Professional Documents
Culture Documents
PJP Volume 4 Issue 2
PJP Volume 4 Issue 2
Uploaded by
Sedric FactorOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PJP Volume 4 Issue 2
PJP Volume 4 Issue 2
Uploaded by
Sedric FactorCopyright:
Available Formats
The PHILIPPINE JOURNAL of
PSYCHIATRY
Official Journal of the Philippine Psychiatric Association
NEW REQUIREMENTS FOR
PSYCHIATRY RESIDENCY
TRAINING PROGRAMS
(PRTPs) IN THE PHILIPPINES
VILLANUEVA, RUTH T., LOPEZ- ROCES, MYRA DEE,
DELLA, CONSTANTINE D.,
GATLABAYAN-CLETO, JANNEL, & GOZO-OLIVER,
GEORGINA M.
SUPPORTING MEDICAL
EDUCATORS TO ENSURE
WELLNESS OF MEDICAL
STUDENTS
DELLA, CONSTANTINE D.
PRACTICE AND PERCEPTIONS OF
PEDIATRIC RESIDENTS IN A
TERTIARY GOVERNMENT
HOSPITAL ON MENTAL
HEALTHCARE AS PART OF
GENERAL PRACTICE
YU-CHUA, CONSTANTINE L. & ELMA, LORELEI MELANIE K
Jewelyn Ann Carpio, MD A CROSS-SECTIONAL STUDY ON
Glessa Francesa Garibay, MD THE PREVALENCE AND SEVERITY
OF SUICIDAL IDEATIONS AND
VOLUME 4 (2) BEHAVIORS OF SENIOR HIGH
ISSN 2980-4884 SCHOOL STUDENTS USING THE
JULY-DECEMBER 2023 COLUMBIA-SUICIDE SEVERITY
RATING SCALE (C-SSRS)
REYES, JOHN MICHAEL L.
EXAMINATION OF THE RIGHT
TO CONFIDENTIALITY
OSORIO-GRAPILON, NINA KRISTY A.
PHILIPPINE PSYCHIATRIC
PHILIPPINE JOURNAL OF PSYCHIATRY
ASSOCIATION
BOARD OF OFFICERS 2023 EDITORIAL BOARD 2023
Georgina Gozo- Oliver, MD, DPBP, FPPA (Life), FPSCAP
ROBERT D. BUENAVENTURA, MD, FPPA (LIFE) Editor - in – Chief
PRESIDENT
Anthony T. Abala, MD, DSBPP
ARNOLD ANGELO M. PINEDA, MD, FPPA, FPNA Hecil Cruz, MD, DSBPP
VICE PRESIDENT Anna Josefina Vazquez-Genuino, MD, MPH, DPBP, FPPA (Life),
FPSCAP
JOAN MAE G. PEREZ-RIFARAEL, MD, FPPA Manuscript Editors
SECRETARY
Nina Kristy A. Osorio-Grapilon, MD, DSBPP
Business Manager
HANNAH MARTELLA M. PAJARILLO, MD, FPPA
TREASURER
Norieta Calma- Balderrama MD, DPBP, FPPA (Life), FPSCAP
Alma Lucindo Jimenez, MD, FPPA (Life)
ANNA LIZZA Y. SALAZAR-MAÑALAC, Christi Annah V. Hipona, MD, DSBPP
MD,FPNA,FPPA,FPSCAP Sedric John V. Factor, MD
PUBLIC RELATIONS OFFICER Associate Editors
MARIA BERNADETTE MANALO-ARCENA, MD, FPPA
EVANGELINE BASCARA DELA FUENTE, MD, MHA, MHPED, FPPA
DOLORES Y. ORTEGA-LARGO, MD FPPA IMELDA BATAR, MD, DPBP, FPPA (LIFE)
AUDITOR TOMAS D. BAUTISTA, MD, MSC
MA. RUTH BORDADO, MD, DPBP, FPPA
MARY DARYL JOYCE LINDO-CALLEJA, MD, FPPA, FPSCAP
ROBERT GERARD O. KELEMEN, MD, FPPA ROBERT B. CAPISTRANO, MD, FPPA
CARLO PAOLO S. CASTRO, MD, DPBP
DIRECTOR FOR LUZON AIMEE G. CHUA, MD, DPBP
VIVIENNE CLEOFAS, MD, FPPA
CORAZON ANGELA M. CUADRO, MD, FPPA
JOY R. ADOLFO- BUENO, MD, FPPA VICTORIA PATRICIA C. DELA LLANA, MD, FPPA
CRISTINA DIAZ, MD, DSBPP
DIRECTOR FOR VISAYAS PROFESSOR ROMEO YU ENRIQUEZ, MD, FPNA, FPPA (LIFE)
EVELYN G. GAPUZ, MD, EMBA, FPPA, FPSCAP
MA. JOCELYN GUAZON-GAYARES, MD, FPPA (LIFE), FPSCAP
JOSE L. CORUÑA, JR., MD, FPPA MARIANO S. HEMBRA, MD, FPPA, MMIP, CESE
DIRECTOR FOR MINDANAO MARIA CYNTHIA R. LEYNES, MD, MSC, FPPA, FPSCAP
MA. LOURDES CORRALES-JOSON, MD, FPPA, FPNA
MELISSA PAULITA V. MARIANO, M.D., MSC, FPPA
ANTONIO C. SISON, MD, FPPA (LIFE), FPDS AIDA MUNCADA, MD, MHA, FPPA, FPSCAP
DINAH PALMERA P. NADERA, MD, MSC., MIMH, FPPA
IMMEDIATE PAST PRESIDENT ENCARNITA RAYA-AMPIL, MD, FPNA, FPPA
SPES REYES, MD, DPBP
PIA NATALYA T. REYES-SIA, MD, FPPA
HON. JUDGE ROSALINA L. PISON (RET.) JOAN MAE PEREZ- RIFAREAL, MD, FPPA
ELEANOR LACUNA-RONQUILLO, MD, FPPA
LEGAL ADVISOR GERARDINE JOSEFINA SAYO, MD
AIZAH JOYCE LEI T. TANA, MD, FPPA
TERESA G. VILLASOR, MD
SALVADOR BENJAMIN D VISTA, MD, FPPA(LIFE), FPCPSYCH, FPCAM
BOARD OF REVIEWERS
All communications should be directed to the Editor-in-
THE PHILIPPINE JOURNAL OF PSYCHIATRY is published twice a year Chief, Philippine Journal of Psychiatry, Philippine
by the Philippine Psychiatric Association. All articles published Psychiatric Association Office, Suite 1011 Medical Plaza,
Ortigas Condominium, #25 San Miguel Avenue, Ortigas,
represent the opinions of the authors and do not reflect the official
Center, Pasig City, Philippines or through email at
policy of the Philippine Psychiatric Association unless this is clearly philpsych.org@gmail.com.
specified. The publisher cannot accept the correctness or accuracy of
the advertiser’s text and/or claims or opinions expressed. The Telephone/Fax: +63(2)635-9858
appearance of the advertisements in this journal does not necessarily Cellphone: (0917) 803 1198
constitute an approval or endorsement by the Philippine Psychiatric
Association of the product or service advertised. Advertisements are
Copyright: 2023 by the Philippine Psychiatric
accepted through the Managing Editor and are subject to approval by
Association, Inc.
the Editorial Board. The contents of this publication are not to be
quoted in the press or reprinted for general distribution for
advertising and promotional purposes, nor for creating new collective
works or for resale, without permission of the Editor-in-chief & Cover:
Editorial Board. War Within the Self by Jewelyn Ann Carpio, MD &
Glessa Francesa Garibay, MD with permission from the
artist
2023 · VOLUME 4 (2-1)
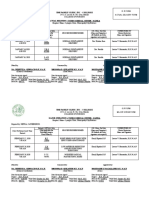
PJP TABLE OF CONTENTS
SPECIAL ARTICLES PAGE
New Requirements for Psychiatry Residency Training Programs (PRTPs)
in the Philippines
1
Villanueva, Ruth T., Lopez- Roces, Myra Dee, Della, Constantine D.,
Gatlabayan-Cleto, Jannel, & Gozo-Oliver, Georgina M.
Supporting Medical Educators to Ensure Wellness of Medical Students
Della, Constantine D.
16
ORIGINAL RESEARCH
Practice and Perceptions of Pediatric Residents in a Tertiary Government 21
Hospital on Mental Healthcare as Part of General Practice
Yu-Chua, Constantine L. & Elma, Lorelei Melanie K
A Cross-Sectional Study on the Prevalence and Severity of Suicidal ideations
and Behaviors of Senior High School Students using the Columbia-Suicide 33
Severity Rating Scale (C-SSRS)
Reyes, John Michael L.
CASE REPORT
Examination of the Right to Confidentiality
Osorio-Grapilon, Nina Kristy A.
42
ABSTRACTS
Major Depressive Disorder Among Patients Receiving Antiretroviral Treatment 51
in a Social Hygiene Clinic: Prevalence, Associated Factors and Effects on Quality
of Life
Bumatay, Leonides Jr., E., Paccial, Rodelen, Cruzada, Joeffrey & Sevilleja, Emmanuela
Determining the Prevalence of Depressive and Anxiety Synptoms Among
Seleced Pregnant Patients in Some Parts of Luzon During the COVID-19
52
Pandemic: A Cross-Sectional Study
Paggadu, Marie Cresanne R.
Resilience Levels Among Filipino Non-Medical Personnel at a Tertiary 53
Government Hospital in Metro Manial during the COVID-19 Pandemic - July
2021
Legaspi, Rafael E. & Della, Constantine D.
Comorbid Sleep Disorders among Patients Presenting with Insomnia Who 54
Underwent Polysomnography
Hernandez, April Fatima & Dela Eva, Roland
INFORMATION FOR CONTRIBUTORS 55
PJP SPECIAL ARTICLE
NEW REQUIREMENTS FOR PSYCHIATRY RESIDENCY
TRAINING PROGRAMS (PRTPs) IN THE PHILIPPINES
THE BOARD OF ACCREDITATION OF THE SPECIALTY
BOARD OF PHILIPPINE PSYCHIATRY
Villanueva, Ruth T., Lopez- Roces, Myra Dee, Della, Constantine D.,
Gatlabayan-Cleto, Jannel, & Gozo-Oliver, Georgina M.
INTRODUCTION Filipinos take pride in the fact that religion and
spirituality occupy a focal point in their mental
It has been more than a decade since the Com- health. Yet, the relevance of religion and
mittee on Standardization and Accreditation of spirituality to mental health and psychiatric care
Residency Training was renamed Board of is barely tackled by residency training programs
Accreditation of the Specialty Board of in the country. In this light, the Board of
Philippine Psychiatry (SBPP). The SBPP is Accreditation recognizes the need for psychiatry
composed of two bodies namely the Boards of residents to apply the principles of gender
Accreditation and Certification. These bodies are sensitivity and religion and spirituality to the
mandated to uphold the highest standards of care of patients with mental health and
accrediting psychiatry residency training psychiatric problems. In the same vein,
programs (Board of Accreditation) and granting improving the quality of mental health and
diplomate status to graduates of these programs psychiatric care by residents must be given
(Board of Certification). Guided by the paramount attention by all training programs.
biopsychosocial and spiritual model of health, The Board of Accreditation strongly believes
the Board of Accreditation remains steadfast in that promoting the wellness of psychiatry
ensuring that psychiatry residency training trainees and arming them with the necessary
programs continue to be relevant to current tools to succeed in their careers are effective
demands of mental health and psychiatric care and efficient ways to ensure that they are able
in the country. In addition, it sees to it that these to provide the highest quality of mental health
programs are in harmony with global standards. and psychiatric care for their patients.
As psychiatry faces new challenges in the third
millennium, certain innovations and iterations in Upon the approval of the Board of Directors of
the manner by which mental illnesses are the Philippine Psychiatric Association, the Board
diagnosed, treated, and prevented must be set of Accreditation now requires the inclusion of
in place. Through its Millennium Developmental the following in the psychiatry residency training
Goals, the United Nations has declared that the programs of all accredited institutions.
achievement of gender equality is an effective
way of combating disease. Mental health 1. Wellness program for residents
problems and psychiatric disorders are closely 2. Mentoring program for residents
linked with gender-related issues. Yet, many 3. Course on gender and psychiatry
residency training programs in the Philippines 4. Course on religion and spirituality and
have not formally and systematically integrated psychiatry
gender sensitivity into their curricula. The same
can be said of the concepts of religion and In the spirit of learning outcomes/competency-
spirituality. Numerous researches have estab- based/outcome-based education and in consi-
lished the positive link between religion and deration of the particular contexts and missions
spirituality and mental health. of PRTPs, the Board provides flexibility for the
1 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
coordinators of PRTPs to innovate their cur- The COVID-19 pandemic highlighted the
riculum on the courses on gender and psy- complex challenges faced by residents.
chiatry and religion and spirituality and psy- Mendonça and colleagues found that the
chiatry. The same flexibility applies to the COVID-19 pandemic contributed to symptoms
development and implementation of the of depression, anxiety, and burnout in majority
wellness and mentoring programs. The PRTPs of medical residents. (4) This pandemic may bear
must design their curricula and programs to suit a long-lasting impact on residents who may need
their own contexts and missions but these must psychological support for a wide range of
achieve the required minimum set of outcomes. personal and professional concerns. (5)
In addition, PRTPs have freedom in curriculum
delivery and in specification and deployment of It has been proposed that medical education
human and physical resources. The PRTPs must may select for individuals who are prone to
show that the alternative route they propose psychological distress because of their high
effectively fulfills the program outcomes and levels of ambition and competition. (6) Medical
satisfies program educational objectives. The students bring these stress-inducing qualities
program outcomes that the Board prescribes are with them to residency making them vulnerable
described in Table 1. to burnout because of disappointment and
frustration. In addition, residents may adopt
maladaptive perfectionism or develop imposter
syndrome. Maladaptive perfectionism involves
unreasonable self-expectation, negative reac-
tions to failure, and constant dissatisfaction with
one’s performance. Maladaptive perfectionism
hinders trainees from being aware of their
vulnerabilities and limitations. Imposter syn-
drome is characterized by lack of self-
confidence and fear of being discovered as un-
derserving despite one’s achievements. Mal-
adaptive perfectionism and imposter syndrome
predispose to psychological distress or patho-
logy. Closely linked with perfectionism and the
imposter syndrome is shame. Shame may arise
from internal and external factors and it may
lead to isolation, distress, or disruption in self-
esteem and self-identity. Intrinsic qualities of
residents such as the lack of resiliency may not
be the sole drivers of diminished well-being.
Studies show that multiple factors associated
with the training environment contribute to lack
or absence of wellness. Experts believe that
systemic factors such as organizational
This paper provides conceptual frameworks on
pressures and work stressors and not personal
the courses on gender and psychiatry and
resilience contribute to burnout among
religion and spirituality and psychiatry and the
healthcare professionals. (7)
programs on wellness and mentoring. The
general and specific objectives for establishing
Although self-directed strategies such as
these courses and programs are described.
mindfulness practice help reduce stress, anxiety,
Furthermore, it also discusses current evidence
and burnout, systemic factors that lead to such
on the relevance of these courses and programs
consequences must also be addressed.
in psychiatry residency training.
Providing interventions geared towards equip-
ping administration and the trainers with the
I. Wellness Program
capacity to optimize their roles as educators and
Residency training is a formative and intense
role models for residents is an example. This
period that has its own set of challenges that
strategy will facilitate a top-down approach
affect the well-being of trainees. (2, 3)
aimed at increasing resident wellness. (6)
2 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Alkatan pointed out the phenomenon of -chiatry residents and showed that burnout was
“generational gap” that training faculty need to not evident. The number of participants of this
appreciate in order to ensure the success of a study, however, was too small (N=18) to be able
wellness program. (8) The current set of trainers to generate substantial conclusions. (15)
belong to the baby boomer and X generations
while the current trainees belong to the As residency training progresses the risk of
millennial or Y generation. The latter is burnout increases as exhaustion, sleep
characterized by being confident, team- deprivation, adjustment difficulties, inter-
oriented, achievement-oriented, pressured, and personal conflicts, demanding workload, disen-
conventional. In dealing with this generational chantment, detachment, and cynicism increase.
difference, trainers are urged to be guided by Burnout may contribute to the spectrum of
certain strategies some of which are described stress conditions and/or clinical health issues of
in Table 2. trainees such as suicide, depression, and
substance use. Burnout has also been
associated with physician attrition and poor
quality of patient care. On the contrary,
physician wellness has been linked with
increased patient satisfaction and improved
treatment adherence. (3, 16) Traditionally, the
Maslach Burnout Inventory is used to diagnose
burnout. This scale assesses emotional
exhaustion (feeling overworked and losing com-
passion), depersonalization (detachment from
colleagues and/or patients), and personal
accomplishment (feelings of competence and
professional satisfaction). (6) Other scales for
burnout include the Copenhagen Burnout
Inventory and Symptom Checklist 90 (SCL 90).
The Philippine government has recognized the Studying the factors that contribute to burnout
value of wellness programs thus the Department is crucial in understanding the factors that
of Health in cooperation with the World Health ensure patient safety and influence the career
Organization and the Australian government, trajectory of residents. (6) It was hypothesized
launched The Wellness Movement on 16 January that burnout resulted from excessive duty
2023. This is an initiative that aims to improve hours. Studies in the US, Canada, and Europe,
the mental health and well-being of Filipino however, did not show that shortening duty
healthcare workers. (9, 10) hours improved sleep, work efficiency, or
depression. In fact, this strategy potentially
Literature shows that burnout is prevalent lessened the time for residents to learn and
among residents across all specialties. (11, 12, compromised patient care. (3) Lu & Ratnapalan
13) In fact, it is believed to be a growing endemic conducted a scoping review of resident burnout
with at least 60% of residents reporting it. (7). interventions and found that longitudinal
Locally, one study showed an average to wellness training, physical activities, healthy
moderate degree of burnout among residents of dietary habits, social activities, formal mentor-
a private tertiary hospital in Metro Manila with ship programs, and health checkups were
single females and those belonging to major or effective in reducing burnout. (17)
non-surgical departments having higher burnout
levels. (13) Another study conducted post- Psychiatry residency training adds another layer
COVID pandemic, showed that a significant of burden that may aggravate stress or lead to
number of Internal Medicine residents at a burnout. These include vicarious traumatization,
government tertiary hospital were at risk for patient suicide and violence, and stigma of the
burnout. (14) There is a dearth of research on profession. International studies showed that
stress or burnout among Filipino psychiatry 31% to 69% of residents experience patient
residents. A study conducted at a government death by suicide. This results in significant
tertiary psychiatric facility in Metro Manila psychosocial stress as residents deal with
measured the occupational stress levels of psy- feelings of helplessness and guilt that may have
3 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
lingering effects. (18) The stigma existing within The wellness committee must conduct a needs
the medical community also poses an additional assessment among residents which includes
stressor that has been unaddressed and has a quantitative and qualitative evaluations of the
negative impact on the morale of residents. degree of resident stress or burnout. This will
Numerous studies have proven that physician identify those trainees who may need certain
burnout is correlated with consequences support or intervention. Ultimately, a wellness
beyond the self, such as negative impact on program must be responsive to the specific
patient care and the health care system. These needs of the residents. In order to optimize
include medical errors, increased risk of success, the wellness committee must work
malpractice, and reduced patient satisfaction, closely with the mentoring program and training
quality of care and patient outcomes. (19) program committees.
The term “wellness” implies a multidimensional Embedding a culture of wellness should be an
and dynamic state of optimal well-being that end goal of every psychiatry residency training
may be generally defined as one’s personal program. While working on wellness on an
recipe for thriving and not just surviving. (20, 21) individual level is a given, a systems approach is
Specifically, the World Health Organization essential in providing the necessary envi-
defines it as “the realization of the fullest ronment where care for oneself is nurtured and
potential of an individual physically, psy- accepted as the norm. In North America, medical
chologically, socially, spiritually and eco- education accreditation bodies now consider
nomically and the fulfillment of [the] individual’s wellness as a core competency. (7) In the US, the
roles in family, workplace and community Accreditation Council for Graduate Medical
settings.” (20) The American Medical Association Education (ACGME) mandated residency pro-
defines it as being composed of six important grams to address trainee wellness within the
markers namely, nutrition, fitness, emotional Common Program Requirements. In 2017, a
health, preventative care, financial health, and Resident Wellness Consensus Summit (RWCS)
mindset and behavior adaptability. (16, 22) was inaugurated in the US. Part of this summit’s
Another model of wellness describes eight output was a proposal for an evidence-based
dimensions: professional (occupation, voc- wellness curriculum that contained seventeen
ational), social (family, community), emotional modules that focus on the spectrum of wellness
(mental), spiritual (values), intellectual, physical and burnout. A study showed that running small
(fitness, nutrition), environmental, and financial. group discussions on these topics significantly
(20) increased empowerment and work engagement
and decreased rates of burnout, emotional
The individual must strive to achieve wellness exhaustion, and depersonalization. (21) Table 3
because it does not come naturally. Further- describes these topics. The psychiatry
more, its inherent multidimensional nature department of McMaster University in Canada
makes quantitative research challenging. The launched its well-being program for residents in
Gallup-Healthways Well-Being Index Composite 2018. This program provided an electronic
Score is one attempt in quantifying wellness. It curriculum on resident resilience, a wellness
emphasizes the presence of health rather than newsletter, and peer groups as infrastructural
the absence of disease. In addition, it describes supports for residents. (7) Table 4 describes this
well-being across the following domains: life wellness program.
evaluation, emotional health, physical health,
healthy behavior, work environment, and basic A wellness program possesses a multidi-
access. (6) mensional approach that integrates individual
needs, institutional and cultural barriers to
Significant features that contribute to the wellness, and systemic issues that contribute to
success of wellness programs for medical stress. (2) At an individual level, wellness is
students have been identified. (6) These features achieved when residents practice healthy habits
may also be applicable to residents. These on a daily basis allowing a balance in the
include the presence of a wellness committee physical, emotional, intellectual, social, spiritual,
that coordinates with administration, con- environmental, and occupational aspects of
sultants, and residents and strategies that are being. Activities and/or interventions through-
designed to decrease the training burdens of out the academic year include, but are not
residents. limited to, retreats, mental health leaves, recrea-
4 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
5 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
-tional and leisure activities, exercise, conducive responding to issues as they emerge. Wellness
workspaces, retreat zones or quiet spaces, programs must allow residents to become an
respite spaces with relaxation apps, open air integral part of program policy changes and to
sitting areas, a simple gym area, a participate in program improvements.
snack/hydration station, self-care workshops, Consequently, wellness programs become more
and communication and stress management successful and leadership and communication
trainings. Avenues for psychosocial support skills are enhanced among residents. The
include, but are not limited to, check-ins with differences in experiences of the learning envi-
mentors or with each other, group peer support ronment among subgroups of residents does not
(structured group sharing), buddy systems, and permit a singular approach to wellness. Under-
therapy sessions. Residents must be made standing such diversity will guide whatever
aware of such interventions using multiple changes to the learning environment are made.
channels of communication such as regular (2, 3, 8, 16) The concept of the learning
emails, fliers posted in work areas, a wellness environment (LE) is defined by two main
website, and announcements in team meetings. dimensions namely, psychosocial and socio-
Ultimately, these programs must be able to material dimensions. Individual characteristics
reduce the barriers to accessing wellness that contribute to or respond to the LE, inter-
services. Studies have identified several barriers personal interactions, and institutional policies,
that include concerns about confidentiality, culture, and regulation constitute the layers of
stigma and stoicism, fears about reporting to the psychosocial dimension. The sociomaterial
credentialing or licensure boards, financial dimension defines how residents interact with
concerns, demanding clinical schedules, and the physical and virtual worlds that they learn in.
identifying therapists experienced in working (20) Incorporating web-based and other digital
with physicians. (5, 16) resources into residency training will contribute
to the success of wellness programs because
Wellness programs should foster a culture that this provides the residents the opportunity to
allows open exchange of ideas and flexibility in learn at their own pace. (7)
6 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Figure 1 depicts a model of the learning Bibliography of Recommended Resource
environment. At present, the relationship Materials for Wellness Programs
between wellness and LE is not well understood
and needs to be studied using high quality 1.AMA STEPS Forward
research. (20)
https://edhub.ama-assn.org/steps-
forward/module/2702511
2. APA Toolkit for Well-Being Ambassadors: A
Manual
(https://www.psychiatry.org/psychiatrists/practi
ce/well-being-and-burnout/well-being-
resources#:~:text=Download%20the-,Toolkit%20
for%20Well%2Dbeing%20Ambassadors,-
Download%20the%C2%A0)
Objectives 3. Nasirzadeh Y., Chertkow L., Smith S. et al.
General: To develop a program that will enhance (2021). What do residents want from wellness? A
the wellbeing of psychiatry residents. needs assessment of Psychiatry residents to
inform a residency wellness strategy. Academic
Specific: The wellness program must aim to Psychiatry.
1. Increase the awareness of psychiatry https://www.ncbi.nlm.nih.gov/pmc/articles/PMC
residents of the factors and resources that 8782672/pdf/40596_2021_Article_1578.pdf
contribute to well-being.
2. Provide information, activities, and services 4. Resident Wellness Toolkit (John Hopkins
designed to support healthy lifestyle choices Medicine)
among psychiatry residents.
3. Encourage habits of wellness among https://christianacare.org/documents/medical-
psychiatry residents. dental%20staff/ResidencyWellnessToolkit-
4. Empower psychiatry residents to take Prototype-Dec17.pdf
responsibility for their own health.
5. Address the physical, emotional, intellectual, 5. Resilience in the Era of Sustainable Physicians:
social, spiritual, environmental, and An International Training Endeavour
occupational needs of psychiatry residents.
6. Improve the quality of life of psychiatry https://respite.machealth.ca
residents.
7. Promote the resiliency of psychiatry In summary, the following steps in developing a
residents. wellness program for psychiatry residents are
8. Recognize the early signs of psychological recommended by the Board. First, a wellness
distress among psychiatry residents. committee must be formed. Second, the
9. Prevent burnout and other psychiatric committee conducts a baseline needs
sequelae of residency training. assessment and burnout inventory profile of the
10. Facilitate access to medical and residents. Although not validated locally, the
psychosocial services to trainees with health Maslach Burnout Inventory may be used as this
concerns. is considered the gold standard. Alternatively,
11. Combat stigma to encourage residents to the Copenhagen Burnout Inventory and
share their experiences with chronic stress screening scales for depression and/or anxiety
and burnout. may also be utilized. Third, the committee
12. Engage residents in program policy making. creates a module (see Table 3 for an example) to
13. Evaluate its effectiveness. introduce stress, burnout and wellness. These
14. Produce and/or publish research outputs topics are introduced not as a formal lecture but
about wellness of psychiatry residents. embedded in various activities (small group dis-
7 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
-cussion or sharing) or in spaces within the Citing the importance of mentorship in the
wellness program structure. Flexibility, creativity continuum of academic medicine, the Office for
and resourcefulness is important in this area. Diversity Inclusion and Community Partnership
Fourth, review existing wellness resources within of the Harvard Medical School, for instance,
the workplace and improve when able and offers mentoring for junior faculty, trainees and
necessary. These include safe/quiet spaces such students. They offer varied mentor trainings and
as residents’ quarters or working spaces, provide online resources for mentors and
hydration stations, access to healthcare, among mentees in order to ensure the quality of the
others. Fifth, the wellness committee must work program. (25) A study of successful physicians
closely with the training and mentoring showed that medical career success was
committees. This will address the stressors that determined by the acquisition during training of
come from the learning environment. Simple core competencies such as patient care, medical
examples of these may be honoring protected knowledge, interpersonal and communication
time or schedules that have been set skills, professionalism, practice-based learning
beforehand and improving avenues of and improvement, and systems-based practice.
communication to allow open exchange of ideas. (26) Mentoring programs should therefore be
designed in line with the core competencies set
In conclusion, data on burnout among by training or accrediting bodies in the specialty.
psychiatry residents in the Philippines is scanty.
This must not hinder initiatives to introduce The perceived benefits of mentoring may cross
wellness programs among the training centers. the personal-professional interface and may
Worldwide data shows an upward trend in override organizational differences. (27) The
burnout and depression and anxiety in the diagram below highlights the complex
medical profession. In order to generate relationships which exist between the three
baseline data, the accredited training centers of areas of professional practice, personal well-
PPA must collaborate to develop a working being, and personal and professional
system that is relevant, dynamic, and adaptable. development. This can be a guide for the
mentoring process for both mentors and
II. Mentoring Program mentees.
Figure 2. The Personal-Professional Overlap: Areas of Benefit
A study of 229 Psychiatry chief residents
and Underlying Processes
participating in the American Psychiatric
Association National Chief Residents Leadership
Program in 2004 and 2005 showed that half of
them reported a lack of clearly defined career
development mentors. These trainees believed
that they were less prepared to practice
psychiatry after graduation. This showed the
need for psychiatric residency training programs
to clarify and implement effective mentorship
programs. (23)
The Standing Committee on Postgraduate
Medical and Dental Education (24), defined
mentoring as, “guiding another individual in the
development and re-examination of their own
ideas, learning and personal and professional Mentors can provide support and
development.” Since the transitions in the encouragement for a resident’s personal
journey from medical student to consultant can development, usually with a professional focus,
be complicated, mentoring can help residents that also factors in work-life balance (22).
cope and adjust to the challenges. Mentoring involves the long-term development
of residents who are helped to manage their
Many graduate medical education programs training and improve their skills. In addition,
internationally have mandated the inclusion of mentoring provides a venue for the residents to
mentoring in postgraduate training. discuss their personal issues in confidence and a
8 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
way of achieving both individual and Informal mentoring between consultants
organizational goals. (28) (mentor) and residents (mentee) is being
conducted in some training programs. These
Mentoring programs during residency training programs, however, must be formalized,
can increase the satisfaction, well-being, structured, and standardized in order to ensure
positive work, and career attitudes of trainees. It the quality and consistency of its benefits.
can help them realize their full potential in Mentoring programs must be embedded in all
Psychiatry and achieve the results they value by Psychiatry residency training programs in the
allowing them to take charge of their own Philippines and must essentially be part of the
development. (29) Additionally, the benefits of evaluation of training programs for accre-
mentoring apply not only to residents but to the ditation.
wider system they are in. Since their personal Training on how to design, run, and evaluate a
and professional developments are enhanced, mentoring program is a significant activity that
these may lead to increased trainee retention in ensures the success of the mentoring endeavor.
training programs, enhanced team relationships, Collaboration among the different training
improve competence in patient care and elevate institutions is highly encouraged and supported
over-all improvement in the quality of mental by the Board because this will guarantee that
healthcare services. (30) the program outcomes are uniformly aspired for
and achieved.
De Souza asserts that mentoring must not be
confused with direct work-related supervision Objectives
and therapy or counseling. (31) Hameed and General: The mentoring program must empower
colleagues point out that mentoring can mean and support Psychiatry residents in their
different things to different people and there training and future career development in order
may be a confusion between mentoring and to increase their professional satisfaction, well-
other formal structures of support such as being, positive work experiences, and career
supervision, coaching, consultation, befriending, attitudes.
and even counseling. (32) Mentoring is none of
the above but at the same time a combination of Specific: The mentoring program must:
them. Mentoring may overlap with coaching,
which is viewed as building particular skills and 1. Provide resources and support to ensure
focusing on a narrowly defined task or goal. The that mentors and mentees have productive,
difference is that mentors, who have more fulfilling, and sustainable interactions.
experience in the profession, convey and instill 2. Help the trainees realize their full potential
the standards, norms and values of the by helping them take charge of their own
profession with a holistic broader view (33). development.
3. Provide a nurturing learning environment
Since there will be investment in time, effort, where networking between mentors and
and resources for mentoring programs, this mentees are facilitated.
demands evaluation that may include any of the 4. Provide mentors with opportunities to
following: mentee empowerment and training, develop their skills, knowledge, and attitudes
mentor training, aligning expectations, mentor related to their mentoring roles.
self-reflection, and mentee evaluation of 5. Provide mentors with opportunities to share
mentor. It is also important in the long run to their wisdom and experience to mentees.
evaluate the sustainability of the program. (34) 6. Support and guide mentees in order to
Mentoring relationships last for varying lengths ensure trainee retention, enhanced team
of time but they can continue after the training relationships, and improvement in the
stages in order to include guidance in the early quality of mental healthcare services.
stages of practice. (24) It is a formative and 7. Evaluate its effectiveness.
developmental relationship that can 8. Produce and/or publish research outputs on
significantly impact the personal and profes- mentorship of psychiatry residents.
sional life of an individual.
Proposed Methodologies
What is the state of mentoring in Psychiatry A. Training of mentors
training in the Philippines at present? B. Matching/selection of mentees/mentors
9 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
C. Orientation sessions Specific: At the end of the course, the
D. Mentorship sessions psychiatric resident must be able to
E. Collaboration among the training institutions
in developing mentoring programs 1. Illustrate how the theoretical foundations of
gender and gender role orientation are
III. Gender Sensitivity applied in medicine and psychiatry.
2. Compose biopsychosocial formulations of
Gender and gender role orientation increasingly patients that integrate gender and gender
assume salient functions in mental health and role concepts.
illness both on the individual and community 3. Design and implement gender sensitive
levels. A study of young adolescents showed interventions for patients and their families.
that perceived gender role influences one’s 4. Propose and/or researches on gender and
expression of empathy. (35) Another study gender role orientations.
showed that adolescents who possessed both
positive masculine and feminine qualities in their Proposed Methodologies
self-concept had optimal levels of school-
related well-being. (36) The rapid increase in 1. Didactics
transgender and gender diverse people seeking 2. Seminars
medical help has created a transgender 3. Workshops
healthcare system that is evolving into an 4. Focus group discussions
interdisciplinary field. (37) Gender may be a 5. Case conferences
factor that contributes to poor mental health 6. Clinical supervision
because of stigma, social inequality, and
discrimination. For instance, mental health Ideally, this learning exercise should be
conditions such as anxiety, depression, and low accomplished during the resident’s second year
levels of well-being are more common among of residency training.
women. (38). Gender and gender roles may also
influence the prevalence, symptom profile, age Proposed Topics
of onset, comorbidities, functional impairment,
and prognosis of mental disorders. Furthermore, Learning activities include, but are not limited
gender-related factors have important impli- to, the following topics.
cations to treatment response. (39) The major
systems of classification of mental disorders, 1. Key concepts on gender
namely DSM 5 and ICD 11, contain stand-alone 2. Sex and gender differences in health
chapters for gender-related mental disorders. 3. Guidelines on anti-sexual harassment
(40, 41, 42). 4. Gender sensitive healthcare
5. Gender sensitive language
It is imperative that psychiatrists possess a firm 6. Gender sensitive clinical practice
and thorough understanding of the concepts of 7. Gender aspects in psychiatry, psycho-
gender and gender role orientation because this dynamics, and psychotherapy
has serious implications on the diagnosis and
management of mental disorders and the IV. Religion and Spirituality (R/S) and Psychiatry
establishment of a therapeutic relationship and
the quality of patient care. (43) The Philippine In recent time, the relevance of R/S to health
Psychiatric Association, through the Board of issues has been increasingly studied. Literature
Accreditation of the Specialty Board of abounds with empirical researches that
Philippine Psychiatry therefore require the demonstrate the relationship between R/S and
incorporation of learning activities on gender health. The concepts of religion and spirituality
sensitivity in all psychiatric residency training (R/S) have been used synonymously because of
programs in the country. the lack of a universally agreed definition. (44) At
present, religion and spirituality are viewed as
Objectives distinct yet overlapping concepts. Spirituality is
General: At the end of the course, the a broad concept that involves a dimension of
psychiatric resident must be able to integrate subjective, embodied, and emotional exper-
the principles of gender sensitivity to clinical iences of closeness and connection with the
practice. sacred or transcendent or to ultimate reality.
10 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Spirituality is intimately linked with values, On the other hand, R/S may be associated with
meaning and purpose and it develops negative health outcomes, such as depression,
individually or in communities and traditions. In obesity, poor compliance to treatment and even
contrast, religion is the institutional aspect of oppression and violence (57). Religious crises
spirituality. It involves a search for importance may lead to distress or be symptoms of
in the context of adhering to established and psychopathology (e.g., delusions or
organized beliefs, behaviors, and practices that hallucinations). Religion may also become a
are part of a particular faith tradition, problem when it is used to avoid making changes
community, or social group. (44, 45, 46, 47, 48) in attitude or behavior or when religious
Spirituality is more popular than religion teachings are rigidly and inflexibly applied. (52)
because it is self-defined and inclusive. Religion, The integration of R/S in psychotherapy has
on the other hand, may be unpopular because of been shown to result in greater improvement in
its potential to be divisive. psychological and spiritual functioning
compared with no treatment and non-R/S
The growing interest in the role of R/S in health psychotherapies. R/S-adapted psychotherapy
care in general and in mental health care in influences treatment through case formulation,
particular has led to studies that show that treatment goals, interventions, and
patients want their R/S concerns addressed by interpersonal processes. (47) Despite this
health care providers. (44) In fact, the World evidence, most psychotherapists receive little or
Health Organization considers R/S as an no training in R/S issues. One possible
essential quality of life element (49). A meta- explanation to this problem is the absence of an
analysis of 48 longitudinal studies showed agreed-upon R/S competencies or training
evidence for a positive effect of R/S on mental guidelines. (48)
health (50). The association of R/S with mental
health has an even greater implication for global R/S contributes to the psychological wellbeing
public health because more than 84% of the of residents which, in turn, is associated with
world’s population has some religious affiliation. greater sense of work accomplishment, overall
(51). Specifically, attendance in religious services self-rated health, lesser burnout and depressive
has been significantly asso-ciated with greater symptoms, and better therapeutic relationship.
longevity, less depression, less suicide, less These redound to better treatment adherence
smoking, less substance abuse, better cancer and coping among patients. (46)
and cardiovascular disease sur-vival, less
divorce, greater social support, greater meaning In the Philippines, the Philippine Council for
and purpose in life, greater life satisfaction, Mental Health (created through Republic Act
greater wellbeing, more charitable giving, more 11036) calls for a reorientation of the concept of
volunteering, and greater civic engagement (44, mental health. It advocates for the integration of
52, 53). King and Bushwick found that 94% of the spiritual dimension of health in the extant
patients believed spiritual health was as biopsychosocial model of health. This
important as physical wellbeing. Although 77% of movement is also being pursued in government
the patients wanted spiritual matters to be sectors apart from the health sector. (58) In
considered in their care, only 10-20% had other parts of the world, psychiatrists –
conversations with their physician on the topic. regardless of their religious, spiritual, or
(54) philosophical orientations – are urged to include
R/S in the evaluation and management of
R/S has significant implications on the patients. Studies show, however, that mental
prevalence, diagnosis, outcomes, and health professionals fail to integrate R/S in
prevention of mental disorders (44). Fitchett and clinical practice because of several reasons. A
colleagues reported that 80% of psychiatric major impediment is the lack of formal training.
patients expressed the need for prayer and 65% Many psychiatry residency training coordinators
of them needed a visit from a chaplain to pray and faculty have an insufficient knowledge of
with them. (55) Studies also suggest that R/S is the subject and a lack of time to include it in
related to greater subjective well-being, life training. In addition, they are apprehensive
satisfaction, and marital satisfaction, as well as about proselytizing or introducing an
to decreases in mental health problems such as unscientific approach and adding another topic
depression, suicide, delinquency, and alcohol to an already full curriculum. (57) There are few
and drug use. (56). psychiatry training programs that integrate R/S
11 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
in research and clinical practice. 1. Conceptualize R/S as an important aspect of
human diversity along with factors such as
The World Psychiatric Association (WPA) and race, ethnicity, sexual orientation,
national psychiatric organizations from Brazil, socioeconomic status, disability, gender, and
India, South Africa, UK, and USA created age.
organizational sections on R/S. In addition, WPA 2. Discuss how R/S are distinct yet overlapping
has included R/S in the core training curriculum constructs.
for psychiatry. (44, 57) Courses in psychiatry 3. Compare the diverse forms of R/S.
residency programs in North America are being 4. Discuss the positive and negative ways by
developed to address this important aspect of which R/S affects mental health.
life. The American Accreditation Council for 5. Discuss how patients’ R/S develops and
Graduate Medical Education and the American changes over the lifespan.
Psychiatric Association (APA) emphasize the 6. Construct a complete R/S history as a
importance of addressing spiritual issues in routine part of psychiatric practice.
psychiatry training. The APA has started to 7. Integrate the bio-psycho-socio-spiritual
establish R/S competencies for psychiatrists. In elements of a case in the diagnostic process
addition, the American Association of Medical and the treatment plan.
Colleges and the Joint Commission on the 8. Demonstrate the psychodynamic aspects
Accreditation of Healthcare Organizations in the involving R/S issues in psychotherapy (e.g.,
US, require the incorporation of R/S in patient transference, countertransference).
care. (47) In Canada, psychiatric residency 9. Disseminate information about the
training programs are increasingly mandating relationship of R/S and mental health to the
training in R/S (59, 60). De Oliveira and wider community as a way of helping
colleagues developed a comprehensive R/S promote the health and wellbeing of
curriculum based on a review of prevalent individuals.
strategies of training and recommendations 10. Formulate ways by which his/her patients
from psychiatric associations. This curriculum may access their R/S strengths and
consists of a 12-hour course for psychiatry resources.
residents that is easily implementable even if 11. Apply evidence-based strategies or
the faculty does not have expertise in R/S and interventions in addressing the mental
there is little time to learn it. (57) health issues and mental disorders of
patients with diverse R/S backgrounds.
R/S is woven into the fabric of the core beliefs, 12. Contrast the experiences of patients that are
values, and experiences of many Filipinos. These consistent with their R/S and those that are
constructs should therefore play a central role part of psychopathological processes.
in academic, clinical, and investigative 13. Examine legal and ethical issues related to
psychiatry in the Philippines. At present, the R/S that may arise when working with
Philippine Council for Health Research and patients.
Development is working on identifying aspects 14. Demonstrate empathy, respect, and
of R/S that are relevant to mental health appreciation for patients from diverse
research in the country. (61) In the Philippines, spiritual, religious, or secular backgrounds
most psychiatry residency training programs do and affiliations.
not incorporate formal and systematic courses 15. Examine how his/her own R/S background
on R/S. The Board of Accreditation therefore and beliefs influence his/her clinical practice
requires inclusion of this course in psychiatry and his/her attitudes, perceptions, and
residency training because of its benefit to assumptions about the nature of mental
resident trainees and, ultimately, patients. processes.
16. Assess his/her R/S competence continuously.
Objectives 17. Demonstrate the willingness to collaborate
General: At the end of the course, the psychiatry with leaders or members of faith
resident must be able to apply the concepts and communities, chaplains, pastoral workers,
principles of R/S in mental health care. clergy, and other qualified individuals and
groups in support of the wellbeing of their
Specific: At the end of the course, the psychiatry patients.
resident must be able to:
12 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
18. Analyze current research on the relationship REFERENCES
of R/S to clinical practice. 1. Commission on Higher Education. CHED memorandum order, No.
18, Series of 2016. Available from: https://www.cem-
19. Propose and/or publish researches on the inc.org.ph/nmat/files/upload/CHED_MO_No__18_Doctor_of_Medic
relationship between R/S and physical and ine_Program.pdf.
mental health. 2. Chaukos D, Zebrowski JP, Benson NM, Celik A, Chad‐Friedman E,
Teitelbaum A et al. (2021). “One size does not fit all” – lessons
learned from a multiple-methods study of a resident wellness
Proposed Pedagogical Strategies curriculum across sites and specialties. BMC Medical Education.
2021; 21: 576. Available from: https://doi.org/10.1186/s12909-
021-02995-z.
1. Blended and hybrid learning 3. Lefebvre D, Dong KA, Dance E, Rosychuk RJ, Yarema M, Blouin D
2. Didactics et al. Resident physician wellness curriculum: A study of efficacy
and satisfaction. Cureus. 2019;11, 8, e5314, DOI
3. Seminars 10.7759/cureus.5314
4. Workshops 4. Mendonça VS, Steil A, Gois AFT. Mental health and the COVID-19
pandemic: a study of medical residency training over the years.
5. Focus Group Discussions
Clinics. 2021; Available from: DOI: 10.6061/clinics/2021/e2907
6. Case conferences 5. Ey S, Soller M, Moffit M. Protecting the well-being of medical
7. Supervision residents and faculty physicians during the COVID-19 pandemic:
Making the case for accessible, comprehensive wellness
8. Feedback resources. Global Advances in Health and Medicine. 2020; 0: 1–4.
9. Reflective practice 6. Klein HJ, McCarthy SM. Student wellness trends and
10. Faculty and peer support interventions in medical education: A narrative review.
Humanities and Social Sciences Communications. 2022; 9: 92,
Available from https://doi.org/10.1057/s41599-022-01105-8.
This course is recommended during second year 7. Hategan A, Riddell T. (2020). Bridging the gap: Responding to
resident burnout and restoring well-being. Perspect Med Educ.
of residency training. In developing this course,
2020; 9: 117-122, Available from: https://doi.org/10.1007/s40037-
the training program committee must be 020-00567-3.
cognizant of the following caveats: (1) R/S is not 8. Alkatan HM. Impact of trainers-related factors and “generation
gap” on the quality of local residency training. International
more important than other core areas of mental Journal of Current Research. 2015; 7(12): 24221-24224.
health; (2) residents are not required to gain in- 9. World Health Organization. DOH, WHO, the Australian
Government launch 'The Wellness Movement' for Filipino
depth knowledge of theologies or R/S concepts
healthcare workers nationwide. 2023; Available from:
and traditions around the world; and (3) R/S https://www.who.int/philippines/news/detail/16-01-2023-doh--
does not apply only when working with highly who--the-australian-government-launch--the-wellness-
movement--for-filipino-healthcare-workers-nationwide
religious or spiritual patients. The residency 10. Palaubsanon ML. DOH launches Wellness Movement. 2023;
training program committee must be able to Available from: https://www.philstar.com/the-freeman/cebu-
identify hindrances to R/S-related training and news/2023/01/29/2241048/doh-launches-wellness-movement.
11. Marcha JC. Correlation between burnout domains and
assess the outcomes of R/S-related curriculum depression severity among resident physicians in the UP-PGH
including how they affect the wellbeing of using Maslach Burnout Inventory and Beck Depression Inventory.
2019; Available from: https://www.herdin.ph/index.php/registry?
patients and residents through time. (46)
view=research&layout=details&cid=2362
12. Turalde CW, Espiritu A, Macinas ID, Jamora RD. Burnout among
neurology residents during Covid-19 Pandemic: A national cross-
AUTHOR INFORMATION AND CONTACT DETAILS: sectional study. Neurol Sci. 2022; 43(3): 1503-1511. Available
Ruth T. Villanueva, M.D. from: https://pubmed.ncbi.nlm.nih.gov/34846584/
Department of Neurosciences and Behavioral Medicine 13. Monforte R. Prevalence of burnout and self-reported patient care
University of Santo Tomas Hospital attitudes and practices of residents in training at The Medical
villanueva.ruth@yahoo.com City in 2005. Phil Journal of Psychiatry. 2011; 33(2): 20-29.
Available from: https://www.herdin.ph/index.php/herdin-
journals?view=research&cid=43848
Myra Dee Lopez-Roces, M.D.
14. Franco PI, Cuaño PMG, Palileo-Villanueva LA, Mendoza J. Burnout
Department of Psychiatry
and resilience of internal medicine physician trainees in a tertiary
Batangas Medical Center government hospital in the Philippines during the COVID-19
myradee.lopez@gmail.com pandemic: A mixed-method study. Acta Medica Philippina. 2022;
56(6): 7-11.
Constantine D. Della, M.D. 15. Bordado MR, Corpuz C, Cruzada J, Valdes-Cabio R. Occupational
Department of Psychiatry and Behavioral Medicine stress level and socio-demographic profiles of psychiatry
College of Medicine and Philippine General Hospital residents at the National Center for Mental Health. Philippine
University of the Philippines Manila Journal of Psychiatry. Jan – June 2011; 33(1): 3-7.
cddella@up.edu.ph 16. Mari S, Meyen R, Kim B. Resident-led organizational initiatives to
reduce burnout and improve wellness. BMC Medical Education.
Jannel Gatlabayan-Cleto, M.D. 2019; 19: 437, Available from: https://doi.org/10.1186/s12909-
019-1756-y.
Department of Psychiatry
17. Lu F, Ratnapalan S. Burnout interventions for resident physicians:
Institute of the Neurosciences
A scoping review of their content, format, and effectiveness. Arch
The Medical City
Pathol Lab Med. 2023; 147: 227–235, doi: 10.5858/ arpa.2021-
jannelgatlabayancleto@gmail.com 0115-EP.
18. Puttagunta R, Lomax ME, McGuinness JE, Coverdale J. What is the
Georgina M. Gozo-Oliver, M.D. prevalence of the experience of a death of a patient by suicide
Department of Psychiatry among medical students and residents? A systematic review.
Veterans Memorial Medical Center Acad Psychiatry. 2014; 38(5): 538-41.
ggozooliver@yahoo.com
13 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
19. Patel RS, Ramya B. Factors related to physician burnout and its 39. Christiansen DM, McCarthy MM, Seeman MV. Where sex meets
consequences: A review. Behav Sci. 2018; 8(11): 98. gender: how sex and gender come together to cause sex differences
20. Gruppen LD, Fogarasi MC. Considerations on conducting in mental illness. Frontiers in Psychiatry. 2022; 13: 856436, doi:
research on wellness in the context of the learning environment. 10.3389/fpsyt.2022.856436.
Global Advances in Health and Medicine. 2021; 10: 1–9, DOI: 40. American Psychiatric Association. Diagnostic and Statistical
10.1177/2164956121989708. Manual of Mental Disorders, Fifth Edition. 2013; Arlington, VA:
21. Arnold J, Tango J, Walker I, Waranch C, McKamie J, Poonja Z., et American Psychiatric Association.
al. An evidence-based, longitudinal curriculum for resident 41. International Classification of Diseases 11th Revision, World
physician wellness: The 2017 resident wellness consensus summit. Health Organization, Available from: https://icd.who.int/en.
Western Journal of Emergency Medicine. 2018; 19(2): 337-341. DOI: 42. Reed GM, Drescher J, Krueger RB, Atalla E, Cochran SD, First MB
10.5811/westjem.2017.12.36244. et al. Disorders related to sexuality and gender identity in the ICD-11:
22. AMA. Preventing burnout in medical residents and fellows: 6 revising the ICD-10 classification based on current scientific
keys for wellness. 2016; Available from: https://wire.ama- evidence, best clinical practices, and human rights considerations.
assn.org/education/preventing-burnout-medical-residents-and- World Psychiatry. 2016; 15: 205–221.
fellows-6-keys-wellness. 43. Yu Chua C. Gender Liaison Program of the Section of
23. Lis LDF, Wood WC, Petkova E, Shatkin J. Mentoring in Consultation-Liaison Psychiatry, Department of Psychiatry &
psychiatric residency programs: A survey of chief residents. Behavioral Medicine, Philippine General Hospital. 2017 (Unpublished
Academic Psychiatry Journal. 2009; 33(4): 307-212. document)
24. Royal College of Psychiatrists (RCPSYCH). Guide to Mentoring 44. Moreira-Almeida, A., Sharma, A., Bernard van Rensburg, B.J.,
for Psychiatric Trainees. 2021; Available from: Verhagen, P.J.,
https://www.rcpsych.ac.uk/docs/default- 45. Christopher C.H. Cook, C.C.H. (2016). WPA position statement on
source/members/supporting-you/mentoring/guide-to-mentoring- spirituality and religion in psychiatry. World Psychiatry. 15, 1.
for-psychiatric-trainees.pdf 46. Davis EB, Worthington EL Jr., Schnitker SA, Glowiak KJ, Lemke
25. Gupta A, Gupta K, Vsudevan V. Excellence in the Accreditation AW, Hamilton C. Integrating positive psychology and the psychology
Council for Graduate Medical Education core competencies: of religion and spirituality: Transcending coexistence to potentiate
Strengthening the mentor-mentee relationship. Cureus. 2020; coevolution. In Davis, E.B., Worthington, E.L. Jr., & Schnitker, S.A.
12(6): e8564. (Eds.). Handbook of Positive Psychology, Religion, and Spirituality. p.
26. Harvard Medical School, Office for Diversity Inclusion and 3-19, 2023; Available at: https://doi.org/10.1007/978-3-031-10274-5.
Community Partnership. Mentoring at Harvard Medical School. 47. Chow HHE, Chew QH, Sim K. Spirituality and religion in residents
Available from: https://dicp.hms.harvard.edu/mentoring. and inter-relationships with clinical practice and residency training: a
27. Steven A, Oxley J, Fleming WG. Mentoring for NHS doctors: scoping review. BMJ Open. 2021; 11(5): e044321, doi:
Perceived benefits across the personal-professional interface. 10.1136/bmjopen-2020-044321.
Journal of the Royal Society of Medicine. 2008; 101(11): 552-557. 48. Captari LE, Hook JN, Hoyt W, Davis DE, McElroy-Heltzel SE,
28. Huline-Dickens S. Coaching and mentoring: an overview for Worthington EL Jr. Integrating clients’ religion and spirituality within
trainers in psychiatry. British Journal of Psych Advances. 2021; 27: psychotherapy: A comprehensive meta‐analysis. J. Clin. Psychol.
219-227. 2018; 74: 1938–1951, DOI: 10.1002/jclp.22681.
29. Ekeh, B.C. (2018). Mentorship in Medicine: A Book on Mentoring 49. Vieten C, Scammell S, Pilato R, Ammondson I, Pargament KI,
in the Medical Profession. USA: Create Space Independent Lukoff D. Spiritual and religious competencies for psychologists.
Publishing Platform. Psychology of Religion and Spirituality. 2013; 5(3): 129–144, DOI:
30. Wilson G, Larkin V, Redfern N, Stewart J, Steven A. Exploring the 10.1037/a0032699.
relationship between mentoring and doctor’s health and wellbeing: 50. WHOQOL SRPB Group. A cross-cultural study of spirituality,
A narrative review. Journal of the Royal Society of Medicine. 2017; religion, and personal beliefs as components of quality of life. Soc Sci
110(5): 188-197. Med. 2006; 62: 1486-1497.
31. De Souza B. Coaching and mentoring skills: necessities for 51. Garssen B, Visser A, Pool G. (2020). Does spirituality or religion
today’s doctors. BMJ. 2014; 348: g4244. positively affect mental health? Meta-analysis of longitudinal
32. Hameed Y, Bosier E, Waal HD, Miller J. Using mentoring to studies. The International Journal for the Psychology of Religion.
improve the foundation placement in psychiatry: Review of 2020; Available from:
literature and a practical example. British Journal of Medical https://doi.org/10.1080/10508619.2020.1729570.
Practitioners. 2016; 9: 4. 52. Pew Research Center. The global religious landscape: A report on
33. FICM Thrive. The Intensive Care Medicine Career Mentoring and the size and distribution of the world’s major religious groups as of
Personal Development Programme – Guidance Document. May 2010. 2012; Washington: Pew Research Center.
2021; Available from: 53. Koenig HG, Peteet JR, VanderWeele TJ. Religion and psychiatry:
https://www.ficm.ac.uk/sites/ficm/files/documents/2021- clinical applications. BJPsych Advances. 2020; 26, 273–281,
10/ficm_thrive_mentoring_guidance_document_v5_-_formatted.pdf. doi:10.1192/bja.2020.11.
34. Sheri K, Too JYJ, Chuah SELC, Toh YP, Mason S, Krishna LKR. 54. VanderWeele TJ. Religious communities, health, and well-being –
(2019). A scoping review of mentor training programs in medicine address to the US Air Force chaplain. Military Medicine. 2018;
between 1990 and 2017. Medical Education Online, 2019; 24(1): 183(5/6): 105-109.
1555435. Available from: 55. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients
https://www.tandfonline.com/doi/full/10.1080/10872981.2018.155 about faith healing and prayer. Journal of Family Practice. 1994; 39:
5435 349-52.
35. Andrews K, Lariccia L, Talwar V, Bosacki S. Empathetic concern 56. Fitchett G., Burton LA, Sivan AB. The religious needs and
in emerging adolescents: the role of theory of mind and gender resources of psychiatric patients. J Ner Ment Dis. 1997; 185: 320-326.
roles. Journal of Early Adolescence, 2021; 41(9): 1394–1424. 57. Puchalski CM, Larson DB, Lu FG. Spirituality in psychiatry
36. Korlat S, Holzer J, Schultes M., Buerger S, Schober B, Spiel C et residency training programs. International Review of Psychiatry.
al. Benefits of psychological androgyny in adolescence: the role of 2001; 13(2): 131-138.
gender role self-concept in school-related well-being. Frontiers in 58. De Oliveira e Oliveira FHA, Peteet JR, Moreira-Almeida A.
Psychology. 2022; 13: 856758, doi: 10.3389/fpsyg.2022.856758. Religiosity and spirituality in psychiatry residency programs: Why,
37. Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, what, and how to teach. Brazilian Journal of Psychiatry. 2021; 43(5):
Deutsch MB et al. Standards of care for the health of transgender 564.
and gender diverse people, version 8. International Journal of 59. Ladrido-Ignacio L. (2022). Spirituality and mental health. 2022;
Transgender Health. 2022; 23(s1): s1–s258, Available from: Available at: https://www.thinkglobalhealth.org/article/spirituality-
https://doi.org/10.1080/26895269.2022.2100644. and-mental-health.
38. Kelmendi K, Jemini-Gashi J. An exploratory study of gender role 60. Roth B, Grabovac A. Spirituality and religion in Canadian
stress and psychological distress of women in Kosovo. Women’s psychiatric residency training: Follow-up survey of Canadian
Health. 2022; 18: 1–15. psychiatry residency programs. Acad Psychiatry. 2023; Available
from: https://doi.org/10.1007/s40596-023-01785-7.
14 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
61. Grabovac AD, Ganesan S. Spirituality and religion in Canadian
psychiatric residency training. Canadian Journal of Psychiatry.
2003; 48: 171-175.
62. Department of Science and Technology – Philippine Council for
Health Research and Development (DOST-PCHRD). PCHRD, MH
Advisory Group explore spiritual dimension of mental health in a
series of RTDs. Available from:
https://www.pchrd.dost.gov.ph/news_and_updates/pchrd-mh-
advisory-group-explore-spiritual-dimension-of-mental-health-in-a-
series-of-rtds/
15 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP SPECIAL ARTICLE
SUPPORTING MEDICAL EDUCATORS TO ENSURE
WELLNESS OF MEDICAL STUDENTS
CONSTANTINE DELLA, MD, FPPA
Most medical faculty members assume various In addition, it describes well-being across the
roles such as educator, administrator, clinician, following domains: life evaluation, emotional
and researcher. (1) Furthermore, they act as role health, physical health, healthy behavior, work
models for students and instruments to improve environment, and basic access. (2)
student wellness. Strategies geared towards the
faculty can therefore promote a top-down In the Philippines, wellness activities are being
approach to enhancing student wellness. (2) conducted for medical faculty but these are not
Unfortunately, there is a dearth of data about organized, systematized, and institutionalized.
this. If we expect the faculty to take care of This presentation will discuss how wellness
students’ wellness, then we must ascertain the initiatives for medical faculty are designed and
faculty’s wellness as well. implemented abroad. It will highlight the critical
role that medical school leadership possesses in
“Wellness” refers to a multidimensional and making faculty wellness a priority.
dynamic state of optimal wellbeing. (3,4)
Specifically, the World Health Organization Medical schools currently face difficulty
defines it as “the realization of the fullest attracting and retaining faculty. Many factors
potential of an individual physically, have been identified to explain this problem.
psychologically, socially, spiritually and These include the income gap between private
economically and the fulfillment of [the] practice and academia, available time for family
individual’s roles in family, workplace and and personal life, quality of departments,
community settings.” (3) The American Medical teaching load, and rigorous and inflexible work
Association defines it as being composed of six schedule. (7,8) Studies have also shown that
important markers namely, nutrition, fitness, many physicians continue to experience high
emotional health, preventative care, financial rates of burnout and decreased wellbeing. (9)
health, and mindset and behavior adaptability.
(5,6) Another model of wellness describes eight Research shows that the rate of burnout is
dimensions: professional (occupation, similar for academic medical faculty and
vocational), social (family, community), physicians in general. Among the different types
emotional (mental), spiritual (values), of medical faculty, the rates of burnout are
intellectual, physical (fitness, nutrition), similar, whether they belong to clinical
environmental, and financial. (3) The individual departments involved in patient care, clinical
must strive to achieve wellness because it does departments not involved in patient care, or
not come naturally. The inherently basic science departments. What varies are the
multidimensional nature of wellness makes factors that contribute to burnout. (1) The high
quantitative research challenging. The Gallup- prevalence of burnout among medical faculty in
Healthways Well-Being Index Composite Score is the West is reflected in the first nationwide
one attempt in quantifying it. It emphasizes the study on medical faculty burnout in South
presence of health rather than the absence of Korea. Faculty members from 40 medical
disease. schools participated in the study. Using the
16 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Maslach Burnout Inventory, the following rates (e.g., stress management workshops,
for burnout parameters were obtained: 34% mindfulness training, resilience training) that are
experienced emotional exhaustion, 66.3% insufficient to produce meaningful outcomes. (2)
experienced depersonalization, and 92.4% Experts believe that systemic factors such as
experienced reduced personal accomplishment. organizational pressures and work stressors and
(10) not personal resilience contribute to burnout
among healthcare professionals. (9)
(Paper was delivered on 15 June 2023 at the
55th Annual Convention of the Association of Although self-directed strategies such as
Philippine Medical Colleges) mindfulness practice help reduce stress, anxiety,
and burnout, systemic factors that lead to such
Burnout among medical faculty has been consequences must also be addressed. (2) Self-
associated with work-life conflict, lack of directed strategies disregard organization-
acknowledgement and appreciation, decreased centric or administration-centric factors that are
number of faculty, inadequate resources, primary drivers of burnout. Framing the issue as
ambiguity about future growth in the academe, a personal problem may push physicians to look
job demands, long working hours, and excessive for solutions that are personally beneficial but
regulation by the government or university. disadvantageous to the organization such as
(10,11,12) Burnout has been closely linked with reducing professional work effort. (13) Providing
personal and professional repercussions among interventions geared towards equipping
physicians. Personal consequences include administration and the faculty with the capacity
broken relationships, alcohol and substance use, to optimize their roles as educators and role
depression, and suicide. Professional models is an example. This strategy will facilitate
repercussions include decreased quality of care a top-down approach aimed at increasing
and increased medical errors, decreased patient medical student wellness. (2) Strategies
satisfaction, decreased productivity and addressing organizational issues have not been
professional effort, and physician turnover. (13) effectively developed because of two main
reasons. First, it is believed that steps geared
Physician burnout has become more towards achieving physician wellbeing will
pronounced during the COVID-19 pandemic. conflict with organizational goals. Second, all
Prior to the pandemic, more than 45% of wellness initiatives are costly. In reality,
physicians were vulnerable to burnout. physician wellness is critical to achieving
Compared to the general population, physicians organizational objectives and many effective
were more likely to experience burnout and to wellness strategies are not cost prohibitive. It is
be dissatisfied with work-life balance. (14) imperative that system-level strategies should
During the pandemic, burnout rate steadily be implemented in order to ensure medical
increased such that in the US, one in five faculty wellness. The Mayo Clinic in the US has
physicians intended to leave practice. (15) What evolved the following nine evidence-based
about academic physicians in particular? organizational strategies to promote physician
wellness: 1) acknowledge and assess problems
A study among Canadian medical faculty related to wellbeing; 2) harness the power of
revealed a burnout rate of almost 76%. Rates leadership; 3) develop and implement targeted
were higher among women and early career interventions; 4) cultivate a sense of community
faculty members, an observation that was also at work; 5) use rewards and incentives wisely; 6)
noted in South Korea. (10, 16) align values and strengthen culture; 7) promote
flexibility and work-life integration; 8) provide
How then can medical schools foster faculty resources to promote resilience and self-care;
engagement in academia while acknowledging and 9) facilitate and fund organizational science.
the challenges and uncertainty of our time? (13)
Experts believe that instituting interventions
that improve physician wellness and reduce Organizations are urged to promote meaningful
burnout have been shown to decrease physician interaction among faculty members and provide
turnover. The mistaken notion that physicians protected time for faculty for their wellness
themselves are solely responsible for burnout activities. (17) The New York University Long
and professional satisfaction lead organizations Island School of Medicine in the US executed a
or administrations to focus on strategies wellness initiative that was created primarily for
17 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
medical faculty. (18) Ultimately, the departments were given the
autonomy to design programs that served them
They formed the Committee for Professional best given the differences among specialties and
Health and Wellbeing that systematically work units. (18)
addressed occupational hazards of burnout.
They invited members who were highly The virtual platform enabled faculty across
passionate and persistent in the field of departments or divisions to conveniently and
wellbeing. In order to develop a multi- effectively share significant life roles and events.
disciplinary approach, this committee created This process was a motivating force for faculty
an Executive Committee that, in turn, crafted a to pursue their academic and personal growth.
wellness ambassador program. This program The committee promoted their own internal
ensured that the wellness initiatives were rolled faculty as keynote speakers in faculty
out departmentally throughout the medical development events. They ensured that their
school. The ambassadors had to participate in wellness initiatives were shaped by locally
50% of committee meetings and document generated data from surveys or studies. For
wellness activities for their departments. The instance, the departmental wellness
ambassadors were also tasked to ensure that ambassadors used the responses to wellness-
their interventions promoted connection with oriented questions from an employee
colleagues and reinvigorated a sense of meaning engagement survey in designing wellness
in work. This committee paved the way for programs. Furthermore, this survey was
sharing and discussing ideas among the various redistributed annually in order to document
departments. The initiatives that were designed change and progress. (18)
by certain departments created a ripple effect
such that other departments replicated wellness The committee provided the following general
strategies that they learned from others. For guidelines for institutions that are looking for
instance, the departments of Obstetrics and ways to reengage their faculty: 1) offer flexible
Gynecology and Surgery implemented an Annual learning environments for faculty development
Wellness Week that focused on different events in order to accommodate different time
emotional, physical, environmental, and mental schedules and geographical locations; 2) provide
components of wellness each day. In order to opportunities that foster conversations about
promote faculty engagement, the departments life roles and hobbies; 3) obtain support from
of Pathology and Obstetrics and Gynecology ran institutional leadership that advocates for
structured annual retreats and social gatherings faculty wellness; 4) organize committees and
that focused on stress reduction and task forces that will promote faculty wellness
mindfulness. In order to promote camaraderie, through departmental activities; and 5) accept
the department of Foundations of Medicine and adapt faculty feedback. The critical need for
conducted monthly department walks (called medical school leadership to make faculty
Infinity walks) at a local park. The department of wellness a priority was consistently highlighted
Radiology implemented a “Wellness Wednesday” by their dean who was highly supportive of their
that comprised of outdoor activities, financial wellness initiatives. (18) Other authors affirmed
planning, and summer socials. The divisions of that harnessing the power of leadership can set
Maternal-Fetal Medicine and Gynecologic the tone of institutional culture and make
Oncology carried out weekly “check ins” and wellness efforts even more effective. (13) This
debriefings during division meetings and an leadership must gradually enact organizational
activity entitled “Three Good Things Exercise.” or system-level changes the impact of which
The department of Pediatrics led a wellness would be felt over time. (5)
activity called “Gratitude Month” that entailed
the posting of thank-you notes at “Appreciation In 2017, a Resident Wellness Consensus Summit
Stations” and “Gratitude Calendar” that involved was inaugurated in the US. Part of this summit’s
hanging daily prompts at workstations. The output was a proposal for an evidence-based
committee also developed structured wellness curriculum that contained modules
educational Wellbeing Grand Rounds that aimed that focus on the spectrum of wellness and
to discuss topics such as work-life balance, burnout. A study showed that running small
resiliency, and mindfulness. In order to group discussions on these topics significantly
encourage participation, faculty members who increased empowerment and work engagement
attended the lectures were granted CME credits. and decreased rates of burnout, emotional
18 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
exhaustion, and depersonalization. This sitting areas, a simple gym area, a
curriculum may also be applicable to medical snack/hydration station, self-care workshops,
faculty. The following topics may be included in and communication and stress management
these wellness initiatives: 1) introduction to trainings. Avenues for psychosocial support
wellness (introduction to physician wellness and include check-ins with each other, group peer
burnout and the wellness curriculum); 2) why support (structured group sharing), and therapy
wellness matters (building awareness on sessions. The faculty must be made aware of
burnout, depression, and mental health issues in such interventions using multiple channels of
medical faculty; wellness is not the absence of communication such as regular emails, fliers
distress); 3) wellness activities of physicians posted in work areas, a wellness website, and
(how physicians stay well through relationships, announcements in team meetings. Ultimately,
religion and spirituality, self-care, work, and these programs must be able to reduce the
approach to life); 4) sleep (education on sleep barriers to accessing wellness services. Studies
hygiene and scheduling); 5) nutrition (education have identified several barriers that include
on the basics of nutrition and how to eat a concerns about confidentiality, stigma and
healthy, balanced diet, particularly for people stoicism, demanding clinical schedules, and
with busy lifestyles); 6) physical fitness identifying therapists experienced in working
(education on the basics and scientifically with physicians. (5,19)
proven benefits of physical fitness, as well as
how to get started on an exercise program); 7) Wellness programs should foster a culture that
financial health (overview of the basics of allows open exchange of ideas and flexibility in
budgeting and living within your means); 8) responding to issues as they emerge. Wellness
mindfulness and reflection (overview of the programs must allow the medical faculty to
concept, scientifically-proven benefits, become an integral part of program policy
unwarranted stigma, and practice of changes and to participate in program
mindfulness for the busy faculty); 9) building improvements. Consequently, wellness
support network (discussion about the programs become more successful and
importance of a support network for the faculty leadership and communication skills are
in promoting wellness and building enhanced among the faculty. The differences in
resiliency);10) physician suicide (education on experiences of the learning environment among
risk factors for depression and suicide specific subgroups of faculty does not permit a singular
for physicians, and how to recognize them in approach to wellness. Understanding such
oneself);11) “I Need Help” (education on how to diversity will guide whatever changes to the
get mental health help for oneself, with a focus learning environment are made. (5, 7, 8, 17, 20)
on systems that ensure confidentiality); 12) The concept of the learning environment (LE) is
wellness in the workplace (discussion about how defined by two main dimensions namely,
individual wellness depends on the supportive psychosocial and socio-material dimensions.
workplace wellness culture). (4) Individual characteristics that contribute to or
respond to the LE, interpersonal interactions,
A wellness program possesses a and institutional policies, culture, and regulation
multidimensional approach that integrates constitute the layers of the psychosocial
individual needs, institutional and cultural dimension. The socio-material dimension defines
barriers to wellness, and systemic issues that how the faculty interacts with the physical and
contribute to stress. (8) At an individual level, virtual worlds that they operate in. (3)
wellness is achieved when the faculty practice Incorporating web-based and other digital
healthy habits on a daily basis allowing a balance resources will contribute to the success of
in the physical, emotional, intellectual, social, wellness programs because this provides the
spiritual, environmental, and occupational faculty and students the opportunity to learn at
aspects of being. their own pace. (9) At present, the relationship
between wellness and LE is not well understood
Activities and strategies throughout the and needs to be studied using high quality
academic year include retreats, mental health research. (3)
leaves, recreational and leisure activities,
exercise, conducive workspaces, retreat zones or As medical education continues to adapt to
quiet spaces with relaxation apps, open air technology and the challenges of a post-
19 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
pandemic landscape, faculty and administration 9. Hategan A, Riddell T. Bridging the gap: Responding to resident
burnout and restoring well-being. Perspect Med Educ. 2020; 9: 117-
will continue to play pivotal roles in student 122. Available from: https://doi.org/10.1007/s40037-020-00567-3
wellness. (2) It is essential that we understand 10. Seo J, Bae H, Kim BJ, Huh S, Ahn YJ, Jung SS, et al. Burnout of
Faculty Members of Medical Schools in Korea. J Korean Med Sci.
the diversity of medical faculty because a one-
2022; 37(9): e74. Available from:
size-fits-all approach to wellness initiatives may https://doi.org/10.3346/jkms.2022.37.e74.
not be effective. (8) Institutions must take into 11. Choudary ZA, Ehsan SB, Ayub A, Farooq HU, Tahir MM. Burnout
among basic sciences faculty: A mixed method research. Pak Armed
account the impact of workplace culture on
Forces Med J. 2022;72(4):1189-1193. DOI:
faculty wellness. By identifying and addressing https://doi.org/10.51253/pafmj.v72i4.7888.
issues arising from day-to-day experiences, 12. Lee RS, Son Hing LS, Gnanakumaran V, Weiss SK, Lero DS,
Hausdorf PA, et al. INSPIRED but tired: How medical faculty’s job
institutional and departmental leaders can help
demands and resources lead to engagement, work-life conflict, and
build faculty resilience. Further research is burnout. Front. Psychol. 2021; 2:609-639. doi:
essential in studying factors that contribute to 10.3389/fpsyg.2021.609639.
13. Shanafelt TD, Noseworthy JH. Executive leadership and
wellness among groups of academic medical physician well-being: Nine organizational strategies to promote
faculty. (1) Ultimately, embedding a culture of engagement and reduce burnout. Mayo Clin Proc. 2017; 92 (1):129-
wellness that is openly and intently supported 146. Available from:
http://dx.doi.org/10.1016/j.mayocp.2016.10.004.
by administration should be a goal of every 14. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et
medical school. al. Pushed to their limits, 1 in 5 physicians intends to leave practice.
JAMA. 2012. Available from:
https://doi.org/10.1001/jama.2022.5074.
In conclusion, academic medical faculty assume 15. Henry TA. Medicine’s Great Resignation? 1 in 5 Doctors Plan Exit
various roles and this predisposes them to in 2 Years. AMA. 2022 Jan18.Available from: https://www.ama-
assn.org/practice-management/physician-health/medicine-s-great-
burnout. In order for a wellness program for
resignation-1-5-doctors-plan-exit-2-years.
medical students to succeed, the faculty should 16. Crist C. Pandemic increased burnout among academic medical
also be recipients of wellness strategies or faculty. Medscape Medical News. 2022 Jun 24. Available from:
https://www.medscape.com/viewarticle/976144
interventions themselves and not just 17. McKinley T. Toward useful interventions for burnout in
implementers of the program. Strategies that academic medical faculty: The case for unit-specific approaches.
Journal of Continuing Education in the Health Professions. 2022
ensure medical faculty wellness should not only
Jan 1; 42(1):e69-e74. DOI: 10.1097/CEH.0000000000000389
be individual-centric but also organization- 18. Savitzky DC, Rekawek P, Shelov S, Nonaillada J. Re-engaging
centric. Finally, no wellness program will faculty during and after a health pandemic: Programmatic
strategies for learning and wellness. The Journal of Faculty
succeed unless the power of leadership is
Development. 2022 Sep 1; 36(3): 87-91.
harnessed. 19. Ey S, Soller M, Moffit M. Protecting the well-being of medical
residents and faculty physicians during the COVID-19 pandemic:
Making the case for accessible, comprehensive wellness resources.
REFERENCES
1. Dandar VM, Grigsby RK, Bunton SA. Burnout among U.S. medical Global Advances in Health and Medicine. 2020 Dec 3;9:
school faculty. Analysis in Brief. 2019; 19: 1. 2164956120973981. doi: 10.1177/2164956120973981. PMID:
2. Klein HJ, McCarthy SM. Student wellness trends and 33329941; PMCID: PMC7720314.
interventions in medical education: A narrative review. 20. Lefebvre D, Dong KA, Dance E, Rosychuk RJ, Yarema M, Blouin
Humanities and Social Sciences Communications. 2022; 9: 92. D, et al. Resident physician wellness curriculum: A study of efficacy
Available from: https://doi.org/10.1057/s41599-022-01105-8. and satisfaction. Cureus. 2019; 11(8): e5314. DOI
3. Gruppen LD, Fogarasi MC. Considerations on conducting 10.7759/cureus.5314
research on wellness in the context of the learning
environment. Global Advances in Health and Medicine. 2021;
10: 1–9. DOI: 10.1177/2164956121989708.
4. Arnold J, Tango J, Walker I, Waranch C, McKamie J, Poonja Z, et
al. (An evidence-based, longitudinal curriculum for resident
physician wellness: The 2017 resident wellness consensus
summit. Western Journal of Emergency Medicine. 2018; 19 (2):
337-341. DOI: 10.5811/westjem.2017.12.36244.
5. Mari S, Rachel Meyen R, Kim B. Resident-led organizational
initiatives to reduce burnout and improve wellness. BMC
Medical Education. 2019;19: 437. Available from:
https://doi.org/10.1186/s12909-019-1756-y.
6. AMA. Preventing burnout in medical residents and fellows: 6
keys for wellness. 2016. Available from: https://wire.ama-
assn.org/education/preventing-burnout-medical-residents-and-
fellows-6-keys-wellness
7. Alkatan HM. Impact of trainers-related factors and “generation
gap” on the quality of local residency training. International
Journal of Current Research. 2015;7(12): 24221-24224.
8. Chaukos D, Zebrowski JP, Benson NM, Celik A, Chad‐Friedman E,
Teitelbaum A, et al, “One size does not fit all” – lessons learned
from a multiple-methods study of a resident wellness curriculum
across sites and specialties. BMC Medical Education. 2021; 21:576.
Avaialble from: https://doi.org/10.1186/s12909-021-02995-z.
20 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP ORIGINAL RESEARCH
PRACTICE AND PERCEPTIONS OF PEDIATRIC RESIDENTS
IN A TERTIARY GOVERNMENT HOSPITAL ON MENTAL
HEALTHCARE AS PART OF GENERAL PRACTICE
CONSTANTINE L. YU CHUA
LORELEI MELANIE K. ELMA
ABSTRACT
OBJECTIVE: This study aimed to describe mental health practice patterns, perceptions,
perceived responsibility, confidence, barriers, and supports of pediatric residents in a tertiary
government hospital to arrive at recommendations in enhancing their mental health
competencies.
METHODOLOGY: As part of needs and baseline assessment within an existing collaboration,
written self-administered questionnaires were distributed among pediatric residents of the
hospital. Frequency of answers were tallied to see clustering and trends. RESULTS: Most of the
37 Pediatric residents had positive perceptions i.e. 78.83% - 83.78% and planned to incorporate
all aspects mental healthcare in their future practice as consultants i.e. 89.19 %- 97.29 %.
However, they did not get to practice or apply it as much during training. All respondents
perceived that diagnosing the neurodevelopmental disorders of Autism Spectrum, Attention
Deficit and Hyperactivity, Intellectual Disability and Learning was their responsibility. When it
came to confidence in diagnosing other psychiatric disorders less than half to 3/5 (45.9%-
64/9%) were confident or very confident in doing so. Approximately three fifths (56.75%
-67.56%) of them were confident in managing neurodevelopmental disorders. There was an even
lower proportion i.e. one fourth (16.21% - 32.43%) of pediatric residents who were confident in
managing other psychiatric disorders. Time was the most often perceived barrier while more
exposure and training were the supportive factors for integrating mental healthcare into
practice.
CONCLUSION: With such positive perceptions already in place, programs to improve knowledge
and skills can be developed to increase confidence, focusing on diagnosing and managing
psychiatric conditions. Target areas as guided by this research can be on how to use screening
tools and psychotropics, diagnosing anxiety and behavioral addictions, and managing psychosis
and trauma. These should be incorporated in a time-efficient manner into usual patient
interviews. Training and added exposure can be utilized in the short-term as well as
institutionalization of collaboration, liaison, and feedback systems in the future.
KEYWORDS: Pediatric Residents, primary mental healthcare, mental health competency
21 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
INTRODUCTION -lems being more pressing. (5) A “referral
mindset” predominates, which may be affected
Integrating mental health (MH) into pediatric by perceptions, perceived responsibility,
practice is seen as an effective way to maximize confidence, barriers, and supports.
access, especially in developing countries. This
utilizes the pediatricians’ long-standing In the Philippines and among Filipino
relationship with the patient and family, as well respondents that also include trainees, a 1994
as the family-friendly nature of their practice. It study by Manapat and Ramos-Leynes showed
is more cost effective and has been linked with that in a local tertiary children’s hospital, none
better outcomes compared to a tertiary care of the pediatric residents and consultants would
model alone. (1) Among child and adolescent ignore various emotional or behavioral
populations, pediatricians are considered the complaints in consultations and very few would
gatekeepers of care and current trends have opt to just observe. However, few would opt to
shown the expansion of their roles to include the manage independently as well. Majority would
MH dimension. (2) This is especially important in “handle and refer” cases like bedwetting beyond
the Philippines where there are very few child five years, poor school performance,
and adolescent psychiatrists to address a nervousness or fearfulness, and school phobia.
growing “mental health crisis” in the youth. The On the other hand, problems like psychotic
recently enacted National Mental Health Law (3) behavior, drug abuse or dependence, stealing,
articulates MH as part of primary care. and truancy would be “referred immediately”.
Collectively, the study showed that in this
In the Western setting, pediatricians were asked population of Filipino pediatricians, the model
in a survey by the American Academy of was to “handle and refer” or “refer immediately”
Pediatrics (AAP) regarding their perceived for emotional and behavioral concerns and not
responsibility to identify, manage, and refer be the primary care provider. (6) This parallels
various MH conditions. More than 80% of the American practice patterns in 2008 where
surveyed pediatric consultants believed they primary care pediatricians (PCP) and also child
should identify ADHD, depression, behavior psychiatrists believe that PCPs should identify
management problems, anxiety disorder, and refer but not necessarily treat children with
substance abuse, and eating disorders. However, MH concerns. (7)
while 70% believed they should manage ADHD,
which approximately coincided with the rate of While the “referral model” has understandable
perceived responsibility for its identification, basis, it is important to note that not all areas in
only around 30% or less believed they should the Philippines have access to child and
manage the other abovementioned concerns. adolescent psychiatrists for referral. Moreover,
Around 80% believed instead that they should pediatricians have a big opportunity for
just refer for those. (4) The discrepancy between promotive and preventive interventions not
ADHD and the other disorders was not explained available to psychiatrists who usually see
but may perhaps be due to pediatricians’ patients already needing treatment. Effective
discomfort with matters that have strong socio- referral is also not a singular step but also
emotional components and are traditionally assumes that the pediatrician is adept in
labeled as part of psychiatry and psychology. identifying a MH concern, explaining it to the
patient and family, forming a trusting
In another study also by the AAP, only 13% of therapeutic relationship with them, and
general pediatricians felt confident overall in performing psychoeducation and supportive
their capability to manage depression. Almost maneuvers. This is especially true where MH
80% recalled referral to a MH professional as stigma is rampant.
their “management” in their most recent case of
depression. In the AAP study, the greatest What supports the engagement of pediatricians
perceived barriers were inadequate time to in MH? It was found by the AAP that those who
provide counseling and conduct adequate completed at least four weeks of
history, plus inadequate training. Other factors developmental-behavioral pediatrics training
implicated included: insurance and financial had 1.8 times increased odds of co-management
issues, authorization and paperwork problems, and those who had prior MH training had 1.4
patient or parent reluctance, or medical prob- times increased odds.
22 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
The factor which mattered most was the simple the study could also guide pediatric residency
fact of having strong interest in the subject program of other hospitals in the future in colla-
matter, which led to an increase of 2.75 times. (8) boration with the professional societies in-
volved.
This highlights that both training and personal
factors such as interest or personality of the METHODOLOGY
physician influence their willingness to tackle Participants / Methods for Selection
MH issues of their patients. Related to this,
another area of effort was not just to integrate The study involved pediatric residents of UP-
MH practice in pediatrics but to increase PGH, from first to third year level, who were
pediatricians who themselves were MH recruited by the principal investigator during
practitioners. In the United States, the “Post their weekly conferences via convenience
Pediatric Portal Project” is a program which sampling. This was permitted as part of the
enables pediatricians to train and be licensed in existing collaborative program between Pedia-
general psychiatry and child & adolescent trics and Psychiatry to improve MH com-
psychiatry within a span of three years as a petencies among pediatric residents. Within May
fellowship program. (9) No such program exists to July 2019, a total of 37 out of a total of
in the Philippines as of now, but this could very seventy residents were recruited – those were
well be a way of increasing pediatricians who present in the conference. Collection was done
could manage psychiatric disorders. in three conferences (once per month) to reach
those who did not attend before. However, not
Have MH practice patterns in pediatrics changed all residents were able to answer despite this
in the Filipino setting after nearly thirty years? effort due to leaves or duties in critical posts.
What are the factors that influence this? In the Sample size was not computed. As the study was
current Filipino context, it is hypothesized that within the context of a program, the goal was to
perceived responsibility and confidence levels collect data from as many residents as possible
may be lower than Western counterparts but at the same time without disrupting their
because standardized MH integration in work. All residents who were present were in-
pediatric residency curricula has not yet been cluded but medical interns, rotators from other
established. Variations in workload, culture, and institutions, and fellows already in subspecialty
education may also cause practice patterns to training were excluded.
differ.
Data Collection
The primary objective of this study was to
describe the baseline practice and perceptions The study followed a cross-sectional, descriptive
of pediatric residents at the University of the design. A written questionnaire was formulated
Philippines-Philippine General Hospital (UP- based on the review of literature, which included
PGH) on MH practice. The focus on residents various factors that would influence the MH
was given that practice and perceptions as practice of pediatricians. This was expanded and
consultants may be rooted and modified during modified based on focus group discussions with
formative years in residency training and it may the pediatric residency training officer, chief
be valuable to focus on this stage. Specific resident of pediatrics, head of the division of
objectives are to describe the following among child psychiatry, and chief fellow of child psy-
pediatric residents: 1) MH practice patterns and chiatry. The questionnaire, phrased in English,
plans; 2) perceptions about MH practice; 3) which is the standard language of education and
perceived responsibility in diagnosing and training in the country, was directly admi-
treating various psychiatric conditions; 4) nistered. No validation study was done as it was
confidence in diagnosing and treating various done in the context of guiding a time-bound
psychiatric conditions; and 5) perceived barriers program. It was divided into five parts, as
and supports in integrating MH into pediatric follows. Part one included questions on patterns
practice. The study was done in the context of for current MH practice as a resident and for
gathering data to guide a capacity building planned clinical engagement as a consultant.
program in MH between the UP-PGH Pediatrics Part two included questions on perceptions
and Child and Adolescent Psychiatry regarding MH practice in pediatrics. Part three
departments. Beyond the program, it is hoped included questions on perceived responsibility
23 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
in diagnosing and managing specific conditions RESULTS
as a pediatrician. Part four included questions Demographic data
on confidence in diagnosing and managing
specific conditions as a pediatrician. These were There was a total of 37 pediatric residents. Most
all in the form of Likert scales corresponding to (29 or 78.38%) of them were female. The mean
the degree of frequency or agreement to age was 28.3 years old. The respondents were
statements. Part five included two open-ended distributed relatively equally among the year
questions on problems encountered and levels: 11 first-years, 10 second-years, and 16
possible supports when it comes to MH third-years. Around one-third (62.16%) of them
integration in practice. (Appendix 1) graduated from the medical school partnered
with the study hospital (UP-PGH). Undergrad-
Data Analysis uate courses taken were: biology (28.73%),
seven-year direct MD program (13.51%), nursing
Percentages of total answers per choice of each (13.51%), psychology (13.51%), other allied
item, calculated using Microsoft Excel, were health courses (8.1%), and others/did not specify
presented for parts 1 to 4. For part 5, common (21.62%).
answers were grouped together by themes and
tallied. Approximately half had their rotation in the var-
This was a purely descriptive study and no -ious MH-related rotations: child protection unit
statistical correlations were analyzed. (48.65%), developmental pediatrics (54.05%),
and adolescent medicine (48.65%). Notably,
Ethical Considerations these rotations were randomly assigned at any
year level. Due to time constraints, not all
The study was approved by the institution’s residents were able to go through all three ro-
research ethics board, part of which required tations within the duration of their training.
that researchers have undergone good clinical
practice training. Participants underwent due Practice Patterns of Pediatric Residents & Future
informed consent process with their confi- Clinical Practice
dentiality upheld in all steps of the process.
Joining the study did not impact participation in Majority of residents (greater than 75%) would
the abovementioned competency building explore and detect MH concerns, discuss MH
workshop in any manner. There were no promotion or prevention, diagnose specific psy-
conflicts of interest that required disclosure. chiatric conditions, and perform counseling so-
Results were presented as a whole without indi- metimes, often, or almost always in their cur-
vidual or sub-group identifying data to the De- rent clinical engagements. On the other hand,
partment of Pediatrics as part of the colla- many residents (greater than 50%) would almost
boration.
24 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
never handle basic MH cases on their own. Highlighting an example of a discrepancy
(Table 1). In contrast to their residency practice between current practice in training and future
patterns, most of the participants planned to plan, 56.76% planned to initiate psychotropics
conduct all aspects of mental healthcare often or almost always as future consultants,
sometimes, often, or always as future while only 5.12% actually did so during their
consultants – even the use of screening tools residency. (Table 2)
(97.29%), initiation of psychotropics (89.19%),
and independently handling MH cases (91.9%). Perceptions on Mental Health Practice
This indicated that most of them plan to
integrate mental healthcare in their practice, Results revealed that pediatric residents had a
even if they did not do it as much when they positive overall perception toward MH practice.
were residents.
25 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
As pediatricians-in-training, majority (83.78%) However, it was notable that around one fourth
felt that patients were open to discuss and (24.32%) believed that medical concerns are
78.38% would take MH directives. Many (81.08%) more pressing than MH concerns and another
were interested in psychiatry as a topic and one fourth (27.03% were ambivalent. Around
86.49% were interested in MH concerns of their one-third (35,84%) also believed that their role
patients. Most (83.78%) of them agreed that as pediatrician was more for medical than MH
dealing with MH problems would be adequately concerns. (Table 3) Pediatric residents all
reimbursed. Notably, all of the respondents wanted to have a MH clinic as part of the
agreed that psychosocial concerns have an pediatric services in the hospital.
impact on health.
26 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Generally, 86.48% expressed willingness to There was more hesitation with regard
rotate in child and adolescent psychiatry. All the conditions that were “traditionally psychiatric”;
respondents felt that the child protection unit given answers of “undecided” and even “not
rotation and 94.4% said that their rotation in responsible” for cases such as depression (8.1%),
adolescent medicine helped them integrate MH anxiety (10.8%), psychosis (18.9%), conduct
in their pediatric rotations. To a significant but disorders (10.8%), and trauma (10.8%);
lesser extent (69%), developmental pediatrics nonetheless, for these conditions, still a great
rotation was also seen to be helpful. The majority (80% or more) felt they should be able
discrepancy in developmental pediatrics may to diagnose. (Table 5)
reflect mindsets about development being a
separate construct from MH. (Table 4) For neurodevelopmental disorders, a significant
majority of residents felt the perceived
For around half of respondents (48.65%), responsibility to manage, ranging from 86.49%
premedical studies helped them in MH aspects to 89.19%, which corresponds well to the 100%
of pediatric care while 64.87% mentioned that it perceived responsibility to diagnose those
was in medical school that they learned to disorders. This was not the case for the
attend to mental health of patients. This showed psychiatric disorders. Less respondents felt
a possibility that not all pediatric residents were responsible to manage, ranging from 56.76% to
equipped in addressing mental health concerns. 78.38%, despite a lot of them feeling responsible
Around one-third (37.84%) of respondents to diagnose (above 80%). On the other hand,
expressed some interest in possibly specializing only 67.56% felt responsible for diagnosing
in child and adolescent psychiatry if there was anxiety and 56.75% felt the same about
such a program from a background of pediatrics. diagnosing psychosis. This downward drift
(Table 4) possibly illustrates where the “referral mindset”
starts to manifest. (Table 6)
Perceived Responsibilities
Confidence in Mental Health Practice
All respondents perceived that diagnosing the
neurodevelopmental disorders (ASD, ADHD, ID, Similar to the pattern in perceived
and LD) was their responsibility. Almost all responsibility, there was greater confidence in
perceived diagnosing substance use problems the diagnosis of neurodevelopmental disorders,
(94.59%) and behavioral addictions (91.88%) to wherein 78.4%-89.2% reported being confident
also be their responsibility. or very confident. In contrast, only approximate-
27 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
-ly half (45.9%- 64.9%) of respondents were Barriers and supports
confident in diagnosing the other psychiatric For the questions regarding barriers and
conditions. The least number of residents were supports, these were open-ended questions to
confident in diagnosing behavioral addictions which not all respondents answered. There were
(45.9%) and anxiety (48.6%). (Table 7) answers which recurred in many answered
questionnaires. The greatest perceived barrier
Approximately three-fifths (56.75 % to 67.56%) to practicing MH in pediatric residency was the
of pediatric residents were confident or very lack of time (13/ 33 respondents or 39.39%). Lack
confident in managing the neurodevelopmental of training was the second biggest barrier (8/ 33
disorders. On the other hand, only around one- respondents or 24.24%). The lack of space or
fourth were confident or very confident in venue was also identified as a barrier (3 /33
managing depression, (24.32%), anxiety (29.73%), respondents or 9.09%). This may point to issues
substance problems (29.73%), and behavioral about conduciveness of environment and
addictions (24.32%). The least number of privacy. The “referral mindset” was also
respondents were confident in managing mentioned, wherein the accessibility of
psychosis (16.21%) and traumatic disorders psychiatry services led residents to just refer
(21.62%), where the approximate ratio falls to and focus their efforts on medical illnesses.
approximately one out of five. This may possibly (Table 9)
reflect their perceived complexity or risk with
these conditions or stricter delegation of these The most relevant support was to have more
as purely within psychiatry. For psychosis, this training or education opportunities in MH, as
may also correlate with the lack of experience in identified by 12 respondents (36.36%). This may
using psychotropics as seen earlier in practice be related to the lack of training mentioned
patterns. (Table 8) earlier. More exposure was the next most
frequent suggestion (9 respondents), followed by These reflect a concern that their pediatric
having more time (3 respondents) and even having residency training might not be adequately
a child and adolescent psychiatry rotation (3 preparing them for something they actually
respondents). (Table 10) consider as important and hope to get involved
with in their future clinical practice. It was noted
DISCUSSION that the questionnaire did not ask if the
The study was able to highlight important gaps or participant planned to take further training or a
discrepancies. First, there were positive fellowship program related to MH to close the
perceptions about MH with residents planning to gap. Requiring fellowship to achieve MH
integrate mental health care as consultants, but competency seems counterintuitive to the
there was hardly any chance to so during pediatric concept of primary care integration. Residents
residency. Second, many recognized that felt responsible and confident in diagnosing but
diagnosing and treating MH problems was their not so much in managing psychiatric conditions,
responsibility, but were not so confident in doing which may reflect that their training may have
so. focused only on detection of such illnesses
28 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
rather than on treatment. The “handle and refer” helpful, akin to the HEADSSS (Home, Education,
or “refer immediately” mindset parallel to the Activities, Drugs, Suicidality, Sexuality, and
Manapat and Ramos-Leynes study done in Safety) in adolescents. The utility of cascading it
another Filipino tertiary hospital almost thirty down to the level of medical students, similar to
years ago in 1994 can be gleaned from this. (6) the adolescent interview, was also emphasized.
This agrees with literature that integrating MH in
pediatrics requires exposure in medical school
and residency, as well as the availability of back-
up and consultation from child and adolescent
psychiatry. (10)
It is also significant to note that only around
two-thirds of the pediatric residents felt that
medical school helped them with the MH
dimension of clinical practice, so there is still
much to be improved in the medical curriculum.
The advantage of this would be that MH would
become part of primary care, rather than “yet
another subspecialty” that pediatric trainees
must learn in addition to their myriad of
rotations. This strengthens views that MH is part
of primary pediatric care. For interventions, it
was discussed that it may be more practical to
start application of MH practice into special
populations integrally encountered in various
Given the results in perceptions, one possible
subspecialties such as abused children,
contributor to this includes role confusion –
chronically ill children, emergency consults for
should they prioritize physical or MH? This
suicide attempts, and in the adolescent clinic.
conceptual divide may be influenced first by the
high workload that limits time. Second is the
Although not necessarily a long-term solution,
presence of dedicated MH service (i.e.,
workshops were also deemed feasible at this
psychiatry) in the current hospital setting that
time, strengthening the hands-on application of
makes referral more practical and perhaps the
clinical skills in handling patients with
pressure to avoid overlaps and infringements in
psychiatric conditions as well as mechanisms for
roles.
feedback from psychiatry. Ideally these
programs can be integrated in the clinics. In the
On the more positive side, the results reflect
US, one model involved hiring a dually-trained
that efforts to integrate MH in pediatric practice
pediatrician and child psychiatrist who initially
are likely to be perceived as relevant and fruitful
educated the pediatricians, performed patient
by the residents should it be established. There
consultations with them in a once-every-two-
is no need to work from the very bottom to
weeks MH clinic, and eventually allowed the
address misconception and resistances
pediatricians to do the consultations alone while
anymore, and institutional efforts are not likely
being available for questions as needed. This
to be left ignored. The residents may benefit
yielded to 11% to 37% increase in MH diagnoses
from capacity building in MH practice. Results
made by pediatricians. (11)
show that many are open to having avenues of
learning and practicing, but also, that it is
There are however no programs that train such
difficult to find additional time. A balance has to
dually-trained specialists in the Philippines.
be created between providing experience
Another model used standard patient
without further adding to their workload.
encounters with trained actors who simulated
behavioral concerns, which were simultaneously
Drawing from the information generated from
interviewed by pediatric trainees and behavioral
the focused group discussions surrounding the
health trainees, to facilitate exposure to and
capacity building program, making MH a
exchange of differing techniques. This was also
convenient part of the usual consult may be
found to improve awareness of behavioral
29 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
health resources, confidence in using screening 1. Knowledge and skills regarding diagnosing
tools, and willingness to adjust future practice and managing non-neurodevelopmental
orientations. (12) Such methods of learning psychiatric conditions can be enhanced
through actual clinical experience could guide through various means, with emphasis on
future MH capacity building efforts. going beyond detection as a point of
emphasis.
In the focused group discussions, it was 2. The following can be focused on in training,
discussed that there were no MH competencies as they attained the lowest ratings: using
articulated in the professional association of screening tools, basic psychotropic
pediatricians as of now. Also, it was not yet part prescription, diagnosing anxiety and
of the residency curriculum of the hospital, but behavioral addictions, and managing
rather incorporated in relevant rotations. psychosis and trauma.
Moving forward, these efforts can ideally be 3. Mental health can be incorporated in routine
institutionalized by professional policy for health interviews in a time-efficient manner
uniformity, sustainability, and continuity. as time constraint was the most common
limiting factor. This can be initiated earlier in
Limitations and Recommendations general medical education.
4. Child protection and adolescent medicine
The limitations of the study were that rotations for all pediatric residents can be
convenience sampling was used and the turn- maximized as they were deemed very helpful
out was only around 50%. There may have been in learning MH. A child and adolescent
selection bias in such that participants were psychiatry rotation can be offered for those
those who were more inclined toward MH who are interested.
practice. Results may also not be directly 5. A capacity building project for MH practice
applicable to other pediatric residency can be initiated since more training was most
programs in the country; the unique factors of identified as a possible support.
the hospital of study were the availability of 6. Further collaborations beyond workshops
child psychiatry services, being a major and seminars such as having a shared
subspecialty referral center, and its location in pediatric MH clinic and integrating principles
the urban center. Findings are expected to of mental health in pediatric training
change in non-specialty rural hospitals without curricula.
proximate access to child psychiatry services. It
REFERENCES
is recommended that the study be expanded to
1. De Maeseneer J, Moosa S, Pongsupap Y, Kaufman A. Primary
multiple centers in the Philippines, using formal
healthcare in a changing world. British Journal of General
sampling methodology and validated Practice, 2008 Nov; 58 (556): 806-809, i-ii. doi:
instruments. 10.3399/bjgp08X342697. PMID: 19000405; PMCID:
PMC2573981.
2. Foy JM, Green CM, Earis MF. Mental health competencies for
Future studies can also go beyond descriptive pediatric practice. American Academy of Pediatrics. 2019;
methodology by comparing changes pre- and 144 (5): 1-16.
post- intervention (e.g., a workshop or liaison 3. Congress of the Philippines. 17th Congress. 2nd Regular
Session. Begun and held 24, 2017. Metro Manila, Republic of
program) using statistical analysis. Factors that
the Philippines. RA 11036. Available from:
increase or decrease actual engagement or legacy.senate.gov.ph/republic_acts/ra%2011036.pdf
outcomes like psychiatric diagnoses, 4. Stein REK, Horwitz SM, Storfer-Isser A, Heneghan A, Olson L,
psychotropic prescription, and the like could Hoagwodd KE. Do pediatricians think they are responsible
for identification and management of child mental health
then be determined and explored. problems? Results of the AAP periodic survey. Ambulatory
pediatrics.2008; 8 (1):11-17.
5. Olson AL, Kelleher KJ, Kemper KJ, Zuckerman BS, Hammond
CS, Dietrich AJ. Primary care pediatricians’ roles and
Therefore, for the hospital of study, the
perceived responsibilities in the identification and
collaboration may go directly to knowledge and management of depression in children and adolescents.
skills enhancement, rather than focusing on Ambulatory Pediatrics. 2001 Mar-Apr; 1 (2): 91-98. doi:
baseline attitudes. To close the gap and bridge 10.1367/1539-4409(2001)001<0091:pcprap>2.0.co;2. PMID:
11888379.
the above discrepancy, specific
recommendations can include the following:
30 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
6. Manapat RC, Ramos-Leynes MCJ. Attitudes of pediatricians at
the Philippine Children’s Medical Center towards psychiatric
problems of children and adolescents. Philippine Journal of
Psychiatry. 1994; 18 (3): 49-54.
7. Heneghan M, Garner AS, Storfer-Isser A, Kortepeter K, Stein R,
Horwitz SM. Pediatricians’ role in providing mental health care
for children and adolescents: Do pediatricians and child and
adolescent psychiatrists agree? Journal of Developmental and
Behavioral Pediatrics. 2008; 29 (4): 262-269.
8. Green C, Storfer-Isser A, Stein REK, Garner AS, Kerker BD,
Szilagyi M, et al. Which pediatricians comanage mental health
conditions. Academic Pediatrics, 2017. 17 (5): 479-486.
9. Ellis R Jr, Anderson AK. Pilot program trains pediatricians in
child and adolescent psychiatry. American Academy of
Pediatrics News. 2010 Nov; 31 (11): 31. Available from:
https://publications.aap.org/aapnews/issue/31/11
10. Gabel S. The integration of mental health into pediatric
practice: Pediatricians and child and adolescent psychiatrists
working together in new models of care. The Journal of
Pediatrics. 2010; 157 (5): 848-851.
11. Goodfriend M, Bryant T 3rd, Livingood W, Goldhagen J. A
model for training pediatricians to expand mental health
services in the community practice setting. Clinical Pediatrics.
2006 Sep; 45 (7): 649-654. doi: 10.1177/0009922806291018.
PMID: 16928843.
12. Jee SH, Baldwin C, Dadiz R, Jones M, Alpert-Gillis R.
Integrated mental health training for pediatric and psychology
trainees using standardized patient encounters. Academic
Pediatrics. 2018 Jan-Feb; 18 (1): 119-121. doi:
10.1016/j.acap.2017.06.014. Epub 2017 Jul 15. PMID: 28716560
31 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP ORIGINAL RESEARCH
A CROSS-SECTIONAL STUDY ON THE PREVALENCE AND
SEVERITY OF SUICIDAL IDEATIONS AND BEHAVIORS OF SENIOR
HIGH SCHOOL STUDENTS USING THE COLUMBIA-SUICIDE
SEVERITY RATING SCALE (C-SSRS)
JOHN MICHAEL L. REYES, MD
ABSTRACT
OBJECTIVES: In the light of increased suicide risk among adolescents, this research aimed at determining
the prevalence and severity of suicidal ideations and behaviors of senior high school students in a public
secondary school in Metro Manila using the Columbia-Suicide Severity Rating Scale (C-SSRS).
METHODOLOGY: This is a descriptive cross-sectional school-based study, conducted on 236 senior high
school students, 18 years old and above, in San Juan National High School (SJNHS) in San Juan, Metro
Manila. The study employed convenience sampling. Upon selection, the C-SSRS was administered. Data
on four constructs of suicide were gathered: 1) suicidal ideation severity; 2) intensity, which was
quantified in terms of frequency, duration, control, deterrents and reasons for suicidal ideation; 3)
suicidal behavior rated on a nominal subscale as actual, aborted, interrupted, preparatory behavior and
non-suicidal injurious behavior; and lastly 4) lethality of actual suicide attempts on a 6-point ordinal scale,
and if actual lethality was zero, potential lethality was further rated on a 3-point ordinal scale.
RESULTS: The majority (67.8%) had mild suicidal ideations; 37.71% had active suicidal ideations with intent
but not necessarily a specific plan and only 13.98% had active suicidal ideation with intent to act and a
specific plan. The intensity of suicidal ideation was not that frequent in 35.59% of the respondents
i.e.18.64% 1x/ week and 16.95% less than 1x/ week. About a third (30.07%) had very short duration of
suicidal ideations i.e. fleetingly (19.92%) or less than an hour/ day (11.02%). A third (32.62%) were able to
easily control (18.64%) or control with minimal difficulty (13.98%). Reason for suicidal ideation were either
to get attention (10.59%) or to end the emotional pain (11.02%). A third (30.93%) had actual attempts
(15.25%) and Non -Suicidal Self Injury (NSSI) (15.68%); while another 35.06 % had interrupted (16.53%) or
aborted (19.07%) attempts. Those who had actual attempts, 41.67% had no physical injury while 50 %
incurred minor injuries. Thirty- two (88.89%) had suicidal attempt that was likely to result in injury but not
likely to cause death.
CONCLUSION: In light of these relatively high prevalence rates for suicidal ideation and behaviors, school-
wide intervention on education or awareness programs, gatekeeper training, peer leadership, skills
training and screening or assessment may have to be instituted to curb the increased suicide risk of the
senior high school students and further prevent suicide attempts.
KEYWORDS: Prevalence, Suicidal Ideations, Suicidal Behavior, High School Students, Columbia- Suicide
Severity Rating Scale (C-SSRS)
33 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
INTRODUCTION increased incidence of depression and suicidal
Background of the Study behavior. (7)
According to the World Health Organization In light of the increased risk and trend of suicide
Global Estimates, among the people ages 10-29 among adolescents (8) this study aimed to
years old, 27% had committed suicide. 27% of determine the prevalence and severity of
suicides were attempted by adolescents (10-19 suicidal ideations and behaviors among senior
years old). (1) Suicide was the second leading high school students using the Columbia-Suicide
cause of death among young people aged 15-29 Severity Rating Scale (C-SSRS) in San Juan
globally. (2) In the Western Pacific Region, National High School, in San Juan, Metro Manila.
suicide was also the second leading cause of
death among young people aged 15-29, eclipsed METHODOLOGY
only by road accidents. Study Design
This is a descriptive cross-sectional school-
In the Philippine setting, a time-trend study based study, conducted on 236 senior high
showed that rates of suicide peaked at the age school students, 18 to 20 years old, in San Juan
range of 15-24. In a study in 2000, exploring the National High School (SJNHS) in San Juan, Metro
trend of suicide rates among adolescents and Manila. Permission to conduct the research in
young adults in the United States, it was found SJNHS was granted by the Assistant Schools
out that adolescents 15 to 19 years old had a Division Superintendent.
suicide rate of 8 per 100 000, with no change in
trend from 2000 to 2007. However, an Sampling
increasing trend from 2007 to 2014 was noted The study employed convenience sampling,
with an annual percentage change (APC) of 3.1% recruiting 236 participants from San Juan
followed by a steep uptrend from 2014 to 2017, National High School (SJNHS) in San Juan in
with an APC of 10.0%. (3) The father of child and Metro Manila, who fulfilled the inclusion and
adolescent psychiatry in the Philippines, Dr. exclusion criteria of the study as follows:
Cornelio Banaag has sounded the alarm that
young Filipinos are in the midst of a mental Inclusion criteria: Subjects aged 18 to 20 years
health crisis. (4) enrolled in senior high school in a public
secondary school in San Juan, Metro Manila,
It is projected by the Philippine Statistics who expressed willingness and gave consent to
Authority that adolescents (10-19) will comprise participate in the study.
19% of the Philippines by year 2020. (5)
Adolescents can be vulnerable since they are in Exclusion criteria: Inability to understand English
one of the most rapid and formative phases of or Filipino; students with diagnoses of
human development with distinct physical, intellectual disability, previously diagnosed with
cognitive, social, emotional and sexual a psychiatric condition or any condition that
development, simultaneously occurring during would preclude a participant from answering the
this phase, it is also characterized by a widening questionnaire.
gap between biological maturity and social
transition to adulthood accompanied by an The minimum required sample size was 216
emerging need for autonomy yet still requiring based on the 17% prevalence of suicidal
adult supervision and guidance. (6) ideations in the youth (9), a level of confidence
of 95% and a margin of error of 5%.
In Erik Erikson’s Eight Stages of Psychosocial
Development he states that adolescents had the Instrument
task of Identity vs Role Confusion. This is the Permission was obtained from the Columbia
stage wherein a sense of self is developed by Lighthouse Project to use the Columbia Suicide
testing roles then integrating these roles to form Severity Rating Scale (C-SSRS) Tagalog version.
a sense of identity. Social and environmental The translation and linguistic validation to
factors also play a role, such as bullying, Tagalog was carried out by Fernandez et al. (10)
impaired parent-child relationship, living outside
of the home, getting out of school, social Training in the use of the C-SSRS was done by
isolation, romantic difficulties. (6) Therefore, watching a prerecorded 20 -minute educational
adolescence can also be accompanied by an course offered by the Columbia Lighthouse
34 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Project. A certificate of learning was obtained. They were given instructions on how to answer
The CSSRS was designed to provide definitions the C-SSRS. Participants were then screened
of suicidal ideation and behavior and non- using the inclusion and exclusion criteria cited
suicidal self-injurious behavior and above. Upon selection, consent from the
corresponding probes; to quantify the full participants was obtained for the study.
spectrum of suicidal ideation and suicidal Thereafter, the researcher administered the
behavior and gauge their severity over specified CSRSS to the students with advanced
periods. The CSSRS also distinguished suicidal coordination with the principal and teachers of
behavior and non-suicidal self-injurious SJNHS. A room for the one -on- one data
behavior. (11) collection was provided and the administration
took only about 3 – 5 minutes per subject.
Demographic information: such as age, sex, and
The C-SSRS dwells on the four constructs of
educational attainment were obtained. Names
suicide. The first is on severity, rated on a 5-
and Contact details were taken for appropriate
point ordinal scale wherein 1 = wish to be dead, 2
referral to the OPD telepsychiatry service for
= non-specific active suicidal thoughts, 3 =
those who scored high on the severity of suicide
suicidal thoughts with methods, 4 = suicidal
risk.
intent, and 5 = suicidal intent with plan. Second
construct is on intensity, which has 5 items that
Statistical Analysis
are each rated on a 5- point ordinal scale:
frequency, duration, controllability, deterrents
Suicidal ideation was separated into a 5 -point
and reason for ideation. The third is on behavior,
ordinal severity scale in which 1=wish to be
rated on a nominal subscale: actual, aborted, dead, 2=nonspecific active suicidal thoughts,
interrupted, preparatory behavior and non- 3=suicidal thoughts with methods, 4=suicidal
suicidal injurious behavior. The fourth is the intent, and 5=suicidal intent with plan. Previous
lethality subscale, which assesses actual studies predicting suicide attempts showed that
attempts; actual lethality rated on a 6-point severity increased relative to method, intent,
ordinal scale, and if actual lethality is zero, and plan, respectively. (11) For the intensity of
potential lethality is rated on a 3-point ordinal suicidal ideation, a 5 -point ordinal severity scale
scale. The assessment of lethality is done by the was used. The suicide risk was greater when
assessor. (11) thoughts were more frequent, of longer
duration, less controllable, fewer deterrents and
As for the validity and reliability, in a study by if stopping the pain was the reason. (14)
Posner et al (11), the internal consistency of the
intensity subscale was high, with a Cronbach’s For suicidal behaviors, interrupted attempts,
alpha of 0.937 for the last visit and 0.946 for the aborted attempts and preparatory behavior
past week. In the C-SSRS compilation of were equally predictive of an attempt, and those
supporting evidence, a study of the with multiple behaviors had greater risk. Non-
psychometric properties of the CSSRS (12), the suicidal self -injury was associated with suicidal
inter-rater reliability for the most severe thoughts that also increased the risk for suicide.
ideation scores in the last month and lifetime (15) For the lethality, suicidal intent correlated
were good (Lifetime Cohen’s kappa at 0.91 and highly with medical lethality when the attempter
recent Cohen’s kappa at 0.76). (13) had sufficient knowledge to assess properly the
probable outcome of his/her attempt.
Data Collection
Descriptive measures such as frequencies and
Due to the large sample size needed for senior proportions were applied for all the data
obtained in the research.
high school students, and the proximity of
SJNHS, it was chosen to be the school where the
This study was limited since it was administered
study was conducted. The setting for
in only one national high school, hence no
administering the questionnaires was in their
generalizations were made on the findings of this
classrooms during their vacant periods in the
study. The study was also limited by the age
afternoon. Students who were present in certain
group since most of the participants were
classrooms were chosen as participants, and
mostly in their late adolescence.
once with their consent, they were given a brief
backgrounder on what the study was and what it
aimed to find out.
35 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Ethical Considerations Follow up assessment of suicide severity was
The study protocol was reviewed and approved done using the CSSRS.
by the Research Institute of Health Science
(RIHS) Ethics Review Committee of the There were no monetary costs in participating in
University of the East – Ramon Magsaysay this study. Likewise, no monetary nor material
Memorial Medical Center Inc. (UERMMCI) in benefits were gained in participating. The only
Quezon City. benefit that the participants received was to get
an earlier referral to a psychiatrist if they had
Informed consent was obtained for all suicidal ideations or behaviors. The findings
participants to be included in this study. They from this study will be shared with SJNHS.
were allowed to withdraw from the study at any
RESULTS
point in time if they preferred to do so. A brief
background and explanation of the purpose of
A total of 236 senior high school students
the study was done to ensure that they were
grade11 and 12, aged 18-19 years old consented
able to understand the objectives of the
to participate and were administered the
research. The risk and benefits of participation
Columbia Suicide Severity Rating Scale. The
were also explained. The researcher had no
majority were 18 -year -olds but grade level and
conflict of interest in conducting this study.
sex were more or less evenly distributed. (Table
1)
The participants of this study were assured of
anonymity in accordance with the Data Privacy
Seventy -four patients out of 236 (31.36%)
Act provisions. (16) Their personal and interview wished to be dead but an even higher number of
data were kept in a private safe in the office of respondents at 86 (36.44%) answered that they
the researcher and only the researcher could had had non-specific active suicidal ideation i.e.
gain access to their data for further analysis. The they had thoughts of wanting to end their life
researcher also considered the stigma attached but had not thought of a specific plan yet. For
to mental health conditions and the impact it this part of the questionnaire, the structure of
could have in the community thus the data the CSSRS gives the patients a chance to answer
privacy of the participants were safely guarded. numbers 3,4 and 5 only if they answer question 1
and 2 with yes; respondents may have multiple
The duration of the participants involvement in responses. (Table 2)
the study lasted up until the CSSRS had been
administered and the informed consent duly
signed, this lasted about 3-5 minutes.
Possible risks that may be experienced while
undergoing this research may include a
recollection of stressors that led to the subject
having suicidal ideations. Should a patient be
noted to have severe suicidality in terms of
ideations and behaviors, he/she was referred to
the Telepsychiatry Outpatient Department
(OPD) for further assessment and management.
It was also explained that there would be a
corresponding fee of 150 PhP for an online OPD
consult. No actively distressed participants were
encountered during the administration of the
survey. Participants who had mild distress due
to remembering their previous suicidal attempts
were asked to do deep breathing exercises and
their expressed feelings and emotions were
supported, acknowledged and validated. The
option of going through further consult was also
given.
36 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Those who answered yes to 1 or 2 or 3, 4 and 5
questions in the suicidal ideations get to answer
the intensity of suicidal ideations subscale that
follows. Due to these multiple options of
answering provided by the CSSRS, the intensity
subscale as well as the other subscales may not
show a consistent tally with the total number of
236 respondents. (Table 3)
There were 109 who admitted to having suicidal
ideation. For the intensity of suicidal ideation,
responses on the subscale of frequency of
suicidal ideations, 44 respondents (18.64%) had
suicidal thoughts once a week and 40 (16.95%)
had suicidal thoughts less than once a week. In
the duration subscale, 47 (19.92%) noted they
had fleeting thoughts of suicide, lasting a few
seconds or minutes and 26 (11.02%) said that the
suicidal thoughts lasted less than an hour. On
the controllability subscale, majority at 44
(18.64%) said they were easily able to control
thoughts, 33 (13.98%) said they were able to
control their thoughts with little difficulty. For
the deterrents, i.e. anyone or anything that has
stopped the respondent from wanting to die or
carrying out the suicidal thoughts, 63 or 26.69%
said that deterrents definitely stopped them
from committing suicide. When it came to the
reasons for the suicidal ideation, there was a
similar proportion of those who said they were
merely trying to get attention, revenge or a
reaction from others (25 or 10.59%), and those
who answered that it was to end or stop the pain
26 (11.01%). The mean scores are displayed to
show the average of the group responses. (Table
3)
For the suicidal behaviors, the more common
description was that their suicidal attempt was
aborted (19.07%) i.e. they had planned to carry
out the suicidal act, but stopped it themselves;
while 16.53% had their attempts interrupted.
Interrupted suicide attempts occur when
individuals initiate action to end their lives but
are stopped by someone or something external
to the individual before actually carrying out the
act. Aborted suicide attempts occur when
individuals start to do something to try to end
their lives but stop themselves before actually
harming themselves. The average number of
attempts for the 36 respondents was 2 but with
a range of 1-3 times. Those who did manifest
suicidal behaviors could have several types and
thus account for the multiple responses. (11)
(Table 4)
37 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
For the suicidal behaviors, the more common This was higher compared to the 17% suicidal
description was that their suicidal attempt was ideation prevalence rate taken from the Youth
aborted (19.07%) i.e. they had planned to carry Risk Behavior Survey (YRBS). (9) The YRBS was
out the suicidal act, but stopped it themselves; administered yearly by the Centers for Disease
while 16.53% had their attempts interrupted. Control and Prevention’s (CDC) Division of
Interrupted suicide attempts occur when Adolescent and School Health (DASH), which
individuals initiate action to end their lives but routinely monitored adolescent health
are stopped by someone or something external behaviors and experiences; and collaborates
to the individual before actually carrying out the with education agencies in the United States to
act. Aborted suicide attempts occur when provide the most recent surveillance data on
individuals start to do something to try to end health behaviors and experiences among high
school students across the country, among
their lives but stop themselves before actually
these are mental health and suicide.
harming themselves. The average number of
attempts for the 36 respondents was 2 but with
The prevalence of suicidal ideation was also in
a range of 1-3 times. Those who did manifest
stark contrast to local data on suicidal ideation
suicidal behaviors could have several types and
as collected in the 2013 Young Adult Fertility
thus account for the multiple responses. (11)
and Sexuality Survey 4 (YAFS 4). (17) The YAFS 4
(Table 4)
is a series of surveys about young adults aged 15
to 24, which tracked some core indicators of
youth status, well-being, risk and non-risk
behaviors and other outcomes and the
determinants of such outcomes. The YAFS 4
survey put the national prevalence of suicidal
ideation at 8.7%. The large disparity of this
research’s results with that of other surveys may
be due to the fact that the C-SSRS referred to a
Of the 36 respondents who said they had actual whole life time, while the YRBS only asked about
suicide attempts, 18 respondents reported the past 12 months and the YAFS 4 was unclear
suffering only minor physical injury. Minor regarding its time frame.
physical injury was defined as having sustained
injury to the body but not needing medical On the other hand, this relatively high
attention. (Table 5) prevalence of suicidal ideation was consistent
with a study by Estrada et al (18), wherein they
used the CSSRS to document suicidal ideation
and behaviors among adolescent learners
enrolled in the Alternative Learning System
(ALS) in Manila, Philippines. They showed that
the lifetime prevalence of suicidal ideation – the
wish to be dead and non-specific active suicidal
thoughts were at 40.4% and 40.9% respectively,
which were approximated the numbers in this
study. The high prevalence of suicidal ideation,
using the CSSRS may be heralding an upward
trend in suicidal ideation, yet may be overlooked
and undetected due to lack of a standardized
method of inquiring regarding suicide.
DISCUSSION This high prevalence rate may reflect the higher
Suicidal Ideation suicide attempts among adolescents and young
adults. It may also be indicative of changing
sociocultural attitudes towards suicide i.e. that
In this study the prevalence of suicidal ideation
the government has mandated a National
severity was at 36.44%, which was described as
Suicide Prevention Strategy of the Department
nonspecific active suicidal thoughts.
of Health in partnership with the WHO. (19)
38 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
This includes a multisectoral approach to mental For the frequency subscale, the mean score was
health that has set up programs and 2 (once a week). In this light, a promising
interventions in schools. development has turned up with Chang et al.
(23) who developed a Frequency of Suicidal
Usage of social media has become a primary Ideation Inventory (FSII). Frequency of suicidal
forum for interpersonal engagement among thoughts in participants over the past year were
teens, which is a period when social contact is measured using a 5-point Likert-type scale,
important in maintaining their well-being but at ranging from 1 (never) to 5 (almost every day).
the same time may have a negative influence Higher scores on the FSII were indicative of
when exposed to other cultures and suicidality. greater suicidal ideation (SI) frequency. This
Another key feature of social media is the could be used in future studies wherein a
reliable and validated tool for measuring the
amount of time adolescents spend engaged with
impact of the frequency of suicidal ideations
it and the fact that it makes social contact
may be required.
available almost without limits. (20)
For the deterrents subscale, 26.69% answered
The rise in suicide rages parallels the rise of
that deterrents definitely stopped them. This
social media usage. The percentage of American
relatively high rate of suicide attempts that have
adults who used social media increased from 5%
been deterred, highlights that suicide risk is
in 2005 to 79% in 2019. (21) This steep rise in
often short term and situation specific, and
social media use is fairly recent and may have
therefore preventable. The examples of
just been unfolding when the YAFS 4 was
deterrents listed in the CSSRS were family, fear
conducted in 2013. (17) Thus, this increased of pain and religion, which could be expected
prevalence may be heralding an uptrend in considering the Philippines is a predominantly
suicidal ideation and behaviors in adolescents. Catholic or Christian nation.
The other items (Items 3, 4 and 5) on the severity In a recent review by Lawrence et al (24), they
ordinal scale of suicidal ideations highlight the found that many studies indicated that religious
importance of asking not just about ideation, but affiliation was protective against suicide
also about ideation relative to method, intent attempts and suicide, but not suicidal ideation.
and plan. These need to be asked for these other Torgler and Schaltegger found that in the 20-
items were based on previous studies predicting year period (1981–2001) in Switzerland, a strong
suicide attempts. Asking about these other items negative correlation between Catholicism and
could also be important in reducing access to the number of suicides per capita was noted.
means, an area of strategic action proposed by (25)
the WHO for suicide prevention. (19)
In terms of sex, 58 (68%) of those who had
Intensity of Ideation suicidal ideations in this study were females.
The intensity of ideation subscale, comprises 5 Thus, the role of gender may also play a role in
items, each rated on a 5-point ordinal scale: the higher prevalence of suicidal ideations, as
frequency, duration, controllability, deterrents, demonstrated by Lie et al. who showed that
and reason for ideation. The intensity subscale Female Filipino junior high school students
scores were significant predictors of suicide showed higher suicidal ideations. (26)
attempts at return psychiatric emergency (PE)
visits across the 1-year study period for Suicidal Behaviors
predictors of suicide attempts among ado- A history of suicide attempts was regarded as
lescents in psychiatric emergency (PE) settings one of the strongest predictors of future suicide
according to Suominen et al. (27) This study’s
in a study by Gipson et al (22). These five
prevalence rate of 15.25% was similar compared
variables examined independently resulted in
to the local study using the CSSRS by Estrada et
the duration item being the only significant in-
al. (18), which showed that the prevalence of
dependent predictor of return PE visits or
suicide attempts was12.9% but was higher when
suicide attempts at return visit. For this
compared with the YRBS, which found that the
research, the mean duration score was at 2.12
prevalence of suicide attempts was 7.4% (9) and
(<1 hr/day) compared to 2.32 for the study by
that of the YAFS 4 local data that reported a
Gipson et al (22).
prevalence of 3.2%. (17)
39 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
The stark difference in rates of the C-SSRS vis a were equally predictive of actual attempts, and
vis the YRBS and YAFS 4 may be due to a more those with multiple behaviors had greater risk.
elaborated, and specified way of asking about
suicide attempt. An actual attempt was defined In a retrospective study by Mckean et al wherein
in the CSSRS to be a potentially self-injurious act they reviewed first suicide attempt outcomes.
committed with at least some wish to die, as a They found that despite composing only 31.7%
result of the act. Behavior was in part thought of of the cohort, male subjects composed most
as method to kill oneself. Intent does not have to completed suicides. (32)
be 100%. If there is any intent/desire to die
associated with the act, then it can be CONCLUSION AND RECOMMENDATIONS
considered an actual suicide attempt. There
For the respondents of this particular National
does not have to be any injury or harm, just the
High School, about one third (36.44%) had non -
potential for injury or harm. For example, if
specific suicidal ideations and only 13.98% had
person pulls the trigger while a gun is in his/ her
active suicidal ideas with intent to carry out a
mouth but the gun broke without any resulting
suicidal plan coupled with 15.25% of actual
injury, this would be considered an attempt.
suicide attempts; both of which are higher than
international data. The severity of the ideations
The prevalence of Non-Suicidal Self Injury (NSSI)
and behavior on the other hand were not as
was 15.68% was relatively lower compared to
alarming since majority of the ideations were low
the 20% prevalence of NSSI described by
in frequency and duration while high in
Masana et al. in their local study with college
controllability. The suicidal behaviors on the
students examining the relationship of adverse other hand mostly resulted in minor physical
childhood experiences, NSSI and pathological injury. In light of these relatively high prevalence
personality traits. (28) rates, school-wide intervention on education or
awareness programs, gatekeeper training, peer
In a study by Cyzy et al (29), NSSI was noted to leadership, skills training and screening or
be a means of coping with suicidal thoughts and assessment should be instituted to curb the
considered to be a particularly high-risk group in suicide risk of senior high school students.
need of more intensive support.
In a systematic review by Surgenor et al (33),
The proportion of interrupted (16.53%) and they identified key issues with the said school-
aborted suicide attempts (19.07%) of this study wide interventions. In this light, they had ten
were surprisingly higher than the actual suicide recommendations, which would also be the
attempts (15.25%). Compared to the findings recommendations for this school and other
with Estrada et al., they found the prevalence of schools in the Philippines: 1) employ longer term
interrupted attempts to be at 6.4% and for strategies; 2) be aware of contextual factors, in
aborted attempts to be at 16.4%. (18) which suicide prevention programs are
delivered; 3) clearly define learning outcomes
Examining the associations between interrupted, when it comes to suicide prevention programs;
aborted, and actual suicide attempts among 4) start with a preparatory phase; 5) create a
adolescent inpatients, Burke et al (30), found flexible design and delivery, 6) tap external
that both interrupted attempts and aborted expert facilitators instead of staff; 8) Not to be
attempts were significantly associated with the restrictive; 9) Not to overemphasize risk factors;
frequency of actual attempts after co-varying 10) implement a varied, interactive and engaging
for suicidal ideation and demographic manner of delivery; and lastly 10) re-evaluate
characteristics. These results suggested that a programs regularly.
failure to integrate interrupted and aborted REFERENCES
1. Fleischmann A. Suicide in the World: Global Health Estimates
attempts into suicide risk assessments may [Internet]. World Health Organization. World Health Organization;
result in underestimating adolescent suicide risk. 1970 [cited 2019Sep]. Available from:
https://apps.who.int/iris/handle/10665/326948
2. Suicide in the World: Global Health Estimates [Internet]. World
Twelve (5.08%) of the 236 respondents had Health Organization. World Health Organization; 1970 [cited
2019Sep]. Available from:
preparatory behavior. In a study by Mundt et al https://apps.who.int/iris/handle/10665/326948
(31) wherein C-SSRS was administered to 3. Redaniel MT, Lebanan-Dalida MA, Gunnell D. Suicide in the
Philippines: Time Trend Analysis (1974-2005) and literature review.
depressed subjects, interrupted attempts, BMC Public Health [Internet]. 2011 [cited 2019Mar21];11(1).
aborted attempts and preparatory behavior
40 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
REFERENCES 21. Ortiz-Ospina E. The rise of Social Media [Internet]. Our World in
https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471- Data. 2019 [cited 2022Nov30]. Available from:
2458-11-536#citeas https://ourworldindata.org/rise-of-social-media
4. Young Filipinos are in the midst of a mental health crisis [Internet]. 22. Gipson PY, Agarwala P, Opperman KJ, Horwitz A, King CA.
Lifestyle.INQ. 2019 [cited 2022Dec25]. Available from: Columbia-Suicide severity rating scale. Pediatric Emergency Care
https://lifestyle.inquirer.net/349884/young-filipinos-are-in-the- [Internet]. 2015 [cited 2019Sep];31(2):88–94. Available from:
midst-of-a-mental-health-crisis/ https://journals.lww.com/pec-online/Abstract/2015/02000/
5. Recide RS. Highlights of the 2010 Census-Based Population Columbia_Suicide_Severity_Rating_ Scale__Predictive.2.aspx
Projections [Internet]. Philippine Statistics Authority. 2016 [cited 23. Chang EC, Chang OD. Development of the frequency of Suicidal
2022Dec25]. Available from: https://psa.gov.ph/content/highlights- Ideation Inventory: Evidence for the validity and reliability of a brief
2010-census-based-population-projections measure of suicidal ideation frequency in a college student
6. Adolescent Health and Development Program Manual of population. Cognitive Therapy and Research [Internet]. 2016 [cited
Operations. Department of Health Philippines. 1st Edition. 2017. 2019Sep];40(4):549–56. Available from:
[Cited 2019 Sept]. Available from: https://link.springer.com/article/10.1007/s10608-016-9758-0#citeas
https://doh.gov.ph/sites/default/files/health_programs/Adolescent% 24. Lawrence RE, Oquendo MA, Stanley B. Religion and suicide risk: A
20Health%20and%20Development%20Program%20Manual%20of%2 systematic review. Archives of Suicide Research [Internet]. 2015
0Operations.pdf [cited 2020Sep];20(1):1–21. Available from:
7. Pisani AR, Schmeelk-Cone K, Gunzler D, Petrova M, Goldston DB, Tu https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7310534/
X, et al. Associations between suicidal high school students’ help- 25. Torgler B, Schalteggefr C. Suicide and Religion: New Evidence on
seeking and their attitudes and perceptions of Social Environment. the Differences Between Protestantism and Catholicism.” Journal for
Journal of Youth and Adolescence [Internet]. 2012 [cited the Scientific Study of Religion. 2014 June; 53 (2): 316–40. Available
2019Sep];41(10):1312–24. Available from: From: http://www.jstor.org/stable/24644267.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3534737/ 26. Lie H, Liou J-C. Suicide behavior among junior high school
8. Miron O, Yu K-H, Wilf-Miron R, Kohane IS. Suicide rates among students in Philippines and Indonesia associated with the social
adolescents and young adults in the United States, 2000-2017. JAMA factors. GSTF Journal of BioSciences [Internet]. 2012 [cited 2019Oct];
[Internet]. 2019 [cited 2019Oct];321(23):2362. Available from: 2(1). Available from: https://www.semanticscholar.org/paper/Suicide-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6582264/ Behavior-among-Junior-High-School-Students-Lie-
9. YRBSS [Internet]. Centers for Disease Control and Prevention. Liou/5cab5a2ee90ff1ed480d1db5d5accb959f4cfa5b
Centers for Disease Control and Prevention. 2018 [cited 2019Sep]. 27. Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, Lönnqvist J.
Available from: Completed suicide after a suicide attempt: A 37-year follow-up study.
https://www.cdc.gov/healthyyouth/data/yrbs/index.htm American Journal of Psychiatry [Internet]. 2004 [cited
10. Fernandez N, Grataloup G, Posner K. QL2 translation of the 2019Sep];161(3):562–3. Available from:
Columbia Suicide Severity Rating Scale (C-SSRS) for use in 33 https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.161.3.562
countries. Value in Health. 2008 Nov;11(6). Doi:10.1016/S1098- 28. Masana LP, Reyes MES, Delariarte CF. Unraveling Non- Suicidal
3015(10)66182-7 Self Injury: Understanding the Behavioral Dynamics of Filipino
11. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo Adolescents at Risk of Deliberate Self Harm. North American J of
MA, et al. The Columbia–Suicide Severity Rating Scale: Initial validity Psychology. 2020; 22(2): 331-354. Available from:
and internal consistency findings from three multisite studies with Researchgate.net/profile/Marc-Eric-
adolescents and adults. American Journal of Psychiatry [Internet]. Reyes/publication/341100218_Unraveling_Non-Suicidal_Self-
2011 [cited 2019Oct];168(12):1266–77. Available from: Injury_Understanding_the_Behavioral_Dynamics_of_Filipino_Adolesce
https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2011.10111704? nts_at_Risk_of_Deliberate_Self-
url_ver=Z39.88- _Harm/links/5ead555145851592d6b21d8a/Unraveling-Non-Suicidal-
2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Self-Injury-Understanding-the-Behavioral-Dynamics-of-Filipino-
12. Kilincaslan A, Gunes A, Eskin M, Madan A. (2019). Linguistic Adolescents-at-Risk-of-Deliberate-Self-Harm.pdf
adaptation and psychometric properties of the Columbia-Suicide 29. Czyz EK, Glenn CR, Busby D, King CA. Daily Patterns in non-suicidal
Severity Rating Scale among a heterogeneous sample of adolescents self-injury and coping among recently hospitalized youth at risk for
in Turkey. The International Journal of Psychiatry in Medicine. 54(2): suicide. Psychiatry Research [Internet]. 2019 [cited
115–132. https://doi.org/10.1177/0091217418791454 2019Nov];281:112588. Available from:
13.Columbia suicide severity rating scale (C-SSRS) [Internet]. https://www.sciencedirect.com/science/article/abs/pii/S01651781193
SAMHSA. [cited 2022Nov30]. Available from: 12727?via%3Dihub
https://www.samhsa.gov/resource/dbhis/columbia-suicide-severity- 30. Burke TA, Hamilton JL, Ammerman BA, Stange JP, Alloy LB.
rating-scale-c-ssrs Suicide risk characteristics among aborted, interrupted, and actual
14. Posner K. Triage and risk identification the Columbia Lighthouse suicide attempters. Psychiatry Research [Internet]. 2016 [cited
Project [Internet]. The Columbia Lighthouse Project. [cited 2019Sep]. 2019Sep];242:357–64. Available from:
Available from: https://cssrs.columbia.edu/the-columbia-scale-c- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5247268/
ssrs/risk-identification/ 31. Mundt JC, Greist JH, Jefferson JW, Federico M, Mann JJ, Posner K.
15. King CA, Berona J, Czyz E, Horwitz AG, Gipson PY. Identifying Prediction of suicidal behavior in clinical research by lifetime suicidal
adolescents at highly elevated risk for suicidal behavior in the ideation and behavior ascertained by the Electronic Columbia-Suicide
emergency department. Journal of Child and Adolescent severity rating scale. The Journal of Clinical Psychiatry [Internet].
Psychopharmacology. 2015;25(2):100–8. 2013 [cited 2020Oct];74(09):887–93. Available from:
16. National Privacy Commission. Republic Act 10173.Data Privacy https://www.psychiatrist.com/jcp/depression/suicide/prediction-
Act of 2012. Available from: privacy.gov.ph/data-privacy-act/ UP suicidal-behavior-clinical-research-lifetime/
Population Institute. 32. McKean AJS, Pabbati CP, Geske JR, Bostwick JM. Rethinking
17. The 2013 Young Adult Fertility and Sexuality Study [Internet]. lethality in youth suicide attempts: First suicide attempt outcomes in
DRDF Inc. 2019 [cited 2022Nov30]. Available from: youth ages 10 to 24. Journal of the American Academy of Child &
https://www.drdf.org.ph/yafs4 Adolescent Psychiatry. 2018;57(10):786–91.
18. Estrada CA, Nonaka D, Gregorio ER, Leynes CR, del Castillo RT, 33. Surgenor PW, Quinn P, Hughes C. Ten recommendations for
Hernandez PM, et al. Suicidal ideation, suicidal behaviors, and Effective School-based, adolescent, Suicide Prevention Programs.
attitudes towards suicide of adolescents enrolled in the Alternative School Mental Health. 2016;8(4):413–24.
Learning System in Manila, Philippines—a mixed methods study. 34. Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International
Tropical Medicine and Health [Internet]. 2019 [cited 2019Sep];47(1). prevalence of adolescent non-suicidal self-injury and deliberate self-
Available from: harm. Child and Adolescent Psychiatry and Mental Health [Internet].
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6439964/ 2012 [cited 2019Nov];6(1). Available from:
19. DOH and WHO promote holistic mental health wellness in light of https://capmh.biomedcentral.com/articles/10.1186/1753-2000-6-10
World Suicide Prevention Day [Internet]. World Health Organization.
World Health Organization; [cited 2022Nov30]. Available from:
https://www.who.int/philippines/news/detail/10-09-2020-doh-and-
who-promote-holistic-mental-health-wellness-in-light-of-world-
suicide-prevention-day
20. Luby J, Kertz S. Increasing suicide rates in early adolescent girls in
the United States and the equalization of sex disparity in suicide.
JAMA Network Open. 2019;2(5).
41 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP CASE REPORT
EXAMINATION OF THE RIGHT TO CONFIDENTIALITY
NINA KRISTY A. OSORIO-GRAPILON, MD, DSBPP
ABSTRACT
With the establishment of the Republic Act No. 11036, more popularly known as the
Mental Health Act, improvement in the mental, neurologic, and psychosocial health took a
step forward in the Philippines. This law, which was signed on June 2018, gave specific
provisions in different aspects of delivery of mental health services to Filipinos. This law
proved very useful in the dilemma faced in the following case where a potential problem
in confidentiality was encountered.
CASE PRESENTATION Fearing for her life, she went back to her house
without saying anything to her family. She
Chief Complaint blamed herself. She felt alone. Since then, she
N.O. is a 15-year-old, Filipino Catholic was noted to be more quiet than usual and was
adolescent female, an only child of her parents’ easily startled, prompting her half-brother
union but the youngest among 4 children on her (A.O.), who came to visit their parents several
father’s side and the youngest of 10 children on days after the alleged incident happened, to ask
her mother’s side, presently residing with her the patient what was happening to her. She con-
parents. N.O. was brought for consult by her fided to A.O. but pleaded with him not to say or
mother due to persistent headaches and do anything. He promised and instead, helped
difficulty in sleeping. her out in determining if she got pregnant by u-
sing a pregnancy test. Negative results were
History of Present Illness noted, and the 2 siblings decided to be quiet
Two years prior to consult, when N.O. was 12 about it for the meantime. She went about her
years old, she was allegedly raped by her 22- usual activities. She attended her classes
year-old neighbor. They were chatting online for without fail and consistently garnered high
a few weeks until she was invited over to his grades. However, she would occasionally have
house because he said he would give her a difficulty in concentrating at school. At home,
surprise gift. Intrigued, she sneaked out one she was terrified at the possibility of encoun-
night and went over to her neighbor’s house. She tering her neighbor. She was able to take com-
was led inside his room, forced to lie down on fort in the fact that she was not allowed to go
the bed, disrobed, and was under the control of outside the house without being accompanied
her neighbor. During that time, the patient felt by either one of her parents and so she stayed
helpless and scared. She did not know what to home most of the time. She would have frequent
do and even failed to fight her neighbor. When it dreams about her neighbor and the alleged inci-
was over, she was warned not to tell anybody of dent. She would distance herself from her half-
the incident or else she would be harmed. brother because she would remember the alle-
42 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
-ged incident. No problems were noted until a She did not want to return but she had no
few weeks after when she was fed up with a choice but to agree despite being very
classmate teasing her and so tried to choke him. apprehensive about it. With the prospect of
She felt it was unfair when she was reprimanded. going back to her old school, she started to have
Despite this, N.O. was still able to maintain high more frequent dreams about her alleged sexual
grades and was at the top of her class but later assault 2 years ago, though unable to recall
the patient was dropped from the 1st rank of the some parts of the alleged incident. During this
class due to her English subject. She felt time, N.O. would see her parents frequently
betrayed because she was usually the favorite in fighting about their financial problems. She
her class. In secret, N.O. would scratch her arms feared that they would separate and leave her.
Since then, the patient was noted to be easily
or would think of hurting herself because she
irritated and quieter. She would scratch her
felt that she was humiliated. She attempted to
forearms to relieve stress and release her
slash her wrist but was prevented by her half-
tension. She would occasionally think of what it
brother. She was then transferred to another
was like to die but at the same time was afraid
school after her parents’ unsuccessful attempts
to try killing herself.
to plead with the patient’s teacher to give her
some consideration.
One month prior to consult, N.O.’s father
underwent a major surgery. She was very
N.O. was initially faring well academically in her
worried about her father as they were very
new school but 1 year prior to consult she
close. She felt guilty that she burdened him with
punched a classmate due to his relentless her problems. She started thinking about what
teasing. She felt ill-used when she was happened to her 2 years prior. Her dreams
reprimanded. She was obedient and well-liked about the alleged incident became more
by her teachers, but she was blamed for the frequent. She wanted to tell her father but she
incident regardless of the teasing by her was too afraid of his reaction. She felt ashamed
classmate. Since then, the patient again felt that and guilty of not having told her father of what
she did not belong in her school because they happened. N.O. started to have frequent
seemed afraid of her. Still, her grades were not headaches and difficulty in sleeping. She had
affected even if she would have some difficulty difficulty concentrating. Her mother noted that
in concentrating while in class. N.O. had frequent blank stares. The patient
would get distressed about feeling that she did
At another time, the patient informed her not belong in her family and in her community
parents that she would be a little late in coming as if she was a ghost.
home from school because of a school project
with her classmates. However, her parents found Two weeks prior to consult, headaches became
out that she and her classmates went to a mall more frequent and persistent, with pain scores
near their school. Her parents, most especially of 6-7/10, prompting her to seek consult in the
her father, got very mad and scolded the patient emergency section of the Pediatrics
and her classmates. She had a big fight with her department, where she was prescribed with
father and wanted to die because no one really Mefenamic acid 500mg/tab, 1 tab every 6 hours
understood her, not even her father. She took 2- and Vitamin B complex 1 tab once a day. No
3 tablets of Trimetazidine (her father’s relief of symptoms were noted with the
medication) when she was stopped by her medications. She was very frustrated up to the
mother and brought to the hospital. She was point that she wanted to die. She was referred
observed and was sent home with no to Psychiatry in the ER due to her difficulty in
sleeping. At that time, she was noted to be
complications. She promised her parents that
depressed with congruent affect. She was
she would not hurt herself again. She went back
anxious and was hesitant to relate her feelings.
to her usual activities, but was more closely
She denied any history of trauma or abuse.
monitored by her parents. Her feelings of
Initial impression was Persistent Depressive
loneliness and isolation persisted but she tried
Disorder; with Borderline Personality Traits and
to divert her feelings.
Suicide Risk. She was prescribed with Sertraline
50mg/tab ½ tab ODHS and Alprazolam
About 2 months prior to consult, she was told
500mg/tab ½ tab PRN for insomnia. They were
hat she would be transferred to her old school
advised to follow-up after 1 week.
because of financial constraints.
43 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
Family and Social History The matter was smoothed over because R.O. had
There were no known psychiatric illnesses in the money at that time, thus he was not arrested or
family. There was hypertension and heart jailed. He met his wife, the patient’s mother,
disease on her paternal side, while dyslipidemia when he was still in the military. When the
and kidney problems on her maternal side. She patient was born, he was observed to have
was a non-smoker and never used illicit drugs. apparently changed. Athough still short-
She occasionally drank wine (1-2 times a year, tempered, he could be pacified by his wife.
half a glass) with her last intake a year prior to
consult.
Family Genogram
Father: R.O., 68 years old He doted on the patient and not once did he hit
He was a retired military pilot, who eventually her. Lately, patient’s parents would be heard
worked in the real estate sector. Before he bickering mostly about money, which would
became ill, he was involved with real estate that alarm the patient, thinking that her parents
occasionally entailed going abroad to work on were going to separate.
projects. One month prior to the patient’s
consult, he was admitted due to hemothorax Mother: D.O., 50 years old
and underwent bullectomy and lobectomy. She was a real estate agent who had a previous
common-law husband with whom she had 9
He had 3 children from his former common-law children; 2 of whom are close to the patient
wife who all live in the United States, thus have (J.O. and A.O.). She separated from her first
a strained relationship with R.O. With his 3 husband due to undisclosed reasons.
children, he was very strict and authoritarian,
especially when he was still in the military. He She was described as talkative, frank and short-
was easily angered and used corporal tempered. She also allegedly stabbed a person
punishment in disciplining his children. He who attempted to pick a fight with her. Like her
separated with his common-law wife when she husband, she doted on the patient and gave her
went to work abroad. whatever she asked for and was the one more
easily swayed by the patient.
He allegedly and impulsively shot a person
point-blank while the said person was drinking Half-Siblings on the Paternal side:
with his friends immediately after discovering
that his daughter (the patient’s half-sister) was 1. G.O., 45 years old, married and currently
bullied by that person. Patient’s father then living abroad. He has no relationship with the
went to the police station because the person patient and has a strained relationship with his
that he killed reportedly had a cousin who was a father.
police officer and also shot the police officer.
44 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
2. J.O., 41 years old, married and currently living Developmental & Social History
abroad. She has no relationship with the patient
and also has a strained relationship with her N.O. was born term and without complications
father. to her then 35 -year-old G10P9 (9009) mother
via Normal Spontaneous Delivery at a private
3. S.O., 38 years old, married and currently living hospital. Her mother had regular prenatal
abroad. She would come and visit every year, check-ups. She took Ferrous Sulfate during the
bring gifts to the patient and allowed the patient 2nd trimester of pregnancy. The pregnancy was
to have a sip of wine with her during dinner. planned and wanted. Mother’s emotional and
physical states were unremarkable, with no
Half- Siblings on the Maternal side history of trauma, substance abuse, and intake
of teratogenic drugs. She reported bleeding
during the 3rd trimester of pregnancy which
All of the patient’s siblings with her mother are
turned out to be due to placenta previa, which
living with their father in the province. They do
resolved eventually. No other complications
not visit their mother in Quezon City due to the
were noted throughout pregnancy. N.O. was
strained relationship between their father and
immediately mixed fed with breastmilk and
the patient’s mother. Only J.O. and A.O. would
formula milk until 3 months because of
come by and stay for a few days with N.O. and
decreased maternal milk output. She was fed
her parents.
immediately as per demand. No eating
problems were noted. The mother was the
1. L.A., 29 years old, currently working in the
primary caregiver. Developmental milestones
province. He has no relationship with the
were noted to be at par with her age. She was
patient. attached to her mother and would cry when
2. R.A., 28 years old, currently working with his another person would carry her away from her
brother, L.O. in the province. He has no mother. However, she would calm down after a
relationship with the patient. few minutes and would respond happily to the
3. J.A., 27 years old, employed in Quezon City, person carrying her.
currently living in an apartment. He would
sometimes visit his mother and half -sister for a Moderately strict toilet training was enforced
few days. He would play and talk with the by the father, who would wake her up at night to
patient and was like one of the patient’s close go to the toilet. Accidents were dealt with
friends. verbal reprimands by the father most of the
4. K.A., 26 years old, working in the province. He time and embraces and kisses from the mother
has no relationship with the patient. whenever she would pee accidentally. Toys
5. L.A.A., 25 years old, married and lives in the were bought almost always. She would throw a
province. She has no relationship with the fit when her wants were not met, and she would
patient. calm down with the reassurances of her
6. T.A., 24 years old, working in the province. She parents. She was shy towards neighbors but
has no relationship with the patient. active at home. She often played alone or with
7. A.A., 23 years old, employed in Quezon City, her half-brothers, because her parents did not
currently living in an apartment. He would allow her to play outside.
occasionally visit his mother and half -sister for
a few days where he would play and talk with the The first memory of N.O. was when she was 5 -
patient and also considered as one of the years-old happily eating together with her
patient’s close friends. Patient is closer to A.0. parents. She was enrolled in a preparatory class
as he was the first one to know of her alleged near her home. She was an active and smart
rape 2 years ago. child, and got along with her peers. On the 1st
day of 1st grade, she was anxious to be left
8. F.A., 22 years old, currently working in the
alone by her mother that she had to be
province. He has no relationship with the
reassured of mother returning after class. She
patient.
was a top student during her grade school and
9. W.A., 21 years old, working in the province.
She has no relationship with the patient.
45 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
was tutored by both parents who encouraged depressed but related that the difference this
her to get high grades. Many of her classmates time was that she will get the help she needed.
were her friends but was not open to share her She denied suicidal or homicidal ideations.
feelings with them. Her activities were limited to Responses were linear and goal-directed. She
school and home because her parents did not was oriented to 3 spheres, with intact memory;
want her to play outside the house. good concentration, calculation, fund of
knowledge, abstract thinking, impulse control,
At home, she would play with 2 of her half- and judgement. Insight level was III. She believed
brothers. The rest of her siblings were away and that she needed help because of what happened
had little to no interaction with her. She would to her in the past.
ask about them, but she would be told not to
mind them because she was their priority. Physical and Neurologic Examinations
Discipline was enforced by both parents, but lax.
The father was firmer in his decisions with Both physical and neurologic examinations
regards to the patient. However, both would revealed unremarkable findings.
waver and give in to the patient most of the
time. She transferred to another school after Diagnosis & Differential Diagnoses
finishing Grade 7 then returned for Grade 9. She
was more at ease in her 2nd school but she was Diagnostic work-up was done to rule out a
transferred back due to financial constraints. DEPRESSIVE DISORDER DUE TO ANOTHER
She was more of a follower than a leader. N.O. MEDICAL CONDITION [293.83 (F06.31)], given
was one of her teachers’ favorites thus often that a general medical condition could cause
given special errands. She was not allowed to go behavioral changes must always be considered.
out on her own with her friends and needed The patient’s symptomatology was able to fulfill
supervision by her parents. She spent most of Criteria A, D, E of the disorder: i.e. there was a
her time at home, watching Korean movies or prominent and persistent depressed mood
television series and spending time with her (Criteria A); that the disturbance did not occur
family. She liked to apply make-up and dress up. exclusively during the course of the delirium
(Criteria D) as there was no report of
Past Medical and Psychiatric History fluctuations of attention and consciousness; and
the disturbance caused clinically significant
There was no history of psychiatric distress and impairment in her social functioning
consultations or hospitalizations. She was (Criteria E). However, she was not able to fulfill
admitted twice for Dengue Fever and once for Criteria B and C i.e. there was no evidence that
Urinary Tract Infection with no complications the disturbance was the direct
noted. She had an early menarche at 10, like her pathophysiological consequence of another
mother. Menstruation was irregular, consuming medical condition (Criteria B), as all laboratory
2-3 pads/day, moderately-soaked, 3-4 days work-ups done upon initial encounter were
duration. She was nulligravid but with 1st sexual normal and she was cleared medically by the
contact at 12 years old. No contraception was Pediatrics Department. Thyroid function tests
used. were also done in her OPD consult, with normal
results. In addition, EEG was done with
Mental Status Examination unremarkable results. And for criteria C i.e. The
disturbance could be explained by another
She was seen and examined as an adolescent mental disorder; thus this diagnosis was ruled
female, medium built, dressed older for her age out.
with tight-fitting top and leggings, and with
slightly heavy make-up; fairly kempt and Thorough review of the patient’s substance or
groomed. No behavioral oddities were noted, drug use history was done, as well as a spot
with fair eye contact. She was cooperative and urine drug test, to rule out a
fairly conversant. Mood was depressed, with SUBSTANCE-/MEDICATION-INDUCED
appropriate affect. She had normo-productive DEPRESSIVE DISORDER [292.84 (F19.94)]. The
speech, slightly slow rate and decreased tone of patient belonged to an age-group with high
voice. She related that she was hearing buzzing potential for illicit drug use. The patient fulfilled
sounds beside her ears. She admitted to feeling Criteria A, D, and E. There was a prominent and
46 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
persistent depressed mood (Criteria A). The fulfilled. She had irritable behavior and angry
disturbance did not occur exclusively during the outbursts at school and she also had problems
course of the delirium (Criteria D). The with concentration and sleep disturbances. Her
disturbance caused clinically significant distress recurrent experiences of unreality of her
to the patient and impairment in her social surroundings necessitated the specifier of
functioning (Criteria E). However, she was not dissociative symptoms. This was ruled in.
able to fulfill Criteria B and C i.e., there was no
evidence that the symptoms developed during BORDERLINE PERSONALITY TRAITS were also
or soon after exposure to a drug (Criteria B), as highly considered. Unstable sense of self,
urine drug test was done with negative results. parasuicidal behavior, feelings of emptiness,
No other medications were taken by the patient episodes of physical violence, dissociative
that could possibly produce her symptoms and symptoms were noted. Although the patient
the disturbance could be explained by another presented with these manifestations, she could
mental disorder (Criteria C); thus, this condition not yet be diagnosed with a personality disorder
was also ruled out. because these traits were not yet inflexible as
required in the diagnosis of personality disorder
Despite the depressive symptoms noted from 1. Despite this, it is important to be aware and to
the history, the patient was unable to fulfill take noted of this because the stability of the
Criterion A for MAJOR DEPRESSIVE DISORDER personality traits needs to be assessed over
[296.24 (F32.3)]. She was only able to fulfill 4 out time and across different situations. Borderline
of the 9 symptoms: depressed mood, insomnia, personality traits have been shown to develop
diminished ability to think or concentration, and to borderline personality disorder in time 2,3.
recurrent thoughts of death. Still, depressive
symptoms could not be overlooked. A Course in the Clinic
PERSISTENT DEPRESSIVE DISORDER
(Dysthymia) [300.4 (F34.1)] was also initially N.O. revealed her alleged sexual assault on the
considered but ruled out. Despite the symptoms 1st follow-up. She was started on Olanzapine
of the patient, these were not apparent to have 5mg/day due to disturbed and hallucinatory
occurred for more days than not, as specified in behavior. Dissociative amnesia was noted. She
Criterion A of the disorder. In any patient related her desire to tell her father, but her
presenting with depression, it is important to mother refused out of fear that he would kill the
probe for possible manic or hypomanic episodes perpetrator. Subsequent follow-ups showed
(BIPOLAR I OR II DISORDER [296.40 (F31.9] / fluctuations between improvement and
296.89 [F31.81)]) in the past. In the case of the disturbed behavior, warranting increase in doses
patient, no manic episode was noted. of Sertraline to 50mg/day and Olanzapine to
10mg/day. Improvement in symptoms were
First follow-up revealed hallucinatory behavior noted and Cognitive Behavior Therapy (CBT) was
and a history of trauma. A trauma-related initiated with promising results. Olanzapine was
disorder was then considered. With the exposure discontinued in her last follow-up, with
of the patient to a traumatic event, as well the preparations for the patient to return to school.
pattern of the patient upon longitudinal review
of her history, a diagnosis of POST-TRAUMATIC DISCUSSION
STRESS DISORDER [309.81 (F43.10)] was highly Psychodynamic Formulation
considered and eventually made. The patient Absence of delayed gratification is a common
had a 2-month long history of intrusive symp- theme throughout the N.O.’s life as all her wants
toms (Criterion B), specifically recurrent distres- and needs were readily given by her parents. In
sing dreams about her attack, as well as intense addition, she was not exposed to relationships
psychological distress upon exposure to outside the family. Her parents both had prob-
external cues reminiscent of her attack. She was lems in controlling their anger, thus were poor
also able to fulfill Criterion C in which she would role models on handling emotions. This lack of
avoid ex-ternal reminders of her attack. Criterion “practice” for social interaction could be the
D was also fulfilled. She had dissociative reason for her apparent lack of close rela-
amnesia as well as feelings of detachment and tionships. She did not know how to act or ad-just
estrangement from others. Criterion E was also accordingly, leading to feelings of being bullied.
47 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
-Ultimately, when the time came that the family memory failure. Instead of working through the
became financially challenged, she was unable painful memories, N.O. somatized her affects i.e.
accept or cope with the need to be deprived of headaches, difficulty sleeping in order to avoid
her material wishes or frustrated of her the powerful emotions, which were viewed as
demands. These restrictions were internalized threats to her. That lack of control led to
by N.O. as a negative experience and became dissociation, which represented N.O.’s failure to
angry at her parents for not giving her what she integrate aspects of her perception, memory,
wanted. identity, and consciousness. It gave her a sense
or illusion of psychological control.
Aggressive feelings led to conflicting and
confusing feelings within N.O. There was a clash Management
between opposing pairs of internal object
relations, that is, between having a good parent Biological: The possibility of admission was
or having a bad parent. Prior to this, her alleged discussed with the mother if the patient’s
sexual assault took a toll on her. She blamed behavior would escalate at home. She was
herself for what happened because she was the thoroughly informed, and her decision was to
one who decided to sneak off to her neighbor’ keep a close watch on the patient instead. The
house. She was raped and humiliated. She was patient was maintained on the following: (1)
overpowered. She had no control of the Sertraline 50mg/tab 1 tablet ODHS-
situation. This humiliation might have devalued Antidepressants have been used as adjuncts to
the patient as an individual, resulting to loss of psychosocial treatments and Sertraline is
self-esteem and self-worth. She might have been approved by the FDA 4,5 in the treatment of
pushed over the edge when her father got sick PTSD in adults, but with scant evidence to
since she had to take care of him. N.O. noticed support the use in the youth. Still, several
how her father was transformed from being very studies 6,7,8 would show that SSRIs have
functional and even aggressive to being weak moderate effects in PTSD. (2) Olanzapine
and useless. Having introjected her father also, 5mg/tab 1 tablet ODHS. An antipsychotic was
this loss of function and purpose reverberated given and eventually discontinued to address
within her. She was both angry and sad that her the hallucinatory behavior of the patient as
father was now helpless (loss of the father image reported in the course of her follow-ups. (3)
as a constant pillar of strength and provision) Alprazolam 500mcg/tab 1 tablet as needed for
while she now had to be burdened with taking anxiety and difficulty sleeping.
care of him and giving up material benefits and
her preferred school. Unconsciously, she may Psychological: Cognitive Behavioral Therapy i.e.
have also blamed herself for his condition. The psychoeducation was conducted for the parents
guilt feelings that were with her for being and the patient. Knowing the low frustration
sexually assaulted, for being angry at her tolerance of the patient, parents were guided on
parents because of their financial problems, all their parenting skills, e.g. on when to say no to
led to her blaming herself. Being subjected to the patient, not giving in to demands and wants
the taunts of her classmates, to her perceived all the time. The patient was encouraged to do
unjustified low grade that cost her top rank in relaxation techniques, and to identify her
class, her father’s illness and recurrent financial feelings and talk about it.
troubles, reactivated that same sense of lack of
control when she was sexually assaulted. She Social: Safety of the patient was the most
was helpless. The old trauma was reawakened by important consideration. Given that the alleged
her recent troubles. Dissociative defenses came perpetrator was still living nearby, it was
into play, trying to keep her intense and painful discussed with the mother on how to ensure the
affects unconscious. safety of the patient and whether patient could
live physically far from the alleged perpetrator.
However, the prominence of the traumatic However, it was not possible at the time for the
memories caused them to be maintained at a family to transfer residence. The mother made
high state of cognitive activation. These factors the initiative to talk to the perpetrator and his
led to N.O.’s memory intrusion alternating with family, warning against any interaction with the
48 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
patient. A threat of filing a case or a police cessary to prevent harm or injury to the service
report was discussed with the perpetrator and user or to other persons.” With the examination
his family. For the patient, the mother was of this provision, it was N.O.’s decision herself to
contemplating on having her on close watch by disclose the information to her father. However,
herself or, if she could hire a nanny, to watch the being a minor, her mother served as her legal
patient while she was away. Strong community guardian who was against the N.O.’s wishes.
support was also discussed. The reputation of Ideally, the patient should be encouraged to
the parents in the community could also be inform her father with the intent of relieving N.O.
harmful to the patient. Outside school, the of her guilt. Yet if the patient would tell her
patient also had limited social interactions in the father, there was a chance of assault towards
community. Both issues were thoroughly the alleged perpetrator.
discussed, and steps were taken to start to
expose the patient to the community. Although Furthermore, examination of the Mental Health
the patient was not able to identify any friends Act showed that informing the father would
in her school, she admitted that she had a few serve as a breach of confidentiality as specified
friends before in the neighborhood and she in Section 5l and the psychiatrist may be held
verbalized the desire to rekindle the criminally liable as stated in Section 44 9:
relationships. “Penalty clause: Any person who commits any of
the following acts shall… be punished by
Dilemma on Confidentiality imprisonment… or a fine…, or both, at the
discretion of the court..”
Establishing rapport could not be over-
emphasized in this case. The first encounter The mother can file for a criminal case of breach
proved that several meetings were needed to of confidentiality against the doctor, since she
fully establish the trust between a doctor and a specifically told the doctor not to tell the father
patient. With N.O. opening about the trauma she anything about the rape incident. Should this
experienced; it was decided that on her sub- happen, the burden would be for the doctor to
sequent follow-ups, a more focused and guided prove his or her own innocence in court. Given
approach would be utilized. that there is that chance of harm to the alleged
perpetrator, is it warranted to warn him? One
In addition to her medications, the need for N.O. case comes to mind: Tarasoff v. Regents of the
to work through her trauma was deemed of University of California (1974) 10. In this case, it
utmost importance. And one step identified, as was held that mental health professionals did
volunteered by N.O., was to inform her father of have a duty to protect individuals who were
what happened. However, her mother was being threatened with bodily harm by a patient.
against the idea out of fear that he would kill the
alleged perpetrator as well as his entire family, However, the father was the one who made the
given his history. The father, when hypo- threat. Despite the father’s statement, the
thetically asked what he would do if such threat was not in absolute terms. Also, the
incident would happen to his daughter, admitted patient’s father was not the patient. The
that he would hunt and kill the perpetrator psychiatrist has no technical responsibility in
without any regard for what will happen to him. preventing him from enacting his threat. There is
no provision in the Act stating an explicit duty to
Given such a situation, what should a reasonable inform another person of a threat of harm (in
psychiatrist do? We turn to the Mental Health contrast to the Tarasoff case). It rather only
Act (Republic Act No. 11036) 9. In Chapter II, creates an exception to the patient’s right to
Section 5 (Rights of Service Users), one of the confidentiality and thus, the only obligation to
rights identified was: (l) “Confidentiality of all the patient’s right to confidentiality under it, was
information, communications, and records…shall to not violate that confidentiality. In
not be disclosed to third parties without the consideration of N.O., the need to inform the
written consent of the service user concerned or father was examined. If the father would be
the service user’s legal representative, except in informed of the rape incident, the guilt feelings
the following circumstances:…(3) A life-threaten- of N.O. would possibly be unloaded.
ing emergency exists, and such disclosure is ne-
49 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
At the same time, if the father indeed would kill REFERENCES
1. American Psychiatric Association. Diagnostic and Statistical
the neighbor and his family, a crime would be Manual of Mental Disorders Fifth Edition. Arlington, VA:
committed, and the patient might suffer more American Psychiatric Association; 2013. 647 p.
with the burden of death of several people. N.O. 2. Warner MB, Morey LC, Finch JF, Gunderson JG, Skodol AE,
Sanislow CA, et al. The Longitudinal Relationship of Personality
ultimately has the right to inform her father or
Traits and Disorders. Focus (Am Psychiatr Publ). 2005;3(3):465-
not. The role of the psychiatrist was not to 477.
influence or force the patient. 3. Trull TJ, Widiger TA, Lynam DR, Costa PTJ. Borderline
Personality Disorder from the Perspective of General
Personality Functioning. Focus (Am Psychiatr Publ).
CONCLUSION 2005;3(3):453-464.
4. Henney JE. Sertraline Approved for Posttraumatic Stress
Physicians, in general, sometimes have the Disorder. [Abstract]. JAMA. 2000;283(5):596.
5. Schoenfeld FB, Marmar CR, Neylan TC. Current Concepts in
difficult task of balancing a decision that will be
Pharmacotherapy for Posttraumatic Stress Disorder. Psychiatric
beneficial for the patient or to the family or even Services. 2004;55(5):519-531.
the public. Now with legal implications for every 6. Gearson R, Rappaport N. Traumatic Stress and Posttraumatic
decision in a patient, the Mental Health Act will Stress Disorder in Youth: Recent Research Findings on Clinical
Impact, Assessment, and Treatment. J Adolesc Health.
serve as a guide for physicians in considering the 2013;52(2):137-143.
welfare of their patients and the community. In 7. American Academy of Child and Adolescent Psychiatry.
N.O.’s case, the decision to give out or withhold Practice Parameter for the Assessment and Treatment of
Children and Adolescents with Posttraumatic Stress Disorder. J
the information rests on the patient. The role of
Am Acad Child Adoles. Psychiatiry. 2010;49(4):414-430.
the psychiatrist is to discuss the pros and cons 8. Stamatako M, Campo JV. Psychopharmacologic Treatment of
of such “telling”, providing support for the Traumatized Youth. Opinion in Pediatrics. 2010;22(5) 599-604.
patient and letting her decide for herself without 9. Public Law: Mental Health Act. Republic Act No. 11036.
(Approved June 20, 2018).
undue influence from the doctor. 10. Supreme Court of California. Tarasoff v. Regents of
University of Californian 1974 [Internet]. Available from:
ACKNOWLEDGEMENTS https://caselaw.findlaw.com/court/ca-supreme-
court/1829929.html
The author thanks the 2019 consultant and
resident staff of Veterans Memorial Medical
Center for their support during the development
of this case report.
50 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP ABSTRACT
MAJOR DEPRESSIVE DISORDER AMONG PATIENTS RECEIVING
ANTIRETROVIRAL TREATMENT IN A SOCIAL HYGIENE CLINIC:
PREVALENCE, ASSOCIATED FACTORS AND EFFECTS ON QUALITY OF LIFE
LEONIDES E. BUMATAY, JR., MD, DSBPP
RODELEN PACCIAL, MD, DSBPP
JOEFFREY CRUZADA, MD, FPPA
EMMANUEL SEVILLEJA, MD
ABSTRACT
OBJECTIVES: The current study aimed to determine the prevalence of depression among
patients who received antiretroviral treatment; describe the sociodemographic and
clinical factors associated with Major Depressive Disorder; as well as compare the quality
of life among those with and without the co morbid psychiatric illness.
METHODOLOGY: A descriptive study was performed at a local hygiene clinic.
Sociodemographic and clinical data were gathered, using the Patient Health
Questionnaire 9 (PHQ-9) for screening depression and confirmed by Mental Status Exam
(MSE). Quality of life assessment was done through WHOQOL-HIV BREF questionnaire.
RESULTS: Of the 130 respondents, 31 (23.85%) subjects were assessed to have
depression. Among the different sociodemographic and clinical factors, younger age (p
value = .0174) was associated with depression. Though the quality of life of a Person Living
with HIV (PLHIV) fell in the acceptable category, those who had depression had poorer
quality of life in all subdomains especially in the psychological and social domains and
these were all highly statistically significant (p value <.0001).
CONCLUSION: The study revealed that Major Depressive Disorder (MDD) was prevalent in
almost one fourth (23.85%) of HIV patients who were mostly of a younger age i.e. less than
45 years old; with 90.32 % of the 31 noted to have MDD were less than 35 years old.
Patients with concomitant depression had a poorer quality of life not only psychologically
but in all subdomains compared to those who were not depressed.
Key Words: Depression, Antiretroviral Treatment, HIV, Person Living with HIV, Quality of
Life
51 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP ABSTRACT
DETERMINING THE PREVALENCE OF DEPRESSIVE AND ANXIETY
SYMPTOMS AMONG SELECTED PREGNANT PATIENTS IN SOME PARTS OF
LUZON DURING THE COVID-19 PANDEMIC: A CROSS- SECTIONAL STUDY
MARIE CRESANNE R. PAGADDU, M.D.
ABSTRACT
OBJECTIVES: This study explored the prevalence of depressive and anxiety symptoms
during the COVID-19 pandemic as well as the relationship between certain
sociodemographic factors these depressive and anxiety symptoms among the
participants.
METHODOLOGY: This research used a quantitative cross sectional study design. The
participants were selected through convenience and snowball sampling. They answered a
Sociodemographic Survey, Hamilton Anxiety Rating Scale and Hamilton Depression Rating
Scale. Frequency and Percentage were used to describe the sociodemographic
characteristics and to tabulate the prevalence of anxiety and depressive symptoms.
Ordinal Logistic Regression Analysis was used to determine the relationship between
certain sociodemographic factors and depressive and anxiety symptoms among the
participants.
RESULTS: Of the 212 women in this sample, 96.2% showed anxiety and 43.9% manifested
depressive symptoms during the COVID-19 Pandemic. Younger participants and those in
post- partum experienced higher levels of anxiety while those with lower educational
attainment had lower levels of anxiety as well as that of depression. Those with more
pregnancies were more likely to have higher levels of depression and those at 2nd and 3rd
Trimester of their pregnancy were less likely to develop higher levels of depression than
those during their postpartum period.
CONCLUSION: This study demonstrated that certain concerns during the pandemic
represented a significant risk factor for mental distress among pregnant women as well as
those who had just given birth. Screening of patients for possible psychiatric symptoms
and common concerns should be prioritized upon their routine ante-natal care. Support
measures must be considered for women during pregnancy or perinatal period to
safeguard this susceptible population.
KEYWORDS: Depression, Anxiety, Pregnancy, Postpartum Women, Covid 19 pandemic
52 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP ABSTRACT
RESILIENCE LEVELS AMONG FILIPINO NON-MEDICAL PERSONNEL AT A
TERTIARY GOVERNMENT HOSPITAL IN METRO MANILA DURING THE
COVID-19 PANDEMIC – JULY 2021
RAFAEL E. LEGASPI, MD,
CONSTANTINE D. DELLA, MD
ABSTRACT
OBJECTIVES: This study aimed to measure the resilience level of non-medical personnel
of the University of the Philippines Manila – Philippine General Hospital (UP-PGH) and
determine whether this was associated with sociodemographic factors such as gender,
length of service and job position.
METHODOLOGY: A cross-sectional study that included non-medical personnel using
convenience sampling via email was done. Data was obtained through the 14-item
Resilience Scale (RS-14) as well as a sociodemographic factors questionnaire. Descriptive
and non-parametric correlational analysis of data was used.
RESULTS: One hundred twenty five of the 153 respondents (81.70%) garnered a resilience
score of 74-98 or moderate to high resilience level, while 28 or 18.30% had a resilience
score corresponding to very low and on the low end. The mean resilience score was 81.8,
corresponding to a moderate resilience level. More women than men had a resilience level
of moderate to high. Respondents with greater than 5 years of work experience within the
hospital had higher resilience levels than those who were less experienced. Moderate to
high resilience levels were found in more administrative than non-administrative
personnel. No significant association was found between resilience level and the factors
analyzed. In terms of Resilience Core Characteristics, all comparisons between
demographic factors of interest and Self-reliance, Purpose, Equanimity, Perseverance and
Authenticity yielded insignificant results except for Self-reliance versus length of service,
which showed a weak but significant relationship. Exploratory factor analysis found that
the unidimensionality of the RS-14 Scale (US Version) still applied when administered to
Filipinos in this particular population.
CONCLUSION: Majority of the non- medical personnel of the UP -PGH had moderate level
of resilience. There was a lack of significant association between resilience level and
demographic characteristics like age, length of service, and position in the study sample.
In terms of Resilience Core Characteristics, comparison between length of service and
self -reliance showed a weak but significant relationship.
KEYWORDS: Resilience, Non- medical Hospital Personnel, Tertiary Government Hospital,
COVID -19 Pandemic
53 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP ABSTRACT
COMORBID SLEEP DISORDERS AMONG PATIENTS PRESENTING WITH
INSOMNIA WHO UNDERWENT
POLYSOMNOGRAPHY
APRIL FATIMA HERNANDEZ MD, FPPA, FPSSM
ROLAND DELA EVA MD, FPPS, FPAPP, FPSSM
ABSTRACT
OBJECTIVE: The aim of this study was to determine the comorbid sleep disorders on
Polysomnography (PSG) of patients complaining of insomnia symptoms.
METHODOLOGY: This is a retrospective study among patients who underwent diagnostic
and split-night polysomnography from April 2014 to February 2019. Those who had at
least one of the following insomnia symptoms of difficulty initiating sleep, difficulty
maintaining sleep and early morning awakening with or without a history of sleep aide use
were identified as patients with insomnia. Polysomnography sleep parameters and
outcome were tabulated and statistical analysis was done using SPSS v 20.0.
RESULTS: Out of the 302 patients who were included in the study, 34.4% of subjects had a
family history of sleep disorder and 70.4% had a history of sleep aide use. Among the
medical comorbidities, 47.7% of the subjects were diagnosed with hypertension while
10.65% were diagnosed with psychiatric disorder. Most of the patients complained of
both difficulty initiating sleep and early morning awakening. PSG sleep parameters
showed that patients did not experience excessive daytime sleepiness or delayed sleep
latency. On the other hand, poor sleep efficiency could be due to increased arousal index.
Half of the patients turned out to have severe obstructive sleep apnea (52%) while 2.3% of
the patients had periodic limb movement disorder. Among those diagnosed with severe
OSA, 53.3% had a history of sleep aide use.
CONCLUSION: The study showed the importance of screening patients with insomnia for
underlying comorbid sleep disorders. The American Academy of Sleep Medicine (AASM)
treatment guidelines for chronic insomnia emphasized the need to have a high index of
suspicion for this population in order to recommend diagnostic procedures such as
polysomnography. Diagnosing a patient with insomnia to have an underlying sleep apnea
and/or periodic limb movement disorder would change the course of management among
patients with chronic insomnia and eventually avoid prescribing medications that could
actually worsen the patient’s condition.
KEYWORDS: Insomnia, Sleep Disorders, Comorbidity in Sleep Problems,
Polysomnography
54 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
INFORMATION FOR CONTRIBUTORS TO THE PHILIPPINE JOURNAL
OF PSYCHIATRY 2017
The Philippine Journal of Psychiatry is a 2) A statement of financial or other
referred journal designed to meet the relationships that might lead to a conflict of
continuing education needs of practicing interest, if that information is not included in
psychiatrists in the Philippines. It is published the manuscript itself or in an authors’ form.
under the auspices of the Philippine
Psychiatric Association. The Philippine Journal 3) A statement that the manuscript has been
of Psychiatry accepts only original and read and approved by all the authors, that the
unpublished articles on psychology, requirements for authorship as stated earlier
psychiatry and other behavioral sciences with in this document have been met, and that
the understanding that that they have not each author believes that the manuscript
been published previously, nor being reviewed represents honest work.
or considered for publication elsewhere,
either as a whole or any substantial part. 4) The full name, postal & email address, cell
phone and telephone number of the
The corresponding author should inform the corresponding author, who is responsible for
editor in chief about all submissions to other communicating with the other authors about
publications and any previous reports that revisions and final approval of the proofs as
might be considered prior or duplicate well as with the editorial board of the PJP.
publications- including data or observations
already reported or patients already SUBMISSION OF MANUSCRIPTS
described- and should include copies of such Hard copy of manuscripts may be submitted
material for the editor to examine. in duplicate, typewritten using Times New
Manuscripts must be accompanied by a cover Roman font 11, double spaced with a minimum
letter, which should include the ff information: of 1.5” for margins on 8” x 11” (letter or short)
bond paper. All pages should be numbered. An
1) A full statement to the editor about all electronic form of the manuscript should be
submissions and previous reports that might stored in a document file- CD ReWritable disk
be regarded as redundant publication of the using Microsoft Word Program and submitted
same or very similar work. Any such work along with the duplicate hard copy. Send all
should be referred to specifically and copies of manuscript to the Editor- in -Chief or
referenced in the new paper. Copies of such to the PPA office. Please include all contact
material should be included with the numbers (residence & office telephone #, fax
submitted paper to help the editor address #, cell phone # and addresses (email,
the situation. residence/ office/ clinic) of the corresponding
55 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
author as well as the email & office/ clinic All forms of financial support, including drug
address and cell phone & landline telephone company support, are listed in the
numbers of ALL authors on the envelope acknowledgments section of the paper.
containing the manuscripts and disk.
Any affiliations or financial interests related to
REVIEW PROCESS subjects or services described in the paper- such
Manuscripts submitted to the PJP are sent for as employment, consultancies, stock ownership, or
blind review to at least 3 reviewers within a honoraria- or any financial relationships that may
week from date of receipt. The reviewers are suggest conflict of interest, are described. Such
given 2-4 weeks to review the manuscript. The interests do not mean automatic rejection of the
suggestions for revision are summarized and manuscript however they must be disclosed for
sent to the author for revision. A second or the editor’s information and for possible
third blind review may ensue until the paper is disclosure to reviewers.
deemed publishable by the editorial board.
The paper is then edited and shown to PREPARATION OF MANUSCRIPTS FOR RESEARCH
corresponding author prior to publication.The PAPERS, BRIEF REPORTS, LITERATURE REVIEWS &
corresponding author is encouraged to check SPECIAL ARTICLES
the edited manuscript for any errors, to answer
any queries of the manuscript editor or clarify Types of articles that can be submitted for
some details in the manuscript. Manuscripts publication to the Philippine Journal of Psychiatry
are accepted with the understanding that they are research reports, brief reports, literature
will be edited for clarity, elimination of reviews, special articles, case reports,
redundancy and conformity with the PJP commentaries, book reviews, monographs, letters
standards. and others.
DISCLOSURE & COPYRIGHT POLICY Manuscript may be submitted in English or
When paper is accepted, the Editor will send Pilipino, type written using New Times Roman font
the corresponding author an agreement and of 11 single spaced and with 1” margins on all sides
authorization from that states in essence that of 8” x 11” sized paper. Number the pages
the material is original, legal and has not been consecutively, placing the page number at the
previously published; that consent from all the lower right hand corner of each page, beginning
authors, when required, for permission to with the title page. The manuscript should be
publish has been obtained; that both the arranged as the ff: 1) Title, 2) Structured Abstract,
Philippine Journal of Psychiatry and the 3) Text, 4) Acknowledgments, 5) References, 6)
Philippine Psychiatric Association are harmless Tables & 7) Appendices. Enclose disclosure and
against any suit arising out of any alleged transfer of copyright duly signed by all the authors
breach of these warranties; that each of the and keep copies of everything submitted. The
authors has full responsibility for the content manuscript must be accompanied by copies of any
of the manuscript; and that the author permission to reproduce published material, to
authorizes the Philippine Psychiatric use illustrations or report information about
Association to publish the article and have the identifiable people or to name people for their
copyright. contributions.
56 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
Manuscripts may be sent through email to the of the study or observations and funding
PPA office, the Editor in Chief and/or the sources. The abstract should not exceed 250
Manuscript Editor. words and list up to 5 key words under which
article will be indexed.
I. Title Page should include a concise and
informative title, author’s name with highest III. Text should consist of Introduction,
academic degree as well as the name of Methods, Results and Discussion.
institution to which work can be attributed or
where research study was conducted. The title A. The INTRODUCTION should provide the
should include the study design especially for context and rationale or the study i.e. nature
randomized controlled trials i.e. any research of the problem and its significance. State the
project that prospectively assigns human specific purpose or research objectives of or
subjects to intervention or concurrent hypothesis being tested by the study. The
comparison or control groups to study the research objective may be stated as a
cause and effect relationship between a question.
medical intervention and a health outcome.
B. The METHODOLOGY section should
Include the name, telephone & cell phone describe how and why the study was done in a
numbers, mailing & email addresses of the particular way in as much detail about the
author responsible for correspondence about Study Design and with enough Technical
the manuscript and the author to whom Information that would allow others to
requests for reprints should be addressed. reproduce the results.
Sources of support in the form of grants, Methods for Selection of study population i.e.
equipment, drugs or all these should also be inclusion & exclusion criteria, data collection,
included. If paper was presented at a national and data analysis procedure should be
or international meeting, full details of the concisely yet easily understandable to the
meetings should be stated such as title, place readers.
and date.
Description of Study Participants should
II. Structured ABSTRACT should include: include the Source Population, explain
OBJECTIVES- purpose of the study or research relevance of inclusion / exclusion criteria and
question; METHODOLOGY- study design, demographic variables chosen e.g. why choose
selection process, setting, subjects, to study only women from 40- 60 years old.
observational and analytical methods, How variables were measured may also be
intervention(s) if any and main outcome important to specify.
measure(s); RESULTS- main findings of
research in relation to objectives stated and Describe the Statistical Methods with enough
give the statistical significance of detail to enable knowledgeable reader with
observations; & CONCLUSION- primary access to the original data to verify the
conclusions with emphasis on new and reported results. When possible, quantify
important aspects findings and present them with appropriate
57 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
indicators of measurement error or each table column and brief title for each
uncertainty i.e. confidence intervals. Define table above the table.Explanation or
statistical terms, abbreviations and symbols discussion of results in the table should be
used as well as specify the computer software placed before the Table and place Table
used. number referred to after paragraph where it is
mentioned e.g. (Table 1).
Ethical Considerations for the protection of
human subjects and animals in the research Figures should be as self explanatory as
should be indicated as when informed consent possible. Figures accepted for publication
was obtained and if the procedures followed must be clear, uncluttered, and two-
were in accordance with the ethical standards dimensional. Figure number and title should
of the responsible committee on human be placed below the figure. Explanations for
experimentation (institutional and national) as the Figures are placed after the Figure and
well as with the Helsinki Declaration of 1975 as indicate in parenthesis which Figure was being
revised in 2008. Do not use patient’s names, described e.g. (Figure 2)
initials, or hospital numbers, especially in
illustrative material. For x-ray films, scans and other diagnostic
images as well as pictures of pathology
C. The RESULTS should report only the specimens or photomicrographs, send sharp,
findings related directly to the research glossy, black and white or color photographic
objectives. Give numeric results as absolute prints 5 x 7 inches or 127 x 173 mm in camera
numbers and as percentages as well as how ready form. The names of the authors should
they were statistically analyzed. Use metric or be written at the back of each plate.
S.I. units of measurement and specify all units
of measurement clearly. Use only standard Photomicrographs should have internal scale
abbreviations. markers. Titles and detailed explanations
should be placed in the legends not on the
Include Tables & Figures only if they present illustrations themselves. Explain the internal
relevant numerical data more clearly than scale and identify the method of staining in
could be done in the text. Do not repeat all the photomicrographs.
data in tables, graphs or illustrations in the
text, where only the most important When symbols, arrows, numbers or letters are
observations are summarized. Label tables & used to identify parts of the illustrations,
figures appropriately and number identify
consecutively in order of their first citation in and explain each one clearly in the legend.
the text using Arabic numerals. Be sure that Please list on a separate page, values for the
each table and figure is cited in the text data points shown on graphs, in case the
otherwise don’t include it. reviewers/editors of the journal has to
recreate some figures. When reporting
Cell alignment of Tables should be to top left, statistically significant results, always report
single spaced or autofitted to contents of cell the observed test statistic value, degrees of
with all grid lines visible. Place a heading for freedom, probability level, and for t & F tests,
58 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
whether repeated measures were used. these to material that has already been
published, accepted for publication or
Supplementary materials and technical detail presented at a major national meeting.
can be placed in an APPENDIX where they will
be accessible but do not interrupt the flow of Citations of material in press must include
the text. Appendices are numbered in journal or publisher’s name followed by “in
sequence of how they are referred to in the press” or forthcoming”. If unpublished
text e.g. (Appendix 3). Checklists and material is cited indicate source and year in
questionnaires are generally not published. parenthesis in the text or written as a
footnote.
D. The DISCUSSION should emphasize the new
and important aspects of the study and the Avoid citing a “personal communication“
conclusions that follow from them. Link the unless it provides essential information
conclusions with the goals of the study but unavailable from a public source, in which
avoid unqualified statement or conclusions case the name of the person and date of
not supported by your data. communication should be cited in
Recommendations when appropriate may be parentheses in the text. For scientific articles,
included. Do not repeat study results in the obtain written permission and confirmation of
discussion but rather give explanations for the accuracy from the source of a personal
findings, compare and contrast the results communication.
with other relevant studies and state the
limitations of the study. Explore the Avoid using abstracts as references. Accuracy
implications of the findings for future research of the citation is the author’s responsibility.
and for clinical practice. Abbreviations of journal names should
conform to those used in Index Medicus.
E. ACKNOWLEDGMENTS. Disclosure
statements of sponsoring body may be Examples:
required for studies promoting products or
services described in the paper. One or more Articles in Journals (see also #36. Journal
statements should specify contributions that article on the Internet)
need acknowledging but do not justify
authorship such as emotional, financial, 1. Standard journal article
material or technical support. The List All authors if 6 or less: Surname and
corresponding author should submit the initials of all authors, tile of article, name of
written permission to be acknowledged from journal, year, volume & first and last pages.
all acknowledged individuals before printing. Halpern SD, Ubel PA, Caplan AL. Solid-organ
transplantation in HIV-infected patients. N
F. REERENCES: Only relevant references, Engl J Med. 2002 Jul 25;347(4):284-7.
preferably from original researches should be
cited in the text and listed according to their
order of appearance in the text using Arabic
numerals in parenthesis or superscript. Limit
59 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
If more than six authors, list only the first 6 of multi-species conserved sequences.
authors and add “et al”: Genome Res. 2003 Dec;13(12):2507-18.
Rose ME, Huerbin MB, Melick J, Marion DW,
Palmer AM, Schiding JK, et al. Regulation of 4. No author given
interstitial excitatory amino acid 21st century heart solution may have a sting in
concentrations after cortical contusion injury. the tail. BMJ. 2002;325(7357):184.
Brain Res. 2002;935(1-2):40-6.
5. Article not in English
Optional addition of a database's unique Ellingsen AE, Wilhelmsen I. Sykdomsangst
identifier for the citation: blant medisin- og jusstudenter. Tidsskr Nor
Forooghian F, Yeh S, Faia LJ, Nussenblatt RB. Laegeforen. 2002;122(8):785-7. Norwegian.
Uveitic foveal atrophy: clinical features and
associations. Arch Ophthalmol. 2009 Optional translation of article title
Feb;127(2):179-86. PubMed PMID: 19204236; (MEDLINE/PubMed practice):
PubMed Central PMCID: PMC2653214. Ellingsen AE, Wilhelmsen I. [Disease anxiety
among medical students and law students].
Optional addition of a clinical trial registration Tidsskr Nor Laegeforen. 2002 Mar
number: 20;122(8):785-7. Norwegian.
Trachtenberg F, Maserejian NN, Soncini JA,
Hayes C, Tavares M. Does fluoride in 6. Volume with supplement
toothpaste prevent future caries in children? J Geraud G, Spierings EL, Keywood C.
Dent Res. 2009 Mar;88(3):276-9. PubMed Tolerability and safety of frovatriptan with
PMID: 19329464. ClinicalTrials.gov registration short- and long-term use for treatment of
number: NCT00065988. migraine and in comparison with sumatriptan.
Headache. 2002;42 Suppl 2:S93-9.
2. Organization as author
Diabetes Prevention Program Research Group. 7. Issue with supplement
Hypertension, insulin, and proinsulin in Glauser TA. Integrating clinical trial data into
participants with impaired glucose tolerance. clinical practice. Neurology. 2002;58(12 Suppl
Hypertension. 2002;40(5):679-86. 7):S6-12.
3. Both personal authors and organization as
author (List all as they appear in the byline.) 8. Volume with part
Vallancien G, Emberton M, Harving N, van Abend SM, Kulish N. The psychoanalytic
Moorselaar RJ; Alf-One Study Group. Sexual method from an epistemological viewpoint. Int
dysfunction in 1,274 European men suffering J Psychoanal. 2002; 83(Pt 2):491-5.
from lower urinary tract symptoms. J Urol.
2003;169(6):2257-61. 9. Issue with part
Ahrar K, Madoff DC, Gupta S, Wallace MJ, Price
Margulies EH, Blanchette M; NISC RE, Wright KC. Development of a large animal
Comparative Sequencing Program, Haussler D, model for lung tumors. J Vasc Interv Radiol.
Green ED. Identification and characterization 2002;13(9 Pt 1):923-8.
60 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
10. Issue with no volume 15. Article retracted
Banit DM, Kaufer H, Hartford JM. Feifel D, Moutier CY, Perry W. Safety and
Intraoperative frozen section analysis in tolerability of a rapidly escalating dose-
revision total joint arthroplasty. Clin Orthop. loading regimen for risperidone. J Clin
2002;(401):230-8. Psychiatry. 2000;61(12):909-11. Retraction in:
Feifel D, Moutier CY, Perry W. J Clin
11. No volume or issue Psychiatry. 2002;63(2):169.
Outreach: bringing HIV-positive individuals
into care. HRSA Careaction. 2002 Jun:1-6. 16. Article republished with corrections
Mansharamani M, Chilton BS. The
12. Pagination in roman numerals reproductive importance of P-type ATPases.
Chadwick R, Schuklenk U. The politics of Mol Cell Endocrinol. 2002;188(1-2):22-5.
ethical consensus finding. Bioethics. Corrected and republished from: Mol Cell
2002;16(2):iii-v. Endocrinol. 2001;183(1-2):123-6.
13. Type of article indicated as needed 17. Article with published erratum
Tor M, Turker H. International approaches to Malinowski JM, Bolesta S. Rosiglitazone in the
the prescription of long-term oxygen therapy treatment of type 2 diabetes mellitus: a critical
[letter]. Eur Respir J. 2002;20(1):242. review. Clin Ther. 2000;22(10):1151-68;
discussion 1149-50. Erratum in: Clin Ther.
Lofwall MR, Strain EC, Brooner RK, Kindbom 2001;23(2):309.
KA, Bigelow GE. Characteristics of older
methadone maintenance (MM) patients 18. Article published electronically ahead of
[abstract]. Drug Alcohol Depend. 2002;66 the print version
Suppl 1:S105. Yu WM, Hawley TS, Hawley RG, Qu CK.
Immortalization of yolk sac-derived precursor
14. Article containing retraction cells. Blood. 2002 Nov 15;100(10):3828-31.
Feifel D, Moutier CY, Perry W. Safety and Epub 2002 Jul 5.
tolerability of a rapidly escalating dose-
loading regimen for risperidone. J Clin Books and Other Monographs
Psychiatry. 2002;63(2):169. Retraction of: 19. Personal author(s)
Feifel D, Moutier CY, Perry W. J Clin Murray PR, Rosenthal KS, Kobayashi GS,
Psychiatry. 2000;61(12):909-11. Pfaller MA. Medical microbiology. 4th ed. St.
Louis: Mosby; 2002.
Article partially retracted:
Starkman JS, Wolter C, Gomelsky A, Scarpero 20. Editor(s), compiler(s) as author
HM, Dmochowski RR. Voiding dysfunction Gilstrap LC 3rd, Cunningham FG, VanDorsten
following removal of eroded synthetic mid JP, editors. Operative obstetrics. 2nd ed. New
urethral slings. J Urol. 2006 Sep;176(3):1040- York: McGraw-Hill; 2002.
4. Partial retraction in: Starkman JS, Wolder
CE, Gomelsky A, Scarpero HM, Dmochowski
RR. J Urol. 2006 Dec;176(6 Pt 1):2749.
61 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
10. Issue with no volume 15. Article retracted
Banit DM, Kaufer H, Hartford JM. Feifel D, Moutier CY, Perry W. Safety and
Intraoperative frozen section analysis in tolerability of a rapidly escalating dose-
revision total joint arthroplasty. Clin Orthop. loading regimen for risperidone. J Clin
2002;(401):230-8. Psychiatry. 2000;61(12):909-11. Retraction in:
Feifel D, Moutier CY, Perry W. J Clin
11. No volume or issue Psychiatry. 2002;63(2):169.
Outreach: bringing HIV-positive individuals
into care. HRSA Careaction. 2002 Jun:1-6. 16. Article republished with corrections
Mansharamani M, Chilton BS. The
12. Pagination in roman numerals reproductive importance of P-type ATPases.
Chadwick R, Schuklenk U. The politics of Mol Cell Endocrinol. 2002;188(1-2):22-5.
ethical consensus finding. Bioethics. Corrected and republished from: Mol Cell
2002;16(2):iii-v. Endocrinol. 2001;183(1-2):123-6.
13. Type of article indicated as needed 17. Article with published erratum
Tor M, Turker H. International approaches to Malinowski JM, Bolesta S. Rosiglitazone in the
the prescription of long-term oxygen therapy treatment of type 2 diabetes mellitus: a critical
[letter]. Eur Respir J. 2002;20(1):242. review. Clin Ther. 2000;22(10):1151-68;
discussion 1149-50. Erratum in: Clin Ther.
Lofwall MR, Strain EC, Brooner RK, Kindbom 2001;23(2):309.
KA, Bigelow GE. Characteristics of older
methadone maintenance (MM) patients 18. Article published electronically ahead of
[abstract]. Drug Alcohol Depend. 2002;66 the print version
Suppl 1:S105. Yu WM, Hawley TS, Hawley RG, Qu CK.
Immortalization of yolk sac-derived precursor
14. Article containing retraction cells. Blood. 2002 Nov 15;100(10):3828-31.
Feifel D, Moutier CY, Perry W. Safety and Epub 2002 Jul 5.
tolerability of a rapidly escalating dose-
loading regimen for risperidone. J Clin Books and Other Monographs
Psychiatry. 2002;63(2):169. Retraction of: 19. Personal author(s)
Feifel D, Moutier CY, Perry W. J Clin Murray PR, Rosenthal KS, Kobayashi GS,
Psychiatry. 2000;61(12):909-11. Pfaller MA. Medical microbiology. 4th ed. St.
Louis: Mosby; 2002.
Article partially retracted:
Starkman JS, Wolter C, Gomelsky A, Scarpero 20. Editor(s), compiler(s) as author
HM, Dmochowski RR. Voiding dysfunction Gilstrap LC 3rd, Cunningham FG, VanDorsten
following removal of eroded synthetic mid JP, editors. Operative obstetrics. 2nd ed. New
urethral slings. J Urol. 2006 Sep;176(3):1040- York: McGraw-Hill; 2002.
4. Partial retraction in: Starkman JS, Wolder
CE, Gomelsky A, Scarpero HM, Dmochowski
RR. J Urol. 2006 Dec;176(6 Pt 1):2749.
62 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
21. Author(s) and editor(s) on Genetic Programming; 2002 Apr 3-5;
Breedlove GK, Schorfheide AM. Adolescent Kinsdale, Ireland. Berlin: Springer; 2002. p.
pregnancy. 2nd ed. Wieczorek RR, editor. 182-91.
White Plains (NY): March of Dimes Education
Services; 2001. 26. Scientific or technical report
Issued by funding/sponsoring agency:
22. Organization(s) as author Yen GG (Oklahoma State University, School of
Advanced Life Support Group. Acute medical Electrical and Computer Engineering,
emergencies: the practical approach. London: Stillwater, OK). Health monitoring on vibration
BMJ Books; 2001. 454 p. signatures. Final report. Arlington (VA): Air
Force Office of Scientific Research (US), Air
American Occupational Therapy Association, Force Research Laboratory; 2002 Feb. Report
Ad Hoc Committee on Occupational Therapy No.: AFRLSRBLTR020123. Contract No.:
Manpower. Occupational therapy manpower: F496209810049.
a plan for progress. Rockville (MD): The
Association; 1985 Apr. 84 p. Issued by performing agency:
National Lawyers’ Guild AIDs Network (US); Russell ML, Goth-Goldstein R, Apte MG, Fisk
National Gay Rights Advocates (US). AIDS WJ. Method for measuring the size distribution
practice manual: a legal and educational guide. of airborne Rhinovirus. Berkeley (CA):
2nd ed. San Francisco: The Network; 1988. Lawrence Berkeley National Laboratory,
Environmental Energy Technologies Division;
23. Chapter in a book 2002 Jan. Report No.: LBNL49574. Contract
Meltzer PS, Kallioniemi A, Trent JM. No.: DEAC0376SF00098. Sponsored by the
Chromosome alterations in human solid Department of Energy.
tumors. In: Vogelstein B, Kinzler KW, editors.
The genetic basis of human cancer. New York: 27. Dissertation
McGraw-Hill; 2002. p. 93-113. Borkowski MM. Infant sleep and feeding: a
telephone survey of Hispanic Americans
24. Conference proceedings [dissertation]. Mount Pleasant (MI): Central
Harnden P, Joffe JK, Jones WG, editors. Germ Michigan University; 2002.
cell tumours V. Proceedings of the 5th Germ
Cell Tumour Conference; 2001 Sep 13-15; 28. Patent
Leeds, UK. New York: Springer; 2002. Pagedas AC, inventor; Ancel Surgical R&D Inc.,
assignee. Flexible endoscopic grasping and
25. Conference paper cutting device and positioning tool assembly.
Christensen S, Oppacher F. An analysis of United States patent US 20020103498. 2002
Koza's computational effort statistic for Aug 1.
genetic programming. In: Foster JA, Lutton E,
Miller J, Ryan C, Tettamanzi AG, editors. Other Published Material
Genetic programming. Euro GP 2002: 29. Newspaper article
Proceedings of the 5th European Conference Tynan T. Medical improvements lower
63 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
homicide rate: study sees drop in assault rate. Tian D, Araki H, Stahl E, Bergelson J, Kreitman
The Washington Post. 2002 Aug 12;Sect. A:2 M. Signature of balancing selection in
(col. 4). Arabidopsis. Proc Natl Acad Sci U S A.
Forthcoming 2002.
30. Audiovisual material
Chason KW, Sallustio S. Hospital preparedness Electronic Material
for bioterrorism [videocassette]. Secaucus 35. CD-ROM
(NJ): Network for Continuing Medical Anderson SC, Poulsen KB. Anderson's
Education; 2002. electronic atlas of hematology [CD-ROM].
Philadelphia: Lippincott Williams & Wilkins;
31. Legal Material 2002.
Public law:
Veterans Hearing Loss Compensation Act of 36. Journal article on the Internet
2002, Pub. L. No. 107-9, 115 Stat. 11 (May 24, Abood S. Quality improvement initiative in
2001). nursing homes: the ANA acts in an advisory
role. Am J Nurs [Internet]. 2002 Jun [cited
Unenacted bill: 2002 Aug 12];102(6):[about 1 p.]. Available
Healthy Children Learn Act, S. 1012, 107th from:http://www.nursingworld.org/AJN/2002/j
Cong., 1st Sess. (2001). une/Wawatch.htmArticle
Code of Federal Regulations:
Cardiopulmonary Bypass Intracardiac Suction Optional presentation (omits bracketed
Control, 21 C.F.R. Sect. 870.4430 (2002). phrase that qualifies the journal title
abbreviation):
Hearing: Abood S. Quality improvement initiative in
Arsenic in Drinking Water: An Update on the nursing homes: the ANA acts in an advisory
Science, Benefits and Cost: Hearing Before the role. Am J Nurs. 2002 Jun [cited 2002 Aug
Subcomm. on Environment, Technology and 12];102(6):[about 1 p.]. Available
Standards of the House Comm. on Science, from:http://www.nursingworld.org/AJN/2002/j
107th Cong., 1st Sess. (Oct. 4, 2001). une/Wawatch.htmArticle
Article published on the Internet ahead of the
32. Map print version:
Pratt B, Flick P, Vynne C, cartographers. See # 18.
Biodiversity hotspots [map]. Washington:
Conservation International; 2000. Optional formats used by NLM in
MEDLINE/PubMed:
33. Dictionary and similar references
Dorland's illustrated medical dictionary. 29th Article with document number in place of
ed. Philadelphia: W.B. Saunders; 2000. traditional pagination:
Filamin; p. 675. Williams JS, Brown SM, Conlin PR. Videos in
clinical medicine. Blood-pressure
Unpublished Material measurement. N Engl J Med. 2009 Jan
34. In press or Forthcoming 29;360(5):e6. PubMed PMID: 19179309.
64 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
Article with a Digital Object Identifier (DOI): American Board of Medical Specialists. c2000
Zhang M, Holman CD, Price SD, Sanfilippo FM, - [cited 2001 Mar 8]. Available from:
Preen DB, Bulsara MK. Comorbidity and repeat http://www.abms.org/newsearch.asp
admission to hospital for adverse drug
reactions in older adults: retrospective cohort Closed database:
study. BMJ. 2009 Jan 7;338:a2752. doi: Jablonski S. Online Multiple Congenital
10.1136/bmj.a2752. PubMed PMID: 19129307; Anomaly/Mental Retardation (MCA/MR)
PubMed Central PMCID: PMC2615549. Syndromes [Internet]. Bethesda (MD): National
Library of Medicine (US); c1999 [updated 2001
Article with unique publisher item identifier Nov 20; cited 2002 Aug 12]. Available from:
(pii) in place of traditional pagination or DOI: http://www.nlm.nih.gov/archive//20061212/m
Tegnell A, Dillner J, Andrae B. Introduction of esh/jablonski/syndrome_title.html
human papillomavirus (HPV) vaccination in
Sweden. Euro Surveill. 2009 Feb 12;14(6). pii: 41. Part of a database on the Internet
19119. PubMed PMID: 19215721. MeSH Browser [Internet]. Bethesda (MD):
National Library of Medicine (US); 2002 - .
37. Monograph on the Internet Meta-analysis [cited 2008 Jul 24]; [about 2 p.].
Foley KM, Gelband H, editors. Improving Available from:
palliative care for cancer [Internet]. http://www.nlm.nih.gov/cgi/mesh/2008/MB_cg
Washington: National Academy Press; 2001 i?mode=&index=16408&view=concept MeSH
[cited 2002 Jul 9]. Available from: Unique ID: D017418.
http://www.nap.edu/books/0309074029/html
/. 42. Blogs
Holt M. The Health Care Blog [Internet]. San
38. Homepage/Web site Francisco: Matthew Holt. 2003 Oct - [cited
Cancer-Pain.org [Internet]. New York: 2009 Feb 13]. Available
Association of Cancer Online Resources, Inc.; from:http://www.thehealthcareblog.com/the_
c2000-01 [updated 2002 May 16; cited 2002 health_care_blog/.
Jul 9]. Available from: http://www.cancer-
pain.org/. KidneyNotes.com [Internet]. New York:
KidneyNotes. c2006 - [cited 2009 Feb 13].
39. Part of a homepage/Web site Available from: http://www.kidneynotes.com/.
American Medical Association [Internet].
Chicago: The Association; c1995-2002 Wall Street Journal. HEALTH BLOG: WSJ's blog
[updated 2001 Aug 23; cited 2002 Aug 12]. on health and the business of health
AMA Office of Group Practice Liaison; [about 2 [Internet]. Hensley S, editor. New York: Dow
screens]. Available from: http://www.ama- Jones & Company, Inc. c2007 - [cited 2009
assn.org/ama/pub/category/1736.html Feb 13]. Available from:
http://blogs.wsj.com/health/.
40. Database on the Internet
Open database: Contribution to a blog:
Who's Certified [Internet]. Evanston (IL): The Mantone J. Head trauma haunts many,
65 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
researchers say. 2008 Jan 29 [cited 2009 Feb Initial Symptoms of the patient, Family &
13]. In: Wall Street Journal. HEALTH BLOG Developmental History, Pre morbid Medical
[Internet]. New York: Dow Jones & Company, History, Initial Examination, Treatment and
Inc. c2008 - . [about 1 screen]. Available from: course of Illness and Discussion.
http://blogs.wsj.com/health/2008/01/29/head & 2) Case Report – Abstract, Introduction
-trauma-haunts-many-researchers-say/. which includes a Literature Review, Case
description in terms of history, Mental Status
Campbell A. Diabetes and alcohol: do the two Exam, Diagnosis and Discussion of the case.
mix? (Part 2). 2008 Jan 28 [cited 2009 Feb 13]. But in either format the ff: must be included:
In: Diabetes Self-Management Blog [Internet]. an unstructured Abstract of a maximum of
New York: Diabetes Self-Management. [2006 100 words, brief Literature Review,
Aug 14] - . 2 p. Available from: description of the case, its treatment/
http://www.diabetesselfmanagement.com/blo management and discussion of analysis
g/Amy_Campbell/Diabetes_and_Alcohol_Do_th (psychodynamics) and at least 10 references.
e_Two_Mix_Part_2 Authors must protect patient anonymity and
disguise their identifying information.
Reider J. Docnotes: Health, Technology,
Family Medicine and other observations Commentaries may be up to a maximum of
[Internet]. [place unknown]: Jacob Reider. 1200 words, and include at least 10
1999 - . CRP again ...; 2004 Apr 2 [cited 2009 references. Authors may be asked for source
Feb 13]; [about 1 screen]. Available from: material to support factual statements in
http://www.docnotes.com/2004/04/crp- opinion pieces.
again.html
Book Reviews may be on books dealing with
More detailed information on how to cite any topic or issue related to or of interest to
references can be found in Citing Medicine. psychiatry, psychology or mental health.
Note Appendix F which covers how citations in Indicate book title, authors/ editors, city
MEDLINE/PubMed differ from the advice where it was published, year published,
inCiting Medicine. publisher, total number of pages and sale
price of book reviewed. References are
PREPARATION OF MANUSCRIPTS FOR CASE optional.
REPORTS, COMMENTARIES, BOOK REVIEWS,
MONOGRAPHS &LETTERS TO THE EDITOR: Letters are published at the editor’s discretion
Case Reports may adapt either of the 2 and should not exceed 500 words, with at
formats: 1) Clinical Case Conference- least 5 references. Letters related to material
Introduction based on Literature Review, published in PJP may be sent to the author
Initial Symptoms of the patient, Family & themselves for possible reply.
Developmental History, Pre morbid Medical
History, Initial Examination, Treatment and REFERENCES:
course of Illness and Discussion. International Committee of Medical Journal
& 2) Case Report – Abstract, Introduction Editors. [home page on the internet].
which includes a Literature Review, Initial Recommendations for the conduct,
66 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
PJP FOR CONTRIBUTORS
Reporting, Editing and Publication of Scholarly
Work in Medical Journals [cited 2016 Dec 24]
Available from: http;//www.ICMJE.org.
2.World Medical Association. World Medical
Association Declaration of Helsinki: Ethical
Principles for Medical Research Involving
Human Subjects. JAMA.2013;310 (20):2191-
94.doi.10.1001/jama.20132810
67 · PJP 2023 · Volume 4 (2) · ISSN 2980-4884
You might also like
- Philippine National Formulary 8thED PDFDocument800 pagesPhilippine National Formulary 8thED PDFGio Mari Marcial100% (3)
- The Healing Codes - Heart Issues FinderDocument10 pagesThe Healing Codes - Heart Issues FinderVladianu Dan100% (1)
- Elliott Eisner Ex Imp NullDocument1 pageElliott Eisner Ex Imp Nullapi-227888640100% (1)
- HUMSS - Q3 - Trends - Mod4 - Understanding Strategic Analysis and Intuitive ThinkingDocument24 pagesHUMSS - Q3 - Trends - Mod4 - Understanding Strategic Analysis and Intuitive ThinkingChernie Deroma Obsenares91% (43)
- Health Psychology An Interdisciplinary Approach To Health 2nd Edition Deborah Test BankDocument31 pagesHealth Psychology An Interdisciplinary Approach To Health 2nd Edition Deborah Test BankJosephMartinezwgrin100% (14)
- CPG Gestational Trophoblastic DiseasesDocument31 pagesCPG Gestational Trophoblastic DiseasesSMR50% (2)
- Case Report: Psychotic Disorder Due To EpilepsyDocument8 pagesCase Report: Psychotic Disorder Due To EpilepsyAshraf IlmanNo ratings yet
- Philippine Journal of Nursing ManuscriptDocument28 pagesPhilippine Journal of Nursing ManuscriptCarlo Paul Castro SanaNo ratings yet
- Philippine Journal of Psychiatry - Volume 4, Issue 2Document64 pagesPhilippine Journal of Psychiatry - Volume 4, Issue 2Sedric FactorNo ratings yet
- PJP 2021 - Volume 2 (1-2)Document80 pagesPJP 2021 - Volume 2 (1-2)Sedric FactorNo ratings yet
- PJP 2023 - Volume 4 (1-2)Document64 pagesPJP 2023 - Volume 4 (1-2)Sedric Factor100% (1)
- Khay Anne L. Aliazas, R.N.Document1 pageKhay Anne L. Aliazas, R.N.Rovianne Joy del MoroNo ratings yet
- Spine Society-NeuroDocument1 pageSpine Society-NeuroSushmica BaquiranNo ratings yet
- 7 11 PB PDFDocument84 pages7 11 PB PDF2B - CELESTE, RUSSEL JASTINENo ratings yet
- Early Cutting - RiveraDocument1 pageEarly Cutting - RiveraSushmica BaquiranNo ratings yet
- Fe Del Mundo Global Health Institute: Philip P. Ines, RNDocument2 pagesFe Del Mundo Global Health Institute: Philip P. Ines, RNYosef OxinioNo ratings yet
- CPG of Leptospirosis Final VersionDocument128 pagesCPG of Leptospirosis Final VersionxtineNo ratings yet
- Graduation Programme 2020Document1 pageGraduation Programme 2020Bobet ReñaNo ratings yet
- Pna Convention 2016 ProgrammeDocument3 pagesPna Convention 2016 ProgrammernrmmanphdNo ratings yet
- Letter Invi For Participants PNARizal MYC 2019Document5 pagesLetter Invi For Participants PNARizal MYC 2019Fitz JaminitNo ratings yet
- PHA 69th Annual National Convention ProgramDocument12 pagesPHA 69th Annual National Convention ProgramMenGuitarNo ratings yet
- Lista de Alunos e Programaã Ã oDocument12 pagesLista de Alunos e Programaã Ã oLuciana MacedoNo ratings yet
- Division of UrologyDocument1 pageDivision of UrologyJune LorenzanaNo ratings yet
- Chasan Taber2008Document10 pagesChasan Taber2008Tudor MotasNo ratings yet
- The Relationship Among Mental Health Status (GHQ-12), Health Related Quality of Life (EQ-5D) and Health-State Utilities in A General PopulationDocument12 pagesThe Relationship Among Mental Health Status (GHQ-12), Health Related Quality of Life (EQ-5D) and Health-State Utilities in A General PopulationNewton BernoullyNo ratings yet
- IFNAH 2020 JouraldistributionDocument64 pagesIFNAH 2020 JouraldistributionmeanyhannahNo ratings yet
- Health - 19-02-06 MEDICAL CANNABIS PDFDocument104 pagesHealth - 19-02-06 MEDICAL CANNABIS PDFJamielyn DilidiliNo ratings yet
- Health - 19-02-06 MEDICAL CANNABIS PDFDocument104 pagesHealth - 19-02-06 MEDICAL CANNABIS PDFJamielyn Dilidili100% (1)
- O Sintoma Na Medicina e Na PsicanáliseDocument8 pagesO Sintoma Na Medicina e Na PsicanáliseBrunoDhaniel Caprari Spadoni FerreiraNo ratings yet
- Ca PsychiaDocument105 pagesCa PsychiaDenise Joy15No ratings yet
- María Eugenia InglesDocument2 pagesMaría Eugenia InglesbassomariaeugeniaNo ratings yet
- Front EnglishDocument1 pageFront EnglishRachel Beatriz MarvaNo ratings yet
- Southwestern University Medical CenterDocument2 pagesSouthwestern University Medical CentercyNo ratings yet
- Case FormatDocument6 pagesCase FormatCatherine MetraNo ratings yet
- Marriage & Family Counselor or Social WorkDocument4 pagesMarriage & Family Counselor or Social Workapi-78065862No ratings yet
- What We Can Learn From Shamanic Healing: Brief Psychotherapy With Latino Immigrant ClientsDocument3 pagesWhat We Can Learn From Shamanic Healing: Brief Psychotherapy With Latino Immigrant ClientsnasimhsNo ratings yet
- Red Band Aid HIV - AIDS Awareness Poster PDFDocument1 pageRed Band Aid HIV - AIDS Awareness Poster PDFMSUVirtual NurseNo ratings yet
- Handbook of Cultural Factors in Behavioral Health: A Guide for the Helping ProfessionalFrom EverandHandbook of Cultural Factors in Behavioral Health: A Guide for the Helping ProfessionalLorraine T. BenutoNo ratings yet
- CP 4Document18 pagesCP 4Rubina MasihNo ratings yet
- Section of Rheumatology: East Avenue, Quezon City 1100, PhilippinesDocument6 pagesSection of Rheumatology: East Avenue, Quezon City 1100, PhilippinesSumayyah Mautante MuslimenNo ratings yet
- Espole-Muhat FinalexamDocument16 pagesEspole-Muhat FinalexamJaja Jr. Evasco EmbarqueNo ratings yet
- VPD HandbookDocument88 pagesVPD HandbookfrhucovidNo ratings yet
- Community Acquired Pneumonia - AdultDocument13 pagesCommunity Acquired Pneumonia - Adultmits98No ratings yet
- CP 3Document18 pagesCP 3Rubina MasihNo ratings yet
- Front Tagalog2Document1 pageFront Tagalog2Rachel Beatriz MarvaNo ratings yet
- UntitledDocument8 pagesUntitledALESNo ratings yet
- BeActive Feb2008-EnwDocument48 pagesBeActive Feb2008-EnwSynergy Taman ratuNo ratings yet
- 24 1 08Document44 pages24 1 08Mohamed Abou El hassanNo ratings yet
- ADA 2018 Diabetes CareDocument150 pagesADA 2018 Diabetes CareRoberto López Mata100% (1)
- Maia Birthing Home: "Caring For Your Health & Wellness"Document1 pageMaia Birthing Home: "Caring For Your Health & Wellness"Imelda NatividadNo ratings yet
- Organizational Chart DesignDocument8 pagesOrganizational Chart DesignMedical ward CvmcNo ratings yet
- Page 1 Health Systems ComposDocument1 pagePage 1 Health Systems ComposJohn Philip TiongcoNo ratings yet
- Medicine Men Tambalans in Maasin So. Leyte Philippines - Their Beliefs and Practices - Warlita K. GalDocument14 pagesMedicine Men Tambalans in Maasin So. Leyte Philippines - Their Beliefs and Practices - Warlita K. Galmaile100% (1)
- Jurnal Terapi Musik 3Document5 pagesJurnal Terapi Musik 3GITA WIBOWONo ratings yet
- Compara 3 ModalidadesDocument16 pagesCompara 3 ModalidadesEthamx RobertoNo ratings yet
- NTRL Manual On Collection, Storage & Transport of Specimens For TB Testing - 2nd EdDocument48 pagesNTRL Manual On Collection, Storage & Transport of Specimens For TB Testing - 2nd EdOspital ng Paranaque 2 Molecular LaboratoryNo ratings yet
- Ca N A D I A N J O U R N A L O F Public HealthDocument48 pagesCa N A D I A N J O U R N A L O F Public Healthbhawna_aroraNo ratings yet
- The Health Ritual of "Pag-Aanito" Among The Aetas of Nabuclod, Pampanga, Philippines PDFDocument7 pagesThe Health Ritual of "Pag-Aanito" Among The Aetas of Nabuclod, Pampanga, Philippines PDFJomari CosgafaNo ratings yet
- The Influence of Social and Spiritual Support Based On Bali Culture On The Depression Level of 'Napza Use' Patient in Psychiatric Hospital Bali ProvinceDocument6 pagesThe Influence of Social and Spiritual Support Based On Bali Culture On The Depression Level of 'Napza Use' Patient in Psychiatric Hospital Bali Provinceallika NurNo ratings yet
- Identificacion de DepresionDocument43 pagesIdentificacion de DepresionEnriqueAlemanNo ratings yet
- Bicol Regional Training and Teaching Hospital Internal Medicine DepartmentDocument1 pageBicol Regional Training and Teaching Hospital Internal Medicine DepartmentCathy EstanislaoNo ratings yet
- ARTICULOPUBLICADODocument10 pagesARTICULOPUBLICADOtiaranindyNo ratings yet
- Icrs 2009 UsaDocument238 pagesIcrs 2009 UsaCannabisIntlNo ratings yet
- Pottenger’s Prophecy: How Food Resets Genes for Wellness or IllnessFrom EverandPottenger’s Prophecy: How Food Resets Genes for Wellness or IllnessNo ratings yet
- Character Strengths and Virtues - WikipediaDocument2 pagesCharacter Strengths and Virtues - WikipediaAnonymous u80JzlozSDNo ratings yet
- Onychophagia (Nail-Biting) Signs of Psychological Disorders or Simple HabitDocument7 pagesOnychophagia (Nail-Biting) Signs of Psychological Disorders or Simple HabitIJAR JOURNALNo ratings yet
- SagePathI WorkbookDocument12 pagesSagePathI Workbookhendrix2112100% (11)
- Influences of Spatial Configuration Learning On Spatial BehaviorDocument13 pagesInfluences of Spatial Configuration Learning On Spatial BehaviorLurbane OsloNo ratings yet
- Chapter 2 - Communication in TeamsDocument16 pagesChapter 2 - Communication in TeamsHeta Shastri100% (1)
- My DlleDocument12 pagesMy DlleMohit Talreja40% (5)
- Indvidual Development Plan Form ( (IDP)Document2 pagesIndvidual Development Plan Form ( (IDP)mary joy dela cruz100% (5)
- Okami Shackelford ARSR 2001 PDFDocument56 pagesOkami Shackelford ARSR 2001 PDFMeredith JoaneNo ratings yet
- NLP PresuppositionsDocument13 pagesNLP PresuppositionsJiří Herby Kysilka100% (2)
- The Science of Making Learning Stick AGES Model PDFDocument19 pagesThe Science of Making Learning Stick AGES Model PDFGilberto GarciaNo ratings yet
- Internship Portfolio DuraDocument24 pagesInternship Portfolio DuraJoan MarieNo ratings yet
- Mental Health Status of The BPed in Relation To Academic PerformanceDocument62 pagesMental Health Status of The BPed in Relation To Academic PerformanceMira, RenzoNo ratings yet
- VCOP Pyramids A3Document1 pageVCOP Pyramids A3mrbalintNo ratings yet
- Exploring The Matching HypothesisDocument19 pagesExploring The Matching HypothesisHERMOSO Anne L.No ratings yet
- Week 4 AsynchronousDocument45 pagesWeek 4 AsynchronousMariana RamosNo ratings yet
- An Introduction To Positive PsychologyDocument24 pagesAn Introduction To Positive PsychologyjkalekattilNo ratings yet
- Collaboration RubricDocument1 pageCollaboration Rubricapi-143975079No ratings yet
- Quarter 1-Week 1-Day 1.revisedDocument7 pagesQuarter 1-Week 1-Day 1.revisedMary JaneNo ratings yet
- OD PractitionersDocument5 pagesOD Practitionerssofronio v aguila jr100% (2)
- Parallelism Between Neural and Social NetworksDocument23 pagesParallelism Between Neural and Social NetworksMaye SaavedraNo ratings yet
- Using Undesirable ConsequencesDocument26 pagesUsing Undesirable Consequencesapi-281361915No ratings yet
- Sorensen Self-Esteem TestDocument2 pagesSorensen Self-Esteem Testruta mhapankarNo ratings yet
- Different Learning StylesDocument3 pagesDifferent Learning StylesJanea GarciaNo ratings yet
- ELTCDocument10 pagesELTCAliza Alexander Selvaratnam SalimNo ratings yet
- Who Wants To Be An EnterpreneurDocument9 pagesWho Wants To Be An EnterpreneurKule89No ratings yet
- FKG - The Difference of Tooth Demineralization After Soaking inDocument237 pagesFKG - The Difference of Tooth Demineralization After Soaking inbsahdnasNo ratings yet