Professional Documents
Culture Documents
A Case of Severe Disseminated Autoeczematization Secondary To Cellulitis Cureus-0014-00000025310
A Case of Severe Disseminated Autoeczematization Secondary To Cellulitis Cureus-0014-00000025310
Uploaded by
cgs08Copyright:
Available Formats
You might also like
- Skin and Soft Tissue Infection InfoDocument4 pagesSkin and Soft Tissue Infection InfoPresura Andreea IulianaNo ratings yet
- Generalized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case ReportDocument3 pagesGeneralized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case Reportcgs08No ratings yet
- Severe Dyshidrotic Eczema After Intravenous Immunoglobulin Therapy For Kawasaki SyndromeDocument2 pagesSevere Dyshidrotic Eczema After Intravenous Immunoglobulin Therapy For Kawasaki SyndromeHallison RanieriNo ratings yet
- UC Davis: Dermatology Online JournalDocument4 pagesUC Davis: Dermatology Online JournalAyu MuskitaNo ratings yet
- Dermatology Case Reports: Diagnosis, Treatment and Prevention of Scabies: A Short CommentaryDocument2 pagesDermatology Case Reports: Diagnosis, Treatment and Prevention of Scabies: A Short CommentaryNidhaSavitriNo ratings yet
- Common Bacterial Skin InfectionsDocument6 pagesCommon Bacterial Skin InfectionsagusNo ratings yet
- Makalah SelulitisDocument26 pagesMakalah Selulitisdr WiyogoNo ratings yet
- Infectious Diseases - 05Document27 pagesInfectious Diseases - 05Arthur YanezNo ratings yet
- Causes and Management of Cellulitis: PathologyDocument4 pagesCauses and Management of Cellulitis: PathologyIsmail YusufNo ratings yet
- Los 1Document9 pagesLos 1azhar naufaldiNo ratings yet
- BR J Dermatol - 2022 - Dissemond - Inflammatory Skin Diseases and WoundsDocument11 pagesBR J Dermatol - 2022 - Dissemond - Inflammatory Skin Diseases and Woundsวสุชล ชัยชาญNo ratings yet
- Kostner 2017Document12 pagesKostner 2017Daisy HamdaliNo ratings yet
- Infeksi StreptoDocument6 pagesInfeksi StreptoRiris SutrisnoNo ratings yet
- Diagnosis of Atopic Dermatitis: Mimics, Overlaps, and ComplicationsDocument35 pagesDiagnosis of Atopic Dermatitis: Mimics, Overlaps, and ComplicationsneleaNo ratings yet
- Ccid 11 175Document11 pagesCcid 11 175Remo Alnovryanda PutraNo ratings yet
- Fever and RashDocument32 pagesFever and Rashanna531No ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsciaranNo ratings yet
- DddsDocument50 pagesDddsOsama AlhaseNo ratings yet
- Kasus Ichthyosis Vulgaris IIDocument4 pagesKasus Ichthyosis Vulgaris IIfitriaNo ratings yet
- Luka 2 PDFDocument6 pagesLuka 2 PDFBarryNo ratings yet
- Ajmcr 10 1 1Document4 pagesAjmcr 10 1 1jghcl.221No ratings yet
- Acute Inflammatory DermatosesDocument29 pagesAcute Inflammatory DermatosesHaniya KhanNo ratings yet
- Journal of Internal Medicine - 2021 - SCH Bitz - So Close and Yet So Far Away The Dichotomy of The Specific ImmuneDocument13 pagesJournal of Internal Medicine - 2021 - SCH Bitz - So Close and Yet So Far Away The Dichotomy of The Specific ImmuneComenderBataliaonBlackNo ratings yet
- An Update On The Treatment and Management of Cellulitis: Practical DermatologyDocument7 pagesAn Update On The Treatment and Management of Cellulitis: Practical DermatologyIndra RukmanaNo ratings yet
- Dermatologia: Anais Brasileiros deDocument11 pagesDermatologia: Anais Brasileiros deAna Raniri UtariNo ratings yet
- Karin Cao Glu 2008Document3 pagesKarin Cao Glu 2008La la landNo ratings yet
- Autoimmune Diseases A Late Complication of Toxic Epidermal Necrolysis A Case ReportDocument4 pagesAutoimmune Diseases A Late Complication of Toxic Epidermal Necrolysis A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Dermatology For The General SurgeonDocument24 pagesDermatology For The General SurgeonAnita HerreraNo ratings yet
- Eczema Monkeypoxicum Report of Monkeypox Transmission in A Patient With Atopic DermatitisDocument5 pagesEczema Monkeypoxicum Report of Monkeypox Transmission in A Patient With Atopic DermatitisA YNo ratings yet
- PDF DocumentDocument4 pagesPDF DocumentAditya Yudha PratamaNo ratings yet
- Bacterial Skin and Soft Tissue Infections Pathogenesis, EpidemiologyDocument11 pagesBacterial Skin and Soft Tissue Infections Pathogenesis, EpidemiologyTony Gomez Luna Leyva0% (1)
- Tom Son 2007Document7 pagesTom Son 2007riedha_chanzNo ratings yet
- Bercak MerahDocument16 pagesBercak MerahFary SatriadiNo ratings yet
- Autosensitisation Autoeczematisation Reactions in A Case of Diaper Dermatitis Candidiasis NMJ-55-274Document2 pagesAutosensitisation Autoeczematisation Reactions in A Case of Diaper Dermatitis Candidiasis NMJ-55-274cgs08No ratings yet
- ULCER DIABETIC Halaman 1296Document30 pagesULCER DIABETIC Halaman 1296wimakrifah istiqomahNo ratings yet
- Welder Et Al (2012) - Herpes Simplex Keratitis. Available At: Accessed On: 20 Agustus 2015Document24 pagesWelder Et Al (2012) - Herpes Simplex Keratitis. Available At: Accessed On: 20 Agustus 2015Silvestri PurbaNo ratings yet
- Bacterial Skin and Soft Tissue Infections: Review of The Epidemiology, Microbiology, Aetiopathogenesis and TreatmentDocument11 pagesBacterial Skin and Soft Tissue Infections: Review of The Epidemiology, Microbiology, Aetiopathogenesis and TreatmentBenor Amri Mustaqim100% (1)
- Host Immune Responses To The Itch Mite, Sarcoptes Scabiei, in HumansDocument12 pagesHost Immune Responses To The Itch Mite, Sarcoptes Scabiei, in HumansSilvia RNo ratings yet
- Systemic Contact DermatitisDocument6 pagesSystemic Contact DermatitisUty PutriNo ratings yet
- Contact DermatitisDocument4 pagesContact DermatitisErlangga D SaputroNo ratings yet
- Referat - CHRONIC WOUNDDocument19 pagesReferat - CHRONIC WOUNDAfifah Syifaul UmmahNo ratings yet
- AltmanDocument12 pagesAltmanAyu WikanNo ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsMARTIN REY EDRICK SANTOSNo ratings yet
- Molusco ContagiosoDocument12 pagesMolusco ContagiosoEduardo Medeiros Tabosa PinheiroNo ratings yet
- (ANDREWS) Folliculitis, Furuncle, CarbuncleDocument8 pages(ANDREWS) Folliculitis, Furuncle, CarbunclempsoletaNo ratings yet
- Heightening Awareness of Blistering Disorders: From The EditorDocument2 pagesHeightening Awareness of Blistering Disorders: From The EditorRaissaNo ratings yet
- Viral Keratitis: Current ConceptsDocument8 pagesViral Keratitis: Current ConceptsDini MayrisdayaniNo ratings yet
- 10.1007@s40257 017 0309 6Document3 pages10.1007@s40257 017 0309 6shf.mxlikNo ratings yet
- 1476 ArticleText 6472 1 10 20100118 PDFDocument6 pages1476 ArticleText 6472 1 10 20100118 PDFJayantiNo ratings yet
- Skin Immunity To Dermatophytes: From Experimental Infection Models To Human DiseaseDocument16 pagesSkin Immunity To Dermatophytes: From Experimental Infection Models To Human Diseaseirwan junNo ratings yet
- Ichthyosis: A Road Model For Skin Research: Review ArticleDocument10 pagesIchthyosis: A Road Model For Skin Research: Review ArticlebaihaqiNo ratings yet
- Allergic and Irritant Contact DermatitisDocument8 pagesAllergic and Irritant Contact DermatitisFenni OktoberryNo ratings yet
- Menichetti 2017Document8 pagesMenichetti 2017IndomedikgramNo ratings yet
- Common Cutaneous Disorders in ElderlyDocument6 pagesCommon Cutaneous Disorders in Elderlyirvinaldi9No ratings yet
- Reconstructive Surgery For Mycetoma: Is There A Need To Establish An Algorithm?Document5 pagesReconstructive Surgery For Mycetoma: Is There A Need To Establish An Algorithm?Yaumil ChoiriNo ratings yet
- 10 Wound Care April 23 1Document31 pages10 Wound Care April 23 1SeRgio MenaNo ratings yet
- Wollenberg Et Al 2000 AllergyDocument9 pagesWollenberg Et Al 2000 AllergyArturo VeraNo ratings yet
- Toxic Epidermal Necrolysis: A Paradigm of Critical IllnessDocument10 pagesToxic Epidermal Necrolysis: A Paradigm of Critical IllnessViolett LiebeNo ratings yet
- Practical Insights into Atopic DermatitisFrom EverandPractical Insights into Atopic DermatitisKwang Hoon LeeNo ratings yet
- 15 Clinical Features and Diagnostic Criteria of Atopic DermatitisDocument19 pages15 Clinical Features and Diagnostic Criteria of Atopic Dermatitiscgs08No ratings yet
- 12 Iatrogenic Disorders of The NewbornDocument12 pages12 Iatrogenic Disorders of The Newborncgs08No ratings yet
- 10 Differential Diagnosis of Neonatal ErythrodermaDocument13 pages10 Differential Diagnosis of Neonatal Erythrodermacgs08No ratings yet
- 13 Epidemiology of Atopic DermatitisDocument17 pages13 Epidemiology of Atopic Dermatitiscgs08No ratings yet
- Generalized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case ReportDocument3 pagesGeneralized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case Reportcgs08No ratings yet
- Autoeczematization A Strange Id Reaction of The SkinDocument4 pagesAutoeczematization A Strange Id Reaction of The Skincgs08No ratings yet
- Drug Study 2.1Document2 pagesDrug Study 2.17y7f66q2qfNo ratings yet
- Cancer PainDocument12 pagesCancer Painsaranya.tNo ratings yet
- Classifying SchizophreniaDocument8 pagesClassifying SchizophreniaAgnes Sophia PenuliarNo ratings yet
- ANALGETIKDocument1 pageANALGETIKsadam huseinNo ratings yet
- Guideline MERS Management in Malaysia, 2023Document123 pagesGuideline MERS Management in Malaysia, 2023Nezly IderusNo ratings yet
- Case ReportDocument12 pagesCase ReportJoão EduardoNo ratings yet
- Prevention Practice For Neuromuscular ConditionsDocument37 pagesPrevention Practice For Neuromuscular ConditionsArham ShamsiNo ratings yet
- Bahasa Inggris Bu FanniDocument5 pagesBahasa Inggris Bu Fanninina purbaNo ratings yet
- PATHO FALCON (Latest Edition)Document17 pagesPATHO FALCON (Latest Edition)Nikhil kumar Sangam.No ratings yet
- BFM 2000 Treatment SchemaDocument2 pagesBFM 2000 Treatment SchemaAnonymous 9dVZCnTXSNo ratings yet
- Osteosarcoma PDFDocument3 pagesOsteosarcoma PDFkc andrea torresNo ratings yet
- Healthy AgingDocument13 pagesHealthy AgingCarissa Mae Tapec EstradaNo ratings yet
- Otorhinolaryngology ENT Paper1 PDFDocument3 pagesOtorhinolaryngology ENT Paper1 PDFRoshni KNo ratings yet
- Family Case SampleDocument25 pagesFamily Case SampleGrInDoVe9097No ratings yet
- Case Presentation - DM (Tantsa Tamia)Document58 pagesCase Presentation - DM (Tantsa Tamia)tantsaNo ratings yet
- BMI For AgeDocument2 pagesBMI For AgeNeil AtanacioNo ratings yet
- Osmosis 7moDocument216 pagesOsmosis 7moFer CasasNo ratings yet
- Viral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDocument14 pagesViral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDARLENE CLAIRE ANDEZANo ratings yet
- Secondary Stroke PreventionDocument54 pagesSecondary Stroke PreventionHùng Phạm Lý ChíNo ratings yet
- Dapa-CKD - Applying Clinical Evidence To Clinical PracticeDocument45 pagesDapa-CKD - Applying Clinical Evidence To Clinical Practicedevikumar kelkarNo ratings yet
- Project in MapehDocument10 pagesProject in MapehRhina Marie Ramos DumaguinNo ratings yet
- Tau Chempath - Acid Base Imbalance & Pahology of Resp FailureDocument31 pagesTau Chempath - Acid Base Imbalance & Pahology of Resp FailureChipego ChiyaamaNo ratings yet
- Causes of DeathDocument12 pagesCauses of DeathMerle Ajcap0% (1)
- InformativeDocument2 pagesInformative3701Dhanush NadarNo ratings yet
- NCM 117 Midterm ReviewerDocument17 pagesNCM 117 Midterm ReviewerPia Rose RoqueNo ratings yet
- Tocilizumab For Rheumatoid Arthritis Results of The Phase III Clinical Trial ProgramDocument10 pagesTocilizumab For Rheumatoid Arthritis Results of The Phase III Clinical Trial ProgramasdffdsaNo ratings yet
- Myocardial Infarction NotesDocument6 pagesMyocardial Infarction NotesAshutosh BhaleraoNo ratings yet
- Ethics 143Document13 pagesEthics 143122ritik goyalNo ratings yet
- Tumour MarkersDocument34 pagesTumour MarkersAbdulelah MurshidNo ratings yet
- AdhdDocument2 pagesAdhdapi-671375887No ratings yet
A Case of Severe Disseminated Autoeczematization Secondary To Cellulitis Cureus-0014-00000025310
A Case of Severe Disseminated Autoeczematization Secondary To Cellulitis Cureus-0014-00000025310
Uploaded by
cgs08Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Case of Severe Disseminated Autoeczematization Secondary To Cellulitis Cureus-0014-00000025310
A Case of Severe Disseminated Autoeczematization Secondary To Cellulitis Cureus-0014-00000025310
Uploaded by
cgs08Copyright:
Available Formats
Open Access Case
Report DOI: 10.7759/cureus.25310
A Case of Severe Disseminated
Autoeczematization Secondary to Cellulitis
Review began 05/15/2022
Yash V. Bhagat 1, 2 , Merve Otles 2 , Brittany Salmon 2 , Roshaye Graham 2 , Miriam Micheal 3, 4
Review ended 05/23/2022
Published 05/24/2022 1. Internal Medicine, University of Maryland Medical Center Midtown Campus, Baltimore, USA 2. Internal Medicine,
© Copyright 2022 American University of Antigua, St. John's, ATG 3. Internal Medicine, Howard University College of Medicine,
Bhagat et al. This is an open access article Washington DC, USA 4. Internal Medicine, University of Maryland School of Medicine, Baltimore, USA
distributed under the terms of the Creative
Commons Attribution License CC-BY 4.0.,
Corresponding author: Yash V. Bhagat, yashvinodbhagat@gmail.com
which permits unrestricted use, distribution,
and reproduction in any medium, provided
the original author and source are credited.
Abstract
Autoeczematization, the dissemination of a local eczematous reaction to a distal site, is closely associated
with lower extremity edema. Our patient is a 50-year-old man with a past medical history of drug-induced
lupus to hydralazine and recent bilateral cellulitis in his lower extremities. He was presented with
complaints of vesicles on his palms and soles and a scaling rash that had spread over his torso, arms, and
trunk. Laboratory studies found no evidence of an active rheumatological condition with complement C3
and C4 levels being normal and no anti-dsDNA, anti-histone, anti-Smith, anti-ribonucleoprotein (anti-RNP),
anti-centromere, anti-neutrophil cytoplasmic antibodies (ANCA), anti-Ro, or anti-La antibodies present.
Moreover, syphilis, HIV, gonorrhea, chlamydia, rickettsia antibody, and Borrelia burgdorferi antibody
testing was negative suggesting a non-infectious etiology of the rash. Hypothesizing a dermatologic origin
of the rash, a skin biopsy was performed that revealed intermittent foci of moderate hyperparakeratosis and
mild hypergranulosis indicative of eczematous dermatitis. Unfortunately, treatment of the disseminated
rash with 10 mg of daily oral prednisone and topical triamcinolone acetonide 0.1% ointment proved
inefficient, and methotrexate therapy was advised. We posit that cellulitis, a soft tissue infection under the
skin, is a potential cause of disruption of the skin barrier that leads to activation of autosensitized T cells.
These activated T cells circulate to distal areas of the skin and may lead to autoeczematization. The
treatment of these id reactions with corticosteroids - both topical and oral - may be insufficient at reducing
dermatitis and require the application of systemic methotrexate or cyclosporine. Through this case, we
demonstrate the importance of treating id reactions by stepping up the intensity of treatment due to the
severity of autosensitization-driven eczema.
Categories: Dermatology, Internal Medicine, Allergy/Immunology
Keywords: skin rash, itch, rash, dermatology, pustule, vesicle, methotrexate, cellulitis, autoimmune, eczema
Introduction
Stasis dermatitis, also known as eczematous dermatitis, is known to present with vesicles, scales, and
pruritus on the lower limbs and ankles in association with chronic venous insufficiency [1]. Patients with
venous stasis often develop autoeczematization or id reaction causing breakout of vesicles in close
proximity to the initial site of dermatitis before widespread dissemination at more distal regions, such as the
arms, feet, and trunk [2]. Biopsies of these vesicles demonstrate a form of eczema with interstitial edema
and the presence of lymphocytic infiltrates such as T cells [3]. In most instances, autoeczematization that
presents with vesicular eruptions primarily on the palms is associated with dermatophyte infections such as
tinea pedis and capitis [4].
The underlying cause of the id reaction dictates the method of treatment. The treatment is aimed at the
resolution of dermatitis in the primary area with subsequent resolution of dermatitis in the distal location.
Therefore, id reactions secondary to tinea pedis resolve following antifungals, while reactions secondary to
stasis dermatitis are treated with steroids [5]. This report highlights a patient with a severe id reaction
secondary to chronic stasis dermatitis resistant to topical and oral steroid therapy and requiring
methotrexate, systemic treatment for severe eczema.
Case Presentation
A 50-year-old male with a past medical history of drug-induced lupus to hydralazine and bilateral lower
extremity cellulitis that occurred two months ago presents with complaints of vesicles on his palms and
soles and a scaling rash that had spread over his body. The patient’s prior cellulitis was treated in-patient
with IV vancomycin and piperacillin-tazobactam and outpatient oral doxycycline with follow-up
appointments at the wound care clinic.
He stated that he first saw the rash begin about a week and a half ago around his left thigh above the
cellulitis. The rash was distinct from his cellulitis and did not seem to cross the border of the area affected by
the cellulitis (Figure 1A). About three days after, he noticed the rash had spread to the right knee and right
medial thigh. A day after, the rash had spread upward to his trunk, to the dorsum of his hands, and to his
How to cite this article
Bhagat Y V, Otles M, Salmon B, et al. (May 24, 2022) A Case of Severe Disseminated Autoeczematization Secondary to Cellulitis. Cureus 14(5):
e25310. DOI 10.7759/cureus.25310
back. Only thereafter, the rash was present as vesicles on his palms (Figures 1B-1E).
FIGURE 1: Pictures of patient's cellulitis (A), vesicular rash on palms
(B), and itchy scaly rash on the dorsum of his hands (C), trunk (D), and
thigh (E).
The patient denies recent sick contacts, insect bites, sexual activity within the last year, and changes in
medications or soap products that he uses. He is also not immunocompromised, has no history of diabetes or
STDs, and is up to date with all of his childhood vaccinations.
The pustules were found only on the palms, were tense, about 2-5 mm wide, and tended to ooze purulent
liquid. In comparison, the rash was scaly, had formed scabs, was itchy, and had a central head with distinct
singular round units that did not overlap. The patient’s mucosa, face, scalp, groin, pelvis, perineum, and
buttocks were spared from the rash and vesicles. The rash had a negative Nikolsky sign and was present in
various stages of healing.
The patient's lab work, including complete blood count (CBC), comprehensive metabolic panel (CMP), and
vitals, was unremarkable. Blood cultures were drawn and empiric antibiotics (vancomycin, piperacillin-
tazobactam, and valacyclovir) were started. Vancomycin and piperacillin-tazobactam were discontinued
after three days and valacyclovir after 10 days due to no leukocytosis, fever, or resolution of symptoms. The
patient’s serum lactate, c-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were elevated
(Table 1). Rheumatologic serology revealed positive anti-nuclear antibody (ANA) titers, but normal C3 and
C4 complement levels. Moreover, several antibody assays were negative (Table 1). Infectious disease testing
with rapid plasma reagin (RPR), HIV antibody, gonorrhea and chlamydia polymerase chain reaction (PCR),
Rickettsia antibody, and Borrelia burgdorferi antibody were also negative. After ruling out rheumatic and
infectious etiologies, a skin punch biopsy was ordered out-patient.
2022 Bhagat et al. Cureus 14(5): e25310. DOI 10.7759/cureus.25310 2 of 5
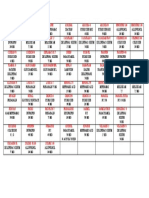
Tests performed Result Reference range
Lactate High; 2.8 mmol/L 0.5-2.2 mmol/L
C-reactive protein High; 1.3 mg/dL <1.0 mg/dL
Erythrocyte sedimentation rate High; 37 mm/h 1-13 mm/h for males
ANA antibodies Positive <1:160
C3 complement Normal 80-160 mg/dL
C4 complement Normal 16-48 mg/dL
Anti-dsDNA antibodies Negative <10 AU/mL
Anti-histone antibodies Negative <1 AU/mL
Anti-Smith antibodies Negative <7 AU/mL
Anti-RNP antibodies Negative <20 AU/mL
Anti-centromere antibodies Negative <30 AU/mL
ANCA antibodies Negative <20 AU/mL
Anti-Ro antibodies Negative <1 AU/mL
Anti-La antibodies Negative <1 AU/mL
RPR Nonreactive Nonreactive
HIV antibody Nonreactive Nonreactive
Gonorrhea and chlamydia PCR Nonreactive Nonreactive
Rickettsia IgG antibody Nonreactive Nonreactive
Borrelia burgdorferi antibody Nonreactive Nonreactive
TABLE 1: Laboratory tests performed on blood drawn from the patient to assess for rheumatic
and infectious etiologies of the rash.
anti-RNP: anti-ribonucleoprotein; ANCA: anti-neutrophil cytoplasmic antibodies; ANA: antinuclear antibody; RPR: rapid plasma regain; PCR: polymerase
chain reaction
Skin biopsy showed that the epidermis had mild acanthosis, mild spongiosis, mild hypergranulosis, and
intermittent foci of mild to moderate hyperparakeratosis. There were focal minimal mounded patterns of
hyperparakeratosis and focal intracorneal serum entrapment. The dermis showed a mild superficial
perivascular and mildly interstitial infiltrate of lymphocytes, eosinophils, and plasma cells. Deeper levels
showed more prominent intracorneal serum entrapment with focal sparse intracorneal neutrophils and more
conspicuous plasma cells. Periodic acid-Schiff (PAS) staining is negative for fungal organisms or hyphae and
spirochetes were not identified on immunohistochemical staining. The microscopic findings were suggestive
of eczematous dermatitis. The patient was prescribed prednisone 10 mg once a day, clobetasol ointment for
his hands, triamcinolone 0.1% ointment for the rest of the body, and doxepin 25 mg nightly. After a month,
the patient reported only minimal improvement in his hands, abdomen, and upper extremities with PO
prednisone and topical steroids; however, the itchy rash was still present on his bilateral lower extremities.
The patient was counseled on the administration of methotrexate as a systemic line of treatment.
Discussion
We presented a case of autoeczematization secondary to stasis dermatitis triggered by a recent episode of
bilateral lower extremity cellulitis. Our patient presented with a rash following bilateral lower extremity
cellulitis which first began on the lower extremities and then spread non-contiguously to cover most of his
body.
Patients with chronic stasis dermatitis are at a 37% lifetime risk of developing autoeczematization later in
the course of the disease when compared to the general population [4,6]. We postulate that stasis dermatitis
causes a reaction involving T cells in the absence of interferon signaling, an autoeczematization reaction.
Immunologically, this T cell reaction is secondary to skin inflammation and cellular damage caused by stasis
2022 Bhagat et al. Cureus 14(5): e25310. DOI 10.7759/cureus.25310 3 of 5
dermatitis which leads to the formation of keratinocyte antigens that are autoreactive. A study by Fehr et al.
postulated that proteins derived from keratinocytes behaved like antigens which caused an autoreaction
involving T cells [7,8]. Other studies demonstrated evidence of a similar reaction in a patient with hypostatic
dermatitis, wherein, an elevated level of activated helper T cells was noted despite no production of
interferon from peripheral mononuclear leukocytes [9]. Bertoli et al. state that these antigenic keratinocytes
are able to produce cytokines - thymic stromal erythropoietin, IL-25, and IL-33 - that lead to activation of T-
cells that travel to distant sites and cause an id reaction [4].
After investigation to rule out infectious and rheumatologic etiologies with similar presentation, our biopsy
demonstrated that the severe rash in our patient was an autoeczematization reaction. Equivocal findings on
biopsy have been reported by Bertoli et al. showing psoriasiform spongiotic dermatitis with mononuclear
cells, eosinophils and lymphohistiocytic infiltrates [4]. The histopathological findings from our skin biopsy
align with our theory that the distant rash is T cell mediated.
Identification of T cell-mediated processes as the pathology underlying autoeczematization has helped
tailor treatment. A study on dupilumab, a monoclonal antibody inhibitor of IL-4 receptor, as a treatment for
autoeczematization found that this treatment shifted the T cell-mediated reaction towards Th1 dominance,
rather than Th2, causing a subsequent resolution of the autoeczematous rash and development of a
psoriatiform rash that was different from the initial autoeczematous rash [6]. This finding guides the choice
of methotrexate as a treatment. Methotrexate is hypothesized to induce apoptosis of activated T
lymphocytes via a Th2-mediated mechanism. Studies by Genestier et al. showed dose-dependent inhibition
of cell proliferation and apoptosis of activated peripheral T cells by methotrexate, sparing nonactivated T
cells in vitro [10]. A study comparing methotrexate treatment in patients with recalcitrant eczema versus
folic acid treatment found a statistically significant reduction in eczema post methotrexate treatment. The
study covered many eczematous presentations, such as atopic dermatitis, allergic contact dermatitis,
idiopathic pompholyx, seborrheic eczema, and lichen simplex chronicus, which they posit to be T cell-
mediated and concluded that methotrexate is a drug of choice in treatment resistant eczema, regardless of
its etiopathogenesis [11].
We do also encourage early treatment of the inciting factor, in this case, the primary venous stasis, which
could lead to improvement of the distal id reaction, a finding seen with the use of compression stockings [4].
Treatment of the stasis dermatitis with prednisone, and at distant sites with clobetasol ointment,
triamcinolone ointment, and doxepin also provided initial improvement but could prove futile in cases of
treatment-resistant eczema, as with our patient.
Further studies should be done to localize markers of T cells from biopsies of the distal rash [4]. Other
studies have identified elevated cell surface expressions of HLD-DR antigen and IL-2R on the surface of T
cells in autoeczematization reactions that were subsequently reduced after treatment and resolution of
symptoms [12]. Of note, this response was only seen in autoeczematization secondary to stasis dermatitis
and not in autoeczematization secondary to psoriasis which aligns with our hypothesis [12]. We suggest that
HLA-DR antigen and IL-2R which were identified using fluorescent antibodies in the above study could be
utilized and therefore could prove to be a standard mechanism by which we diagnose these rare episodes of
autoeczematization in the future cases.
Conclusions
In conclusion, we present a severe case of autoeczematization that was difficult to diagnose, needed lengthy
workup to rule out other causes, and harder to treat, requiring stepping-up of medications from topic and
oral prednisone to methotrexate. We hope that sharing this case will make clinicians aware of the varied
presentation of disseminated eczema in the future, and inspire rapid diagnosis and treatment of such cases.
Additional Information
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In
compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services
info: All authors have declared that no financial support was received from any organization for the
submitted work. Financial relationships: All authors have declared that they have no financial
relationships at present or within the previous three years with any organizations that might have an
interest in the submitted work. Other relationships: All authors have declared that there are no other
relationships or activities that could appear to have influenced the submitted work.
References
1. Section 17: skin signs of vascular insufficiency . Fitzpatrick's Color Atlas and Synopsis of Clinical
Dermatology. Eighth Edititon. Wolff K, Johnson R, Saavedra AP, Roh EK (ed): McGraw-Hill, New York, NY;
2017. 475-9.
2. Shelley WB: Id reaction. Consultations in Dermatology. Saunders, Philadelphia, PA; 1972. 262-7.
3. Ilkit M, Durdu M, Karakaş M: Cutaneous id reactions: a comprehensive review of clinical manifestations,
2022 Bhagat et al. Cureus 14(5): e25310. DOI 10.7759/cureus.25310 4 of 5
epidemiology, etiology, and management. Crit Rev Microbiol. 2012, 38:191-202.
10.3109/1040841X.2011.645520
4. Bertoli MJ, Schwartz RA, Janniger CK: Autoeczematization: a strange id reaction of the skin. Cutis. 2021,
108:163-6. 10.12788/cutis.0342
5. Nedorost S, White S, Rowland DY, et al.: Development and implementation of an order set to improve value
of care for patients with severe stasis dermatitis. J Am Acad Dermatol. 2019, 80:815-7.
10.1016/j.jaad.2018.10.034
6. Schrom KP, Kobs A, Nedorost S: Clinical psoriasiform dermatitis following dupilumab use for
autoeczematization secondary to chronic stasis dermatitis. Cureus. 2020, 12:10.7759/cureus.7831
7. Belsito DV: Chapter 17: autosensitization dermatitis. Fitzpatrick's Dermatology in General Medicine. Eighth
Edition. Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K (ed): McGraw Hill, Philadelphia,
PA; 2012.
8. Fehr BS, Takashima A, Bergstresser PR, Cruz PD Jr.: T cells reactive to keratinocyte antigens are generated
during induction of contact hypersensitivity in mice. A model for autoeczematization in humans? . Am J
Contact Dermat. 2000, 11:145-54. 10.1053/ajcd.2000.7187
9. Cunningham MJ, Zone JJ, Petersen MJ, Green JA: Circulating activated (DR-positive) T lymphocytes in a
patient with autoeczematization. J Am Acad Dermatol. 1986, 14:1039-41. 10.1016/s0190-9622(86)70129-1
10. Genestier L, Paillot R, Fournel S, Ferraro C, Miossec P, Revillard JP: Immunosuppressive properties of
methotrexate: apoptosis and clonal deletion of activated peripheral T cells. J Clin Invest. 1998, 102:322-8.
10.1172/JCI2676
11. Syed AR, Aman S, Nadeem M, Kazmi AH: The efficacy and safety of oral methotrexate in chronic eczema . J
Pak Assoc Dermatol. 2009, 19:220-4.
12. Kasteler JS, Petersen MJ, Vance JE, Zone JJ: Circulating activated T lymphocytes in autoeczematization .
Arch Dermatol. 1992, 128:795-8. 10.1001/archderm.1992.01680160079008
2022 Bhagat et al. Cureus 14(5): e25310. DOI 10.7759/cureus.25310 5 of 5
You might also like
- Skin and Soft Tissue Infection InfoDocument4 pagesSkin and Soft Tissue Infection InfoPresura Andreea IulianaNo ratings yet
- Generalized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case ReportDocument3 pagesGeneralized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case Reportcgs08No ratings yet
- Severe Dyshidrotic Eczema After Intravenous Immunoglobulin Therapy For Kawasaki SyndromeDocument2 pagesSevere Dyshidrotic Eczema After Intravenous Immunoglobulin Therapy For Kawasaki SyndromeHallison RanieriNo ratings yet
- UC Davis: Dermatology Online JournalDocument4 pagesUC Davis: Dermatology Online JournalAyu MuskitaNo ratings yet
- Dermatology Case Reports: Diagnosis, Treatment and Prevention of Scabies: A Short CommentaryDocument2 pagesDermatology Case Reports: Diagnosis, Treatment and Prevention of Scabies: A Short CommentaryNidhaSavitriNo ratings yet
- Common Bacterial Skin InfectionsDocument6 pagesCommon Bacterial Skin InfectionsagusNo ratings yet
- Makalah SelulitisDocument26 pagesMakalah Selulitisdr WiyogoNo ratings yet
- Infectious Diseases - 05Document27 pagesInfectious Diseases - 05Arthur YanezNo ratings yet
- Causes and Management of Cellulitis: PathologyDocument4 pagesCauses and Management of Cellulitis: PathologyIsmail YusufNo ratings yet
- Los 1Document9 pagesLos 1azhar naufaldiNo ratings yet
- BR J Dermatol - 2022 - Dissemond - Inflammatory Skin Diseases and WoundsDocument11 pagesBR J Dermatol - 2022 - Dissemond - Inflammatory Skin Diseases and Woundsวสุชล ชัยชาญNo ratings yet
- Kostner 2017Document12 pagesKostner 2017Daisy HamdaliNo ratings yet
- Infeksi StreptoDocument6 pagesInfeksi StreptoRiris SutrisnoNo ratings yet
- Diagnosis of Atopic Dermatitis: Mimics, Overlaps, and ComplicationsDocument35 pagesDiagnosis of Atopic Dermatitis: Mimics, Overlaps, and ComplicationsneleaNo ratings yet
- Ccid 11 175Document11 pagesCcid 11 175Remo Alnovryanda PutraNo ratings yet
- Fever and RashDocument32 pagesFever and Rashanna531No ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsciaranNo ratings yet
- DddsDocument50 pagesDddsOsama AlhaseNo ratings yet
- Kasus Ichthyosis Vulgaris IIDocument4 pagesKasus Ichthyosis Vulgaris IIfitriaNo ratings yet
- Luka 2 PDFDocument6 pagesLuka 2 PDFBarryNo ratings yet
- Ajmcr 10 1 1Document4 pagesAjmcr 10 1 1jghcl.221No ratings yet
- Acute Inflammatory DermatosesDocument29 pagesAcute Inflammatory DermatosesHaniya KhanNo ratings yet
- Journal of Internal Medicine - 2021 - SCH Bitz - So Close and Yet So Far Away The Dichotomy of The Specific ImmuneDocument13 pagesJournal of Internal Medicine - 2021 - SCH Bitz - So Close and Yet So Far Away The Dichotomy of The Specific ImmuneComenderBataliaonBlackNo ratings yet
- An Update On The Treatment and Management of Cellulitis: Practical DermatologyDocument7 pagesAn Update On The Treatment and Management of Cellulitis: Practical DermatologyIndra RukmanaNo ratings yet
- Dermatologia: Anais Brasileiros deDocument11 pagesDermatologia: Anais Brasileiros deAna Raniri UtariNo ratings yet
- Karin Cao Glu 2008Document3 pagesKarin Cao Glu 2008La la landNo ratings yet
- Autoimmune Diseases A Late Complication of Toxic Epidermal Necrolysis A Case ReportDocument4 pagesAutoimmune Diseases A Late Complication of Toxic Epidermal Necrolysis A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Dermatology For The General SurgeonDocument24 pagesDermatology For The General SurgeonAnita HerreraNo ratings yet
- Eczema Monkeypoxicum Report of Monkeypox Transmission in A Patient With Atopic DermatitisDocument5 pagesEczema Monkeypoxicum Report of Monkeypox Transmission in A Patient With Atopic DermatitisA YNo ratings yet
- PDF DocumentDocument4 pagesPDF DocumentAditya Yudha PratamaNo ratings yet
- Bacterial Skin and Soft Tissue Infections Pathogenesis, EpidemiologyDocument11 pagesBacterial Skin and Soft Tissue Infections Pathogenesis, EpidemiologyTony Gomez Luna Leyva0% (1)
- Tom Son 2007Document7 pagesTom Son 2007riedha_chanzNo ratings yet
- Bercak MerahDocument16 pagesBercak MerahFary SatriadiNo ratings yet
- Autosensitisation Autoeczematisation Reactions in A Case of Diaper Dermatitis Candidiasis NMJ-55-274Document2 pagesAutosensitisation Autoeczematisation Reactions in A Case of Diaper Dermatitis Candidiasis NMJ-55-274cgs08No ratings yet
- ULCER DIABETIC Halaman 1296Document30 pagesULCER DIABETIC Halaman 1296wimakrifah istiqomahNo ratings yet
- Welder Et Al (2012) - Herpes Simplex Keratitis. Available At: Accessed On: 20 Agustus 2015Document24 pagesWelder Et Al (2012) - Herpes Simplex Keratitis. Available At: Accessed On: 20 Agustus 2015Silvestri PurbaNo ratings yet
- Bacterial Skin and Soft Tissue Infections: Review of The Epidemiology, Microbiology, Aetiopathogenesis and TreatmentDocument11 pagesBacterial Skin and Soft Tissue Infections: Review of The Epidemiology, Microbiology, Aetiopathogenesis and TreatmentBenor Amri Mustaqim100% (1)
- Host Immune Responses To The Itch Mite, Sarcoptes Scabiei, in HumansDocument12 pagesHost Immune Responses To The Itch Mite, Sarcoptes Scabiei, in HumansSilvia RNo ratings yet
- Systemic Contact DermatitisDocument6 pagesSystemic Contact DermatitisUty PutriNo ratings yet
- Contact DermatitisDocument4 pagesContact DermatitisErlangga D SaputroNo ratings yet
- Referat - CHRONIC WOUNDDocument19 pagesReferat - CHRONIC WOUNDAfifah Syifaul UmmahNo ratings yet
- AltmanDocument12 pagesAltmanAyu WikanNo ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsMARTIN REY EDRICK SANTOSNo ratings yet
- Molusco ContagiosoDocument12 pagesMolusco ContagiosoEduardo Medeiros Tabosa PinheiroNo ratings yet
- (ANDREWS) Folliculitis, Furuncle, CarbuncleDocument8 pages(ANDREWS) Folliculitis, Furuncle, CarbunclempsoletaNo ratings yet
- Heightening Awareness of Blistering Disorders: From The EditorDocument2 pagesHeightening Awareness of Blistering Disorders: From The EditorRaissaNo ratings yet
- Viral Keratitis: Current ConceptsDocument8 pagesViral Keratitis: Current ConceptsDini MayrisdayaniNo ratings yet
- 10.1007@s40257 017 0309 6Document3 pages10.1007@s40257 017 0309 6shf.mxlikNo ratings yet
- 1476 ArticleText 6472 1 10 20100118 PDFDocument6 pages1476 ArticleText 6472 1 10 20100118 PDFJayantiNo ratings yet
- Skin Immunity To Dermatophytes: From Experimental Infection Models To Human DiseaseDocument16 pagesSkin Immunity To Dermatophytes: From Experimental Infection Models To Human Diseaseirwan junNo ratings yet
- Ichthyosis: A Road Model For Skin Research: Review ArticleDocument10 pagesIchthyosis: A Road Model For Skin Research: Review ArticlebaihaqiNo ratings yet
- Allergic and Irritant Contact DermatitisDocument8 pagesAllergic and Irritant Contact DermatitisFenni OktoberryNo ratings yet
- Menichetti 2017Document8 pagesMenichetti 2017IndomedikgramNo ratings yet
- Common Cutaneous Disorders in ElderlyDocument6 pagesCommon Cutaneous Disorders in Elderlyirvinaldi9No ratings yet
- Reconstructive Surgery For Mycetoma: Is There A Need To Establish An Algorithm?Document5 pagesReconstructive Surgery For Mycetoma: Is There A Need To Establish An Algorithm?Yaumil ChoiriNo ratings yet
- 10 Wound Care April 23 1Document31 pages10 Wound Care April 23 1SeRgio MenaNo ratings yet
- Wollenberg Et Al 2000 AllergyDocument9 pagesWollenberg Et Al 2000 AllergyArturo VeraNo ratings yet
- Toxic Epidermal Necrolysis: A Paradigm of Critical IllnessDocument10 pagesToxic Epidermal Necrolysis: A Paradigm of Critical IllnessViolett LiebeNo ratings yet
- Practical Insights into Atopic DermatitisFrom EverandPractical Insights into Atopic DermatitisKwang Hoon LeeNo ratings yet
- 15 Clinical Features and Diagnostic Criteria of Atopic DermatitisDocument19 pages15 Clinical Features and Diagnostic Criteria of Atopic Dermatitiscgs08No ratings yet
- 12 Iatrogenic Disorders of The NewbornDocument12 pages12 Iatrogenic Disorders of The Newborncgs08No ratings yet
- 10 Differential Diagnosis of Neonatal ErythrodermaDocument13 pages10 Differential Diagnosis of Neonatal Erythrodermacgs08No ratings yet
- 13 Epidemiology of Atopic DermatitisDocument17 pages13 Epidemiology of Atopic Dermatitiscgs08No ratings yet
- Generalized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case ReportDocument3 pagesGeneralized Eczematous Rash in A Patient With Shoe Contact Dermatitis A Case Reportcgs08No ratings yet
- Autoeczematization A Strange Id Reaction of The SkinDocument4 pagesAutoeczematization A Strange Id Reaction of The Skincgs08No ratings yet
- Drug Study 2.1Document2 pagesDrug Study 2.17y7f66q2qfNo ratings yet
- Cancer PainDocument12 pagesCancer Painsaranya.tNo ratings yet
- Classifying SchizophreniaDocument8 pagesClassifying SchizophreniaAgnes Sophia PenuliarNo ratings yet
- ANALGETIKDocument1 pageANALGETIKsadam huseinNo ratings yet
- Guideline MERS Management in Malaysia, 2023Document123 pagesGuideline MERS Management in Malaysia, 2023Nezly IderusNo ratings yet
- Case ReportDocument12 pagesCase ReportJoão EduardoNo ratings yet
- Prevention Practice For Neuromuscular ConditionsDocument37 pagesPrevention Practice For Neuromuscular ConditionsArham ShamsiNo ratings yet
- Bahasa Inggris Bu FanniDocument5 pagesBahasa Inggris Bu Fanninina purbaNo ratings yet
- PATHO FALCON (Latest Edition)Document17 pagesPATHO FALCON (Latest Edition)Nikhil kumar Sangam.No ratings yet
- BFM 2000 Treatment SchemaDocument2 pagesBFM 2000 Treatment SchemaAnonymous 9dVZCnTXSNo ratings yet
- Osteosarcoma PDFDocument3 pagesOsteosarcoma PDFkc andrea torresNo ratings yet
- Healthy AgingDocument13 pagesHealthy AgingCarissa Mae Tapec EstradaNo ratings yet
- Otorhinolaryngology ENT Paper1 PDFDocument3 pagesOtorhinolaryngology ENT Paper1 PDFRoshni KNo ratings yet
- Family Case SampleDocument25 pagesFamily Case SampleGrInDoVe9097No ratings yet
- Case Presentation - DM (Tantsa Tamia)Document58 pagesCase Presentation - DM (Tantsa Tamia)tantsaNo ratings yet
- BMI For AgeDocument2 pagesBMI For AgeNeil AtanacioNo ratings yet
- Osmosis 7moDocument216 pagesOsmosis 7moFer CasasNo ratings yet
- Viral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDocument14 pagesViral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDARLENE CLAIRE ANDEZANo ratings yet
- Secondary Stroke PreventionDocument54 pagesSecondary Stroke PreventionHùng Phạm Lý ChíNo ratings yet
- Dapa-CKD - Applying Clinical Evidence To Clinical PracticeDocument45 pagesDapa-CKD - Applying Clinical Evidence To Clinical Practicedevikumar kelkarNo ratings yet
- Project in MapehDocument10 pagesProject in MapehRhina Marie Ramos DumaguinNo ratings yet
- Tau Chempath - Acid Base Imbalance & Pahology of Resp FailureDocument31 pagesTau Chempath - Acid Base Imbalance & Pahology of Resp FailureChipego ChiyaamaNo ratings yet
- Causes of DeathDocument12 pagesCauses of DeathMerle Ajcap0% (1)
- InformativeDocument2 pagesInformative3701Dhanush NadarNo ratings yet
- NCM 117 Midterm ReviewerDocument17 pagesNCM 117 Midterm ReviewerPia Rose RoqueNo ratings yet
- Tocilizumab For Rheumatoid Arthritis Results of The Phase III Clinical Trial ProgramDocument10 pagesTocilizumab For Rheumatoid Arthritis Results of The Phase III Clinical Trial ProgramasdffdsaNo ratings yet
- Myocardial Infarction NotesDocument6 pagesMyocardial Infarction NotesAshutosh BhaleraoNo ratings yet
- Ethics 143Document13 pagesEthics 143122ritik goyalNo ratings yet
- Tumour MarkersDocument34 pagesTumour MarkersAbdulelah MurshidNo ratings yet
- AdhdDocument2 pagesAdhdapi-671375887No ratings yet