Professional Documents
Culture Documents
Pharma Antibiotics
Pharma Antibiotics
Uploaded by
valdez.adler.lCopyright:
Available Formats
You might also like
- Celtic Ogham BookletDocument11 pagesCeltic Ogham Bookletoftaran100% (3)
- Leonard Baskin & Ted HughesDocument16 pagesLeonard Baskin & Ted Hughesmgter100% (1)
- CHAPTER 9 ReviewerDocument4 pagesCHAPTER 9 ReviewerHannah BuquironNo ratings yet
- Semifinal TransesDocument9 pagesSemifinal TransesDianneNo ratings yet
- Antibiotics PharmaDocument4 pagesAntibiotics PharmaJohn Dave V. VillarmenteNo ratings yet
- L16 ANTIBIOTICS - IN - ORAL - MAXILLOFACIAL - SURGERY Copy 2Document19 pagesL16 ANTIBIOTICS - IN - ORAL - MAXILLOFACIAL - SURGERY Copy 2Ju JuNo ratings yet
- ANTIBIOTICS Pharmacology NursingDocument10 pagesANTIBIOTICS Pharmacology NursingRalph Alfonse De JesusNo ratings yet
- Midterms PharmacologyDocument35 pagesMidterms PharmacologyMutya XDNo ratings yet
- Byron - Recurrent Resistant Urinary Tract InfectionsDocument8 pagesByron - Recurrent Resistant Urinary Tract InfectionsC GNo ratings yet
- Anti InfectivesDocument4 pagesAnti InfectivespaderamosNo ratings yet
- Anti InfectivesDocument126 pagesAnti Infectiveseunice lachicaNo ratings yet
- Emnc 4 North Drug StudyDocument12 pagesEmnc 4 North Drug StudyFrancesca Aurea MagumunNo ratings yet
- (PHARMA A) 3.3 - Antibiotics I - Dr. Cruz (2024)Document15 pages(PHARMA A) 3.3 - Antibiotics I - Dr. Cruz (2024)Miguel Luis NavarreteNo ratings yet
- Mechanisms of Antimicrobial ResistanceDocument12 pagesMechanisms of Antimicrobial ResistanceFrances Lau Yee ChinNo ratings yet
- 6-Introduction To AntibioticsDocument10 pages6-Introduction To AntibioticsKanishka TiwariNo ratings yet
- Pharma-Lesson 1-3 Therapeutic DrugsDocument7 pagesPharma-Lesson 1-3 Therapeutic DrugsFia CelerioNo ratings yet
- Reviewer in PharmacologyDocument20 pagesReviewer in PharmacologyJhayneNo ratings yet
- Unit 4Document111 pagesUnit 4Bea Bianca CruzNo ratings yet
- Table of AntibioticsDocument5 pagesTable of AntibioticsBerenese DianneNo ratings yet
- Overview of Infections and AntimicrobialsDocument43 pagesOverview of Infections and Antimicrobialszainab ElsayedNo ratings yet
- Lec - Bacte - Non Fermentative Gram Negative Bacilli - MidtermsDocument2 pagesLec - Bacte - Non Fermentative Gram Negative Bacilli - MidtermsJashmine May TadinaNo ratings yet
- Antimicrobial AgentsDocument14 pagesAntimicrobial AgentsAllyssa TolibasNo ratings yet
- Microbiology and Parasitology Week 3. ABCDDocument21 pagesMicrobiology and Parasitology Week 3. ABCDohsehuns wifeuNo ratings yet
- Antimicrobial Lecture NotesDocument55 pagesAntimicrobial Lecture Noteshunarsandhu100% (2)
- C. Bacteriology L6 Antimicrobial Agents and Resistance LaboratoryDocument6 pagesC. Bacteriology L6 Antimicrobial Agents and Resistance LaboratoryChelze Faith DizonNo ratings yet
- 659fdeb8aea86969913c25a1-1704984472-IHBB Lec IS Lecture NotesDocument3 pages659fdeb8aea86969913c25a1-1704984472-IHBB Lec IS Lecture NotesAnne Chelsea Ramirez OritNo ratings yet
- Controlling Microbial Growth in Vivo Using Antimicrobial AgentsDocument30 pagesControlling Microbial Growth in Vivo Using Antimicrobial AgentsJen PanganibanNo ratings yet
- Biosel-Mikro Mekanisme Antibiotik 2022Document45 pagesBiosel-Mikro Mekanisme Antibiotik 20226. Putu Arbita DivyaNo ratings yet
- ToB S5 Lecture 1Document2 pagesToB S5 Lecture 1LT DRAGONXNo ratings yet
- Lec 5: Antimycobacerial Drugs by Dr. Frederick Loyola July 7, 2010Document7 pagesLec 5: Antimycobacerial Drugs by Dr. Frederick Loyola July 7, 2010Rachel Leslie de LeonNo ratings yet
- CefuroximeDocument1 pageCefuroximehahahahaaaaaaaNo ratings yet
- Antibiotics 2Document38 pagesAntibiotics 2Tommy ZeusNo ratings yet
- Antibiotics (Role and Abuse) 2016Document35 pagesAntibiotics (Role and Abuse) 2016Mohd Johari Mohd ShafuwanNo ratings yet
- Antibacterial and Antiinfective AgentsDocument80 pagesAntibacterial and Antiinfective AgentsAbbeygale GalanNo ratings yet
- Lecture 4 - SCI 8007SEF Medical Microbiology & Virology-Introduction To Medical Microbiology I - 24 Sep 2023Document62 pagesLecture 4 - SCI 8007SEF Medical Microbiology & Virology-Introduction To Medical Microbiology I - 24 Sep 2023Ada ChanNo ratings yet
- Pharma Part 1 and 2Document10 pagesPharma Part 1 and 2BRYCE WILLIAM GONo ratings yet
- W1 Antimicrobial DrugsDocument8 pagesW1 Antimicrobial Drugsseanne kskwkwkaNo ratings yet
- 6 Inhibiting The Growth of Pathogens in VivoDocument27 pages6 Inhibiting The Growth of Pathogens in VivoAinaB ManaloNo ratings yet
- Summary of AntibioticsDocument11 pagesSummary of AntibioticsAamir MunawarNo ratings yet
- Module 3Document6 pagesModule 3richelleambrocio054No ratings yet
- (BACTE-LEC) 8. Antimicrobial Susceptibility TestingDocument6 pages(BACTE-LEC) 8. Antimicrobial Susceptibility TestingCarlo CataagNo ratings yet
- Using Antimicrobial Agents To Control Mirobial Growth in VivoDocument39 pagesUsing Antimicrobial Agents To Control Mirobial Growth in VivoHannah BuquironNo ratings yet
- Chapter 29 Child With CancerDocument9 pagesChapter 29 Child With CancerMARCERA JERALDINE ALESSA P.No ratings yet
- PHARMACOLOGY Anti Microbial DrugsDocument17 pagesPHARMACOLOGY Anti Microbial DrugsLeilani Sablan100% (2)
- CampylobacterDocument2 pagesCampylobactersarguss14No ratings yet
- Drug StudyDocument9 pagesDrug StudyGenovee Angela FayeNo ratings yet
- Antibiotics 1Document64 pagesAntibiotics 1Justin Ancog100% (1)
- Pharma-Module 8Document5 pagesPharma-Module 8Myles CardelNo ratings yet
- Antibiotics and Spectrum of ActionDocument40 pagesAntibiotics and Spectrum of ActionNUBWA MEDUGUNo ratings yet
- Inhibiting The Growth of Pathogens in VivoDocument25 pagesInhibiting The Growth of Pathogens in VivoRoshwell RegalaNo ratings yet
- NCM 106 Module 3FDocument18 pagesNCM 106 Module 3FMega SoundNo ratings yet
- C.antibiotic PolicyDocument3 pagesC.antibiotic PolicySCQA SHEIKHPURANo ratings yet
- Lesson 3 Adr ClassificationDocument3 pagesLesson 3 Adr ClassificationVincent Joshua TriboNo ratings yet
- Drug StudyDocument10 pagesDrug StudySam Eunice ChuaNo ratings yet
- Anti InfectivesDocument145 pagesAnti Infectivescharles babasaNo ratings yet
- Antibiotics en NurseDocument118 pagesAntibiotics en Nurseabsolomon777No ratings yet
- DS - Format - MedDocument3 pagesDS - Format - MedChristian MarquezNo ratings yet
- Chapter 10. ChemotherapyDocument157 pagesChapter 10. ChemotherapyAbel GirmaNo ratings yet
- Chapter 9 Inhibiting Growth of Pathogens in Vivo Using Antimicrobial AgentsDocument5 pagesChapter 9 Inhibiting Growth of Pathogens in Vivo Using Antimicrobial AgentsMa. Kate Nicole D. PadpadNo ratings yet
- Part 2 Controlling Microbial Growth in VitroDocument28 pagesPart 2 Controlling Microbial Growth in VitrosantiagofjannNo ratings yet
- A. Bacterial Cell Envelope: Contraindications (Antibiotics)Document28 pagesA. Bacterial Cell Envelope: Contraindications (Antibiotics)Mike GNo ratings yet
- On Guard: Build Resilience - Boost Immunity - Beat InfectionFrom EverandOn Guard: Build Resilience - Boost Immunity - Beat InfectionNo ratings yet
- Agra Case DigestDocument18 pagesAgra Case DigestCarla Virtucio50% (2)
- 1) Politics - Gilles Deleuze & Claire ParnetDocument2 pages1) Politics - Gilles Deleuze & Claire Parnetrayrod614No ratings yet
- Estate Admin NotesDocument119 pagesEstate Admin NotesLandon HangNo ratings yet
- Lopez Vs Pan American World AirwaysDocument2 pagesLopez Vs Pan American World AirwaysMark Gabriel B. MarangaNo ratings yet
- Macro Ecosystem ReportDocument27 pagesMacro Ecosystem ReportRhodelizaDeLeonTiotangco100% (1)
- Height Balanced Trees: Laboratory Module 4Document12 pagesHeight Balanced Trees: Laboratory Module 4ZafarIqbalNo ratings yet
- Meaning and Evolution of EntrepreneurshipDocument5 pagesMeaning and Evolution of EntrepreneurshipAnurag AllaNo ratings yet
- Bowen V Van Bramer Complaint With ExhibitDocument11 pagesBowen V Van Bramer Complaint With ExhibitQueens PostNo ratings yet
- Family Relations Questions Bar 2011 To 2008Document8 pagesFamily Relations Questions Bar 2011 To 2008Stephanie Dawn Sibi Gok-ongNo ratings yet
- GR 4 Eng FAL ExemplarDocument12 pagesGR 4 Eng FAL ExemplarShane WrightNo ratings yet
- Ïïa Su M!: (Source: Åg-Veda 10-151)Document6 pagesÏïa Su M!: (Source: Åg-Veda 10-151)vinod660No ratings yet
- WSC - BSBFIA401 SD Asset Register Worksheet V 1.0Document6 pagesWSC - BSBFIA401 SD Asset Register Worksheet V 1.0Gursheen KaurNo ratings yet
- DC CasesDocument104 pagesDC CasespaescorpisoNo ratings yet
- Flat Earth Mythology and Fact (Biblical Astronomer, No. 94, 2000)Document8 pagesFlat Earth Mythology and Fact (Biblical Astronomer, No. 94, 2000)tjmigoto@hotmail.comNo ratings yet
- NUMBERS AND WORDS Combining Quantitative and Qualitative Methods in A Single Large Scale Evaluation Study by Gretchen RossmanDocument24 pagesNUMBERS AND WORDS Combining Quantitative and Qualitative Methods in A Single Large Scale Evaluation Study by Gretchen Rossmanahmed elnimeiriNo ratings yet
- Class 2 PPT 1 Unit 1Document83 pagesClass 2 PPT 1 Unit 1ece Ms.G.Bhargavi100% (1)
- Intermediaries Liability in IndiaDocument42 pagesIntermediaries Liability in IndiaIshita ChadhaNo ratings yet
- BOLTER, Jay David. Writing Space Computers, Hypertext, and Remediation of PrintDocument4 pagesBOLTER, Jay David. Writing Space Computers, Hypertext, and Remediation of PrintGiovanna GuimarãesNo ratings yet
- ObstetricsDocument55 pagesObstetricsKristine Alejandro100% (1)
- Let Water Burn: SUMMARY (Expounded Perchapter)Document10 pagesLet Water Burn: SUMMARY (Expounded Perchapter)Johndale DimayugaNo ratings yet
- Nityananda SongsDocument32 pagesNityananda SongsMann Mahesh HarjaiNo ratings yet
- Houses Around The World: Read The Texts and Then Answer The QuestionsDocument2 pagesHouses Around The World: Read The Texts and Then Answer The QuestionsPORNESIAN - NAMJOONNo ratings yet
- Saba Final Book For EdittingDocument643 pagesSaba Final Book For Edittingfaresjohnson4No ratings yet
- Joao Baptista Lukombo Nzatuzola-2 PDFDocument4 pagesJoao Baptista Lukombo Nzatuzola-2 PDFMadaleno Sita António DiasNo ratings yet
- Jeeweon Moon Research PaperDocument11 pagesJeeweon Moon Research PaperJeeweon MoonNo ratings yet
- Sift RegisterDocument16 pagesSift RegisterSinta Ariyanti50% (2)
- The Leaf E-Newspaper - 2nd Semester, A.Y. 2022-2023Document20 pagesThe Leaf E-Newspaper - 2nd Semester, A.Y. 2022-2023Gilvert PanganibanNo ratings yet
- GannHarmonicTraders - Yahoo GroupsDocument2 pagesGannHarmonicTraders - Yahoo GroupsrajeshrraikarNo ratings yet
Pharma Antibiotics
Pharma Antibiotics
Uploaded by
valdez.adler.lOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharma Antibiotics
Pharma Antibiotics
Uploaded by
valdez.adler.lCopyright:
Available Formats
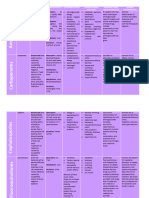
PHARMA ANTIBIOTICS
• Drug-to-Drug Interactions
Antibiotics − Diuretics, neuromuscular blockers, succinylcholine, or citrate
anticoagulated blood
Antibiotics are defined as:
Nursing Considerations for Patients Receiving
• Chemicals that inhibit specific bacteria
• Made in three ways Aminoglycosides
o By living microorganisms
• Assess:
o By synthetic manufacture
o For possible contraindications or cautions: allergy to any
o Through genetic engineering
aminoglycoside
o Perform a physical assessment
Signs of Infection
o Perform culture and sensitivity tests at the site of infection
o Conduct orientation and reflex assessment
• Fever
o Assess vital signs
• Lethargy
o Perform renal and liver function tests
• Slow-wave sleep induction
• Classic signs of inflammation (redness, swelling, heat, and pain)
Prototype Summary: Gentamicin
Antibiotic Use Across the Life Span
• Pediatric Population
• Adult Population
• Geriatric Population
• (See box 9.1)
Types of Antibiotics
• Bacteriostatic
o Those substances that prevent the growth of bacteria
• Bactericidal
o Those that kill bacteria directly
Bacteria and antibiotics
• Gram positive/negative
• Aerobic
Carbapenems
• Anaerobic
• New class of broad-spectrum antibiotics effective against gram-
positive and gram-negative bacteria
Goal of Antibiotic Therapy • Common medications:
o Doripenem (Doribax)
Decrease the population of the invading bacteria to a point where the
o Ertapenem (Invanz)
human immune system can effectively deal with the invader
o Imipenem– Cilastatin (Primaxin)
o Meropenem (Merrem IV).
Selecting Treatment • Bactericidal
• Indications
• Identification of the causative organism
− Treatment of serious infections caused by susceptible bacteria
• Based on the culture report, an antibiotic is chosen that has been
• Actions
known to be effective at treating the invading organism
− Inhibit cell membrane synthesis in susceptible bacteria, leading to
cell death
Bacteria Classification • Pharmacokinetics
− These drugs are rapidly absorbed if given IM and reach peak
• Gram-positive
levels at the end of the infusion if given IV.
− The cell wall retains a stain or resists decolorization with alcohol
− They are widely distributed throughout the body, although it is not
• Gram-negative
known whether they cross the placenta or enter breastmilk
− The cell wall loses a stain or is decolorized by alcohol
− Excreted unchanged in the urine and have an average half-life
• Aerobic
of 1 to 4 hours
− Depend on oxygen for survival
• Contraindications
• Anaerobic
• Known allergy to any of the carbapenms or betalactams; seizure
− Do not use oxygen
disorders, meningitis, pregnancy and lactation
• Adverse Effects
Bacteria and Resistance to Antibiotics • Pseudomembranous colitis, Clostridium difficile diarrhea, and
nausea and vomiting can lead to serious dehydration and
• Adapt to their environment
electrolyte imbalances, as well as to new serious
• The longer an antibiotic has been in use, the greater the chance
infections/Superinfections
that the bacteria will develop into a resistant strain
• Drug-to-drug interactions
• Valproic acid and Meropenem
Aminoglycosides
• A group of powerful antibiotics used to treat serious infections
Nursing Considerations for Patients Receiving
caused by gram-negative aerobic bacilli Carbapenems
• Common medications:
o Amikacin (Amikin), Gentamicin (Garamycin) • Assess:
o Kanamycin (Kantrex) o For possible contraindications or cautions: allergy to any
o Neomycin (Mycifradin) Carbapenem or beta-lactam
o Streptomycin o Perform physical assessment
o Tobramycin (Nebcin, Tobrex) o Perform culture and sensitivity tests
• Bactericidal o Conduct orientation and reflex assessment
• Indications: o VS and renal function tests
− Treatment of serious infections caused by susceptible bacteria
• Actions: Prototype Summary: Ertapenem
− Inhibits protein synthesis in susceptible strains of gram-negative
bacteria causing cell death
• Pharmacokinetics
− Poorly absorbed from the GI tract, but rapidly absorbed after
IM injection, reaching peak levels within 1 hour
− Widely distributed throughout the body, crossing the placenta
and entering breast milk
− Excreted unchanged in the urine and have an average half-life
of 2 to 3 hours
− Depend on the kidney for excretion and are toxic to the kidney
• Contraindications
− Known allergies, renal or hepatic disease, hearing loss
• Adverse Effects
− Ototoxicity and nephrotoxicity are the most significant
Cephalosporin's o Perform physical assessment
o Examine the skin for any rash or lesions
• Similar to penicillin in structure and activity o Perform culture and sensitivity tests
• Common medications o Orientation, affect, and reflexes
o First generation: cefadroxil (generic) and cephalexin (Keflex) o VS, and renal function tests
o Second: cefaclor (Ceclor), cefoxitin (generic), cefprozil
(generic), and cefuroxime (Zinacef) Prototype Summary: Ciprofloxacin
o Third: cefdinir (Omnicef), cefotaxime (Claforan), cefpodoxime
(generic), ceftazidime (Ceptaz,Tazicef), ceftibuten (Cedax),
and ceftriaxone (Rocephin)
o Fourth: cefditoren (Spectracef) and ceftaroline (Teflaro)
• Bactericidal and bacteriostatic
• Indications
− Treatment of infections caused by susceptible bacteria
• Action
− Interfere with the cell wall–building ability of bacteria when they
divide
• Pharmacokinetics
− Well absorbed from the GI tract
− Metabolized in the liver, excreted in the urine
− Cross the placenta and enter breast milk (see
Contraindications)
• Contraindications
− Allergies to cephalosporins or penicillin, hepatic or renal
impairment
• Adverse Effects
− Most significant - GI track
• Drug-to-Drug Interactions
− Aminoglycosides, oral anticoagulants, ETOH
Penicillins and Penicillinase – Resistant Antibiotics
Nursing Considerations for Patients Receiving • First antibiotic introduced for clinical use
Cephalosporins • Common medications
o G benzathine (Bicillin, Permapen), penicillin G potassium
• Assess: (Pfizerpen), penicillin G procaine (Wycillin), penicillin V (generic),
o For possible contraindications or cautions: known allergy to any amoxicillin (Amoxil, Trimox), and ampicillin (Principen)
cephalosporin or penicillin • Bactericidal
o Perform physical assessment • Indications
o Skin for any rash or lesions − Severe infections caused by sensitive organisms and broad
o Culture and sensitivity tests spectrum use
o Renal function tests • Actions
− Interfere with the ability of susceptible bacteria to build their cell
Prototype Summary: Cefaclor walls
• Pharmacokinetics
− rapidly absorbed from the GI tract, reaching peak levels in 1 hour.
excreted unchanged in the urine and enter breast milk
• Contraindications
− Allergies to penicillin or cephalosporins, renal disease, use
cautiously in patients who are pregnant or lactating
• Adverse Effects
− Most significant GI tract
• Drug–Drug Interactions
− Tetracyclines, parenteral aminoglycosides
Nursing Considerations for Patients Receiving Penicillins
and Penicillinase-Resistant Antibiotics
• Assess:
o Known allergy to any cephalosporins and penicillins
o Physical
o Skin and mucous membranes for any rashes or lesions
o Culture and sensitivity tests
o Respiratory status
o Abdomen and renal function
Fluoroquinolones
Prototype Summary: Amoxicillin
• Relatively new class of antibiotics with a broad spectrum of activity
• Common medications
o ciprofloxacin (Cipro), which is the most widely used
o fluoroquinolone, gemifloxacin (Factive), levofloxacin (Levaquin),
moxifloxacin (Avelox),norfloxacin (Noroxin), ofloxacin (Floxin,
Ocuflox), and finafloxacin (Xtoro)
• Bactericidal
• Indications
− Treating infections caused by susceptible strains of gram-negative
bacteria. Includes: urinary track, respiratory track, and skin
infections
• Actions
− Interferes with DNA replication in susceptible gram-negative
bacteria, preventing cell reproduction
• Pharmacokinetics
− Absorbed in GI tract, metabolized in the liver, excreted in urine
and feces and cross the placenta and enter breast milk
• Contraindications
− Known allergy, pregnancy, or lactating women and renal
disfunction
• Adverse Effects
− Most common: Headache, dizziness, insomnia and depression Sulfonamides
• Drug-to-Drug Interactions
− Antacids, quinidine, theophylline • Drugs that inhibit folic acid synthesis
• Most common medications
Nursing Considerations for Patients Receiving o sulfadiazine (generic)
o sulfasalazine (Azulfidine)
Fluoroquinolones o cotrimoxazole (Septra, Bactrim)
• Bacteriostatic
• Assess:
o Known allergy to any fluoroquinolone
• Action Prototype Summary: Tetracycline
− block para-aminobenzoic acid to prevent the synthesis of folic acid
in susceptible bacteria
• Indications
− Treatment of infections caused by gram-negative and gram-
positive bacteria
• Pharmacokinetics
− Well absorbed from the GI tract
− Metabolized in the liver, excreted in the urine and are teratogenic
• Contraindications
− Known allergy to any sulfonamide, thiazide diuretics and
pregnancy
• Adverse Effects
− GI symptoms; Renal effects related to the filtration of the drug
• Drug-to-Drug Interactions
− tolbutamide, tolazamide, glyburide, glipizide, or chlorpropamide
and cyclosporine
Nursing Considerations for Patients Receiving
Sulfonamides
• Assessment:
o Known allergy to any sulfonamide, sulfonylureas, or thiazide
Antimycobacterial
diuretics
o Physical status
• Contain pathogens causing TB and leprosy
o Skin and mucous membranes for any rash or lesions
• Most common medications
o Specimens for culture and sensitivity tests
o Rifabutin (Mycobutin), isoniazid (generic), rifampin (Rifadin),
o Respiratory status
pyrazinamide (generic), ethambutol, (Myambutol), streptomycin
o Orientation, affect, and reflexes
(generic), and rifapentine, (Priftin)
o Abdomen
• Action
o Renal function tests
− Act on the DNA of the bacteria leading to lack of growth and
o Complete blood count
eventual bacterial death for TB and Leprosy
• Indications
Prototype Summary: Cotrimoxazole − Treatment of TB and Leprosy
• Pharmacokinetics
− Well absorbed from the GI tract
− Metabolized in the liver, excreted in the urine, cross the placenta
and enter breast
• Contraindications
− Allergy, renal or hepatic failure, CNS dysfunction and pregnancy
• Adverse Effects
− CNS effects and GI irritation
• Drug-to-Drug Interactions
− Rifampin and INH can cause liver toxicity
Nursing Considerations for Patients Receiving
Antimycobacterials
• Assess:
o Known allergy to any antimycobacterial drug
o History of renal or hepatic disease and CNS dysfunction
o Physical examination
o Skin for any rash or lesions
o Culture and sensitivity testing
o Respiratory status and evaluate renal and hepatic function tests
Tetracyclines
Prototype Summary: Isoniazid
• Developed as semisynthetic antibiotics based on the structure of a
common soil mold
• Most common medications
o Tetracycline (generic)
o demeclocycline (generic)
o doxycycline (Doryx, Vibromycin)
o minocycline (Arestin, Minocin)
• Bacteriostatic
• Action
− Inhibits protein synthesis in susceptible bacteria, preventing cell
replication
• Indications
− Treatment of various infections caused by susceptible strains of
bacteria; acne when penicillin is contraindicated for eradication
of susceptible organisms and when penicillin is contraindicated
• Pharmacokinetics
− Adequately absorbed from the GI tract
− Concentrated in the liver, excreted unchanged in the urine
− Cross the placenta and pass into breast milk
• Contraindications
− Known allergy to tetracyclines or to tartrazine, pregnancy,
lactation and renal and hepatic dysfunction, Penicillin G, oral
contraceptive therapy, methoxyflurane, digoxin Other Antibiotics
• Adverse Effects
− Most GI, but possible damage to the teeth and bones. Ketolides, Lincosamides, Lipoglycopeptides,
• Drug-to-Drug Interactions Macrolides, Oxazolidinones, Monobactam,
− penicillin G, oral contraceptives, Digoxin
• Antibiotics that do not fit into the large antibiotic classes
Nursing Considerations for Patients Receiving • Most common medications
Tetracyclines o telithromycin (Ketek), telithromycin, Clindamycin (Cleocin)
televancin (Vibativ), dalbavancin (Dalvance), and oritavancin
• Assess: (Orbactiv), azithromycin (Zithromax), clarithromycin (Biaxin),
o Known allergy to any tetracycline or to tartrazine Tedizolid (Sivextra) and linezolid (Zyvox), and aztreonam (Azactam)
o Physical examination • Bactericidal and bacteriostatic
o Skin for any rash or lesions • Actions and Indications
o Culture and sensitivity tests − Treatment of severe infections
o Respiratory status • Pharmacokinetics
o Renal and liver function test reports − All rapidly absorbed, metabolized by the liver and excreted in urine
or feces and may cross the placenta, and does pass into breast milk
• Contraindications and Cautions Prototype Summary: Aztreonam
− Known allergy, hepatic or renal impairment, Myasthenia Gravis,
pregnant and lactating patients, phenylketonuria, MAO inhibitors,
• Adverse Effects
− Most significant CNS and GI, hepatic enzyme elevation and
superinfections
• Drug to -Drug Interactions
− Pimozide, simvastatin, lovastatin, or atorvastatin, NSAIDs, nafcillin,
cephradine, and metronidazole, foods containing tyramine with
Oxazolidinones and MAO inhibitors
Nursing Considerations for patients receiving Other
Antibiotics
• Assess
o Known allergy to ketolides, lincosamides, lipoglycopeptides,
macrolides, oxazolidinones, and monobactams
o History of renal and hepatic disease
o Physical assessment
o Skin for any rash or lesions
o Culture and sensitivity testing
o Temperature to detect infection
o Liver and renal function test values
o Baseline electrocardiogram New Classes of Antibiotics and Adjuncts
Prototype Summary: Telithromycin • Daptomycin
• Linezolid (Zyvox)
• Fidaxomicin (Dificid)
• Tigecycline
Prototype Summary: Clindamycin
Prototype Summary: Erythromycin
You might also like
- Celtic Ogham BookletDocument11 pagesCeltic Ogham Bookletoftaran100% (3)
- Leonard Baskin & Ted HughesDocument16 pagesLeonard Baskin & Ted Hughesmgter100% (1)
- CHAPTER 9 ReviewerDocument4 pagesCHAPTER 9 ReviewerHannah BuquironNo ratings yet
- Semifinal TransesDocument9 pagesSemifinal TransesDianneNo ratings yet
- Antibiotics PharmaDocument4 pagesAntibiotics PharmaJohn Dave V. VillarmenteNo ratings yet
- L16 ANTIBIOTICS - IN - ORAL - MAXILLOFACIAL - SURGERY Copy 2Document19 pagesL16 ANTIBIOTICS - IN - ORAL - MAXILLOFACIAL - SURGERY Copy 2Ju JuNo ratings yet
- ANTIBIOTICS Pharmacology NursingDocument10 pagesANTIBIOTICS Pharmacology NursingRalph Alfonse De JesusNo ratings yet
- Midterms PharmacologyDocument35 pagesMidterms PharmacologyMutya XDNo ratings yet
- Byron - Recurrent Resistant Urinary Tract InfectionsDocument8 pagesByron - Recurrent Resistant Urinary Tract InfectionsC GNo ratings yet
- Anti InfectivesDocument4 pagesAnti InfectivespaderamosNo ratings yet
- Anti InfectivesDocument126 pagesAnti Infectiveseunice lachicaNo ratings yet
- Emnc 4 North Drug StudyDocument12 pagesEmnc 4 North Drug StudyFrancesca Aurea MagumunNo ratings yet
- (PHARMA A) 3.3 - Antibiotics I - Dr. Cruz (2024)Document15 pages(PHARMA A) 3.3 - Antibiotics I - Dr. Cruz (2024)Miguel Luis NavarreteNo ratings yet
- Mechanisms of Antimicrobial ResistanceDocument12 pagesMechanisms of Antimicrobial ResistanceFrances Lau Yee ChinNo ratings yet
- 6-Introduction To AntibioticsDocument10 pages6-Introduction To AntibioticsKanishka TiwariNo ratings yet
- Pharma-Lesson 1-3 Therapeutic DrugsDocument7 pagesPharma-Lesson 1-3 Therapeutic DrugsFia CelerioNo ratings yet
- Reviewer in PharmacologyDocument20 pagesReviewer in PharmacologyJhayneNo ratings yet
- Unit 4Document111 pagesUnit 4Bea Bianca CruzNo ratings yet
- Table of AntibioticsDocument5 pagesTable of AntibioticsBerenese DianneNo ratings yet
- Overview of Infections and AntimicrobialsDocument43 pagesOverview of Infections and Antimicrobialszainab ElsayedNo ratings yet
- Lec - Bacte - Non Fermentative Gram Negative Bacilli - MidtermsDocument2 pagesLec - Bacte - Non Fermentative Gram Negative Bacilli - MidtermsJashmine May TadinaNo ratings yet
- Antimicrobial AgentsDocument14 pagesAntimicrobial AgentsAllyssa TolibasNo ratings yet
- Microbiology and Parasitology Week 3. ABCDDocument21 pagesMicrobiology and Parasitology Week 3. ABCDohsehuns wifeuNo ratings yet
- Antimicrobial Lecture NotesDocument55 pagesAntimicrobial Lecture Noteshunarsandhu100% (2)
- C. Bacteriology L6 Antimicrobial Agents and Resistance LaboratoryDocument6 pagesC. Bacteriology L6 Antimicrobial Agents and Resistance LaboratoryChelze Faith DizonNo ratings yet
- 659fdeb8aea86969913c25a1-1704984472-IHBB Lec IS Lecture NotesDocument3 pages659fdeb8aea86969913c25a1-1704984472-IHBB Lec IS Lecture NotesAnne Chelsea Ramirez OritNo ratings yet
- Controlling Microbial Growth in Vivo Using Antimicrobial AgentsDocument30 pagesControlling Microbial Growth in Vivo Using Antimicrobial AgentsJen PanganibanNo ratings yet
- Biosel-Mikro Mekanisme Antibiotik 2022Document45 pagesBiosel-Mikro Mekanisme Antibiotik 20226. Putu Arbita DivyaNo ratings yet
- ToB S5 Lecture 1Document2 pagesToB S5 Lecture 1LT DRAGONXNo ratings yet
- Lec 5: Antimycobacerial Drugs by Dr. Frederick Loyola July 7, 2010Document7 pagesLec 5: Antimycobacerial Drugs by Dr. Frederick Loyola July 7, 2010Rachel Leslie de LeonNo ratings yet
- CefuroximeDocument1 pageCefuroximehahahahaaaaaaaNo ratings yet
- Antibiotics 2Document38 pagesAntibiotics 2Tommy ZeusNo ratings yet
- Antibiotics (Role and Abuse) 2016Document35 pagesAntibiotics (Role and Abuse) 2016Mohd Johari Mohd ShafuwanNo ratings yet
- Antibacterial and Antiinfective AgentsDocument80 pagesAntibacterial and Antiinfective AgentsAbbeygale GalanNo ratings yet
- Lecture 4 - SCI 8007SEF Medical Microbiology & Virology-Introduction To Medical Microbiology I - 24 Sep 2023Document62 pagesLecture 4 - SCI 8007SEF Medical Microbiology & Virology-Introduction To Medical Microbiology I - 24 Sep 2023Ada ChanNo ratings yet
- Pharma Part 1 and 2Document10 pagesPharma Part 1 and 2BRYCE WILLIAM GONo ratings yet
- W1 Antimicrobial DrugsDocument8 pagesW1 Antimicrobial Drugsseanne kskwkwkaNo ratings yet
- 6 Inhibiting The Growth of Pathogens in VivoDocument27 pages6 Inhibiting The Growth of Pathogens in VivoAinaB ManaloNo ratings yet
- Summary of AntibioticsDocument11 pagesSummary of AntibioticsAamir MunawarNo ratings yet
- Module 3Document6 pagesModule 3richelleambrocio054No ratings yet
- (BACTE-LEC) 8. Antimicrobial Susceptibility TestingDocument6 pages(BACTE-LEC) 8. Antimicrobial Susceptibility TestingCarlo CataagNo ratings yet
- Using Antimicrobial Agents To Control Mirobial Growth in VivoDocument39 pagesUsing Antimicrobial Agents To Control Mirobial Growth in VivoHannah BuquironNo ratings yet
- Chapter 29 Child With CancerDocument9 pagesChapter 29 Child With CancerMARCERA JERALDINE ALESSA P.No ratings yet
- PHARMACOLOGY Anti Microbial DrugsDocument17 pagesPHARMACOLOGY Anti Microbial DrugsLeilani Sablan100% (2)
- CampylobacterDocument2 pagesCampylobactersarguss14No ratings yet
- Drug StudyDocument9 pagesDrug StudyGenovee Angela FayeNo ratings yet
- Antibiotics 1Document64 pagesAntibiotics 1Justin Ancog100% (1)
- Pharma-Module 8Document5 pagesPharma-Module 8Myles CardelNo ratings yet
- Antibiotics and Spectrum of ActionDocument40 pagesAntibiotics and Spectrum of ActionNUBWA MEDUGUNo ratings yet
- Inhibiting The Growth of Pathogens in VivoDocument25 pagesInhibiting The Growth of Pathogens in VivoRoshwell RegalaNo ratings yet
- NCM 106 Module 3FDocument18 pagesNCM 106 Module 3FMega SoundNo ratings yet
- C.antibiotic PolicyDocument3 pagesC.antibiotic PolicySCQA SHEIKHPURANo ratings yet
- Lesson 3 Adr ClassificationDocument3 pagesLesson 3 Adr ClassificationVincent Joshua TriboNo ratings yet
- Drug StudyDocument10 pagesDrug StudySam Eunice ChuaNo ratings yet
- Anti InfectivesDocument145 pagesAnti Infectivescharles babasaNo ratings yet
- Antibiotics en NurseDocument118 pagesAntibiotics en Nurseabsolomon777No ratings yet
- DS - Format - MedDocument3 pagesDS - Format - MedChristian MarquezNo ratings yet
- Chapter 10. ChemotherapyDocument157 pagesChapter 10. ChemotherapyAbel GirmaNo ratings yet
- Chapter 9 Inhibiting Growth of Pathogens in Vivo Using Antimicrobial AgentsDocument5 pagesChapter 9 Inhibiting Growth of Pathogens in Vivo Using Antimicrobial AgentsMa. Kate Nicole D. PadpadNo ratings yet
- Part 2 Controlling Microbial Growth in VitroDocument28 pagesPart 2 Controlling Microbial Growth in VitrosantiagofjannNo ratings yet
- A. Bacterial Cell Envelope: Contraindications (Antibiotics)Document28 pagesA. Bacterial Cell Envelope: Contraindications (Antibiotics)Mike GNo ratings yet
- On Guard: Build Resilience - Boost Immunity - Beat InfectionFrom EverandOn Guard: Build Resilience - Boost Immunity - Beat InfectionNo ratings yet
- Agra Case DigestDocument18 pagesAgra Case DigestCarla Virtucio50% (2)
- 1) Politics - Gilles Deleuze & Claire ParnetDocument2 pages1) Politics - Gilles Deleuze & Claire Parnetrayrod614No ratings yet
- Estate Admin NotesDocument119 pagesEstate Admin NotesLandon HangNo ratings yet
- Lopez Vs Pan American World AirwaysDocument2 pagesLopez Vs Pan American World AirwaysMark Gabriel B. MarangaNo ratings yet
- Macro Ecosystem ReportDocument27 pagesMacro Ecosystem ReportRhodelizaDeLeonTiotangco100% (1)
- Height Balanced Trees: Laboratory Module 4Document12 pagesHeight Balanced Trees: Laboratory Module 4ZafarIqbalNo ratings yet
- Meaning and Evolution of EntrepreneurshipDocument5 pagesMeaning and Evolution of EntrepreneurshipAnurag AllaNo ratings yet
- Bowen V Van Bramer Complaint With ExhibitDocument11 pagesBowen V Van Bramer Complaint With ExhibitQueens PostNo ratings yet
- Family Relations Questions Bar 2011 To 2008Document8 pagesFamily Relations Questions Bar 2011 To 2008Stephanie Dawn Sibi Gok-ongNo ratings yet
- GR 4 Eng FAL ExemplarDocument12 pagesGR 4 Eng FAL ExemplarShane WrightNo ratings yet
- Ïïa Su M!: (Source: Åg-Veda 10-151)Document6 pagesÏïa Su M!: (Source: Åg-Veda 10-151)vinod660No ratings yet
- WSC - BSBFIA401 SD Asset Register Worksheet V 1.0Document6 pagesWSC - BSBFIA401 SD Asset Register Worksheet V 1.0Gursheen KaurNo ratings yet
- DC CasesDocument104 pagesDC CasespaescorpisoNo ratings yet
- Flat Earth Mythology and Fact (Biblical Astronomer, No. 94, 2000)Document8 pagesFlat Earth Mythology and Fact (Biblical Astronomer, No. 94, 2000)tjmigoto@hotmail.comNo ratings yet
- NUMBERS AND WORDS Combining Quantitative and Qualitative Methods in A Single Large Scale Evaluation Study by Gretchen RossmanDocument24 pagesNUMBERS AND WORDS Combining Quantitative and Qualitative Methods in A Single Large Scale Evaluation Study by Gretchen Rossmanahmed elnimeiriNo ratings yet
- Class 2 PPT 1 Unit 1Document83 pagesClass 2 PPT 1 Unit 1ece Ms.G.Bhargavi100% (1)
- Intermediaries Liability in IndiaDocument42 pagesIntermediaries Liability in IndiaIshita ChadhaNo ratings yet
- BOLTER, Jay David. Writing Space Computers, Hypertext, and Remediation of PrintDocument4 pagesBOLTER, Jay David. Writing Space Computers, Hypertext, and Remediation of PrintGiovanna GuimarãesNo ratings yet
- ObstetricsDocument55 pagesObstetricsKristine Alejandro100% (1)
- Let Water Burn: SUMMARY (Expounded Perchapter)Document10 pagesLet Water Burn: SUMMARY (Expounded Perchapter)Johndale DimayugaNo ratings yet
- Nityananda SongsDocument32 pagesNityananda SongsMann Mahesh HarjaiNo ratings yet
- Houses Around The World: Read The Texts and Then Answer The QuestionsDocument2 pagesHouses Around The World: Read The Texts and Then Answer The QuestionsPORNESIAN - NAMJOONNo ratings yet
- Saba Final Book For EdittingDocument643 pagesSaba Final Book For Edittingfaresjohnson4No ratings yet
- Joao Baptista Lukombo Nzatuzola-2 PDFDocument4 pagesJoao Baptista Lukombo Nzatuzola-2 PDFMadaleno Sita António DiasNo ratings yet
- Jeeweon Moon Research PaperDocument11 pagesJeeweon Moon Research PaperJeeweon MoonNo ratings yet
- Sift RegisterDocument16 pagesSift RegisterSinta Ariyanti50% (2)
- The Leaf E-Newspaper - 2nd Semester, A.Y. 2022-2023Document20 pagesThe Leaf E-Newspaper - 2nd Semester, A.Y. 2022-2023Gilvert PanganibanNo ratings yet
- GannHarmonicTraders - Yahoo GroupsDocument2 pagesGannHarmonicTraders - Yahoo GroupsrajeshrraikarNo ratings yet