Professional Documents
Culture Documents
PNEUMOTHORAX
PNEUMOTHORAX
Uploaded by
joemarie SalduaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PNEUMOTHORAX
PNEUMOTHORAX
Uploaded by
joemarie SalduaCopyright:
Available Formats
NCM 112 - Care of Clients with Problems in Oxygenation, Fluid & Electrolytes, Infectious
Inflammatory and Immunologic Response, Cellular Aberrations (Acute & Chronic)
walled air sacs in the lung tissue that can
rupture, resulting in pneumothorax.
PNEUMOTHORAX
Ruptured air blisters. Small air blisters
Definition (blebs) can develop on the top of the lungs.
These air blisters sometimes burst
Pneumothorax, or a collapsed lung, is the allowing air to leak into the space that
collection of air in the spaces around the surrounds the lungs.
lungs. The air buildup puts pressure on the
lungs, so it cannot expand as much as it Mechanical ventilation. A severe type of
normally. pneumothorax can occur in people who
The pressure in the pleural space is need mechanical assistance to breathe.
normally negative. The ventilator can create an imbalance of
Chest injury that allows air to enter the air pressure within the chest. The lung
pleural space resulting in a rise in may collapse completely.
intrathoracic pressure and the reduction in
Risk Factors
vital capacity.
Smoking. The risk increases with the
length of time and the number of
cigarettes smoked, even without
emphysema.
Genetics. Certain types of pneumothorax
appear to run in families.
Previous pneumothorax. Anyone who
has had one pneumothorax is at increased
risk of another.
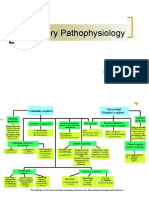
Pathophysiology
Air enters pleural space
Air accumulation in pleural cavity (Build up
positive pressure)
Etiology/Causes
Chest injury. Any blunt or penetrating
Compression and collapse of lungs
injury to your chest can cause lung
collapse. Some injuries may happen
during physical assaults or car crashes,
while others may inadvertently occur Decrease vital capacity of lungs and
during medical procedures that involve mediastinal shift
the insertion of a needle into the chest.
Lung disease. Damaged lung tissue is Pressure on lungs, trachea, heart and other
more likely to collapse. Lung damage can structures
be caused by many types of underlying
diseases, such as chronic obstructive
pulmonary disease (COPD), cystic
PNEUMOTHORAX
fibrosis, lung cancer or pneumonia.
Cystic lung diseases, such as
lymphangioleiomyomatosis and Birt-
Hogg-Dube syndrome, cause round, thin-
Classification DISEASE ASSOCIATED WITH SECONDARY
SPONTANEOUS PNEUMOTHORAX
Spontaneous pneumothorax.
COPD
Traumatic pneumothorax.
Tension pneumothorax. Asthma
HIV with pneumocystis pneumonia
Sponteneous Pneumothorax
Necrotizing pneumonia
A simple or spontaneous pneumothorax
occurs when air enters the pleural space Tuberculosis
through a breach of either the parietal or
visceral pleura. Sarcoidosis
Spontaneous pneumothorax refers to the Cystic fibrosis
abnormal collection of gas in the pleural
space between the lungs and the chest Bronchogenic carcinoma
wall. Idiopathic pulmonary fibrosis
Spontaneous pneumothorax occurs
without an obvious etiology such as Severe ARDS
trauma or iatrogenic causes. Langerhans cell histiocytosis
SYMPTOMS Lymphangioleiomyomatosis
Tachycardia
Collagen vascular disease
Dyspnea
Inhalational drug use like cocaine or
A feared COMPLICATION is tension marijuana
pneumothorax.
The DIAGNOSIS of spontaneous Thoracic endometriosis
pneumothorax is based on clinical
suspicion and can be confirmed with
imaging. Traumatic Pneumothorax
MANAGEMENT of spontaneous A traumatic pneumothorax occurs when
pneumothorax depends on multiple factors air escapes from a laceration in the lung
including the patient’s stability, the size of itself and enters the pleural space or from
the pneumothorax a wound in the chest wall.
Traumatic pneumothorax occurs when air
CLASSIFICATION
accumulates between the chest wall and
the lung because of an injury. It causes
Primary- Primary spontaneous
the lung to collapse partially or completely.
pneumothorax (PSP) occurs when the
patient does not have a history of the
underlying pulmonary disease
Secondary- secondary spontaneous CAUSES:
pneumothorax (SSP) is associated with a Penetrating or blunt trauma
history of an underlying pulmonary
disease. Rib fracture
Diving or flying
RISK FACTORS FOR PRIMARY
SPONTANEOUS PNEUMOTHORAX
SYMPTOMS:
Smoking
Tall thin body habitus in an otherwise Chest pain. (Most of the pain is due to the
healthy person injury that caused the pneumothorax)
Pregnancy Short of breath or breathe rapidly and feel
that their heart is racing (particularly if the
Marfan syndrome amount of air is large)
Familial pneumothorax
If air accumulates under the skin, the skin
feels crackly and makes a crackling sound
when touched.
DIAGNOSTIC low blood oxygen levels
increased heart rate
Chest x-ray low blood pressure
altered mental status
Doctors usually diagnose a pneumothorax Jugular venous distension
based on a chest x-ray. Sometimes Cyanosis
pneumothorax is diagnosed when CT or Respiratory failure
ultrasonography is done to diagnose other Cardiac arrest
chest or abdominal injuries.
Signs and Symptoms
Sharp chest or shoulder pain, made worse
TREATMENT by a deep breath or a cough
Removal of air from the pleural space Shortness of breath
Nasal flaring (from shortness of breath)
The goal of treatment is to remove the air Bluish color of the skin due to lack of
from the pleural space and allow the lung to oxygen
reinflate. Usually, a tube (thoracostomy or Chest tightness
chest tube) is inserted into the chest between
two ribs. The tube is attached to a suction Lightheadedness and near fainting
device to remove the air and to allow the lung
Easy fatigue
to reinflate. This procedure can be done using
only a local anesthetic. Abnormal breathing patterns or increased
effort of breathing
Rapid heart rate
Tension Pneumothorax
A tension pneumothorax occurs when air Shock and collapse
is drawn into the pleural space from a
lacerated lung or through a small opening
or wound in the chest wall. Diagnostics
Tension pneumothorax is an uncommon Thoracic CT: Studies show that CT is
condition with a malignant course that more sensitive than x-ray in detecting
might result in death if left untreated. thoracic injuries, lung contusion,
It is a severe condition that results when hemothorax, and pneumothorax. Early CT
air is trapped in the pleural space under may influence therapeutic management.
positive pressure, displacing mediastinal Chest x-ray: Reveals air and/or fluid
structures and compromising accumulation in the pleural space; may
cardiopulmonary function. show a shift of mediastinal structures
(heart).
ABGs: Variable depending on the degree
CAUSES of compromised lung function, altered
Penetrating or blunt trauma breathing mechanics, and the ability to
compensate. Paco2 occasionally elevated.
Barotrauma due to positive pressure Pao2 may be normal or decreased;
ventilation oxygen saturation usually decreased.
Percutaneous tracheostomy Thoracentesis: Presence
of blood/serosanguineous fluid indicates
Conversion of hemothorax.
spontaneous pneumothorax to tension Hb: Maybe decreased, indicating blood
loss.
Open pneumothorax when occlusive
dressing work as one way valve
Medical Management
SIGNS AND SYMPTOMS Chest tube. A small chest tube is inserted
severe shortness of breath near the second intercostal space to drain
shallow breathing the fluid and air. For patients with
acute chest pain jeopardized gas exchange, chest
tube insertion may be necessary to
achieve lung re-expansion. The priority is Monitor ABG levels.
to maintain the airway, breathing, and
circulation. The most important Assist with chest tube thoracostomy.
interventions focus on reinflating the lung
by evacuating the pleural air. Patients with
Encourage deep breathing exercises.
a primary spontaneous pneumothorax that
is small with minimal symptoms may have
spontaneous sealing and lung re- Conduct a comprehensive pain
expansion. assessment.
Maintain a closed chest drainage Nursing Diagnosis
system. Be sure to tape all connections, Acute pain related to the positive pressure
and secure the tube carefully at the in the pleural space.
insertion site with adhesive bandages. Ineffective breathing pattern related to
Regulate suction according to the chest respiratory distress.
tube system directions; generally, suction Ineffective peripheral tissue
does not exceed 20 to 25 cm H2O perfusion related to severe hypoxemia.
negative pressure. Anxiety related to difficulty in breathing.
Monitor a chest tube unit for any kinks
or bubbling. These could indicate an air Evaluation
leak, but do not clamp a chest tube Pain is relieved.
without a physician’s order because Adhered to prescribed pharmacological
clamping may lead to tension regimen.
pneumothorax. Established a normal, effective respiratory
pattern as evidenced by absence of
Autotransfusion. Autotransfusion cyanosis.
involves taking the patient’s own blood Demonstrated increase in perfusion.
that has been drained from the chest, Patient is relaxed and reported anxiety is
filtering it, and then transfusing it back into reduced to a manageable level.
the vascular system.
Antibiotics. Antibiotics are usually Prepared by:
prescribed to combat infection from
contamination. PASCUA, HEANGEL ORIO
Oxygen therapy. The patient with SALDUA, MARJELLA
possible tension pneumothorax should
immediately be given a high concentration
of supplemental oxygen to treat the
hypoxemia.
Surgical Management
If more than 1500 ml of blood is aspirated
initially by thoracentesis, the rule is to open the
chest wall surgically.
Thoracotomy. The chest wall is opened
surgically to remove the blood or air
trapped in the pleural space.
Nursing Intervention
Assess lung sounds.
Assess respiratory rate and rhythm.
Evaluate imaging studies.
Apply oxygen as ordered.
You might also like
- Pneumothorax Concept Map: Diagnostic TestsDocument1 pagePneumothorax Concept Map: Diagnostic TestsJoshua Villarba80% (5)
- Risk Management PlanDocument4 pagesRisk Management PlanHannah BalucaNo ratings yet
- Introduction To Clinical Psychology Notes 1Document83 pagesIntroduction To Clinical Psychology Notes 1Paulo Miguel GernaleNo ratings yet
- Bariatric Case StudyDocument11 pagesBariatric Case Studyapi-346620455100% (3)
- Chest DrainDocument4 pagesChest DrainGALINDO PE?A JOSE EDUARDONo ratings yet
- Chapter 63 - Pleural Disease - Rosen's Emergency Medicine 10thDocument10 pagesChapter 63 - Pleural Disease - Rosen's Emergency Medicine 10thAlex DegraciaNo ratings yet
- Pneumothorax: Glenna B. Winnie and Steven V. LossefDocument5 pagesPneumothorax: Glenna B. Winnie and Steven V. LossefJha BhoenkNo ratings yet
- Pleural Disease: Joshua M. Kosowsky and Heidi H. KimberlyDocument10 pagesPleural Disease: Joshua M. Kosowsky and Heidi H. KimberlyJha BhoenkNo ratings yet
- Other Conditions of The Lung (Abscesses, Inhaled Foreign Bodies, Bullous Lung Disease, Hydatid)Document5 pagesOther Conditions of The Lung (Abscesses, Inhaled Foreign Bodies, Bullous Lung Disease, Hydatid)Zilvia TambengiNo ratings yet
- PneumothoraxDocument7 pagesPneumothoraxKareliya ChiragNo ratings yet
- TBL Enfermedades de La Pleura - Lectura 2Document13 pagesTBL Enfermedades de La Pleura - Lectura 2Jose LunaNo ratings yet
- Pneumothorax: TiologyDocument1 pagePneumothorax: TiologySiti Komariyah21No ratings yet
- Pneumothorax and Pneumomediastinum: Dr. Emad EfatDocument89 pagesPneumothorax and Pneumomediastinum: Dr. Emad Efatinterna MANADONo ratings yet
- SAL273Document17 pagesSAL273sumNo ratings yet
- Pneumothorax: ClinicalDocument5 pagesPneumothorax: ClinicalAlexander PazNo ratings yet
- What Is A Pneumothorax?Document7 pagesWhat Is A Pneumothorax?llyrycNo ratings yet
- Pneumothorax: David E. Manthey and Bret A. NicksDocument9 pagesPneumothorax: David E. Manthey and Bret A. NicksJha BhoenkNo ratings yet
- Spontaneous PneumothoraxDocument4 pagesSpontaneous PneumothoraxĐřë Ťįmmý ŤūřněŗNo ratings yet
- Tension Pneumothorax PDFDocument2 pagesTension Pneumothorax PDFClarissa Aileen Caliva AdoraNo ratings yet
- PneumothoraksDocument19 pagesPneumothoraksLee' a MiinnNo ratings yet
- Peneumotorak (Repaired)Document28 pagesPeneumotorak (Repaired)vitha guslawNo ratings yet
- Case Study For PneumothoraxDocument4 pagesCase Study For PneumothoraxGabbii CincoNo ratings yet
- Pneumothorax and AsthmaDocument8 pagesPneumothorax and AsthmaKyle FernandezNo ratings yet
- Learning Objectives: Niken Rahmatia 1418011152Document17 pagesLearning Objectives: Niken Rahmatia 1418011152Taro RahmatiaNo ratings yet
- Lecture 5 Pneumonia and SepsisDocument9 pagesLecture 5 Pneumonia and Sepsishenlo hiNo ratings yet
- Tension Pneumothorax - StatPearls - NCBI BookshelfDocument9 pagesTension Pneumothorax - StatPearls - NCBI Bookshelfshinta damayantiNo ratings yet
- Pneumothorax Facts: SmokingDocument2 pagesPneumothorax Facts: SmokingDiana Laura LeiNo ratings yet
- Pneumothorax: Dr. Ibnu DharmajatiDocument16 pagesPneumothorax: Dr. Ibnu DharmajatiIbnu DharmajatiNo ratings yet
- Nejm 200003233421207Document7 pagesNejm 200003233421207Ami DhaniaNo ratings yet
- PneumothoraxDocument11 pagesPneumothoraxManoj RanadiveNo ratings yet
- Eumothorax: Assessment and Diagnostic TestingDocument4 pagesEumothorax: Assessment and Diagnostic TestingPANTS1No ratings yet
- Pleural Cavity Lung Physical Trauma Blast Injury Complication of Medical TreatmentDocument3 pagesPleural Cavity Lung Physical Trauma Blast Injury Complication of Medical TreatmentMansi KhullarNo ratings yet
- PULMO - Pleural DiseaseDocument11 pagesPULMO - Pleural DiseaseHajime NakaegawaNo ratings yet
- Bronchopneumonia or Bronchial Pneumonia or "Bronchogenic Pneumonia" (Not To BeDocument3 pagesBronchopneumonia or Bronchial Pneumonia or "Bronchogenic Pneumonia" (Not To Beverniejhoy09No ratings yet
- Pneumothora X: Oleh: Dela Oktarini, S.Ked Pembimbing: Dr. Amran Sinaga, SP.BDocument20 pagesPneumothora X: Oleh: Dela Oktarini, S.Ked Pembimbing: Dr. Amran Sinaga, SP.BSafira Amilia RamadaniNo ratings yet
- Pneumonia IsDocument17 pagesPneumonia IsRadman Dormendo ItelluNo ratings yet
- Oral Revalida FinalsDocument10 pagesOral Revalida FinalsRaven PerejaNo ratings yet
- Week 4 Restrictive DisordersDocument212 pagesWeek 4 Restrictive Disordersdelrosariojm87No ratings yet
- Wa0039.Document20 pagesWa0039.shadesofcuddaloreNo ratings yet
- Diagnosis of Pneumothorax in Critically Ill Adults: James J Rankine, Antony N Thomas, Dorothee FluechterDocument6 pagesDiagnosis of Pneumothorax in Critically Ill Adults: James J Rankine, Antony N Thomas, Dorothee FluechternovywardanaNo ratings yet
- Pneumothorax: Disturbance in OxygenationDocument27 pagesPneumothorax: Disturbance in Oxygenationamier90No ratings yet
- Pneumothorax: Risk Factors For A PneumothoraxDocument12 pagesPneumothorax: Risk Factors For A Pneumothoraxyangi dokaNo ratings yet
- Respiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDocument12 pagesRespiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDoc JacqueNo ratings yet
- Principles of Diagnosis and Management of Traumatic PneumothoraxDocument14 pagesPrinciples of Diagnosis and Management of Traumatic PneumothoraxEkaNo ratings yet
- What Is A PneumothoraxDocument2 pagesWhat Is A PneumothoraxpawnayNo ratings yet
- Bab I Pendahuluan 1.1. Latar BelakangDocument18 pagesBab I Pendahuluan 1.1. Latar BelakangAntasiaSiregarNo ratings yet
- PneumothoraxDocument43 pagesPneumothoraxSravani KanchiNo ratings yet
- Prof. M. A. Wahab Department of Medicine Holy Family Red Crescent Medical College HospitalDocument6 pagesProf. M. A. Wahab Department of Medicine Holy Family Red Crescent Medical College Hospitalram krishnaNo ratings yet
- PneumomediastinumDocument6 pagesPneumomediastinumsteven hkNo ratings yet
- Pulmonary InfectionDocument9 pagesPulmonary InfectionlalaNo ratings yet
- Absceso de Pulmon ErsDocument9 pagesAbsceso de Pulmon ErsAngela Fonseca LatinoNo ratings yet
- Introduction BronchoPneumoniaDocument2 pagesIntroduction BronchoPneumoniaJanna FavilaNo ratings yet
- Diseases of Respiratory SystemDocument23 pagesDiseases of Respiratory SystemMarchelle Fae EsmallaNo ratings yet
- Update On The Diagnosis and Treatment of Tracheal and Bronchial InjuryDocument7 pagesUpdate On The Diagnosis and Treatment of Tracheal and Bronchial InjurymeiutaNo ratings yet
- Pneumothorax: From Definition To Diagnosis and Treatment: Review ArticleDocument5 pagesPneumothorax: From Definition To Diagnosis and Treatment: Review ArticleRiani NazilaNo ratings yet
- Pneumothorax, Spontaneous: Basic Information DiagnosisDocument4 pagesPneumothorax, Spontaneous: Basic Information DiagnosisJha BhoenkNo ratings yet
- Pneumothorax Emergency DepartmentDocument2 pagesPneumothorax Emergency DepartmentDaud YudhistiraNo ratings yet
- Pneumothorax (Collapsed Lung) : What Is A Pneumothorax?Document17 pagesPneumothorax (Collapsed Lung) : What Is A Pneumothorax?Hazel EstayanNo ratings yet
- Lung Abscess Handout PDFDocument3 pagesLung Abscess Handout PDFTansanee MalivalayaNo ratings yet
- Get Homework/Assignment DoneDocument9 pagesGet Homework/Assignment DoneHomework PingNo ratings yet
- KHUZDocument9 pagesKHUZNoor Ashraff Bin MohamadNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- Pleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Community Health RevisionDocument21 pagesCommunity Health Revisionconradlin06No ratings yet
- KSM Orthopedi New1Document20 pagesKSM Orthopedi New1rspku mayongNo ratings yet
- Undertaking Declaration: Examination in Physics For Class Xii Aatthe Millennium School, IndoreDocument29 pagesUndertaking Declaration: Examination in Physics For Class Xii Aatthe Millennium School, IndoreAnirudh VermaNo ratings yet
- Trauma GuidelinesDocument592 pagesTrauma GuidelinesAlvaro Perez Henriquez100% (1)
- 4Document19 pages4engineering_readerNo ratings yet
- Lansium Domesticum Corr. Leaf Extract Spray As Bioinsecticide For Aedes Aegypti Mosquito ControlDocument9 pagesLansium Domesticum Corr. Leaf Extract Spray As Bioinsecticide For Aedes Aegypti Mosquito ControlPeterson RonquilloNo ratings yet
- Paediatric Proton Therapy (Thomas 2019)Document9 pagesPaediatric Proton Therapy (Thomas 2019)Milda InayahNo ratings yet
- Labyrinth It IsDocument45 pagesLabyrinth It IsNana OkujavaNo ratings yet
- Atopic DermatitisDocument43 pagesAtopic DermatitisSaurav Arora100% (2)
- Example of Short Story A Little HeroDocument3 pagesExample of Short Story A Little HeroDina MardaniNo ratings yet
- Narrative Report - NSTP 2nd Sem Chapter 3Document1 pageNarrative Report - NSTP 2nd Sem Chapter 3Clint Kove YtemNo ratings yet
- Chemistry Project Final 1Document12 pagesChemistry Project Final 1mokey420opNo ratings yet
- LIC Health Plus Plan No.901 Full FormDocument15 pagesLIC Health Plus Plan No.901 Full FormDhaval SarvaiyaNo ratings yet
- Viruses - Bacteria - Health 5th Sep, 2023Document27 pagesViruses - Bacteria - Health 5th Sep, 2023nazNo ratings yet
- Evaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisDocument5 pagesEvaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisyoanaNo ratings yet
- (Speech and Language Disorders) Zbigniew Tarkowski-A New Approach To Stuttering - Diagnosis and Therapy-Nova Biomedical (2017) PDFDocument233 pages(Speech and Language Disorders) Zbigniew Tarkowski-A New Approach To Stuttering - Diagnosis and Therapy-Nova Biomedical (2017) PDFjozanekNo ratings yet
- Rectal Cancer,: Clinical Practice Guidelines in OncologyDocument28 pagesRectal Cancer,: Clinical Practice Guidelines in OncologyRaíla SoaresNo ratings yet
- Neuroanatomy NotesDocument26 pagesNeuroanatomy Notesdeyar janblyNo ratings yet
- PTB Guidelines 2006 IntroductionDocument17 pagesPTB Guidelines 2006 IntroductionMaria Concepcion Connie DingleNo ratings yet
- Small Pox: A Child Infected With SmallpoxDocument5 pagesSmall Pox: A Child Infected With SmallpoxJavee_Viccent__5618No ratings yet
- 1 SMDocument55 pages1 SMCharlotteNo ratings yet
- Endocrine SystemDocument8 pagesEndocrine SystemgabbypeigNo ratings yet
- Challenges and Opportunities in Oncology Drug DeveDocument6 pagesChallenges and Opportunities in Oncology Drug Devevictor.m.camposNo ratings yet
- FIFe EMS System User GuidelinesDocument3 pagesFIFe EMS System User GuidelinesAlexanderSmithNo ratings yet
- Chapter 6 Lesson 3 Health Institution. 11stem CDocument11 pagesChapter 6 Lesson 3 Health Institution. 11stem Cygyeon97No ratings yet
- Amphotericin B: Component Mg/liter Mol. Wt. Mol. (MM)Document7 pagesAmphotericin B: Component Mg/liter Mol. Wt. Mol. (MM)Echa Alifyanty SyarifNo ratings yet
- SMH Bristol Anaesthetic Chart HarveyDocument2 pagesSMH Bristol Anaesthetic Chart Harveyihtisham1No ratings yet