Professional Documents
Culture Documents
Dental MI EHB High 2024
Dental MI EHB High 2024
Uploaded by
Clifton JuraCopyright:
Available Formats
You might also like
- (Medicalstudyzone - Com) Medicine - Irfan Masood LatestDocument701 pages(Medicalstudyzone - Com) Medicine - Irfan Masood LatestMajid Ahmed FareaNo ratings yet
- Dental CodingDocument74 pagesDental CodingSakshi Bishnoi100% (2)
- NUR 3032 Immune System Study PlanDocument5 pagesNUR 3032 Immune System Study PlanThalia Fortune100% (1)
- Banco Kap. - CK 2Document1,099 pagesBanco Kap. - CK 2Lucas OrtizNo ratings yet
- Dental OH EHB Low 2024Document3 pagesDental OH EHB Low 2024Clifton JuraNo ratings yet
- Da Kim 01-23-2024 DD WEBDocument4 pagesDa Kim 01-23-2024 DD WEBhaWk FYZiXNo ratings yet
- Delta Dental Individual Enrollee Overview Flyer Plan III II Notre DameDocument2 pagesDelta Dental Individual Enrollee Overview Flyer Plan III II Notre DameObi-Wan KenobiNo ratings yet
- Premier 2000 NWDocument2 pagesPremier 2000 NWacolyteNo ratings yet
- Dental Plan Side-By-Side Comparison: Fast FactsDocument2 pagesDental Plan Side-By-Side Comparison: Fast FactsellenNo ratings yet
- Unitedhealthcare Dental Ppo Plan 2022 Summary of Benefits and CoverageDocument1 pageUnitedhealthcare Dental Ppo Plan 2022 Summary of Benefits and CoverageAdam CliftonNo ratings yet
- Delta Dental Plan Compare Highlight SheetDocument2 pagesDelta Dental Plan Compare Highlight SheetTiffany BarnesNo ratings yet
- 2022 Dental Plan BenefitsDocument1 page2022 Dental Plan BenefitsBrian ThurmondNo ratings yet
- Safari - Mar 11, 2019 at 11:00 PM PDFDocument1 pageSafari - Mar 11, 2019 at 11:00 PM PDFjohn jugoNo ratings yet
- Dental PrivilegioDocument11 pagesDental PrivilegioCarlos Andres ANo ratings yet
- Aetna Dental High DmoDocument5 pagesAetna Dental High DmoBeau PeskaNo ratings yet
- Dental Services Low Plan: PreventativeDocument2 pagesDental Services Low Plan: PreventativeIan PeabodyNo ratings yet
- 2021 2022 Aetna Justworks Dental Dmo Benefit SummaryDocument10 pages2021 2022 Aetna Justworks Dental Dmo Benefit SummarySunflowieNo ratings yet
- Dental by Design Broch 5.10Document16 pagesDental by Design Broch 5.10raviNo ratings yet
- 2022 1027 Ahs SD 1058-1 BroDocument8 pages2022 1027 Ahs SD 1058-1 BroFernanda VargasNo ratings yet
- 3610 - DENTAL Smart Health - Certificate-Revised 12 - 8 - 17-SalDocument28 pages3610 - DENTAL Smart Health - Certificate-Revised 12 - 8 - 17-SalOkolokin JohnsonNo ratings yet
- Snap Guardian Dental Plan Summary 2022Document4 pagesSnap Guardian Dental Plan Summary 2022Samson FungNo ratings yet
- 2021 2022 Aetna Justworks Dental Low Ppo 3 Benefit SummaryDocument10 pages2021 2022 Aetna Justworks Dental Low Ppo 3 Benefit SummarySunflowieNo ratings yet
- Cod Capitol 6 Nume Capitol (Engleza) Dental Services Nume Capitol (Romana) Servicii DentareDocument15 pagesCod Capitol 6 Nume Capitol (Engleza) Dental Services Nume Capitol (Romana) Servicii DentareMihaela VelcuNo ratings yet
- Ottonova Highlights For Dental InsuranceDocument2 pagesOttonova Highlights For Dental Insurancetomislavdrvar798No ratings yet
- Dental AwarenessDocument100 pagesDental AwarenessShourya HegdeNo ratings yet
- Rite Dentist-Studio CityDocument4 pagesRite Dentist-Studio Cityapi-731924299No ratings yet
- List of DentistsDocument21 pagesList of DentistsSaurabh Gupta100% (1)
- Trifold BrochureDocument2 pagesTrifold BrochureRendanLumbertNo ratings yet
- 2021 - Life, Dental, Vision PacketDocument12 pages2021 - Life, Dental, Vision PacketEberNo ratings yet
- 2011 Delta Dental General MarketingDocument1 page2011 Delta Dental General MarketingKristieNo ratings yet
- Epidemiology, Aetiology and Prevention of Oral CancerDocument9 pagesEpidemiology, Aetiology and Prevention of Oral Cancerpemirafkgunair 2020No ratings yet
- What Happens During A Routine Dental Checkup?: Say Hello To Your ReceptionistDocument1 pageWhat Happens During A Routine Dental Checkup?: Say Hello To Your ReceptionistAishani MeggiNo ratings yet
- Ottonova Coverage For Dental InsuranceDocument3 pagesOttonova Coverage For Dental Insurancetomislavdrvar798No ratings yet
- Generic Open Enrollment KitDocument22 pagesGeneric Open Enrollment KitSteve BarrowsNo ratings yet
- BDA Advice Tooth WhiteningDocument3 pagesBDA Advice Tooth WhiteningMariam Waseem0% (1)
- Cubierta Dental D-611 P.ideal C.P. 2Document4 pagesCubierta Dental D-611 P.ideal C.P. 2JessicaNo ratings yet
- BlueDental Copayment QF Plan BrochureDocument4 pagesBlueDental Copayment QF Plan BrochureJoshua JohnsonNo ratings yet
- DentalDocument3 pagesDentalCarl WiltNo ratings yet
- Delta Dental of California - Dental Ppo 12Document2 pagesDelta Dental of California - Dental Ppo 12api-252555369No ratings yet
- One Arch Braces & Pain Free Dentist London - Dental-SpaDocument2 pagesOne Arch Braces & Pain Free Dentist London - Dental-SpadentalspaukNo ratings yet
- Aetna Y0001 H5521 380 PR25 SB24 M 2024 SF20240425Document23 pagesAetna Y0001 H5521 380 PR25 SB24 M 2024 SF20240425kevin.mccreaNo ratings yet
- Keep Smiling: Delta Dental PPO™Document2 pagesKeep Smiling: Delta Dental PPO™olimaziNo ratings yet
- 888674a Ooc Cigna Dental 1500 CaDocument13 pages888674a Ooc Cigna Dental 1500 CaImmanuel TaquonNo ratings yet
- MEDICARDDocument19 pagesMEDICARDSrcdc CooperativeNo ratings yet
- Guardian - Dental PPO Plan Summary 2022Document4 pagesGuardian - Dental PPO Plan Summary 2022Jessi ChallagullaNo ratings yet
- Avant Dental Welness ProgramDocument4 pagesAvant Dental Welness Programskarthik011No ratings yet
- Rite Dentist-North HollywoodDocument3 pagesRite Dentist-North Hollywoodapi-731909862No ratings yet
- 2003 Delta SumDocument1 page2003 Delta SumbpracticalNo ratings yet
- Tooth WhiteningDocument3 pagesTooth WhiteningrizwanNo ratings yet
- Slater Inc Dental EnglishDocument4 pagesSlater Inc Dental Englishapi-531507901No ratings yet
- LSG DentalDocument1 pageLSG Dentalres6250No ratings yet
- Hospital ProposalDocument8 pagesHospital ProposalMurali MohanNo ratings yet
- Carefree: Show Your Card. Save Your MoneyDocument7 pagesCarefree: Show Your Card. Save Your MoneyMichelle Angelina CortezNo ratings yet
- LoyaltyCard 2016 July11 PDFDocument14 pagesLoyaltyCard 2016 July11 PDFchico_belandresNo ratings yet
- Epidemiology, Aetiology and Prevention of Periodontal Disease (Recovered)Document8 pagesEpidemiology, Aetiology and Prevention of Periodontal Disease (Recovered)pemirafkgunair 2020No ratings yet
- Outpatient One Pager Version 1.0 Apr 20Document1 pageOutpatient One Pager Version 1.0 Apr 20naval730107No ratings yet
- Our Mission: Yp Yp Yp Yp Yp Yp Yp YpDocument3 pagesOur Mission: Yp Yp Yp Yp Yp Yp Yp YpalshadNo ratings yet
- Dental Plans and Rates: Bay AreaDocument6 pagesDental Plans and Rates: Bay AreaJDanaNo ratings yet
- Welcome To Lifetime Smiles Dental Hygiene ClinicDocument7 pagesWelcome To Lifetime Smiles Dental Hygiene CliniclifetimesmileNo ratings yet
- Dental Wellness Plan: Our Exclusive In-House Savings PlanDocument1 pageDental Wellness Plan: Our Exclusive In-House Savings PlanJamez MattauzNo ratings yet
- Welcome To Lifetime Smiles Dental Hygiene ClinicDocument7 pagesWelcome To Lifetime Smiles Dental Hygiene CliniclifetimesmileNo ratings yet
- Your Path to Healthier Dentistry: A Holistic Approach to Keeping Your Teeth for a LifetimeFrom EverandYour Path to Healthier Dentistry: A Holistic Approach to Keeping Your Teeth for a LifetimeRating: 5 out of 5 stars5/5 (1)
- DENTURES: The Ultimate Guide to Dentures & Denture Care for a Beautifully Restored SmileFrom EverandDENTURES: The Ultimate Guide to Dentures & Denture Care for a Beautifully Restored SmileNo ratings yet
- Dental - Docushare-App-12 - 10 - 2023 6 - 29 - 09 PMDocument6 pagesDental - Docushare-App-12 - 10 - 2023 6 - 29 - 09 PMClifton JuraNo ratings yet
- HACCP WATER FinalDocument68 pagesHACCP WATER FinalClifton JuraNo ratings yet
- 2001 Dewettincketal HACCPDocument9 pages2001 Dewettincketal HACCPClifton JuraNo ratings yet
- IBWA MODEL CODE 2016 Rev 02 2016Document30 pagesIBWA MODEL CODE 2016 Rev 02 2016Katherine KimNo ratings yet
- HACCP FOR WATER OPERATIONS AN OPERATORS EXPERIENCE - GrahamMcKeonDocument6 pagesHACCP FOR WATER OPERATIONS AN OPERATORS EXPERIENCE - GrahamMcKeonClifton JuraNo ratings yet
- SilosDocument3 pagesSilosapi-548205221100% (1)
- Vazno IstrazivanjeDocument2 pagesVazno IstrazivanjeDomagoj BažantNo ratings yet
- Blood Bank UnitDocument9 pagesBlood Bank UnitMary CabalceNo ratings yet
- Drug StudyDocument8 pagesDrug StudyTheresa Reyes De JesusNo ratings yet
- Daftar Harga Produk Generik 2022 New (DITEMPEL)Document1 pageDaftar Harga Produk Generik 2022 New (DITEMPEL)Ade IrawanNo ratings yet
- 8776 00Document30 pages8776 00Elma MufidhaNo ratings yet
- Biodata Dr. P. Sirohi - 2021.06.16Document10 pagesBiodata Dr. P. Sirohi - 2021.06.16kvpy iisc bangloreNo ratings yet
- PRC LeahDocument8 pagesPRC LeahInes Hamoy JunioNo ratings yet
- Landrus Unit IIDocument4 pagesLandrus Unit IIRobert ContiNo ratings yet
- Patient Rights Patient ResponsibilitiesDocument1 pagePatient Rights Patient ResponsibilitiesHassan KhanNo ratings yet
- Phillipine Herbal MedicineDocument23 pagesPhillipine Herbal MedicineCENTHREE MAGALLANESNo ratings yet
- MVS Pulmonary AuscultationDocument8 pagesMVS Pulmonary Auscultationvashini9151No ratings yet
- Foreign Body in Eye Icd 10 - Google SearchDocument1 pageForeign Body in Eye Icd 10 - Google SearchAnandita ParamastutiNo ratings yet
- Suzhou Vocaional University Courses NAVTTC OnlineDocument10 pagesSuzhou Vocaional University Courses NAVTTC Onlineshafiq rehmanNo ratings yet
- Republic Act No. 9173: The Philippine Nursing Act O F 2 0 0 2 Presented By: Judith Leano RNDocument167 pagesRepublic Act No. 9173: The Philippine Nursing Act O F 2 0 0 2 Presented By: Judith Leano RNJohnasse Sebastian NavalNo ratings yet
- Ref. Safety Guide On "Safe Working at Height and Fragile Roof" No. NPCIL/04700/CE (IS&F) /2006/M/139, Dated July 19, 2006Document2 pagesRef. Safety Guide On "Safe Working at Height and Fragile Roof" No. NPCIL/04700/CE (IS&F) /2006/M/139, Dated July 19, 2006Bhagat DeepakNo ratings yet
- Physical Examination of The PatientDocument9 pagesPhysical Examination of The PatientzbrojkoNo ratings yet
- Medication Errors - Where Do They Happen - The Pharmaceutical JournalDocument7 pagesMedication Errors - Where Do They Happen - The Pharmaceutical JournalAre Pee EtcNo ratings yet
- Systemic Light Chain Amyloidosis: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document26 pagesSystemic Light Chain Amyloidosis: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Adina StemateNo ratings yet
- Occupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesAnit XingNo ratings yet
- Barlet Juliette Optimized 3d Flair Sequences ToDocument10 pagesBarlet Juliette Optimized 3d Flair Sequences ToFontas LadoprakopoulosNo ratings yet
- Submental Intubation in Patients With Complex Maxillofacial InjuriesDocument4 pagesSubmental Intubation in Patients With Complex Maxillofacial InjuriesMudassar SattarNo ratings yet
- Camus 2016Document7 pagesCamus 2016Dra CarrascoNo ratings yet
- Vascular DisordersDocument13 pagesVascular DisordersMichelle Dona MirallesNo ratings yet
- Journal of Hematology & Oncology: A Journal Open To AllDocument2 pagesJournal of Hematology & Oncology: A Journal Open To AllKay BristolNo ratings yet
- Obstetric EmbolismDocument81 pagesObstetric Embolismmiss_izzniNo ratings yet
- Form C AuthorizationRequestForm PDFDocument4 pagesForm C AuthorizationRequestForm PDFKalaimani SNo ratings yet
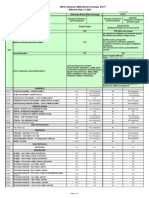
Dental MI EHB High 2024
Dental MI EHB High 2024
Uploaded by
Clifton JuraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dental MI EHB High 2024
Dental MI EHB High 2024
Uploaded by
Clifton JuraCopyright:
Available Formats
EHB Certified Gold Plan
Pediatric Essential Health Benefits (EHB) included in plan
For individuals age 18 and under
IN NETWORK OUT OF NETWORK
Delta Dental Delta Dental Nonparticipating WAITING
Delta Dental PPO (Point-of-Service) PPOTM dentist Premier® dentist dentist PERIODS
Plan pays Plan pays Plan pays
DIAGNOSTIC AND PREVENTIVE SERVICES
Diagnostic and preventive services—exams, cleanings, fluoride and
100% 100% 100% None
space maintainers
Brush biopsy—to detect oral cancer 100% 100% 100% None
Emergency palliative treatment—to temporarily relieve pain 100% 100% 100% None
Radiographs—X-rays 100% 100% 100% None
Sealants—to prevent decay of permanent teeth 100% 100% 100% None
BASIC SERVICES
Minor restorative services—fillings and crown repair 80% 60% 60% None
Oral surgery services—extractions and dental surgery 80% 60% 60% None
Endodontic services—root canals 80% 60% 60% None
Periodontic services—to treat gum disease 80% 60% 60% None
Relines and repairs—prosthetic appliances 80% 60% 60% None
Other basic services—miscellaneous services 80% 60% 60% None
MAJOR SERVICES
Prosthodontic services—bridges, dentures and crowns over implants 50% 50% 50% None
Major restorative services—crowns 50% 50% 50% None
EHB Certified Gold Plan
Non-EHB covered services included in plan
For individuals 19 years of age or older, or individuals age 18 and under seeking non-EHB covered services
IN NETWORK OUT OF NETWORK
Delta Dental Delta Dental Nonparticipating WAITING
Delta Dental PPO (Point-of-Service) PPOTM dentist Premier® dentist dentist PERIODS
Plan pays Plan pays Plan pays
DIAGNOSTIC AND PREVENTIVE SERVICES
Diagnostic and preventive services—exams, cleanings, fluoride and
100% 100% 100% None
space maintainers
Brush biopsy—to detect oral cancer 100% 100% 100% None
Emergency palliative treatment—to temporarily relieve pain 100% 100% 100% None
Radiographs—X-rays 100% 100% 100% None
BASIC SERVICES
Minor restorative services—fillings and crown repair 80% 60% 60% 6 months
Endodontic services—root canals 80% 60% 60% 6 months
Periodontic services—to treat gum disease 80% 60% 60% 6 months
Oral surgery services—extractions and dental surgery 80% 60% 60% 6 months
Periodontal maintenance—cleanings following periodontal therapy 80% 60% 60% 6 months
Relines and repairs—prosthetic appliances 80% 60% 60% 6 months
Other basic services—miscellaneous services 80% 60% 60% 6 months
MAJOR SERVICES
Major restorative services—crowns 50% 50% 50% 12 months
TMD treatment—treatment of the disorder of the temporomandibular
50% 50% 50% 12 months
joint, including related films
Prosthodontic services—bridges, dentures and crowns over implants 50% 50% 50% 12 months
Stay in network and save!
You can go to any licensed dentist, but you generally will save money if you go to a dentist who participates in one of our
two networks—Delta Dental PPO or Delta Dental Premier. That’s because Delta Dental has established maximum approved
fees for nearly all dental services, and participating dentists agree to accept the maximum approved fee as full payment for
those services. If the dentist’s fee is higher than Delta Dental’s, he or she cannot charge you the difference. This means you
are responsible only for your copayments and deductibles, if any, when you visit a Delta Dental participating dentist.
What if I go to a nonparticipating dentist?
If you go to a dentist who does not participate in Delta Dental PPO or Delta Dental Premier, you will still be covered, but
you may have to pay more. The percentages shown above indicate the portion of Delta Dental’s nonparticipating dentist fee
that will be paid for those services. This amount may be less than what the dentist charges and you are responsible for the
difference. We will pay you directly and you will be responsible for paying the dentist whatever he or she charges. You may
also have to submit your own claims.
EHB covered services Non-EHB covered services
EHB covered services include covered services to individuals age 18 Non-EHB covered services include all covered services that are not
and under that are considered Essential Health Benefits as defined Essential Health Benefits as defined by the Patient Protection and
by the Patient Protection and Affordable Care Act. Affordable Care Act.
In-network annual out-of-pocket maximum for EHB covered services Maximum payment for non-EHB covered services
An annual out-of-pocket maximum is the maximum amount that you $
1,000 per person total per calendar year on all non-EHB
or an eligible person will pay for EHB covered services throughout covered services. $300 per person total per lifetime maximum
a benefit year. The in-network annual out-of-pocket maximum for for TMD treatment.
EHB covered services shall be $400 per benefit year if this policy
covers one eligible person age 18 and under, or $800 per benefit Annual out-of-pocket maximum payment for non-EHB
year if this policy covers two or more eligible persons age 18 and covered services
under. Any coinsurance, copayments, deductibles or other out-of- An annual out-of-pocket maximum is the maximum amount that you
pocket expenses paid by an eligible person for in-network EHB or your eligible dependent will pay for covered services throughout
covered services shall count toward that in-network annual out-of- a benefit year. There is no annual out-of-pocket maximum
pocket maximum. The in-network annual out-of-pocket maximum payment for non-EHB covered services. You will be responsible
will not include any amounts paid for the following: (i) premiums; (ii) for all copayments, deductibles and other out-of-pocket expenses
non-covered services; (iii) out-of-network dentists; (iv) coinsurance, associated with all non-EHB covered services provided to you or
copayments, deductibles or other out-of-pocket expenses for your eligible dependent throughout the benefit year.
services other than EHB covered services; or (v) coinsurance,
copayments, deductibles or other out-of-pocket expenses for EHB Deductible for non-EHB covered services
covered services provided to individuals 19 years of age and older.
None.
Once your applicable in-network annual out-of-pocket maximum
is reached for the benefit year, all in-network EHB covered services Waiting period for non-EHB covered services
provided to an eligible person will be covered at 100 percent of the
maximum approved fee. Individuals 19 years of age or older, or individuals age 18 and under
seeking non-EHB covered services, will be eligible for coverage for
Out-of-network annual out-of-pocket maximum for EHB diagnostic and preventive, basic and major services in concordance
covered services with the applicable waiting periods set forth in the covered services
chart above, measured from your or their date of coverage under
There is no annual out-of-pocket maximum for out-of-network
this policy.
EHB covered services. Eligible persons will be responsible for
all copayments, deductibles and other out-of-pocket expenses Eligible dependents enrolled after your date of enrollment will have
associated with all out-of-network EHB covered services provided their own waiting periods in accordance with the above.
to eligible persons throughout the benefit year.
Deductible for EHB covered services
None.
Annual and lifetime maximum for EHB covered services
There are no annual or lifetime maximum payments for EHB
covered services under this policy.
Waiting period for EHB covered services
There are no waiting periods for eligible persons age 18 and under
seeking EHB covered services.
NOTE: The above summary is a sample of benefits. Policies have exclusions and limitations that may limit coverage. For complete coverage
details, please refer to your policy.
EXCLUSIONS: Charges or treatment for correction of congenital or developmental malformations or dentistry for aesthetic reasons;
cosmetic surgery (including repairs to facings posterior to second bicuspid); treatment by anyone other than a licensed dentist or dental
hygienist; veneers; prefabricated crowns as final restoration on permanent teeth and paste-type root canal fillings on permanent teeth;
appliances, procedures and restorations for increasing vertical dimension, occlusion, tooth structure loss due to attrition, abrasion or erosion,
or for periodontal splinting; lost, missing or stolen appliances; services not in the policy.
LIMITATIONS: Coverage for services may be limited based on the age of the person receiving services; coverage for certain services may
be limited to maximum number of occurrences during a specified time period (such as two times per year or one time every three years);
coverage for general anesthesia and/or intravenous sedation, sealants, prosthodontics (implants), orthodontic services, space maintainers
and temporomandibular disorders (TMD) is limited.
MI EHB Gold 2024 Delta Dental Plan of Michigan, Inc. C3 9/23
You might also like
- (Medicalstudyzone - Com) Medicine - Irfan Masood LatestDocument701 pages(Medicalstudyzone - Com) Medicine - Irfan Masood LatestMajid Ahmed FareaNo ratings yet
- Dental CodingDocument74 pagesDental CodingSakshi Bishnoi100% (2)
- NUR 3032 Immune System Study PlanDocument5 pagesNUR 3032 Immune System Study PlanThalia Fortune100% (1)
- Banco Kap. - CK 2Document1,099 pagesBanco Kap. - CK 2Lucas OrtizNo ratings yet
- Dental OH EHB Low 2024Document3 pagesDental OH EHB Low 2024Clifton JuraNo ratings yet
- Da Kim 01-23-2024 DD WEBDocument4 pagesDa Kim 01-23-2024 DD WEBhaWk FYZiXNo ratings yet
- Delta Dental Individual Enrollee Overview Flyer Plan III II Notre DameDocument2 pagesDelta Dental Individual Enrollee Overview Flyer Plan III II Notre DameObi-Wan KenobiNo ratings yet
- Premier 2000 NWDocument2 pagesPremier 2000 NWacolyteNo ratings yet
- Dental Plan Side-By-Side Comparison: Fast FactsDocument2 pagesDental Plan Side-By-Side Comparison: Fast FactsellenNo ratings yet
- Unitedhealthcare Dental Ppo Plan 2022 Summary of Benefits and CoverageDocument1 pageUnitedhealthcare Dental Ppo Plan 2022 Summary of Benefits and CoverageAdam CliftonNo ratings yet
- Delta Dental Plan Compare Highlight SheetDocument2 pagesDelta Dental Plan Compare Highlight SheetTiffany BarnesNo ratings yet
- 2022 Dental Plan BenefitsDocument1 page2022 Dental Plan BenefitsBrian ThurmondNo ratings yet
- Safari - Mar 11, 2019 at 11:00 PM PDFDocument1 pageSafari - Mar 11, 2019 at 11:00 PM PDFjohn jugoNo ratings yet
- Dental PrivilegioDocument11 pagesDental PrivilegioCarlos Andres ANo ratings yet
- Aetna Dental High DmoDocument5 pagesAetna Dental High DmoBeau PeskaNo ratings yet
- Dental Services Low Plan: PreventativeDocument2 pagesDental Services Low Plan: PreventativeIan PeabodyNo ratings yet
- 2021 2022 Aetna Justworks Dental Dmo Benefit SummaryDocument10 pages2021 2022 Aetna Justworks Dental Dmo Benefit SummarySunflowieNo ratings yet
- Dental by Design Broch 5.10Document16 pagesDental by Design Broch 5.10raviNo ratings yet
- 2022 1027 Ahs SD 1058-1 BroDocument8 pages2022 1027 Ahs SD 1058-1 BroFernanda VargasNo ratings yet
- 3610 - DENTAL Smart Health - Certificate-Revised 12 - 8 - 17-SalDocument28 pages3610 - DENTAL Smart Health - Certificate-Revised 12 - 8 - 17-SalOkolokin JohnsonNo ratings yet
- Snap Guardian Dental Plan Summary 2022Document4 pagesSnap Guardian Dental Plan Summary 2022Samson FungNo ratings yet
- 2021 2022 Aetna Justworks Dental Low Ppo 3 Benefit SummaryDocument10 pages2021 2022 Aetna Justworks Dental Low Ppo 3 Benefit SummarySunflowieNo ratings yet
- Cod Capitol 6 Nume Capitol (Engleza) Dental Services Nume Capitol (Romana) Servicii DentareDocument15 pagesCod Capitol 6 Nume Capitol (Engleza) Dental Services Nume Capitol (Romana) Servicii DentareMihaela VelcuNo ratings yet
- Ottonova Highlights For Dental InsuranceDocument2 pagesOttonova Highlights For Dental Insurancetomislavdrvar798No ratings yet
- Dental AwarenessDocument100 pagesDental AwarenessShourya HegdeNo ratings yet
- Rite Dentist-Studio CityDocument4 pagesRite Dentist-Studio Cityapi-731924299No ratings yet
- List of DentistsDocument21 pagesList of DentistsSaurabh Gupta100% (1)
- Trifold BrochureDocument2 pagesTrifold BrochureRendanLumbertNo ratings yet
- 2021 - Life, Dental, Vision PacketDocument12 pages2021 - Life, Dental, Vision PacketEberNo ratings yet
- 2011 Delta Dental General MarketingDocument1 page2011 Delta Dental General MarketingKristieNo ratings yet
- Epidemiology, Aetiology and Prevention of Oral CancerDocument9 pagesEpidemiology, Aetiology and Prevention of Oral Cancerpemirafkgunair 2020No ratings yet
- What Happens During A Routine Dental Checkup?: Say Hello To Your ReceptionistDocument1 pageWhat Happens During A Routine Dental Checkup?: Say Hello To Your ReceptionistAishani MeggiNo ratings yet
- Ottonova Coverage For Dental InsuranceDocument3 pagesOttonova Coverage For Dental Insurancetomislavdrvar798No ratings yet
- Generic Open Enrollment KitDocument22 pagesGeneric Open Enrollment KitSteve BarrowsNo ratings yet
- BDA Advice Tooth WhiteningDocument3 pagesBDA Advice Tooth WhiteningMariam Waseem0% (1)
- Cubierta Dental D-611 P.ideal C.P. 2Document4 pagesCubierta Dental D-611 P.ideal C.P. 2JessicaNo ratings yet
- BlueDental Copayment QF Plan BrochureDocument4 pagesBlueDental Copayment QF Plan BrochureJoshua JohnsonNo ratings yet
- DentalDocument3 pagesDentalCarl WiltNo ratings yet
- Delta Dental of California - Dental Ppo 12Document2 pagesDelta Dental of California - Dental Ppo 12api-252555369No ratings yet
- One Arch Braces & Pain Free Dentist London - Dental-SpaDocument2 pagesOne Arch Braces & Pain Free Dentist London - Dental-SpadentalspaukNo ratings yet
- Aetna Y0001 H5521 380 PR25 SB24 M 2024 SF20240425Document23 pagesAetna Y0001 H5521 380 PR25 SB24 M 2024 SF20240425kevin.mccreaNo ratings yet
- Keep Smiling: Delta Dental PPO™Document2 pagesKeep Smiling: Delta Dental PPO™olimaziNo ratings yet
- 888674a Ooc Cigna Dental 1500 CaDocument13 pages888674a Ooc Cigna Dental 1500 CaImmanuel TaquonNo ratings yet
- MEDICARDDocument19 pagesMEDICARDSrcdc CooperativeNo ratings yet
- Guardian - Dental PPO Plan Summary 2022Document4 pagesGuardian - Dental PPO Plan Summary 2022Jessi ChallagullaNo ratings yet
- Avant Dental Welness ProgramDocument4 pagesAvant Dental Welness Programskarthik011No ratings yet
- Rite Dentist-North HollywoodDocument3 pagesRite Dentist-North Hollywoodapi-731909862No ratings yet
- 2003 Delta SumDocument1 page2003 Delta SumbpracticalNo ratings yet
- Tooth WhiteningDocument3 pagesTooth WhiteningrizwanNo ratings yet
- Slater Inc Dental EnglishDocument4 pagesSlater Inc Dental Englishapi-531507901No ratings yet
- LSG DentalDocument1 pageLSG Dentalres6250No ratings yet
- Hospital ProposalDocument8 pagesHospital ProposalMurali MohanNo ratings yet
- Carefree: Show Your Card. Save Your MoneyDocument7 pagesCarefree: Show Your Card. Save Your MoneyMichelle Angelina CortezNo ratings yet
- LoyaltyCard 2016 July11 PDFDocument14 pagesLoyaltyCard 2016 July11 PDFchico_belandresNo ratings yet
- Epidemiology, Aetiology and Prevention of Periodontal Disease (Recovered)Document8 pagesEpidemiology, Aetiology and Prevention of Periodontal Disease (Recovered)pemirafkgunair 2020No ratings yet
- Outpatient One Pager Version 1.0 Apr 20Document1 pageOutpatient One Pager Version 1.0 Apr 20naval730107No ratings yet
- Our Mission: Yp Yp Yp Yp Yp Yp Yp YpDocument3 pagesOur Mission: Yp Yp Yp Yp Yp Yp Yp YpalshadNo ratings yet
- Dental Plans and Rates: Bay AreaDocument6 pagesDental Plans and Rates: Bay AreaJDanaNo ratings yet
- Welcome To Lifetime Smiles Dental Hygiene ClinicDocument7 pagesWelcome To Lifetime Smiles Dental Hygiene CliniclifetimesmileNo ratings yet
- Dental Wellness Plan: Our Exclusive In-House Savings PlanDocument1 pageDental Wellness Plan: Our Exclusive In-House Savings PlanJamez MattauzNo ratings yet
- Welcome To Lifetime Smiles Dental Hygiene ClinicDocument7 pagesWelcome To Lifetime Smiles Dental Hygiene CliniclifetimesmileNo ratings yet
- Your Path to Healthier Dentistry: A Holistic Approach to Keeping Your Teeth for a LifetimeFrom EverandYour Path to Healthier Dentistry: A Holistic Approach to Keeping Your Teeth for a LifetimeRating: 5 out of 5 stars5/5 (1)
- DENTURES: The Ultimate Guide to Dentures & Denture Care for a Beautifully Restored SmileFrom EverandDENTURES: The Ultimate Guide to Dentures & Denture Care for a Beautifully Restored SmileNo ratings yet
- Dental - Docushare-App-12 - 10 - 2023 6 - 29 - 09 PMDocument6 pagesDental - Docushare-App-12 - 10 - 2023 6 - 29 - 09 PMClifton JuraNo ratings yet
- HACCP WATER FinalDocument68 pagesHACCP WATER FinalClifton JuraNo ratings yet
- 2001 Dewettincketal HACCPDocument9 pages2001 Dewettincketal HACCPClifton JuraNo ratings yet
- IBWA MODEL CODE 2016 Rev 02 2016Document30 pagesIBWA MODEL CODE 2016 Rev 02 2016Katherine KimNo ratings yet
- HACCP FOR WATER OPERATIONS AN OPERATORS EXPERIENCE - GrahamMcKeonDocument6 pagesHACCP FOR WATER OPERATIONS AN OPERATORS EXPERIENCE - GrahamMcKeonClifton JuraNo ratings yet
- SilosDocument3 pagesSilosapi-548205221100% (1)
- Vazno IstrazivanjeDocument2 pagesVazno IstrazivanjeDomagoj BažantNo ratings yet
- Blood Bank UnitDocument9 pagesBlood Bank UnitMary CabalceNo ratings yet
- Drug StudyDocument8 pagesDrug StudyTheresa Reyes De JesusNo ratings yet
- Daftar Harga Produk Generik 2022 New (DITEMPEL)Document1 pageDaftar Harga Produk Generik 2022 New (DITEMPEL)Ade IrawanNo ratings yet
- 8776 00Document30 pages8776 00Elma MufidhaNo ratings yet
- Biodata Dr. P. Sirohi - 2021.06.16Document10 pagesBiodata Dr. P. Sirohi - 2021.06.16kvpy iisc bangloreNo ratings yet
- PRC LeahDocument8 pagesPRC LeahInes Hamoy JunioNo ratings yet
- Landrus Unit IIDocument4 pagesLandrus Unit IIRobert ContiNo ratings yet
- Patient Rights Patient ResponsibilitiesDocument1 pagePatient Rights Patient ResponsibilitiesHassan KhanNo ratings yet
- Phillipine Herbal MedicineDocument23 pagesPhillipine Herbal MedicineCENTHREE MAGALLANESNo ratings yet
- MVS Pulmonary AuscultationDocument8 pagesMVS Pulmonary Auscultationvashini9151No ratings yet
- Foreign Body in Eye Icd 10 - Google SearchDocument1 pageForeign Body in Eye Icd 10 - Google SearchAnandita ParamastutiNo ratings yet
- Suzhou Vocaional University Courses NAVTTC OnlineDocument10 pagesSuzhou Vocaional University Courses NAVTTC Onlineshafiq rehmanNo ratings yet
- Republic Act No. 9173: The Philippine Nursing Act O F 2 0 0 2 Presented By: Judith Leano RNDocument167 pagesRepublic Act No. 9173: The Philippine Nursing Act O F 2 0 0 2 Presented By: Judith Leano RNJohnasse Sebastian NavalNo ratings yet
- Ref. Safety Guide On "Safe Working at Height and Fragile Roof" No. NPCIL/04700/CE (IS&F) /2006/M/139, Dated July 19, 2006Document2 pagesRef. Safety Guide On "Safe Working at Height and Fragile Roof" No. NPCIL/04700/CE (IS&F) /2006/M/139, Dated July 19, 2006Bhagat DeepakNo ratings yet
- Physical Examination of The PatientDocument9 pagesPhysical Examination of The PatientzbrojkoNo ratings yet
- Medication Errors - Where Do They Happen - The Pharmaceutical JournalDocument7 pagesMedication Errors - Where Do They Happen - The Pharmaceutical JournalAre Pee EtcNo ratings yet
- Systemic Light Chain Amyloidosis: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document26 pagesSystemic Light Chain Amyloidosis: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Adina StemateNo ratings yet
- Occupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesAnit XingNo ratings yet
- Barlet Juliette Optimized 3d Flair Sequences ToDocument10 pagesBarlet Juliette Optimized 3d Flair Sequences ToFontas LadoprakopoulosNo ratings yet
- Submental Intubation in Patients With Complex Maxillofacial InjuriesDocument4 pagesSubmental Intubation in Patients With Complex Maxillofacial InjuriesMudassar SattarNo ratings yet
- Camus 2016Document7 pagesCamus 2016Dra CarrascoNo ratings yet
- Vascular DisordersDocument13 pagesVascular DisordersMichelle Dona MirallesNo ratings yet
- Journal of Hematology & Oncology: A Journal Open To AllDocument2 pagesJournal of Hematology & Oncology: A Journal Open To AllKay BristolNo ratings yet
- Obstetric EmbolismDocument81 pagesObstetric Embolismmiss_izzniNo ratings yet
- Form C AuthorizationRequestForm PDFDocument4 pagesForm C AuthorizationRequestForm PDFKalaimani SNo ratings yet