Professional Documents
Culture Documents
Effectiveness of T-Piece Resuscitator Versus Self-Inflating Bag During Birth Resuscitation in Very Low Birth Weight Infants
Effectiveness of T-Piece Resuscitator Versus Self-Inflating Bag During Birth Resuscitation in Very Low Birth Weight Infants
Uploaded by
Raja SekarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effectiveness of T-Piece Resuscitator Versus Self-Inflating Bag During Birth Resuscitation in Very Low Birth Weight Infants
Effectiveness of T-Piece Resuscitator Versus Self-Inflating Bag During Birth Resuscitation in Very Low Birth Weight Infants
Uploaded by
Raja SekarCopyright:
Available Formats
EFFECTIVENESS OF T-PIECE RESUSCITATOR VERSUS
SELF-INFLATING BAG DURING BIRTH RESUSCITATION
IN VERY LOW BIRTH WEIGHT INFANTS
Pitiporn Siripattanapipong, Kittaya Nakornchai, Punnanee Wutthigate and Ratchada Kitsommart
Division of Neonatology, Department of Pediatrics, Faculty of Medicine Siriraj Hospital, Mahidol University,
Bangkok, Thailand
Abstract. T-piece resuscitator (TPR) and self-inflating bag (SIB) are two different devices used
for positive-pressure ventilation (PPV) during birth resuscitation. However, the effectiveness
of TPR has not been clearly demonstrated. The aim of this study was to compare the rate of
endotracheal intubation between TPR and SIB for PPV during birth resuscitation in very low
birth weight (VLBW) infants. This retrospective cohort study was conducted in infants born with
either gestational age <33 weeks or birth weight <1,500 grams and who received PPV during
birth resuscitation at Siriraj Hospital during the 2014 and 2016 study period. Medical charts
were reviewed to identify type of device and respiratory outcome. A total of 128 infants were
included 67 infants received PPV via TPR and 61 received PPV via SIB. The TPR group had lower
gestational age and lower birth weight than the SIB group (28.6 vs 30.2 weeks; p<0.001 and
1,061.1 vs 1,288.3 g; p<0.001). There was no significant difference in intubation rate between
groups (adjusted odds ratio=0.83, 95% confidence interval: 0.38-1.80). However, incidence of
mortality or oxygen requirement at 36 weeks postmenstrual age was significantly higher in the
TPR group (44.8% vs 25.4%; p=0.02). In conclusion, use of TPR for PPV in VLBW infants did
not improve intubation rate during birth resuscitation when compared with SIB.
Keywords: birth resuscitation, positive-pressure ventilation, self-inflating bag, T-piece
resuscitator, very low birth weight infants
INTRODUCTION faced by clinicians during birth resuscitation of
preterm infants is to promoting ventilation with
Preterm infants are born with several minimal lung injury. Strategies to promote lung
physiological limitations that adversely affect recruitment in preterm infants with breathing
their ability to establish effective ventilation, such difficulty at birth in order to avoid intubation have
as poor respiratory control, compliant chest wall, been accepted in modern neonatal practice (te
surfactant deficiency, and large amount of lung Pas and Walther, 2007; te Pas et al, 2009; Lista
fluid (Polin et al, 2011). One of the challenges et al, 2011; Grasso et al, 2015). However, infants
with severe lung conditions may require positive-
Correspondence: Ratchada Kitsommart, pressure ventilation (PPV). PPV provides forced
MD, Division of Neonatology, Department of ventilation and oxygenation into the respiratory
Pediatrics, Faculty of Medicine Siriraj Hospital, system. As a result, there is some associated risk
Mahidol University, 2 Wanglang Road, Bangkok of inflicting lung damage. Experimental studies
Noi, Bangkok, 10700, Thailand. have shown that aggressive ventilation during
Tel: +66 (0) 86 066 6860; Fax: +66 (0) 2411 3010 birth resuscitation triggers a process of lung injury
E-mail: rkitsommart@hotmail.com, ratchada.kit that can last for several weeks (Bjorklund et al,
@mahidol.ac.th 1997; Wilson et al, 2003; Hillman et al, 2007).
Vol. 48 (Supplement 2) 2017 249
Southeast Asian J Trop Med Public Health
Among recommended PPV devices, self- were excluded. Included infants who received
inflating bag (SIB) is commonly used due to PPV during birth resuscitation were allocated
several recognized advantages (Perlman et al, into either the T-piece resuscitator (TPR) group
2010; John, 2011). However, the use of T-piece or the self-inflating bag (SIB) group.
resuscitator (TPR) has been increasing over the
As a tertiary care center and a teaching
past several years especially during preterm re-
hospital, the Department of Obstetrics and
suscitation, because it provides constant pressure
Gynecology manages 7,000 to 9,000 deliveries
delivery throughout the maneuver (Hoskyns et
each year, including both normal and high-risk
al, 1987; Finer et al, 2001; Bennett et al, 2005;
pregnancies. Obstetric practices for preterm
Oddie et al, 2005).
delivery at our center follow American College
American Academy of Pediatrics (AAP) 2011 of Obstetrics and Gynecology (ACOG) and
guidelines and International Liaison Committee institutional guidelines, including antenatal
on Resuscitation (ILCOR) guidelines (John, 2011) corticosteroid administration, intrapartum
recommend either device for PPV during birth antibiotic prophylaxis, and tocolytic treatment
resuscitation. Some controlled trials reported for the management of preterm labor (ACOG
higher efficacy in TPR than in SIB (Dawson et al, Committee on Obstetric Practice, 2011a; ACOG
2011b; Szyld et al, 2014; Thakur et al, 2015). Committee on Obstetric Practice, 2011b; ACOG
However, few studies have demonstrated the Committee on Practice Bulletins - Obstetrics,
superiority of TPR over SIB in real-life clinical 2012). All preterm deliveries are attended and
practice. resuscitated by a dedicated team that includes a
neonatal fellow, a pediatric resident, and at least
The primary aim of this study was to compare
one experienced nurse following the AAP/ILCOR
the rate of endotracheal intubation between TPR
guidelines (2011) (John, 2011). We routinely
and SIB for PPV during birth resuscitation in very
attempt non-invasive ventilation in newly born
low birth weight infants. The secondary objec-
infants who develop signs of respiratory distress.
tive was to compare other short-term outcomes
Intubation is considered only in infants who
between groups.
develop significant respiratory distress despite
nasal continuous positive-airway pressure or
MATERIALS AND METHODS
severely depressed conditions, such as perinatal
This retrospective cohort study was con- asphyxia.
ducted in infants born with either gestational
Both TPR and SIB are available for resuscita-
age less than 33 weeks or birth weight less
tion in the delivery rooms at our center. TPR
than 1,500 grams and who received PPV dur-
can take of form of a mobile device (Neopuff®;
ing birth resuscitation at Siriraj Hospital from
Fisher & Paykel Healthcare, Auckland, New Zea-
January 2014 to March 2016. Siriraj Hospital is
land) or a TPR system that is a component part of
tertiary referral center. The protocol for this study
a comprehensive resuscitation system. According
was approved by the Siriraj Institutional Review
to policy at our center, PPV is initiated in infants
Board (SIRB), Faculty of Medicine Siriraj Hospital,
with less than 30 weeks gestation using a TPR
Mahidol University, Bangkok, Thailand.
with an initial peak inspiratory pressure (PIP) set-
Medical records were reviewed for prenatal ting of 20 cm H2O and a positive end-expiratory
history, type of PPV device used, and respiratory pressure (PEEP) of 5 cm H2O. The SIB system uses
outcomes. Infants who did not require PPV, and a 280 ml MR-100TM Silicone Manual Resuscitator
those who had major congenital malformation (GaleMed, Taipei, Taiwan). The self-inflating bag
that could affect respiratory outcomes at birth was not routinely connected to a PEEP valve.
250 Vol. 48 (Supplement 2) 2017
T-Piece Resuscitator During Birth Resuscitation
Oxygen administration during study period was Statistical analysis
initiated at FiO2 of 0.4, and was adjusted accord- Data analysis was performed using PASW
ing to pre-ductal target saturation. Statistics version 18.0 (IBM, Armonk, NY). Cat-
egorical variables are presented as number and
Sample size calculation percentage. Normally distributed continuous
The sample size was calculated using intuba- variables are presented as mean ± standard de-
tion rate data from a previous study (52% vs viation, and non-normally distributed continuous
69% in the TPR group and SIB group, respec- variables are presented as median and interquar-
tively) (Szyld et al, 2014). Using a significance tile range. Continuous variables were compared
level of 0.05 (2-sided) and a power of 80%, a using Student’s t-test or Mann-Whitney U
total of 258 infants (129 infants per group) was test, depending on their distribution pattern.
calculated. However a strict preterm resuscita- Categorical variables were compared using chi-
tion protocol was established at our center in square test or Fisher’s exact test. A p-value <0.05
2013, we decided to include only infants that was considered statistically significant. Adjusted
were born in 2014 and later. odds ratios for protective factors or risk factors
Infants with <33 weeks gestation or
birth weight <1,500 g
(N=332)
Excluded (203)
• Congenital anomaly 7
• Diaphragmatic hernia 3
• Hydrops fetalis 7
• Lung hypoplasia 2
• Birth before arrival 1
• Positive pressure ventilation not given 183
Eligible infants
(N=129)
Excluded
• Unknown device 1
T-Piece Resuscitator group Self-Inflating Bag group
(TPR) (SIB)
(n=67) (n=61)
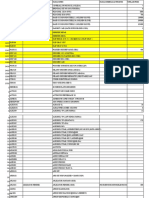
Fig 1– Flow diagram of very low birth weight infants who required positive-pressure ventilation during
birth resuscitation (N=128).
Vol. 48 (Supplement 2) 2017 251
Southeast Asian J Trop Med Public Health
for endotracheal intubation were derived from SIB group mothers (p=0.02). Median 1-minute
binary logistic regression analysis. Apgar score was similar between groups.
RESULTS A comparison of infant outcomes between
groups is given in Table 2. There was no sig-
Of 332 eligible preterm infants, 128 infants
nificant difference in intubation rate between
(38.9%) that required PPV during birth resus-
groups (58.2% vs 54.1% for the TPR and SIB
citation were included in the final analysis. Of
groups, respectively; p=0.64). Infants in the TPR
those 128 infants, 67 received PPV via T-piece
group had a higher rate of chest compression,
resuscitator (TPR group) and 61 received PPV via
but the difference between groups did not reach
self-inflating bag (SIB group). A flow diagram
statistical significance. Importantly – although
of the infant selection and allocation process is
respiratory outcomes, including respiratory dis-
shown in Fig 1.
tress syndrome (RDS), requirement for surfactant
Demographic and clinical characteristics of administration, and air leak syndrome were simi-
mothers and infants are presented in Table 1. lar, the incidence of mortality or oxygen require-
TPR group infants had lower gestational age ment at 36 weeks postmenstrual age (PMA) was
and lower birth weight than SIB group infants higher in the TPR group than in the SIB group
(28.6 vs 30.2 weeks; p<0.001 and 1,061.1 vs (44.8% vs 25.4%; p=0.02). Using binary logistic
1,288.3 g; p<0.001, respectively). TPR group regression model and adjusted for birth weight,
mothers had significantly more fetal distress than gender, singleton, fetal distress, and maternal
Table 1
Demographic and clinical characteristics of mothers and infants.
Characteristics TPR group SIB group p-value
Mothers, n 62 60
Age (years), mean±SD 29.9±7.6 29.7±8.3 0.725
Hypertensive disorder, n (%) 20 (32.3) 14 (23.3) 0.272
Diabetes, n (%) 4 (6.5) 9 (15) 0.151
Preterm labor, n (%) 39 (62.9) 47 (78.3) 0.062
Antepartum hemorrhage, n (%) 5 (8.1) 6 (10) 0.709
Fetal distress, n (%) 57 (91.9) 46 (76.7) 0.020a
Antenatal corticosteroids, n (%) 61 (91.0) 49 (80.3) 0.082
Cesarean delivery, n (%) 47 (75.8) 36 (60) 0.061
Infants, n 67 61
Gestational age (weeks), mean±SD 28.6±2.3 30.2±2.7 <0.001a
Birth weight (grams), mean±SD 1,061.1± 312.5 1,288.3±321.4 <0.001a
Male gender, n (%) 30 (44.8) 22 (36.1) 0.316
Singleton, n (%) 47 (70.1) 45 (73.8) 0.649
Intrauterine growth retardation, n (%) 9 (13.4) 8 (13.1) 0.958
a
p< 0.05, statistically significant. SIB, self-inflating bag; TPR, T-piece resuscitator.
252 Vol. 48 (Supplement 2) 2017
T-Piece Resuscitator During Birth Resuscitation
corticosteroid administration, the adjusted odds tively small RCT (Dawson et al, 2011a) conducted
ratio for intubation in the TPR group was 0.83 in very preterm infants found no difference in
(95% confidence interval: 0.38-1.80; p=0.63). resuscitation outcomes between devices. The
other two studies (Szyld et al, 2014; Thakur et
DISCUSSION al, 2015) reported more favorable outcomes,
including intubation rate in the delivery room, in
T-piece resuscitator (TPR) is increasingly used
the TPR group than the SIB group. It should be
for PPV during birth resuscitation. TPR is a pres-
noted that the latter two studies recruited only a
sure limiting device that has been documented
small proportion of very low birth weight infants,
as an alternative device in the Neonatal Resusci-
and their results are more likely to represent late
tation Program (NRP) guideline since 2011(John,
preterm infants than very preterm infants.
2011). The device comes with an adjustable PEEP
and controlled PIP. Although it is a simple device, This study focused on very low birth weight
experienced staff are needed to effectively set-up infants, because they are more likely to develop
and adjust all necessary parameters during resus- respiratory compromise at birth and chronic lung
citation (McHale et al, 2008; Hawkes et al, 2010; disease later in life. Interestingly, our intubation
Roehr et al, 2010). The potential advantages of rate in both study groups was higher than rates
lung protection and lung recruitment at birth published in other reports. One potential explana-
in preterm infants has influenced the increased tion is that over three quarter of our population
popularity of TPR among clinicians. Experimen- had history of fetal distress (92% and 77% in
tal studies reported that pressure delivered by the TPR- and SIB groups, respectively), which was
the TPR is more accurate and consistent than reflected in the median Apgar score at 1 minute
SIB throughout the PPV maneuver (Finer et al, of only 4 in both groups. This indicates that our
2001; O’Donnell et al, 2005; Oddie et al, 2005; study population was a high-risk population that
Dawson et al, 2011a). Three major RCT studies had not only respiratory issues, but also perfusion
compared efficacy between TPR and SIB. A rela- problems. This population is commonly encoun-
Table 2
Comparison of infant outcomes between groups.
Outcome measure TPR group SIB group p-value OR 95% CI
(n = 67) (n = 61)
1-minute Apgar scorea 4 (1,5) 4 (3,5) 0.210 - -
5-minute Apgar score a
7 (5,8) 8 (5,9) 0.149 - -
Intubation in delivery room, n (%) 39 (58.2) 33 (54.1) 0.640 1.18 0.59-2.38
Chest compression, n (%) 8 (11.9) 3 (4.9) 0.212 2.62 0.66-10.37
Diagnosis of RDS, n (%) 20 (29.9) 16 (26.2) 0.649 1.19 0.55-2.60
Surfactant administration, n (%) 13 (19.4) 11 (18) 0.843 1.09 0.45-2.67
Air leaks, n (%) 8 (11.9) 6 (9.8) 0.703 1.24 0.41-3.81
Mortality/use of oxygen at 36 week- 30 (44.8) 15 (25.4) 0.024b
2.38 1.11-5.08
PMA, n (%)
a
Apgar scores are presented as median (interquartile range). CI, confidence interval; OR, odds ratio;
PMA, post-menstrual age; RDS, respiratory distress syndrome; SIB, self-inflating bag; TPR, T-piece
resuscitator. bp< 0.05, statistically significant.
Vol. 48 (Supplement 2) 2017 253
Southeast Asian J Trop Med Public Health
tered in real-life clinical practice, which may be want to report the setup of using device rather
in contrast to relatively well preterm infants that than the efficacy of the device itself.
were included in previous RCT studies (Szyld et
In conclusion, use of T-piece resuscitator
al, 2014; Thakur et al, 2015). We also found no
for PPV in preterm infants less than 33 weeks
significant difference in intubation rate between
gestation or in very low birth weight infants did
the TPR and SIB groups. This finding is consistent
not improve intubation rate in a real-life clinical
with a previous RCT study in preterm infants
setting when compared to self-inflating bags.
(Dawson et al, 2011b).
Other short-term respiratory morbidities, includ-
More importantly, the TPR group had signifi- ing respiratory distress syndrome, surfactant
cantly higher rate of composite outcome of mor- administration, and air leak syndrome, were also
tality or oxygen dependence at 36 weeks PMA. similar between devices. However, infants who
However, this finding should be interpreted were resuscitated with a T-piece resuscitator had
with caution because birth weight, which is an a significantly higher rate of either mortality or
important confounder, could not be adjusted oxygen dependence at 36 week post-menstrual
due to the limited number of infants that had age. Further study with an appropriate sample
a composite outcome. Morbidity and mortality size is needed to confirm this outcome.
in preterm infants might also be influenced by
other factors, including necrotizing enterocolitis, REFERENCES
sepsis, and severe intraventricular hemorrhage.
American College of Obstericians and
These factors were not accounted for in this
Gynecologists: Committee on Obstetric
study, because the relatively small sample size
Practice. ACOG Committee Opinion No.
could lead to invalid results and conclusions. The
485: Prevention of early-onset group B
involvement of these factors should be investi-
streptococcal disease in newborns. Obstet
gated in future study with a larger sample size.
Gynecol 2011a; 117: 1019-27.
Our study reflects similar effectiveness be-
ACOG Committee on Obstetric Practice. ACOG
tween T-piece resuscitator and self-inflation bag
Committee Opinion No. 475: antenatal
in a more practical and real-life situation profile.
corticosteroid therapy for fetal maturation.
We did not find any different in either intuba-
Obstet Gynecol 2011b; 117: 422-4.
tion rate or incidence of respiratory morbidities
between the groups. Therefore, the resuscitation American College of Obstetricians and
team can select the PPV device upon availability Gynecologists: Committee on Practice
and user preference. Nevertheless, we realize Bulletins–Obstetrics. ACOG practice bulletin
several limitations of the study. Our sample size no. 127: Management of preterm labor.
is only half of the required number which conse- Obstet Gynecol 2012; 119: 1308-17.
quently undermined the power to detect differ-
Bennett S, Finer NN, Rich W, Vaucher Y. A
ences. This problem has been diluted by a higher
comparison of three neonatal resuscitation
than expected rate of intubation, therefore
devices. Resuscitation 2005; 67: 113-8.
the power of our study may not be very much
disturbed. The other issue is the alternation of Bjorklund LJ, Ingimarsson J, Curstedt T, et al.
types of PPV devices in between the resuscita- Manual ventilation with a few large breaths
tion process when a team leader believed better at birth compromises the therapeutic effect
ventilation can be achieved. In this situation, the of subsequent surfactant replacement in
influence of both types of PPV devices on infant immature lambs. Pediatr Res 1997; 42:
outcomes cannot be separated. Once again, we 348-55.
254 Vol. 48 (Supplement 2) 2017
T-Piece Resuscitator During Birth Resuscitation
Dawson JA, Gerber A, Kamlin CO, Davis PG, O’Donnell CP, Davis PG, Lau R, Dargaville PA,
Morley CJ. Providing PEEP during neonatal Doyle LW, Morley CJ. Neonatal resuscitation
resuscitation: which device is best? J Paediatr 3: manometer use in a model of face mask
Child Health 2011a; 47: 698-703. ventilation. Arch Dis Child Fetal Neonatal Ed
Dawson JA, Schmolzer GM, Kamlin CO, et al. 2005; 90: F397-400.
Oxygenation with T-piece versus self-inflating Oddie S, Wyllie J, Scally A. Use of self-inflating
bag for ventilation of extremely preterm bags for neonatal resuscitation. Resuscitation
infants at birth: a randomized controlled trial. 2005; 67: 109-12.
J Pediatr 2011b; 158: 912-8 e1-2.
Perlman JM, Wyllie J, Kattwinkel J, et al. Part 11:
Finer NN, Rich W, Craft A, Henderson C.
neonatal resuscitation: 2010 international
Comparison of methods of bag and mask
consensus on cardiopulmonary resuscitation
ventilation for neonatal resuscitation.
and emergency cardiovascular care science
Resuscitation 2001; 49: 299-305.
with treatment recommendations. Circulation
Grasso C, Sciacca P, Giacchi V, et al. Effects of
2010; 122: S516-38.
sustained lung inflation, a lung recruitment
maneuver in primary acute respiratory Polin RA, Fox WW, Abman SH. Fetal and
distress syndrome, in respiratory and cerebral neonatal physiology. 4th ed. Philadelphia:
outcomes in preterm infants. Early Hum Dev Saunders Elsevier, 2011.
2015; 91: 71-5. Roehr CC, Kelm M, Proquitte H, Schmalisch G.
Hawkes CP, Oni OA, Dempsey EM, Ryan CA. Equipment and operator training denote
Should the neopuff t-piece resuscitator be manual ventilation performance in neonatal
restricted to frequent users? Acta Paediatr resuscitation. Am J Perinatol 2010; 27: 753-8.
2010; 99: 452-3. Szyld E, Aguilar A, Musante GA, et al. Comparison
Hillman NH, Moss TJ, Kallapur SG, et al. Brief, of devices for newborn ventilation in the
large tidal volume ventilation initiates lung delivery room. J Pediatr 2014; 165: 234-9 e3.
injury and a systemic response in fetal sheep. te Pas AB, Siew M, Wallace MJ, et al. Effect of
Am J Respir Crit Care Med 2007; 176: 575-81. sustained inflation length on establishing
Hoskyns EW, Milner AD, Hopkin IE. A simple functional residual capacity at birth in
method of face mask resuscitation at birth. ventilated premature rabbits. Pediatr Res
Arch Dis Child 1987; 62: 376-8. 2009; 66: 295-300.
John K. Textbook of neonatal resuscitation. 6th
te Pas AB, Walther FJ. A randomized, controlled
ed. Washington DC: Amrican Academy of
trial of delivery-room respiratory management
Pediatrics and American Heart Asscoiation,
in very preterm infants. Pediatrics 2007; 120:
2011.
322-9.
Lista G, Fontana P, Castoldi F, Cavigioli F, Dani C.
Does sustained lung inflation at birth improve Thakur A, Saluja S, Modi M, et al. T-piece or self
outcome of preterm infants at risk for inflating bag for positive pressure ventilation
respiratory distress syndrome? Neonatology during delivery room resuscitation: an RCT.
2011; 99: 45-50. Resuscitation 2015; 90: 21-4.
McHale S, Thomas M, Hayden E, Bergin Wilson MR, Choudhury S, Goddard ME,
K, McCallion N, Molloy EJ. Variation in O’Dea KP, Nicholson AG, Takata M. High
inspiratory time and tidal volume with tidal volume upregulates intrapulmonary
t-piece neonatal resuscitator: association cytokines in an in vivo mouse model of
with operator experience and distraction. ventilator-induced lung injury. J Appl Physiol
Resuscitation 2008; 79: 230-3. (1985) 2003; 95: 1385-93.
Vol. 48 (Supplement 2) 2017 255
You might also like
- Comprehensive Handbook Obstetrics & Gynecology 3rd EdFrom EverandComprehensive Handbook Obstetrics & Gynecology 3rd EdRating: 5 out of 5 stars5/5 (1)
- Medical-Surgical Nursing Knowledge & Skills ChecklistDocument3 pagesMedical-Surgical Nursing Knowledge & Skills Checklistnorthweststaffing100% (1)
- 1233 FullDocument4 pages1233 FullMarielos Livengood de SanabriaNo ratings yet
- Impact of Prophylactic Continuous Positive Airway Pressure On Transient Tachypnea of The Newborn and Neonatal Intensive Care Admission in Newborns Delivered by Elective Cesarean SectionDocument8 pagesImpact of Prophylactic Continuous Positive Airway Pressure On Transient Tachypnea of The Newborn and Neonatal Intensive Care Admission in Newborns Delivered by Elective Cesarean SectionFabiano SilvaNo ratings yet
- Ventilator-Associated Pneumonia in Low Birth Weight Neonates at A Neonatal Intensive Care Unit A Retrospective ObserDocument6 pagesVentilator-Associated Pneumonia in Low Birth Weight Neonates at A Neonatal Intensive Care Unit A Retrospective ObserDevi Arnes SimanjuntakNo ratings yet
- Shimokaze Et Al-2015-Journal of Obstetrics and Gynaecology ResearchDocument8 pagesShimokaze Et Al-2015-Journal of Obstetrics and Gynaecology ResearchMusa LandeNo ratings yet
- Ventilator-Associated Pneumonia in Low Birth Weight Neonates at A Neonatal Intensive Care Unit: A Retrospective Observational StudyDocument6 pagesVentilator-Associated Pneumonia in Low Birth Weight Neonates at A Neonatal Intensive Care Unit: A Retrospective Observational StudyLuize KrulciferNo ratings yet
- ProneDocument8 pagesPronesophiaNo ratings yet
- Simorangkir (2021) - DONEDocument13 pagesSimorangkir (2021) - DONEMaya HammoudNo ratings yet
- Does Antenatal Corticosteroid Therapy Improve Neonatal Outcomes in Late Preterm Birth?Document8 pagesDoes Antenatal Corticosteroid Therapy Improve Neonatal Outcomes in Late Preterm Birth?faikaoesmaniaNo ratings yet
- Obgyn 1Document4 pagesObgyn 1Auzia Tania UtamiNo ratings yet
- Reanimacion NeonatalDocument6 pagesReanimacion NeonatalDaniela AraujoNo ratings yet
- Problem StatementDocument15 pagesProblem StatementhuylimalaNo ratings yet
- DIT SoniyaRDocument4 pagesDIT SoniyaRLaelannie MagpayoNo ratings yet
- BBLR 2Document6 pagesBBLR 2refiNo ratings yet
- Delivery Room Handling of The Newborn: Stephanie Marshall, Asta Maria Lang, Marta Perez and Ola D. SaugstadDocument10 pagesDelivery Room Handling of The Newborn: Stephanie Marshall, Asta Maria Lang, Marta Perez and Ola D. SaugstadRaja SekarNo ratings yet
- 343-Article Text-653-1-10-20190607Document5 pages343-Article Text-653-1-10-20190607Zulkifli FachriyanNo ratings yet
- Research Proposal - SammyDocument24 pagesResearch Proposal - SammyOfosu AugustineNo ratings yet
- Differences in The Swallowing Process of Newborns and HealthyDocument12 pagesDifferences in The Swallowing Process of Newborns and Healthysiramliw3No ratings yet
- The Effects of Premature Infant Oral Motor Intervention (PIOMI) On Oral Feeding of Preterm Infants - A Randomized Clinical TrialDocument8 pagesThe Effects of Premature Infant Oral Motor Intervention (PIOMI) On Oral Feeding of Preterm Infants - A Randomized Clinical TrialAndreas Arie WidiadiaksaNo ratings yet
- Basic EcgDocument19 pagesBasic EcgIrma SihotangNo ratings yet
- Effect of Osteopathic Manipulative Treatment On Gastrointestinal Function and Length of Stay of Preterm Infants: An Exploratory StudyDocument6 pagesEffect of Osteopathic Manipulative Treatment On Gastrointestinal Function and Length of Stay of Preterm Infants: An Exploratory StudySandro PerilloNo ratings yet
- Pi Is 1028455916300389Document5 pagesPi Is 1028455916300389Ana AdamNo ratings yet
- 2015 Neonatal Resuscitation AHADocument19 pages2015 Neonatal Resuscitation AHAJoyceAltamiranoEncisoNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- Circulation 2015 Wyckoff S543 60Document18 pagesCirculation 2015 Wyckoff S543 60Kahfi Rakhmadian KiraNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- 1 s2.0 S1875957222000195 MainDocument7 pages1 s2.0 S1875957222000195 MainElenaNo ratings yet
- Manajemen NyeriDocument8 pagesManajemen Nyeriagung yulisaputraNo ratings yet
- Yoshida 2019Document6 pagesYoshida 2019triska antonyNo ratings yet
- Non Invasive Versus Invasive Respiratory Support in Preterm InfantsDocument25 pagesNon Invasive Versus Invasive Respiratory Support in Preterm InfantshosnameskarNo ratings yet
- Neonatos Guias 2010Document3 pagesNeonatos Guias 2010minessotNo ratings yet
- Journal NicuDocument4 pagesJournal NicuMargaret LlavorNo ratings yet
- Transpyloric FeedingDocument10 pagesTranspyloric FeedingdryogkNo ratings yet
- 33 - 10.1080@14767058.2020.1735339Document8 pages33 - 10.1080@14767058.2020.1735339Rosa PerezNo ratings yet
- Atosiban 2Document7 pagesAtosiban 2Meliana JayasaputraNo ratings yet
- Induction of Labor Using Foley Catheter With Weight Attached Vs Without WeightDocument14 pagesInduction of Labor Using Foley Catheter With Weight Attached Vs Without Weightgrace liwantoNo ratings yet
- Premedication With Fentanyl For Less Invasive SurfDocument19 pagesPremedication With Fentanyl For Less Invasive SurfRochnald PigaiNo ratings yet
- Comparison of Devices For Newborn Ventilation in The Delivery RoomDocument9 pagesComparison of Devices For Newborn Ventilation in The Delivery RoomRaja SekarNo ratings yet
- Trends in Use of Neonatal CPAP - A Population-Based StudyDocument7 pagesTrends in Use of Neonatal CPAP - A Population-Based StudyGabrielaNo ratings yet
- Early Total Enteral Feeding in Stable Very Low Birth Weight Infants: A Before and After StudyDocument7 pagesEarly Total Enteral Feeding in Stable Very Low Birth Weight Infants: A Before and After StudySupriya M A SuppiNo ratings yet
- Development of A Nursing Care Protocol For Care of Neonates With Esophageal Atresia/ Tracheo - Esophageal FistulaDocument14 pagesDevelopment of A Nursing Care Protocol For Care of Neonates With Esophageal Atresia/ Tracheo - Esophageal FistulaSanket TelangNo ratings yet
- 1 ChestDocument5 pages1 ChestZakiyah Nur HaqqiNo ratings yet
- Providing PEEP During Neonatal Resuscitation: Which Device Is Best?Document6 pagesProviding PEEP During Neonatal Resuscitation: Which Device Is Best?Raja SekarNo ratings yet
- PIIS0002937820311923Document3 pagesPIIS0002937820311923FebbyNo ratings yet
- MD 0000000000012257Document5 pagesMD 0000000000012257Sykat ZamanNo ratings yet
- Fped-08-00250n NBDocument8 pagesFped-08-00250n NBfitriNo ratings yet
- Sorensen 2010Document5 pagesSorensen 2010Anonymous EmbvvI1ct2No ratings yet
- RP 00531Document5 pagesRP 00531Silja ManojNo ratings yet
- Journal Pone 0000192Document5 pagesJournal Pone 0000192TriponiaNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument8 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biologyana pintoNo ratings yet
- Atosiban Improves Implantation and Pregnancy Rates in Patients With Repeated Implantation FailureDocument7 pagesAtosiban Improves Implantation and Pregnancy Rates in Patients With Repeated Implantation FailureLaura LealNo ratings yet
- Oral Plenary I: Study DesignDocument2 pagesOral Plenary I: Study DesignLestari LifaNo ratings yet
- Articulo 2Document7 pagesArticulo 2Christian Yzaguirre AbantoNo ratings yet
- 26-05-2020-1590469891-8-IJANS-10. IJANS - The Effect of Prone Position Versus Supine Position On Oxygen Saturation Among Jordanian PretermDocument6 pages26-05-2020-1590469891-8-IJANS-10. IJANS - The Effect of Prone Position Versus Supine Position On Oxygen Saturation Among Jordanian Pretermiaset123No ratings yet
- Neonatal ResuscitationDocument7 pagesNeonatal ResuscitationJavier López García100% (1)
- Study of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreDocument11 pagesStudy of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1 s2.0 S2352556818300389 MainDocument5 pages1 s2.0 S2352556818300389 Main吴善统No ratings yet
- CalostroDocument12 pagesCalostroluzhelanapaezNo ratings yet
- Thesis ProtocolDocument7 pagesThesis ProtocolhoneyworksNo ratings yet
- Possible Role of Vacuum Systems and Compressed Air Generators in Cross-Infection in The IcuDocument3 pagesPossible Role of Vacuum Systems and Compressed Air Generators in Cross-Infection in The IcuRaja SekarNo ratings yet
- L13Document4 pagesL13Raja SekarNo ratings yet
- Comparison of Devices For Newborn Ventilation in The Delivery RoomDocument9 pagesComparison of Devices For Newborn Ventilation in The Delivery RoomRaja SekarNo ratings yet
- Clinical Risk Management in Newborn and Neonatal ResuscitationDocument17 pagesClinical Risk Management in Newborn and Neonatal ResuscitationRaja SekarNo ratings yet
- Resuscitation of Premature Infants: What Are We Doing Wrong and Can We Do Better?Document7 pagesResuscitation of Premature Infants: What Are We Doing Wrong and Can We Do Better?Raja SekarNo ratings yet
- Case Study MSDocument21 pagesCase Study MSEduard0% (1)
- Version FinalDocument22 pagesVersion Finalsanthiyasandy100% (1)
- Multiple PregnancyDocument55 pagesMultiple PregnancyNathaniel YeriNo ratings yet
- Amy Dhillon Levine, DPM: Education & TrainingDocument3 pagesAmy Dhillon Levine, DPM: Education & TrainingapnipatNo ratings yet
- Handout of Acupuncture PointsDocument105 pagesHandout of Acupuncture PointsAlexander AntonakakisNo ratings yet
- Seminarppt 130325005413 Phpapp02Document18 pagesSeminarppt 130325005413 Phpapp02SAURAV KUMARNo ratings yet
- 3 LIT208RevH BrainPath-Product-Info FINAL 181003Document2 pages3 LIT208RevH BrainPath-Product-Info FINAL 181003Carlos Minino P.No ratings yet
- A History of The Penile Implant To 1974: Sex Med Rev 2016 4:285 E293 285Document9 pagesA History of The Penile Implant To 1974: Sex Med Rev 2016 4:285 E293 285Anonymous S0MyRHNo ratings yet
- SO MaterialDocument112 pagesSO MaterialkinkinNo ratings yet
- Med Surg Nursing Cheat Sheets 76 Cheat Sheets For Nursing Students Nodrm PDFDocument101 pagesMed Surg Nursing Cheat Sheets 76 Cheat Sheets For Nursing Students Nodrm PDFEya BaldostamonNo ratings yet
- Stages of Labor and DeliveryDocument9 pagesStages of Labor and Deliverykhrysty1506No ratings yet
- Science F3 Chap 2-Blood Circulation and TransportDocument34 pagesScience F3 Chap 2-Blood Circulation and TransportRebecca Choong Xin Hui93% (15)
- DR Case Presentation FinalDocument35 pagesDR Case Presentation FinalLord Allen B. GomezNo ratings yet
- Undescended Testicle PathwayDocument8 pagesUndescended Testicle PathwayJessa MaeNo ratings yet
- Distal Shoes Space MaintainerDocument5 pagesDistal Shoes Space MaintainerEduardo FernandezNo ratings yet
- The Vein BookDocument568 pagesThe Vein Booknazar shekhoNo ratings yet
- Laparoscopy AppendectomyDocument3 pagesLaparoscopy AppendectomyRoxiutaLNo ratings yet
- L&D PDFDocument2 pagesL&D PDFChandace JanineNo ratings yet
- Management of Forgen Body InhalationDocument31 pagesManagement of Forgen Body Inhalationmonir61No ratings yet
- Lohchab Nursing Home SlipDocument3 pagesLohchab Nursing Home SlipsalimNo ratings yet
- Central Venous Pressure Monitoring ManualDocument6 pagesCentral Venous Pressure Monitoring ManualCristina L. JaysonNo ratings yet
- Vascular Surgery MiamiDocument5 pagesVascular Surgery MiamiwilberespinosarnNo ratings yet
- Bandaging and SplintingDocument88 pagesBandaging and Splintinggbsreg gbsregNo ratings yet
- Radiologi EndokrinDocument76 pagesRadiologi EndokrinAndi9993100% (1)
- Single-Visit Endodontics: A ReviewDocument6 pagesSingle-Visit Endodontics: A ReviewPrawira SetiadarmaNo ratings yet
- Warming Up: 1. Discuss in Your Class: (Write Your Own Answers. Points Only Given For Reference)Document8 pagesWarming Up: 1. Discuss in Your Class: (Write Your Own Answers. Points Only Given For Reference)FOXTROTNo ratings yet
- Explor LaparotomyDocument14 pagesExplor LaparotomyGracia NievesNo ratings yet
- CDH and Pulmonary HypertensionDocument6 pagesCDH and Pulmonary HypertensionStollery SandboxNo ratings yet
- Cardiovascular System - ReviewerDocument11 pagesCardiovascular System - ReviewerEva Marie GaaNo ratings yet