Professional Documents
Culture Documents
(19330715 - Journal of Neurosurgery - Pediatrics) Selective Dorsal Rhizotomy - An Illustrated Review of Operative Techniques
(19330715 - Journal of Neurosurgery - Pediatrics) Selective Dorsal Rhizotomy - An Illustrated Review of Operative Techniques
Uploaded by
clinica vet ensenadaCopyright:
Available Formats
You might also like
- Computer System Validation Risk Assessment ToolDocument3 pagesComputer System Validation Risk Assessment Toolcpkakope100% (1)
- The Woman Speaks To The Man Who Has Employed Her SonDocument3 pagesThe Woman Speaks To The Man Who Has Employed Her SonSerena SulawammotNo ratings yet
- Hydraulic Axial Piston Eaton Vickers PVB Pump: - Basic CharacteristicsDocument13 pagesHydraulic Axial Piston Eaton Vickers PVB Pump: - Basic Characteristicsjose alberto olvera gomezNo ratings yet
- Dorsal RhizotomyDocument13 pagesDorsal RhizotomyAiman MaidanNo ratings yet
- Fnhum 16 778347Document5 pagesFnhum 16 778347Josue GarciaNo ratings yet
- Abat F. 2019. Comparison US Guided vs. Blind Interventions Supraspinatus TendinopathyDocument10 pagesAbat F. 2019. Comparison US Guided vs. Blind Interventions Supraspinatus TendinopathyJavier MartinNo ratings yet
- The Evolution of Selective Dorsal Rhizotomy For The Management of SpasticityDocument6 pagesThe Evolution of Selective Dorsal Rhizotomy For The Management of SpasticityJessica MaiaNo ratings yet
- Understanding Carpal Tunnel Syndrome.4Document8 pagesUnderstanding Carpal Tunnel Syndrome.4ayu permata dewiNo ratings yet
- Microsurgical Resection of Vestibular SchwznomaDocument2 pagesMicrosurgical Resection of Vestibular SchwznomaWilson Quispe AlanocaNo ratings yet
- Journal of Hand Therapy: Scienti Fic/clinical ArticleDocument7 pagesJournal of Hand Therapy: Scienti Fic/clinical ArticleDaniel GuevaraNo ratings yet
- Deland 2005Document10 pagesDeland 2005DavidNo ratings yet
- Postoperative Spinal CT: What The Radiologist Needs To KnowDocument22 pagesPostoperative Spinal CT: What The Radiologist Needs To KnowMauricio RuizNo ratings yet
- Fneur 14 1138661Document2 pagesFneur 14 1138661ChadiIbrahimNo ratings yet
- Clinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoDocument5 pagesClinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoSerque777No ratings yet
- Clinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoDocument5 pagesClinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoSerque777No ratings yet
- Quantitative Anatomical Comparison of Anterior, Anterolateral and Lateral, Microsurgical and Endoscopic Approaches To The Middle Cranial FossaDocument49 pagesQuantitative Anatomical Comparison of Anterior, Anterolateral and Lateral, Microsurgical and Endoscopic Approaches To The Middle Cranial FossaAndrés BotelloNo ratings yet
- Ask Us : Readers' ForumDocument1 pageAsk Us : Readers' ForumakNo ratings yet
- Radiol 2291020222Document10 pagesRadiol 2291020222javiervuNo ratings yet
- Evolution of The Surgical Management of Cauda Equina SyndromeDocument13 pagesEvolution of The Surgical Management of Cauda Equina SyndromeAtul JainNo ratings yet
- 1 s2.0 S1878875018300159 MainDocument9 pages1 s2.0 S1878875018300159 MainAlexandreNo ratings yet
- Connectivity of the Superficial Muscles of the Human Perineum a Diffusion Tensor Imaging-Based Global Tractography StudyDocument10 pagesConnectivity of the Superficial Muscles of the Human Perineum a Diffusion Tensor Imaging-Based Global Tractography Studychaiyadol tantasithNo ratings yet
- Ultrasound of The Hand and Wrist in RheumatologyDocument8 pagesUltrasound of The Hand and Wrist in RheumatologyRaphael SiqueiraNo ratings yet
- Superficial Radial Nerve Compression Due To Fibrom 2019 Acta Orthopaedica EtDocument3 pagesSuperficial Radial Nerve Compression Due To Fibrom 2019 Acta Orthopaedica EtanggiNo ratings yet
- Rodilla Inervación Tran2018 PDFDocument8 pagesRodilla Inervación Tran2018 PDFLore BarreraNo ratings yet
- Anatomical Variation of Sciatic Nerve Course in Saudi Population A Magnetic Resonance Imaging StudyDocument8 pagesAnatomical Variation of Sciatic Nerve Course in Saudi Population A Magnetic Resonance Imaging StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Kerasnoudis 2014Document10 pagesKerasnoudis 2014Laura A M MNo ratings yet
- Singh 2012Document6 pagesSingh 2012NadewdewNo ratings yet
- FNIRS2018 AbstractDocument312 pagesFNIRS2018 AbstractJn5omEghSU0j0FNo ratings yet
- Standard Reference Values For Musculoskeletal - Schmidt Schicke Gromnica-IhleDocument7 pagesStandard Reference Values For Musculoskeletal - Schmidt Schicke Gromnica-IhleFer Hijar FraustoNo ratings yet
- Carpal Tunnel SyndromeDocument28 pagesCarpal Tunnel Syndromems bsNo ratings yet
- Chordoma of The Corpus Callosum: Case Report: Literature SearchDocument7 pagesChordoma of The Corpus Callosum: Case Report: Literature SearchAleksandar DimovskiNo ratings yet
- Beyaz 2016Document7 pagesBeyaz 2016nisannnNo ratings yet
- Ultrasound-Guided Injection For Lacertus SyndromeDocument3 pagesUltrasound-Guided Injection For Lacertus SyndromeAhmed sahliNo ratings yet
- Imaging Anatomy of The Cranial Nerves: December 2015Document22 pagesImaging Anatomy of The Cranial Nerves: December 2015Alejandro VanegasNo ratings yet
- Role of High Resolution Ultrasound in Assessment oDocument16 pagesRole of High Resolution Ultrasound in Assessment oilham Maulana ArifNo ratings yet
- Green 2013Document4 pagesGreen 2013Angel GutierrezNo ratings yet
- MontotenniselbowDocument7 pagesMontotenniselbowPURVA THAKURNo ratings yet
- Literature Review Endoscopic Techniques For Spinal Oncology: A SystematicDocument8 pagesLiterature Review Endoscopic Techniques For Spinal Oncology: A SystematicAhana MukherjeeNo ratings yet
- Weiner 2008Document6 pagesWeiner 2008Indira Ulfa DunandNo ratings yet
- 1 s2.0 S0749806314004009 MainDocument10 pages1 s2.0 S0749806314004009 MainbilourNo ratings yet
- Labiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFDocument13 pagesLabiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFAlexandra DumitracheNo ratings yet
- How Many Joints in The Hands and Wrists Should Included in A Score Radiologic Abnormalities Used To Assess Rheumatoid Arthritis?Document10 pagesHow Many Joints in The Hands and Wrists Should Included in A Score Radiologic Abnormalities Used To Assess Rheumatoid Arthritis?Devi PrilliantiNo ratings yet
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocument9 pagesSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNo ratings yet
- FVVinObGyn 14 17Document13 pagesFVVinObGyn 14 17Carlos Eduardo QueirozNo ratings yet
- Diagnostics 13 01928Document30 pagesDiagnostics 13 01928fahaxa7201No ratings yet
- Techniques in Hand and Amp Upper ExtremiDocument6 pagesTechniques in Hand and Amp Upper ExtremiSotiris PlakoutsisNo ratings yet
- The Roof of The Labyrinthine Facial Nerve Canal and The Geniculate Ganglion Fossa On High-Resolution Computed Tomography - Dehiscence Thickness and PneumatizationDocument11 pagesThe Roof of The Labyrinthine Facial Nerve Canal and The Geniculate Ganglion Fossa On High-Resolution Computed Tomography - Dehiscence Thickness and PneumatizationSa'Deu FondjoNo ratings yet
- Morphology of Cranial Sutures and RadiologicDocument6 pagesMorphology of Cranial Sutures and RadiologicEvans RodrigezNo ratings yet
- Radial Nerve and PIN JSS 2019Document6 pagesRadial Nerve and PIN JSS 2019MercedesNo ratings yet
- Bloqueo Facetario UsgDocument7 pagesBloqueo Facetario UsgManolin KinNo ratings yet
- Results of Surgical TreatmentDocument4 pagesResults of Surgical TreatmentChristine Yohana SianturiNo ratings yet
- Uso de Ultrasonografia para Medial EpycondilitisDocument5 pagesUso de Ultrasonografia para Medial EpycondilitisSantiago BianchiNo ratings yet
- What Should We Be Careful of Ankle Arthroscopy?: or Thopaedic Surger yDocument9 pagesWhat Should We Be Careful of Ankle Arthroscopy?: or Thopaedic Surger yJaysellePuguonTabijeNo ratings yet
- Comparison of The Pharyngeal Airways of PatientsDocument10 pagesComparison of The Pharyngeal Airways of PatientsfriscaNo ratings yet
- Research Article: The Effect of Parkinson's Disease On Patients Undergoing Lumbar Spine SurgeryDocument8 pagesResearch Article: The Effect of Parkinson's Disease On Patients Undergoing Lumbar Spine SurgeryMelanie Arabsky LedgerNo ratings yet
- Mandibular Rest Position and ElectricalDocument6 pagesMandibular Rest Position and ElectricalPaula GuerreroNo ratings yet
- The Veterinary Journal: D.A. Portela, N. Verdier, P.E. OteroDocument12 pagesThe Veterinary Journal: D.A. Portela, N. Verdier, P.E. Oteromouxritsa_83No ratings yet
- Marcuzzo 2019Document12 pagesMarcuzzo 2019QuiLeNo ratings yet
- Nakama 2005Document7 pagesNakama 2005angelica barrazaNo ratings yet
- High Contrast High Resolution Imaging of PosttraumDocument10 pagesHigh Contrast High Resolution Imaging of PosttraumPaulo Ferreira OrtodontiaNo ratings yet
- Comparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisDocument6 pagesComparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisWilliam ChienNo ratings yet
- Advances in Vestibular Schwannoma Microneurosurgery: Improving Results with New TechnologiesFrom EverandAdvances in Vestibular Schwannoma Microneurosurgery: Improving Results with New TechnologiesLuciano MastronardiNo ratings yet
- Planning and Facilities: Building StorageDocument31 pagesPlanning and Facilities: Building Storagequsai migdadiNo ratings yet
- Piping SpecificationDocument5 pagesPiping SpecificationShandi Hasnul FarizalNo ratings yet
- Laboratory Information Management System: Prepared By: Mariela C. Ronquillo, RMTDocument33 pagesLaboratory Information Management System: Prepared By: Mariela C. Ronquillo, RMTRonel RonquilloNo ratings yet
- Product Manual 26361V1 (Revision F) : 505DE Digital Governor For Steam TurbinesDocument198 pagesProduct Manual 26361V1 (Revision F) : 505DE Digital Governor For Steam TurbinesGuilherme Marquezin100% (1)
- Statement of Account: State Bank of IndiaDocument1 pageStatement of Account: State Bank of Indiavishalasharma0% (1)
- Grade 12 LM Physical Science 1 Module4Document21 pagesGrade 12 LM Physical Science 1 Module4ladyheart ۦۦNo ratings yet
- Inorganic Chemistry HomeworkDocument3 pagesInorganic Chemistry HomeworkAlpNo ratings yet
- Use of AI in Medicinal Product Lifecycle 1689684121Document17 pagesUse of AI in Medicinal Product Lifecycle 1689684121vivek rakhaNo ratings yet
- Material HPLCDocument19 pagesMaterial HPLCIsmil ImamaNo ratings yet
- Model: Stored Energy Solutions For A Demanding World: Dimensions MM InchDocument2 pagesModel: Stored Energy Solutions For A Demanding World: Dimensions MM Incheddywidjaya9No ratings yet
- Towncall Rural Bank, Inc.: To Adjust Retirement Fund Based On Retirement Benefit Obligation BalanceDocument1 pageTowncall Rural Bank, Inc.: To Adjust Retirement Fund Based On Retirement Benefit Obligation BalanceJudith CastroNo ratings yet
- This Tongue Is Not My Own Dogtooth and TDocument11 pagesThis Tongue Is Not My Own Dogtooth and TGeorgiana Geo GeoNo ratings yet
- IPC in Family PlanningDocument12 pagesIPC in Family PlanningHari MurtiNo ratings yet
- Case Study On A Highway Project: Environmental Impact AssesmentDocument10 pagesCase Study On A Highway Project: Environmental Impact AssesmentSRUTHI FRANCIS M.Tech Environmental Engineering 2020-2022No ratings yet
- MCN KweenDocument4 pagesMCN KweenAngelo SigueNo ratings yet
- T N M M T N M M: HE EW Essies Anual HE EW Essies AnualDocument8 pagesT N M M T N M M: HE EW Essies Anual HE EW Essies AnualMunna100% (1)
- Compensation Practice Cathy Alonso Strayer University (BUS409008VA016-1174-001) Compensation Management Anthony Jacob April 29, 2017Document8 pagesCompensation Practice Cathy Alonso Strayer University (BUS409008VA016-1174-001) Compensation Management Anthony Jacob April 29, 2017Srestha ChatterjeeNo ratings yet
- Wear Solutions BrochureDocument16 pagesWear Solutions BrochureOkan KalendarNo ratings yet
- Bence Bays Resume July 2015Document2 pagesBence Bays Resume July 2015api-292242662No ratings yet
- 956-0302 Onan DFE Operator's and Parts Manual (4-1977)Document54 pages956-0302 Onan DFE Operator's and Parts Manual (4-1977)appplesNo ratings yet
- Test Bank For The Practice of Statistics in The Life Sciences 4th Edition Brigitte BaldiDocument23 pagesTest Bank For The Practice of Statistics in The Life Sciences 4th Edition Brigitte BaldiDebra Franken100% (31)
- Covalence S1301-M Epoxy Primer: DescriptionDocument4 pagesCovalence S1301-M Epoxy Primer: DescriptionJuan Carlos Contreras CherresNo ratings yet
- Astm C 592Document9 pagesAstm C 592hoseinNo ratings yet
- Discard ManagementDocument9 pagesDiscard ManagementDevvrath SinghNo ratings yet
- Chemistry Project 2021-2022Document19 pagesChemistry Project 2021-2022Rudra SathwaraNo ratings yet
- Taino by The Sea Lunch MenuDocument8 pagesTaino by The Sea Lunch Menuinfo_tainobeach0% (1)
- Capinew Account June13Document7 pagesCapinew Account June13ashwinNo ratings yet
(19330715 - Journal of Neurosurgery - Pediatrics) Selective Dorsal Rhizotomy - An Illustrated Review of Operative Techniques
(19330715 - Journal of Neurosurgery - Pediatrics) Selective Dorsal Rhizotomy - An Illustrated Review of Operative Techniques
Uploaded by
clinica vet ensenadaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(19330715 - Journal of Neurosurgery - Pediatrics) Selective Dorsal Rhizotomy - An Illustrated Review of Operative Techniques
(19330715 - Journal of Neurosurgery - Pediatrics) Selective Dorsal Rhizotomy - An Illustrated Review of Operative Techniques
Uploaded by
clinica vet ensenadaCopyright:
Available Formats
LITERATURE REVIEW
J Neurosurg Pediatr 25:540–547, 2020
Selective dorsal rhizotomy: an illustrated review of
operative techniques
Nebras M. Warsi, MD, CM,1,2 Jignesh Tailor, FRCS(SN), PhD,2 Ian C. Coulter, FRCS(SN), MSc,2
Husain Shakil, MD, MSc,1 Adriana Workewych, BSc,3 Renée Haldenby, MSc(PT),4
Sara Breitbart, MSc,2 Samuel Strantzas, MSc,2 Michael Vandenberk, MSc,2
Michael C. Dewan, MD, MSCI,2 and George M. Ibrahim, MD, PhD1,2
1
Division of Neurosurgery, Department of Surgery, University of Toronto; 2Division of Neurosurgery, Hospital for Sick Children;
3
Faculty of Medicine and 4Department of Pediatrics, University of Toronto, Ontario, Canada
OBJECTIVE Selective dorsal rhizotomy (SDR) is a procedure primarily performed to improve function in a subset of
children with limitations related to spasticity. There is substantial variability in operative techniques among centers and
surgeons. Here, the authors provide a technical review of operative approaches for SDR.
METHODS Ovid MEDLINE, Embase, and PubMed databases were queried in accordance with PRISMA guidelines. All
studies included described a novel surgical technique. The technical nuances of each approach were extracted, includ-
ing extent of exposure, bone removal, and selection of appropriate nerve roots. The operative approach preferred at the
authors’ institution (the “2 × 3 exposure”) is also detailed.
RESULTS Five full-text papers were identified from a total of 380 articles. Operative approaches to SDR varied signifi-
cantly with regard to level of exposure, extent of laminectomy, and identification of nerve roots. The largest exposure
involved a multilevel laminectomy, while the smallest exposure involved a keyhole interlaminar approach. At the Hospital
for Sick Children, the authors utilize a two-level laminoplasty at the level of the conus medullaris. The benefits and disad-
vantages of the spectrum of techniques are discussed, and illustrative figures are provided.
CONCLUSIONS Surgical approaches to SDR vary considerably and are detailed and illustrated in this review as a
guide for neurosurgeons. Future studies should address the long-term impact of these techniques on functional out-
comes and complications such as spinal deformity.
https://thejns.org/doi/abs/10.3171/2019.12.PEDS19629
KEYWORDS selective dorsal rhizotomy; cerebral palsy; spasticity; spine
S
elective dorsal rhizotomy (SDR) is a neurosurgical respondence of each nerve root to specific muscle groups;
treatment primarily for a subset of children with ce- those that contributed the most to spasticity were cut,
rebral palsy (CP) characterized by spastic diplegia. while rootlets thought to contribute to gait and postural
Dorsal rhizotomy was originally practiced in the late 19th control were spared.5,23 The procedure also became mul-
century for the relief of intractable pain by Abbe, Bennett, tidisciplinary, with physical therapy and electrophysiology
and Dana.5 After Sherrington demonstrated that section- working alongside the surgical team. In parallel, Fasano
ing dorsal roots could reduce tone in an affected limb, et al. described the electrophysiological characteristics
dorsal rhizotomy was adopted for the treatment of spastic- of rootlets thought most likely to contribute to abnormal
ity rather than pain.5 These early procedures carried sub- muscular tone.6 He advocated for sectioning nerve roots
stantial morbidity, primarily related to severe sensory loss, that had abnormal stimulation thresholds and spread ac-
bladder denervation, postoperative weakness, and persis- tivity to muscles not normally innervated by that spinal
tence of spasticity.23 level.6 Following his 1987 description of the procedure,
In the 1970s dorsal rhizotomy started to become more Peacock is credited with popularizing SDR by expanding
“selective.” In Montpellier, France, Gros introduced intra- upon these previous advances.17
operative electromyography (EMG) to determine the cor- Today, SDR is experiencing a resurgence in popularity
ABBREVIATIONS CP = cerebral palsy; EMG = electromyography; SDR = selective dorsal rhizotomy.
SUBMITTED October 20, 2019. ACCEPTED December 6, 2019.
INCLUDE WHEN CITING Published online February 7, 2020; DOI: 10.3171/2019.12.PEDS19629.
540 J Neurosurg Pediatr Volume 25 • May 2020 ©AANS 2020, except where prohibited by US copyright law
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
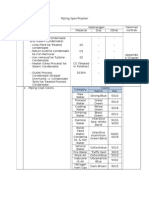
TABLE 1. Summary of operative techniques
Authors & Year Level of Exposure Extent of Bony Exposure Nerve Root Identification
Peacock et al., 1987 L2–5 Multilevel laminectomy/laminoplasty Simple anatomical/EMG
Park & Johnston, 2006 Level of conus (determined on Single-level laminectomy Anatomical/EMG w/ operating microscope; identify
ultrasound) cleft at conus
Bales et al., 2016 Below conus (determined on Single-level laminectomy EMG thresholds used to separate dorsal & ventral
MRI) roots
Sindou & Georgoulis, 2 to 3 levels of interest (most 2- to 3-level interlaminar keyhole Anatomical/EMG based on the position w/in neural
2015 affected nerve roots) approach foramen
Funk & Haberl, 2016 Level of conus (determined on Single-level laminoplasty Anatomical/EMG w/ operating microscope; cleft at
MRI) conus identified
Current technique (2 × 3 Level of conus (determined on 2-level laminoplasty Anatomical/EMG w/ operating microscope; cleft at
exposure) MRI) conus identified
among neurosurgeons, patients, and healthcare networks. Results
The rise of social media has strengthened patient and fam- A total of 380 manuscripts were identified by our initial
ily interest in the procedure, while health-economic analy- search (Supplementary Fig. 1). Overall, 343 studies were
ses have demonstrated its cost-effectiveness.2,15 In 2014 the excluded following title and abstract review. Of the 37 full-
National Health Service in England commissioned a pro- text articles that were assessed, 14 reviews were excluded,
spective study across five hospitals to revaluate the state 11 were nontechnical papers, 3 were repeat descriptions
of funding for the procedure, leading to its recognition of previously published techniques, 2 were conference pa-
and funding from 2018 onwards.26 However, despite this pers, and 2 were in a foreign language. The remaining 5
growth in popularity, multiple variations in the procedure articles consisted of original work written in English and
have been described with respect to location of exposure, describing a unique operative approach to SDR. These
extent of bone removal, and the identification and selection findings are summarized in Table 1 and detailed graphi-
of most appropriate roots for sectioning. The present study cally in Fig. 1.
aims to serve as a technical review of published methods
for SDR. To this end, we conducted a systematic review of
all described surgical approaches to SDR assessing their Peacock et al.
technical nuances, benefits, and potential limitations. We In the early 1980s, Peacock and Eastman pioneered
conclude by describing modifications of the procedure at a form of SDR for children with spasticity secondary to
Toronto’s Hospital for Sick Children. CP, which involved rhizotomies performed in the cauda
equina rather than the conus.18 This technique was later
described in greater detail, coinciding with the reemer-
Methods gence of SDR for the treatment of CP-associated lower-
Study Selection limb spasticity in the modern era.17
The search protocol was developed according to the Under general anesthesia, patients are positioned prone
PRISMA guidelines (see Supplementary Fig. 1 for full and a midline incision is made to expose the lumbar ver-
search strategy and Supplementary Fig. 2 for PRISMA tebrae. Partial L2–5 laminectomies are undertaken with
checklist).13 Briefly, a literature search was performed on adjacent facet joint preservation. Following a longitudi-
August 20, 2019, using the keywords “cerebral palsy,” “rhi- nal dural opening and arachnoid dissection, the posterior
zotomy,” and/or “selective dorsal rhizotomy” in combina- roots of L2–S1 are identified and isolated. Utilizing two
tion. The databases searched included Ovid MEDLINE, unipolar probes, rootlets of each posterior root are sequen-
Embase, and PubMed with no search restrictions. Title, tially subjected to electrical stimulation via single and te-
abstract, and full-text review were conducted by two in- tanic stimuli in the range of 10–150 V, as described by
dependent authors (N.M.W., M.C.D.). Disagreements were Fasano et al.6,7 The corresponding muscle responses were
resolved with discussion and re-review. All final studies observed both visually and with EMG.
included described a novel surgical technique not previ- Criteria that support the decision to divide the rootlet/s
ously published. of interest include a low threshold associated with a sus-
tained muscular contraction or spread of contraction to
Data Synthesis contiguous muscle groups beyond the rootlet’s segmental
Data pertaining to operative technique—with a particu- distribution. Conversely, rootlets are left intact if thresh-
lar emphasis on the extent of exposure, bony removal, and olds are relatively high and muscle contraction is brief
selection of appropriate nerve roots—were extracted for without diffusion.
each study and are summarized in Table 1. Surgical illus-
trations were created for each approach by a professional Park and Johnston
illustrator (A.W.). In 2006, Park and Johnston16 subsequently reported
J Neurosurg Pediatr Volume 25 • May 2020 541
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
FIG. 1. Illustrations of the different bony exposures in SDR. Peacock and colleagues’ 1987 technique17 utilized a multilevel
laminectomy below the conus; in 2006, Park and Johnston16 modified this to a single-level laminectomy at the conus; Sindou and
Georgoulis22 used a less-invasive but more challenging keyhole interlaminar exposure; in 2016, Funk and Haberl8 described a
single-level laminoplasty at the conus; that same year, Bales et al. modified Park’s exposure to a single-level laminectomy below
the conus, with EMG to identify relevant nerve roots; and finally, our so-called 2 × 3 approach is based on a two-level laminoplasty
at the level of the conus. Copyright Nebras Warsi. Published with permission.
542 J Neurosurg Pediatr Volume 25 • May 2020
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
FIG. 2. Ultrasound and MR images of the CSF “cleft” used to distinguish dorsal and ventral roots. A: Sagittal ultrasound view
of the conus medullaris below bony exposure. B: Axial ultrasound view at the conus showing the CSF cleft used to distinguish
dorsal and ventral roots (arrowheads [upper]) and below the conus (lower), where the cleft can no longer be appreciated. C: MRI
correlation of the CSF cleft as seen on ultrasonic views (upper image at the conus and lower image below). Figure is available in
color online only.
their experience of limiting the lumbar exposure.16 Follow- roots (S3–5). The lower sacral nerves characteristically
ing induction of general anesthesia, patients are positioned have little space between them and are left intact. A Silas-
prone on gel bolsters in Trendelenburg angulation to en- tic sheet is positioned under the dorsal L2–S2 nerve roots
courage rostral pooling of cerebrospinal fluid (CSF). In to gently separate them from the ventral roots as the pro-
children younger than 10 years of age, ultrasound images cedure proceeds.
of the conus and cauda equina are obtained to guide the Once the dorsal roots are spread on the Silastic sheet,
approach. In older children, where this would not be pos- EMG testing on each root takes place to establish an in-
sible, the L1 spinous process is localized using x-ray imag- nervation pattern using the hooks of the rhizotomy probes.
ing and marked with infiltration of indigo carmine dye. Threshold voltages are determined via recordings from
Following a limited midline lumbar incision over the the lower-limb musculature. The root is then dissected
interspinous space overlying the conus, the interspinous into 3–5 rootlets or fascicles of equal size using a Scheer
ligament and ligamentum flavum are excised to permit needle and stimulated with constant square-wave pulses
further ultrasonic views. Typically, two levels are exam- of 0.1 msec at a rate of 0.5 Hz. An increasing stimulus
ined to localize the conus and cauda equina. A laminecto- is applied until a reflex response is visualized from the
my over the index level is performed using a craniotome to ipsilateral muscles. When a reflex threshold is determined,
minimize facet joint disruption, whereupon the ultrasound the rootlet is then subjected to a train of a 50-Hz tetanic
is reemployed to reassess the conus’ position to determine stimulation for 1 second and the resulting reflex graded.
whether additional caudal laminectomies are necessary to Park and Johnston16 based their decision to divide a giv-
expose at least 5 mm of the caudal conus. This allows safe en rootlet on the number of rootlets producing sustained
separation of the dorsal and ventral roots. responses at that level and their response intensity, as de-
A linear dural incision is made and the operating mi- scribed by Phillips and Park.19 Rootlets producing a signif-
croscope is then introduced. The operating table may be icant reflex response (typically 3+ or 4+) undergo division.
tilted away from the surgeon to permit dissection of the At least one rootlet is left intact in order to preserve sensa-
contralateral nerve roots. The arachnoid is divided and the tion. Deafferented roots are sequentially placed below the
conus and filum terminale are visualized. The L2 nerve Silastic sheet to separate them from the untested bundle.
roots are next identified at their respective foramina. The The authors report sectioning 60%–65% of the examined
dorsal and ventral roots are separated and traced back nerve roots. Half of the L1 root is routinely divided with-
to the conus in order to appreciate the cleft that defines out EMG testing as it was deemed unreliable for this level.
ventral and dorsal sections (Fig. 2). Following medial dis- The dura mater is closed with a 4-0 monofilament nylon.
placement of the L2 root and neighboring dorsal roots, the An intradural injection of clonidine and morphine is ap-
ventral roots are covered with a cottonoid. Next the sur- plied, and Gelfoam is left over the laminectomy defect
geon is advised to identify the S2 root and lower sacral before a layered wound closure is performed. Since their
J Neurosurg Pediatr Volume 25 • May 2020 543
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
initial publication, the group has also described the addi- through electrophysiology, and reduction of the risks of
tion of a postoperative epidural catheter to improve patient spinal instability.
analgesia.14 Anatomical accuracy is achieved by surgically access-
ing roots where both their ventral and dorsal components
Bales et al. are clearly separated at the exit to/entry from their forami-
In 2016, Bales et al.1 described a modification of Park’s nal sheath. This anatomical localization is then followed
technique that selectively analyzed each individual nerve by functional verification of the dorsal root by electrical
root with EMG to separate dorsal and ventral nerve roots stimulation and subsequent interruption of the dorsal root/
through comparison of stimulus responses. They argued rootlets likely to participate in spasticity. According to
that the anatomical variation present at the level of the the authors, the risk of spinal instability is minimized by
conus can make Park’s anatomical approach to identify- maximal preservation of the bony and posterior ligamen-
ing the dorsal roots particularly challenging, and therefore tous structures through an interlaminar spinal approach.
they advocated for the use of electrophysiology to dichoto- Preoperatively, afferents from the most affected mus-
mize the rootlets. cles are identified based on anatomical knowledge. These
Preoperative MRI is performed to determine the level specific dorsal nerve roots are then targeted through 2 or 3
of the conus. After induction of general anesthesia, the pa- interlaminar spaces. For example, the transiting L3 and L4
tient is placed in the prone position and the laminectomy dorsal roots could be accessed through an L2–3 interlami-
nar keyhole. The patient is positioned prone, and a midline
is planned for one vertebral level below the conus, typi-
lumbar incision is performed according to the topography
cally at L2. An intraoperative radiograph is taken to verify
of the predetermined interlaminar spaces. An intraopera-
the location of the appropriate level, which is then marked
tive radiograph is used to confirm the operative levels. The
at the level of the skin. A single-level laminectomy is per- muscles are dissected, while leaving the spinous processes
formed, and intraoperative ultrasound is used to visualize and interspinous ligaments intact. At the selected inter-
the nerve roots and ensure the exposure is below the level laminar spaces, the ligamentum flavum is removed and
of the conus. Care is taken to remain medial to the facets the space is expanded with rongeurs. The lower two-thirds
to minimize the risk of postlaminectomy spinal deformity. of the upper lamina and the upper two-thirds of the lower
The dura and arachnoid are opened, and a Silastic sheet lamina are removed in the midline underneath the inter-
cut to a width of 3–4 mm is placed ventrally around all the spinous ligaments.
roots of the cauda equina. A 2-cm midline opening is made in the dura and arach-
Direct stimulation of the nerve rootlets is achieved with noid. The microscope is then employed, and an oblique
bipolar stimulation using rhizotomy probes. The initial trajectory, on the order of 45°, is used to access the con-
goal is to differentiate the ventral and dorsal nerve root- tralateral roots by passing underneath the preserved in-
lets by recording motor thresholds. Motor responses fol- terspinous ligaments. Through this approach, Sindou et
lowing direct stimulation of ventral (motor) rootlets are al.,23 have found that the ventral and dorsal components of
typically achieved at a range of less than 0.4–0.5 mA and the nerve root are identified constantly at the exit to/entry
most commonly stimulate at 0.1 mA. By comparison, dor- from their corresponding dural sheath. Two roots can be
sal (sensory) rootlets have thresholds greater than 0.5 mA accessed on each side, one upward and one downward. At
and most commonly stimulate above 1.0 mA. Rootlets that this point, the posteriorly located dorsal root with its 4–5
stimulate at low thresholds (typically < 0.4 mA) are ex- rootlets are tested with electrophysiology, as previously
cluded as ventral (motor) rootlets and are tucked behind described, and subsequently sectioned if selected based
the Silastic dam. Rootlets that elicited an anal sphincter on the Phillips and Park criteria.19
response are also preserved. Rootlets that stimulate at the
established threshold for sensory rootlets are further stim- Funk and Haberl
ulated with a 1-second train of 50-Hz tetanic stimulation.
In 2016, Funk and Haberl8 published a paper describing
Dorsal rootlet responses are graded based on Park’s
a single-level laminoplasty approach. Their aim was again
criteria, as previously described.16 If the response is mark-
to minimize instability of the spine, and by extension re-
edly abnormal, 75%–90% of the rootlet is cut. If slightly duce the incidence of late scoliosis.
abnormal, 50% of the rootlet is cut. If the response to Their technique begins with preoperative MRI to lo-
tetanic stimulation is normal but the rootlet elicits a re- cate the level of the conus medullaris. The patient is
sponse only in affected muscle groups, 50% of the rootlet placed prone, and a laminectomy utilizing a craniotome
is incised. Once all the rootlets have been stimulated in drill at the level of the conus is used to provide interlami-
this fashion, the number of rootlets that are incised is re- nar access. The authors then describe the use of long-blade
viewed to ensure that there is adequate representation of Ruskin bone-splitting forceps to make oblique cuts in the
the affected muscle groups. spinous processes above and below the level where the
laminae are dissected. With these cuts, a midline complex
Sindou et al. is disconnected from the rest of the spine and stored in a
In 2015, Sindou and Georgoulis22 described the keyhole damp cloth. This complex consists of the spinous process
interlaminar dorsal rhizotomy technique in an attempt to of the MRI-defined level, the adjoining medial lamina, the
overcome the potential disadvantages of multilevel lami- adjacent superior and inferior spinous process segments
nectomy. The goals were to achieve anatomical accuracy attached through the intervening posterior ligaments.
of the ventral and dorsal nerve roots, functional selectivity A midline dural incision follows, and the L1–S2 dorsal
544 J Neurosurg Pediatr Volume 25 • May 2020
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
sensory roots are separated and placed in a Silastic sheet.
For the L1 rootlet, 50% of the sensory rootlets are cut
without EMG. From L2 to S1, at each given level, roots are
separated into anywhere from 4 to 8 rootlets. According to
EMG evaluation using the Phillips and Park grading scale,
50%–60% of the rootlets are cut.19 The S2 root is divided
into 2 parts, the bulbocavernous reflex is stimulated, and
the fascicle showing the least pudendal nerve activity is
severed.
Following the SDR, the dura is closed tightly, and the
aforementioned midline complex is replated to the spine,
across the intact spinous process and dissected lamina.
This is done using multihole miniplates. The superior and
inferior obliquely cut spinous processes are fixed to their
respective ends using single sutures. In younger children, FIG. 3. Schematic representation of rootlet division. As shown, a Silastic
this suturing is done once through the bony spinous pro- sheet is placed between the dorsal and ventral nerve roots. The dorsal
(sensory) nerve roots are then divided into individual rootlets using
cess. In older children, the stitch is placed twice around the microdissectors. Stimulation of each individual rootlet then proceeds as
spinous process fragments through the interspinous liga- described. Copyright Nebras Warsi. Published with permission.
ments. Muscle and fascia are closed with sutures running
through the interspinous and supraspinous ligaments.
The 2 × 3 Exposure Technique
L3 to S1 (Fig. 3). The L3 nerve root is followed inferiorly
Patients are initially assessed in a multidisciplinary
toward its lateral exit site in the dura, which can be visu-
clinic. Candidates are typically 4–8 years old, with am- alized by sharply angling the operating microscope. This
bulatory spastic diplegic CP. Clinical examinations and provides final anatomical confirmation of the separation of
EMG recordings from the L1–S1 muscle groups are used motor and sensory roots. From lateral to medial, L4 to S1
to form a preoperative rhizotomy plan. This plan is made are stimulated and sectioned systematically thereafter. We
in consensus with the neurosurgical and physiotherapy repeat the procedure on the contralateral side, and finally,
teams. The anticipated amount of dorsal root transection when indicated, L1 may be sectioned by sharply angling
at each level is generally on the order of 50%–70%. the microscope superiorly. If indicated, the exposure also
A preoperative MR image of the spine is used to identi- provides opportunity to selectively section the S2 dorsal
fy the level of the conus so as to inform the ideal location of rootlets, as previously described, although this is not rou-
a 2-level laminoplasty aimed at unroofing the L2–S1 nerve tinely performed for all patients.
roots. With the patient in the prone position, intraoperative Our stimulation protocol uses a bipolar probe with a
fluoroscopy is used to identify the target levels for the lami- 100-μsec pulse width, which is delivered at 2.1 Hz to the
noplasty, and these levels are demarcated on the skin. A left and right L2–S1 nerve roots in order to obtain both
clear drape is placed inferiorly and tented over a curtain to sensory and motor stimulation intensity thresholds. At
allow physiotherapists access to the lower extremities. each level, both dorsal sensory and ventral motor roots
A midline dissection is performed until the supraspi- are identified and separated with a Silastic sheet. Rootlets
nous ligament overlying the planned laminoplasty site within the sensory roots are dissected apart using micro-
is identified. Bilateral subperiosteal dissections are then dissectors. The S2–4 nerve roots are confirmed via stimu-
performed while sparing this ligament. A 2-level lamino- lation and are spared.
plasty respecting the medial facet is then performed (Fig. Tetanic stimulation at sensory thresholds is then ap-
1). Inferiorly, the supraspinous ligament, interspinous liga- plied to separate rootlets at a frequency of 50 Hz for 1 sec-
ment, and ligamentum flavum are divided. The spinous ond. We grade responses to stimulation of rootlets using
processes and posterior ligament complex above the target the Phillips and Park classification system.19 Rootlets with
site are preserved and reflected superiorly. The ultrasound the most abnormal responses are transected. The number
probe is used to confirm the level of the conus, as well as of rootlets transected at a given level is based on the pre-
to appreciate the cleft between dorsal and ventral roots vis- operative rhizotomy plan described above. This process is
ible only at this level (Fig. 2). This allows us to identify the continued systematically to bilateral L2–S1 nerve roots.
optimal location for the midline dural opening. The dural Evoked potentials are then used to confirm the functional
leaflets are then tacked dorsolaterally to fascia to maxi- integrity of the ventral roots prior to closure.
mize intradural visualization. The dura is closed in a watertight fashion, and the lami-
The method is described herein as a 2 × 3 exposure noplasty complex is reflected back into position and fixed
because two nerve roots (most commonly L2 and L3) can to native bone using miniplates. The remaining closure
be visualized at the dural exit site, and 3 nerve roots (most process proceeds in standard multilayer fashion for the
commonly L4, L5, and S1) are identified in the midline. L2 lumbar spine.
is readily identified beneath the L2 pedicle, and anatomi-
cally, the dorsal and ventral roots are separated and L2 is
sectioned. A Silastic sheet is then placed in the CSF cleft Discussion
at the conus separating the dorsal and ventral roots from As interest in SDR continues to grow, there is a need to
J Neurosurg Pediatr Volume 25 • May 2020 545
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
evaluate and compare the various surgical nuances of this cal for adequate exposure and identification of relevant
procedure. A variety of techniques have been described, nerve roots. In this regard, Peacock and colleagues’ initial
which vary with regard to the extent of bony exposure, approach is simplest,17 followed by Bales et al.’s dichoto-
identification of dorsal and ventral nerve roots, and selec- mizations of nerve roots using EMG.1
tion of appropriate rootlets for sectioning (Table 1). Beyond identification of nerve roots, the extent to which
Peacock et al.17 have described the largest bony expo- each root should be transected is unclear. There is evi-
sure, which may be associated with an increased incidence dence to suggest a direct relationship between the percent-
of spinal deformity.10 Alternatively, 1- and 2-level proce- age of dorsal root transected and postoperative functional
dures come at the cost of easy anatomical identification improvement.12 At our institution, we employ preoperative
of individual nerve roots. To circumvent this problem, the assessments to determine the amount to transect at each
use of extended EMG recordings increases the specificity level; however, this is not widely accepted. Intraopera-
of nerve root identification.11 The technique described by tively, we only transect rootlets with the most abnormal
Bales et al.1 has considerable overlap with that initially de- responses, and our target is on the order of 50%–70% per
scribed by Park and Johnston.16 However, a key difference level. This is in keeping with the technique described by
is that Bales et al. make their opening below the conus Funk and Haberl. However, it is not clear whether it is
and identify nerve roots using EMG, which is an entirely more important to transect simply a larger percentage of
different process from the anatomical identification de- the dorsal root or simply a larger percentage of the subset
scribed by Park and Johnston. Sindou and colleagues22,23 of abnormal rootlets.
described a keyhole interlaminar approach, whereas Funk Given that no single approach is clearly superior, the
and Haberl used a single-level laminoplasty. Our 2-level technique used will depend on individual surgeon prefer-
laminoplasty potentially mitigates the risk of multilevel ence and comfort with the variable interrelationship be-
laminectomy with several advantages over a single-level tween anatomy and neurophysiology in this patient popu-
approach. Cranially, the anatomy of the conus, and the lation.
CSF cleft between dorsal and ventral roots is preserved
(Fig. 2), facilitating separation of the ventral and dorsal Conclusions
roots. Caudally, two levels of exiting nerves (typically
L2 and L3) can be identified at the dural exit site, pro- A number of questions remain to be answered as they
viding confirmation of the separation between motor and pertain to these different operative approaches to SDR.
sensory roots. Distal to the conus, the sensory roots are One critical avenue of further study will be a comparison
best appreciated and can be traced backward toward the of each of these operative techniques vis-à-vis the out-
conus. Furthermore, with regard to bony exposure, there comes and potential complications. Similarly, it would be
is evidence to suggest that laminoplasty confers increased important to evaluate these factors among different centers
biomechanical stability to the spine compared with lami- and surgeons, as significant heterogeneity has been previ-
nectomy, although the exact extent of this advantage is ously reported. For example, Park’s group, reported only a
unclear.10,25 single CSF leak requiring operative repair in their series of
With regard to postoperative spinal deformity, there is a 1500 patients and no spinal deformity requiring operation,
growing body of literature to support the long-term risks of while other articles put the incidence of significant spinal
this complication with multilevel bony exposures.3,4,9,20,24,27 deformity in the 10% range.3,4,9,16,20,24,27 The value of ad-
The incidence of postoperative spinal deformity ranges juncts, including intraoperative neuromonitoring, should
from approximately 12% to greater than 35% in the lit- also be the subject of future research.
erature.3,4,9,20,24,27 Interestingly, even without surgery Saito
et al. estimated the rate of spinal deformity in CP to be References
68%, especially scoliosis, with large multilevel exposures 1. Bales J, Apkon S, Osorio M, Kinney G, Robison RA, Hooper
thought to increase this risk.21 Unfortunately, at present, E, et al: Infra-conus single-level laminectomy for selective
no comparative studies exist that have assessed whether dorsal rhizotomy: technical advance. Pediatr Neurosurg
approaches such as the keyhole interlaminar approach and 51:284–291, 2016
laminotomy techniques offer a significant advantage in 2. Canty MJ, Breitbart S, Siegel L, Fehlings D, Milo-Manson
this regard. G, Alotaibi NM, et al: The role of social media in selective
Identification of appropriate nerve roots is another chal- dorsal rhizotomy for children: information sharing and social
support. Childs Nerv Syst 35:2179–2185, 2019
lenge in SDR as the procedure by which candidate nerve 3. Cobb MA, Boop FA: Replacement laminoplasty in selective
roots are targeted can vary widely based on the operative dorsal rhizotomy: possible protection against the develop-
approach. For example, many of the procedures described ment of musculoskeletal pain. Pediatr Neurosurg 21:237–
require tracing back each root with an operative micro- 242, 1994
scope and identifying the cleft at the conus to separate 4. Crawford K, Karol LA, Herring JA: Severe lumbar lordosis
dorsal and ventral roots. The benefits of these conus-level after dorsal rhizotomy. J Pediatr Orthop 16:336–339, 1996
approaches are that they allow a more limited bony expo- 5. Enslin JMN, Langerak NG, Fieggen AG: The evolution of
selective dorsal rhizotomy for the management of spasticity.
sure. In our experience and in the literature, this procedure Neurotherapeutics 16:3–8, 2019
has been successful but does require thorough knowledge 6. Fasano VA, Broggi G, Zeme S: Intraoperative electrical stim-
of the anatomy at the level of the conus. Similarly, for the ulation for functional posterior rhizotomy. Scand J Rehabil
keyhole interlaminar approach, intimate operative experi- Med Suppl 17:149–154, 1988
ence with lumbar laminoforaminotomy techniques is criti- 7. Fasano VA, Broggi G, Zeme S, Lo Russo G, Sguazzi A:
546 J Neurosurg Pediatr Volume 25 • May 2020
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
Warsi et al.
Long-term results of posterior functional rhizotomy. Acta 22. Sindou M, Georgoulis G: Keyhole interlaminar dorsal rhizot-
Neurochir Suppl (Wien) 30:435–439, 1980 omy for spastic diplegia in cerebral palsy. Acta Neurochir
8. Funk JF, Haberl H: Monosegmental laminoplasty for selec- (Wien) 157:1187–1196, 2015
tive dorsal rhizotomy—operative technique and influence 23. Sindou M, Georgoulis G, Mertens P: History of neurosurgi-
on the development of scoliosis in ambulatory children with cal treatment for spasticity, in Neurosurgery for Spasticity.
cerebral palsy. Childs Nerv Syst 32:819–825, 2016 A Practical Guide for Treating Children and Adults. Vi-
9. Golan JD, Hall JA, O’Gorman G, Poulin C, Benaroch TE, enna: Springer, 2014
Cantin MA, et al: Spinal deformities following selective dor- 24. Steinbok P, Hicdonmez T, Sawatzky B, Beauchamp R,
sal rhizotomy. J Neurosurg 106 (6 Suppl):441–449, 2007 Wickenheiser D: Spinal deformities after selective dorsal
10. Johnson MB, Goldstein L, Thomas SS, Piatt J, Aiona M, rhizotomy for spastic cerebral palsy. J Neurosurg 102 (4
Sussman M: Spinal deformity after selective dorsal rhi- Suppl):363–373, 2005
zotomy in ambulatory patients with cerebral palsy. J Pediatr 25. Subramaniam V, Chamberlain RH, Theodore N, Baek S,
Orthop 24:529–536, 2004 Safavi-Abbasi S, Senoğlu M, et al: Biomechanical effects
11. Legatt AD, Schroeder CE, Gill B, Goodrich JT: Electrical of laminoplasty versus laminectomy: stenosis and stability.
stimulation and multichannel EMG recording for identifica- Spine (Phila Pa 1976) 34:E573–E578, 2009
tion of functional neural tissue during cauda equina surgery. 26. Summers J, Coker B, Eddy S, Elstad M, Bunce C, Bourmpaki
Childs Nerv Syst 8:185–189, 1992 E, et al: Selective dorsal rhizotomy in ambulant children with
12. McLaughlin J, Bjornson K, Temkin N, Steinbok P, Wright V, cerebral palsy: an observational cohort study. Lancet Child
Reiner A, et al: Selective dorsal rhizotomy: meta-analysis of Adolesc Health 3:455–462, 2019
three randomized controlled trials. Dev Med Child Neurol 27. Turi M, Kalen V: The risk of spinal deformity after selective
44:17–25, 2002 dorsal rhizotomy. J Pediatr Orthop 20:104–107, 2000
13. Moher D, Liberati A, Tetzlaff J, Altman DG: Preferred re-
porting items for systematic reviews and meta-analyses: the
PRISMA statement. PLoS Med 6:e1000097, 2009 Disclosures
14. Moore RP, Wester T, Sunder R, Schrock C, Park TS: Peri- The authors report no conflict of interest concerning the materi-
operative pain management in children with cerebral palsy: als or methods used in this study or the findings specified in this
comparative efficacy of epidural vs systemic analgesia proto- paper.
cols. Paediatr Anaesth 23:720–725, 2013
15. National Institute for Health and Care Excellence: Final Author Contributions
Report: Selective Dorsal Rhizotomy (SDR). London:
Centre for Health Technology Evaluation Observational Data Conception and design: Ibrahim, Warsi, Dewan. Acquisition of
Unit, 2018 (https://www.england.nhs.uk/commissioning/ data: Warsi, Tailor, Coulter, Shakil. Analysis and interpretation
wp-content/uploads/sites/12/2019/04/SDR-CtE-NICE- of data: Ibrahim, Warsi, Tailor, Coulter, Shakil, Breitbart, Dewan.
Evaluation-Report.pdf) [Accessed December 20, 2019] Drafting the article: Warsi, Tailor, Coulter, Shakil, Workewych,
16. Park TS, Johnston JM: Surgical techniques of selective dorsal Haldenby. Critically revising the article: all authors. Reviewed
rhizotomy for spastic cerebral palsy. Technical note. Neuro- submitted version of manuscript: all authors. Approved the final
surg Focus 21(2):e7, 2006 version of the manuscript on behalf of all authors: Ibrahim.
17. Peacock WJ, Arens LJ, Berman B: Cerebral palsy spasticity. Statistical analysis: Administrative/technical/material support:
Selective posterior rhizotomy. Pediatr Neurosci 13:61–66, Haldenby, Breitbart, Strantzas, Vandenberk. Study supervision:
1987 Ibrahim, Dewan. Illustrations: Workewych.
18. Peacock WJ, Eastman RW: The neurosurgical management
of spasticity. S Afr Med J 60:849–850, 1981 Supplemental Information
19. Phillips LH, Park TS: Electrophysiology studies of selective Online-Only Content
posterior rhizotomy patients, in Park TS, Phillips LH, Pea- Supplemental material is available with the online version of the
cock WJ (eds): Management of Spasticity in Cerebral Pal- article.
sy and Spinal Cord Injury. Neurosurgery. State of the Art Supplementary Figs. 1 & 2. https://thejns.org/doi/suppl/
Reviews. Philadelphia: Hanley & Belfus, 1989, pp 459–469 10.3171/2019.12.PEDS19629.
20. Ravindra VM, Christensen MT, Onwuzulike K, Smith JT,
Halvorson K, Brockmeyer DL, et al: Risk factors for progres- Correspondence
sive neuromuscular scoliosis requiring posterior spinal fu-
George M. Ibrahim: Hospital for Sick Children, Toronto, ON,
sion after selective dorsal rhizotomy. J Neurosurg Pediatr
Canada. george.ibrahim@sickkids.ca.
20:456–463, 2017
21. Saito N, Ebara S, Ohotsuka K, Kumeta H, Takaoka K:
Natural history of scoliosis in spastic cerebral palsy. Lancet
351:1687–1692, 1998
J Neurosurg Pediatr Volume 25 • May 2020 547
Unauthenticated | Downloaded 05/07/21 11:39 AM UTC
You might also like
- Computer System Validation Risk Assessment ToolDocument3 pagesComputer System Validation Risk Assessment Toolcpkakope100% (1)
- The Woman Speaks To The Man Who Has Employed Her SonDocument3 pagesThe Woman Speaks To The Man Who Has Employed Her SonSerena SulawammotNo ratings yet
- Hydraulic Axial Piston Eaton Vickers PVB Pump: - Basic CharacteristicsDocument13 pagesHydraulic Axial Piston Eaton Vickers PVB Pump: - Basic Characteristicsjose alberto olvera gomezNo ratings yet
- Dorsal RhizotomyDocument13 pagesDorsal RhizotomyAiman MaidanNo ratings yet
- Fnhum 16 778347Document5 pagesFnhum 16 778347Josue GarciaNo ratings yet
- Abat F. 2019. Comparison US Guided vs. Blind Interventions Supraspinatus TendinopathyDocument10 pagesAbat F. 2019. Comparison US Guided vs. Blind Interventions Supraspinatus TendinopathyJavier MartinNo ratings yet
- The Evolution of Selective Dorsal Rhizotomy For The Management of SpasticityDocument6 pagesThe Evolution of Selective Dorsal Rhizotomy For The Management of SpasticityJessica MaiaNo ratings yet
- Understanding Carpal Tunnel Syndrome.4Document8 pagesUnderstanding Carpal Tunnel Syndrome.4ayu permata dewiNo ratings yet
- Microsurgical Resection of Vestibular SchwznomaDocument2 pagesMicrosurgical Resection of Vestibular SchwznomaWilson Quispe AlanocaNo ratings yet
- Journal of Hand Therapy: Scienti Fic/clinical ArticleDocument7 pagesJournal of Hand Therapy: Scienti Fic/clinical ArticleDaniel GuevaraNo ratings yet
- Deland 2005Document10 pagesDeland 2005DavidNo ratings yet
- Postoperative Spinal CT: What The Radiologist Needs To KnowDocument22 pagesPostoperative Spinal CT: What The Radiologist Needs To KnowMauricio RuizNo ratings yet
- Fneur 14 1138661Document2 pagesFneur 14 1138661ChadiIbrahimNo ratings yet
- Clinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoDocument5 pagesClinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoSerque777No ratings yet
- Clinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoDocument5 pagesClinical Neurophysiology: Yukiko Tsuji, Yu-Ichi Noto, Takamasa Kitaoji, Yuta Kojima, Toshiki MizunoSerque777No ratings yet
- Quantitative Anatomical Comparison of Anterior, Anterolateral and Lateral, Microsurgical and Endoscopic Approaches To The Middle Cranial FossaDocument49 pagesQuantitative Anatomical Comparison of Anterior, Anterolateral and Lateral, Microsurgical and Endoscopic Approaches To The Middle Cranial FossaAndrés BotelloNo ratings yet
- Ask Us : Readers' ForumDocument1 pageAsk Us : Readers' ForumakNo ratings yet
- Radiol 2291020222Document10 pagesRadiol 2291020222javiervuNo ratings yet
- Evolution of The Surgical Management of Cauda Equina SyndromeDocument13 pagesEvolution of The Surgical Management of Cauda Equina SyndromeAtul JainNo ratings yet
- 1 s2.0 S1878875018300159 MainDocument9 pages1 s2.0 S1878875018300159 MainAlexandreNo ratings yet
- Connectivity of the Superficial Muscles of the Human Perineum a Diffusion Tensor Imaging-Based Global Tractography StudyDocument10 pagesConnectivity of the Superficial Muscles of the Human Perineum a Diffusion Tensor Imaging-Based Global Tractography Studychaiyadol tantasithNo ratings yet
- Ultrasound of The Hand and Wrist in RheumatologyDocument8 pagesUltrasound of The Hand and Wrist in RheumatologyRaphael SiqueiraNo ratings yet
- Superficial Radial Nerve Compression Due To Fibrom 2019 Acta Orthopaedica EtDocument3 pagesSuperficial Radial Nerve Compression Due To Fibrom 2019 Acta Orthopaedica EtanggiNo ratings yet
- Rodilla Inervación Tran2018 PDFDocument8 pagesRodilla Inervación Tran2018 PDFLore BarreraNo ratings yet
- Anatomical Variation of Sciatic Nerve Course in Saudi Population A Magnetic Resonance Imaging StudyDocument8 pagesAnatomical Variation of Sciatic Nerve Course in Saudi Population A Magnetic Resonance Imaging StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Kerasnoudis 2014Document10 pagesKerasnoudis 2014Laura A M MNo ratings yet
- Singh 2012Document6 pagesSingh 2012NadewdewNo ratings yet
- FNIRS2018 AbstractDocument312 pagesFNIRS2018 AbstractJn5omEghSU0j0FNo ratings yet
- Standard Reference Values For Musculoskeletal - Schmidt Schicke Gromnica-IhleDocument7 pagesStandard Reference Values For Musculoskeletal - Schmidt Schicke Gromnica-IhleFer Hijar FraustoNo ratings yet
- Carpal Tunnel SyndromeDocument28 pagesCarpal Tunnel Syndromems bsNo ratings yet
- Chordoma of The Corpus Callosum: Case Report: Literature SearchDocument7 pagesChordoma of The Corpus Callosum: Case Report: Literature SearchAleksandar DimovskiNo ratings yet
- Beyaz 2016Document7 pagesBeyaz 2016nisannnNo ratings yet
- Ultrasound-Guided Injection For Lacertus SyndromeDocument3 pagesUltrasound-Guided Injection For Lacertus SyndromeAhmed sahliNo ratings yet
- Imaging Anatomy of The Cranial Nerves: December 2015Document22 pagesImaging Anatomy of The Cranial Nerves: December 2015Alejandro VanegasNo ratings yet
- Role of High Resolution Ultrasound in Assessment oDocument16 pagesRole of High Resolution Ultrasound in Assessment oilham Maulana ArifNo ratings yet
- Green 2013Document4 pagesGreen 2013Angel GutierrezNo ratings yet
- MontotenniselbowDocument7 pagesMontotenniselbowPURVA THAKURNo ratings yet
- Literature Review Endoscopic Techniques For Spinal Oncology: A SystematicDocument8 pagesLiterature Review Endoscopic Techniques For Spinal Oncology: A SystematicAhana MukherjeeNo ratings yet
- Weiner 2008Document6 pagesWeiner 2008Indira Ulfa DunandNo ratings yet
- 1 s2.0 S0749806314004009 MainDocument10 pages1 s2.0 S0749806314004009 MainbilourNo ratings yet
- Labiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFDocument13 pagesLabiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFAlexandra DumitracheNo ratings yet
- How Many Joints in The Hands and Wrists Should Included in A Score Radiologic Abnormalities Used To Assess Rheumatoid Arthritis?Document10 pagesHow Many Joints in The Hands and Wrists Should Included in A Score Radiologic Abnormalities Used To Assess Rheumatoid Arthritis?Devi PrilliantiNo ratings yet
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocument9 pagesSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNo ratings yet
- FVVinObGyn 14 17Document13 pagesFVVinObGyn 14 17Carlos Eduardo QueirozNo ratings yet
- Diagnostics 13 01928Document30 pagesDiagnostics 13 01928fahaxa7201No ratings yet
- Techniques in Hand and Amp Upper ExtremiDocument6 pagesTechniques in Hand and Amp Upper ExtremiSotiris PlakoutsisNo ratings yet
- The Roof of The Labyrinthine Facial Nerve Canal and The Geniculate Ganglion Fossa On High-Resolution Computed Tomography - Dehiscence Thickness and PneumatizationDocument11 pagesThe Roof of The Labyrinthine Facial Nerve Canal and The Geniculate Ganglion Fossa On High-Resolution Computed Tomography - Dehiscence Thickness and PneumatizationSa'Deu FondjoNo ratings yet
- Morphology of Cranial Sutures and RadiologicDocument6 pagesMorphology of Cranial Sutures and RadiologicEvans RodrigezNo ratings yet
- Radial Nerve and PIN JSS 2019Document6 pagesRadial Nerve and PIN JSS 2019MercedesNo ratings yet
- Bloqueo Facetario UsgDocument7 pagesBloqueo Facetario UsgManolin KinNo ratings yet
- Results of Surgical TreatmentDocument4 pagesResults of Surgical TreatmentChristine Yohana SianturiNo ratings yet
- Uso de Ultrasonografia para Medial EpycondilitisDocument5 pagesUso de Ultrasonografia para Medial EpycondilitisSantiago BianchiNo ratings yet
- What Should We Be Careful of Ankle Arthroscopy?: or Thopaedic Surger yDocument9 pagesWhat Should We Be Careful of Ankle Arthroscopy?: or Thopaedic Surger yJaysellePuguonTabijeNo ratings yet
- Comparison of The Pharyngeal Airways of PatientsDocument10 pagesComparison of The Pharyngeal Airways of PatientsfriscaNo ratings yet
- Research Article: The Effect of Parkinson's Disease On Patients Undergoing Lumbar Spine SurgeryDocument8 pagesResearch Article: The Effect of Parkinson's Disease On Patients Undergoing Lumbar Spine SurgeryMelanie Arabsky LedgerNo ratings yet
- Mandibular Rest Position and ElectricalDocument6 pagesMandibular Rest Position and ElectricalPaula GuerreroNo ratings yet
- The Veterinary Journal: D.A. Portela, N. Verdier, P.E. OteroDocument12 pagesThe Veterinary Journal: D.A. Portela, N. Verdier, P.E. Oteromouxritsa_83No ratings yet
- Marcuzzo 2019Document12 pagesMarcuzzo 2019QuiLeNo ratings yet
- Nakama 2005Document7 pagesNakama 2005angelica barrazaNo ratings yet
- High Contrast High Resolution Imaging of PosttraumDocument10 pagesHigh Contrast High Resolution Imaging of PosttraumPaulo Ferreira OrtodontiaNo ratings yet
- Comparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisDocument6 pagesComparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisWilliam ChienNo ratings yet
- Advances in Vestibular Schwannoma Microneurosurgery: Improving Results with New TechnologiesFrom EverandAdvances in Vestibular Schwannoma Microneurosurgery: Improving Results with New TechnologiesLuciano MastronardiNo ratings yet
- Planning and Facilities: Building StorageDocument31 pagesPlanning and Facilities: Building Storagequsai migdadiNo ratings yet
- Piping SpecificationDocument5 pagesPiping SpecificationShandi Hasnul FarizalNo ratings yet
- Laboratory Information Management System: Prepared By: Mariela C. Ronquillo, RMTDocument33 pagesLaboratory Information Management System: Prepared By: Mariela C. Ronquillo, RMTRonel RonquilloNo ratings yet
- Product Manual 26361V1 (Revision F) : 505DE Digital Governor For Steam TurbinesDocument198 pagesProduct Manual 26361V1 (Revision F) : 505DE Digital Governor For Steam TurbinesGuilherme Marquezin100% (1)
- Statement of Account: State Bank of IndiaDocument1 pageStatement of Account: State Bank of Indiavishalasharma0% (1)
- Grade 12 LM Physical Science 1 Module4Document21 pagesGrade 12 LM Physical Science 1 Module4ladyheart ۦۦNo ratings yet
- Inorganic Chemistry HomeworkDocument3 pagesInorganic Chemistry HomeworkAlpNo ratings yet
- Use of AI in Medicinal Product Lifecycle 1689684121Document17 pagesUse of AI in Medicinal Product Lifecycle 1689684121vivek rakhaNo ratings yet
- Material HPLCDocument19 pagesMaterial HPLCIsmil ImamaNo ratings yet
- Model: Stored Energy Solutions For A Demanding World: Dimensions MM InchDocument2 pagesModel: Stored Energy Solutions For A Demanding World: Dimensions MM Incheddywidjaya9No ratings yet
- Towncall Rural Bank, Inc.: To Adjust Retirement Fund Based On Retirement Benefit Obligation BalanceDocument1 pageTowncall Rural Bank, Inc.: To Adjust Retirement Fund Based On Retirement Benefit Obligation BalanceJudith CastroNo ratings yet
- This Tongue Is Not My Own Dogtooth and TDocument11 pagesThis Tongue Is Not My Own Dogtooth and TGeorgiana Geo GeoNo ratings yet
- IPC in Family PlanningDocument12 pagesIPC in Family PlanningHari MurtiNo ratings yet
- Case Study On A Highway Project: Environmental Impact AssesmentDocument10 pagesCase Study On A Highway Project: Environmental Impact AssesmentSRUTHI FRANCIS M.Tech Environmental Engineering 2020-2022No ratings yet
- MCN KweenDocument4 pagesMCN KweenAngelo SigueNo ratings yet
- T N M M T N M M: HE EW Essies Anual HE EW Essies AnualDocument8 pagesT N M M T N M M: HE EW Essies Anual HE EW Essies AnualMunna100% (1)
- Compensation Practice Cathy Alonso Strayer University (BUS409008VA016-1174-001) Compensation Management Anthony Jacob April 29, 2017Document8 pagesCompensation Practice Cathy Alonso Strayer University (BUS409008VA016-1174-001) Compensation Management Anthony Jacob April 29, 2017Srestha ChatterjeeNo ratings yet
- Wear Solutions BrochureDocument16 pagesWear Solutions BrochureOkan KalendarNo ratings yet
- Bence Bays Resume July 2015Document2 pagesBence Bays Resume July 2015api-292242662No ratings yet
- 956-0302 Onan DFE Operator's and Parts Manual (4-1977)Document54 pages956-0302 Onan DFE Operator's and Parts Manual (4-1977)appplesNo ratings yet
- Test Bank For The Practice of Statistics in The Life Sciences 4th Edition Brigitte BaldiDocument23 pagesTest Bank For The Practice of Statistics in The Life Sciences 4th Edition Brigitte BaldiDebra Franken100% (31)
- Covalence S1301-M Epoxy Primer: DescriptionDocument4 pagesCovalence S1301-M Epoxy Primer: DescriptionJuan Carlos Contreras CherresNo ratings yet
- Astm C 592Document9 pagesAstm C 592hoseinNo ratings yet
- Discard ManagementDocument9 pagesDiscard ManagementDevvrath SinghNo ratings yet
- Chemistry Project 2021-2022Document19 pagesChemistry Project 2021-2022Rudra SathwaraNo ratings yet
- Taino by The Sea Lunch MenuDocument8 pagesTaino by The Sea Lunch Menuinfo_tainobeach0% (1)
- Capinew Account June13Document7 pagesCapinew Account June13ashwinNo ratings yet