę÷Üđïî
öćêøåćîđöČęĂđðøĊ÷ïđìĊ÷ïÖĆïÙŠćđÞúĊę÷öüúÖøąéĎÖÿĎÜÿčéĔîñĎšĀâĉÜüĆ÷ÿćü (T-score œ -1)
ÖøąéĎÖïćÜ (osteopenia) ÙüćöĀîćĒîŠîÖøąéĎÖĂ÷ĎŠĔîđÖèæŤêęĞćÖüŠć -1 ÿŠüîđïĊę÷ÜđïîöćêøåćîĒêŠöćÖÖüŠć -2.5
đöČęĂđðøĊ÷ïđìĊ÷ïÖĆïÙŠćđÞúĊę÷öüúÖøąéĎÖÿĎÜÿčéĔîñĎšĀâĉÜüĆ÷ÿćü (-2.5 > T-score -1)
ÖøąéĎÖóøčî (osteoporosis) ÙüćöĀîćĒîŠîÖøąéĎÖêęĞćÖüŠćĀøČĂđìŠćÖĆï -2.5 ÿŠüîđïĊę÷ÜđïîöćêøåćîđöČęĂđðøĊ÷ïđìĊ÷ï
ÖĆïÙŠćđÞúĊę÷öüúÖøąéĎÖÿĎÜÿčéĔîñĎšĀâĉÜüĆ÷ÿćü (T-score Œ -2.5)
ÖøąéĎÖóøčîøąéĆïøčîĒøÜ ÙüćöĀîćĒîŠîÖøąéĎÖêęĞćÖüŠćĀøČĂđìŠćÖĆï -2.5 ÿŠüîđïĊę÷ÜđïîöćêøåćîđöČęĂđðøĊ÷ïđìĊ÷ï
(severe/established ÖĆïÙŠćđÞúĊę÷öüúÖøąéĎÖÿĎÜÿčéĔîñĎšĀâĉÜüĆ÷ÿćü (T-score Œ -2.5)
osteoporosis) øŠüöÖĆïöĊÖøąéĎÖĀĆÖÝćÖÙüćöđðøćąïćÜ (fragility fracture)
ēøÙÖøąéĎÖóøčîđðŨîðŦâĀćìćÜÿćíćøèÿč×ìĊęöĊĒîüēîšöÿĎÜĔîìčÖõĎöĉõćÙ×ĂÜēúÖøüöìĆĚÜðøąđìýĕì÷ ēøÙÖøąéĎÖóøčî
ÝąìĞ ć ĔĀš ñĎš ðś ü ÷ÖøąéĎ Ö ĀĆ Ö ĕéš ÜŠ ć ÷ îĞ ć öćàċę Ü õćüąìč ó óúõćóìĞ ć ĔĀš ĕ öŠ ÿ ćöćøëÖúĆ ï ĕðéĞ ć øÜßĊ üĉ ê ĕéš ð Öêĉ ĒúąĂćÝđÖĉ é
õćüąĒìøÖàšĂîìĞćĔĀšđÿĊ÷ßĊüĉêĕéš ÝćÖÖćøÿĞćøüÝðŦâĀćÿč×õćó×ĂÜñĎšÿĎÜĂć÷čĕì÷ìĊęñŠćîēé÷ÿĞćîĆÖÜćîÿëĉêĉĒĀŠÜßćêĉ óïüŠćðŦâĀć
ìĊęÿĞćÙĆâĂĆîéĆïêšîė ÝąđÖĊę÷üךĂÜÖĆïøąïïÖøąéĎÖĒúąÖúšćöđîČĚĂ
ēøÙÖøąéĎÖóøčîđðŨîēøÙđøČĚĂøĆÜìĊęöĊĒîüēîšöđóĉęöÿĎÜ×ċĚî đîČęĂÜÝćÖðøąßćÖøñĎšÿĎÜĂć÷čđóĉęöÿĎÜ×ċĚî îĂÖÝćÖîĊĚÖćøđÖĉé
ÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčîÝąÿŠÜñúĔĀšĂĆêøćÖćøêć÷đóĉęööćÖ×ċĚîĂ÷ŠćÜöćÖ ÝćÖÖćøýċÖþćĂĆêøćêć÷õć÷ĀúĆÜÖøąéĎÖÿąēóÖìĊę
ÝĆÜĀüĆéđßĊ÷ÜĔĀöŠ ĔîðŘ 1997-1998 óïüŠćøšĂ÷úą 2.1 đÿĊ÷ßĊüĉêøąĀüŠćÜđךćøĆïÖćøøĆÖþćĔîēøÜó÷ćïćú ĂĆêøćêć÷ĀúĆÜÝćÖ
ÖøąéĎÖÿąēóÖĀĆÖìĊę 3 đéČĂî, 6 đéČĂî Ēúą 1 ðŘ đìŠćÖĆïøšĂ÷úą 9.0, 12.0 Ēúą 17.0 êćöúĞćéĆï ÝćÖÖćøýċÖþćēé÷êĉéêćöđðŨî
øą÷ą 5 ðŘ4 óïüŠćĂĆêøćêć÷Ă÷ĎŠìĊęøšĂ÷úą 29.0 ĒúąÖćøýċÖþć×ĂÜ Jitapunkul ðŘ 1995-19975 óïüŠćñĎšĀâĉÜĂć÷č 50 ðŘ ìĊęöĊ
ÖøąéĎÖÿąēóÖĀĆÖöĊĂĆêøćêć÷öćÖÖüŠćüĆ÷đéĊ÷üÖĆîìĊęĕöŠöĊÖøąéĎÖÿąēóÖĀĆÖ îĂÖÝćÖîĊĚ Chariyalertsak ĔîðŘ 1997-19986 ýċÖþć
óïüŠćĂĆêøćêć÷ĔîñĎšßć÷ìĊęđÖĉéÖøąéĎÖÿąēóÖĀĆÖÝąÿĎÜÖüŠćñĎšĀâĉÜ ĒúąñĎšìĊęĕéšøĆïÖćøøĆÖþćĒïïðøąÙĆïðøąÙĂÜÝąöĊĂĆêøćêć÷
öćÖÖüŠćñĎšìĊęĕéšøĆïÖćøøĆÖþćéšü÷ÖćøñŠćêĆé 2 đìŠć
ÖćøýċÖþćÙčèõćóßĊüĉêõć÷ĀúĆÜđÖĉéÖøąéĎÖĀĆÖĔîÙîĕì÷óïüŠćúéúÜĂ÷ŠćÜßĆéđÝî ñĎšðśü÷ìĊęđÖĉéÖøąéĎÖÿąēóÖĀĆÖ
17
óïüŠćøšĂ÷úą 22.1 ×ĂÜñĎšðśü÷ĕöŠÿćöćøëđéĉîĕéš øšĂ÷úą 23.2 êšĂÜĔßšøëđ×Ęî øšĂ÷úą11.2 êšĂÜöĊÙîߊü÷ĔîÖćøđÙúČęĂî÷šć÷7
Pongchaiyakul8 ĕéšĔßšĒïïÿĞćøüÝÿč×õćó SF-36 óïüŠćÙčèõćóßĊüĉê×ĂÜñĎšðśü÷ÖøąéĎÖÿąēóÖĀĆÖēé÷øüöúéúÜøšĂ÷úą 60.0
ĒúąöĊîšĂ÷ÖüŠćøšĂ÷úą 5.0 ìĊęÖúĆïĕðöĊÿč×õćóĒ×ĘÜĒøÜđĀöČĂîđéĉö
*ēøÜó÷ćïćúđúĉéÿĉî
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-2 โรคกระดูกพรุน (Osteoporosis)
øąïćéüĉì÷ć (Epidemiology)
ÿćđĀêč×ĂÜÖćøđÖĉéēøÙ (Cause)
ēøÙÖøąéĎÖóøčî ÙČĂ ēøÙ×ĂÜÖøąéĎÖìĊęöĊÙüćöĒ×ĘÜĒÖøŠÜ×ĂÜÖøąéĎÖúéúÜ öĊ 2 ÿćđĀêčĀúĆÖĔĀâŠė ÙČĂ ðøĉöćèöüú
ÖøąéĎÖìĊęÿąÿöĕüšöĊîšĂ÷ÖüŠćìĊęÙüøÝąđðŨî (peak bone mass) ĀøČĂöĊÖćøÿúć÷ÖøąéĎÖöćÖÖüŠćðÖêĉ ĔîߊüÜĂć÷č 40-45 ðŘ Ýą
đøĉęööĊÖ ćøÿúć÷ÖøąéĎÖ öćÖÖüŠ ć Öćøÿøšć ÜÖøąéĎÖ ìĞć ĔĀš öüúÖøąéĎ Öđøĉęö úéúÜĔîĂĆê øćßšć ė ĒêŠĀ úĆÜ ÝćÖñĎšĀâĉ Ü đך ć üĆ÷Āöé
ðøąÝĞćđéČĂî ĂĆêøćÖćøÿúć÷ÖøąéĎÖÝąÿĎÜ×ċĚîĂ÷ŠćÜöćÖ ìĞćĔĀšöüúÖøąéĎÖúéúÜêęĞćÝîëċÜđÖèæŤìĊęìĞćĔĀšÙüćöđÿĊę÷ÜêŠĂÖøąéĎÖĀĆÖ
đóĉęööćÖ×ċĚî
ðŦÝÝĆ÷ìĊęđÖĊę÷üךĂÜÖĆïÖćøđÖĉéēøÙ (Risk factor)
ðŦÝÝĆ÷đÿĊę÷ÜìĊęĕöŠÿćöćøëðøĆïđðúĊę÷îĕéš (non-modifiable risk factors)
1. Ăć÷čêĚÜĆ ĒêŠ 65 ðŘ×ċĚîĕð
2. đóýĀâĉÜ
3. ßîßćêĉñĉü×ćüĒúąđĀúČĂÜ9
4. ĀöéðøąÝĞćđéČĂîÖŠĂîĂć÷č 45 ðŘ øüöìĆĚÜñĎšìĊęëĎÖêĆéøĆÜĕ׊ÿĂÜךćÜÖŠĂîĀöéðøąÝĞćđéČĂî (early menopause)
5. ēÙøÜÿøšćÜ×ĂÜøŠćÜÖć÷đúĘÖ (small body build)
6. ïĉéć öćøéć óĊęîšĂÜđðŨîēøÙÖøąéĎÖóøčîĀøČĂÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî
7. ÖøąéĎÖĀĆÖÝćÖõćüąÖøąéĎÖđðøćąïćÜ (fragility fracture)
ðŦÝÝĆ÷đÿĊę÷ÜìĊęðøĆïđðúĊę÷îĕéš (modifiable risk factors)
1. ïøĉēõÙĒÙúđàĊ÷öĕöŠóĂđóĊ÷Ü (inadequate calcium intake)
2. ĕöŠÙŠĂ÷ĕéšĔßšĒøÜÖć÷ (sedentary lifestyle)10
3. ÿĎïïčĀøĊęđðŨîðøąÝĞć
4. éČęöÿčøć/ÖćĒôđÖĉî×îćéđðŨîðøąÝĞć
5. éĆßîĊöüúÖć÷êęĞćÖüŠć 19 ÖÖ./êø.ö.
6. öĊõćüą×ćéăĂøŤēöîđĂÿēêøđÝîÖŠĂîđךćÿĎŠüĆ÷ĀöéðøąÝĞćđéČĂî
7. öĊÙüćöđÿĊę÷ÜêŠĂÖćøĀÖúšö (propensity to falls)
ĔîðøąđìýÿĀøĆåĂđöøĉÖćðŘ 1993 öĊñĎšìĊęđÖĉéõćüąÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî (osteoporotic fractures)
öćÖÖüŠć 1.3 úšćîÙøĆĚÜĔîĒêŠúąðŘ ēé÷óïüŠćøšĂ÷úą 50.0 đÖĉéìĊęÖøąéĎÖÿĆîĀúĆÜ (vertebral fractures) øšĂ÷úą 25.0 đÖĉéìĊę
ÖøąéĎÖÿąēóÖ (hip fractures) ĒúąøšĂ÷úą 25.0 đÖĉéìĊęÖøąéĎÖðúć÷Ē×î (Colles’ fractures) ÿĞćĀøĆïÙüćößčÖ×ĂÜēøÙ
ÖøąéĎÖóøčîöĊøć÷ÜćîüŠć ÖüŠćøšĂ÷úą 30.0 ×ĂÜÿêøĊĔîìüĊð÷čēøðìĊęöĊĂć÷čêĆĚÜĒêŠ 50 ðŘ×ċĚîĕðÝąđðŨîēøÙÖøąéĎÖóøčî11
Ĕîðøąđìýĕì÷öĊÖćøÿĞćøüÝÙüćößčÖ×ĂÜēøÙÖøąéĎÖóøčîĔîñĎšìĊęöćøĆïïøĉÖćøĔîēøÜó÷ćïćú×ĂÜøĆåïćÜĒĀŠÜ ĒúąÝćÖ
ÖćøÿčŠöêøüÝÿêøĊĔîßčößîÝćÖìĆęüìčÖõćÙ×ĂÜðøąđìýĔîðŘ 254112 Ēúą 254413 êćöúĞćéĆï óïüŠćøšĂ÷úą 19.0-21.0 ×ĂÜÿêøĊ
ìĊęöĊĂć÷čêĆĚÜĒêŠ 40 ðŘ×ċĚîĕð đðŨîēøÙÖøąéĎÖóøčî×ĂÜÖøąéĎÖÿĆîĀúĆÜÿŠüîđĂü (lumbar spine, L1-L4) ĒúąøšĂ÷úą 11.0-13.0
đðŨîēøÙÖøąéĎÖóøčî×ĂÜÖøąéĎÖÙĂÿąēóÖ (femoral neck osteoporosis)
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-3
êćøćÜìĊę 17.2 ÙüćößčÖ×ĂÜÖøąéĎÖïćÜĒúąēøÙÖøąéĎÖóøčîĔîñĎšĀâĉÜĕì÷ ðŘ 254413
ÖøąéĎÖÿĆîĀúĆÜÿŠüîđĂüøąéĆïìĊę 1-4 ÖøąéĎÖÙĂÿąēóÖ
Ăć÷č ÖøąéĎÖïćÜ ÖøąéĎÖóøčî ÖøąéĎÖïćÜ ÖøąéĎÖóøčî
(øšĂ÷úą) (øšĂ÷úą) (øšĂ÷úą) (øšĂ÷úą)
40-44 14.1 1.7 24.0 0.4
45-49 19.2 4.0 25.0 1.6
50-54 35.5 9.4 38.0 4.9
55-59 38.0 22.6 47.0 10.3
60-64 37.3 39.4 57.0 20.1
65-69 41.7 40.8 58.0 32.6
70-74 28.2 57.7 48.0 49.6
75 ðŘ×Ěîċ ĕð 28.0 59.6 34.0 59.2
ÿĞćĀøĆïĂčïĆêĉÖćøèŤ×ĂÜÿąēóÖĀĆÖ (hip fractures) Ĕîðøąđìýĕì÷öĊøć÷ÜćîÝćÖÖćøÿĞćøüÝìĊęÝĆÜĀüĆéđßĊ÷ÜĔĀöŠ
øąĀüŠćÜðŘ 2540-254114 óïĂčïĆêĉÖćøèŤ×ĂÜÖøąéĎÖÿąēóÖĀĆÖĔîðøąßćÖøìĆĚÜßć÷ĒúąĀâĉÜìĊęöĊĂć÷čêĆĚÜĒêŠ 50 ðŘ×ċĚîĕð ÝĞćîüî
162 ÙøĆĚÜêŠĂ 100,000 ðøąßćÖøêŠĂðŘ ĒêŠÝąđóĉęö×ċĚîđðŨî 851 ÙøĆĚÜĔîðøąßćÖøìĊęĂć÷čđÖĉî 75 ðŘ×ċĚîĕð ĒêŠđöČęĂóĉÝćøèćđÞóćąĔî
ðøąßćÖøđóýĀâĉÜÝąóïĂčïĆêĉÖćøèŤ×ĂÜÖøąéĎÖÿąēóÖĀĆÖ 289 ÙøĆĚÜêŠĂðŘĔîĀâĉÜìĊęĂć÷čđÖĉî 50 ðŘ×ċĚîĕð ĒúąÝąđóĉęö×ċĚîđðŨî
1,011 ÙøĆĚÜëšćĂć÷čđÖĉî 75 ðŘ Öćøđóĉęö×ċĚî×ĂÜēøÙÖøąéĎÖóøčîĒúąÖøąéĎÖĀĆÖÿŠüîĀîċęÜđßČęĂüŠćđðŨîñúöćÝćÖĂć÷č×Ć÷ìĊęđóĉęö×ċĚî éĆÜìĊę
óïüŠćĂć÷č×Ć÷đÞúĊę÷×ĂÜðøąßćÖøēúÖĕéšđóĉęö×ċĚîÝćÖ 45.1 ðŘĔîßć÷ Ēúą 47.8 ðŘĔîĀâĉÜøąĀüŠćÜðŘ 2493-2498 đðŨî 65.1 ðŘĔî
ßć÷ Ēúą 69.3 ðŘĔîĀâĉÜøąĀüŠćÜðŘ 2543-254815 đߊîđéĊ÷üÖĆïĔîðøąđìýĕì÷ìĊęóïüŠćĂć÷č×Ć÷đÞúĊę÷×ĂÜðøąßćÖøĕì÷ĕéšđóĉęö
ÝćÖ 62 ðŘĔîßć÷ Ēúą 68 ðŘĔîĀâĉÜøąĀüŠćÜðŘ 2523-252816 đðŨî 68 ðŘĔîßć÷ Ēúą 72 ðŘĔîĀâĉÜøąĀüŠćÜðŘ 2543-2548 Ēúą
đðŨî 69.5 ðŘĔîßć÷ Ēúą 76.3 ðŘĔîĀâĉÜ ĔîðŘ 2551 ìĆĚÜîĊĚđîČęĂÜÝćÖõć÷ĀúĆÜöüúÖøąéĎÖđóĉęö×ċĚîÿĎÜÿčéĒúšü (peak bone mass)
ÝąđðŨîøą÷ąìĊęđøĉęööĊÖćøÿĎâđÿĊ÷öüúÖøąéĎÖĂ÷ŠćÜÙŠĂ÷đðŨîÙŠĂ÷ĕð ēé÷óïüŠćĔîÿêøĊĕì÷öüúÖøąéĎÖÝąđóĉęöÿĎÜÿčéĂć÷čøąĀüŠćÜ 30-
34 ðŘ ĂĆêøćÖćøÿĎâđÿĊ÷ÖøąéĎÖÝąđóĉęö×ċĚîĂ÷ŠćÜøüéđøĘüĔîÿêøĊđöČęĂđךćÿĎŠüĆ÷ĀöéðøąÝĞćđéČĂî ēé÷đÞóćąõć÷Ĕî 5 ðŘĒøÖ×ĂÜÖćø
ĀöéðøąÝĞćđéČĂî
đÙøČęĂÜßĊĚüĆéõćøąēøÙ (Burden of Disease)
ēé÷ìĆęüĕðēøÙÖøąéĎÖóøčîđðŨîēøÙìĊęĕöŠöĊĂćÖćøĔéė ĒêŠñúìĊęêćööćĀøČĂ clinical consequence ìĊęÿĞćÙĆâ×ĂÜēøÙîĊĚ
ÙČĂ ÖćøđÖĉéÖøąéĎÖĀĆÖĕéšÜŠć÷ àċęÜĒïŠÜĂĂÖĕéšđðŨî 2 ÖøèĊ ÙČĂ
1) ÖøąéĎÖĀĆÖÝćÖõ÷Ćîêøć÷ĒïïĕöŠøčîĒøÜ (low-energy trauma) đߊî ÖøąéĎÖÿąēóÖĀĆÖÝćÖÖćøĀÖúšö
ÝćÖìŠć÷Čî ĀøČĂêÖÝćÖìĊęÿĎÜĔîøąéĆïĔÖúšđÙĊ÷ÜÖĆïÖćøúšöÝćÖìŠć÷Čî đðŨîêšî
2) ÖøąéĎÖĀĆÖēé÷ĕöŠöĊĒøÜÖøąĒìÖÝćÖõć÷îĂÖ đߊî ÖøąéĎÖÿĆîĀúĆÜĀĆÖÝćÖÖćøÖšöêĆü ĀøČĂÖćø÷Ö×ĂÜ
ĀîĆÖ đðŨîêšî
ÖøąéĎÖĀĆÖđĀúŠćîĊĚÝąđøĊ÷Öøüöė üŠć ÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî ĀøČĂ osteoporotic fractures ìĊęđðŨîñúúĆóíŤ
ĀúĆÖìĊęđÖĉé×ċĚîÝćÖÖćøìĊęÖøąéĎÖÿĎâđÿĊ÷ÙüćöĒ×ĘÜĒÖøŠÜĕð àċęÜÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčîîĊĚđĂÜìĊęđðŨîêĆüÖŠĂĔĀšđÖĉéõćøąĒúą
ñúÖøąìïêćööć
ĂĆêøćêć÷ĒúąóĉÖćøÝćÖÖćøđÖĉéÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî (osteoporosis related mortality and
morbidity)
1. ÖćøđÖĉéÖøąéĎÖÿĆîĀúĆÜĀĆÖÝćÖēøÙÖøąéĎÖóøčî (osteoporotic vertebral fractures) ÝąđÖĉéÝćÖÖćø
ìĞćÜćîêćöðÖêĉĀøČĂÖĉÝüĆêøðøąÝĞćüĆî ēé÷ÿŠüîöćÖÝąĕöŠöĊðøąüĆêĉĕéšøĆïĂčïĆêĉđĀêčĔéė ÝċÜđðŨîđĀêčñúüŠćöĊđóĊ÷Ü øšĂ÷úą 40.0 ×ĂÜ 17
ñĎšĀâĉÜìĊęöĊÖøąéĎÖÿĆîĀúĆÜĀĆÖđĀúŠćîĊĚđìŠćîĆĚîìĊęøĎšêĆüüŠćđðŨî
2. ÖøąéĎÖĀúĆÜĀĆÖÝćÖēøÙÖøąéĎÖóøčî ĂćÝÝąöĊĂćÖćøđóĊ÷ÜĒÙŠðüéđúĘÖîšĂ÷ĕðÝîëċÜðüéöćÖÝîêšĂÜîĂî
ēøÜó÷ćïćú ĒêŠēé÷ìĆęüĕðñĎšìĊęöĊÖøąéĎÖÿĆîĀúĆÜĀĆÖÝćÖēøÙÖøąéĎÖóøčîÝąöĊĂĆêøćÖćøđÝĘïðśü÷ (morbidity)17 ĒúąĂĆêøćêć÷
(mortality) öćÖÖüŠćñĎšìĊę÷ĆÜĕöŠöĊÖøąéĎÖĀĆÖĂ÷ŠćÜßĆéđÝî18ñĎšðśü÷ÝąöĊĂćÖćøðüéĀúĆÜđøČĚĂøĆÜ êĆüđêĊĚ÷úÜ (height loss) ĀúĆÜÙŠĂö
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-4 โรคกระดูกพรุน (Osteoporosis)
(kyphosis) ĀúĆÜÙé (scoliosis) ìšĂÜĂČé đïČęĂĂćĀćø đîČęĂÜÝćÖÙüćöÝčߊĂÜìšĂÜúéúÜ ĒúąĂćÝÝąöĊĂćÖćøðüéđĂüđîČęĂÜÝćÖ
ÖøąéĎÖßć÷ēÙøÜúÜöćÖøąìïÖĆïÖøąéĎÖđßĉÜÖøćî
3. ÖćøÿĎâđÿĊ÷ÙüćöÿćöćøëĔîÖćøìĞćÖĉÝüĆêøðøąÝĞćüĆî (functional disability) ÖćøöĊÝĞćîüîðúšĂÜךĂ
ÖøąéĎÖÿĆîĀúĆÜìĊęĀĆÖĀúć÷ðúšĂÜ ÷ĉęÜĀĆÖöćÖđìŠćĕøÝą÷ĉęÜđóĉęöĂĆêøćÖćøđÝĘïðśü÷ ĒúąĂĆêøćêć÷öćÖ×ċĚîđìŠćîĆĚî Ēúą÷ĆÜđóĉęöÙüćö
đÿĊę÷ÜìĊęÝąđÖĉéÖøąéĎÖĀúĆÜĀĆÖĔîðúšĂÜìĊęđĀúČĂ ĒúąÖøąéĎÖÿąēóÖĀĆÖéšü÷19
4. ÖøąéĎÖÿąēóÖĀĆÖ (hip fractures) đðŨîÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčîìĊęöĊðŦâĀćöćÖìĊęÿčé îĂÖÝćÖÝą
öĊĂĆêøćêć÷ìĊęÿĎÜöćÖêćöĀúĆÜÖćøĀĆÖĒúšü ÷ĆÜöĊÙüćöóĉÖćøĒúąÖćøÿĎâđÿĊ÷ÙüćöÿćöćøëĔîÖćøìĞćÖĉÝüĆêøðøąÝĞćüĆîĔîĂĆêøćìĊęÿĎÜ
ĂĊÖéšü÷ îĂÖÝćÖîĊĚÙŠćĔߚ݊ć÷ĔîÖćøéĎĒúøĆÖþćĀúĆÜÖøąéĎÖÿąēóÖĀĆÖÖĘ÷ĆÜÿĎÜöćÖÖüŠćÖøąéĎÖĀĆÖìĊęĂČęîė đîČęĂÜÝćÖëšćĕöŠĕéšøĆïÖćø
ñŠćêĆéøĆÖþćñĎšðśü÷ÝąĕöŠÿćöćøëđéĉîĕéš ĂĊÖìĆĚÜēøÙĒúąõćüąĒìøÖàšĂîĀúĆÜñŠćêĆéÖĘóïĕéšïŠĂ÷ĒúąøčîĒøÜ
5. öĊÖćøýċÖþćĂĆêøćêć÷ĒúąĂĆêøćÖćøđÝĘïðśü÷õć÷ĀúĆÜÖøąéĎÖÿąēóÖĀĆÖĔîÙîñĉü×ćüÿĎÜĂć÷č óïĂĆêøć
êć÷ÿĎÜëċÜðøąöćèøšĂ÷úą 20.0 õć÷Ĕî 1 ðŘĀúĆÜÖøąéĎÖĀĆÖ ÿĞćĀøĆïñĎšìęĊøĂéßĊüĉê óïüŠćøšĂ÷úą 30.0 ÝąöĊÙüćöóĉÖćøđÖĉé×ċĚî
Ēïïëćüø (permanent disability) êšĂÜĕéšøĆïÖćøéĎĒúÝćÖñĎšĂČęî ĀøČĂĂ÷ĎŠĔîÿëćîó÷ćïćú (nursing home) øšĂ÷úą 40.0 ĕöŠ
ÿćöćøëđéĉîĕéšĂ÷ŠćÜðÖêĉêšĂÜĔßšđÙøČęĂÜߊü÷đéĉîĂ÷ŠćÜĔéĂ÷ŠćÜĀîċęÜ ĒúąøšĂ÷úą 80.0 ĕöŠÿćöćøëðäĉïĆêĉÖĉÝüĆêøðøąÝĞćüĆîĂ÷ŠćÜ
îšĂ÷ĀîċęÜĂ÷ŠćÜ ìĊęđÙ÷ìĞćĕéšđĂÜÖŠĂîÖøąéĎÖÿąēóÖĀĆÖ20
6. Ĕîðøąđìýĕì÷ ĂĆêøćêć÷õć÷ĀúĆÜÖøąéĎÖÿąēóÖĀĆÖÝćÖÖćøýċÖþćìĊęÝĆÜĀüĆéđßĊ÷ÜĔĀöŠ4 óïüŠć øšĂ÷úą
2.1 êć÷øąĀüŠćÜ÷ĆÜøĆÖþćêĆüĔîēøÜó÷ćïćú ĒúąĂĆêøćêć÷ĀúĆÜÝćÖÖøąéĎÖÿąēóÖĀĆÖìĊę 3 đéČĂî 6 đéČĂî Ēúą 1 ðŘ đìŠćÖĆï
øšĂ÷úą 9.0, 12.0 Ēúą 17.0 êćöúĞćéĆï ÿĞćĀøĆïÖćøýċÖþćđÖĊę÷üÖĆïÙčèõćóßĊüĉêĀúĆÜÖøąéĎÖÿąēóÖĀĆÖĔîÙîĕì÷7 óïüŠć 1 Ĕî
5 ×ĂÜñĎšðśü÷ (øšĂ÷úą 22.0) ĕöŠÿćöćøëđéĉîĕéš øšĂ÷úą 23.0 êšĂÜĔßš wheel chair ĔîÖćøđÙúČęĂî÷šć÷ îĂÖÝćÖîĆĚîñĎšðśü÷đĀúŠćîĊĚ
÷ĆÜêšĂÜĕéšøĆïÖćøߊü÷đĀúČĂĔîÖćøðäĉïĆêĉÖĉÝüĆêøðøąÝĞćüĆîêŠćÜė ĔîĂĆêøćìĊęÿĎÜ đߊî øšĂ÷úą 11.0 êšĂÜߊü÷ĂćïîĚĞć øšĂ÷úą 10.0
êšĂÜߊü÷ĒêŠÜêĆü øšĂ÷úą 22.0 êšĂÜߊü÷ĔîÖćø×ĆïëŠć÷ ĒúąøšĂ÷úą 5.0 êšĂÜߊü÷ĔîÖćøøĆïðøąìćîĂćĀćø
ÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčîĔîđßĉÜđýøþåýćÿêøŤìćÜÿćíćøèÿč× (health economics aspects of osteoporotic
fractures)
Ĕîðøąđìýĕì÷÷ĆÜĕöŠóïÖćøýċÖþćÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčîĔîđßĉÜđýøþåýćÿêøŤìćÜÿćíćøèÿč×ìĊęßĆéđÝî ÝćÖ
øć÷Üćî×ĂÜ International Osteoporosis Foundation (IOF) ìĊęĕéšÿĞćøüÝÙŠćĔߚ݊ć÷ (cost) ĔîÖćøéĎĒúøĆÖþćÖøąéĎÖĀĆÖÝćÖ
ēøÙÖøąéĎÖóøčî (osteoporotic fractures) Ĕî÷čēøð óïüŠćÿĀõćó÷čēøðĔߚ݊ć÷đÜĉîĔîÖćøéĎĒúøĆÖþćÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖ
óøčîÿĎÜëċÜðŘúą 25 óĆîúšćî÷Ďēø ÝćÖךĂöĎú×ĂÜðøąđìýĂĆÜÖùþðøąđìýđéĊ÷ü óïüŠćöĊÖćøĔßšđÜĉîĔîÖćøéĎĒúøĆÖþćÖøąéĎÖĀĆÖÝćÖ
ēøÙÖøąéĎÖóøčîëċÜðŘúą 1.8 óĆîúšćîðĂîéŤ21 ĒúąÝćÖÖćøðøąöćèēé÷ National Osteoporosis Foundation (NOF) ×ĂÜ
ÿĀøĆåĂđöøĉÖćĔîðŘ 1995 óïüŠćÙŠćĔߚ݊ć÷ĔîÖćøéĎĒúøĆÖþćÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî îŠćÝąÿĎÜëċÜðŘúą 17 óĆîúšćîđĀøĊ÷â22
Cost and Interventions
đîČę Ă ÜÝćÖēøÙÖøąéĎ Ö óøč î ÝąĕöŠ Ē ÿéÜĂćÖćøñĉ é ðÖêĉ Ý îÖüŠ ć ÝąđÖĉ é ÖøąéĎ Ö ĀĆ Ö Ĕî×èąìĊę đ öČę Ă óĉ Ý ćøèćĔîđßĉ Ü
đýøþåýćÿêøŤìćÜÿćíćøèÿč×Ēúšü ĕöŠöĊÙüćöÙčšöÙŠćìĊęÝąìĞćÖćøêøüÝÙĆéÖøĂÜéšü÷đÙøČęĂÜüĆéÙüćöĀîćĒîŠîÖøąéĎÖĔîðøąßćÖø
ēé÷ìĆęüĕðìĆĚÜĀöé éĆÜîĆĚîÝċÜĔßšÖćøðøąđöĉîðŦÝÝĆ÷đÿĊę÷Ü àċęÜđðŨîđÙøČęĂÜöČĂìĊęĔßšĕéšÜŠć÷ ÿąéüÖ ĒúąðøąĀ÷ĆéĔîìćÜðäĉïĆêĉ đóČęĂÙšîĀć
ñĎšìĊęöĊðŦÝÝĆ÷đÿĊę÷ÜìĊęÝąđÖĉéēøÙÖøąéĎÖóøčîĀøČĂÖøąéĎÖĀĆÖ23
ÖćøðøąđöĉîðŦÝÝĆ÷đÿĊę÷Ü êøüÝÙĆéÖøĂÜ ĒúąüĉîĉÝÞĆ÷
1. ÖćøðøąđöĉîðŦÝÝĆ÷đÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî ēé÷Ĕßš FRAXTM (Risk assessment of
osteoporotic fracture) ×ĂÜĂÜÙŤÖćøĂîćöĆ÷úĞć (WHO-FRAX) ëČĂđðŨîöćêøåćîđðŨîìĊę÷ĂöøĆïĂ÷ŠćÜÖüšćÜ×üćÜ
ðŦÝÝĆ÷đÿĊę÷ÜÿĞćÙĆâìĊę WHO îĞćöćĔßšĔî FRAXTM 24
- Age
- BMD (FN)/BMI (T-score or kg/m2)
- Prior fragility fracture (yes/no)
- Parental history of hip fracture (yes/no)
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-5
- Current tobacco smoking (yes/no)
- Ever long-term use of oral glucocorticoids (yes/no)
- Rheumatoid arthritis (yes/no)
- Other causes of secondary osteoporosis (yes/no)
- Daily alcohol consumption of three or more units daily (yes/no)
Āöć÷đĀêč: BMD (FN) = femoral neck bone mass density, BMI = bone mass index
ךĂöĎúĒúąðŦÝÝĆ÷đÿĊę÷ÜêŠćÜė éĆÜÖúŠćüëĎÖÖĞćĀîéĕüšĒúąÙĞćîüèēé÷ìĞćđðŨîēðøĒÖøöÿĞćđøĘÝøĎð àċęÜÝąÿćöćøëÙĞćîüè
ĂĂÖöćđðŨîÙüćöîŠćÝąđðŨîìĊęÝąđÖĉéÖøąéĎÖĀĆÖĔîøą÷ą 10 ðŘ (10-year probability of fracture) ēé÷ēðøĒÖøö FRAXTM îĊĚ
ÿćöćøëđךćĕðĔßšĕéšìćÜ internet ìĊę http://www.shef.ac.uk/FRAX25 àċęÜĔîÙüćöđðŨîÝøĉÜ 10-year probability îĊĚöĊÙüćö
ñĆîĒðøÖĆïðøąđìýđßČĚĂßćêĉêŠćÜė éšü÷ àċęÜÝąĕéšñúúĆóíŤ 2 ĒïïÙČĂ 10-year probability of hip fracture Ēúą 10-year
probability of other major osteoporotic fractures ìĆĚÜîĊĚÿćöćøëîĞćìĆĚÜÿĂÜÙŠćöćĔßšðøąđöĉîÙüćöđÿĊę÷Ü×ĂÜñĎšðśü÷đóČęĂĔßš
đøĉęöÖćøøĆÖþćĕéš (therapeutic threshold) ÙČĂëšćñĎšðśü÷öĊ 10-year probability of hip fracture œ3% ĀøČĂ 10-year
probability of other major osteoporotic fractures œ20% ÖĘĔĀš÷ćøĆÖþćĕéš
ðŦÝÝčïĆî÷ĆÜĕöŠöĊךĂöĎú×ĂÜðøąßćÖøĕì÷ĔîÖćøÙĞćîüè FRAXTM ìćÜöĎúîĉíĉēøÙÖøąéĎÖóøčîĒĀŠÜðøąđìýĕì÷ÝċÜĕéš
ìĞćÖćøýċÖþćĒúąìĞćÖćøìéÿĂï FRAXTM ēé÷ÖćøĂšćÜĂĉÜךĂöĎúĔîßîßćêĉđĂđßĊ÷ ĔîđïČĚĂÜêšîóïüŠć ÖćøĔßš FRAXTM ×ĂÜ
ðøąßćÖøđßČĚĂßćêĉđĂđßĊ÷ ĕéšĒÖŠ US-Asian ĒúąâĊęðčśî îŠćÝąöĊÙüćöđĀöćąÿö đöČęĂóĉÝćøèćÝćÖךĂöĎúìćÜøąïćéüĉì÷ć×ĂÜēøÙ
ÖøąéĎÖóøčîĔîðøąđìýĕì÷ Ă÷ŠćÜĕøÖĘêćöđîČęĂÜÝćÖ÷ĆÜĕöŠöĊÖćøýċÖþćÝčéêĆéìĊęđĀöćąÿöĔîÖćøĔĀšÖćøøĆÖþćéšü÷÷ćĔîÙîĕì÷ ÝċÜ
ĒîąîĞćĔĀšĔßšÙŠćÝčéêĆéêćöÙĞćĒîąîĞć×ĂÜ NOF ÙČĂ 10-year probability of hip fracture œ3% ĀøČĂ 10-year probability
of other major osteoporotic fractures œ20% ÖĘĔĀš÷ćøĆÖþćĕéš
2. ÖćøÙĆéÖøĂÜðŦÝÝĆ÷đÿĊę÷Üēé÷ OSTA, KKOS, Nomogram
ÖćøêøüÝÙĆéÖøĂÜĀćñĎšìĊęöĊÙüćöđÿĊę÷ÜĔîÖćøđÖĉéēøÙÖøąéĎÖóøčîĔîðŦÝÝčïĆî öĊ 3 üĉíĊ ÙČĂ Osteoporosis Self–
Assessment Tool for Asian (OSTA)26, Khon Kaen Osteoporosis Study (KKOS) Score27 ĒúąēîēöĒÖøö
(nomogram)28
2.1 OSTA (Osteoporosis Self-Assessment Tool for Asians)
êćøćÜìĊę 17.3 ÖćøÙĆéÖøĂÜÙüćöđÿĊę÷Üéšü÷üĉíĊ Osteoporosis Self-Assessment Tool for Asians26
Ăć÷č îĚĞćĀîĆÖ (ÖĉēúÖøĆö)
(ðŘ) 40-44 45-49 50-54 55-59 60-64 65-69 70-74 75-79 80-84 85-89 90-94
40-44
45-49
50-54 ÙüćöđÿĊę÷ÜêęćĞ
55-59
60-64
65-69
70-74 ÙüćöđÿĊę÷ÜðćîÖúćÜ
75-79
80-84 17
85-89 ÙüćöđÿĊę÷ÜÿĎÜ
90-94
95-99
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-6 โรคกระดูกพรุน (Osteoporosis)
ÖćøÙĞćîüèÙüćöđÿĊę÷Ü OSTA index ēé÷ĔßšÿĎêøéĆÜîĊĚ
OSTA index = 0.2 X [îĚĞćĀîĆÖ (ÖĉēúÖøĆö)–Ăć÷č (ðŘ)] (ñúúĆóíŤìĊęĕéšĔĀšêĆéÝčéìýîĉ÷öĂĂÖ)
ÖćøĒðúñú
OSTA index îšĂ÷ÖüŠć -4 Āöć÷ëċÜ ÙüćöđÿĊę÷ÜÿĎÜ
øąĀüŠćÜ -4 ëċÜ -1 Āöć÷ëċÜ ÙüćöđÿĊę÷ÜðćîÖúćÜ
öćÖÖüŠć -1 Āöć÷ëċÜ ÙüćöđÿĊę÷ÜêęĞć
ĔîÖøèĊìĊęöĊÙüćöđÿĊę÷ÜÿĎÜøŠüöÖĆïöĊ osteopenia ÝćÖõćóøĆÜÿĊìĊęêĞćĒĀîŠÜ TL-spine ĒúąĕöŠÿćöćøëÿŠÜêøüÝÙüćö
ĀîćĒîŠîÖøąéĎÖéšü÷đÙøČęĂÜ dual-energy x-ray absorptiometry (DXA) ĕéš ĂćÝóĉÝćøèćĔĀšÖćøøĆÖþć ÿŠüîÖøèĊìĊęöĊÙüćö
đÿĊę÷ÜðćîÖúćÜÙüøÿŠÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖÖŠĂîóĉÝćøèćĔĀšÖćøøĆÖþć ÿĞćĀøĆïÖúčŠöÙüćöđÿĊę÷ÜêęĞćĕöŠêšĂÜÿŠÜêøüÝÙüćö
ĀîćĒîŠî×ĂÜÖøąéĎÖđóøćąöĊÙüćöđÿĊę÷ÜêęĞćĔîÖćøđÖĉéēøÙÖøąéĎÖóøčî
2.2 Khon Kaen Osteoporosis Study (KKOS) Score
êćøćÜìĊę 17.4 ÖćøÙĆéÖøĂÜÙüćöđÿĊę÷Üéšü÷üĉíĊ Khon Kaen Osteoporosis Study (KKOS) Score27
Age (yr) Score Weight (kg) Score
<45 +7.5 <30 -14
45-49 +6.0 30-34 -12
50-54 +4.5 35-39 -10
55-59 +3.0 40-44 -8
60-64 +1.5 45-49 -6
65-69 0 50-54 -4
70-74 -1.5 55-59 -2
75-79 -3.0 60-64 0
80-84 -4.5 65-69 +2
85-89 -6.0 70-74 +4
>90 -7.5 75-79 +6
80-84 +8
85-89 +10
>90 +12
ÖćøÙĞćîüè KKOS ĔĀšîĞćÙŠćÙąĒîîÝćÖĂć÷č (ðŘ) ĒúąîĚĞćĀîĆÖ (ÖĉēúÖøĆö) öćïüÖÖĆî
KKOS < -1 Āöć÷ëċÜ ÙüćöđÿĊę÷ÜÿĎÜĔîÖćøđÖĉéēøÙÖøąéĎÖóøčî
KKOS > -1 Āöć÷ëċÜ ÙüćöđÿĊę÷ÜêęĞćĔîÖćøđÖĉéēøÙÖøąéĎÖóøčî
êĆüĂ÷ŠćÜÖćøÙĞćîüè
ñĎšĀâĉÜĂć÷č 52 ðŘ îĚĞćĀîĆÖ 48 ÖĉēúÖøĆö KKOS = (+4.5) + (-6) = -1.5 = ÙüćöđÿĊę÷ÜÿĎÜ
KKOS ÷ĆÜÿćöćøëÙĞćîüèēĂÖćÿ×ĂÜÖćøđÖĉéēøÙÖøąéĎÖóøčîĕéšēé÷éĎÝćÖêćøćÜìĊę 17.5 ĔîÖøèĊìĊęêĆĚÜĒêŠøšĂ÷úą
80.0 ×ċĚîĕðÝĆéĂ÷ĎŠÖúčŠöÙüćöđÿĊę÷ÜÿĎÜ øąĀüŠćÜ 20.0-79.0 ÝĆéĂ÷ĎŠĔîÖúčŠöÙüćöđÿĊę÷ÜðćîÖúćÜ ĒúąÖüŠćøšĂ÷úą 20.0 ÝĆéĂ÷ĎŠÖúčŠö
ÙüćöđÿĊę÷ÜêęĞć
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-7
êćøćÜìĊę 17.5 êĆüĂ÷ŠćÜÖćøÙĞćîüèēĂÖćÿ×ĂÜÖćøđÖĉéēøÙÖøąéĎÖóøčîéšü÷üĉíĊ KKOS27
îĚĞćĀîĆÖ Ăć÷č (ðŘ)
(ÖĉēúÖøĆö) <45 45-49 50-54 55-59 60-64 65-69 70-74 75-79 80-84 85-89 >90
< 30 58.7 67.4 75.0 81.3 86.3 90.2 93.0 95.1 96.6 97.6 98.3
30-34 47.5 56.8 65.6 73.5 80.1 85.4 89.5 92.5 94.7 96.3 97.4
35-39 36.6 45.6 54.9 63.8 71.9 78.8 84.4 88.7 91.9 94.3 96.0
40-44 26.9 34.8 43.6 52.9 62.0 70.3 77.5 83.3 87.9 91.3 93.9
45-49 19.0 25.4 33.0 41.7 51.0 60.2 68.7 76.1 82.2 87.0 90.7
50-54 13.0 17.5 23.9 31.3 39.8 49.0 58.3 67.0 74.6 81.0 86.1
55-59 8.7 12.1 16.7 22.5 29.7 38.0 47.1 56.4 65.2 73.1 80.0
60-64 5.7 8.1 11.3 15.6 21.2 28.1 36.2 45.1 54.4 63.4 71.6
65-69 3.7 5.3 7.5 10.5 14.6 19.9 26.5 34.4 43.2 52.5 61.6
70-74 2.4 3.4 4.9 7.0 9.8 13.7 18.7 25.0 32.6 41.3 50.5
75-79 1.5 2.2 3.2 4.6 6.5 9.2 12.8 17.5 23.6 30.9 39.4
80-84 1.0 1.4 2.1 3.0 4.2 6.0 8.5 11.9 16.4 22.2 29.3
85-89 0.6 0.9 1.3 1.9 2.7 3.9 5.6 7.9 11.1 15.4 20.9
> 90 0.4 0.6 0.8 1.2 1.8 2.5 3.6 5.2 7.4 10.4 14.4
2.3 Nomogram ĔîÖćøìĞćîć÷ÖćøđÖĉéēøÙÖøąéĎÖóøčîĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂîēé÷ĔßšĂć÷č îĚĞćĀîĆÖ
28
Ēúą QUS
õćóìĊę 17.1 ÖćøìĞćîć÷ÖćøđÖĉéēøÙÖøąéĎÖóøčîĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂîēé÷ĔßšĂć÷č îĚĞćĀîĆÖ Ēúą QUS28
17
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-8 โรคกระดูกพรุน (Osteoporosis)
üĉíĊÖćøÙĞćîüè
1. úćÖđÿšîÝćÖĒÖîĂć÷č×ċĚîĕð÷ĆÜĒÖîÙąĒîî (point)
2. úćÖđÿšîÝćÖĒÖîîĚĞćĀîĆÖĕð÷ĆÜĒÖîÙąĒîî (point)
3. úćÖđÿšîÝćÖĒÖî QUS (T-score) ĕð÷ĆÜĒÖîÙąĒîî (point)
4. îĞćìĆĚÜ 3 ÙąĒîîöćøüöÖĆî (total points)
5. úćÖđÿšîÝćÖĒÖîÙąĒîîøüö (total points) úÜöć÷ĆÜĒÖîÙüćöđÿĊę÷Ü×ĂÜēøÙÖøąéĎÖóøčî (risk of
osteoporosis)
6. ĔîÖøèĊìĊęÙüćöđÿĊę÷Ü×ĂÜÖćøđÖĉéēøÙÖøąéĎÖóøčîêĆĚÜĒêŠ 0.3 ×ċĚîĕðÝĆéđðŨîÖúčŠöìĊęöĊÙüćöđÿĊę÷ÜÿĎÜĔîÖćø
đÖĉéēøÙÖøąéĎÖóøčîÙüøÿŠÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖéšü÷đÙøČęĂÜ DXA êŠĂĕð
ĔîÖćøêøüÝÙĆéÖøĂÜðøąđöĉîðŦÝÝĆ÷đÿĊę÷Ü ÖćøđúČĂÖĔßš FRAXTM ĔîÖćøðøąđöĉîëČĂđðŨîìĊęĔßšÖĆîĂ÷ŠćÜÖüšćÜ×üćÜđðŨîìĊę
÷ĂöøĆï ÿćöćøëđךćëċÜĕéšÜŠć÷ ĒêŠđĀöćąÖĆïñĎšöĊÙüćöøĎšĔîõćþćĂĆÜÖùþĒúąÿćöćøëđךćëċÜךĂöĎúìćÜ internet ĕéš ÿŠüî OSTA
index Ēúą KKOS score ÖĘđðŨîêĆüÙĆéÖøĂÜìĊęéĊ đךćĔÝÜŠć÷ ÿŠüî nomogram ÙŠĂîךćÜđךćĔÝĕéš÷ćÖÖüŠć ĒîąîĞćĔĀšđúČĂÖĔßšêćö
ÙüćöđĀöćąÿö
3. ÖćøêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ
3.1 ÖćøÿŠÜêøüÝ BMD éšü÷đÙøČęĂÜ axial DXA29
WHO ÖĞćĀîéĔĀšđðŨîöćêøåćîĔîÖćøüĉîĉÝÞĆ÷õćüąēøÙÖøąéĎÖóøčî ÙČĂ axial dual-energy x-ray
absorptiometry (axial DXA) đìŠćîĆĚî ĔîÖćøêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖđóČęĂüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčî ĔĀšêøüÝìĊęÖøąéĎÖ
ÿĆîĀúĆÜÿŠüîđĂü ĒúąÖøąéĎÖÿąēóÖךćÜìĊęĕöŠëîĆéĒúą/ĀøČĂךćÜìĊęĕöŠĀĆÖđìŠćîĆĚî àċęÜđøĊ÷ÖüŠć axial DXA ĔîìĊęîĊĚĀöć÷ëċÜ dual
energy X-ray absorptiometry đìŠćîĆĚî ĕöŠĒîąîĞćĔĀšêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖðúć÷Ē×î (peripheral DXA) ÷Öđüšî
ĔîñĎšðśü÷ìĊęĂšüîöćÖ (>130 ÖĉēúÖøĆö) ĀøČĂĕöŠÿćöćøëêøüÝĀøČĂĒðúñúÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖÝćÖ axial DXA ĕéš
ךĂïŠÜßĊĚĔîÖćøÿŠÜêøüÝ BMD éšü÷đÙøČęĂÜ axial DXA29
1) ñĎšĀâĉÜĂć÷čêĆĚÜĒêŠ 65 ðŘ×ċĚîĕð ĒúąñĎšßć÷Ăć÷čêĆĚÜĒêŠ 70 ðŘ×ċĚîĕð
2) ÿĞćĀøĆïñĎšĀâĉÜìĊęöĊĂć÷čêęĞćÖüŠć 65 ðŘ ĒúąñĎšßć÷ìĊęöĊĂć÷čêęĞćÖüŠć 70 ðŘ ìĊęöĊðŦÝÝĆ÷đÿĊę÷ÜéĆÜêŠĂĕðîĊĚĂ÷ŠćÜîšĂ÷
1 ךĂ
- ĀöéðøąÝĞćđéČĂîÖŠĂîĂć÷č 45 ðŘ (early menopause) àċęÜĀöć÷øüöëċÜñĎšìĊęëĎÖêĆéøĆÜĕ׊ìĆĚÜÿĂÜךćÜ
- öĊõćüą×ćéăĂøŤēöîđĂÿēêøđÝî (estrogen deficiency) ÖŠĂîđךćÿĎŠüĆ÷ĀöéðøąÝĞćđéČĂî êŠĂđîČęĂÜ
îćîÖüŠć 1 ðŘ ÷ÖđüšîÖøèĊêĆĚÜÙøøõŤĒúąĔĀšîöïčêø
- ĕéšøĆï÷ćÖúĎēÙÙĂøŤêĉÙĂ÷éŤđðŨîøą÷ąđüúćîćî (đóøéîĉēàēúî×îćéêĆĚÜĒêŠ 5 öÖ.êŠĂüĆî×ċĚîĕðĀøČĂ
đìĊ÷ïđìŠćđðŨîđüúćîćîÖüŠć 3 đéČĂî)
- öĊðøąüĆêĉïĉéćĀøČĂöćøéćÖøąéĎÖÿąēóÖĀĆÖĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂîĀøČĂñĎšßć÷Ăć÷čêĆĚÜĒêŠ 50
ðŘ×ċĚîĕð
- ñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂîìĊęöĊéĆßîĊöüúÖć÷îšĂ÷ÖüŠć 19 ÖĉēúÖøĆöêŠĂêćøćÜđöêø
3) êøüÝóïõćüąÖøąéĎ Ö ïćÜĀøČ Ă ÖøąéĎ Ö ÿĆ î ĀúĆ Ü ñĉ é øĎ ð ÝćÖÖćøëŠ ć ÷õćóøĆ Ü ÿĊ đ ĂÖàŤ (radiographic
osteopenia and/or vertebral deformity by x-ray)
4) öĊðøąüĆêĉÖøąéĎÖĀĆÖÝćÖõ÷Ćîêøć÷ĒïïĕöŠøčîĒøÜĀúĆÜĂć÷č 40 ðŘ
5) öĊðøąüĆêĉÿŠüîÿĎÜúéúÜöćÖÖüŠć 4 đàîêĉđöêø ĀøČĂúéúÜöćÖÖüŠć 2 đàîêĉđöêøêŠĂðŘ
6) Ă÷ĎŠĔîÖúčŠöìĊęöĊÙüćöđÿĊę÷ÜðćîÖúćÜ×ċĚîĕðÝćÖÖćøêøüÝÙĆéÖøĂÜéšü÷ OSTA score, KKOS score ĀøČĂ
ēĂÖćÿđÿĊę÷ÜÝćÖēîēöĒÖøö (nomogram probability) êĆĚÜĒêŠ 0.3 ×ċĚîĕðÿĞćĀøĆïñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂî
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-9
3.2 Quantitative CT scan (QCT)
ðŦÝÝčïĆî QCT ÿćöćøëðøąđöĉîÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖĕéš ĒêŠđîČęĂÜÝćÖøĆÜÿĊÝćÖÖćøüĆéöĊðøĉöćèÿĎÜ øćÙć
ĒóÜĒúąĕöŠĔߊđÖèæŤöćêøåćîêćöĂÜÙŤÖćøĂîćöĆ÷ēúÖ ÝċÜĕöŠĒîąîĞćĔĀšÿŠÜêøüÝ
3.3 Quantitative ultrasound ìĊęÖøąéĎÖÿšîđìšć
ðŦÝÝčïĆî÷ĆÜĕöŠöĊךĂĒîąîĞćĔĀšĔßšĔîÖćøüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčî ÷ÖđüšîĔîÖøèĊêøüÝÙĆéÖøĂÜēé÷ĔßšøŠüöÖĆï
éĆßîĊÙüćöđÿĊę÷ÜìćÜÙúĉîĉÖ đߊî Ăć÷č îĚĞćĀîĆÖ ĀøČĂĔîÖøèĊìĊęÿëćîó÷ćïćúĕöŠöĊ ĀøČĂĕöŠÿćöćøëÿŠÜñĎšðśü÷ĕðêøüÝéšü÷đÙøČęĂÜ
DXA
ÝćÖÖćøýċÖþć×ĂÜ Pongchaiyakul33 óïüŠćÖćøĔßš Quantitative ultrasound øŠüöÖĆï clinical risk
indices (OSTA/KKOS) óïüŠćöĊ senvitivity ×ċĚî 88% Ĕî×èąìĊęÖćøĔßš Quantitative ultrasound đóĊ÷ÜĂ÷ŠćÜđéĊ÷üöĊ
sensitivity đóĊ÷Ü 60%
3.4 ÖćøêøüÝÙŠćìćÜßĊüđÙöĊ×ĂÜÖćøĀöčîđüĊ÷îÖøąéĎÖ (biochemical markers of bone turnover)
ÙŠć ìćÜßĊü đÙöĊ× ĂÜÖøąïüîÖćøÿøš ć ÜĒúąÿúć÷ÖøąéĎÖ ĕöŠĒîąîĞćĔĀšĔßšĔ îÖćøüĉîĉÝ ÞĆ÷ēøÙÖøąéĎÖóøčî
đîČęĂÜÝćÖÙŠćìĊęüĆéĕéšĂćÝëĎÖøïÖüîĕéšÝćÖĀúć÷ðŦÝÝĆ÷ ĒúąĂćÝóïÙüćöñĉéðÖêĉĕéšĔîĀúć÷ēøÙìĊęĕöŠĔߊēøÙÖøąéĎÖóøčîĒêŠĂćÝĔßš
øŠüöÖĆïñúêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖđóČęĂðøąđöĉîÙüćöđÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖĕéšĂ÷ŠćÜĕøÖĘêćöÙŠćìćÜßĊüđÙöĊ×ĂÜÖćø
ĀöčîđüĊ÷îÖøąéĎÖéĆÜÖúŠćü ĂćÝöĊðøąē÷ßîŤĔîÖćøêĉéêćöÖćøøĆÖþćēé÷ĒîąîĞćĔĀšêøüÝÖŠĂîđøĉęöĔĀš÷ćĒúąðøąđöĉîàĚĞćõć÷ĀúĆÜ
ÖćøøĆÖþćìĊę 3 đéČĂî 6 đéČĂî ĀøČĂ 1 ðŘ àċęÜߊü÷ĔĀšìøćïÖćøêĂïÿîĂÜêŠĂÖćøøĆÖþćéšü÷÷ćĕéšøüéđøĘüÖüŠćÖćøêøüÝÙüćö
ĀîćĒîŠî×ĂÜÖøąéĎÖéšü÷đÙøČęĂÜ DXA
êćøćÜìĊę 17.6 ñúÖćøðøąđöĉîÙüćöđÿĊę÷ÜĒúąÖćøêøüÝÙĆéÖøĂÜēøÙÖøąéĎÖóøčîéšü÷üĉíĊÖćøêŠćÜė
sensitivity specificity positive predictive negative predictive
Tools
(%) (%) value (%) value (%)
30
FRAX 60.1 85.8 3.3 99.6
31
OSTA 51.7 71.4 20.9 96.9
Khon Kaen 72.5 73.0 36.0 NA
Osteoporosis study
(KKOS) score32
Quantitative 21-60 88-96 72.4 73.1
33
ultrasound
17
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-10 โรคกระดูกพรุน (Osteoporosis)
õćóìĊę 17.2 ÖćøéĎĒúøĆÖþćēøÙÖøąéĎÖóøčî34
ÙüćöÙčšöÙŠćĒúąñúÖøąìïéšćîÜïðøąöćè×ĂÜÖćøÙĆéÖøĂÜēøÙÖøąéĎÖóøčî
ÝćÖøć÷ÜćîÖćøüĉđÙøćąĀŤÙüćöÙčšöÙŠćĒúąñúÖøąìïéšćîÜïðøąöćè×ĂÜÖćøÙĆéÖøĂÜēøÙÖøąéĎÖóøčîĔîñĎšĀâĉÜüĆ÷
ĀöéðøąÝĞ ć đéČ Ă îïîóČĚ î åćî×ĂÜÖćøĔßš Ē ïïÝĞ ć úĂÜìćÜđýøþåýćÿêøŤ ēé÷õćÙüĉ ß ćĂć÷č ø ýćÿêøŤ ÙèąĒóì÷Ť ý ćÿêøŤ
öĀćüĉì÷ćúĆ÷×ĂîĒÖŠîĔîðŘ 255635 óïüŠćđöČęĂđðøĊ÷ïđìĊ÷ïÖćøÙĆéÖøĂÜéšü÷ĒîüìćÜêŠćÜė ÖĆïĕöŠöĊÖćøÙĆéÖøĂÜĔîñĎšĀâĉÜüĆ÷Āöé
ðøąÝĞćđéČĂî óïüŠćÖćøÙĆéÖøĂÜéšü÷éĆßîĊÙĆéÖøĂÜÙüćöđÿĊę÷Ü KKOS öĊÙüćöÙčšöÙŠćöćÖìĊęÿčé øĂÜúÜöćÙČĂ éĆßîĊÙĆéÖøĂÜÙüćö
đÿĊę÷Ü OSTA éĆßîĊÙĆéÖøĂÜÙüćöđÿĊę÷Ü KKOS øŠüöÖĆïÖćøüĆéÖøąéĎÖÿšîđìšć (QUS) éĆßîĊÙĆéÖøĂÜÙüćöđÿĊę÷Ü OSTA øŠüöÖĆï QUS
ĒúąÖćøðøąđöĉîÙüćöđÿĊę÷ÜÖćøđÖĉéÖøąéĎÖĀĆÖéšü÷đÙøČęĂÜöČĂðøąđöĉîÙüćöđÿĊę÷ÜÖćøđÖĉéÖøąéĎÖĀĆÖÝćÖĂÜÙŤÖćøĂîćöĆ÷ēúÖ
(FRAXTM) êćöúĞćéĆï ĒúąÖćøÙĆéÖøĂÜēøÙÖøąéĎÖóøčîéšü÷éĆßîĊÙĆéÖøĂÜÙüćöđÿĊę÷Ü OSTA ĀøČĂ KKOS öĊÙüćöÙčšöÙŠćđöČęĂÙĆé
ÖøĂÜñĎšĀâĉÜĂć÷č 65 ðŘ×ċĚîĕð ēé÷öĊĂĆêøćÿŠüîêšîìčîðøąÿĉìíĉñúÿŠüîđóĉęöìĊęĔÖúšđÙĊ÷ÜÖĆî ĒúąÖćøÙĆéÖøĂÜßîĉéĂČęîė ÝąöĊÙüćö
ÙčšöÙŠćđöČęĂÙĆéÖøĂÜñĎšĀâĉÜĂć÷č 70-75 ðŘ (êćøćÜìĊę 17.7)
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-11
êćøćÜìĊę 17.7 ĂĆêøćÿŠüîêšîìčîðøąÿĉìíĉñúÿŠüîđóĉęö×ĂÜÖćøÙĆéÖøĂÜēøÙÖøąéĎÖóøčîđðøĊ÷ïđìĊ÷ïÖĆïÖćøĕöŠöĊÖćøÙĆéÖøĂÜ
ĒúąøĆÖþćéšü÷÷ć ÝĞćĒîÖêćöÖćøÙĆéÖøĂÜìĊęĂć÷čêŠćÜė (öčööĂÜìćÜÿĆÜÙö)35
ĂĆêøćÿŠüîêšîìčîðøąÿĉìíĉñúÿŠüîđóĉęö (ïćìêŠĂðŘÿč×õćüąìĊęđóĉęö×ċĚî)*
Ăć÷č OSTA KKOS OSTA Ēúą QUS KKOS Ēúą QUS FRAXTM
50 469,000 446,000 677,000 651,000 731,000
55 272,000 263,000 360,000 350,000 381,000
60 191,000 187,000 233,000 228,000 241,000
65 117,000 115,000 137,000 135,000 141,000
70 78,000 78,000 90,000 89,000 92,000
75 98,000 98,000 110,000 109,000 111,000
80 126,000 125,000 138,000 137,000 139,000
85 135,000 134,000 148,000 147,000 149,000
Āöć÷đĀêč: * ĕéšðøĆïêĆüđú×ĔĀšĔÖúšđÙĊ÷ÜĀúĆÖóĆî (1,000)
ÖćøøĆÖþćēøÙÖøąéĎÖóøčî
1. ÖćøøĆÖþćēé÷ĕöŠĔßš÷ć (non-pharmacologic treatment)
ÖćøĕéšøĆïðøĉöćèĒÙúđàĊ÷öĒúąüĉêćöĉîéĊìĊęđóĊ÷ÜóĂ ÝćÖÖćøýċÖþć meta-analysis36 óïüŠćÖćøĔĀšüĉêćöĉî
D ×îćé 700-800 IU êŠĂüĆî øŠüöÖĆïĒÙúđàĊ÷öÝąúéĂčïĆêĉÖćøèŤ×ĂÜÖøąéĎÖÿąēóÖĒúąÖøąéĎÖìĊęêĞćĒĀîŠÜĂČęîîĂÖđĀîČĂÝćÖ
ÖøąéĎÖÿĆîĀúĆÜ (non-vertebral fracture)
ÖćøĂĂÖÖĞćúĆÜÖć÷ öĊĀúĆÖåćîìĊęĒÿéÜĔĀšđĀĘîüŠćÖćøĂĂÖÖĞćúĆÜÖć÷ߊü÷úéÖćøÿĎâđÿĊ÷öüúÖøąéĎÖ ēé÷đÞóćą
ÖćøĂĂÖÖĞćúĆÜÖć÷ìĊęöĊÖćøĒïÖøĆïîĚĞćĀîĆÖìĊęđĀöćąÿö (appropriate weight-bearing exercise) ÖćøĂĂÖÖĞćúĆÜÖć÷ìĊęöĊĒøÜ
ÖøąĒìÖÿĎÜ (high impact aerobic exercise) ĒúąÖćøĂĂÖÖĞćúĆÜÖć÷ìĊęĂĂÖĒøÜêšćî (resistance exercise) ݹߊü÷đóĉęö
ÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖĕéš37
2. ÖćøøĆÖþćéšü÷ÖćøĔßš÷ć (pharmacologic treatment)
ĔîêŠćÜðøąđìýöĊÖćøýċÖþćÙüćöÙčšöÙŠć×ĂÜÖćøĔĀš÷ć Bisphosphonate ĔîñĎšðśü÷ÖúčŠöêŠćÜė éĆÜîĊĚ
2.1 ÖúčŠöñĎšðśü÷ĀâĉÜìĊęöĊöüúÖøąéĎÖêęĞćĒúąöĊÖøąéĎÖĀĆÖöćÖŠĂî (women with low BMD and
previous fractures ÝćÖÖćøýċÖþć×ĂÜ Stevenson38 ĔîÿĀøćßĂćèćÝĆÖøìĊęĂć÷č 70 ðŘ êšîìčî×ĂÜÖćøĔßš Bisphosphonate
êŠĂ QALY gained đìŠćÖĆï 16,934 ðĂîéŤ (33,601 đĀøĊ÷â) ÿĞćĀøĆï Alendronate đìŠćÖĆï 22,001 ðĂîéŤ (43,655 đĀøĊ÷â)
ÿĞć ĀøĆï Risedronate đìĊ÷ïÖĆïÖćøĕöŠĕéš ĔĀš÷ćĔîÖúčŠöîĊĚ ĂĊÖÖćøýċÖþćĀîċęÜ ×ĂÜ Kanis39 đðŨîÖćøüĉđÙøćąĀŤ ÖćøĔĀš÷ć
Bisphosphonate (Alendronate and Etidronate) đìĊ÷ïÖĆïÖćøĕöŠĕéš÷ćĔîÖúčŠöîĊĚìĊęĂć÷čêŠćÜė ÙŠćĔߚ݊ć÷êŠĂ QALY gained
đìŠćÖĆï 36,100 ðĂîéŤ (71,631 đĀøĊ÷â) ìĊęĂć÷č 50 ðŘ, 19,800 ðĂîéŤ (39,288 đĀøĊ÷â) ìĊęĂć÷č 60 ðŘ Ēúą 5700 ðĂîéŤ
(11,310 đĀøĊ÷â) ìĊęĂć÷č 70 ðŘ
2.2 ñĎšĀâĉÜìĊęöĊöüúÖøąéĎÖêęĞćĒêŠ÷ĆÜĕöŠöĊÖøąéĎÖĀĆÖ ĔîÿĀøĆåĂđöøĉÖćÖćøĔßš Bisphosphonate ìĊęöĊ
ÖøąéĎÖóøčîìĊęĂć÷čöćÖÖüŠć 60 ðŘ ëČĂüŠć cost effectiveness ĔîÖćøðŜĂÜÖĆîÖøąéĎÖĀĆÖÝćÖÖøąéĎÖóøčî ÖćøýċÖþćóïüŠć costs
per QALY gained đìŠćÖĆï 37,482 đĀøĊ÷â
2.3 ñĎšĀâĉÜìĊęöĊÖøąéĎÖïćÜĔîÿĀøĆåĂđöøĉÖć óïüŠćĔîñĎšĀâĉÜìĊęöĊĂć÷čöćÖÖüŠć 65 ðŘ ìĊę BMD T-score
-2.4 SD öĊ cost êŠĂ QALY đìŠćÖĆï 70,732 Ĕî×èąđéĊ÷üÖĆîñĎšĀâĉÜìĊęöĊĂć÷č 75 ðŘ ìĊę BMD T-score -1.5 SD öĊ cost êŠĂ
QALY đìŠćÖĆï 332,250 đĀøĊ÷â40
÷ćìĊęöĊðøąÿĉìíĉñúéĊĔîÖćøðŜĂÜÖĆîÖćøđÖĉéēøÙÖøąéĎÖóøčî ēé÷đÞóćąĂ÷ŠćÜ÷ĉęÜëšćÿćöćøëðŜĂÜÖĆîÖćøđÖĉé
ÖøąéĎÖĀĆÖĕéšöćÖĒúąĀúć÷êĞćĒĀîŠÜÝą÷ĉęÜÿŠÜñúéĊĔîÖćøîĞćöćĔßšøĆÖþćñĎšðśü÷ (êćøćÜìĊę 17.8)41-44 ĕéšøüïøüöðøąÿĉìíĉñú×ĂÜ÷ć
17
øĆÖþćēøÙÖøąéĎÖóøčîßîĉéêŠćÜė ĔîÖćøúéĂčïĆêĉÖćøèŤ×ĂÜÖøąéĎÖĀĆÖìĊęêĞćĒĀîŠÜÖøąéĎÖÿĆîĀúĆÜĒúąÖøąéĎÖêĞćĒĀîŠÜĂČęî
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-12 โรคกระดูกพรุน (Osteoporosis)
êćøćÜìĊę 17.8 ðøąÿĉìíĉñú×ĂÜÖćøĔßš÷ćøĆÖþćÖćøĀĆÖ×ĂÜÖøąéĎÖ41-44
ñúêŠĂÖćøúéÖøąéĎÖÿĆîĀúĆÜĀĆÖ ñúêŠĂÖćøúéÖøąéĎÖĀĆÖĔîêĞćĒĀîŠÜĂČęî
(Vertebral fracture) (Non-vertebral fracture)
÷ć Osteoporosis Osteoporosis
Osteoporosis + Previous Osteoporosis + Previous vertebral
vertebral fracture fracture
Alendronate + + + +
Risedronate + + + +
Ibandronate ĕöŠöĊĀúĆÖåćî + ĕöŠöĊĀúĆÖåćî +
Zoledronic acid + + ĕöŠöĊĀúĆÖåćî +
HRT + + + +
Raloxifene + + ĕöŠöĊĀúĆÖåćî ĕöŠöĊĀúĆÖåćî
Calcitonin + + ĕöŠöĊĀúĆÖåćî ĕöŠöĊĀúĆÖåćî
Strontium + + + +
ranelate
Teriparatide ĕöŠöĊĀúĆÖåćî + ĕöŠöĊĀúĆÖåćî +
Āöć÷đĀêč: + Āöć÷ëċÜ øĆÖþćĕéšñú
ÙüćöÙčšöÙŠćĒúąñúÖøąìïéšćîÜïðøąöćè×ĂÜÖćøĔßš÷ćêšćîÖøąéĎÖóøčî
ÝćÖÖćøýċÖþć×ĂÜ Fleurence45 óïüŠćĔîìćÜ÷čēøðĒúąĂđöøĉÖćöĊÖćøýċÖþćēé÷đĂćêĆüêĆéÿĉîìĊęüŠć ÙŠćĔߚ݊ć÷êŠĂ
Quality-adjusted Life Year (QALY) îšĂ÷ÖüŠć 30,000 ðĂîéŤ46 ĀøČĂ 50,000 đĀøĊ÷â ëČĂüŠć cost effective ךĂÿøčðìĊę
ßĆéđÝîìĊęĕéšÝćÖÖćøýċÖþćóïüŠć ñĎšĀâĉÜìĊęöĊĂć÷čêĆĚÜĒêŠ 70 ðŘ×ċĚîĕð ĒúąöĊÙŠć BMD îšĂ÷ÖüŠćĀøČĂđìŠćÖĆï 2.5 øŠüöÖĆïöĊÖøąéĎÖĀĆÖ
ÖŠĂîĀîšćîĊĚ ÖćøĔßš Bisphosphonate ëČĂüŠć cost effective ÿŠüîÖćøĔßšĔîñĎšĀâĉÜìĊęĂć÷čìĊęîšĂ÷ÖüŠć 50 ðŘ ëČĂüŠćĕöŠ cost
effective ÿŠüîĂć÷čìĊęĂ÷ĎŠøąĀüŠćÜîĊĚñúìĊęĕéš÷ĆÜĕöŠßĆéđÝî
đöČęĂĔßšĒïïÝĞćúĂÜìćÜđýøþåýćÿêøŤ óïüŠćÖćøøĆÖþćēøÙÖøąéĎÖóøčîéšü÷÷ć Alendronate è øćÙćðŦÝÝčïĆî
öĊÙüćöÙčšöÙŠćìćÜđýøþåýćÿêøŤìĊęđÖèæŤ 120,000 ïćìêŠĂðŘÿč×õćüąìĊęđóĉęö×ċĚîĔîñĎšĀâĉÜĂć÷č 65 ðŘ×ċĚîĕð ìĊęöĊ BMD T-score
îšĂ÷ÖüŠć -2.5 ĀøČĂñĎšĀâĉÜìĊęÙĞćîüèÙŠć FRAXTM with BMD ĒúšüđÖĉéēĂÖćÿđÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖìĊęêĞćĒĀîŠÜÿĞćÙĆâìĊę
øą÷ąđüúć 10 ðŘ öćÖÖüŠćĀøČĂđìŠćÖĆïøšĂ÷úą 7.4 ĒúąēĂÖćÿđÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖìĊęÿąēóÖìĊęøą÷ąđüúć 10 ðŘ öćÖÖüŠć
ĀøČĂđìŠćÖĆïøšĂ÷úą 2.4 Ă÷ŠćÜĕøÖĘêćöÖćøøĆÖþćēøÙÖøąéĎÖóøčîđóČęĂÖćøðŜĂÜÖĆîÖøąéĎÖĀĆÖàĚĞć óïüŠć÷ćìčÖêĆüĕöŠöĊÙüćöÙčšöÙŠć
ìćÜđýøþåýćÿêøŤìĊęđÖèæŤóĉÝćøèćÙüćöÙčšöÙŠćéĆÜÖúŠćü øćÙć÷ć Alendronate ÝąêšĂÜúéøćÙćúÜøšĂ÷úą 60.0 ĒúąøćÙć÷ć
Zoledronic acid ÝąêšĂÜúéøćÙćúÜøšĂ÷úą 70.0 ÝċÜÝąöĊÙüćöÙčšöÙŠćìĊęÖćøøĆÖþćĔîñĎšĀâĉÜĂć÷č 65 ðŘ ×ċĚîĕðìĊęöĊ BMD T-score
îšĂ÷ÖüŠć -2.535
ÿĞćĀøĆïÖćøÙĆéÖøĂÜēøÙÖøąéĎÖóøčîóøšĂöìĆĚÜÖćøøĆÖþćđöČęĂđðøĊ÷ïđìĊ÷ïÖĆïĕöŠöĊÖćøÙĆéÖøĂÜĒúąÖćøøĆÖþćéšü÷
ĒÙúđàĊ÷öĒúąüĉêćöĉîéĊ óïüŠćÖćøÙĆéÖøĂÜĔîñĎšìĊęĂć÷č 65 ðŘ×ċĚîĕð éšü÷ÖćøĔßšéĆßîĊÙüćöđÿĊę÷ÜìćÜÙúĉîĉÖ OSTA ĀøČĂ KKOS Ēúšü
÷Čî÷ĆîēøÙÖøąéĎÖóøčîéšü÷đÙøČęĂÜ DXA óøšĂöìĆĚÜøĆÖþćñĎšðśü÷ēøÙÖøąéĎÖóøčîéšü÷÷ć Alendronate öĊÙüćöÙčšöÙŠćìćÜ
đýøþåýćÿêøŤ Ă÷ŠćÜĕøÖĘêćö ĀćÖìĞćÖćøÙĆéÖøĂÜĔîñĎšìĊęĂć÷č 70 ðŘ×ċĚîĕð đÙøČęĂÜöČĂÙĆéÖøĂÜìčÖßîĉéöĊøąéĆïÙüćöÙčšöÙŠćìĊęêęĞćÖüŠć
đÖèæŤ 120,000 ïćìêŠĂðŘÿč×õćüąìĊęđóĉęö×ċĚîìĆĚÜÿĉĚî35
Ă÷ŠćÜĕøÖĘêćö ēøÙÖøąéĎÖóøčîĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂîîĆĚîóïĕéšöćÖ ĀćÖìĞćÖćøøĆÖþćĔîñĎšðśü÷ìčÖøć÷Ýą
ÿŠÜñúÖøąìïéšćîÜïðøąöćèêŠĂõćÙøĆåđðŨîÝĞćîüîöćÖÙČĂðøąöćè 12,866 úšćîïćìêŠĂðŘ éĆÜîĆĚîÝċÜÙüøöĊÖćøÖĞćĀîéđÖèæŤ
ÖćøøĆÖþćĔîñĎšìĊęöĊÙüćöđÿĊę÷ÜêŠĂÖćøđÖĉéÖøąéĎÖĀĆÖÿĎÜđðŨîúĞćéĆïĒøÖÖŠĂî ÷ÖêĆüĂ÷ŠćÜđߊî ÖćøĔßš ēĂÖćÿđÿĊę÷Ü×ĂÜÖćøđÖĉé
ÖøąéĎÖĀĆÖìĊęêĞćĒĀîŠÜÿĞćÙĆâìĊęøą÷ąđüúć 10 ðŘ đìŠćÖĆïøšĂ÷úą 20.0 ĀøČĂöćÖÖüŠćîĆĚî đóČęĂĕöŠÖŠĂðŦâĀćêŠĂÙüćööĆęîÙÜéšćî
ÖćøđÜĉî×ĂÜÖĂÜìčîðøąÖĆîÿč×õćóêŠćÜė
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-13
öĊÖćøýċÖþćĔîÖćøĔßš Alendronate đóČęĂðŜĂÜÖĆîÖćøđÖĉéÖøąéĎÖĀĆÖĔîÖúčŠöñĎšðśü÷ìĊęöĊ BMD ìĊęîšĂ÷ÖüŠć -2.5 Ēúą
öćÖÖüŠć -2.047 óïüŠćëšćĔîÖúčŠö -2.5 êšĂÜĔĀš÷ćĔîÖćøðŜĂÜÖĆîÖøąéĎÖĀĆÖĒÖŠñĎšðśü÷ÝĞćîüî 15 Ùî ĒúąðŜĂÜÖĆîÖøąéĎÖÿąēóÖ
ĀĆÖ 81 Ùî ÝċÜÝąÿćöćøëðŜĂÜÖĆîÖćøđÖĉéÖøąéĎÖĀĆÖĕéš 1 Ùî ×èąđéĊ÷üÖĆîĔîÖúčŠöñĎšðśü÷ìĊęöĊ BMD ìĊęöćÖÖüŠć -2.0 êšĂÜĔĀš÷ćĔî
ÖćøðŜĂÜÖĆîÖøąéĎÖĀĆÖĒÖŠñĎšðśü÷ÝĞćîüî 30 Ùî ÝċÜÝąÿćöćøëðŜĂÜÖĆîÖćøđÖĉéÖøąéĎÖĀĆÖĕéš 1 Ùî (êćøćÜìĊę 17.9)
êćøćÜìĊę 17.9 ÝĞćîüî Number needed to treat ×ĂÜÖćøĔßš÷ć Alendronate ĔîÿêøĊìĊęöĊÙüćöĀîćĒîŠîöüúÖøąéĎÖêęĞćìĊę
đךćøĆïÖćøøĆÖþćđðŨîđüúć 4 ðŘ đóČęĂðŜĂÜÖĆîÖćøđÖĉéÖøąéĎÖĀĆÖ47
NNT to prevent one clinical NNT to prevent one hip
Category
fracture fracture
Alendronate
baseline bone density at femoral
neck
T-score < –2.5 15 81
T-score > –2.0 30 no effect
Āöć÷đĀêč: NNT = Number needed to treat (ÝĞćîüî×ĂÜñĎšðśü÷ìĊęîšĂ÷ìĊęÿčéìĊęĕéšøĆï÷ćðŜĂÜÖĆîÖćøđÖĉéÖøąéĎÖĀĆÖđóČęĂúéÖćøđÖĉéÖøąéĎÖĀĆÖ 1 øć÷)
ðøąöćèÖćøÜïðøąöćèÖćøĔßš÷ćêšćîÖøąéĎÖóøčî×ĂÜðøąđìýĕì÷
ÝćÖøć÷ÜćîÖćøüĉđÙøćąĀŤñúÖøąìïéšćîÜïðøąöćè×ĂÜÖćøøĆÖþćēøÙÖøąéĎÖóøčîĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂî
éšü÷÷ćïîóČĚîåćî×ĂÜÖćøĔßšĒïïÝĞćúĂÜìćÜđýøþåýćÿêøŤ ēé÷õćÙüĉßćĂć÷čøýćÿêøŤ ÙèąĒóì÷ŤýćÿêøŤ öĀćüĉì÷ćúĆ÷×ĂîĒÖŠî
ĔîðŘ 255635 óïüŠćĀćÖóĉÝćøèćĔĀšÖćøøĆÖþćéšü÷÷ć Alendronate ĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂîĂć÷č 65 ðŘ×ċĚîĕð ìĊęöĊ BMD
T-score îšĂ÷ÖüŠć -2.5 ìčÖøć÷ ÝąöĊõćøąÜïðøąöćèÝćÖÖćøøĆÖþćéšü÷÷ćđÞúĊę÷ðŘúą 12,866 úšćîïćì (1.18 úšćîøć÷)
Ă÷ŠćÜĕøÖĘêćöÖćøðøąđöĉîÖćøøĆÖþćéšü÷ÖćøüĆéöüúÖøąéĎÖÝćÖđÙøČęĂÜ DXA ĔîìčÖøć÷öĊÙüćöđðŨîĕðĕéš÷ćÖĔîìćÜðäĉïĆêĉ ĀćÖ
óĉÝćøèćÖćøðøąđöĉîÙüćöđÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖéšü÷ FRAXTM êćöĒîüìćÜÖćøøĆÖþćÝćÖĒîüđüßðäĉïĆêĉ×ĂÜøćßüĉì÷ćúĆ÷
Ēóì÷ŤĂĂøŤēíðŗéĉÖÿŤĒĀŠÜðøąđìýĕì÷ ĒúąöĎúîĉíĉēøÙÖøąéĎÖóøčîĒĀŠÜðøąđìýĕì÷öćðøąÖĂïÖćøóĉÝćøèćÿĆęÜĔßš÷ć óïüŠćĔî
ÖøèĊìĊęóĉÝćøèćÖćøĔßšēĂÖćÿđÿĊę÷ÜìĊęøą÷ąđüúć 10 ðŘ ×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖìĊęêĞćĒĀîŠÜÿĞćÙĆâöćÖÖüŠćĀøČĂđìŠćÖĆï øšĂ÷úą 20.0
ĀøČĂēĂÖćÿđÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖìĊęÿąēóÖöćÖÖüŠćĀøČĂđìŠćÖĆïøšĂ÷úą 3.0 óïüŠćöĊõćøąÜïðøąöćèúéúÜđĀúČĂēé÷đÞúĊę÷
ðŘúą 2,013 úšćîïćì (185,000 øć÷) Ēúą 4,330 úšćîïćì (398,000 øć÷) êćöúĞćéĆï
ÙčèõćóÖćøïøĉÖćø (Quality of Care)
ÿëćîÖćøèŤ×ĂÜøąïïïøĉÖćøðŦÝÝčïĆî÷ĆÜĕöŠöĊךĂöĎúìĊęïŠÜßĊĚëċÜÙčèõćóïøĉÖćøéšćîÖćøÙĆéÖøĂÜĒúąøĆÖþćēøÙÖøąéĎÖ
óøčîĔîðøąđìýĕì÷ àċęÜÙüøöĊÖćøýċÖþćĒúąøüïøüöđóČęĂđðŨîðøąē÷ßîŤĔîÖćøéĎĒúñĎšðśü÷ĔîõćüąîĊĚêŠĂĕð ēé÷öĊðøąđéĘîÙčèõćó
ìĊęÿĞćÙĆâ ĕéšĒÖŠ
ÖćøđךćëċÜïøĉÖćøÿč×õćó
ÖćøđךćëċÜïøĉÖćøÿč×õćóĂćÝ÷ĆÜöĊךĂÝĞćÖĆéĀúć÷ðøąÖćø đߊî ÖćøêøüÝüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčî đîČęĂÜÝćÖðøąđìý
ĕì÷÷ĆÜöĊðøĉöćèđÙøČęĂÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖÝĞćÖĆé ÿŠüîĔĀâŠÖøąÝć÷Ă÷ĎŠđÞóćąĔîēøÜđøĊ÷îĒóì÷Ť ēøÜó÷ćïćúđĂÖßî
Ĕî×èąìĊęēøÜó÷ćïćúÝĆÜĀüĆé ēøÜó÷ćïćúßčößîÿŠüîĔĀâŠ÷ĆÜĕöŠöĊđÙøČęĂÜêøüÝéĆÜÖúŠćü ìĞćĔĀšðøąßćÖøÿŠüîĔĀâŠ÷ĆÜĕöŠĕéšøĆïÖćø
êøüÝüĆéÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ
ÖćøđךćëċÜÖćøÙĆéÖøĂÜ 17
ðŦÝÝčïĆîüĉíĊöćêøåćîìĊęĔßšĔîÖćøüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčî ÙČĂ ÖćøüĆéÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖéšü÷đÙøČęĂÜ DXA ĒêŠ
ðŦÝÝčïĆîÖćøđךćëċÜÖćøĔßšđÙøČęĂÜ÷ĆÜÝĞćÖĆé óïüŠćöĊÝĞćîüîđóĊ÷Üðøąöćè 50 đÙøČęĂÜìĆęüðøąđìý ĒúąöĊÖøąÝć÷Ă÷ĎŠêćöēøÜó÷ćïćú
êêĉ÷õĎöĉ ĀøČĂēøÜó÷ćïćúđĂÖßîđìŠćîĆĚî ĂĊÖìĆĚÜÖćøüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčîĔîðŦÝÝčïĆî ìĞćĕéšēé÷ÖćøðøąđöĉîÝćÖĒóì÷ŤĂćÝÝą
ĕöŠĕéšøĆïÖćøêøüÝéšü÷đÙøČęĂÜ ĒöšÝąöĊÖćøüĉîĉÝÞĆ÷ìĊęîĞćðŦÝÝĆ÷đÿĊę÷ÜêŠćÜė ×ĂÜēøÙöćøüöÖĆîđóČęĂÙĆéÖøĂÜĒúąðøąđöĉîÙüćöđÿĊę÷Ü
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-14 โรคกระดูกพรุน (Osteoporosis)
×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖēé÷ĂćÝĕöŠêšĂÜüĆéöüúÖøąéĎÖĔîðøąßćÖøìčÖÙî ĒêŠüĉíĊÖćøđĀúŠćîĊĚ÷ĆÜöĊךĂÝĞćÖĆéĂ÷ĎŠïšćÜĒúąêšĂÜöĊÖćø
ðøąđöĉî÷Čî÷ĆîÙüćöîŠćđßČęĂëČĂ ÖćøìĊę÷ĆÜĕöŠöĊĒîüìćÜðäĉïĆêĉĔîÖćøÙĆéÖøĂÜĒúąøĆÖþćēøÙÖøąéĎÖóøčî×ĂÜðøąđìýĕì÷ĔîðŦÝÝčïĆî
ÝċÜĂćÝÖŠĂĔĀšđÖĉéÖćøÿĉĚîđðúČĂÜÝćÖÖćøĔßš÷ćēé÷ĕöŠđĀöćąÿöĕéš
ÖćøđךćëċÜÖćøøĆÖþć
ðŦÝÝčïĆîÖćøøĆÖþćēøÙÖøąéĎÖóøčîöĊđðŜćĀöć÷đóČęĂðŜĂÜÖĆîĒúąúéÙüćöđÿĊę÷ÜĔîÖćøđÖĉéÖøąéĎÖĀĆÖ àċęÜöĊìĆĚÜÖćøøĆÖþć
ĒïïìĊęĔßš÷ćĒúąĕöŠĔßš÷ć đîČęĂÜÝćÖ÷ćøĆÖþćēøÙÖøąéĎÖóøčîĕöŠĂ÷ĎŠĔîïĆâßĊ÷ćĀúĆÖĒĀŠÜßćêĉ ÝċÜìĞćĔĀšđÖĉéÙüćöĕöŠđÿöĂõćÙ×ĂÜÖćø
đךćëċÜ÷ćĔîñĎšðśü÷ìĊęöĊøąïïðøąÖĆîÿč×õćóĒêÖêŠćÜÖĆî ÝćÖÖćøýċÖþć×ĂÜ Werayingyong48 ĒÿéÜĔĀšđĀĘîüŠć ÿŠüîĔĀâŠñĎšìĊęöćìĞć
ÖćøøĆÖþćēøÙÖøąéĎÖóøčîĔîēøÜó÷ćïćúóøąöÜÖčãđÖúšć ĔîðŘ 2549 ÷ĆÜêšĂÜĒïÖøĆïÙŠćĔߚ݊ć÷éšü÷êĆüđĂÜ øĂÜúÜöćĕéšĒÖŠñĎšöĊÿĉìíĉ
ÿüĆÿéĉÖćøøĆÖþćó÷ćïćúךćøćßÖćøĒúąÙøĂïÙøĆü đðŨîÖúčŠöìĊęÿćöćøëđךćëċÜ÷ćēøÙÖøąéĎÖóøčîĕéšöćÖÖüŠćøąïïðøąÖĆîÿč×õćó
ĂČęîė
ÙćéüŠćĔîĂîćÙêðŦâĀćđøČęĂÜÖćøðŜĂÜÖĆîÖøąéĎÖĀĆÖĔîēøÙÖøąéĎÖóøčîÝąöĊÙüćöÿĞćÙĆâöćÖ×ċĚî đóøćąĂć÷č×Ć÷đÞúĊę÷
×ĂÜÙîĕì÷đóĉęöÿĎÜ×ċĚî ĒúąÖćøöĊøąïïðøąÖĆîÿč×õćóëšüîĀîšć ÖćøóĉÝćøèćÙüćöÙčšöÙŠć×ĂÜÖćøÙĆéÖøĂÜĒúąÖćøðŜĂÜÖĆîēøÙ
ÖøąéĎÖĀĆÖĔîĀâĉÜüĆ÷ĀúĆÜĀöéðøąÝĞćđéČĂîĔîÖúčŠöĂć÷čêŠćÜė ÝċÜöĊÙüćöÿĞćÙĆâ đóøćąÝąßŠü÷ĔîÖćøüćÜĒñîÿĞćĀøĆïÝĆéÿøø
ìøĆó÷ćÖøìĊęđÖĊę÷üךĂÜìĊęöĊĂ÷ĎŠĂ÷ŠćÜÝĞćÖĆéĔĀšđÖĉéðøąÿĉìíĉõćóÿĎÜÿčé
ÖćøïøĉÖćøìĊęđðŨîìĊę÷ĂöøĆïĀøČĂÖćøĔĀšñĎšðśü÷đðŨîýĎî÷ŤÖúćÜĔîÖćøïøĉÖćøÿč×õćó
ĔîðŘ 2548 ÖøöÖćøĒóì÷Ť ÖøąìøüÜÿćíćøèÿč× ĕéšÿøšćÜĒîüìćÜđüßðäĉïĆêĉÿĞćĀøĆïēøÙÖøąéĎÖóøčî49 ēé÷öĊךĂïŠÜßĊĚ
ĔîÖćøđøĉęöêšîøĆÖþćéĆÜîĊĚ
1. ךĂïŠÜßĊĚÿĆöïĎøèŤ (absolute indication) ðøąÖĂïéšü÷ñĎšìĊęöĊÙüćöĀîćĒîŠîÖøąéĎÖÙĂ ÿąēóÖ ĀøČĂ
ÖøąéĎÖÿĆîĀúĆÜÿŠüîđĂüêęĞćÖüŠć -2.5 ÿŠüîđïĊę÷ÜđïîöćêøåćîđöČęĂđðøĊ÷ïđìĊ÷ïÖĆïüĆ÷ÿćü (T-score <-2.5) ÝćÖÖćøêøüÝéšü÷
đÙøČęĂÜ DXA ĒúąĀøČĂđÙ÷öĊÖøąéĎÖĀĆÖÝćÖÙüćöđðøćąïćÜ (fragility fracture) ĀøČĂÝćÖÖćøÖøąĒìÖìĊęĕöŠøčîĒøÜ (low
trauma fracture) ìĊęêĞćĒĀîŠÜÿĞćÙĆâĕéšĒÖŠ ÖøąéĎÖÿąēóÖ ĒúąÖøąéĎÖÿĆîĀúĆÜ
2. ךĂïŠÜßĊĚÿĆöóĆìíŤ (relative indication) ÙüøĔĀšÖćøøĆÖþćëšćöĊðŦÝÝĆ÷éĆÜêŠĂĕðîĊĚ êĆĚÜĒêŠ 2 ðŦÝÝĆ÷×ċĚîĕð
2.1 ñĎšìĊęöĊÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖĔîÿŠüîĂČęîė îĂÖđĀîČĂÝćÖÙĂ ÿąēóÖ ĒúąÖøąéĎÖÿĆîĀúĆÜ êęĞć
ÖüŠć -2.5 ÿŠüîđïĊę÷ÜđïîöćêøåćîđöČęĂđðøĊ÷ïđìĊ÷ïÖĆïüĆ÷ĀîčŠöÿćü (T-score <2.5)
2.2 ñĎšìĊęđÙ÷öĊÖøąéĎÖĀĆÖđîČęĂÜÝćÖÙüćöđðøćąïćÜĔîÿŠüîĂČęîė îĂÖđĀîČĂÝćÖÖøąéĎÖÿąēóÖĒúą
ÖøąéĎÖÿĆîĀúĆÜ
2.3 Ăć÷čđÖĉîÖüŠć 65 ðŘ
2.4 ñĎšìĊęöĊÖćøÿĎâđÿĊ÷öüúÖøąéĎÖĂ÷ŠćÜøüéđøĘü (fast bone loser) ēé÷ÿĎâđÿĊ÷ĔîĂĆêøćđøĘüÖüŠć
øšĂ÷úą 3.0 êŠĂðŘ õć÷ĔêšđÜČęĂîĕ×üŠćđÙøČęĂÜêøüÝ DXA öĊÙüćöÙúćéđÙúČęĂî (precision error ĀøČĂ coefficient of Variation
ĕöŠđÖĉîøšĂ÷úą 1.0)
2.5 ñĎšìĊęöĊÙüćöđÿĊę÷ÜÿĎÜêŠĂÖøąéĎÖĀĆÖÝćÖÙüćöđðøćąïćÜ ĕéšĒÖŠ öĊðŦÝÝĆ÷đÿĊę÷ÜêŠĂÖøąéĎÖóøčîĒúą
ðŦÝÝĆ÷đÿĊę÷ÜêŠĂÖćøĀÖúšö
ÿëćîÖćøèŤ×ĂÜøąïïïøĉÖćøĔîðŦÝÝčïĆî (Service Plan)
ĔîðŦÝÝčïĆî÷ĆÜöĊñĎšðśü÷ÝĞćîüîöćÖìĊęĕöŠĕéšøĆïÖćøüĉîĉÝÞĆ÷ēøÙÖøąéĎÖ àċęÜðŦâĀćîĊĚöćÝćÖðøąßćßîÿŠüîĔĀâŠ÷ĆÜ×ćé
ÙüćöøĎšÙüćöđךćĔÝđøČęĂÜēøÙÖøąéĎÖóøčî ïčÙúćÖøìćÜÖćøĒóì÷Ť÷ĆÜĕöŠđĀĘîÙüćöÿĞćÙĆâ×ĂÜÖćøêøüÝÙĆéÖøĂÜĒúąüĉîĉÝÞĆ÷ēøÙ
ÖøąéĎÖóøčî ĒúąēøÜó÷ćïćúÿŠüîĔĀâŠ÷ĆÜ×ćéĒÙúîđÙøČęĂÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖìĊęĕéšöćêøåćî ÝċÜìĞćĔĀšēøÙÖøąéĎÖ
óøčîĕöŠĕéšøĆïÖćøĔĀšÙüćöÿĞćÙĆâĔîÖćøøèøÜÙŤÙšîĀć ðŜĂÜÖĆî øüöìĆĚÜéĎĒúđßĉÜøčÖĔîßčößî
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-15
đÙøČęĂÜöČĂ ĂčðÖøèŤ đìÙēîēú÷ĊìćÜÖćøĒóì÷Ť
ðøąđìýĕì÷÷ĆÜöĊðŦâĀć×ćéĒÙúîđÙøČęĂÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ (dual X-rays absorptiometry) đóČęĂĔßš
ÿĞ ć ĀøĆ ï üĉ îĉ Ý ÞĆ ÷ ēøÙÖøąéĎ Ö óøč î ÿŠ ü îĔĀ⊠đ ÙøČę Ă ÜêøüÝÙüćöĀîćĒîŠ î ×ĂÜÖøąéĎ Ö ÝąöĊ Ă ÷ĎŠ ē øÜó÷ćïćú×ĂÜöĀćüĉ ì ÷ćúĆ ÷
ēøÜó÷ćïćúđĂÖßî ēøÜó÷ćïćúĔîÖøčÜđìóöĀćîÙø ĒúąēøÜó÷ćïćúýĎî÷ŤïćÜĒĀŠÜ ĒêŠĔîēøÜó÷ćïćúÝĆÜĀüĆéĒúąēøÜó÷ćïćú
ßčößî÷ĆÜ×ćéĒÙúîđÙøČęĂÜöČĂîĊĚĂ÷ĎŠ ìĞćĔĀšñĎšðśü÷ēøÙÖøąéĎÖóøčîÿŠüîĔĀâŠĕöŠĕéšøĆïÖćøüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčî ìĆĚÜîĊĚēøÙÖøąéĎÖóøčî
Ĕîøą÷ąĒøÖĕöŠöĊĂćÖćøñĉéðÖêĉÝċÜìĞćĔĀšñĎšðśü÷ĕöŠìøćïüŠćêîđĂÜđðŨîēøÙÖøąéĎÖóøčî ñĎšðśü÷ÝąöćøĆïÖćøøĆÖþćĒúąêøüÝóïĕéšÖĘ
êŠĂđöČęĂöĊõćüąÖøąéĎÖĀĆÖđÖĉé×ċĚîĒúšü ðŦâĀćÖćøîĞćđÙøČęĂÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖìĊęĕöŠĔߊüĉíĊöćêøåćîöćĔßšêøüÝ
üĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčî đîČęĂÜÝćÖðŦâĀć×ćéĒÙúîđÙøČęĂÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖàċęÜöĊøćÙćĒóÜ ÝċÜöĊÖćøîĞćÖćøêøüÝ
ÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖēé÷üĉíĊĂČęîàċęÜĕöŠĔߊüĉíĊöćêøåćî đߊî ÖćøêøüÝÙúČęîđÿĊ÷ÜÙüćöëĊęÿĎÜïøĉđüèÿšîđìšć (QUS) àċęÜöĊøćÙćĕöŠ
ĒóÜ ÿąéüÖ ĒúąÝĆéĀćÜŠć÷ ĒêŠÖĘĕöŠöĊÙüćöđìĊę÷ÜêøÜđóĊ÷ÜóĂ ÖćøĔßšñúÖćøêøüÝéšü÷üĉíĊîĊĚđóĊ÷ÜĂ÷ŠćÜđéĊ÷üĔîÖćøüĉîĉÝÞĆ÷ēøÙĒúą
êĉéêćöÖćøøĆÖþć ĂćÝìĞćĔĀšđÖĉéðŦâĀćñĉéóúćéĕéš éĆÜîĆĚîĒîüìćÜÖćøðäĉïĆêĉđóČęĂĔĀšÖćøøĆÖþćìĊęëĎÖêšĂÜĒöŠî÷ĞćöćÖ×ċĚîĔîÖøèĊìĊę
ĕöŠöĊđÙøČęĂÜêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ ÖćøêøüÝÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖéšü÷ÙúČęîđÿĊ÷ÜÙüćöëĊęÿĎÜïøĉđüèÿšîđìšćĂćÝ
îĞćöćĔßšĕéš ĒêŠÙüøĔßšøŠüöÖĆïéĆßîĊÙüćöđÿĊę÷ÜìćÜÙúĉîĉÖđóČęĂĔĀšöĊÙüćöĒöŠî÷ĞćöćÖ×ċĚîĔîÖćøðøąđöĉîÙüćöđÿĊę÷Ü×ĂÜÖćøđÖĉéēøÙ
ÖøąéĎÖóøčî
øąïïךĂöĎú ĒúąÖćøêĉéêćö
ÖćøéĎĒúøĆÖþćēøÙÖøąéĎÖóøčîĔîðøąđìýĕì÷÷ĆÜÙÜóïðŦâĀćĒúąĂčðÿøøÙĂ÷ĎŠĀúć÷ðøąÖćø àċęÜìĞćĔĀšñúÖćøøĆÖþć
ĕöŠđÖĉéðøąÿĉìíĉõćóÿĎÜÿčé éĆÜîĆĚîÙüøöĊÖćøÝĆéìĞćĒîüìćÜÖćøéĎĒúøĆÖþćēøÙÖøąéĎÖóøčîĔĀšđðŨîĕðĔîĒîüìćÜđéĊ÷üÖĆî ĒîüÙĉé
đóČęĂóĆçîćøąïïÖćøéĎĒúøĆÖþćēøÙÖøąéĎÖóøčî ÿøčðĕéšéĆÜêŠĂĕðîĊĚ
1. öĊÖćøðøąđöĉî×ĊéÙüćöÿćöćøë óĆçîćĒúąëŠć÷ìĂéÙüćöøĎšĔĀšĒÖŠïčÙúćÖø ĒúąÿîĆïÿîčîéšćîđÙøČęĂÜöČĂ
đóČęĂĔĀšÿëćîïøĉÖćøĔîĒêŠúąđ×êĔĀšÿćöćøëüĉîĉÝÞĆ÷ēøÙÖøąéĎÖóøčîĕéš
2. öĊÖćøÝĆéêĆĚÜöćêøåćîðøąđöĉîÙüćöđÿĊę÷Ü×ĂÜÖćøđÖĉéÖøąéĎÖĀĆÖĔîñĎšðśü÷ÿĎÜĂć÷čđóČęĂÝąÙĆéÖøĂÜñĎšðśü÷
ÖúčŠöđÿĊę÷ÜđךćøĆïÖćøøĆÖþćõćüąÖøąéĎÖóøčîÖŠĂîìĊęÝąđÖĉéÖøąéĎÖĀĆÖ
3. ĔĀšÙüćöøĎšÿĎŠðøąßćßîĔĀšêøąĀîĆÖëċÜÙüćöÿĞćÙĆâ×ĂÜēøÙÖøąéĎÖóøčî ĒîüìćÜðŜĂÜÖĆîĒúąøĆÖþćìĊęëĎÖêšĂÜ
4. öĊÖćøÝĆéêĆĚÜĀîŠü÷ĔĀšïøĉÖćøøĆÖþćđÞóćąēøÙÖøąéĎÖóøčî đߊî ÙúĉîĉÖēøÙÖøąéĎÖóøčî ĀĂñĎšðśü÷ÿĞćĀøĆï
ñĎšðśü÷ÿĎÜĂć÷čìĊęöĊõćüąÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčî ēé÷ïčÙúćÖøìĞćÜćîøŠüöÖĆîĒïïÿĀÿć×ćüĉßćßĊóđóČęĂéĎĒúñĎšðśü÷
5. öĊÖćøÿîĆïÿîčîĔĀšñĎšðśü÷ìĊęöĊēøÙÖøąéĎÖóøčî ĒúąÖøąéĎÖĀĆÖÝćÖõćüąÖøąéĎÖóøčî ĕéšÖćøøĆÖþćìĊęëĎÖêšĂÜ
ĒúąóĂđóĊ÷Ü ìĆĚÜìćÜéšćî÷ćøĆÖþćēøÙ đÙøČęĂÜöČĂĒúąĂčðÖøèŤ ÿĞćĀøĆïÖćøñŠćêĆéøĆÖþćÖøąéĎÖĀĆÖđóČęĂúéÙüćöđÝĘïðüé õćüą
ìčóóúõćó ĒúąĔĀšñĎšðśü÷ÖúĆïöćߊü÷đĀúČĂêĆüđĂÜĕéšđøĘüìĊęÿčé
6. ÿøšćÜđÙøČĂ׊ć÷ÖĆïÿëćîó÷ćïćúøąéĆïðåöõĎöĉ ìčêĉõĎöĉ ēé÷óĆçîćøąïïđìÙēîēú÷Ċÿćøÿîđìý đóČęĂĔĀšöĊ
øąïïðøċÖþć (consultation) øąĀüŠćÜÿëćîó÷ćïćúĕéšÿąéüÖ đóČęĂĔĀšÿëćîó÷ćïćúøąéĆïêšîÿćöćøëéĎĒúñĎšðśü÷ĕéš úéÖćø
ÿŠÜêŠĂĔîÖøèĊìĊęĕöŠÝĞćđðŨî đóČęĂðøąĀ÷ĆéđüúćĒúąÙŠćĔߚ݊ć÷ĒÖŠñĎšðśü÷
7. ÿîĆïÿîčîÖćøöĊÿŠüîøüö×ĂÜßčößîĔîÖćøéĎĒúߊü÷ôŚŪîôĎÿöøøëõćó×ĂÜñĎšÿĎÜĂć÷čìĊęöĊõćüąÖøąéĎÖĀĆÖ öĊ
ēÙøÜÖćøÿîĆïÿîčîĔĀšÙüćöøĎšđóĉęöÙüćöÿćöćøëĒÖŠĂćÿćÿöĆÙøßčößîĔîÖćøéĎĒúñĎšÿĎÜĂć÷čēøÙÖøąéĎÖóøčî
8. ÿîĆïÿîčîïčÙúćÖøĔĀšòřÖĂïøöÖćøéĎĒúøĆÖþćñĎšðśü÷ÿĎÜĂć÷čìĊęöĊõćüąÖøąéĎÖóøčî ĒúąÖćøøĆÖþćÖøąéĎÖĀĆÖ
9. ÖĞćĀîéêĆüßĊĚüĆéìĊęïŠÜïĂÖëċÜðøąÿĉìíĉõćóÖćøéĎĒúñĎšðśü÷ĒúąÖćøïøĉĀćøÝĆéÖćøõćüąēøÙÖøąéĎÖóøčî đߊî
ÙĉéĂĆêøćÝĞćîüîñĎšðśü÷ìĊęđךćøĆïÖćøøĆÖþć ĂĆêøćÖćøÿŠÜêŠĂĀøČĂđךćøĆïÖćøøĆÖþćĔîēøÜó÷ćïćú ĂĆêøćêć÷ ĒúąõćüąĒìøÖàšĂî
×ĂÜñĎšðśü÷ÖøąéĎÖĀĆÖÝćÖēøÙÖøąéĎÖóøčîĔîēøÜó÷ćïćú öĊÖćøÝĆéìĞćÖćøðøąßčö Morbidity and Mortality conference,
Root Cause Analysis
10. öĊøąïïêĉéêćöñĎšðśü÷ìĊęĕéšøĆïÖćøøĆÖþćõćüąÖøąéĎÖĀĆÖĀúĆÜĂĂÖÝćÖēøÜó÷ćïćúĔĀšÙüćöߊü÷đĀúČĂ 17
ñĎšðśü÷ĒúąÙøĂïÙøĆüĔîÖćøôŚŪîôĎ ÿöøøëõćó ĒúąĒîąîĞćĒîüðŜĂÜÖćøĀÖúšöĔîñĎšÿĎÜĂć÷č øüöìĆĚÜêĉéêćöĔĀšñĎšðśü÷øĆïÖćøøĆÖþć
õćüąÖøąéĎÖóøčîêŠĂđîČęĂÜ ÖćøðŜĂÜÖĆîĀÖúšöēé÷đÞóćąÖćøĂĂÖÖĞćúĆÜÖć÷ óïüŠćÿćöćøëúéÖćøĀÖúšöĔîñĎšÿĎÜĂć÷čĕéšñúÝøĉÜ
ÖćøýċÖþćĔî Cochrane review óïüŠćÖćøĂĂÖÖĞćúĆÜÖć÷ đߊî ÖćøøĞćĕìđÖŢÖĔîñĎšÿĎÜĂć÷čߊü÷úéÖćøĀÖúšöĕéš50 Tousignant51
ĕéšìĞćÖćøýċÖþćĒïïÿčŠöđÖĊę÷üÖĆïÖćøøĞćĕìđÖŢÖĔîñĎšðśü÷Ăć÷čöćÖìĊęĂŠĂîĒĂĔîðøąđìýĒÙîćéć ÝĞćîüî 76 Ùî Ĕî 15 ÿĆðéćĀŤ ÖĆï
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-16 โรคกระดูกพรุน (Osteoporosis)
ÖćøìĞćÖć÷õćóïĞćïĆéĒïïðÖêĉ óïüŠćìĆĚÜ 2 Ă÷ŠćÜÿćöćøëúéÖćøĀÖúšöĕéš ēé÷ÖúčŠöìĊęøĞćĕìđÖŢÖúéÖćøúšöĕéšéĊÖüŠć ÿĞćĀøĆïĔî
đøČęĂÜ cost effectiveness îĆĚî Frick52 ĕéšìĞćÖćøýċÖþćđðøĊ÷ïđìĊ÷ïÙüćöÙčšöÙŠć ēé÷Ĕßš mathematical epidemiological
model ÙĞćîüèĒúšüóïüŠć ÖćøøĆÖþćēé÷ psychotropics ĒúąøĞćĕìđÖŢÖđðŨîÖćøøĆÖþćìĊęëĎÖìĊęÿčé ĒúąĔĀšñúéĊöćÖìĊęÿčéĔîÖćø
øąüĆÜÖćøúšö
ךĂđÿîĂđóČęĂÖćøýċÖþć üĉÝĆ÷ ĒúąÝĆéÖćøÙüćöøĎš
ĔîðŦÝÝčïĆîëċÜĒöšÝąöĊÖćøýċÖþćđÖĊę÷üÖĆïēøÙÖøąéĎÖóøčîĒúąöĊÖćøóĆçîćĂÜÙŤÙüćöøĎšêŠćÜė ìĆĚÜÙüćöøĎšóČĚîåćî Ēúą
ìćÜÙúĉ îĉÖ ĒêŠÖĘ ÷ĆÜ öĊךà ÝĞć ÖĆé Āúć÷ðøąÖćø ñúÖćøýċ Ö þćïćÜĂ÷Šć Ü÷Ć Ü öĊך Ă ēêšĒ ÷šÜ ÖĆ î Ýċ Ü ÝĞć đðŨî êš Ă ÜöĊÖ ćøýċÖ þćđóĉęö đêĉ ö
êĆüĂ÷ŠćÜđߊî ÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ ÖĆïÙüćöđÿĊę÷ÜêŠĂÖćøđÖĉéÖøąéĎÖĀĆÖ ÝćÖÖćøýċÖþćóïÙüćöÿĆöóĆîíŤ×ĂÜÙüćöĀîćĒîŠî
ÖøąéĎÖìĊęúéúÜĒêŠöĊÙüćöđÿĊę÷ÜìĊęÝąđÖĉéÖøąéĎÖĀĆÖöćÖ×ċĚî23 ĒêŠøć÷ÜćîĀúć÷ÞïĆïìĊęóïüŠćñĎšðśü÷ÖøąéĎÖÿąēóÖĀĆÖđÖČĂïøšĂ÷úą
50.0 öĊÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖĕöŠĂ÷ĎŠĔîđÖèæŤÖøąéĎÖóøčî53-55 ĒúąñúÝćÖÖćøøĆÖþćéšü÷÷ćøĆÖþćÖøąéĎÖóøčî óïüŠćìĞćĔĀš
ÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖđóĉęö×ċĚî ĒêŠñúĔîÖćøðŜĂÜÖĆîÖćøđÖĉéÖøąéĎÖĀĆÖÖúĆïúéúÜđóĊ÷ÜđúĘÖîšĂ÷ ĒúąĕöŠÿĆöóĆîíŤÖĆïÙüćö
ĀîćĒîŠî×ĂÜÖøąéĎÖìĊęđóĉęö×ċĚî ÝćÖךĂöĎúéĆÜÖúŠćüìĞćĔĀšđÖĉéĒîüÙĉéðŦÝÝĆ÷ĂČęîė îĂÖđĀîČĂÝćÖÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖìĊęöĊñú
êŠĂÖćøđÖĉéÖøąéĎÖĀĆÖ àċęÜîĞćöćÿĎŠÖćøýċÖþćÙčèõćó×ĂÜÖøąéĎÖ éĆÜîĆĚîÖćøýċÖþćüĉÝĆ÷ÙüøđîšîĕðĔîìćÜÖćøüĉÝĆ÷ÙšîĀćüĉíĊÖćø
êøüÝðøąđöĉîÙčèõćó×ĂÜÖøąéĎÖ ĒúąÖćøøĆÖþćìĊęÿćöćøëđóĉęöÙčèõćó×ĂÜÖøąéĎÖöćÖÖüŠćìĊęđîšîđóĊ÷ÜÙüćöĀîćĒîŠî×ĂÜ
ÖøąéĎÖđóĊ÷ÜĂ÷ŠćÜđéĊ÷ü
ÜćîüĉÝĆ÷ìćÜÙúĉîĉÖ×ĂÜēøÙÖøąéĎÖóøčî đߊî ðŦÝÝĆ÷đÿĊę÷ÜĀøČĂÙüćöîŠćÝąđðŨîĔîÖćøđÖĉéÖøąéĎÖĀĆÖ (fracture
probability) ĀøČĂ éĆßîĊÙüćöđÿĊę÷ÜìćÜÙúĉîĉÖ (clinical risk index) ÿŠüîĔĀâŠđðŨîÖćøýċÖþćĔîðøąđìýêąüĆîêÖĔîðøąßćÖø
ñĉü×ćü àċęÜöĊךĂÝĞćÖĆéĔîÖćøîĞćöćĔßšĔîìćÜðäĉïĆêĉ đîČęĂÜÝćÖ÷ĆÜ×ćéÖćøìéÿĂïĔîÙîĕì÷ éĆÜîĆĚîĒîüìćÜÖćøýċÖþćüĉÝĆ÷Ùüø
ìĞćÖćøýċÖþćðŦÝÝĆ÷ìćÜÙúĉîĉÖ×ĂÜēøÙÖøąéĎÖóøčîĔîÖúčŠöðøąßćÖøßćüĕì÷ ĒúąÙüøöĊÖćøìéÿĂïÙüćöĒöŠî÷ĞćđóČęĂìĊęÝą
îĞćöćĔßšĔîìćÜðäĉïĆêĉ àċęÜݹߊü÷ÙĆéÖøĂÜñĎšìĊęĕöŠöĊÙüćöÝĞćđðŨîĔîÖćøÿŠÜêøüÝüĆéÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖ øüöìĆĚÜ÷ĆÜđðŨîđÙøČęĂÜ
ĔîÖćøêĆéÿĉîĔÝøĆÖþćĔîÖøèĊìĊęĕöŠÿćöćøëêøüÝüĆéÙüćöĀîćĒîŠî×ĂÜÖøąéĎÖĕéš
đîČęĂÜÝćÖÖćøêøüÝĀćēøÙÖøąéĎÖóøčîéšü÷ÖćøüĆéÙüćöĀîćĒîŠîÖøąéĎÖĒúą÷ćøĆÖþćēøÙÖøąéĎÖóøčîöĊøćÙćĒóÜ
éĆÜîĆĚîÙüøöĊÖćøýċÖþćÙüćöÙčšöÙŠćĔîđßĉÜđýøþåýćÿêøŤìćÜÿćíćøèÿč×đóČęĂĔĀšđÖĉéÙüćöÙčšöÙŠćÿĎÜÿčéĔîøąéĆïðøąđìý ðŦÝÝčïĆî
ðøąđìýĕì÷÷ĆÜĕöŠöĊךĂöĎúÖćøýċÖþćøą÷ą÷ćüđóČęĂêĉéêćöÖćøđÖĉéÖøąéĎÖĀĆÖĔîøąéĆïðøąßćÖø éĆÜîĆĚîÝċÜÙüøöĊøąïïÖćøÝĆéđÖĘï
ךĂöĎúìćÜøąïćéüĉì÷ć đߊî ÙüćößčÖ×ĂÜēøÙÖøąéĎÖóøčî ĂčïĆêĉÖćøèŤ×ĂÜÖøąéĎÖÿąēóÖĀĆÖ ÖøąéĎÖÿĆîĀúĆÜĀĆÖ ĂĆêøćêć÷
øüöìĆĚÜÿč×õćóēé÷øüöõć÷ĀúĆÜÖøąéĎÖĀĆÖ
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-17
đĂÖÿćøĂšćÜĂĉÜ (References)
1. Osteoporosis prevention, diagnosis and therapy NIH concensus statements 2000;17:1-36.
2. Chavassieux PM, Delmas PD. Bone remodeling: biochemical markers or bone biopsy? J Bone Miner
Res 2006;21:178-9; author reply 80.
3. World Health Organization. Assessment of fracture risk and its application to screening for
postmenopausal osteoporosis. No 843 of technical reports series 1994;Geneva.
4. Chariyalertsak S, Suriyawongpisal P, Thakkinstain A. Mortality after hip fractures in Thailand. Int
Orthop 2001;25:294-7.
5. Jitapunkul S, Yuktanandana P. Consequences of hip fracture among Thai women aged 50 years and
over: a prospective study. Journal of the Medical Association of Thailand = Chotmaihet thangphaet.
2000 Dec;83(12):1447-51.
6. Chariyalertsak S, Suriyawongpisal P, Thakkinstain A. Mortality after hip fractures in Thailand.
International orthopaedics. 2001;25(5):294-7
7. Suriwongpaisal P CS, Wanvarie S. Quality of life and functional status of patients with hip fractures in
Thailand. Southeast Asian J Trop Med Public Health 2003;34:427-32.
8. Pongchaiyakul C, Songpattanasilp T, Taechakraichana N. Burden of osteoporosis in Thailand. J Med
Assoc Thai 2008;91:261-7.
9. Krall EA, Dawson-Hughes B. Heritable and life-style determinants of bone mineral density. J Bone
Miner Res 1993;8:1-9.
10. Taaffe DR, Robinson TL, Snow CM, Marcus R. High-impact exercise promotes bone gain in well-trained
female athletes. J Bone Miner Res 1997;12:255-60.
11. Consensus Development Conference: prophylaxis and treatment of osteoporosis. Am J Med
1991;90:107-10.
12. Taechakraichana N, Angkawanich P, Panyakhamlerd K, Limpaphayom K. Postmenopausal
osteoporosis: what is the real magnitude of the problem in the Thai population? J Med Assoc Thai
1998;81:397-401.
13. Limpaphayom KK, Taechakraichana N, Jaisamrarn U, et al. Prevalence of osteopenia and osteoporosis
in Thai women. Menopause 2001;8:65-9.
14. Lau EM, Lee JK, Suriyawongpaisal P, Saw SM, Das De S, Khir A, et al. The incidence of hip fracture in
four Asian countries : the Asian Osteoporosis Study (AOS). Osteoporos Int 2001;12:239-43.
15. United Nations Development for Economic and Social Information and Policy Analysis, Population
Division. World population prospects, the 1994 revision. New York: United Nations, 1995.
16. Alpha Research, Manager Information Services. Pocket Thailand Public Health 1995. Bangkok: Sukhum
and Sons, 1994:29.
17. Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures
with back pain and function: a prospective study. Ann Intern Med 1998;128:793-800.
18. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and
mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group.
Arch Intern Med 1999;159:1215-20. 17
19. Pongchaiyakul C, Nguyen ND, Jones G, Center JR, Eisman JA, Nguyen TV. Asymptomatic vertebral
deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective
study. J Bone Miner Res 2005;20:1349-55.
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-18 โรคกระดูกพรุน (Osteoporosis)
20. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of
osteoporotic fracture in men and women: an observational study. Lancet 1999;353:878-82.
21. Burge RT WD, Johansen A, Bhattacharyya S, Bose U. The cost of osteoporotic fractures in the UK:
projections for 2000-2020. J Med Econ 2001;4:51-62.
22. Ray NF, Chan JK, Thamer M, Melton LJ, 3rd. Medical expenditures for the treatment of osteoporotic
fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone
Miner Res 1997;12:24-35.
23. Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict
occurrence of osteoporotic fractures. BMJ 1996;312:1254-9.
24. Kanis JA, Black D, Cooper C, Dargent P, Dawson HB, De LC, et al; International Osteoporosis
Foundation; National Osteoporosis Foundation. A new approach to the development of assessment
guidelines for osteoporosis. Osteoporosis Int 2002; 13(7):527-36.
25. FRAX. [Internet]. WHO fracture risk assessment tool [cite 2014 Jul 29]. Available from:
http://www.shef.ac.th/FRAX.
26. Koh LK, Sedrine WB, Torralba TP, Kung A, Fujiwara S, Chan SP, et al. A simple tool to identify asian
women at increased risk of osteoporosis. Osteoporosis Int 2001;12:699-705
27. Pongchaiyakul C, Nguyen ND, Pongchaiyakul C, Nguyen TV. Development and validation of a new
clinical risk index for prediction of osteoporosis in Thai women. J Med Assoc Thai 2004;87:910-6.
28. Pongchaiyakul C, Panichkul S, Songpatanasilp T, Nguyen TV. A nomogram for predicting osteoporosis
risk based on age, weight and quantitative ultrasound measurement. Osteoporos Int 2007;18:525-31.
29. Kanis JA, Melton LJ, 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J
Bone Miner Res 1994;9:1137-41.
30. Julia Hipisley-Cox, University of Nottingham Validation of QFracture and FRAX for NICE 2011.
31. Panichyawat N, Tanmahasamut P. Comparison of OSTA index and KKOS scoring system for prediction
of osteoporosis in postmenopausal women who attended Siriraj Menopause Clinic. J Med Assoc Thai
2012;95:1365-71.
32. Pongchaiyakul C, Wanothayaroj E. Performance of the Khon Kaen Osteoporosis Study (KKOS) score
for identifying osteoporosis in men. J Med Assoc Thai 2007;90:1518-23.
33. Pongchaiyakul C, Panichkul S, Songpatanasilp T. Combined clinical risk indices with quantitative
ultrasound calcaneus measurement for identifying osteoporosis in Thai postmenopausal women. J
Med Assoc Thai 2007;90:2016-23.
34. øćßüĉì÷ćúĆ÷Ēóì÷ŤĂĂøŤēíðŗéĉÖÿŤĒĀŠÜðøąđìýĕì÷, öĎúîĉíĉēøÙÖøąéĎÖóøčîĒĀŠÜðøąđìýĕì÷. ĒîüðäĉïĆêĉïøĉÖćøÿćíćøèÿč×
ēøÙÖøąéĎÖóøčî ó.ý. 2553 [ĂĉîđìĂøŤđîĘê]. 2553 [đךćëċÜđöČęĂ 29 Ö.Ù. 2557]. đךćëċÜĕéšÝćÖ:
http://www.rcost.or.th/thai/data/2554/Guideline_osteoporosis2011.pdf.
35. ðùþåóø ÖĉęÜĒÖšü, ÞĆêøđúĉý óÜþŤĕß÷Öčú, ÿčöćúĆ÷ ÿöõĉìĆÖþŤ, íîóø ïčþïćüĕú, ÷ý êĊøąüĆçîćîîìŤ. øć÷ÜćîüĉÝĆ÷ÞïĆï
ÿöïĎøèŤ ÖćøðøąđöĉîÙüćöÙčšöÙŠć×ĂÜÖćøÙĆéÖøĂÜĒúąÖćøøĆÖþćēøÙÖøąéĎÖóøčî ĔîñĎšĀâĉÜüĆ÷ĀöéðøąÝĞćđéČĂî. ēÙøÜÖćø
ðøąđöĉîđìÙēîēú÷ĊĒúąîē÷ïć÷éšćîÿč×õćó õćÙüĉßćĂć÷čøýćÿêøŤ ÙèąĒóì÷ŤýćÿêøŤ öĀćüĉì÷ćúĆ÷×ĂîĒÖŠî; 2556
36. Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture
prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA
2005;293:2257-64.
37. Englund U, Littbrand H, Sondell A, Pettersson U, Bucht G. A 1-year combined weight-bearing training
program is beneficial for bone mineral density and neuromuscular function in older women.
Osteoporos Int 2005;16:1117-23.
Thailand Medical Services Profile 2011 - 2014
โรคกระดูกพรุน (Osteoporosis) 17-19
38. Stevenson M, Jones ML, De Nigris E, Brewer N, Davis S, Oakley J. A systematic review and economic
evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and
treatment of postmenopausal osteoporosis. Health Technol Assess 2005;9:1-160.
39. Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M. Treatment of established osteoporosis:
a systematic review and cost-utility analysis. Health Technol Assess 2002;6:1-146.
40. Schousboe JT, Nyman JA, Kane RL, Ensrud KE. Cost-effectiveness of alendronate therapy for
osteopenic postmenopausal women. Ann Intern Med 2005;142:734-41.
41. Kanis JA, Burlet N, Cooper C, Delmas PD. Reginster JY, Borgstrom F, Rizzoli R. European guidance for
the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int
2008;19:399-428.
42. Pols HA, Felsenberg D, Hanley DA, Stepan J, Munoz-Torres M, Wilkin TJ, et al. Multinational, placebo-
controlled, randomized trial of the e.ects of alendronate on bone density and fracture risk in
postmenopausal women with low bone mass: results of the FOSIT study. Fosamax International Trial
Study Group. Osteoporos Int 1999;9:461-8.
43. Heaney RP, Zizic TM, Fogelman I, Olszynski WP, Geusens P, Kasibhatla C, et al. Risedronate Reduces the
Risk of First Vertebral Fracture in Osteoporotic Women. Osteoporos Int 2002;13:501-5.
44. Harrington JT, Ste-Marie LG, Brandi ML, Civitelli R, Fardellone P, Grauer A, et al. Risedronate Rapidly
Reduces the Risk for Nonvertebral Fractures in Women with Postmenopausal Osteoporosis. Calcif
Tissue Int 2004;74:129-35.
45. Fleurence RL, Iglesias CP, Johnson JM. The cost effectiveness of bisphosphonates for the prevention
and treatment of osteoporosis: a structured review of the literature. Pharmacoeconomics
2007;25:913-33.
46. Raftery J. NICE: faster access to modern treatments? Analysis of guidance on health technologies.
BMJ 2001;323:1300-3.
47. Ebeling PR. Bisphosphonates clinical applications in osteoporosis. Aust Prescr 2000;23:133-6.
48. Werayingyong P. Health resource utilization of osteoporosis patients at Phramongkutklao Hospital
[Master of Science in Pharmacy]. Nakhon Pathom: Mahidol University; 2006.
49. ÿĞćîĆÖóĆçîćüĉßćÖćøĒóì÷Ť ÖøöÖćøĒóì÷Ť ÖøąìøüÜÿćíćøèÿč×. ĒîüìćÜđüßðäĉïĆêĉđøČęĂÜēøÙÖøąéĎÖóøčî. îîìïčøĊ: ēøÜ
óĉöóŤßčöîčöÿĀÖøèŤÖćøđÖþêøĒĀŠÜðøąđìýĕì÷; 2548. Āîšć 12.
50. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people
living in the community. The Cochrane database of systematic reviews 2012;9:CD007146.
51. Tousignant M, Corriveau H, Roy PM, Desrosiers J, Dubuc N, Hebert R. Efficacy of supervised Tai Chi
exercises versus conventional physical therapy exercises in fall prevention for frail older adults: a
randomized controlled trial. Disability and rehabilitation 2013;35:1429-35.
52. Frick KD, Kung JY, Parrish JM, Narrett MJ. Evaluating the cost-effectiveness of fall prevention programs
that reduce fall-related hip fractures in older adults. Journal of the American Geriatrics Society
2010;58:136-41.
53. Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD. Identification of osteopenic women at
high risk of fracture: the OFELY study. J Bone Miner Res 2005;20:1813-9.
54. Schuit SC, van der Klift M, Weel AE, et al. Fracture incidence and association with bone mineral 17
density in elderly men and women: the Rotterdam Study. Bone 2004;34:195-202.
55. Wainwright SA, Marshall LM, Ensrud KE, et al. Hip fracture in women without osteoporosis. J Clin
Endocrinol Metab 2005;90:2787-93.
การแพทยไทย ๒๕๕๔-๒๕๕๗ First Edition
17-20 โรคกระดูกพรุน (Osteoporosis)
Thailand Medical Services Profile 2011 - 2014
You might also like
- Anatomy ราม 2559 & ใบประกอบ 2558-9Document70 pagesAnatomy ราม 2559 & ใบประกอบ 2558-9Zatann Angel100% (1)
- แนวทางการดูแลรักษากลุ่มอาการสูงอายุ 2558Document142 pagesแนวทางการดูแลรักษากลุ่มอาการสูงอายุ 2558THATAPZ0% (1)
- ราชวิถี อาชีวเวชศาสตร์Document36 pagesราชวิถี อาชีวเวชศาสตร์Angela DuangchitNo ratings yet
- โรคมะเร็ง (Cancer)Document36 pagesโรคมะเร็ง (Cancer)HiiNo ratings yet
- หนังสือ คู่มือศึกษาความหลากหลาย เห็ด (Mushrooms) - compressedDocument160 pagesหนังสือ คู่มือศึกษาความหลากหลาย เห็ด (Mushrooms) - compressedAlpameawNo ratings yet
- อุ๋งอิ๋งDocument13 pagesอุ๋งอิ๋งChotika InbutNo ratings yet
- kinnaree chai,+วารสาร+ฉ.3+เรื่องที่+14Document17 pageskinnaree chai,+วารสาร+ฉ.3+เรื่องที่+14Mor OB-GYNNo ratings yet
- การผลิตภาชนะชีวภาพจากผักตบชวาDocument14 pagesการผลิตภาชนะชีวภาพจากผักตบชวาmercurybkkNo ratings yet
- คู่มือสำรวจแมลงDocument100 pagesคู่มือสำรวจแมลงnv5dhbtfcnNo ratings yet
- b7afca163d495614d310e0b9d2feeb6aDocument66 pagesb7afca163d495614d310e0b9d2feeb6aCenny EndearNo ratings yet
- GTE092Document5 pagesGTE092MaxMaximumNo ratings yet
- eauheritagestaff,+##default.groups.name.manager##,+10 วิวรณ์+วงศ์อรุณDocument13 pageseauheritagestaff,+##default.groups.name.manager##,+10 วิวรณ์+วงศ์อรุณsuriyaporn kamonthomNo ratings yet
- (2559) เขตปกครองพิเศษคลองเตยฯDocument34 pages(2559) เขตปกครองพิเศษคลองเตยฯArjin ThongyuukongNo ratings yet
- เล่มปรับพื้นฐานชีววิทยา 64 สมบูรณ์Document26 pagesเล่มปรับพื้นฐานชีววิทยา 64 สมบูรณ์Pigletpooh PoohNo ratings yet
- บ้านครอบครัวไทยร่วมสมัย 2 PDFDocument77 pagesบ้านครอบครัวไทยร่วมสมัย 2 PDFPlakaemNo ratings yet
- WNT Signaling CPEDocument14 pagesWNT Signaling CPEศักดิ์ชัย พูนศรีเจริญกุลNo ratings yet
- 213481911 ซักประวัติได อย างตรงประเด นในเวลาที จำกัดDocument36 pages213481911 ซักประวัติได อย างตรงประเด นในเวลาที จำกัดเกมกวี MedicalStudentNo ratings yet
- filesNameCONTENT1051935443083 PDFDocument8 pagesfilesNameCONTENT1051935443083 PDFfuyuck12345No ratings yet
- ข้อสอบโอเน็ตการงานปี2550Document46 pagesข้อสอบโอเน็ตการงานปี2550Arisara SasomNo ratings yet
- บ้านครอบครัวไทยร่วมสมัย 1Document66 pagesบ้านครอบครัวไทยร่วมสมัย 1PlakaemNo ratings yet
- Back PainDocument54 pagesBack PainthaispineclinicNo ratings yet
- Hip frac มชDocument43 pagesHip frac มชThanawat SimaNo ratings yet
- 2.Cell & Microscope - ของนักเรียน ปี 2566Document17 pages2.Cell & Microscope - ของนักเรียน ปี 2566พศิกาญจน์ ยางสูงNo ratings yet
- Guideline For Management of OA KneeDocument32 pagesGuideline For Management of OA KneeNattawara KampirapawongNo ratings yet
- สไลด์กระดูกพรุน PDFDocument16 pagesสไลด์กระดูกพรุน PDFTrithep PannawatsakunNo ratings yet
- 03 253377 Siravich v4n2Document8 pages03 253377 Siravich v4n2Rapeepan JutananNo ratings yet
- Hip FXDocument16 pagesHip FXVutthivong MnvNo ratings yet
- เฉลยใบงานเคมี 2Document142 pagesเฉลยใบงานเคมี 2ปุณ ปุณณวิชญ์ ก้อนนาคNo ratings yet
- ฟอนต์เส้นประ2แบบภาค3Document10 pagesฟอนต์เส้นประ2แบบภาค3ซาหริม อึนNo ratings yet
- คู่มือการดูแลโรคตาเบื้องต้นDocument54 pagesคู่มือการดูแลโรคตาเบื้องต้นSupalerk Kowinthanaphat50% (4)
- โรคข้อเสื่อมDocument45 pagesโรคข้อเสื่อมHom Jee WonNo ratings yet
- เอกสาร วิทยากรแผนการสอน 63Document34 pagesเอกสาร วิทยากรแผนการสอน 63Nunthawun KhoomthongNo ratings yet
- เอกสาร วิทยากรแผนการสอน 63Document34 pagesเอกสาร วิทยากรแผนการสอน 63Nunthawun KhoomthongNo ratings yet
- บ้านครอบครัวไทยร่วมสมัย 6 PDFDocument68 pagesบ้านครอบครัวไทยร่วมสมัย 6 PDFPlakaemNo ratings yet
- KnowDocument22 pagesKnowแก้มใส GahMzNo ratings yet
- สื่อระบบกระดูกDocument39 pagesสื่อระบบกระดูกSuwapit BoonrangkawNo ratings yet
- d47205cb605b4ba396c42aa52423d2e5Document16 pagesd47205cb605b4ba396c42aa52423d2e5Lala lola 757No ratings yet
- บ้านครอบครัวไทยร่วมสมัย 5 PDFDocument95 pagesบ้านครอบครัวไทยร่วมสมัย 5 PDFPlakaemNo ratings yet
- รพศรพทDocument3 pagesรพศรพทpondchoNo ratings yet
- กล้ามเนื้อ เกณฑ์วินิจฉัยโรคกระดูกกล้ามเนื้อและโครงร่าง PDFDocument34 pagesกล้ามเนื้อ เกณฑ์วินิจฉัยโรคกระดูกกล้ามเนื้อและโครงร่าง PDFNop KongNo ratings yet
- การทดสอบสมรรถภาพทางกายวัยผู้สูงอายุDocument9 pagesการทดสอบสมรรถภาพทางกายวัยผู้สูงอายุคนบางแคร์ แคร์บางคน0% (1)
- TDRG 633 VSup 11 Fin CDocument289 pagesTDRG 633 VSup 11 Fin CmintunlananobgynNo ratings yet
- แผนการออกกำลังกาย นายอดิศร คุตโคสาย Tme2n 623Document7 pagesแผนการออกกำลังกาย นายอดิศร คุตโคสาย Tme2n 623Adisron KhutkhoNo ratings yet
- Thai Guideline Osteoporosis 2021Document26 pagesThai Guideline Osteoporosis 2021Nattawara KampirapawongNo ratings yet
- ตารางสอน ตารางสอบ ตารางคลินิก ปีการศึกษา 2563Document9 pagesตารางสอน ตารางสอบ ตารางคลินิก ปีการศึกษา 2563wits joobNo ratings yet
- Japanese101HD 2022aoysensei (v2) PDFDocument35 pagesJapanese101HD 2022aoysensei (v2) PDFSirawit BumrungsriNo ratings yet
- เวทีเสวนา ร่วมพัฒนาระบบสุขภาพชุมชน ครั้งที่ 7 เรื่อง การจัดการโรคเรื้อรังในชุมชนDocument106 pagesเวทีเสวนา ร่วมพัฒนาระบบสุขภาพชุมชน ครั้งที่ 7 เรื่อง การจัดการโรคเรื้อรังในชุมชนadkittipong100% (1)
- ExampleDocument23 pagesExampleปกป้อง คับNo ratings yet
- ปทรูปสิทธิบาลีDocument492 pagesปทรูปสิทธิบาลีNabhadr BijjayeshbaipoolvangshaNo ratings yet
- ภาวะภูมิคุ้มกันไวเกินจากยาเคมีบำบัดกลุ่มแพลทินัมDocument9 pagesภาวะภูมิคุ้มกันไวเกินจากยาเคมีบำบัดกลุ่มแพลทินัมเด็กชายสมันตภัทร แฟนคลับอาจารย์กวงNo ratings yet
- TDRG 633 VSup 44 Fin CDocument276 pagesTDRG 633 VSup 44 Fin CmintunlananobgynNo ratings yet
- Sheet 2565-2-08-09Document18 pagesSheet 2565-2-08-09Watsana MahasinNo ratings yet
- แนวทางเวชปฏิบัติการดูแลรักษาผู้ป่วยท้องDocument90 pagesแนวทางเวชปฏิบัติการดูแลรักษาผู้ป่วยท้องPasut ChangeNo ratings yet
- คู่มือการปฏิบัติตามมาตรฐานจีเอพี มกษ.7436-2563 สำหรับฟาร์มเลี้ยงสัตว์น้ำเพื่อการบริโภคDocument12 pagesคู่มือการปฏิบัติตามมาตรฐานจีเอพี มกษ.7436-2563 สำหรับฟาร์มเลี้ยงสัตว์น้ำเพื่อการบริโภคStuart GlasfachbergNo ratings yet
- Md 306 สมถกัมมัฏฐาน 40 วิธีDocument156 pagesMd 306 สมถกัมมัฏฐาน 40 วิธีSutus AramrattanaNo ratings yet
- อจท แบบวัดฯคณิตศาสตร์ม 3Document24 pagesอจท แบบวัดฯคณิตศาสตร์ม 3PraeMaiSamart73% (11)
- ฟอมเคส Stady เลือกสรร22Document90 pagesฟอมเคส Stady เลือกสรร22ketsara95302No ratings yet