Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
2 viewsNCP 1 3
NCP 1 3
Uploaded by
Allyzah Faith BernalesThe nursing care plan is for a 66-year-old client with fluid volume excess related to electrolyte imbalance as evidenced by an enlarged abdomen. Short term goals include the client understanding dietary and fluid restrictions and monitoring their fluid status after 8 hours. Long term goals include stabilizing fluid volume after 3 days. Interventions include determining fluid intake and output, monitoring the abdomen, elevating the extremities and providing care to reduce edema. Collaborative care includes administering ordered medications and treatments to reduce congestion and edema.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- Textbook of Physical Diagnosis: History and Examination: Mark H SwartzDocument1 pageTextbook of Physical Diagnosis: History and Examination: Mark H SwartzMudassar SattarNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- HydroceleDocument10 pagesHydroceleRyan ReNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJobelyn TunayNo ratings yet
- Gastroenteritis NCPDocument1 pageGastroenteritis NCPVenus Bactol67% (3)
- Renal Failure NCPDocument3 pagesRenal Failure NCPjsksNo ratings yet
- Activity On Care PlanningDocument14 pagesActivity On Care PlanningClaire Maurice JuaneroNo ratings yet
- FHP - NCP - Kidney FailureDocument9 pagesFHP - NCP - Kidney FailureFrancis AdrianNo ratings yet
- NCP - Impaired Urinary EliminationDocument3 pagesNCP - Impaired Urinary EliminationFretzgine Lou ManuelNo ratings yet
- Nursing Care PlansDocument31 pagesNursing Care PlansCyril Jane Caanyagan AcutNo ratings yet
- INTIA, Crisset O. Iii - BN: Submitted byDocument4 pagesINTIA, Crisset O. Iii - BN: Submitted byCrisset IntiaNo ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPJet Ray-Ann GaringanNo ratings yet
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- Fluid Volume Deficit Related To Loose Watery Stool Diarrhea)Document2 pagesFluid Volume Deficit Related To Loose Watery Stool Diarrhea)Jesse James Advincula Edjec100% (15)
- Liver Cirrhosis - NCPDocument18 pagesLiver Cirrhosis - NCPIshmael Solamillo83% (6)
- NCP - 3B - Naila Ferdia Putri1130019059 - Uts Bahasa Inggris.Document7 pagesNCP - 3B - Naila Ferdia Putri1130019059 - Uts Bahasa Inggris.Nayla FerdianaNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- Activity Intolerance R/T Increased Energy Demands Due To Disease Condition and Increased Fetal Nutrient UptakeDocument8 pagesActivity Intolerance R/T Increased Energy Demands Due To Disease Condition and Increased Fetal Nutrient UptakeAbdelmar SusulanNo ratings yet
- Liver Cirrhosis NCPDocument21 pagesLiver Cirrhosis NCPJeco Valdez100% (4)
- Assessment Nursing Diagnosis Nursing Goals Intervention Rationale EvaluationDocument5 pagesAssessment Nursing Diagnosis Nursing Goals Intervention Rationale EvaluationKobe ManuelNo ratings yet
- Diarrhea (AGE)Document2 pagesDiarrhea (AGE)NursesLabs.com100% (1)
- Facto NCPDocument3 pagesFacto NCPkkd nyleNo ratings yet
- NCP 3rd ROTATIONDocument17 pagesNCP 3rd ROTATIONMarie Ashley CasiaNo ratings yet
- PAPER 11 NewDocument27 pagesPAPER 11 NewOGU CourageNo ratings yet
- NCP (Diarrhea)Document2 pagesNCP (Diarrhea)Rodj Bilang Jr.83% (30)
- Ugib NCPDocument5 pagesUgib NCPJhuRise Ann Mangana100% (1)
- Nursing Care Plan 5 Altered Nutrition: Less Than Body RequirementsDocument9 pagesNursing Care Plan 5 Altered Nutrition: Less Than Body Requirementsdbryant010183% (24)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermLorie May GuillangNo ratings yet
- Client: Care Plan Initiated By: DateDocument3 pagesClient: Care Plan Initiated By: DateSIMON KYLE BAKIL DICHUASIDONo ratings yet
- NCP JaundiceDocument9 pagesNCP JaundiceMeena Koushal100% (1)
- Excess Fluid Volume Related To Sodium IntakeDocument5 pagesExcess Fluid Volume Related To Sodium IntakeNil GyiNo ratings yet
- Assessing Patient HydrationDocument5 pagesAssessing Patient HydrationDuvan F Triana ViviescasNo ratings yet
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 pagesSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- Gestational Diabetes - Case Study 2Document13 pagesGestational Diabetes - Case Study 2Bb RabbitNo ratings yet
- MS Soapie #1Document2 pagesMS Soapie #1Fatima KateNo ratings yet
- Prince NCPDocument9 pagesPrince NCPALVARADO, KRISTINE JOYNo ratings yet
- NCP - Activity Intolerance & Excess Fluid VolumeDocument2 pagesNCP - Activity Intolerance & Excess Fluid VolumeCindy MariscotesNo ratings yet
- BSN2 C Ihps NCP FinalDocument7 pagesBSN2 C Ihps NCP FinalAdrian DecolongonNo ratings yet
- Postpartal Discharge InstructionsDocument3 pagesPostpartal Discharge InstructionsDuchess Juliane Jose MirambelNo ratings yet
- C. Case Study thesis-NCP (Revised)Document5 pagesC. Case Study thesis-NCP (Revised)Lopirts NiganiNo ratings yet
- Fluid Volume Deficit Related To Nausea and VomitDocument3 pagesFluid Volume Deficit Related To Nausea and VomitJakeNo ratings yet
- DX Spine Injury PDFDocument5 pagesDX Spine Injury PDFSherree HayesNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- KKKKDocument22 pagesKKKKMARY CLAIRE SUMILHIGNo ratings yet
- Client Care Plan ADocument12 pagesClient Care Plan AArithmajikNo ratings yet
- Name: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralDocument2 pagesName: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralRainier IbarretaNo ratings yet
- Nursing Care Plan DiarrheaDocument2 pagesNursing Care Plan DiarrheaCzarina AeriNo ratings yet
- Ncp-Ckd-Janry FinalDocument6 pagesNcp-Ckd-Janry Finalcjpalapuz07No ratings yet
- Nursing Care Plan Patient's Name: Age: Sex: Address:: Nursing-Notes/communicable - Diseases - Notes/amoebiasisDocument4 pagesNursing Care Plan Patient's Name: Age: Sex: Address:: Nursing-Notes/communicable - Diseases - Notes/amoebiasisGILIANNE MARIE JIMENEANo ratings yet
- Askep GE..by SaryDocument11 pagesAskep GE..by Sarysoca wanaNo ratings yet
- NCM 116 Alterations in Nutri and GI Rev5Document100 pagesNCM 116 Alterations in Nutri and GI Rev5JxshxzsNo ratings yet
- NCP EsrfDocument9 pagesNCP EsrfKen RegalaNo ratings yet
- Provides Baseline Information For Monitoring Changes and Evaluating The Effectiveness of TherapyDocument8 pagesProvides Baseline Information For Monitoring Changes and Evaluating The Effectiveness of TherapyJannen CasasNo ratings yet
- Crohn's Disease Seminar FinalDocument27 pagesCrohn's Disease Seminar Finalshahad alshareefNo ratings yet
- DX Diarrhea PDFDocument11 pagesDX Diarrhea PDFSherree HayesNo ratings yet
- HYPONATREMIADocument3 pagesHYPONATREMIADienizs Labini TadenaNo ratings yet
- Aguinaldo, Sophia Kaye M. Nursing Care Plan On Problem-Based LearningDocument9 pagesAguinaldo, Sophia Kaye M. Nursing Care Plan On Problem-Based LearningSophia Kaye AguinaldoNo ratings yet
- Atlas of High-Resolution Manometry, Impedance, and pH MonitoringFrom EverandAtlas of High-Resolution Manometry, Impedance, and pH MonitoringNo ratings yet
- Simmond's Disease MSDocument22 pagesSimmond's Disease MSJennylyn Bartolome Pentz0% (1)
- Management of StemisDocument20 pagesManagement of Stemisapi-269001337No ratings yet
- Safety Data Sheet: Armohib 31Document12 pagesSafety Data Sheet: Armohib 31Dr. Pushkar ShuklaNo ratings yet
- UTI (Urinary Tract Infection)Document9 pagesUTI (Urinary Tract Infection)Carson BirthNo ratings yet
- Pasquini, L, Et Al. (2018) - Neurological Signs As Early Determinants of Dementia and Predictors of Mortality Among Older Adults inDocument11 pagesPasquini, L, Et Al. (2018) - Neurological Signs As Early Determinants of Dementia and Predictors of Mortality Among Older Adults inManuela Bedoya GartnerNo ratings yet
- Youth Development Specialist Cover LetterDocument7 pagesYouth Development Specialist Cover LetterafmrokptolzieaNo ratings yet
- P.4 Scie Package 26TH May To 2ND June 2020Document8 pagesP.4 Scie Package 26TH May To 2ND June 2020Monydit santinoNo ratings yet
- Table of Contents MBTP 5ED PDFDocument10 pagesTable of Contents MBTP 5ED PDFSamiNo ratings yet
- MCPHS Drug Information QuestionDocument5 pagesMCPHS Drug Information QuestionG TeenaNo ratings yet
- TLA On Nutrition in Late AdulthoodDocument4 pagesTLA On Nutrition in Late AdulthoodEdda Marie PidutNo ratings yet
- Reinforcing Antara Ibu Yang Memberikan Asi EksklusifDocument13 pagesReinforcing Antara Ibu Yang Memberikan Asi EksklusifBaiq RianaNo ratings yet
- Pressure InjuriesDocument1 pagePressure InjuriesPaola OrtizNo ratings yet
- Understanding The SelfDocument7 pagesUnderstanding The SelfCarmela DandayNo ratings yet
- EAU Guidelines Urological Infections 2016 1 PDFDocument16 pagesEAU Guidelines Urological Infections 2016 1 PDFMaria Jose Zamorano SepulvedaNo ratings yet
- A Clinical Study On The Inguinal Hernia and Its Management in The General Surgical Practice at Tertiary Care HospitalDocument4 pagesA Clinical Study On The Inguinal Hernia and Its Management in The General Surgical Practice at Tertiary Care Hospitalmelon segerNo ratings yet
- Bapt ToolDocument11 pagesBapt ToolShafiNo ratings yet
- EXSA - Silver Award Recipients 2005Document9 pagesEXSA - Silver Award Recipients 2005applebarrelNo ratings yet
- IPIECA - IOGP - Oil Spill Response Introduction - GPGDocument24 pagesIPIECA - IOGP - Oil Spill Response Introduction - GPGseawolf50No ratings yet
- Amartya Sen - Public Health Ethics and EquityDocument331 pagesAmartya Sen - Public Health Ethics and EquityVNo ratings yet
- LG - Hazards Identification (Level 5)Document64 pagesLG - Hazards Identification (Level 5)Ang Tze WeiNo ratings yet
- Axonal Sensorimotor Neuropathy in Patients With B-ThalassemiaDocument5 pagesAxonal Sensorimotor Neuropathy in Patients With B-ThalassemiaDesty PurnamasariNo ratings yet
- Pelvic Floor DysfunctionDocument92 pagesPelvic Floor DysfunctionWindy Puspa KusumahNo ratings yet
- Laminine - The Symbol of Life and RenewalDocument44 pagesLaminine - The Symbol of Life and RenewalNoel NievesNo ratings yet
- Pendidikan Kedokteran Di Masa Pnademi COVID-19Document9 pagesPendidikan Kedokteran Di Masa Pnademi COVID-19Aisyah FawNo ratings yet
- BTEC Assignment Brief: Qualification Centre Number and Name Unit or Number and TitleDocument4 pagesBTEC Assignment Brief: Qualification Centre Number and Name Unit or Number and TitlemaysNo ratings yet
- Hubungan Lama Berobat Dan Keteraturan Berobat Dengan Kadar Hba1C Pasien DM Tipe 2 Di Poli Endokrin Rsup Prof. Dr. R. D. Kandou ManadoDocument8 pagesHubungan Lama Berobat Dan Keteraturan Berobat Dengan Kadar Hba1C Pasien DM Tipe 2 Di Poli Endokrin Rsup Prof. Dr. R. D. Kandou ManadoBerlianti Citra MaulidyaNo ratings yet
- ACC Silicones LTD Silcoset 101: Safety Data SheetDocument6 pagesACC Silicones LTD Silcoset 101: Safety Data SheetNICKYNo ratings yet
- Riya Parikh Essay 4 1Document6 pagesRiya Parikh Essay 4 1api-3026862950% (1)
- Healthy Lifestyle!: Part of ADocument2 pagesHealthy Lifestyle!: Part of ARon GumapacNo ratings yet
NCP 1 3
NCP 1 3
Uploaded by
Allyzah Faith Bernales0 ratings0% found this document useful (0 votes)
2 views6 pagesThe nursing care plan is for a 66-year-old client with fluid volume excess related to electrolyte imbalance as evidenced by an enlarged abdomen. Short term goals include the client understanding dietary and fluid restrictions and monitoring their fluid status after 8 hours. Long term goals include stabilizing fluid volume after 3 days. Interventions include determining fluid intake and output, monitoring the abdomen, elevating the extremities and providing care to reduce edema. Collaborative care includes administering ordered medications and treatments to reduce congestion and edema.
Original Description:
Original Title
NCP-1-3 (1)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe nursing care plan is for a 66-year-old client with fluid volume excess related to electrolyte imbalance as evidenced by an enlarged abdomen. Short term goals include the client understanding dietary and fluid restrictions and monitoring their fluid status after 8 hours. Long term goals include stabilizing fluid volume after 3 days. Interventions include determining fluid intake and output, monitoring the abdomen, elevating the extremities and providing care to reduce edema. Collaborative care includes administering ordered medications and treatments to reduce congestion and edema.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
2 views6 pagesNCP 1 3
NCP 1 3
Uploaded by
Allyzah Faith BernalesThe nursing care plan is for a 66-year-old client with fluid volume excess related to electrolyte imbalance as evidenced by an enlarged abdomen. Short term goals include the client understanding dietary and fluid restrictions and monitoring their fluid status after 8 hours. Long term goals include stabilizing fluid volume after 3 days. Interventions include determining fluid intake and output, monitoring the abdomen, elevating the extremities and providing care to reduce edema. Collaborative care includes administering ordered medications and treatments to reduce congestion and edema.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 6
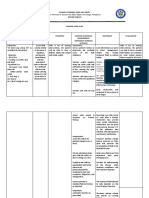
ADVENTIST MEDICAL CENTER COLLEGE
Brgy. San Miguel, Iligan City
SCHOOL OF NURSING
NURSING CARE PLAN
Client Name:
Age: 66 years old
Assessment Nursing Planning Nursing Rationale Evaluation
Data based on Diagnosis (Desired or Interventions
PEROS and Expected
GORDON’S Outcomes)
Subjective Data: Fluid volume STO: Independent: Independent: STO:
“Nikalit lang jud ug excess r/t After 8 hours of 1) Determine or 1) Potential exists for After 8 hours of
kadako iyang tiyan electrolyte nursing estimate the amount of fluid overload due to nursing
ma’am atong imbalance interventions, client fluid intake from all fluid shifts and changes interventions, client
Sabado. Pero wala AEB enlarged will be able to: sources. in electrolyte balance. was able to:
na siya nagsuka” as abdomen - Verbalize 2) Review nutritional 2) Imbalances in these - Verbalize
verbalized by the understanding of issues (e.g., intake of areas are associated understanding of
S/O. individual dietary sodium, potassium). with fluid imbalances. individual dietary
and fluid restrictions 3) Measure abdominal 3) For changes that may and fluid restrictions
Objective Data: - Demonstrate girth. indicate increasing fluid - Demonstrate
- Confusion behaviors to monitor 4) Record I&O retention/edema. behaviors to monitor
- Decreased urinary fluid status and accurately; calculate 4) So that adjustments fluid status and
output reduce recurrence of 24-hour fluid balance. can be made in the reduce recurrence of
- Total I&O fluid excess 5) Elevate edematous following 24-hour fluid excess
- Nonpitting edema extremities and intake if needed.
on both lower LTO: change position 5) To reduce tissue LTO:
extremities After 3 days of frequently. pressure and risk of After 3 days of
- Abdominal girth nursing 6) Place in semi- skin breakdown. nursing
((Day 1) = 98 cm interventions, client Fowler’s position 6) May promote interventions, client
Abdominal Girth will be able to: when at bed rest, as recumbency-induced was able to:
(Day 2) = 91 cm - Stabilize fluid appropriate. diuresis and facilitate - Stabilize fluid
Abdominal Girth volume as evidenced 7) Set an appropriate respiratory effort when volume as evidenced
(Day 3) = 93 cm) by balanced input rate of fluid intake and movement of the by balanced input
- Ileus upon and output and free infusion throughout diaphragm is limited. and output and free
auscultation signs of edema 24-hr period. 7) To prevent signs of edema
- Dullness over exacerbation of excess
percussion Collaborative or fluid volume and to
- Low sodium level Interdisciplinary prevent peaks and
= 116.4 (normal Care: valleys in fluid level.
level should be 135- 1) Administer
148mmol/L) medications as Collaborative or
- Low albumin level ordered. Interdisciplinary
= 28.07 (normal (Human Albumin Care:
level should be 38- 25% q12h) (Lasix 1) To reduce congestion
54g/L) 40mg slow IVTT q8h) and edema.
(Heraclene Forte 3mg
1 cap OD) (NaCl 2
tabs TID)
References: Doenges, M., Moorhouse, M., & Murr, A. (2022). In Nurse's Pocket Guide, Diagnoses, Prioritized Interventions, and
Rationales, 16th ed. (pp. 395-399). Philadelphia: F.A. Davis Company.
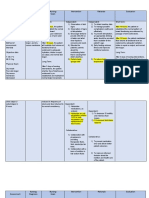
Assessment Nursing Planning Nursing Rationale Evaluation
Data based on Diagnosis (Desired or Interventions
PEROS and Expected
GORDON’S Outcomes)
Subjective Data: Dysfunctional STO: Independent: Independent: STO:
- Reports of gastrointestinal After 8 hours of 1) Note lifestyle. 1) There are issues that STO:
abdominal pain motility r/t nursing 2) Inspect abdomen, can affect GI function After 8 hours of
decrease in interventions, client noting contour. and health. nursing
“Ang problema peristaltic will be able to: 3) Auscultate 2) Distention of bowel interventions, client
ma’am kana ra gyud activity AEB - Verbalize abdomen. may indicate was able to:
iyang tiyan ni dako” absence of understanding of 4) Measure abdominal accumulation of fluids - Verbalize
as verbalized by the BM, and causative factors and girth. and gases formed. understanding of
S/O. abdominal rationale for 5) Note frequency and 3) Hypoactive bowel causative factors and
distention treatment regimen characteristics of sounds may indicate rationale for
Objective Data: - Demonstrate bowel movements. ileus. treatment regimen
- Absence of flatus appropriate 6) Measure GI output 4) To monitor - Demonstrate
until third day behaviors to assist periodically and note development or appropriate
- Constipation/no with resolution of characteristics of progression of behaviors to assist
BM causative factors drainage. distention. with resolution of
- Distended or 7) Manage pain with 5) May reveal an causative factors
enlarged abdomen LTO: nonpharmacological underlying problem or
- NGT open to drain After 3 days of interventions such as effect of pathology. LTO:
with dark green nursing positioning, back rub, 6) To manage fluid After 3 days of
discharges noted interventions, client or heating pad (unless losses and replacement nursing
(Day 1 = 15cc will be able to: contraindicated). needs and electrolyte interventions, client
Day 2 = 315cc - Reestablish and balance. was able to:
Day 3 = ?) maintain normal Collaborative or 7) To enhance muscle - Reestablish and
- Hypoactive bowel pattern of bowel Interdisciplinary relaxation and reduce maintain normal
sounds functioning Care: discomfort. pattern of bowel
1) Maintain GI rest functioning
when indicated – Collaborative or
NPO, fluids only as Interdisciplinary
ordered. Care:
2) Collaborate in 1) To reduce intestinal
treatment of bloating and risk of
underlying conditions. vomiting.
3) Administer fluids 2) To correct or treat
and electrolytes as disorders associated
indicated. with client’s current GI
4) Administer dysfunction.
medication as ordered 3) To replace losses and
(Fleet Enema) to improve GI
circulation and
function.
4) To reduce risk of GI
dysfunction.
References: Doenges, M., Moorhouse, M., & Murr, A. (2022). In Nurse's Pocket Guide, Diagnoses, Prioritized Interventions, and
Rationales, 16th ed. (pp. 419-425). Philadelphia: F.A. Davis Company.
Assessment Nursing Planning Nursing Rationale Evaluation
Data based on Diagnosis (Desired or Interventions
PEROS and Expected
GORDON’S Outcomes)
Subjective Data: Impaired STO: Independent: Independent: STO:
“Kapoyan siya ug physical After 4-8 hours of 1) Note factors 1) Identifies potential After 4-8 hours of
tindog” as mobility r/t nursing affecting current impairments and nursing
verbalized by the pain AEB interventions, client situation. determines types of interventions, client
S/O. reports of pain will be able to: 2) Assist with interventions needed to was able to:
when sitting or - Verbalize treatment of provide for client’s - Verbalize
“Kana raman gyud standing up understanding of underlying condition safety. understanding of
iyang sakit sa tiyan and physical situation and causing pain and/or 2) To maximize the situation and
iyang problema” as deconditioning individual treatment dysfunction. potential for mobility individual treatment
verbalized by the regimen and safety 3) Promote comfort and function. regimen and safety
S/O measures measures and provide 3) To enhance ability to measures
- Demonstrate relief of pain. participate in activities. - Demonstrate
“Sakit akong luyo” techniques or 4) Identify energy- 4) Limits fatigue, techniques or
as verbalized by the behaviors that enable conserving techniques maximizing behaviors that enable
client. resumption of for ADLs. participation. resumption of
activities 5) Encourage 5) Enhances self- activities
Objective Data: - Report pain is participation in self- concept and sense of - Report pain is
- Slow movement relieved or care. independence. relieved or
- Needs support controlled controlled
when sitting or Collaborative or Collaborative or
standing LTO: Interdisciplinary Interdisciplinary LTO:
- Weak in After 3 days of Care: Care: After 3 days of
appearance nursing 1) Involve client and 1) Enhances nursing
- Cannot perform interventions, client S/O in care, assisting commitment to plan, interventions, client
ADL’s alone will be able to: them to learn ways of optimizing outcomes. was able to:
- Facial grimace - Participate in managing problems of 2) To permit maximal - Participate in
when moving ADLs and desired immobility. effort and involvement ADLs and desired
- Irritability activities 2) Administer in activity. activities
- Maintain or medications as needed - Maintain or
increase strength and for pain relief. increase strength and
function of affected (Starcox 120mg tab function of affected
and/or compensatory OD pc breakfast) and/or compensatory
body parts (Algesia 1 tab TID po body parts
RTC)
References: Doenges, M., Moorhouse, M., & Murr, A. (2022). In Nurse's Pocket Guide, Diagnoses, Prioritized Interventions, and
Rationales, 16th ed. (pp. 616-621). Philadelphia: F.A. Davis Company.
You might also like
- Textbook of Physical Diagnosis: History and Examination: Mark H SwartzDocument1 pageTextbook of Physical Diagnosis: History and Examination: Mark H SwartzMudassar SattarNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- HydroceleDocument10 pagesHydroceleRyan ReNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJobelyn TunayNo ratings yet
- Gastroenteritis NCPDocument1 pageGastroenteritis NCPVenus Bactol67% (3)
- Renal Failure NCPDocument3 pagesRenal Failure NCPjsksNo ratings yet
- Activity On Care PlanningDocument14 pagesActivity On Care PlanningClaire Maurice JuaneroNo ratings yet
- FHP - NCP - Kidney FailureDocument9 pagesFHP - NCP - Kidney FailureFrancis AdrianNo ratings yet
- NCP - Impaired Urinary EliminationDocument3 pagesNCP - Impaired Urinary EliminationFretzgine Lou ManuelNo ratings yet
- Nursing Care PlansDocument31 pagesNursing Care PlansCyril Jane Caanyagan AcutNo ratings yet
- INTIA, Crisset O. Iii - BN: Submitted byDocument4 pagesINTIA, Crisset O. Iii - BN: Submitted byCrisset IntiaNo ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPJet Ray-Ann GaringanNo ratings yet
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- Fluid Volume Deficit Related To Loose Watery Stool Diarrhea)Document2 pagesFluid Volume Deficit Related To Loose Watery Stool Diarrhea)Jesse James Advincula Edjec100% (15)
- Liver Cirrhosis - NCPDocument18 pagesLiver Cirrhosis - NCPIshmael Solamillo83% (6)
- NCP - 3B - Naila Ferdia Putri1130019059 - Uts Bahasa Inggris.Document7 pagesNCP - 3B - Naila Ferdia Putri1130019059 - Uts Bahasa Inggris.Nayla FerdianaNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- Activity Intolerance R/T Increased Energy Demands Due To Disease Condition and Increased Fetal Nutrient UptakeDocument8 pagesActivity Intolerance R/T Increased Energy Demands Due To Disease Condition and Increased Fetal Nutrient UptakeAbdelmar SusulanNo ratings yet
- Liver Cirrhosis NCPDocument21 pagesLiver Cirrhosis NCPJeco Valdez100% (4)
- Assessment Nursing Diagnosis Nursing Goals Intervention Rationale EvaluationDocument5 pagesAssessment Nursing Diagnosis Nursing Goals Intervention Rationale EvaluationKobe ManuelNo ratings yet
- Diarrhea (AGE)Document2 pagesDiarrhea (AGE)NursesLabs.com100% (1)
- Facto NCPDocument3 pagesFacto NCPkkd nyleNo ratings yet
- NCP 3rd ROTATIONDocument17 pagesNCP 3rd ROTATIONMarie Ashley CasiaNo ratings yet
- PAPER 11 NewDocument27 pagesPAPER 11 NewOGU CourageNo ratings yet
- NCP (Diarrhea)Document2 pagesNCP (Diarrhea)Rodj Bilang Jr.83% (30)
- Ugib NCPDocument5 pagesUgib NCPJhuRise Ann Mangana100% (1)
- Nursing Care Plan 5 Altered Nutrition: Less Than Body RequirementsDocument9 pagesNursing Care Plan 5 Altered Nutrition: Less Than Body Requirementsdbryant010183% (24)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermLorie May GuillangNo ratings yet
- Client: Care Plan Initiated By: DateDocument3 pagesClient: Care Plan Initiated By: DateSIMON KYLE BAKIL DICHUASIDONo ratings yet
- NCP JaundiceDocument9 pagesNCP JaundiceMeena Koushal100% (1)
- Excess Fluid Volume Related To Sodium IntakeDocument5 pagesExcess Fluid Volume Related To Sodium IntakeNil GyiNo ratings yet
- Assessing Patient HydrationDocument5 pagesAssessing Patient HydrationDuvan F Triana ViviescasNo ratings yet
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 pagesSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- Gestational Diabetes - Case Study 2Document13 pagesGestational Diabetes - Case Study 2Bb RabbitNo ratings yet
- MS Soapie #1Document2 pagesMS Soapie #1Fatima KateNo ratings yet
- Prince NCPDocument9 pagesPrince NCPALVARADO, KRISTINE JOYNo ratings yet
- NCP - Activity Intolerance & Excess Fluid VolumeDocument2 pagesNCP - Activity Intolerance & Excess Fluid VolumeCindy MariscotesNo ratings yet
- BSN2 C Ihps NCP FinalDocument7 pagesBSN2 C Ihps NCP FinalAdrian DecolongonNo ratings yet
- Postpartal Discharge InstructionsDocument3 pagesPostpartal Discharge InstructionsDuchess Juliane Jose MirambelNo ratings yet
- C. Case Study thesis-NCP (Revised)Document5 pagesC. Case Study thesis-NCP (Revised)Lopirts NiganiNo ratings yet
- Fluid Volume Deficit Related To Nausea and VomitDocument3 pagesFluid Volume Deficit Related To Nausea and VomitJakeNo ratings yet
- DX Spine Injury PDFDocument5 pagesDX Spine Injury PDFSherree HayesNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- KKKKDocument22 pagesKKKKMARY CLAIRE SUMILHIGNo ratings yet
- Client Care Plan ADocument12 pagesClient Care Plan AArithmajikNo ratings yet
- Name: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralDocument2 pagesName: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralRainier IbarretaNo ratings yet
- Nursing Care Plan DiarrheaDocument2 pagesNursing Care Plan DiarrheaCzarina AeriNo ratings yet
- Ncp-Ckd-Janry FinalDocument6 pagesNcp-Ckd-Janry Finalcjpalapuz07No ratings yet
- Nursing Care Plan Patient's Name: Age: Sex: Address:: Nursing-Notes/communicable - Diseases - Notes/amoebiasisDocument4 pagesNursing Care Plan Patient's Name: Age: Sex: Address:: Nursing-Notes/communicable - Diseases - Notes/amoebiasisGILIANNE MARIE JIMENEANo ratings yet
- Askep GE..by SaryDocument11 pagesAskep GE..by Sarysoca wanaNo ratings yet
- NCM 116 Alterations in Nutri and GI Rev5Document100 pagesNCM 116 Alterations in Nutri and GI Rev5JxshxzsNo ratings yet
- NCP EsrfDocument9 pagesNCP EsrfKen RegalaNo ratings yet
- Provides Baseline Information For Monitoring Changes and Evaluating The Effectiveness of TherapyDocument8 pagesProvides Baseline Information For Monitoring Changes and Evaluating The Effectiveness of TherapyJannen CasasNo ratings yet
- Crohn's Disease Seminar FinalDocument27 pagesCrohn's Disease Seminar Finalshahad alshareefNo ratings yet
- DX Diarrhea PDFDocument11 pagesDX Diarrhea PDFSherree HayesNo ratings yet
- HYPONATREMIADocument3 pagesHYPONATREMIADienizs Labini TadenaNo ratings yet
- Aguinaldo, Sophia Kaye M. Nursing Care Plan On Problem-Based LearningDocument9 pagesAguinaldo, Sophia Kaye M. Nursing Care Plan On Problem-Based LearningSophia Kaye AguinaldoNo ratings yet
- Atlas of High-Resolution Manometry, Impedance, and pH MonitoringFrom EverandAtlas of High-Resolution Manometry, Impedance, and pH MonitoringNo ratings yet
- Simmond's Disease MSDocument22 pagesSimmond's Disease MSJennylyn Bartolome Pentz0% (1)
- Management of StemisDocument20 pagesManagement of Stemisapi-269001337No ratings yet
- Safety Data Sheet: Armohib 31Document12 pagesSafety Data Sheet: Armohib 31Dr. Pushkar ShuklaNo ratings yet
- UTI (Urinary Tract Infection)Document9 pagesUTI (Urinary Tract Infection)Carson BirthNo ratings yet
- Pasquini, L, Et Al. (2018) - Neurological Signs As Early Determinants of Dementia and Predictors of Mortality Among Older Adults inDocument11 pagesPasquini, L, Et Al. (2018) - Neurological Signs As Early Determinants of Dementia and Predictors of Mortality Among Older Adults inManuela Bedoya GartnerNo ratings yet
- Youth Development Specialist Cover LetterDocument7 pagesYouth Development Specialist Cover LetterafmrokptolzieaNo ratings yet
- P.4 Scie Package 26TH May To 2ND June 2020Document8 pagesP.4 Scie Package 26TH May To 2ND June 2020Monydit santinoNo ratings yet
- Table of Contents MBTP 5ED PDFDocument10 pagesTable of Contents MBTP 5ED PDFSamiNo ratings yet
- MCPHS Drug Information QuestionDocument5 pagesMCPHS Drug Information QuestionG TeenaNo ratings yet
- TLA On Nutrition in Late AdulthoodDocument4 pagesTLA On Nutrition in Late AdulthoodEdda Marie PidutNo ratings yet
- Reinforcing Antara Ibu Yang Memberikan Asi EksklusifDocument13 pagesReinforcing Antara Ibu Yang Memberikan Asi EksklusifBaiq RianaNo ratings yet
- Pressure InjuriesDocument1 pagePressure InjuriesPaola OrtizNo ratings yet
- Understanding The SelfDocument7 pagesUnderstanding The SelfCarmela DandayNo ratings yet
- EAU Guidelines Urological Infections 2016 1 PDFDocument16 pagesEAU Guidelines Urological Infections 2016 1 PDFMaria Jose Zamorano SepulvedaNo ratings yet
- A Clinical Study On The Inguinal Hernia and Its Management in The General Surgical Practice at Tertiary Care HospitalDocument4 pagesA Clinical Study On The Inguinal Hernia and Its Management in The General Surgical Practice at Tertiary Care Hospitalmelon segerNo ratings yet
- Bapt ToolDocument11 pagesBapt ToolShafiNo ratings yet
- EXSA - Silver Award Recipients 2005Document9 pagesEXSA - Silver Award Recipients 2005applebarrelNo ratings yet
- IPIECA - IOGP - Oil Spill Response Introduction - GPGDocument24 pagesIPIECA - IOGP - Oil Spill Response Introduction - GPGseawolf50No ratings yet
- Amartya Sen - Public Health Ethics and EquityDocument331 pagesAmartya Sen - Public Health Ethics and EquityVNo ratings yet
- LG - Hazards Identification (Level 5)Document64 pagesLG - Hazards Identification (Level 5)Ang Tze WeiNo ratings yet
- Axonal Sensorimotor Neuropathy in Patients With B-ThalassemiaDocument5 pagesAxonal Sensorimotor Neuropathy in Patients With B-ThalassemiaDesty PurnamasariNo ratings yet
- Pelvic Floor DysfunctionDocument92 pagesPelvic Floor DysfunctionWindy Puspa KusumahNo ratings yet
- Laminine - The Symbol of Life and RenewalDocument44 pagesLaminine - The Symbol of Life and RenewalNoel NievesNo ratings yet
- Pendidikan Kedokteran Di Masa Pnademi COVID-19Document9 pagesPendidikan Kedokteran Di Masa Pnademi COVID-19Aisyah FawNo ratings yet
- BTEC Assignment Brief: Qualification Centre Number and Name Unit or Number and TitleDocument4 pagesBTEC Assignment Brief: Qualification Centre Number and Name Unit or Number and TitlemaysNo ratings yet
- Hubungan Lama Berobat Dan Keteraturan Berobat Dengan Kadar Hba1C Pasien DM Tipe 2 Di Poli Endokrin Rsup Prof. Dr. R. D. Kandou ManadoDocument8 pagesHubungan Lama Berobat Dan Keteraturan Berobat Dengan Kadar Hba1C Pasien DM Tipe 2 Di Poli Endokrin Rsup Prof. Dr. R. D. Kandou ManadoBerlianti Citra MaulidyaNo ratings yet
- ACC Silicones LTD Silcoset 101: Safety Data SheetDocument6 pagesACC Silicones LTD Silcoset 101: Safety Data SheetNICKYNo ratings yet
- Riya Parikh Essay 4 1Document6 pagesRiya Parikh Essay 4 1api-3026862950% (1)
- Healthy Lifestyle!: Part of ADocument2 pagesHealthy Lifestyle!: Part of ARon GumapacNo ratings yet