Professional Documents
Culture Documents
Visual Summary On Neonatal Infection Determining The Need For Antibiotic Treatment of Babies Within 72 Hours of Birth PDF 9078464413
Visual Summary On Neonatal Infection Determining The Need For Antibiotic Treatment of Babies Within 72 Hours of Birth PDF 9078464413
Uploaded by
walaa alsharanyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Visual Summary On Neonatal Infection Determining The Need For Antibiotic Treatment of Babies Within 72 Hours of Birth PDF 9078464413
Visual Summary On Neonatal Infection Determining The Need For Antibiotic Treatment of Babies Within 72 Hours of Birth PDF 9078464413
Uploaded by
walaa alsharanyCopyright:
Available Formats
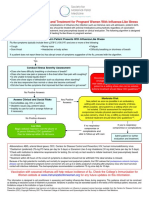
Neonatal infection: determining the need for antibiotic treatment of babies within 72 hours of birth (pg 1 of 2)
If there are any risk factors for early-
Before birth: for women in labour, identify If group B streptococcus is first identified in
onset neonatal infection (see box 1) or
and assess risk factors for early-onset the mother within 72 hours of baby’s birth:
if there are clinical indicators of possible
neonatal infection (see box 1). Throughout
early-onset neonatal infection (see box 2) • ask those directly involved in the baby’s
labour, monitor for any new risk factors.
perform an immediate clinical assessment. care if they have any concerns in
For guidance on managing prelabour relation to clinical indicators (see box 2)
Review the maternal and neonatal history
rupture of membranes at term, see the
and carry out a physical examination of the • identify any other risk factors present, and
NICE guideline on intrapartum care.
baby, including assessment of vital signs. look for clinical indicators of infection.
Any red flag No red flags, but 1 non-red-flag risk factor No red flags, risk factors or
OR OR clinical indicators
2 or more non-red-flag risk factors or No red flags, but 1 non-red-flag No laboratory evidence of
clinical indicators clinical indicator possible infection
Use clinical judgement: Do not routinely give
Perform investigations and
• Is it safe to withold antibiotics? antibiotic treatment.
start antibiotic treatment.
• Do the baby’s vital signs and clinical Continue routine care
Do not wait for test results
condition need to be monitored? (see the NICE guideline on
before starting antibiotics.
postnatal care).
If monitoring, continue for at least 12 hours
using a newborn early warning system.
YES NO
Consider performing Any clinical concerns during monitoring? Reassure family. When the
investigations and starting baby is discharged, give
antibiotic treatment. advice to parents or carers.
Note: The Kaiser Permanente neonatal
sepsis calculator can be used as an This is a summary of some of the advice in the NICE guideline on
alternative to the NICE red flag framework neonatal infection: antibiotics for prevention and treatment.
© NICE 2021. All rights reserved. Subject to Notice of rights.
Neonatal infection: determining the need for antibiotic treatment of babies within 72 hours of birth (pg 2 of 2)
Box 1: Risk factors for early-onset Box 2: Clinical indicators of possible early-onset neonatal infection
neonatal infection
Red flag clinical indicators:
Red flag risk factor: • Apnoea (temporary stopping of • Need for cardiopulmonary resuscitation
• Suspected or confirmed infection in another baby breathing)
• Need for mechanical ventilation
in the case of a multiple pregnancy. • Seizures
• Signs of shock
Other risk factors (non-red-flag):
Other clinical indicators (non-red-flag):
• Invasive group B streptococcal infection
in a previous baby or maternal group B • Altered behaviour or responsiveness • Persistent pulmonary hypertension of
streptococcal colonisation, bacteriuria or newborns
infection in the current pregnancy. • Altered muscle tone (for example,
floppiness) • Jaundice within 24 hours of birth
• Preterm birth following spontaneous labour
before 37 weeks’ gestation. • Feeding difficulties (for example, feed • Signs of neonatal encephalopathy
refusal)
• Confirmed rupture of membranes for more than • Temperature abnormality (lower than
18 hours before a preterm birth. • Feed intolerance, including vomiting, 36°C or higher than 38°C) unexplained
excessive gastric aspirates and by environmental factors
• Confirmed prelabour rupture of membranes at abdominal distension
term for more than 24 hours before the onset • Unexplained excessive bleeding,
of labour. • Abnormal heart rate (bradycardia or thrombocytopenia, or abnormal
tachycardia) coagulation
• Intrapartum fever higher than 38°C, if there is
suspected or confirmed bacterial infection. • Signs of respiratory distress (including • Altered glucose homeostasis
grunting, recession, tachypnoea) (hypoglycaemia or hyperglycaemia)
• Clinical diagnosis of chorioamnionitis.
• Hypoxia (for example, central cyanosis or • Metabolic acidosis (base deficit of
reduced oxygen saturation level) 10 mmol/litre or greater)
This is a summary of some of the advice in the NICE guideline on
neonatal infection: antibiotics for prevention and treatment.
© NICE 2021. All rights reserved. Subject to Notice of rights.
You might also like
- Labor-Vaginal Delivery Anne Jones, 17 Years Old Case Study With Complete Solutions 2023Document13 pagesLabor-Vaginal Delivery Anne Jones, 17 Years Old Case Study With Complete Solutions 2023CHARLES MAINANo ratings yet
- PNC Checklist AfricanDocument2 pagesPNC Checklist AfricanAudrey Andini0% (1)
- NICE 2021 Assessing and Managing The Risk of Early Onset SepsisDocument4 pagesNICE 2021 Assessing and Managing The Risk of Early Onset Sepsisradualina26No ratings yet
- Pil201702 01 Matab Antibiotics Baby Updated4Document4 pagesPil201702 01 Matab Antibiotics Baby Updated4min suhoNo ratings yet
- Niceng195guid Pathway1Document11 pagesNiceng195guid Pathway1Vane LévanoNo ratings yet
- Managing Postpartum Complications-SepsisDocument9 pagesManaging Postpartum Complications-SepsisRukaiya Auwal AliNo ratings yet
- 150327 Neonatal Sepsis 김세현 PDFDocument30 pages150327 Neonatal Sepsis 김세현 PDFirene aureliaNo ratings yet
- Journal Report FinalDocument33 pagesJournal Report FinalKevin Marcial AralarNo ratings yet
- 20 - Neonatal InfectionsDocument4 pages20 - Neonatal InfectionsYassboy MsdNo ratings yet
- Managing Postpartum Complications-SepsisDocument9 pagesManaging Postpartum Complications-SepsisDeepika khairwarNo ratings yet
- 2017 Influenza AlgorithmDocument1 page2017 Influenza AlgorithmFrandita Ivana TanisiwaNo ratings yet
- OB CH 19Document9 pagesOB CH 19Kaitlyn RayNo ratings yet
- Neonatal SepsisDocument31 pagesNeonatal Sepsisanwar jabariNo ratings yet
- Neonatal SepsisDocument7 pagesNeonatal Sepsispaningbatan.kristine.bNo ratings yet
- Fever With Focus in Well Appearing Child - 3yearsDocument15 pagesFever With Focus in Well Appearing Child - 3yearsShenillee BurgessNo ratings yet
- Management of Adult PUI With ILI 30042013-1Document3 pagesManagement of Adult PUI With ILI 30042013-1Rudzahan RamliNo ratings yet
- Prenatal Care AndreDocument29 pagesPrenatal Care AndreAndre PutraNo ratings yet
- Prenatal Care AndreDocument29 pagesPrenatal Care AndreAndre PutraNo ratings yet
- Preterm labour د.علية شعيبDocument58 pagesPreterm labour د.علية شعيبMohammad BelbahaithNo ratings yet
- Well Baby 2020 With NotesDocument119 pagesWell Baby 2020 With NotesSamsam Almarez BacaltosNo ratings yet
- SOP Neonatal SepsisDocument3 pagesSOP Neonatal SepsisEidi IdhamNo ratings yet
- Newborn Sepsis GuidelineDocument2 pagesNewborn Sepsis GuidelineAmelia ArnisNo ratings yet
- Assessment and Management Women in PregnantDocument1 pageAssessment and Management Women in Pregnantanisah tri agustiniNo ratings yet
- Postnatal Care Pre-Discharge Checklist:, CH IpDocument2 pagesPostnatal Care Pre-Discharge Checklist:, CH IpJharaNo ratings yet
- Young Febrile Infants Step by Step EvaluationDocument2 pagesYoung Febrile Infants Step by Step Evaluationhossein kasiriNo ratings yet
- Case 2 TG Retype PDFDocument15 pagesCase 2 TG Retype PDFElma CorpusNo ratings yet
- Risk Factor PneumoniaDocument6 pagesRisk Factor Pneumoniaali subchanNo ratings yet
- NUH - Hello BabyDocument32 pagesNUH - Hello BabyTony AndersonNo ratings yet
- Postpartum PDFDocument6 pagesPostpartum PDFPatrícia OliveiraNo ratings yet
- Preterm Labor: Ahmed Barefah Ahmed Al-Ghamdi Mohammed Al-TalhiDocument52 pagesPreterm Labor: Ahmed Barefah Ahmed Al-Ghamdi Mohammed Al-TalhiAdams Westlifer SophianoNo ratings yet
- Insidence of Fever in Labor and Risk of Neonatal SepsisDocument5 pagesInsidence of Fever in Labor and Risk of Neonatal SepsisSNFauziaNo ratings yet
- NCMA219 - W8 - Newborn ScreeningDocument10 pagesNCMA219 - W8 - Newborn ScreeningKayNo ratings yet
- NNF RecommendationDocument15 pagesNNF RecommendationSuman MondalNo ratings yet
- COVID 19 AlgorithmDocument1 pageCOVID 19 AlgorithmSonia Capirosi AyuningtiasNo ratings yet
- Trabajo Final de InglésDocument9 pagesTrabajo Final de Inglésliuvas Boizán CobasNo ratings yet
- Week 53 - Second Trimester LossDocument16 pagesWeek 53 - Second Trimester Lossnurishalo35No ratings yet
- Pre e Learning PlanDocument14 pagesPre e Learning Planapi-555538380No ratings yet
- Neonatal SepsisDocument63 pagesNeonatal SepsisDemewoz Fikir100% (2)
- Sepsis Updated AlgorithmDocument2 pagesSepsis Updated AlgorithmWahid Hilmy SulaimanNo ratings yet
- No. 197a-Fetal Health Surveillance: Antepartum Consensus GuidelineDocument21 pagesNo. 197a-Fetal Health Surveillance: Antepartum Consensus GuidelineFabricio EguíaNo ratings yet
- Newborn Resuscitation and Support of Transition of Infants at Birth GuidelinesDocument23 pagesNewborn Resuscitation and Support of Transition of Infants at Birth GuidelinesdodiNo ratings yet
- Maternal NSG ProceduresDocument18 pagesMaternal NSG ProceduresGARCIA, KYLA MAE A.No ratings yet
- 2.04 Surgical Illness in PregnancyDocument6 pages2.04 Surgical Illness in PregnancyRaquel ReyesNo ratings yet
- Needle Stick InjuryDocument27 pagesNeedle Stick InjuryVishal ThakareNo ratings yet
- Pre and Post PregnancyDocument23 pagesPre and Post PregnancyJitendra ChaudharyNo ratings yet
- Neonatal ObservationsDocument3 pagesNeonatal ObservationsMuhammad Bayu Zohari HutagalungNo ratings yet
- Hiv in Children AnnDocument6 pagesHiv in Children AnnAdakun SamuelNo ratings yet
- Neonatal Infection: Julniar M Tasli Herman Bermawi Afifa RamadantiDocument56 pagesNeonatal Infection: Julniar M Tasli Herman Bermawi Afifa RamadantiOtchi Pudtrie WijayaNo ratings yet
- Monkeypox and Pregnancy - What Maternal-Fetal Medicine Subspecialists Need To KnowDocument7 pagesMonkeypox and Pregnancy - What Maternal-Fetal Medicine Subspecialists Need To KnowariniNo ratings yet
- Obgm0331226 Id Consult DuffDocument6 pagesObgm0331226 Id Consult Duffsuraj rajpurohitNo ratings yet
- Group B Streptococcus: Women's & Children's ServicesDocument7 pagesGroup B Streptococcus: Women's & Children's ServicesYwagar YwagarNo ratings yet
- PRETERM LABOUR DR - ERTEQADocument24 pagesPRETERM LABOUR DR - ERTEQAMihraban OmerNo ratings yet
- Tumaob, Lealyn A. Group HDocument4 pagesTumaob, Lealyn A. Group H002No ratings yet
- Newborn Sepsis Clinical Practice GuidelineDocument2 pagesNewborn Sepsis Clinical Practice GuidelineAgus WijayaNo ratings yet
- Neonatal InfectionDocument56 pagesNeonatal InfectionajengdwintaNo ratings yet
- New Born ClassificationDocument47 pagesNew Born ClassificationEyob MizanNo ratings yet
- Ultimo NSTDocument21 pagesUltimo NSTj1b2v3No ratings yet
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)