Professional Documents
Culture Documents
Damage - Control - Resus - Quick - Reference - Guide - Medics - Corpsmen - 2023-Quick Reference Guide For Combat Medics and Corpsmen
Damage - Control - Resus - Quick - Reference - Guide - Medics - Corpsmen - 2023-Quick Reference Guide For Combat Medics and Corpsmen
Uploaded by
chou youOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Damage - Control - Resus - Quick - Reference - Guide - Medics - Corpsmen - 2023-Quick Reference Guide For Combat Medics and Corpsmen
Damage - Control - Resus - Quick - Reference - Guide - Medics - Corpsmen - 2023-Quick Reference Guide For Combat Medics and Corpsmen
Uploaded by
chou youCopyright:
Available Formats
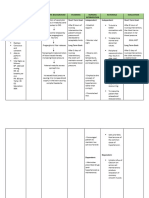
Clinical Practice Guideline
Quick Reference Guide
Update (JTS CPG ID: 18)
Defense Health Agency
for Combat Medics and Corpsmen
This document highlights updates to the Damage Control Resuscitation (DCR) Clinical Practice Guideline.
Goal Updated Guidance Actions
• Triage: Look for severe injury patterns:
Rapid Assessment
proximal, bilateral, or multiple amputations;
penetrating injury to chest/abdomen; pelvic or
To reduce mortality due to junctional hemorrhage, and weak/absent radial
hemorrhage, rapidly recognize the Maintain a target Systolic Blood
Pressure (SBP) for DCR at 100 • pulse. Initiate Rapid Casualty Assessment
Triage /
need for early DCR and initiate Assess for signs of hemorrhagic shock:
early hemorrhage control and blood mmHg (100-110mmHg if TBI is •
presumed) when resuscitating - Altered mental status
transfusion as close to time-of-injury - Cool extremities
as possible. with blood products.
- Delayed capillary refill
- Pulse > 100 bpm
- SBP < 100 mmHg
- Clinical signs of impaired clotting (e.g.,
bleeding from minor wounds)
Hemorrhage
Apply
INFORMATIONAL ONLY: Know that
• tourniquets,
Control
Resuscitative Endovascular Balloon
To stop or reduce hemorrhage
Occlusion of the Aorta (REBOA) is • pressure bandages,
as close to time-of-injury as
possible. now an option for the temporary • hemostatic dressings, and
control of non-compressible torso assist with REBOA if assigned to a
hemorrhage. designated resuscitation team.
Administer pre-hospital DCR fluids from
Resuscitation
most to least preferred:
To treat and reverse hemorrhagic 1. Whole Blood (LTOWB preferred)
shock, provide warm whole blood Prioritize using Low Titer O Whole
Blood (LTOWB) as the fluid of 2. Plasma, platelets, and red blood cells
as close to the time-of-injury as (RBCs) in a 1:1:1 ratio
possible. choice for DCR.
3. Plasma and RBCs in a 1:1 ratio
4. Plasma or RBCs alone
NOTES: Warm fluids to 37°C/98.6°F with approved devices to prevent hypothermia.
Consider transfusion during transport to ensure rapid transfer to a surgical team.
To reduce mortality, fibrinolysis, Consider administering undiluted TXA Administer TXA 2g IV/IO in 100mL NS over
and stabilize clot, administer by slow IV push (over 1 minute) is 1 minute within 3 HOURS of injury
TXA IV/IO within 3 HOURS of acceptable ONLY if supplies or tactical
Pharmacologic Adjuncts
injury for casualties at high risk of situation prevents providing a diluted
hemorrhagic shock. infusion.
NOTES: Rapid TXA IV push may cause hypotension.
Provide IV/IO calcium to all hemorrhagic 1g calcium IV/IO immediately after first blood
To prevent hypocalcemia related shock patients whenever blood unit transfused, then again after every four
to massive transfusion, monitor transfusion occurs during or immediately units.
ionized calcium. Administer calcium after first unit of blood.
early.
NOTES: Calcium gluconate is preferred for peripheral IV administration.
DISCONTINUE USE for DCR: Hydroxyethyl starch (Hextend, Hespan)
* Note: View the full CPG at https://jts.health.mil/index.cfm/PI_CPGs/damage_control. Last updated June 2023.
You might also like
- Mentor Teacher Letter of RecommendationDocument1 pageMentor Teacher Letter of Recommendationapi-311641812100% (3)
- Girl, Interrupted: Overview of The MovieDocument7 pagesGirl, Interrupted: Overview of The MovieJake Yvan DizonNo ratings yet
- Nursing Care Plan For Palliative Care Nursing NotesDocument2 pagesNursing Care Plan For Palliative Care Nursing NotesblaireNo ratings yet
- Drug Study Heparin and FenylDocument4 pagesDrug Study Heparin and FenylAnisa Jamito75% (4)
- Nursing Care Plan For HELLP SyndromeDocument17 pagesNursing Care Plan For HELLP SyndromeRosemarie Carpio75% (4)
- JD Guided Surgery Kit Instruction For UseDocument21 pagesJD Guided Surgery Kit Instruction For UseTeaca DumitruNo ratings yet
- Micro GreensDocument2 pagesMicro GreensVipul Surana67% (3)
- Angiography (Cardiac Catherization) : Patient Teaching/preparationDocument2 pagesAngiography (Cardiac Catherization) : Patient Teaching/preparationpsyNo ratings yet
- NCP HypertensionDocument2 pagesNCP HypertensionJet BautistaNo ratings yet
- CT 11 - HPNDocument12 pagesCT 11 - HPNLycah RotoneNo ratings yet
- ICU One Pager Massive Hemoptysis v11Document1 pageICU One Pager Massive Hemoptysis v11Nicholas HelmstetterNo ratings yet
- Reviewer 112Document18 pagesReviewer 112Andrea GatuzNo ratings yet
- NCP NeuroDocument20 pagesNCP NeuroNica Gaborne Navarro100% (3)
- Tams NCP and DrugDocument5 pagesTams NCP and DrugNicholas Xavier VenturaNo ratings yet
- Ineffective Breathing Pattern Related To Shortness of Breath Possible Evidence by CuesDocument7 pagesIneffective Breathing Pattern Related To Shortness of Breath Possible Evidence by CuesLouie ParillaNo ratings yet
- Vas OpressorDocument41 pagesVas Opressorstevanus handrawanNo ratings yet
- College of Nursing and Allied Medical Sciences: WesleyanDocument3 pagesCollege of Nursing and Allied Medical Sciences: WesleyanMay Anne ManuzonNo ratings yet
- Blood Pressure-For StudentsDocument79 pagesBlood Pressure-For StudentsAshok Kumar P100% (1)
- NEURO2 1.02C Hemorrhagic Stroke - Dr. HiyadanDocument2 pagesNEURO2 1.02C Hemorrhagic Stroke - Dr. HiyadanAra Diocos100% (1)
- Drug Study and NCP OutlineDocument3 pagesDrug Study and NCP Outlinerobertvaliente471No ratings yet
- NCP SGH DianaDocument2 pagesNCP SGH Dianadaniloabautista44No ratings yet
- NCP For HypertensionDocument6 pagesNCP For HypertensionJaic Ealston D. Tampus0% (2)
- Assessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermDocument4 pagesAssessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermGensen Cu RoxasNo ratings yet
- Blood Pressure Regulation MechanismsDocument68 pagesBlood Pressure Regulation MechanismsPhysiology by Dr RaghuveerNo ratings yet
- 12 Internal BleedingDocument40 pages12 Internal BleedingNoval LiadyNo ratings yet
- Fisiologi ShockDocument31 pagesFisiologi Shockdmandatari7327No ratings yet
- NCP - PreeclampsiaDocument3 pagesNCP - PreeclampsiaRap De la Cruz50% (2)
- Hemodynamics CVP Notes FromDocument5 pagesHemodynamics CVP Notes Fromwannawook14No ratings yet
- Icu 4Document7 pagesIcu 4GemilleDaphneAndradaNo ratings yet
- Activity 5Document4 pagesActivity 5AngieNo ratings yet
- NCPGLOVINGDocument3 pagesNCPGLOVINGJoyce MadarangNo ratings yet
- Neuro-Stroke NotesDocument4 pagesNeuro-Stroke NotesanalizaNo ratings yet
- Drug StudyDocument3 pagesDrug Studyunkown userNo ratings yet
- NCP SGHDocument2 pagesNCP SGHdaniloabautista44No ratings yet
- ShockDocument8 pagesShockPIH SHTNo ratings yet
- Drug Study - AmlodipineDocument2 pagesDrug Study - AmlodipineKian HerreraNo ratings yet
- ShockDocument36 pagesShockNoura RihanNo ratings yet
- Guideline For Management of Massive Blood Loss in Trauma UpDocument6 pagesGuideline For Management of Massive Blood Loss in Trauma UpHarmonicgan TengkurNo ratings yet
- Guidelines For The Management of Intracerebral HaemorrhageDocument18 pagesGuidelines For The Management of Intracerebral Haemorrhagerebeca marityNo ratings yet
- Poster SpecCircs Traumatic Cardiac Arrest Algorithm SERB V20160714 HRESDocument1 pagePoster SpecCircs Traumatic Cardiac Arrest Algorithm SERB V20160714 HRESJelena TadićNo ratings yet
- Screenshot 2023-03-23 at 11.04.14 PMDocument1 pageScreenshot 2023-03-23 at 11.04.14 PMRenad AlharbiNo ratings yet
- PositionDocument23 pagesPositionCharlene RojasNo ratings yet
- Algorithm of Resuscitation CareDocument1 pageAlgorithm of Resuscitation CarejyothiNo ratings yet
- Actual NCP Eclampsia - PESCADERO 4CDocument1 pageActual NCP Eclampsia - PESCADERO 4COrlando VillanuevaNo ratings yet
- Acs - 12.01.2022Document41 pagesAcs - 12.01.2022SabariNo ratings yet
- Cardiovascular SystemDocument26 pagesCardiovascular SystemJenny Torreda100% (1)
- Drug Name Brand Name Classification Dosage Indications Side/ Adverse Effects Nursing ResponsibilitiesDocument2 pagesDrug Name Brand Name Classification Dosage Indications Side/ Adverse Effects Nursing ResponsibilitiesRonald BurkeNo ratings yet
- CardioDocument9 pagesCardioKESLING KAB. PANGANDARANNo ratings yet
- Akut Limb IskemikDocument31 pagesAkut Limb IskemikLaluMuhammadSabarSetiawanNo ratings yet
- Shock SepsisDocument8 pagesShock SepsisCeljie OmresoNo ratings yet
- Ineffective Tissue Perfusion Nursing Care PlanDocument1 pageIneffective Tissue Perfusion Nursing Care PlankimmybapkiddingNo ratings yet
- Nursing Care Plan: St. Anthony's College San Jose, Antique Nursing Department Name: M.L.HDocument3 pagesNursing Care Plan: St. Anthony's College San Jose, Antique Nursing Department Name: M.L.HNicolne LorraineNo ratings yet
- NCP Chest PainDocument2 pagesNCP Chest PainCG Patron BamboNo ratings yet
- 01 Cir 0000038923 61628 3DDocument3 pages01 Cir 0000038923 61628 3DGet BetterNo ratings yet
- Dilantin (Phenytoin) : Drug Classification Actions Side Effects ConsiderationsDocument4 pagesDilantin (Phenytoin) : Drug Classification Actions Side Effects ConsiderationsbreehaireNo ratings yet
- Anaphylactic Shock Due To Contrast Dye Allergy HF Due To Left Ventricle Damage and MIDocument3 pagesAnaphylactic Shock Due To Contrast Dye Allergy HF Due To Left Ventricle Damage and MIpsyNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermFrancis Xavier S. MendezNo ratings yet
- Central Venous Pressure 55Document2 pagesCentral Venous Pressure 55Pamipam100% (1)
- UpToDate Key Periods During Cardiac SurgeryDocument5 pagesUpToDate Key Periods During Cardiac SurgeryGaurish SawantNo ratings yet
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument51 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticedrhendyjuniorNo ratings yet
- Jade R. Dinolan BSN-4: Diagnosi SDocument5 pagesJade R. Dinolan BSN-4: Diagnosi SJhade Relleta100% (1)
- Licensed Nurse CheckDocument9 pagesLicensed Nurse CheckBianca MaeNo ratings yet
- 6 Alterations On Tissue Perfusion Poleno Serrano TajalaDocument18 pages6 Alterations On Tissue Perfusion Poleno Serrano TajalaSophia A. GoNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- SHORT - DCR - 5 - 2023-Medical AdministrationDocument1 pageSHORT - DCR - 5 - 2023-Medical Administrationchou youNo ratings yet
- MR1335Document72 pagesMR1335chou youNo ratings yet
- SHORT - DCR - 2 - 2023-Systolic Blood Pressure ControlDocument1 pageSHORT - DCR - 2 - 2023-Systolic Blood Pressure Controlchou youNo ratings yet
- The Symbiotic Relationship Between Operational MilDocument6 pagesThe Symbiotic Relationship Between Operational Milchou youNo ratings yet
- Medical Echelon of Care Conceptual Models For Wargaming - SBIR - GovDocument4 pagesMedical Echelon of Care Conceptual Models For Wargaming - SBIR - Govchou youNo ratings yet
- 2021 11CRS新兴军事技术R46458Document37 pages2021 11CRS新兴军事技术R46458chou youNo ratings yet
- 2020 - 04 - 01 - nasa - hdbk - 1004 - approved-NASA 数字工程采办框架手册Document217 pages2020 - 04 - 01 - nasa - hdbk - 1004 - approved-NASA 数字工程采办框架手册chou youNo ratings yet
- 246 Hause Hart-基于模型的采集Document25 pages246 Hause Hart-基于模型的采集chou youNo ratings yet
- NAVSEA 0905 LP 120 0010 Technical Manual For DSRV SystemDocument135 pagesNAVSEA 0905 LP 120 0010 Technical Manual For DSRV Systemchou youNo ratings yet
- J-11 8010 Manual ACN-3-ADocument198 pagesJ-11 8010 Manual ACN-3-Achou youNo ratings yet
- Dokumen - Tips - Us Navy Ship Salvage Manual Volume 6 Oil Spill Response 2016 02 18 Us NavyDocument251 pagesDokumen - Tips - Us Navy Ship Salvage Manual Volume 6 Oil Spill Response 2016 02 18 Us Navychou youNo ratings yet
- Dokumen - Tips - Pdfus Navy Salvage Manual Volume 2 Pol Docsus Navy Salvage Manual VolumeDocument148 pagesDokumen - Tips - Pdfus Navy Salvage Manual Volume 2 Pol Docsus Navy Salvage Manual Volumechou youNo ratings yet
- 800m Training PlansDocument6 pages800m Training PlansWalcyr GuilhermeNo ratings yet
- Developing A Civic Action Plan WorksheetDocument3 pagesDeveloping A Civic Action Plan WorksheetMirella CostaNo ratings yet
- Update On The Management of Symptoms in Schizophrenia: Focus On AmisulprideDocument11 pagesUpdate On The Management of Symptoms in Schizophrenia: Focus On AmisulpridepaulNo ratings yet
- Med Sci PostDocument122 pagesMed Sci PostTyeana CampbellNo ratings yet
- Menopause - RajonivrittiDocument13 pagesMenopause - RajonivrittiSivaram Shanmugha VilasNo ratings yet
- Research Proposal FinalDocument6 pagesResearch Proposal Finalapi-408377873No ratings yet
- Weber, J. and Kelley, J. (2018) Health Assessment in Nursing. Sixth EditionDocument5 pagesWeber, J. and Kelley, J. (2018) Health Assessment in Nursing. Sixth EditionKi TzNo ratings yet
- BWS - Ultimate Pull-Ups GuideDocument17 pagesBWS - Ultimate Pull-Ups GuideDebabrata BanerjeeNo ratings yet
- ADHD Dari KaplanDocument25 pagesADHD Dari KaplanAldo D'vatho MpNo ratings yet
- Clinebell Howard J., Jr. - The Mental Health Ministry of The Local ChurchDocument211 pagesClinebell Howard J., Jr. - The Mental Health Ministry of The Local ChurchGuilherme EmilioNo ratings yet
- Decent Work Employment Transcultural Nursing SAS Session 6Document10 pagesDecent Work Employment Transcultural Nursing SAS Session 6King NavsunNo ratings yet
- Calvary Public Bruce Campus MapDocument2 pagesCalvary Public Bruce Campus MapAlana TindaleNo ratings yet
- Comparing The Effectiveness of Gottman and Dattilio Regulacion EmocionalDocument24 pagesComparing The Effectiveness of Gottman and Dattilio Regulacion EmocionalLicMarinaGarayNo ratings yet
- Calf Rumen DevelopmentDocument5 pagesCalf Rumen DevelopmentWaqas NawazNo ratings yet
- Unseen Impact of Online Gambling To National Integration of The Unitary State of Republic Indonesia - Khayriz Zafran NandikaDocument5 pagesUnseen Impact of Online Gambling To National Integration of The Unitary State of Republic Indonesia - Khayriz Zafran NandikaKhayriz Zafran NandikaNo ratings yet
- II. Task 2: Write An Analytical Exposition TextDocument2 pagesII. Task 2: Write An Analytical Exposition TextYunika VandiaNo ratings yet
- Awareness of Tooth Replacement Options Among Adult PopulationDocument39 pagesAwareness of Tooth Replacement Options Among Adult PopulationFatima GaladimaNo ratings yet
- Examining The Oral Health of Filipinos: Policy Analysis: Original ArticleDocument7 pagesExamining The Oral Health of Filipinos: Policy Analysis: Original ArticleTimothy LimaNo ratings yet
- Methyl MercaptideDocument5 pagesMethyl MercaptideNicol AlejandraNo ratings yet
- Sr. # Product Name Unit Price QTY Amount RemarksDocument1 pageSr. # Product Name Unit Price QTY Amount RemarksaliNo ratings yet
- Test Bank For Gerontological Nursing 8th Edition Charlotte Eliopoulos DownloadDocument18 pagesTest Bank For Gerontological Nursing 8th Edition Charlotte Eliopoulos Downloaddillonmillerjasqrpgnez100% (34)
- Life of A Single MomDocument2 pagesLife of A Single MomBSAScitiNo ratings yet
- SDS en-MY 20220501Document13 pagesSDS en-MY 20220501MUHAMMAD AMIR BIN RASIDNo ratings yet
- Newground Safety Tool Box Talks: DermatitisDocument2 pagesNewground Safety Tool Box Talks: Dermatitisابو محمد عليNo ratings yet
- Punctuation Worksheet 2Document6 pagesPunctuation Worksheet 2mukizaromain2020No ratings yet
- Racism Essay Thesis StatementDocument5 pagesRacism Essay Thesis Statementjfepyntgg100% (2)