Professional Documents
Culture Documents
Poster
Poster
Uploaded by
Raif RizqullahCopyright:
Available Formats
You might also like
- ISO 7889 - 2003 - Bactérias LáticasDocument18 pagesISO 7889 - 2003 - Bactérias LáticasMaiara FonsecaNo ratings yet
- Beckett, Samuel - Eleutheria (Foxrock, 1995) PDFDocument225 pagesBeckett, Samuel - Eleutheria (Foxrock, 1995) PDFSiddharthGaikwad100% (3)
- Mastering Apache SparkDocument1,044 pagesMastering Apache SparkArjun Singh100% (6)
- Ken Black QA 5th Chapter 9 SolutionDocument44 pagesKen Black QA 5th Chapter 9 SolutionRushabh Vora50% (2)
- Case Report: Iatrogenic Intraspinal Epidermoid CystDocument3 pagesCase Report: Iatrogenic Intraspinal Epidermoid CystWilda HanimNo ratings yet
- Brainstem Epidermoid Cyst: An Update: Review ArticleDocument7 pagesBrainstem Epidermoid Cyst: An Update: Review ArticletiaraNo ratings yet
- DOI: 10.1515/jbcr-2015-0170: Case ReportDocument4 pagesDOI: 10.1515/jbcr-2015-0170: Case ReporttaufikolingNo ratings yet
- Intracranial Epidermoid CystDocument3 pagesIntracranial Epidermoid CystWildaHanimNo ratings yet
- Spinal Tumors ArticleDocument5 pagesSpinal Tumors ArticleMariaLakhaniNo ratings yet
- Spinal Tumors ArticleDocument5 pagesSpinal Tumors ArticleNouman Safdar AliNo ratings yet
- Forefoot Myopericytoma: A Case Reportand Review of The LiteratureDocument4 pagesForefoot Myopericytoma: A Case Reportand Review of The LiteratureIJAR JOURNALNo ratings yet
- TMP 33 BFDocument6 pagesTMP 33 BFFrontiersNo ratings yet
- Medial Orbital Epidermoid Cyst: Case ReportDocument3 pagesMedial Orbital Epidermoid Cyst: Case ReportTeodorNo ratings yet
- 1208 Case 1Document2 pages1208 Case 1willygopeNo ratings yet
- AsianJNeurosurg8121-7546405 205744Document8 pagesAsianJNeurosurg8121-7546405 205744WildaHanimNo ratings yet
- EPOSTER PABI Dr. Defri HeryadiDocument1 pageEPOSTER PABI Dr. Defri HeryadiSeptia Pristi RahmahNo ratings yet
- Ajr v8 Id1157Document2 pagesAjr v8 Id1157jenifer paathNo ratings yet
- Osteoma NepalDocument5 pagesOsteoma NepalRafael Lemos de SouzaNo ratings yet
- Kimura Disease, Pott'S Puffy - XXXXXDocument28 pagesKimura Disease, Pott'S Puffy - XXXXXHossam ThabetNo ratings yet
- Raval PDFDocument5 pagesRaval PDFdebby claudiNo ratings yet
- Diag DifDocument3 pagesDiag DifJulia LemboNo ratings yet
- 1808 8694 Bjorl 86 s1 0s23Document3 pages1808 8694 Bjorl 86 s1 0s23VITOR PEREZNo ratings yet
- Follicular Carcinoma of Thyroid Presenting As Brain MetastasisDocument3 pagesFollicular Carcinoma of Thyroid Presenting As Brain MetastasisArif Susilo RahadiNo ratings yet
- Mature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportDocument5 pagesMature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportHaribabuBabuNo ratings yet
- Spindle Cell Sarcoma of The Vagus Nerve Presenting As A Neck Lump - Case ReportDocument2 pagesSpindle Cell Sarcoma of The Vagus Nerve Presenting As A Neck Lump - Case Reportahmed_ateegNo ratings yet
- Surgical Removal of Spinal Tumors: Article by James Willey, Cst/Cfa, and Mark V. Iarkins, M DDocument8 pagesSurgical Removal of Spinal Tumors: Article by James Willey, Cst/Cfa, and Mark V. Iarkins, M DLuwiNo ratings yet
- Primary Spinal Cord Glioblastoma Multiforme A Report of Two CasesDocument4 pagesPrimary Spinal Cord Glioblastoma Multiforme A Report of Two CasesginadaisluNo ratings yet
- Extra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalDocument5 pagesExtra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalRonald QuezadaNo ratings yet
- Primary Intracranial Leiomyoma: A Case Report and Literature ReviewDocument3 pagesPrimary Intracranial Leiomyoma: A Case Report and Literature ReviewcandiddreamsNo ratings yet
- Iloretta Et Alsurgery ChordomaDocument5 pagesIloretta Et Alsurgery Chordomaricha kumalasariNo ratings yet
- JCDR 2Document4 pagesJCDR 2rajvolgaNo ratings yet
- Ccaass Cclliinniiq Quuee //ccaassee Rreeppo OrrttDocument4 pagesCcaass Cclliinniiq Quuee //ccaassee Rreeppo OrrttCamil ChouairyNo ratings yet
- Surgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year SurvivalDocument5 pagesSurgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year Survivallucasnegromonte0001No ratings yet
- Article in Press: Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument6 pagesArticle in Press: Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyOMFS FKG UnimusNo ratings yet
- 1 s2.0 S0899707121004113 MainDocument15 pages1 s2.0 S0899707121004113 MainJulian Rodriguez CelyNo ratings yet
- Intradiploic Meningioma of The Orbit A Case ReportDocument3 pagesIntradiploic Meningioma of The Orbit A Case ReportNurzulifa 15 104No ratings yet
- Surgical Outcome of Primary Intradural Surgical Outcome of Primary IntraduralDocument6 pagesSurgical Outcome of Primary Intradural Surgical Outcome of Primary Intraduralmazen alkarrasNo ratings yet
- Primary Extraskeletal Ewing Sarcoma of The Sinonasal Tract - A Rare Case Report and Review of The LiteratureDocument7 pagesPrimary Extraskeletal Ewing Sarcoma of The Sinonasal Tract - A Rare Case Report and Review of The LiteraturemohammadsayfooNo ratings yet
- 4 Meningoencefalocele PDFDocument4 pages4 Meningoencefalocele PDFOmar Lopez ArbolayNo ratings yet
- Surgical Neurology International: Unusual Growth Pattern of A MeningiomaDocument3 pagesSurgical Neurology International: Unusual Growth Pattern of A MeningiomaJamie NicholsNo ratings yet
- Steatocystoma Multiplex A Case Report of A Rare Disease Diagnosed in A Trauma PatientDocument5 pagesSteatocystoma Multiplex A Case Report of A Rare Disease Diagnosed in A Trauma Patientma hNo ratings yet
- Solitary Plasmacytoma of The Thoracolumbar Spine A Rare Cas - 2022 - InterdisciDocument5 pagesSolitary Plasmacytoma of The Thoracolumbar Spine A Rare Cas - 2022 - Interdiscib00403007No ratings yet
- AsianJNeurosurg102126-4310714 115827 PDFDocument3 pagesAsianJNeurosurg102126-4310714 115827 PDFSucipto HartonoNo ratings yet
- Medip, IJRMS-7729 ODocument7 pagesMedip, IJRMS-7729 ORagupathi MNo ratings yet
- Hannoun 2021Document4 pagesHannoun 2021mahaaNo ratings yet
- Por Rino 2021Document28 pagesPor Rino 2021lucedejonNo ratings yet
- Paraganglioma of Neck in Middle Aged Male: A Case ReportDocument4 pagesParaganglioma of Neck in Middle Aged Male: A Case ReportIJAR JOURNALNo ratings yet
- CE (Ra1) F (GH) PF1 (ANAK) PFA (AK) PF2 (PAG)Document2 pagesCE (Ra1) F (GH) PF1 (ANAK) PFA (AK) PF2 (PAG)Diana CantúNo ratings yet
- Intradural Spinal Tumors in Adults - Update On Management and OutcomeDocument18 pagesIntradural Spinal Tumors in Adults - Update On Management and OutcomeSuciatije PenelitianNo ratings yet
- Case Poster 2023Document1 pageCase Poster 2023Gladys Jan RealNo ratings yet
- 2017 Article 713Document5 pages2017 Article 713فرجني موغNo ratings yet
- Chondrosarcoma of The Cervical Spine: C Ase ReportDocument3 pagesChondrosarcoma of The Cervical Spine: C Ase ReportChoirina Nur AzizaNo ratings yet
- Boco 2008Document6 pagesBoco 2008Ananth BalakrishnanNo ratings yet
- Case Report - Epidermoid CystDocument1 pageCase Report - Epidermoid CystRaif RizqullahNo ratings yet
- Spinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SDocument3 pagesSpinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SRonald QuezadaNo ratings yet
- (10920684 - Neurosurgical Focus) Multiple Spinal Extradural Arachnoid Cysts Occurring in A ChildDocument4 pages(10920684 - Neurosurgical Focus) Multiple Spinal Extradural Arachnoid Cysts Occurring in A ChildRafael Mujica OreNo ratings yet
- Surgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsDocument7 pagesSurgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsHugo JBNo ratings yet
- Large Cerebral Arachnoid CystDocument2 pagesLarge Cerebral Arachnoid CystAtiquzzaman RinkuNo ratings yet
- 01 Testis Sparing Surgery For Epidermoid Cyst of Testis in A 3 Year Old BoyDocument3 pages01 Testis Sparing Surgery For Epidermoid Cyst of Testis in A 3 Year Old BoyAli AhmadNo ratings yet
- Intramedullary Spinal Cord Tumors: Part I - Epidemiology, Pathophysiology, and DiagnosisDocument11 pagesIntramedullary Spinal Cord Tumors: Part I - Epidemiology, Pathophysiology, and DiagnosiszixzaxoffNo ratings yet
- 1009 Case 2Document4 pages1009 Case 2willygopeNo ratings yet
- Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument7 pagesJournal of Oral and Maxillofacial Surgery, Medicine, and PathologyOMFS FKG UnimusNo ratings yet
- Cerebellopontine Angle Epidermoid CYST: Case ReportDocument3 pagesCerebellopontine Angle Epidermoid CYST: Case ReportTamajyoti GhoshNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- NECKDocument8 pagesNECKRaif RizqullahNo ratings yet
- Cranial Nerves - AADocument71 pagesCranial Nerves - AARaif RizqullahNo ratings yet
- PneumoperitoneumDocument31 pagesPneumoperitoneumRaif RizqullahNo ratings yet
- Pneumo PeritoneumDocument31 pagesPneumo PeritoneumRaif RizqullahNo ratings yet
- Revised 04/01/2021Document33 pagesRevised 04/01/2021Kim PowellNo ratings yet
- Electronics and Communication Engineering Sample ThesisDocument7 pagesElectronics and Communication Engineering Sample Thesiseifvhpugg100% (1)
- 1097-1136 Metallogenic Provinces in An Evolving Geodynamic FrameworkDocument40 pages1097-1136 Metallogenic Provinces in An Evolving Geodynamic FrameworkLYNAMARICELA83No ratings yet
- SSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Document16 pagesSSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Vj AleserNo ratings yet
- Prototyping & Storyboarding: IT2622 Chapter 4Document16 pagesPrototyping & Storyboarding: IT2622 Chapter 4empresscpy crackerNo ratings yet
- F.Y.B.Sc. CS Syllabus - 2021 - 22Document47 pagesF.Y.B.Sc. CS Syllabus - 2021 - 22D91Soham ChavanNo ratings yet
- Botech. IDocument37 pagesBotech. IKevin Rose BarnuevoNo ratings yet
- Exercises No 1: Exercise 1Document6 pagesExercises No 1: Exercise 1M ILHAM HATTANo ratings yet
- TTD Series Configurable Fault AnnunciatorDocument4 pagesTTD Series Configurable Fault AnnunciatorAlejandroMuñozNo ratings yet
- Experiment 1Document9 pagesExperiment 1Mehar HamzaNo ratings yet
- Death of A Salesman by Arthur MillerDocument125 pagesDeath of A Salesman by Arthur MillerNaman VasalNo ratings yet
- Midtown Ratepayers Association's Letter To Ontario OmbudsmenDocument3 pagesMidtown Ratepayers Association's Letter To Ontario OmbudsmenAndrew GrahamNo ratings yet
- First Quarterly Assessment Intle7: School Year 2021-2022Document3 pagesFirst Quarterly Assessment Intle7: School Year 2021-2022marjorie rochaNo ratings yet
- Brainy kl7 Unit Test 7 CDocument5 pagesBrainy kl7 Unit Test 7 CMateusz NochNo ratings yet
- Bio Drosophilia Mini Project 2 1Document15 pagesBio Drosophilia Mini Project 2 1jocyeo0% (1)
- Airside Driving HandbookDocument23 pagesAirside Driving HandbookBrandon Wong100% (1)
- Microsoft Software License Terms Windows 7 Professional These License TermsDocument14 pagesMicrosoft Software License Terms Windows 7 Professional These License Termsma mayNo ratings yet
- शरीर में सन्निहित शक्ति-केंद्र या चक्र Inner Powers Center or Chakra in BodyDocument33 pagesशरीर में सन्निहित शक्ति-केंद्र या चक्र Inner Powers Center or Chakra in BodygujjuNo ratings yet
- Railway Recruitment Board SiliguriDocument9 pagesRailway Recruitment Board SiliguripranavsircarNo ratings yet
- Field Report of Sargodha: Bs-Geology 8Document36 pagesField Report of Sargodha: Bs-Geology 8Zara MathewNo ratings yet
- Or On LineDocument10 pagesOr On LinekateNo ratings yet
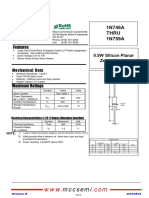
- Mccsemi: 1N746 A Thru 1N759 ADocument3 pagesMccsemi: 1N746 A Thru 1N759 AЕвгений ИвановNo ratings yet
- Classroom Management and Student Motivation: Clare Heaney: Director of StudiesDocument28 pagesClassroom Management and Student Motivation: Clare Heaney: Director of StudiesRyan BantidingNo ratings yet
- The Silt Verses - Chapter 21 TranscriptDocument32 pagesThe Silt Verses - Chapter 21 TranscriptVictória MoraesNo ratings yet
- Canadian Soil Quality Guidelines For The Protection of Environmental and Human Health Uranium 2007Document14 pagesCanadian Soil Quality Guidelines For The Protection of Environmental and Human Health Uranium 2007njcojann_co901745No ratings yet
Poster
Poster
Uploaded by
Raif RizqullahCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Poster
Poster
Uploaded by
Raif RizqullahCopyright:
Available Formats
A Rare Case of Intradural Extramedullar Epidermoid Cyst at Cauda
Equina level in 2- Years Old Female Child : A CASE REPORT
Muh. Raif Risqullah1, Aristianti1, Andi Asadul Islam1
1Department of Neurosurgery, Medical Faculty of Hasanuddin University, Makassar, Indonesia
Introduction Discussion
Epidermoid cyst tumors are benign tumor and comprising of less than 1% of We describe here a rare case of a patient with a nondysraphic spine in
tumors found in the spine [1]. These tumors originate from pathological whom the anamnestic and radiological elements were suggestive of a dermal
implanting of epidermal cells into the spinal canal. Consequently, these sinus and that the diagnosis of epidermoid cyst was only objectified
tumors may be congenital when there is inappropriate closure of the neural intraoperatively.
tube or iatrogenic cause of patients who have had former lumbar punctures, Epidermoid cysts (ECs) are uncommon benign lesions with an incidence of
trauma, or surgery [1, 2]. Epidermoid cyst is a slow growing tumor with less than 1% in the spine. The etiology of these tumors is classiied as
nonspecific clinical and radiology characteristics. In this report, we present congenital or acquired [1,3]
case of a 2 Years old female with a congenital Epidermoid Cyst at cauda Congenital ECs are rare and frequently associated with others spinal
equina[2]. dysraphism following spina biida, dermal si- nus, and syringomyelia while
acquired ECs occur following re- peated lumbar punctures, trauma, or surgery
Case Report [4]
The signs and symptoms of these tumors vary with the level of involvement
but do not differ from other lesions in the spinal column [2,5]
A 2-year-old female child presented to the outpatient clinic with a nodule that Owing to the characteristic slow growing of this tumor, the diagnosis is
was brownish discoloured and a skin fold on the sacrum region observed sometimes delayed. On imaging, the MRI is the imaging of choice, the lesion
since birth without deficits neurologic and was healthy, feeding, and playing ap- peared T1-weighted images isointense and hyperintense on T2-weighted
well. In her past medical history, there was no history of lumbal puncture, and contrast enhancement is uncommon [4,6]
trauma or surgery of the spine. The parents come to hospital because the child However, other tumor in children may have the same characteristics including
fell and her nodule is burst and bleeding. After that, we had a radiological meningiomas, lipomas, dermoids cyst, and teratomas [3]Our patient’s MRI of
examination the spine demonstrated
an intradural tumor from L3 to L4 levels. It was isointense on T1-weighted
images, hyperintense on T2-weighted.
Radiologic examination using MRI of the lumbosacral was obtained, and an
Nevertheless, in view of these radiological features, the pre- operative
intradural extramedullary lesion was detected, suggesting multiple epidermoid diagnosis of epidermoid cyst was not retained in the first instance but was
cysts at the level of the cauda equina L3-L4. The patient underwent based on the intraoperative macroscopic inspection and confirmed by
laminectomy and durotomy for tumour resection. The histology confirmed the histology subsequently. Per operatively, an encapsulated “pearly white” tumor
diagnosis of an epidermoid cyst was encountered. This macroscopic aspect of the tumor is the same as those
reported in the literature [1,2,6,8].
Surgical resection is the treatment of choice. Gross total resection is the goal
of surgery to avoid the risk of recurrence and aseptic meningitis. However,
when the tumor is tightly attached to the surrounding neural tissue a subtotal
excision should be performed to preserve neural function [2,5,6,8].
Unfortunately, in our patient, total tumor resection cannot be obtained because
after emptying of the cyst content, the capsule tightly adheres to the adjacent
nerve roots.
Conclusion
In this case report, spinal epidermoid cysts are rare and slow-growing, and
Intraoperative image show a circumscribed pearly white tumor on opening
surgery is the treatment of choice. Complete excision is curative and offers the
duramater Magnetic resonance imaging (MRI) of the spine demonstrated an
prospect of a disease free life devoid of deficiencies. Follow-up with post-
intradural tumor from L3 to L4 levels. It was isointense on T1-weighted
operative magnetic resonance imaging and a tumor marker are helpful.
images and hyperintense on T2- weighted images with contrast. Following
clinical and radiological examination dermal sinus diagnosis was considered
She underwent L3-L4 laminectomies tumor resection. After the dural opening, References
an encapsulated “pearly white” tumor was encountered. Emptying of the cyst
content was performed easily. Unfortunately, the tumor could not be easily [1] Dai Duong H, Pham AH, Chu HT, Le TD, Pham DT, Van Dong H.
removed because the capsule tightly adheres to the adjacent nerve roots. In Microsurgery for intradural epidermoid cyst at cauda equina level in a 9-year-
addition, an inspection of the intradural space did not reveal any spinal old child: a case report. Int J Surg Case Rep 2021;82:105932.
dysraphism. Histopathologic examination conirmed an epidermoid cyst [2] Er U, Yigitkanli K, Kazanci A, Bavbek M. Primary lumbar epidermoid tumor
mimicking schwannoma. J Clin Neurosci 2006;13(1):130–3.
[3] Morita M, Miyauchi A, Okuda S, Oda T, Aono H, Iwasaki M. Intraspinal
epidermoid tumor of the cauda equina region: seven cases and a review of the
literature. Clin Spine Surg 2012;25(5):292–8.
[4] Sivaraju L, Thakar S, Ghosal N, Hegde AS. Primary intradural sacral
epidermoid in a nondysraphic spine: case report and review of literature. J
Craniovertebr Junct Spine 2016;7(2):105.
[5] Liu H, Zhang JN, Zhu T. Microsurgical treatment of spinal epidermoid and
dermoid cysts in the lumbosacral region. J Clin Neurosci 2012;19(5):712–17.
[6] Beechar VB, Zinn PO, Heck KA, Fuller GN, Han I, Patel AJ,
et al. Spinal epidermoid tumors: case report and review of the literature.
Neurospine 2018;15(2):117–22.
[7] Teksam M, Casey SO, Michel E, Benson M, Truwit CL. Intraspinal
epidermoid cyst: diffusion-weighted MRI. Neuroradiology 2001;43(7):572–4.
[8] Sîrbu OM, Chirtes ̧ AV, Mitricã M, Sîrbu CA. Spinal intramedullary
epidermoid cyst: case report and updated literature review. World Neurosurg
2020;139:39–50.
You might also like
- ISO 7889 - 2003 - Bactérias LáticasDocument18 pagesISO 7889 - 2003 - Bactérias LáticasMaiara FonsecaNo ratings yet
- Beckett, Samuel - Eleutheria (Foxrock, 1995) PDFDocument225 pagesBeckett, Samuel - Eleutheria (Foxrock, 1995) PDFSiddharthGaikwad100% (3)
- Mastering Apache SparkDocument1,044 pagesMastering Apache SparkArjun Singh100% (6)
- Ken Black QA 5th Chapter 9 SolutionDocument44 pagesKen Black QA 5th Chapter 9 SolutionRushabh Vora50% (2)
- Case Report: Iatrogenic Intraspinal Epidermoid CystDocument3 pagesCase Report: Iatrogenic Intraspinal Epidermoid CystWilda HanimNo ratings yet
- Brainstem Epidermoid Cyst: An Update: Review ArticleDocument7 pagesBrainstem Epidermoid Cyst: An Update: Review ArticletiaraNo ratings yet
- DOI: 10.1515/jbcr-2015-0170: Case ReportDocument4 pagesDOI: 10.1515/jbcr-2015-0170: Case ReporttaufikolingNo ratings yet
- Intracranial Epidermoid CystDocument3 pagesIntracranial Epidermoid CystWildaHanimNo ratings yet
- Spinal Tumors ArticleDocument5 pagesSpinal Tumors ArticleMariaLakhaniNo ratings yet
- Spinal Tumors ArticleDocument5 pagesSpinal Tumors ArticleNouman Safdar AliNo ratings yet
- Forefoot Myopericytoma: A Case Reportand Review of The LiteratureDocument4 pagesForefoot Myopericytoma: A Case Reportand Review of The LiteratureIJAR JOURNALNo ratings yet
- TMP 33 BFDocument6 pagesTMP 33 BFFrontiersNo ratings yet
- Medial Orbital Epidermoid Cyst: Case ReportDocument3 pagesMedial Orbital Epidermoid Cyst: Case ReportTeodorNo ratings yet
- 1208 Case 1Document2 pages1208 Case 1willygopeNo ratings yet
- AsianJNeurosurg8121-7546405 205744Document8 pagesAsianJNeurosurg8121-7546405 205744WildaHanimNo ratings yet
- EPOSTER PABI Dr. Defri HeryadiDocument1 pageEPOSTER PABI Dr. Defri HeryadiSeptia Pristi RahmahNo ratings yet
- Ajr v8 Id1157Document2 pagesAjr v8 Id1157jenifer paathNo ratings yet
- Osteoma NepalDocument5 pagesOsteoma NepalRafael Lemos de SouzaNo ratings yet
- Kimura Disease, Pott'S Puffy - XXXXXDocument28 pagesKimura Disease, Pott'S Puffy - XXXXXHossam ThabetNo ratings yet
- Raval PDFDocument5 pagesRaval PDFdebby claudiNo ratings yet
- Diag DifDocument3 pagesDiag DifJulia LemboNo ratings yet
- 1808 8694 Bjorl 86 s1 0s23Document3 pages1808 8694 Bjorl 86 s1 0s23VITOR PEREZNo ratings yet
- Follicular Carcinoma of Thyroid Presenting As Brain MetastasisDocument3 pagesFollicular Carcinoma of Thyroid Presenting As Brain MetastasisArif Susilo RahadiNo ratings yet
- Mature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportDocument5 pagesMature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportHaribabuBabuNo ratings yet
- Spindle Cell Sarcoma of The Vagus Nerve Presenting As A Neck Lump - Case ReportDocument2 pagesSpindle Cell Sarcoma of The Vagus Nerve Presenting As A Neck Lump - Case Reportahmed_ateegNo ratings yet
- Surgical Removal of Spinal Tumors: Article by James Willey, Cst/Cfa, and Mark V. Iarkins, M DDocument8 pagesSurgical Removal of Spinal Tumors: Article by James Willey, Cst/Cfa, and Mark V. Iarkins, M DLuwiNo ratings yet
- Primary Spinal Cord Glioblastoma Multiforme A Report of Two CasesDocument4 pagesPrimary Spinal Cord Glioblastoma Multiforme A Report of Two CasesginadaisluNo ratings yet
- Extra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalDocument5 pagesExtra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalRonald QuezadaNo ratings yet
- Primary Intracranial Leiomyoma: A Case Report and Literature ReviewDocument3 pagesPrimary Intracranial Leiomyoma: A Case Report and Literature ReviewcandiddreamsNo ratings yet
- Iloretta Et Alsurgery ChordomaDocument5 pagesIloretta Et Alsurgery Chordomaricha kumalasariNo ratings yet
- JCDR 2Document4 pagesJCDR 2rajvolgaNo ratings yet
- Ccaass Cclliinniiq Quuee //ccaassee Rreeppo OrrttDocument4 pagesCcaass Cclliinniiq Quuee //ccaassee Rreeppo OrrttCamil ChouairyNo ratings yet
- Surgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year SurvivalDocument5 pagesSurgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year Survivallucasnegromonte0001No ratings yet
- Article in Press: Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument6 pagesArticle in Press: Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyOMFS FKG UnimusNo ratings yet
- 1 s2.0 S0899707121004113 MainDocument15 pages1 s2.0 S0899707121004113 MainJulian Rodriguez CelyNo ratings yet
- Intradiploic Meningioma of The Orbit A Case ReportDocument3 pagesIntradiploic Meningioma of The Orbit A Case ReportNurzulifa 15 104No ratings yet
- Surgical Outcome of Primary Intradural Surgical Outcome of Primary IntraduralDocument6 pagesSurgical Outcome of Primary Intradural Surgical Outcome of Primary Intraduralmazen alkarrasNo ratings yet
- Primary Extraskeletal Ewing Sarcoma of The Sinonasal Tract - A Rare Case Report and Review of The LiteratureDocument7 pagesPrimary Extraskeletal Ewing Sarcoma of The Sinonasal Tract - A Rare Case Report and Review of The LiteraturemohammadsayfooNo ratings yet
- 4 Meningoencefalocele PDFDocument4 pages4 Meningoencefalocele PDFOmar Lopez ArbolayNo ratings yet
- Surgical Neurology International: Unusual Growth Pattern of A MeningiomaDocument3 pagesSurgical Neurology International: Unusual Growth Pattern of A MeningiomaJamie NicholsNo ratings yet
- Steatocystoma Multiplex A Case Report of A Rare Disease Diagnosed in A Trauma PatientDocument5 pagesSteatocystoma Multiplex A Case Report of A Rare Disease Diagnosed in A Trauma Patientma hNo ratings yet
- Solitary Plasmacytoma of The Thoracolumbar Spine A Rare Cas - 2022 - InterdisciDocument5 pagesSolitary Plasmacytoma of The Thoracolumbar Spine A Rare Cas - 2022 - Interdiscib00403007No ratings yet
- AsianJNeurosurg102126-4310714 115827 PDFDocument3 pagesAsianJNeurosurg102126-4310714 115827 PDFSucipto HartonoNo ratings yet
- Medip, IJRMS-7729 ODocument7 pagesMedip, IJRMS-7729 ORagupathi MNo ratings yet
- Hannoun 2021Document4 pagesHannoun 2021mahaaNo ratings yet
- Por Rino 2021Document28 pagesPor Rino 2021lucedejonNo ratings yet
- Paraganglioma of Neck in Middle Aged Male: A Case ReportDocument4 pagesParaganglioma of Neck in Middle Aged Male: A Case ReportIJAR JOURNALNo ratings yet
- CE (Ra1) F (GH) PF1 (ANAK) PFA (AK) PF2 (PAG)Document2 pagesCE (Ra1) F (GH) PF1 (ANAK) PFA (AK) PF2 (PAG)Diana CantúNo ratings yet
- Intradural Spinal Tumors in Adults - Update On Management and OutcomeDocument18 pagesIntradural Spinal Tumors in Adults - Update On Management and OutcomeSuciatije PenelitianNo ratings yet
- Case Poster 2023Document1 pageCase Poster 2023Gladys Jan RealNo ratings yet
- 2017 Article 713Document5 pages2017 Article 713فرجني موغNo ratings yet
- Chondrosarcoma of The Cervical Spine: C Ase ReportDocument3 pagesChondrosarcoma of The Cervical Spine: C Ase ReportChoirina Nur AzizaNo ratings yet
- Boco 2008Document6 pagesBoco 2008Ananth BalakrishnanNo ratings yet
- Case Report - Epidermoid CystDocument1 pageCase Report - Epidermoid CystRaif RizqullahNo ratings yet
- Spinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SDocument3 pagesSpinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SRonald QuezadaNo ratings yet
- (10920684 - Neurosurgical Focus) Multiple Spinal Extradural Arachnoid Cysts Occurring in A ChildDocument4 pages(10920684 - Neurosurgical Focus) Multiple Spinal Extradural Arachnoid Cysts Occurring in A ChildRafael Mujica OreNo ratings yet
- Surgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsDocument7 pagesSurgical Management of Sacral Chordomas - Illustrative Cases and Current Management ParadigmsHugo JBNo ratings yet
- Large Cerebral Arachnoid CystDocument2 pagesLarge Cerebral Arachnoid CystAtiquzzaman RinkuNo ratings yet
- 01 Testis Sparing Surgery For Epidermoid Cyst of Testis in A 3 Year Old BoyDocument3 pages01 Testis Sparing Surgery For Epidermoid Cyst of Testis in A 3 Year Old BoyAli AhmadNo ratings yet
- Intramedullary Spinal Cord Tumors: Part I - Epidemiology, Pathophysiology, and DiagnosisDocument11 pagesIntramedullary Spinal Cord Tumors: Part I - Epidemiology, Pathophysiology, and DiagnosiszixzaxoffNo ratings yet
- 1009 Case 2Document4 pages1009 Case 2willygopeNo ratings yet
- Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument7 pagesJournal of Oral and Maxillofacial Surgery, Medicine, and PathologyOMFS FKG UnimusNo ratings yet
- Cerebellopontine Angle Epidermoid CYST: Case ReportDocument3 pagesCerebellopontine Angle Epidermoid CYST: Case ReportTamajyoti GhoshNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- NECKDocument8 pagesNECKRaif RizqullahNo ratings yet
- Cranial Nerves - AADocument71 pagesCranial Nerves - AARaif RizqullahNo ratings yet
- PneumoperitoneumDocument31 pagesPneumoperitoneumRaif RizqullahNo ratings yet
- Pneumo PeritoneumDocument31 pagesPneumo PeritoneumRaif RizqullahNo ratings yet
- Revised 04/01/2021Document33 pagesRevised 04/01/2021Kim PowellNo ratings yet
- Electronics and Communication Engineering Sample ThesisDocument7 pagesElectronics and Communication Engineering Sample Thesiseifvhpugg100% (1)
- 1097-1136 Metallogenic Provinces in An Evolving Geodynamic FrameworkDocument40 pages1097-1136 Metallogenic Provinces in An Evolving Geodynamic FrameworkLYNAMARICELA83No ratings yet
- SSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Document16 pagesSSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Vj AleserNo ratings yet
- Prototyping & Storyboarding: IT2622 Chapter 4Document16 pagesPrototyping & Storyboarding: IT2622 Chapter 4empresscpy crackerNo ratings yet
- F.Y.B.Sc. CS Syllabus - 2021 - 22Document47 pagesF.Y.B.Sc. CS Syllabus - 2021 - 22D91Soham ChavanNo ratings yet
- Botech. IDocument37 pagesBotech. IKevin Rose BarnuevoNo ratings yet
- Exercises No 1: Exercise 1Document6 pagesExercises No 1: Exercise 1M ILHAM HATTANo ratings yet
- TTD Series Configurable Fault AnnunciatorDocument4 pagesTTD Series Configurable Fault AnnunciatorAlejandroMuñozNo ratings yet
- Experiment 1Document9 pagesExperiment 1Mehar HamzaNo ratings yet
- Death of A Salesman by Arthur MillerDocument125 pagesDeath of A Salesman by Arthur MillerNaman VasalNo ratings yet
- Midtown Ratepayers Association's Letter To Ontario OmbudsmenDocument3 pagesMidtown Ratepayers Association's Letter To Ontario OmbudsmenAndrew GrahamNo ratings yet
- First Quarterly Assessment Intle7: School Year 2021-2022Document3 pagesFirst Quarterly Assessment Intle7: School Year 2021-2022marjorie rochaNo ratings yet
- Brainy kl7 Unit Test 7 CDocument5 pagesBrainy kl7 Unit Test 7 CMateusz NochNo ratings yet
- Bio Drosophilia Mini Project 2 1Document15 pagesBio Drosophilia Mini Project 2 1jocyeo0% (1)
- Airside Driving HandbookDocument23 pagesAirside Driving HandbookBrandon Wong100% (1)
- Microsoft Software License Terms Windows 7 Professional These License TermsDocument14 pagesMicrosoft Software License Terms Windows 7 Professional These License Termsma mayNo ratings yet
- शरीर में सन्निहित शक्ति-केंद्र या चक्र Inner Powers Center or Chakra in BodyDocument33 pagesशरीर में सन्निहित शक्ति-केंद्र या चक्र Inner Powers Center or Chakra in BodygujjuNo ratings yet
- Railway Recruitment Board SiliguriDocument9 pagesRailway Recruitment Board SiliguripranavsircarNo ratings yet
- Field Report of Sargodha: Bs-Geology 8Document36 pagesField Report of Sargodha: Bs-Geology 8Zara MathewNo ratings yet
- Or On LineDocument10 pagesOr On LinekateNo ratings yet
- Mccsemi: 1N746 A Thru 1N759 ADocument3 pagesMccsemi: 1N746 A Thru 1N759 AЕвгений ИвановNo ratings yet
- Classroom Management and Student Motivation: Clare Heaney: Director of StudiesDocument28 pagesClassroom Management and Student Motivation: Clare Heaney: Director of StudiesRyan BantidingNo ratings yet
- The Silt Verses - Chapter 21 TranscriptDocument32 pagesThe Silt Verses - Chapter 21 TranscriptVictória MoraesNo ratings yet
- Canadian Soil Quality Guidelines For The Protection of Environmental and Human Health Uranium 2007Document14 pagesCanadian Soil Quality Guidelines For The Protection of Environmental and Human Health Uranium 2007njcojann_co901745No ratings yet