Professional Documents
Culture Documents
0.05vs 0.1
0.05vs 0.1
Uploaded by
nivethitaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
0.05vs 0.1
0.05vs 0.1
Uploaded by
nivethitaCopyright:
Available Formats
Insulin infused at 0.05 versus 0.
1 units/kg/hr in children admitted
to intensive care with diabetic ketoacidosis*
Said Al Hanshi, MD, MRCPCH; Frank Shann, MD, FRACP, FJFICM
Objective: To compare the effects of infusing insulin at 0.05 received 0.05 units/kg/hr of insulin were younger (median age, 25
units/kg/hr rather than 0.1 units/kg/hr in children admitted to the mos vs. 62 mos, p ⴝ .024) and had a more gradual reduction in
intensive care unit with diabetic ketoacidosis. the effective plasma osmolality over the first 12 hrs (p < .0005);
Design: A retrospective observational study. this was because plasma glucose decreased more slowly (p ⴝ
Setting: A tertiary pediatric intensive care unit. .004) and plasma sodium increased faster (p < .0005). Both
Patients: All children with diabetic ketoacidosis admitted dur- groups had a satisfactory improvement in acidosis and ketosis,
ing the 6-yr period from 2000 to 2005. and they had a similar length of stay in the intensive care unit.
Interventions: None. Conclusions: Further studies are needed to evaluate the role of
Measurements and Main Results: The effective plasma osmo- using 0.05 units/kg/hr of insulin to treat children with diabetic
lality (plasma glucose concentration in mmol/L ⴙ twice the ketoacidosis. The smaller dose of insulin may make it easier to lower the
plasma sodium concentration in mmol/L), plasma glucose, effective plasma osmolality gradually and might, therefore, reduce the
plasma sodium, fluid intake, and acid-base status 12 hrs after the risk of cerebral edema. (Pediatr Crit Care Med 2011; 12:137–140)
commencement of the insulin infusion. Compared to the 34 chil- KEY WORDS: brain edema; diabetic ketoacidosis; diabetes mel-
dren who received 0.1 units/kg/hr of insulin, the 33 children who litus; insulin
C erebral edema is the major concentration (1). Several factors may management of diabetic ketoacidosis rec-
cause of morbidity and mor- prevent an increase in the plasma sodium ommend the infusion of 0.1 units/kg/hr
tality in children with diabetic concentration: the use of intravenous flu- of insulin from 1 to 2 hrs after the start of
ketoacidosis (1– 4). There is ids with a sodium concentration lower fluid replacement therapy (10). However,
increasing evidence that a rapid de- than the patient’s plasma sodium concen- only two papers are cited in support of
crease in the effective plasma osmolality tration; the infusion of enough fluid to this dose of insulin: the first paper stud-
may increase the risk of cerebral edema cause expansion of the extracellular fluid ied only insulin doses of 0.1 units/kg/hr
(1, 5– 8). The effective plasma osmolality volume, which may lead to enhanced re- and 1.0 units/kg/hr in 32 children with
is equal to the plasma glucose concentra- nal excretion of sodium and “desalina- diabetic ketoacidosis (11); and the second
tion in mmol/L plus twice the plasma tion”; absorption from the bowel of large gave 0.01 units/kg/hr, 0.1 units/kg/hr,
sodium concentration in mmol/L (5, 9), volumes of hypotonic fluid ingested be- and 1.0 units/kg/hr for only 60 mins to
so the rate of change of the effective os- fore admission to hospital; and a high six insulin-dependent adult volunteers
molality will be determined by the dose of insulin (1). who had been given dexamethasone (12).
amounts of glucose, insulin, sodium, and Much of the discussion about how to Schade and Eaton (12) in the second pa-
water administered. preserve the effective plasma osmolality per stated explicitly that their results “are
If the effective osmolality is to fall in diabetic ketoacidosis has been about not directly applicable to insulin therapy
slowly during the treatment of diabetic sodium and water therapy, rather than for spontaneous diabetic ketoacidosis.”
ketoacidosis, the plasma sodium concen- the changes in plasma glucose (1, 5– 8). Neither of these studies provides evidence
tration has to rise by nearly 1 mmol/L for
This is understandable, because a 1 that 0.1 units/kg/hr is superior to lower
every 2 mmol/L fall in the plasma glucose
mmol/L change in plasma sodium con- doses of insulin for the treatment of dia-
centration has double the effect on osmo- betic ketoacidosis in children. In the sec-
lality of a 1 mmol/L change in plasma ond study (12), an insulin dose of only
*See also p. 217. glucose concentration. However, if the 0.01 units/kg/hr reduced the total plasma
From the Pediatric Intensive Care Unit (SAH), The plasma glucose concentration falls very ketone body concentration by 42% and the
Royal Hospital, Sultanate of Oman; and Intensive Care rapidly, it is difficult to increase the plasma glucose concentration by 8.4% (a
(FS), Royal Children’s Hospital, Melbourne, Victoria,
Australia. plasma sodium concentration quickly rate of 1.6 mmol/L/hr) in just 1 hr.
The authors have not disclosed any potential con- enough to maintain the effective plasma For several years, many of the children
flicts of interest. osmolality. It is, therefore, important to admitted to our intensive care unit (ICU)
For information regarding this article, E-mail: avoid a very rapid fall in the plasma glu- with diabetic ketoacidosis have been
frank.shann@rch.org.au
Copyright © 2011 by the Society of Critical Care cose concentration (2). treated with an infusion of 0.05 units/
Medicine and the World Federation of Pediatric Inten- The International Society for Pediatric kg/hr of insulin, in the hope that this will
sive and Critical Care Societies and Adolescent Diabetes 2006 –2007 Clin- make it easier to achieve a gradual reduc-
DOI: 10.1097/PCC.0b013e3181e2a21b ical Practice Consensus Guidelines on the tion in the effective plasma osmolality.
Pediatr Crit Care Med 2011 Vol. 12, No. 2 137
Approximately half the admissions have Table 1. Biochemistry at the start of treatment and 12 hrs after the commencement of insulin therapy,
been treated with an initial infusion of by dose of insulin: median (interquartile range)
0.05 units/kg/hr of insulin, and half with
Dose of Insulin
0.1 u/kg/hr. This paper describes the ef-
fects of these two regimens in the first 12 0.05 units/kg/hr (n ⫽ 33) 0.1 units/kg/hr (n ⫽ 34)
hrs of treatment.
Effective Osmolality (mOsm/kg)
Start 300 (285,311) 311 (298,327)
12 hrs 295 (284,311) 293 (287,332)
METHODS Glucose (mmol/L)
Start 29 (23,39) 32 (26,68)
A computerized database is used to record 12 hrs 11 (9,17) 14 (8,18)
all admissions to the pediatric ICU at the Royal Sodium (mmol/L)
Start 135 (129,139) 137 (134,140)
Children’s Hospital, Melbourne. In the 6 yrs
12 hrs 140 (138,149) 141 (138,157)
between January 2000 and December 2005, 69 Potassium (mmol/L)
children were admitted with a diagnosis of Start 4.3 (4.0,5.2) 4.0 (3.8,4.7)
diabetic ketoacidosis (plasma glucose of ⬎11 12 hrs 3.6 (3.4,4.0) 3.9 (3.4,4.5)
mmol/L, and an arterial pH of ⬍7.30, or pH
Start 7.03 (6.95,7.16) 7.07 (6.95,7.15)
plasma bicarbonate of ⬍15 mmol/L). The 12 hrs 7.25 (7.21,7.31) 7.28 (7.24,7.32)
medical records of two children were not Base Excess (mmol/L)
available, so 67 children are included in this Start ⫺24 (⫺26,⫺22) ⫺23 (⫺26,⫺19)
review. Children were managed according to 12 hrs ⫺12 (⫺16,⫺11) ⫺12 (⫺14,⫺9)
the section on diabetic ketoacidosis in the Bicarbonate (mmol/L)
Start 5 (4,7) 5 (4,7)
Unit’s book of Pediatric Intensive Care Guide- 12 hrs 13 (10,15) 14 (11,17)
lines (13). After fluid resuscitation using 0.9% PaCO2 (torr)
saline, insulin was given by continuous infu- Start 20 (15,24) 20 (16,25)
sion in 4% albumin with no loading dose, and 12 hrs 27 (22,31) 33 (27,36)
Urine ketones (0 to ⫹⫹⫹)
0.9% saline was used as maintenance fluid
Start 2.9 pluses* 2.8 plusesa
without bicarbonate or citrate. 12 hrs 2.0 pluses* 2.0 plusesa
Each child’s age and weight, and the dose
of insulin and the volume of fluid infused from To convert torr to kPa, multiply by 0.1317.
a
the start of treatment until the completion of Arithmetic mean.
12 hrs of insulin therapy were obtained from
the medical record. The following biochemical
results were obtained from the medical record RESULTS kg (IQR, 12– 45 kg), and stayed in the
and the Hospital’s computerized database: the intensive care unit for a median of 0.92
urine ketone test results; the plasma pH, PCO2 Of the 67 children, 33 were given 0.05 days (IQR, 0.43–1.45 days). The children
and base excess; and the plasma concentration of units/kg/hr of insulin, and 34 were given in the 0.05-units/kg/hr group were
glucose, bicarbonate, sodium, and potassium— 0.1 units/kg/hr of insulin. Four children younger (p ⫽ .024, Student’s t test of the
which were usually measured every 2– 4 hrs up were started on 0.1 units/kg/hr but had logarithm of age).
to the completion of 12 hrs of insulin therapy. the dose reduced to 0.05 units/kg/hr after The biochemical findings at the start
The effective plasma osmolality in mOsm/kg was 6 –12 hrs; they were classified as having of treatment and at the completion of 12
calculated from the plasma glucose concentra- received 0.1 units/kg/hr. Three children hrs of insulin therapy are shown in Table
tion in mmol/L plus twice the plasma sodium were given doses of 0.075– 0.1 units/kg/ 1. The volume of fluid administered and
concentration in mmol/L (5, 9). hr, 0.08 units/kg/hr, and 0.09 units/kg/hr, the change in the plasma glucose, so-
The effect of the dose of insulin on the respectively; they were also classified as dium, and effective osmolality from the
effective osmolality (or glucose or sodium) at having received 0.1 units/kg/hr. One start of treatment until the completion of
12 hrs (the dependent variable) was assessed, child had the dose reduced from 0.05 to 12 hrs of insulin therapy are shown in
using analysis of covariance, with the indepen- 0.03 units/kg/hr, and another had the Table 2. Children who received 0.05
dent variables being the dose of insulin, the dose increased from 0.05 units/kg/hr to units/kg/hr of insulin had a more gradual
initial value of effective osmolality (or glucose 0.1 units/kg/hr after 9 hrs; both were reduction in effective plasma osmolality
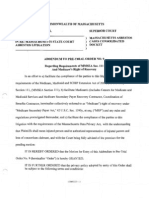
or sodium), and the logarithm of age in classified as having received 0.05 units/ in the first 12 hrs (Table 2 and Fig. 1).
months. The percentage of normal daily fluid kg/hr. Cerebral edema was not detected clini-
intake was calculated from the actual total The 33 children (16 boys) given 0.05 cally in any child, and no child died.
fluid intake up to 12 hrs, divided by the nor- units/kg/hr of insulin had a median age of
mal daily intake for a child of that weight 25 mos (interquartile range [IQR], 14 – 87 DISCUSSION
(0 –10 kg 100 mL/kg, 11–20 kg 1000 mL ⫹ 50 mos, 20 aged ⬍36 mos), a median weight
mL/kg, ⬎20 kg 1500 mL ⫹ 20 mL/kg) (14). of 12 kg (IQR, 9 –25 kg), and stayed in the This study is a retrospective survey of
Stata (StataCorp, College Station, TX) was ICU for a median of 0.91 days (IQR, 0.74 – children admitted to the ICU with dia-
used for statistical analysis. 1.14 days). The 34 children (n ⫽ 15 boys) betic ketoacidosis. By chance, approxi-
The study was approved by the Royal Chil- given 0.1 units/kg/hr of insulin had a mately half the children were treated
dren’s Hospital Ethics and Human Research median age of 62 mos (IQR, 20 –97 mos; with 0.05 units/kg/hr of insulin and half
Committee. 13 aged ⬍36 mos), a median weight of 20 received 0.1 units/kg/hr. The dose was
138 Pediatr Crit Care Med 2011 Vol. 12, No. 2
Table 2. Volume of fluid administered and the change in plasma sodium,glucose and effective dren who received the lower dose of in-
osmolality from the start of treatment until the completion of 12 hrs of insulin therapy, by dose of sulin did not have persistent acidosis or
insulin: median (interquartile range)
persistent ketosis (Table 1).
Insulin 0.05 Insulin 0.1 Adjusted It is very uncommon for a child with
units/kg/hr units/kg/hr p R2 diabetic ketoacidosis to present with cir-
culatory shock caused by hypovolemia
Fluid before intensive care (mL/kg) 20 (19,29) 20 (10,31) .612a (14), but when this does occur, intravas-
Total fluid intake to 12 hr (mL/kg) 75 (68,91) 69 (57,86) .075a cular volume needs to be restored quickly
Percentage of normal daily fluid 90 (79,117) 101 (82,131) .273a
Change in sodium 0–12 hrs (mmol/L) 8 (5,11) 5 (1,17) ⬍.0005b .63b with 0.9% saline. However, it is rarely
Change in glucose 0–12 hrs (mmol/L) ⫺17 (⫺26,⫺12) ⫺21 (⫺52,⫺15) .004b .38b necessary to infuse ⬎7.5–10 mL/kg of
Change in osmolality 0–12 hrs (mOsm/kg) ⫺4 (⫺12,⫹5) ⫺15 (⫺24,⫺6) ⬍.0005b .80b 0.9% saline in the first hour of treatment
a
(15). Most children presenting with dia-
Kruskal-Wallis test; bEffect of insulin dose on the value at 12 hours adjusted for the initial value betic ketoacidosis have adequate tissue
and age using analysis of covariance (see Methods).
perfusion, and cerebral edema is by far
the greatest risk—and it is, therefore,
prudent to correct the hyperglycemia, ac-
idosis, and dehydration slowly over
48 –72 hrs (1, 5– 8).
In addition to osmotic effects, vaso-
genic, metabolic, and inflammatory fac-
tors may be involved in the pathogenesis
of cerebral edema in children with dia-
betic ketoacidosis (1, 3, 16 –18). However,
the evidence (1, 5– 8) suggests that it is
prudent to avoid a rapid fall in the effec-
tive plasma osmolality by ensuring that
the plasma glucose concentration does
not fall too rapidly, and that the reduc-
tion that does occur is offset by a rise in
the plasma sodium. It is interesting that
this recommendation remains controver-
sial (5, 19), when there is general agree-
ment that, when cerebral edema does oc-
cur, it should be treated with measures
that result in a higher effective osmolal-
Figure 1. Change in the effective plasma osmolality in the first 12 hrs of insulin therapy, by age and
dose of insulin in units/kg/hr. Boxes show the interquartile range; whiskers indicate 1.5 times beyond
ity: the administration of mannitol or hy-
the first or third quartile. pertonic saline, and a reduction in the
rate of administration of fluid and insulin
(5, 10, 15).
chosen by the doctors who happened to insulin receiving more fluid during re- Two large case-control studies (2, 20)
be looking after the child, and allocation suscitation and the first 12 hrs in the of children with diabetic ketoacidosis
was not formally randomized; intensive pediatric ICU when this was expressed in concluded that osmolality had no effect
care specialists usually prescribed 0.05 mL per kg, but the trend was reversed on cerebral edema, but they did not study
units/kg/hr of insulin and endocrinolo- when the amount of fluid was expressed the effective osmolality because urea was
gists 0.1 units/kg/hr. The children who as a percentage of the normal daily fluid included in the calculation. Urea passes
received the lower dose were younger intake for the age of the child (Table 2); quickly between extracellular and intra-
(median age, 25 mos vs. 62 mos, p ⫽ neither of these differences was statisti- cellular fluid, and so does not influence
.024), so the analysis was adjusted for cally significant. water shifts in diabetic ketoacidosis (5, 9)
age. However, there may well be other There was a smaller reduction in ef- The U.K. case-control study (2) found
undetected differences, so only very ten- that children given insulin in the first
fective plasma osmolality among the chil-
tative comparisons can be made between hour had an increased risk of cerebral
dren who received only 0.05 units/kg/hr
the outcomes in the two groups. Our ICU edema; these children are likely to have
of insulin (p ⬍ .0005) (Table 2), partly
(13) has published a book of treatment received a higher total dose of insulin in
because of a smaller reduction in plasma the first few hours of treatment.
guidelines that includes a protocol for the
management of diabetic ketoacidosis; pa- glucose (p ⫽ .004) and partly because of Although the standard dose of 0.1
tients in the unit are usually treated in a larger increase in plasma sodium (p ⬍ units/kg/hr of insulin is widely referred to
accordance with the guidelines, so the .0005). Because the comparison was not as “low dose,” it actually achieves high
management of these children is likely to randomized, we cannot be sure that the physiological or low pharmacological
have been fairly consistent. smaller reduction in effective osmolality concentrations of insulin (100 –200 U/
There was a trend toward children was due to the lower dose of insulin. mL) with complete inhibition of lipolysis
who were treated with 0.05 units/kg/hr of However, the study does show that chil- and ketogenesis, complete suppression of
Pediatr Crit Care Med 2011 Vol. 12, No. 2 139
hepatic glucose production, and near- al: Mechanism of cerebral edema in children need for water in parenteral fluid therapy.
maximal stimulation of tissue glucose with diabetic ketoacidosis. J Pediatr 2004; Pediatrics 1957; 19:823– 832
uptake - except in an occasional patient 145:164 –171 15. Bohn D, Daneman D: Diabetic ketoacidosis
4. Lawrence SE, Cummings EA, Gaboury I, et and cerebral edema. Curr Opin Pediatr 2002;
with severe insulin resistance that per-
al: Population-based study of incidence and 14:287–291
sists despite the correction of hypovolae-
risk factors for cerebral edema in pediatric 16. Cameron FJ, Kean MJ, Wellard RM, et al:
mia (11, 21). Insights into the acute cerebral metabolic
diabetic ketoacidosis. J Pediatr 2005; 146:
A recent observational study sug- 688 – 692 changes associated with childhood diabetes.
gested that 0.05 units/kg/hr of insulin 5. Rosenbloom AL: Comment on: Treatment of Diabet Med 2005; 22:648 – 653
was as effective as 0.1 units/kg/hr in the diabetic ketoacidosis and the risk of cerebral 17. Toledo JD, Modesto V, Peinador M, et al:
treatment of 93 episodes of diabetic keto- edema. J Pediatr 2007; 150:467– 473. J Pedi- Sodium concentration in rehydration fluids
acidosis in children (22), and an earlier atr 2008; 152:146 –147; author reply, for children with ketoacidotic diabetes: Ef-
study found that a median dose of 0.045 147–149 fect on serum sodium concentration. J Pedi-
(range 0.02– 0.1) units/kg/hr of insulin 6. Carlotti APCP, Bohn D, Halperin ML: Impor- atr 2009; 154:895–900
18. Hoffman WH, Stamatovic SM, Andjelkovic
normalized blood hydroxybutyrate levels tance of timing of risk factors for cerebral
oedema during therapy for diabetic ketoaci- AV: Inflammatory mediators and blood brain
in 35 episodes of diabetic ketoacidosis in
dosis. Arch Dis Child 2003; 88:170 –173 barrier disruption in fatal brain edema of
children (23). These papers, and the re- diabetic ketoacidosis. Brain Res 2009; 1254:
sults of our study, suggest that it may be 7. Harris GD, Fiordalisi I, Yu C: Maintaining
138 –148
safe to treat most children who have di- normal intracranial pressure in a rabbit
19. Rosenbloom AL: Treatment of diabetic keto-
model during treatment of severe diabetic
abetic ketoacidosis with an infusion of acidosis and the risk of cerebral edema. J Pe-
ketoacidemia. Life Sci 1996; 59:1695–1702
0.05 units/kg/hr of insulin, and that even diatr 2008; 152:146 –147; author reply,
8. Harris GD, Fiordalisi I, Harris WL, et al:
lower doses may be optimal in some cir- Minimizing the risk of brain herniation dur-
147–149
cumstances. The use of doses of insu- 20. Glaser N, Barnett P, McCaslin I, et al: Risk
ing treatment of diabetic ketoacidemia: A
lin ⬍0.1 units/kg/hr may make it easier factors for cerebral edema in children with
retrospective and prospective study. J Pediatr
diabetic ketoacidosis. The Pediatric Emer-
to achieve a very gradual reduction in the 1990; 117:22–31
gency Medicine Collaborative Research Com-
effective plasma osmolality in children 9. Oster JR, Singer I: Hyponatremia, hyposmo-
mittee of the American Academy of Pediat-
with diabetic ketoacidosis, and this might lality, and hypotonicity: tables and fables. rics. N Engl J Med 2001; 344:264 –269
reduce the risk of cerebral oedema. Fur- Arch Intern Med 1999; 159:333–336 21. DeFronzo R, Matsuda M, Barrett E: Diabetic
ther studies are needed to evaluate this 10. Wolfsdorf J, Craig ME, Daneman D, et al: ketoacidosis: A combined metabolic-nephro-
possibility. Diabetic ketoacidosis. Pediatr Diabetes 2007; logic approach to therapy. Diabetes Rev
8:28 – 43 1994; 2:209 –238
11. Kitabchi AE: Low-dose insulin therapy in di- 22. Puttha R, Cooke D, Subbarayan A, et al: Low
REFERENCES abetic ketoacidosis: Fact or fiction? Diabetes dose (0.05 units/kg/h) is comparable with
1. Hoorn EJ, Carlotti APCP, Costa LAA, et al: Metab Rev 1989; 5:337–363 standard dose (0.1 units/kg/h) intravenous
Preventing a drop in effective plasma osmo- 12. Schade DS, Eaton RP: Dose response to in- insulin infusion for the initial treatment of
lality to minimize the likelihood of cerebral sulin in man: differential effects on glucose diabetic ketoacidosis in children with type 1
edema during treatment of children with di- and ketone body regulation. J Clin Endocri- diabetes—an observational study. Pediatr Di-
abetic ketoacidosis. J Pediatr 2007; 150: nol Metab 1977; 44:1038 –1053 abetes 2010; 11:12–17
467– 473 13. Shann F, Henning R, Shekerdemian L, et al: 23. Noyes KJ, Crofton P, Bath LE, et al: Hydroxy-
2. Edge JA, Jakes RW, Roy Y, et al: The UK Paediatric Intensive Care Guidelines. Third butyrate near-patient testing to evaluate a
case-control study of cerebral oedema com- Edition. Melbourne, Collective; 2008. Avail- new end-point for intravenous insulin ther-
plicating diabetic ketoacidosis in children. able at www.drugdoses.net/iPhone/. Accessed apy in the treatment of diabetic ketoacidosis
Diabetologia 2006; 49:2002–2009 May 8, 2010 in children. Pediatr Diabetes 2007;
3. Glaser NS, Wootton-Gorges SL, Marcin JP, et 14. Holliday MA, Segar WE: The maintenance 8:150 –156
140 Pediatr Crit Care Med 2011 Vol. 12, No. 2
You might also like
- Guia Ispad 2022 Cetoacidosis Diabetica y Estadi HiperosmolarDocument22 pagesGuia Ispad 2022 Cetoacidosis Diabetica y Estadi HiperosmolarElizabeth Cross50% (2)
- 2022 ISPAD Clinical Practice Consensus Guidelines 2022Document70 pages2022 ISPAD Clinical Practice Consensus Guidelines 2022WenSarmientoBNo ratings yet
- High Dose Vs Low DoseDocument6 pagesHigh Dose Vs Low DosenivethitaNo ratings yet
- Jurnal 1Document7 pagesJurnal 1Jonathan FebiantoNo ratings yet
- Improving Management of Diabetic Ketoacidosis in Children: 2001 108 735-740 Eric I. Felner and Perrin C. WhiteDocument8 pagesImproving Management of Diabetic Ketoacidosis in Children: 2001 108 735-740 Eric I. Felner and Perrin C. Whiterien2903No ratings yet
- Amj-Hiponatremia Corregida Por Hiperglicemia-1999Document5 pagesAmj-Hiponatremia Corregida Por Hiperglicemia-1999Mayra Alejandra Prada SerranoNo ratings yet
- Sodium Bicarbonate: Brand Names Medication Error PotentialDocument2 pagesSodium Bicarbonate: Brand Names Medication Error PotentialMohammedNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults Treatment - UpToDateDocument20 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults Treatment - UpToDateSteffNo ratings yet
- Crystalloid For The Management of Burn ShockDocument18 pagesCrystalloid For The Management of Burn ShockTahir S.MNo ratings yet
- DM 22 Part 2 FFFFFDocument10 pagesDM 22 Part 2 FFFFFalhussaintariqNo ratings yet
- 10 3390@nano10102005Document10 pages10 3390@nano10102005bm rdNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentDocument35 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentyorghiLNo ratings yet
- 4-Efficacy of Alpha-Lipoic Acid Against Diabetic Cataract in Rat.Document4 pages4-Efficacy of Alpha-Lipoic Acid Against Diabetic Cataract in Rat.Anni MuharomahNo ratings yet
- Treatment of Diabetic Ketoacidosis With Subcutaneous Insulin AspartDocument6 pagesTreatment of Diabetic Ketoacidosis With Subcutaneous Insulin AspartAiko Cheryl SalsabilaNo ratings yet
- Gilang, 1 FitriDocument8 pagesGilang, 1 FitriVeren PattipeilohyNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults TreatmentDocument25 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults TreatmentGabriel MarçalNo ratings yet
- 1 Insulin Infusion Responses inDocument6 pages1 Insulin Infusion Responses inPedro Henrique SoaresNo ratings yet
- Cetoacidosis MetabolicaDocument36 pagesCetoacidosis MetabolicaHector ArandaNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults - Treatment - UpToDateDocument36 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults - Treatment - UpToDateHiKa SaGoNo ratings yet
- Bolus Vs No BolusDocument5 pagesBolus Vs No BolusnivethitaNo ratings yet
- Reduced Versus Conventional Dose Insulin For Hyperkalemia TreatmentDocument5 pagesReduced Versus Conventional Dose Insulin For Hyperkalemia TreatmentvictorNo ratings yet
- Noninsulin-Dependent Diabetes: Effects of Insulin Peripheral Splanchnic Glucose Metabolism in 11)Document7 pagesNoninsulin-Dependent Diabetes: Effects of Insulin Peripheral Splanchnic Glucose Metabolism in 11)agiekNo ratings yet
- 16 Nanoglod InsulinDocument6 pages16 Nanoglod InsulinM. Imran QadirNo ratings yet
- 10 Glycemic Control in Perioperative PeriodDocument5 pages10 Glycemic Control in Perioperative PeriodAna-Maria CroitoruNo ratings yet
- DKACalculatorDocument1 pageDKACalculatorRitch BassNo ratings yet
- DKA and HHS The Washington Manual of Critical CareDocument6 pagesDKA and HHS The Washington Manual of Critical Careمحمد عقيلي100% (1)
- Insulin Pump Therapy in Children and Adolescents - Improvements in Key Parameters of Diabetes Management Including Quality of LifeDocument5 pagesInsulin Pump Therapy in Children and Adolescents - Improvements in Key Parameters of Diabetes Management Including Quality of Lifeasdv eqdNo ratings yet
- Diabetes 3Document7 pagesDiabetes 3JimmyNo ratings yet
- Approach To Hypercalcemia - EndotextDocument40 pagesApproach To Hypercalcemia - EndotextMelisa RieloNo ratings yet
- AerobicDocument7 pagesAerobicMayra PereiraNo ratings yet
- Objective: Methods: Results: Conclusions:: What's Known On This SubjectDocument12 pagesObjective: Methods: Results: Conclusions:: What's Known On This SubjectAnonymous AzkHFgubueNo ratings yet
- Post Cancer Dialysis Linked in To Post 34Document36 pagesPost Cancer Dialysis Linked in To Post 34sarah0shawarNo ratings yet
- Pediatric DiabeticDocument9 pagesPediatric Diabeticperla islasNo ratings yet
- Use of Conivaptan To Allow Aggressive Hydration To Prevent Tumor Lysis Syndrome in A Pediatric Patient With Large-Cell Lymphoma and SIADHDocument5 pagesUse of Conivaptan To Allow Aggressive Hydration To Prevent Tumor Lysis Syndrome in A Pediatric Patient With Large-Cell Lymphoma and SIADHmaryNo ratings yet
- Fluids and Electrolytes - PaediatricsDocument52 pagesFluids and Electrolytes - PaediatricsZweNo ratings yet
- Oral Nanotherapeutic Formulation of Insulin With Reduced Episodes of HypoglycaemiaDocument32 pagesOral Nanotherapeutic Formulation of Insulin With Reduced Episodes of Hypoglycaemia1584422dNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: Treatment - UpToDateDocument23 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: Treatment - UpToDateAlex KuliaNo ratings yet
- Pediatric PharmacotherapyDocument4 pagesPediatric Pharmacotherapyvk89.naharNo ratings yet
- A Case Report of Hyperosmolar Hyperglycemic StateDocument1 pageA Case Report of Hyperosmolar Hyperglycemic StateHareesh ChanderNo ratings yet
- Chapter 8 Hyperosmolar Therapy.9Document6 pagesChapter 8 Hyperosmolar Therapy.9Benjamin PeregrinaNo ratings yet
- Neonatal Convulsions Treated With Continuous Intravenous Infusion of DiazepamDocument8 pagesNeonatal Convulsions Treated With Continuous Intravenous Infusion of DiazepamAhmed KassemNo ratings yet
- Diabetic Medicine - 2022 - Mustafa - Management of Hyperosmolar Hyperglycaemic State HHS in Adults An Updated GuidelineDocument12 pagesDiabetic Medicine - 2022 - Mustafa - Management of Hyperosmolar Hyperglycaemic State HHS in Adults An Updated GuidelineGiancarlo SanteNo ratings yet
- Dka CalculatorDocument1 pageDka CalculatordelfiaNo ratings yet
- Diabetic Ketoacidosis PathwayDocument22 pagesDiabetic Ketoacidosis PathwaySri Nath100% (1)
- 1-A Mother Calls You About Her 8 Years Old Son, Known Case of DM-1 Fell Comatose - She Is Not Sure If He Took The Night & Morning Dose of Insulin. You Will Advice Her ToDocument4 pages1-A Mother Calls You About Her 8 Years Old Son, Known Case of DM-1 Fell Comatose - She Is Not Sure If He Took The Night & Morning Dose of Insulin. You Will Advice Her Tomahi_elsemary7011No ratings yet
- Guidelines For The Management of Patients With Hyperglycaemia or Diabetes and Suspected Acute Coronary SyndromesDocument4 pagesGuidelines For The Management of Patients With Hyperglycaemia or Diabetes and Suspected Acute Coronary SyndromesRebecca ChenNo ratings yet
- Neonatal DiabetesDocument5 pagesNeonatal DiabetesSitaNo ratings yet
- AntibioticsDocument13 pagesAntibioticsVjfsyuiNo ratings yet
- KETOPROFEN-ketoprofen Capsule, Extended Release Mylan Pharmaceuticals IncDocument29 pagesKETOPROFEN-ketoprofen Capsule, Extended Release Mylan Pharmaceuticals IncBobeico TatianaNo ratings yet
- Guia 13481Document22 pagesGuia 13481CarmenNo ratings yet
- SPEG DFT Handbook v1.0Document25 pagesSPEG DFT Handbook v1.0bassam alharaziNo ratings yet
- Insulin Degludec - Pharmacokinetics in Patients With Renal ImpairmentDocument9 pagesInsulin Degludec - Pharmacokinetics in Patients With Renal ImpairmentThúy Trang PhanNo ratings yet
- Plasma and Salivary Glucose in Diabetics Attending Tertiary Hospital in Maiduguri, Northeastern NigeriaDocument3 pagesPlasma and Salivary Glucose in Diabetics Attending Tertiary Hospital in Maiduguri, Northeastern NigeriaChiranjeevi Kumar EndukuruNo ratings yet
- Antihyperglycemic Effect of Catalpol in Streptozotocin-Induced Diabetic RatsDocument3 pagesAntihyperglycemic Effect of Catalpol in Streptozotocin-Induced Diabetic RatsGokuNo ratings yet
- ISPAD Clinical Practice Consensus Guidelines 2018: Exercise in Children and Adolescents With DiabetesDocument22 pagesISPAD Clinical Practice Consensus Guidelines 2018: Exercise in Children and Adolescents With Diabetesdesak indryNo ratings yet
- Revised DKA 2015 PDFDocument6 pagesRevised DKA 2015 PDFDr AhmedNo ratings yet
- Manejo de Coma Hipermosmolar HHODocument12 pagesManejo de Coma Hipermosmolar HHOCristian Daniel Espinoza ValdezNo ratings yet
- Ch15 Cyclosporine.Document8 pagesCh15 Cyclosporine.tiba.qasem2000No ratings yet
- Diabetic Ketoacidosis in Children: Diagnosis and Management: Rasika GunapalaDocument10 pagesDiabetic Ketoacidosis in Children: Diagnosis and Management: Rasika GunapalaHoney LaxNo ratings yet
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?From EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?No ratings yet
- Bolus Dose of Insulin 3Document3 pagesBolus Dose of Insulin 3nivethitaNo ratings yet
- PatientCareProcess PDFDocument6 pagesPatientCareProcess PDFnivethitaNo ratings yet
- Liposomes - : A Novel Drug Delivery SystemDocument20 pagesLiposomes - : A Novel Drug Delivery Systemnivethita100% (2)
- Hypertension: Definition and Classification of HypertensionDocument13 pagesHypertension: Definition and Classification of HypertensionnivethitaNo ratings yet
- MIL-I-17563C - Impregnation StdsDocument18 pagesMIL-I-17563C - Impregnation StdsMohanrajMJNo ratings yet
- Orthopaedic Study Guide 2014Document126 pagesOrthopaedic Study Guide 2014Yip Kar Jun100% (1)
- ERBEJETDocument8 pagesERBEJETHossain TanjilaaNo ratings yet
- Analette Manual Service Rev. D 2-6-08Document149 pagesAnalette Manual Service Rev. D 2-6-08RosanaCriolloNo ratings yet
- Case PresentationDocument12 pagesCase PresentationJude Remso LabajoNo ratings yet
- Pre-Test in Science 6: M.S. Garcia Elementary SchoolDocument3 pagesPre-Test in Science 6: M.S. Garcia Elementary SchoolAnepsu HohoNo ratings yet
- Insurance Loss DigestDocument12 pagesInsurance Loss DigestRyan AcostaNo ratings yet
- AssignmentDocument12 pagesAssignmentShubham Jain ModiNo ratings yet
- Tecan Sunrise Absorbance Reader Analyser - User ManualDocument74 pagesTecan Sunrise Absorbance Reader Analyser - User Manualomer oartbNo ratings yet
- CEM1008F Applied Solution Chemistry Part 1 2021Document29 pagesCEM1008F Applied Solution Chemistry Part 1 2021Simlindile NgobelaNo ratings yet
- Corsica-4-East v1 m56577569830517767 PDFDocument9 pagesCorsica-4-East v1 m56577569830517767 PDFxavi-697360No ratings yet
- Nameplate PDFDocument8 pagesNameplate PDFobida adailehNo ratings yet
- Reflection Paper On Inorganic ChemistryDocument4 pagesReflection Paper On Inorganic ChemistryRachelle Joy VerzonNo ratings yet
- Anxiety DisordersDocument10 pagesAnxiety DisordersAhmed AntarNo ratings yet
- Westcott 2013Document13 pagesWestcott 2013Jose ManuelNo ratings yet
- Mass. Proposed AddendumsDocument25 pagesMass. Proposed AddendumsKirk HartleyNo ratings yet
- Debate Speech of First SpeakerDocument3 pagesDebate Speech of First SpeakerDixie DumagpiNo ratings yet
- c7 Manual Rbau A5 Pp33440 Fa PDFDocument8 pagesc7 Manual Rbau A5 Pp33440 Fa PDFae00505No ratings yet
- Growth Evaluation and Meat Assessment of Native Pig in Romblon Province, PhilippinesDocument7 pagesGrowth Evaluation and Meat Assessment of Native Pig in Romblon Province, PhilippinesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- All About StarDocument9 pagesAll About StarRukanuzzaman RaselNo ratings yet
- E Mannual Temperate Fruits 1Document44 pagesE Mannual Temperate Fruits 1gamerrr.mahiNo ratings yet
- Science Journalism ReviewerDocument15 pagesScience Journalism ReviewerHiyami ChanNo ratings yet
- Improving Fast-Food Restaurants' Method of Operation: Automated Drive-Through Ordering SystemDocument12 pagesImproving Fast-Food Restaurants' Method of Operation: Automated Drive-Through Ordering SystemAllin John FranciscoNo ratings yet
- Family Life Group 9Document32 pagesFamily Life Group 9Quỳnh AngNo ratings yet
- Nutri QuizDocument26 pagesNutri QuizChona Candace Christian AndalNo ratings yet
- Consol P 200heDocument2 pagesConsol P 200heimmanuel lumbantobingNo ratings yet
- Gen 017 - Sas Lesson #4Document5 pagesGen 017 - Sas Lesson #4ABM - Villanueva, Jaimee Lyn C.No ratings yet
- Interactive Schematic: This Document Is Best Viewed at A Screen Resolution of 1024 X 768Document13 pagesInteractive Schematic: This Document Is Best Viewed at A Screen Resolution of 1024 X 768maquinariakypcon100% (2)
- Gate 2000 CyDocument9 pagesGate 2000 CyYocobSamandrewsNo ratings yet
- Fresh and Simple PDFDocument3 pagesFresh and Simple PDFthivashnee padayacheeNo ratings yet