Professional Documents
Culture Documents
Oschman 2011
Oschman 2011
Uploaded by
Cee AsmatOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oschman 2011
Oschman 2011
Uploaded by
Cee AsmatCopyright:
Available Formats
clinical Consultation Dexmedetomidine
clinical c o n s u ltat i o n
Dexmedetomidine for opioid and benzodiazepine
withdrawal in pediatric patients
Alexandra Oschman, Tara McCabe, and Robert J. Kuhn
O
pioids and benzodiazepines
are mainstays of sedation and Purpose. The published literature on the ciated with use of bolus doses and mainly
analgesia in the pediatric inten- use of dexmedetomidine as an adjunct involve central nervous system effects (e.g.,
to sedation and analgesia in the manage- hypotension, bradycardia), with no hemo-
sive care unit (PICU). Use of these
ment of pediatric narcotic withdrawal was dynamic manifestations. When bolus doses
medications often requires a balance reviewed. are used, strategies described in published
of pain relief and sedation, along Summary. Pediatric narcotic withdrawal reports entail a loading dose of 0.5–1.0
with the management of narcotic syndromes are reported to be increasingly mg/kg administered over 5–10 minutes, fol-
withdrawal. Narcotic withdrawal frequent in pediatric intensive care units. lowed by a continuous infusion at 0.1–1.4
syndromes were first described in the A number of tools specifically designed mg/kg/hr for a period of 1–16 days. More re-
neonatal population in the 1970s.1,2 for assessment of withdrawal in newborns search is needed to define the optimal use
and infants are in current use, including of dexmedetomidine in the management
Only in the last 20 years have narcotic
the widely used Finnegan Scoring System. of pediatric narcotic withdrawal.
withdrawal syndromes been recog- A limited number of studies and case re- Conclusion. A limited body of published
nized in other pediatric patients; ports suggest that dexmedetomidine, an evidence from retrospective studies and
most cases are a result of iatrogenic a2-receptor agonist with a mechanism of case reports suggests a potential role for
exposure to narcotics during long action similar to that of clonidine but with dexmedetomidine as an adjunct therapy to
hospital stays.2,3 Dexmedetomidine greater a2-receptor specificity, might have provide sedation and analgesia to reduce
is an a2-adrenergic receptor agonist a role in the treatment of pediatric with- narcotic withdrawal symptoms in pediatric
drawal (by blunting withdrawal symptoms patients.
that has the potential to decrease nar-
without causing respiratory depression
cotic withdrawal symptoms.4 While and by permitting shorter narcotic taper- Index terms: Benzodiazepines; Dexme-
published data are available regard- ing schedules) and also in the prevention of detomidine hydrochloride; Dosage; Drug
ing the use of dexmedetomidine as pediatric narcotic withdrawal (by reducing withdrawal; Hospitals; Mechanism of ac-
an adjunct for sedation and analgesia narcotic requirements). Potential adverse tion; Opiates; Pediatrics; Sympathomimetic
in pediatric patients, there are limited effects associated with dexmedetomidine agents; Toxicity
data on the use of dexmedetomidine use in pediatric patients are generally asso- Am J Health-Syst Pharm. 2011; 68:1233-8
for pediatric narcotic withdrawal
syndromes. For this review, clinical
studies were evaluated to assess the and subjective withdrawal symp- of narcotic withdrawal in the pedi-
appropriateness of dexmedetomi- toms. Several retrospective studies atric population has led to questions
dine use in this population. have reported withdrawal symptoms as to how to best prevent and treat
Withdrawal may be difficult to as- in 35–57% of children receiving con- pediatric narcotic withdrawal.
sess in the PICU due to the wide vari- tinuous infusion opioids and benzo- Withdrawal symptoms are often
ability and nonspecificity of objective diazepines.3 The increased awareness related to sympathetic system acti-
Alexandra Oschman, Pharm.D., is Neonatal Intensive Care Unit Hospital and Clinics, 2401 Gillham Road, Kansas City, MO 64108
Clinical Pharmacist Specialist, Children’s Mercy Hospital and Clin- (aoschman@cmh.edu).
ics, Kansas City, MO. Tara McCabe, Pharm.D., is Pediatric Clinical The authors have declared no potential conflicts of interest.
Pharmacy Specialist, Shands at the University of Florida Hospital,
Gainesville. Robert J. Kuhn, Pharm.D., is Associate Director of Copyright © 2011, American Society of Health-System Pharma-
Pharmacy Services, Kentucky Children’s Hospital, University of cists, Inc. All rights reserved. 1079-2082/11/0701-1233$06.00.
Kentucky Healthcare. DOI 10.2146/ajhp100257
Address correspondence to Dr. Oschman at Children’s Mercy
Am J Health-Syst Pharm—Vol 68 Jul 1, 2011 1233
clinical consultation Dexmedetomidine
The Clinical Consultation section features retrospective chart review involving withdrawal is not standardized, and
articles that provide brief advice on how to 40 pediatric patients found a 35% a variety of approaches are in cur-
handle specific drug therapy problems. All rate of withdrawal in patients receiv- rent use.3,7,8 Using a scoring system
articles are based on a systematic review ing mid azolam continuous infu- is an effective way to standardize the
of the literature. The assistance of ASHP’s sions.9 Other research indicates that evaluation of narcotic withdrawal,
Section of Clinical Specialists and Scientists patients who receive a cumulative and there are several scoring systems
in soliciting Clinical Consultation submis- midazolam dosage of 60 mg/kg or available; while all have limitations,
sions is acknowledged. Unsolicited submis- higher are more likely to experience they can help guide assessment for
sions are also welcome. withdrawal.7,8 narcotic withdrawal. Of the six scales
Fentanyl is a rapid-acting, syn- currently used for assessment of
thetic mu–opioid receptor agonist.10 pediatric withdrawal, several were
vation, which includes tachycardia, Fentanyl is a highly lipid-soluble developed specifically for use in new-
tachypnea, diaphoresis, and hyper- drug and distributes effectively into borns and infants.
pyrexia. Other common symptoms adipose tissue. Acidosis can increase One widely used assessment tool
are vomiting and diarrhea. In severe the capacity of fentanyl to bind to is the Neonatal Abstinence Score
cases, muscle convulsion and seizure muscle and adipose tissue, resulting developed by Finnegan et al.1 for
activity can occur.3,5-8 There are sev- in prolongation of fentanyl storage.11 evaluation of newborns and infants
eral case reports of movement dis- The delayed release of fentanyl from for withdrawal resulting from mater-
orders in children upon removal of adipose tissue may result in delayed nal exposure to narcotics. Using this
fentanyl or fentanyl and midazolam withdrawal. method, also known as the Finnegan
for sedation; the movement disorders The rate of withdrawal in pediat- Scoring System (FSS), patients are
included tremor, clonus, and choreic ric patients receiving fentanyl con- assessed for the presence and severity
facial movements.3,5,6 tinuous infusions has been reported of 31 signs and symptoms in three
Manifestations of withdrawal are as 57%.10,12 Katz et al.10 performed a categories (CNS, gastrointestinal, and
related to the half-life of the narcotic retrospective study of 23 infants who metabolic/vasomotor/respiratory);
used; thus, the onset can vary from received at least 24 hours of contin- each sign or symptom is assigned a
hours to days. Medications with uous infusion fentanyl. Withdrawal score of 1–5, with an aggregate score
active metabolites (e.g., morphine, was seen in 13 of the 23 infants; of 0–7 indicating mild withdrawal,
diazepam) are more likely to be as- those who experienced withdrawal a score of 8–11 indicating moderate
sociated with delayed withdrawal had higher mean cumulative fentan- withdrawal, and a score of 12–15
onset. Patients with renal or hepatic yl dosages (2.96 mg/kg versus 0.53 indicating severe withdrawal. As
dysfunction may also experience mg/kg) and a longer mean duration several of the signs and symptoms
delayed withdrawal onset due to of fentanyl use (13.1 days versus are specific to neonates and infants,
their decreased ability to metabolize 3.8 days). Other studies have shown the use and clinical utility of the
and clear drugs.7 Drug elimination is that a total fentanyl dosage of ≥1.5 Finnegan method in older pediatric
impaired to some degree in critically mg/kg or a duration of use of 5 days patients are limited; the method also
ill patients as a result of probable hy- or more resulted in a 50% rate of is thought by some to be too com-
poperfusion of the liver and kidneys withdrawal. Patients receiving dos- plicated for use in the PICU setting.3
during the acute-illness phase. This ages of ≥2.5 mg/kg or infusions last- Nonetheless, the method can be use-
phenomenon can result in accumu- ing 9 days or more had a 100% rate of ful in the clinical assessment of opi-
lation of drug with prolonged use withdrawal.2,7,8 oid and benzodiazepine withdrawal
and may influence the development The choice of pharmacotherapy in children.
of withdrawal syndromes. for prevention of narcotic withdraw- Other clinical assessment tools
al through use of tapering schedules specifically designed for assessment of
Opioid and benzodiazepine varies among institutions. The most withdrawal in children receiving long-
withdrawal common agents used are morphine, term opioid therapy in the PICU in-
Benzodiazepines provide sedation methadone, diazepam, lorazepam, clude the Sedation Withdrawal Score
via attachment to g-aminobutyric and phenobarbital. Regardless of the (SWS), derived from assessment of 12
receptors in the central nervous sys- medication chosen, an important neonatal signs and symptoms,13 and
tem (CNS). The result is a decrease aspect is observation for signs, symp- the Opioid–Benzodiazepine With-
in sympathetic outflow, which results toms, and alleviation of withdrawal. drawal Scale (OBWS), which is used
in sedation. Withdrawal has been to evaluate 16 parameters adapted
seen with a wide duration of use: Withdrawal assessment scales from the Finnegan method.14 The
from 11 hours to two months. A Assessment of pediatric narcotic validity and reliability of the SWS
1234 Am J Health-Syst Pharm—Vol 68 Jul 1, 2011
clinical Consultation Dexmedetomidine
and OBWS have not been firmly reflection of the small sample size of continued tapering of fentanyl and
established. patients and substantial variability of midazolam continuous infusions.16
individual patient response, empha- Finkel and Elrefai25 reported the
Use of dexmedetomidine sizing the need for clinical trials to case of an eight-month-old infant
Current pharmacotherapy regi- determine effective dosing. who had been mechanically venti-
mens for narcotic withdrawal consist Literature review. A PubMed lated since birth in the neonatal in-
of other narcotic agents. Clonidine search using the terms pediatric tensive care unit. At the age of seven
has been shown to have a role narcotic withdrawal, dexmedeto- months, the patient underwent a tra-
in neonatal abstinence syndrome midine, Precedex, clonidine, and cheostomy; 253 mg/kg/day of fentan-
(NAS) and is used as an adjunctive pediatric sedation was performed yl and 20.3 mg/kg/day of midazolam
therapy for opioid withdrawal in to identify articles addressing use were required for adequate sedation.
adults.15 Agathe et al.15 found that the of dexmedetomidine hydrochloride Dexmedetomidine was used for
use of oral clonidine hydrochloride for narcotic withdrawal in pediatric prevention of narcotic withdrawal.
1 mg/kg/dose every four hours as an patients. The published literature A Bispectral Index Score (BIS, a unit-
adjunct to diluted tincture of opium on dexmedetomidine use for opioid less scale of 0–100 on which 0 indi-
resulted in a 27% decrease in the me- withdrawal mainly consists of sev- cates coma, 60–90 indicates sedation,
dian length of therapy for NAS. eral case studies and two retrospec- and 100 indicates awake) was used
Dexmedetomidine’s chemical tive reviews involving a total of 20 to titrate dexmedetomidine with a
structure is similar to that of cloni- pediatric patients.16,22-25 target BIS of 60–80. Dexmedetomi-
dine, but the former has a greater Bejian and colleagues17 found a dine was initiated immediately after
specificity for the a2- (as opposed decrease in total daily doses of fen- discontinuation of the fentanyl and
to a1) receptor (1620:1 for dexme- tanyl (mean ± S.D., 16.58 ± 4.2 mg/kg/ midazolam continuous infusions
detomidine versus 220:1 for cloni- day versus 47.5 ± 15.1 mg/kg/day) and at a bolus dose of 1 mg/kg over 10
dine).4 With both drugs, activation midazolam (0.26 ± 0.1 mg/kg/day minutes and a continuous infusion
of a2-receptors results in analgesia, versus 1.08 ± 0.47 mg/kg/day) in 45 rate of 0.2–0.7 mg/kg/hr. Bolus doses
sedation, and anxiolysis. Due to the pediatric patients who received dex- were given every six hours until the
drugs’ similar mechanisms of action, medetomidine when compared with cumulative dose was 0.7 mg/kg/hr
it has been hypothesized that dexme- those who did not receive the drug. and the BIS was over 80, or until arte-
detomidine, like clonidine, may have The decreased opioid requirements rial blood pressures were greater than
a role in the management of opioid reported with dexmedetomidine use 20% of baseline. Bolus doses were
withdrawal syndromes. might help reduce the rate of with- needed on days 2–4. Dexmedetomi-
When used as an adjunct for seda- drawal and allow shorter tapering dine was tapered on day 7, and no
tion and analgesia, dexmedetomi- schedules. symptoms of narcotic withdrawal
dine was administered at a continu- Finkel et al.16 discussed two pe- were seen in the following two weeks.
ous infusion range of 0.1–1.4 mg/kg/ diatric patients who received dex- Baddigam et al. 22 reported on
hr.16-21 Several studies have indicated medetomidine for prevention of three pediatric patient cases in which
a median effective dose of 0.6–1 mg/ withdrawal and to aid in acute dexmedetomidine was used for
kg/hr.16,17,20,21 Carroll et al.18 reported discontinuation of fentanyl and mid- treatment of withdrawal syndromes.
a median effective dose of 0.7 mg/kg/ azolam continuous infusions after In one case, dexmedetomidine was
hr in patients who received dexme- cardiac transplantation. Bolus doses started due to a diagnosis of drug
detomidine for more than 24 hours of dexmedetomidine were used (1 and substance withdrawal. In the
(either as an adjunct, in anticipation mg/kg over 10 minutes), followed by other two cases, dexmedetomidine
of extubation, or alone for sedation) a continuous infusion of 0.8–1 mg/ was used when withdrawal symp-
and a median effective dose of 0.9 kg/hr for the first 10 postoperative toms were observed three to five
m g/kg/hr when dexmedetomidine days. In one case, bolus doses of days after surgery while the patients
was used as an adjunct for sedation. dexmedetomidine were given when were receiving continuous infusion
Patients who received dexmedetomi- signs of withdrawal were seen; dex- fentanyl (4–6 mg/kg/hr) and inter-
dine for more than 24 hours required medetomidine was tapered on days mittent midazolam (0.1 mg/kg/dose
higher median doses (0.5 mg/kg/hr 11 and 16 and then discontinued. every two hours as needed); one of
versus 1 mg/kg/hr), indicating that A similar protocol was followed for those patients required four mid-
there may be some tachyphylaxis the second patient. In both cases, the azolam doses per day, and the other
with extended use. The variability in patients responded to dexmedeto- required four to eight doses per day.
the dosage range of dexmedetomi- midine boluses for control of with- Dexmedetomidine was started after
dine observed in the study may be a drawal symptoms, which allowed for withdrawal symptoms were seen us-
Am J Health-Syst Pharm—Vol 68 Jul 1, 2011 1235
clinical consultation Dexmedetomidine
ing a bolus dose of 0.5 mg/kg over or treatment of narcotic withdrawal hypotension (30% of reported cases),
15 minutes, followed by a continu- is limited. While the studies and case hypertension (12% of cases), and
ous infusion at 0.25 mg/kg/hr, with reports described here provide useful bradycardia (9% of cases).27 Honey et
a maximum infusion rate of 0.6 mg/ insights, they involved a total of only al.28 conducted a retrospective study
kg/hr. All three patients experienced 20 patients, and 90% of the patients of 36 pediatric patients (median age,
amelioration of their withdrawal were less than four years old. In ad- 3.2 years; range, 0.01–16.75 years)
symptoms (hypertension, tachycar- dition, all five case reports (most by who received dexmedetomidine for
dia, diaphoresis, agitation, and trem- the same author) described the use at least two hours during a total of 41
ors) with dexmedetomidine. of bolus doses; although it is not infusions. They found an overall ad-
Two retrospective studies assessed reported in the literature, many in- verse event rate of 51%; bradycardia
the use of dexmedetomidine for stitutions do not use bolus doses of and hypotension occurred in 15%
opioid withdrawal in pediatric pa- dexmedetomidine due to the risk of and 22% of cases, respectively. The
tients.23,24 The first study reported on adverse events. Moreover, the range frequency of hypotension and bra-
seven infants (3–24 months old) who of reported continuous infusion dycardia reported by Honey et al.28
had received continuous fentanyl rates is wide, and rates were typi- is higher than that reported in other
infusions with intermittent mid- cally titrated to patient response, retrospective studies.19 In the review
azolam for extubation procedures.24 with the dose-limiting factors being conducted by Carroll et al.,18 brady-
Fentanyl and midazolam exposure hypotension and bradycardia. In ad- cardia was seen in 3% of cases and
was four to nine days, with a fentanyl dition to those issues, the package hypotension in 9% of cases, which is
infusion range of 4–9 mg/kg/hr. All insert states that dexmedetomidine consistent with the findings of other
seven patients had Finnegan scores is to be used for less than 24 hr,26 studies. The patients in the study by
of 12 or more along with signs and but in all of the reports described Carroll et al. ranged from 0.1 to 17.2
symptoms of severe withdrawal. here, dexmedetomidine was used years of age, with a median age of 1.5
Dexmedetomidine was given for for 2–16 days without additional years. Hypotension and bradycardia
treatment of withdrawal as a bolus of adverse events or development of are thought to be associated more
0.5 mg/kg over 10 minutes, followed withdrawal symptoms. with use of bolus doses than with
by a continuous infusion at 0.5 mg/ Adverse events. Dexmedetomi- continuous infusion of dexmedeto-
kg/hr. After the addition of dexme- dine is an imidazole compound midine; that might explain the dis-
detomidine, Finnegan scores were specific for the a2-adrenergic re- crepant adverse-event rates reported
consistently 7 or lower. The dexme- ceptors in the brain and spinal in the study by Carroll et al.,18 which
detomidine dose was decreased by cord. Its inhibition of neuronal fir- did not include patients who received
0.1 mg/kg/hr every 12–24 hours.24 ing in the CNS also results in hypo- bolus doses of dexmedetomidine,
The second study assessed use of a tension and bradycardia, which are and the study by Honey et al.,28 in
subcutaneous continuous infusion of dose-dependent, common adverse which 43.9% of patients received
dexmedetomidine for prevention or effects of dexmedetomidine.22 Dex- bolus doses.
treatment of withdrawal in seven pe- medetomidine does not have direct There is a potential for withdrawal
diatric patients (the patients required effects on the hemodynamics of the after the discontinuation of long-
i.v. access solely for the purpose heart. Bolus doses of dexmedeto- term infusions of dexmedetomidine.
of the dexmedetomidine continu- midine have been found to be com- Defining long-term dexmedetomi-
ous infusion).23 The subcutaneous monly associated with hypotension dine use is difficult. As previously
continuous infusion was initiated and bradycardia, which are thought mentioned, dexmedetomidine has a
at the same rate as the i.v. infusion to be mediated by the effects of mechanism of action similar to that
(0.8–1.4 mg/kg/hr). Subcutaneous dexmedetomidine on a1-adrenergic of clonidine, and withdrawal symp-
dexmedetomidine was used for pe- receptors in the brain and spinal cord toms have been reported after rapid
riods of four to seven days, with no at high doses. In addition, it has been discontinuation of long-term cloni-
reported adverse effects and modi- hypothesized that rapid boluses may dine therapy administered by oral,
fied Finnegan scores ranging from produce some peripheral a2B-receptor epidural, and transdermal routes.29
3 to 7, suggesting that subcutaneous stimulation; that is overcome with While more data on withdrawal after
continuous infusion may be an al- slow infusion. rapid discontinuation of dexmedeto-
ternative to i.v. continuous infusion Few studies have been conducted midine are needed, a few case reports
for delivery of dexmedetomidine.23 to assess adverse events associ- indicate that tolerance and with-
Limitations of published evi- ated with use of dexmedetomidine drawal phenomena can occur.7,30,31
dence. The available literature on in pediatric patients. In adults, the Proposed mechanisms for develop-
dexmedetomidine use for prevention most common adverse events are ment of tolerance include receptor
1236 Am J Health-Syst Pharm—Vol 68 Jul 1, 2011
clinical Consultation Dexmedetomidine
desensitization via loss of receptors Dexmedetomidine has a mecha- 8. Cho HH, O’Connell JP, Cooney MF et al.
Minimizing tolerance and withdrawal to
or receptor–effector uncoupling. nism of action similar to that of prolonged pediatric sedation: case report
Relief of withdrawal symptoms clonidine, with the benefit of greater and review of the literature. J Intensive
such as hypertension, tachycardia, selectivity for the a2-receptor. Dex- Care Med. 2007; 22:173-9.
9. Fonsmark L, Rasmussen YH, Carl P. Oc-
emesis, agitation, facial drooping, medetomidine may have a role in currence of withdrawal in critically ill
decreased verbal communication, decreasing the occurrence of narcotic sedated children. Crit Care Med. 1999;
and tonic–clonic seizures has been withdrawal after discontinuation 27:196-9.
10. Katz R, Kelly HW, Hsi A. Prospective
reported with reinitiation of dexme- of continuous infusion opioids and study on the occurrence of withdrawal in
detomidine.30 Unlike the reported benzodiazepines in pediatric pa- critically ill children who receive fentanyl
experience with other continuous tients. While the available evidence by continuous infusion. Crit Care Med.
1994; 22:763-7.
infusion medications for seda- demonstrates the usefulness of dex- 11. Caspi J, Klausner JM, Safadi T et al. De-
tion and analgesia, the symptoms medetomidine in pediatric critical layed respiratory depression following
of dexmedetomidine withdrawal care, questions persist as to the drug’s fentanyl anesthesia for cardiac surgery.
Crit Care Med. 1988; 16:238-40.
(e.g., agitation, irritability, dystonic safety and efficacy for analgesia and 12. Arnold JH, Troug RD, Orav EJ et al. Toler-
movements, centrally mediated re- sedation. Data on use of dexmedeto- ance and dependence in neonatal seda-
bound hypertension) appear to be midine specifically for the prevention tion with fentanyl during extracorporeal
membrane oxygenation. Anesthesiology.
CNS related, with no hemodynamic and treatment of opioid and ben- 1990; 73:1136-40.
manifestations.30,31 zodiazepine withdrawal are limited, 13. Cunliffe M, McArthur L, Dooley F. Man-
indicating the need for additional aging sedation withdrawal in children
Discussion who undergo prolonged PICU admis-
well-designed studies exploring its sion after discharge to the ward. Paediatr
Dexmedetomidine is an a 2 - use for pediatric narcotic withdrawal. Anaesth. 2004; 14:293-8.
agonist whose use in the PICU has 14. Franck LS, Naughton I, Winter I. Opioid
Conclusion and benzodiazepine withdrawal symp-
increased in the last few years as an toms in paediatric intensive care patients.
adjunct to sedation and analgesia. A limited body of published evi- Intensive Crit Care Nurse. 2004; 20:344-
The use and typical dosages of dex- dence from retrospective studies and 51.
15. Agathe AG, Kim GR, Mathias KB et al.
medetomidine vary, primarily due to case reports suggests a potential role Clonidine as an adjunct therapy to opi-
concern about potential hypotension for dexmedetomidine as an adjunct oids for neonatal abstinence syndrome:
and bradycardia, which have been therapy to provide sedation and an- a randomized, controlled trial. Pediatrics.
2009; 123:e849-56.
reported in the published literature algesia to reduce narcotic withdrawal 16. Finkel JC, Johnson YJ, Quezado ZM. The
in association with the use of bolus symptoms in pediatric patients. use of dexmedetomidine to facilitate
doses. When bolus doses are used, a acute discontinuation of opioids after
References cardiac transplantation in children. Crit
typical loading dose is 0.5–1 mg/kg 1. Finnegan L, Connaughton J, Kron R et al. Care Med. 2005; 33:2110-2.
given intravenously over 10 minutes; Neonatal abstinence syndrome: assess- 17. Bejian S, Valasek C, Nigro JJ et al. Pro-
bolus doses are followed by a con- ment and management. Addict Dis. 1975; longed use of dexmedetomidine in the
2:141-58. paediatric cardiothoracic intensive care
tinuous infusion of 0.1–1.4 mg/kg/hr. 2. Tobias JD. Tolerance, withdrawal, and unit. Cardiol Young. 2009; 19:98-104.
Dexmedetomidine has the ben- physical dependency after long-term 18. Carroll CL, Krieger D, Campbell M et al.
efits of being an effective adjunct sedation and analgesia of children in the Use of dexmedetomidine for sedation of
pediatric intensive care unit. Crit Care children hospitalized in the intensive care
therapy for sedation and analgesia Med. 2000; 28:2122-32. unit. J Hosp Med. 2008; 3:142-7.
without producing the respira- 3. Ista E, van Dijk M, Gamel C et al. With- 19. Chrysostomou C, Flippo SD, Manrique
tory depression seen with most other drawal symptoms in children after long- AM et al. Use of dexmedetomidine in
term administration of sedative and/or children after cardiac and thoracic sur-
sedatives and analgesics. In addition, analgesics: a literature review. Intensive gery. Pediatr Crit Care Med. 2006; 7:126-
when used as an adjunct, dexme- Care Med. 2007; 33:1396-406. 31.
detomidine allows for decreased 4. Gertler R, Brown HC, Mitchell DH et 20. Berkenbosch JW, Wankum PC, Tobias JD.
al. Dexmedetomidine: a novel sedative- Prospective evaluation of dexmedetomi-
fentanyl and midazolam require- analgesic agent. Proc (Bayl Univ Med dine for noninvasive procedural sedation
ments. Common adverse effects of Cent). 2001; 14:13-21. in children. Pediatr Crit Care Med. 2005;
dexmedetomidine use are hypoten- 5. Lane JC, Tennison MB, Lawless ST et 6:435-9.
al. Movement disorder after withdrawal 21. Finkel JC, Quezado ZM. Hypothermia-
sion and bradycardia; these effects of fentanyl infusion. J Pediatr. 1991; induced bradycardia in a neonate receiv-
are thought to be related to the use of 119:649-51. ing dexmedetomidine. J Clin Anesth.
bolus doses, high cumulative doses, 6. Bergman I, Steeves M, Burkart G et al. 2007; 19:290-2.
Reversible neurologic abnormalities asso- 22. Baddigam K, Russo P, Russo J et al.
and longer duration of therapy. The ciated with prolonged iv midazolam and Dexmedetomidine in the treatment of
majority of published reports about fentanyl administration. J Pediatr. 1991; withdrawal syndromes in cardiothoracic
the use of dexmedetomidine in pedi- 119:644-9. surgery patients. J Intensive Care Med.
7. Zapantis A, Leung S. Tolerance and with- 2005; 20:118-23.
atric patients only describe its use for drawal issues with sedation. Crit Care 23. Tobias JD. Subcutaneous dexmedetomi-
analgesia and sedation. Nurs Clin North Am. 2005; 17:211-23. dine infusions to treat or prevent drug
Am J Health-Syst Pharm—Vol 68 Jul 1, 2011 1237
clinical consultation Dexmedetomidine
withdrawal in infants and children. J sion following dilution, package insert. drome following cessation of antihy-
Opioid Manag. 2008; 4:187-91. Lake Forest, IL: Hospira, Inc.; 2010 Sep. pertensive drug therapy. Int J Clin Pract.
24. Tobias JD. Dexmedetomidine to treat 27. Bhana N, Goa KL, McClellan KJ. Dexme- 2005; 59:562-70.
opioid withdrawal in infants following detomidine. Drugs. 2000; 59:263-8. 30. Miller JL, Allen C, Johnson PN. Neuro-
prolonged sedation in the pediatric ICU. 28. Honey BL, Harrison DL, Gormley AK et logic withdrawal symptoms following
J Opioid Manag. 2006; 2:201-5. al. Evaluation of adverse events noted in abrupt discontinuation of a prolonged
25. Finkel JC, Elrefai A. The use of dexme- children receiving continuous infusions dexmedetomidine infusion in a child. J
detomidine to facilitate opioid and ben- of dexmedetomidine in the intensive Pediatr Pharmacol Ther. 2010; 15:38-42.
zodiazepine detoxification of an infant. care unit. J Pediatr Pharmacol Ther. 2010; 31. Tobias JD. Dexmedetomidine: are there
Anesth Analg. 2004; 98:1658-9. 15:30-7. going to be issues with prolonged admin-
26. Precedex (dexmedetomidine hydrochlo- 29. Karachalios GN, Charalabopoulos A, istration? J Pediatr Pharmacol Ther. 2010;
ride) for injection, for intravenous infu- Papalimnou V et al. Withdrawal syn- 15:4-9.
1238 Am J Health-Syst Pharm—Vol 68 Jul 1, 2011
You might also like
- DNB Question Paper-System wise-DNB AnaesthesiaDocument88 pagesDNB Question Paper-System wise-DNB AnaesthesiaSirisha Ckv83% (18)
- When To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsDocument9 pagesWhen To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsepraetorianNo ratings yet
- CCJC BodinDocument2 pagesCCJC Bodinapi-495663503No ratings yet
- Analysis of 67 CasesDocument8 pagesAnalysis of 67 CasesHitesh ChandwaniNo ratings yet
- Antipsychotic PolypharmacyDocument10 pagesAntipsychotic PolypharmacymarcoNo ratings yet
- Pediatric Premedication: A Double-Blind Randomized Trial of Dexmedetomidine or Ketamine Alone Versus A Combination of Dexmedetomidine and KetamineDocument7 pagesPediatric Premedication: A Double-Blind Randomized Trial of Dexmedetomidine or Ketamine Alone Versus A Combination of Dexmedetomidine and KetamineFatty MaulidiraNo ratings yet
- En A09v83n2s0 PDFDocument12 pagesEn A09v83n2s0 PDFRiriNo ratings yet
- Ketamine As Rescue Treatment FDocument8 pagesKetamine As Rescue Treatment Fandrew herringNo ratings yet
- ACEP Ketamine Guideline 2011Document13 pagesACEP Ketamine Guideline 2011Daniel Crook100% (1)
- MeduriDocument4 pagesMeduriSilvia Leticia BrunoNo ratings yet
- Withdrawal Syndrome in The Pediatric Intensive Care Unit. Incidence and Risk FactorsDocument8 pagesWithdrawal Syndrome in The Pediatric Intensive Care Unit. Incidence and Risk Factorsfuka priesleyNo ratings yet
- ChayapathiDocument8 pagesChayapathiVINICIUS CAMARGO KISSNo ratings yet
- Clozapine: SchizophrenicDocument8 pagesClozapine: SchizophrenicVictoria FellowsNo ratings yet
- PCCM Suppl Mar 2016Document13 pagesPCCM Suppl Mar 2016Xavier AbrilNo ratings yet
- Kane1988 PDFDocument8 pagesKane1988 PDFRavi KumarNo ratings yet
- A Selective Summary of Psychopharmacology Research Published in First Half of 2017Document3 pagesA Selective Summary of Psychopharmacology Research Published in First Half of 2017gion.nandNo ratings yet
- Mahatme M S Et. Al., 2018Document6 pagesMahatme M S Et. Al., 2018kaniNo ratings yet
- New Drugs: Self-Test QuestionsDocument3 pagesNew Drugs: Self-Test QuestionscNo ratings yet
- Ann EmergDocument8 pagesAnn EmergDyan TonyNo ratings yet
- Pharmacological Sedation Management in Paediatric Intensive Care UnitDocument16 pagesPharmacological Sedation Management in Paediatric Intensive Care Unitfuka priesleyNo ratings yet
- RSI Post IntubationDocument8 pagesRSI Post IntubationshinjiNo ratings yet
- Ijpd 22 303Document6 pagesIjpd 22 303bellaNo ratings yet
- Chudnofsky 2000Document8 pagesChudnofsky 2000Sanjeewa de AlwisNo ratings yet
- E423 FullDocument11 pagesE423 FullCecepNo ratings yet
- Jurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresDocument15 pagesJurnal Efficacy and Tolerability of Adjunctive Lacosamide in Pediatric Patients With Focal SeizuresAnida HasnaNo ratings yet
- Phase 1 A Randomized Double Blind Placebo Controlled Study of The Safety Tolerability Pharmacokinetics and Pharmacodynamics of LB 102 July 2022 Springer NatureDocument10 pagesPhase 1 A Randomized Double Blind Placebo Controlled Study of The Safety Tolerability Pharmacokinetics and Pharmacodynamics of LB 102 July 2022 Springer Naturecm911No ratings yet
- Epilepsia - 2018 - Maglalang - Rescue Therapies For Seizure Emergencies New Modes of AdministrationDocument9 pagesEpilepsia - 2018 - Maglalang - Rescue Therapies For Seizure Emergencies New Modes of AdministrationKikie Rizky HeningNo ratings yet
- MRX Clinical Alert-August 2018Document6 pagesMRX Clinical Alert-August 2018Nattawat TeerawattanapongNo ratings yet
- Analgesicos y Sedativos en UCI - BZD Propofol y OpioidesDocument19 pagesAnalgesicos y Sedativos en UCI - BZD Propofol y OpioidesManuel MontellanosNo ratings yet
- Refractory Epi ManagementDocument4 pagesRefractory Epi Managementjonniwal sanusiNo ratings yet
- 2020 Troy CefaleasManejo RTDocument6 pages2020 Troy CefaleasManejo RTJULIO CESAR CASTRO MURILLONo ratings yet
- Marketed New Drug Delivery Systems For Opioid Agonists/Antagonists Administration: A Rapid OverviewDocument8 pagesMarketed New Drug Delivery Systems For Opioid Agonists/Antagonists Administration: A Rapid OverviewFaradila Putri SoegiyonoNo ratings yet
- Schizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapyDocument13 pagesSchizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapydilaNo ratings yet
- Therapeutic Use of Medicinal Cannabis in Dif Ficult To Manage EpilepsyDocument3 pagesTherapeutic Use of Medicinal Cannabis in Dif Ficult To Manage EpilepsyEnrique Molina LeonNo ratings yet
- Abaya 2018Document6 pagesAbaya 2018Muhammad Imam NoorNo ratings yet
- Efek SedasiDocument5 pagesEfek Sedasidheva akilNo ratings yet
- Daughton - 2009 - Review of ADHD PharmacotherapiesDocument9 pagesDaughton - 2009 - Review of ADHD PharmacotherapiesRene LutherNo ratings yet
- Safety Update: Dverse Drug ReactionDocument6 pagesSafety Update: Dverse Drug ReactionWilliam ChandraNo ratings yet
- 2006-Long-Term Use of Oxcarbazepine Oral Suspension in Childhood Epilepsy - Open-Label Study PDFDocument6 pages2006-Long-Term Use of Oxcarbazepine Oral Suspension in Childhood Epilepsy - Open-Label Study PDFAnonymous bEwTSXJ1gNo ratings yet
- Mann, Mackay, Et Al.Document9 pagesMann, Mackay, Et Al.Paulina AlonsoNo ratings yet
- HCN 153Document9 pagesHCN 153Suck my dickNo ratings yet
- Modafinil and Armodafinil in Schizophrenia: Chittaranjan Andrade, MDDocument3 pagesModafinil and Armodafinil in Schizophrenia: Chittaranjan Andrade, MDbenedicte lewinNo ratings yet
- Dopamine Vs EpinephrineDocument11 pagesDopamine Vs EpinephrineAyiek WicaksonoNo ratings yet
- 105.basic Clin Pharma Tox - 2015 - Penninga - Adverse Events Associated With Flumazenil Treatment For The Management ofDocument8 pages105.basic Clin Pharma Tox - 2015 - Penninga - Adverse Events Associated With Flumazenil Treatment For The Management oftereNo ratings yet
- Wjem 13 01 26 PDFDocument9 pagesWjem 13 01 26 PDFMoises Vega RodriguezNo ratings yet
- Famacologia Da Epilepsia e Estado de Mal EpilepticoDocument15 pagesFamacologia Da Epilepsia e Estado de Mal Epilepticorafael rocha novaesNo ratings yet
- Disinhibition of Behaviors With Midazolam:: Report of A CaseDocument5 pagesDisinhibition of Behaviors With Midazolam:: Report of A CaserajtanniruNo ratings yet
- Pi Is 0149291820302836Document15 pagesPi Is 0149291820302836John SMithNo ratings yet
- Geriatric Pharmacotherapy PDFDocument6 pagesGeriatric Pharmacotherapy PDFverry aswardsNo ratings yet
- Antiepileptic Drugs-Best Practice Guidelines ForDocument38 pagesAntiepileptic Drugs-Best Practice Guidelines ForAbraham Escobedo MoratillaNo ratings yet
- KETODEXDocument5 pagesKETODEXBarbarita Alvarado CamposNo ratings yet
- AAP Emergencies Ped Drug Doses PDFDocument20 pagesAAP Emergencies Ped Drug Doses PDFUlvionaNo ratings yet
- Clonidine WeanDocument10 pagesClonidine WeanJorge HinojosaNo ratings yet
- STart StroppDocument1 pageSTart StroppHoang Mai NguyenNo ratings yet
- Antiemetic Drug Use in Children What The.3Document6 pagesAntiemetic Drug Use in Children What The.3Zafitri AsrulNo ratings yet
- Opioid and Benzodiazepine Weaning in Pediatric PatientsDocument25 pagesOpioid and Benzodiazepine Weaning in Pediatric PatientsMaverick 18No ratings yet
- Dex Review 2007Document11 pagesDex Review 2007Jackelyne VilelaNo ratings yet
- Methylprednisolone in West SyndromeDocument5 pagesMethylprednisolone in West SyndromeBandya SahooNo ratings yet
- Chapter 12Document59 pagesChapter 12Alif riadiNo ratings yet
- CPT 1435 PDFDocument17 pagesCPT 1435 PDFarramithaNo ratings yet
- Review of The Newer Antiepileptic Drugs PDFDocument28 pagesReview of The Newer Antiepileptic Drugs PDFnickyNo ratings yet
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Delirium in The Intensive Care Unit Is Dexmedetomidine EffectiveDocument15 pagesDelirium in The Intensive Care Unit Is Dexmedetomidine EffectiveArgenis SalinasNo ratings yet
- MCPHS Drug Information QuestionDocument5 pagesMCPHS Drug Information QuestionG TeenaNo ratings yet
- Duncan Et Al-2018-Cochrane Database of Systematic ReviewsDocument150 pagesDuncan Et Al-2018-Cochrane Database of Systematic Reviewsluis.fe.gd84No ratings yet
- Journal Homepage: - : Manuscript HistoryDocument7 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- 2348 0548.190064 1Document8 pages2348 0548.190064 1Ankita MohtaNo ratings yet
- Manage Delirium in Critically Ill Patients Through Prevention, Early Diagnosis and Treatment PDFDocument6 pagesManage Delirium in Critically Ill Patients Through Prevention, Early Diagnosis and Treatment PDFPablo RamirezNo ratings yet
- Key Points: Balanced Anesthesia in Small Animal Patients: Incorporating Cri'SDocument2 pagesKey Points: Balanced Anesthesia in Small Animal Patients: Incorporating Cri'SAlejandro Estrada RiosNo ratings yet
- Picco Monitoring During Liver Transplantation For.701Document1 pagePicco Monitoring During Liver Transplantation For.701Chang TruNo ratings yet
- Textbook of Pediatric Dentistry-3rd EditionDocument18 pagesTextbook of Pediatric Dentistry-3rd EditionAnna NgNo ratings yet
- Comparison of Dexmedetomidine, Pethidine and Tramadol in The Treatment of Post-Neuraxial Anaesthesia ShiveringDocument6 pagesComparison of Dexmedetomidine, Pethidine and Tramadol in The Treatment of Post-Neuraxial Anaesthesia ShiveringabdulNo ratings yet
- Smith - S Anesthesia For Infants and Children (Eighth Edition) 2011-384-391Document8 pagesSmith - S Anesthesia For Infants and Children (Eighth Edition) 2011-384-391Alexiel BathoryNo ratings yet
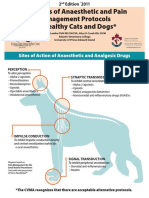
- Examples of Anaesthetic and Pain Management Protocols For Healthy Cats and DogsDocument3 pagesExamples of Anaesthetic and Pain Management Protocols For Healthy Cats and DogsEka FirmanNo ratings yet
- Dexmedetomidine: Pediatric Drug InformationDocument15 pagesDexmedetomidine: Pediatric Drug InformationАлексей НиколаевNo ratings yet
- Anestesia - Cardiovascular - Luna OrtizDocument11 pagesAnestesia - Cardiovascular - Luna OrtizWeimar Andres Bonilla MosqueraNo ratings yet
- Post-Operative Pain: Mechanisms and ManagementDocument6 pagesPost-Operative Pain: Mechanisms and ManagementDevana MaelissaNo ratings yet
- Management of Sedation and Delirium in Ventilated ICU PatientsDocument35 pagesManagement of Sedation and Delirium in Ventilated ICU PatientsJheng-Dao YangNo ratings yet
- General Management in ICUDocument8 pagesGeneral Management in ICUNurzawani Shamsudin67% (3)
- General Topics: Anesthesia, Analgesia, and Sedation of Small MammalsDocument23 pagesGeneral Topics: Anesthesia, Analgesia, and Sedation of Small Mammalsdoja catNo ratings yet
- Awake Intubation: David Leslie BSC (Hons) MBBCH (Hons) Frca Mark Stacey MB Mchir Frca Ilthe MSC (Med Ed)Document4 pagesAwake Intubation: David Leslie BSC (Hons) MBBCH (Hons) Frca Mark Stacey MB Mchir Frca Ilthe MSC (Med Ed)Fadilah SorayaNo ratings yet
- Anesthesia For Craniotomy - UpToDateDocument47 pagesAnesthesia For Craniotomy - UpToDateAna Belén Artero CastañoNo ratings yet
- Anesthetic Considerations For Geriatric DogsDocument3 pagesAnesthetic Considerations For Geriatric DogsFernanda PérezNo ratings yet
- Stanford Anesthesia - CA1 Tutorial Book PDFDocument63 pagesStanford Anesthesia - CA1 Tutorial Book PDFKhamini Dilly Kannan100% (1)
- Anesthesia and Analgesia Book 2Document186 pagesAnesthesia and Analgesia Book 2Diana NiculaeNo ratings yet
- TivaDocument38 pagesTivasunny kumar100% (1)
- SA Anesthesia Drug Dosages 2022Document3 pagesSA Anesthesia Drug Dosages 2022KRLITHIU Borja100% (1)
- ISAPS News Letter 2018Document52 pagesISAPS News Letter 2018Man Koon Suh, M.D.No ratings yet
- Out of Operating Room Anesthesia - A Comprehensive Review-Springer International Publishing (2017)Document467 pagesOut of Operating Room Anesthesia - A Comprehensive Review-Springer International Publishing (2017)Tahseen Talib100% (1)
- Drug Literature Assignment FINALDocument6 pagesDrug Literature Assignment FINALToqa ElmansouryNo ratings yet