Professional Documents
Culture Documents
Maternal Outcomes of Severe Preeclampsia Eclampsia and Associated Factorsamong Mothers Admitted in Referral Hospitals N
Maternal Outcomes of Severe Preeclampsia Eclampsia and Associated Factorsamong Mothers Admitted in Referral Hospitals N
Uploaded by
talilaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maternal Outcomes of Severe Preeclampsia Eclampsia and Associated Factorsamong Mothers Admitted in Referral Hospitals N
Maternal Outcomes of Severe Preeclampsia Eclampsia and Associated Factorsamong Mothers Admitted in Referral Hospitals N
Uploaded by
talilaCopyright:
Available Formats
Clinics in Mother & Child Health Research Article
Maternal Outcomes of Severe Preeclampsia / Eclampsia and Associated Factors
among Mothers Admitted in Referral Hospitals, North West Ethiopian Context,
2018
Misganaw Fikirie Melese1, Getie Lake Aynalem2*, Marta Berta Badi2
1Department of Midwifery, Debre Markos University, Debre Markos City, Ethiopia
2School of Midwifery, College of Medicine and Health Science, University of Gondar, Gondar City, Ethiopia
ABSTRACT
Objective
Severe preeclampsia/eclampsia is a multi-systemic disorder of pregnancy occurring after 20 weeks of gestation
associated with significant maternal morbidity and mortality worldwide. The study`s objective was to assess factors
associated with unfavorable maternal outcomes of severe preeclampsia/eclampsia, North West Ethiopian context,
2018.
Methods
Institutional based cross-sectional study was conducted among severe preeclamptic/Eclamptic mothers admitted in
Amhara regional state referral Hospitals, Northern part of Ethiopia, 2018. All severe preeclamptic/Eclamptic mothers
available during the data collection period were included as a census sampling technique. Bivariate and multivariate
logistic regression model was employed. Variables with P-Value <0.05 at 95% CI level was taken as statistically
significant. Data were collected with pre-tested and semi-structured questionnaire, entered into Epi-info and exported
to SPSS for analysis.
Results
The study shows that the overall unfavorable maternal outcomes of severe preeclampsia/eclampsia were found to be
37.7% which is tragically high when compared with different previous study findings mentioned in the discussion
section. Variables which were positively associated with unfavorable maternal outcomes were: Maternal educational
status (AOR= 4.5, 95% CI: 1.95, 12.31), Residence (AOR= 2.1, 95% CI: 1.17, 3.72), Monthly family income (AOR=
2.7 95% CI: 1.25, 6.12), Parity (AOR= 6.7, 95% CI: 1.55, 12.6), History of abortion perceived (AOR= 3.5, 95% CI:
1.63, 7.58), Booking status (AOR= 5.8, 95% CI: 3.15, 9.72) and Time of drug given (AOR= 4.9, 95% CI: 1.86,
13.22).
Conclusion and Recommendation
This study revealed that the overall unfavorable maternal outcomes of severe preeclampsia and eclampsia are found to
be relatively high in Amhara regional state referral hospitals. Improving booking status of pregnant women and
timely providing appropriate drugs for severe pre-eclamptic/eclamptic mothers may reduce unfavorable outcomes.
Correspondence to: Getie Lake Aynalem, School of Midwifery, College of Medicine and Health Science, University of Gondar, Gondar City,
Ethiopia, Tel: 251920469610; E-mail: getie.lake@yahoo.com
Received: August 30, 2021; Accepted: August 24, 2021; Published: September 03, 2021
Citation: Aynalem GL (2021) Maternal Outcomes of Severe Preeclampsia / Eclampsia and Associated Factors among Mothers Admitted in Referral
Hospitals, North West Ethiopian Context, 2018. Clinics Mother Child Health. 18:p436.
Copyright: © 2021 Aynalem GL. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 1
Aynalem GL
Introduction September 30, 2018. This region has a total catchment area
population of 17,221,976 of whom 8,641,580 were men and
Preeclampsia is a pregnancy specific syndrome that can affect 8,580,396 women and from which urban inhabitants account
every organ system .It usually occurs after 20weeks of gestation 2,112,595(12.27%) of the population (23). This regional state
and can be diagnosed in the absence of proteinuria if there is has 67 Hospitals, 839 health centers, and 3336 health posts;
evidence of new hypertension and multi-organ involvement(1, among them 5 are Referral Hospitals which include University
2). of Gondar Teaching Referral Hospital, Felege Hiwot Referral
Severe PE is diagnosed when one or more of the following Hospital, Dessie referral Hospital, Debremarkos Referral
criteria are present: Systolic/diastolic blood pressure ≥160/110 Hospital, and Debrebirhan Referral Hospital. Each Hospital is
mm Hg, thrombocytopenia, renal insufficiency, impaired liver assumed to be serving for about 5 million catchment
function, pulmonary edema or visual loss or cerebral populations, have 200-400 beds, 2000-4000 deliveries per year
disturbance (3, 34). and 5-10 deliveries per day (24, 25, 34).
Hypertension was the second most common direct cause of Sample Size Determination and Sampling
maternal death worldwide, an estimated 303,000 maternal
Procedures
death occur globally from which hypertension accounts 14%. In
developed countries, maternal mortality from hypertension is Sampling was done based on the 2017 severe preeclampsia/
relatively rare (12.9%), however, in developing region where Eclampsia case flows in each study Hospitals. Here were the case
approximately 99% of all maternal death occurs, hypertension flows in 2017 six months prior to the data collection: Dessie
accounts 14% of it and also in sub-Saharan Africa including Referral Hospital 102, Debre-Markos referral Hospital 138 and
Ethiopia, it accounts 16% maternal death (3, 4). Felege-Hiwot 174 cases of the study (34). The sample size we
used was the total cases of the three referral Hospitals which was
Worldwide, Preeclampsia affects 8-10% of pregnancies and is a
totaled as 414 we added a 10% expected non-response rate
common cause of preterm delivery and also it accounts 20% of
which became 456. We used census to get enough sample size
all neonatal intensive care admissions. In Africa and Asia, it
and we have gone with data collection until our sample size was
accounts 10% of maternal death(5). The Ethiopian National
saturated from each of the Referral Hospitals according to their
Emergency Obstetric and Newborn Care review (EMONC)
case flows.
showed that preeclampsia/eclampsia is the second most
common cause of maternal morbidity and third leading cause of
maternal mortality (12). It affects 5.47% of pregnancy (6) and Operational Definitions
severe preeclampsia or eclampsia accounts 10% of maternal Severe preeclampsia: is a preeclampsia with one of the severity
mortality(7). signs (Blood pressure 160/110 or more, severe headache,
A study conducted in Jimma University Hospital, Ethiopia pulmonary edema, epigastric pain, renal insufficiency,
showed that pregnancy induced thrombocytopenia, blurring of vision and increased liver
enzymes) that occurs at any gestational age after 20 weeks of
Hypertension (20%) was the second leading cause of maternal pregnancy.
death next to hemorrhage (54%) (13)
Maternal complication: complication of the mother due to
The Government of Ethiopia in line with WHO and other severe preeclampsia including Abruptio placenta, HELLP
nongovernmental organizations takes a commitment to reduce syndrome, Acute renal failure, DIC, Pulmonary edema, Death,
maternal mortality through multiple high impact interventions eclampsia, PPH, aspiration pneumonia(1).
at both facility and community levels to remove bottlenecks such
as harmful traditional practices, poor infrastructure, shortage of Favorable maternal outcome: patient with severe preeclampsia
transportation facilities and inadequate care at health facilities remote from term who managed and improved without any
that can hamper access to safe motherhood services(14). complication(19).
Even though, different health sectors and funding agencies Unfavorable maternal outcome: patient with severe
devoted a lot to reduce maternal deaths due to severe preeclampsia remote from term that develops at least one
preeclampsia/eclampsia is still increasing worldwide (7,13, 15). complication (19).
This study, therefore, was conducted to determine the outcomes Data Collection Procedures and Instrumentations
of severe preeclampsia/Eclampsia by incorporating time of drug
initiation in addition to the variables of the previous studies Data were collected using semi-structured questionnaire adapted
used. from similar literatures. The questionnaire was first developed
in English and translated to local language, Amharic version
METHODS then back to English by language experts to keep its consistency.
Data collection was done by two data collectors and one
supervisor for each hospital. The data collectors were BSC
Study Design and Setting Midwives with previous experiences from nearby health centers
An institution based cross-sectional study was conducted in and the supervisors were MSc Midwives from respective Referral
Referral Hospitals of Amhara Regional State from, April 1 to Hospitals.
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 2
Aynalem GL
Data Quality Control Orthodox 347 76.1
Semi-structured data collection tool was utilized and clarity of
Muslim 101 22.2
the tool was tested before the final utilization. The pretest was
conducted among 5% of the sample size in Debre Berhan Protestant 7 1.5
referral Hospital. A one day training was given for data
collectors and supervisors regarding the objectives of the study, Catholic 1 0.2
data collection method and significance of the study. During
data collection each data collector was supervised for any Marital Status
difficulties and directions and necessary corrections were
provided. Married 429 94.1
Single 20 4.4
Data Processing and Analysis
All collected data were rechecked for completeness and coded. Divorced 4 0.9
Then these data were entered using Epi Info 7.2 software, and
exported to SPSS version 23 for cleaning and analysis. Bivariate Widowed 3 0.7
logistic regression was employed to identify association, and
Educational status
multivariate logistic regression model was used to control the
effect of confounders and identify independent predictors. Unable to read and 193 42.3
Variables having P-value less than 0.2 in the bivariate analysis write
were fitted into the multivariable logistic regression model. 95%
confidence interval of odds ratio was computed and variables Able to read and 38 8.3
write
having P-value less than 0.05 in the multivariate logistic
regression analysis was considered to declare statistical Elementary school 56 12.3
significant. Before the actual logistic regression analysis was
done, the necessary assumption of logistic regression model was Secondary school 71 15.6
checked by using Hosmer-Lemeshow test of goodness of fit
which has a chi-square distribution (P-values > 0.05 was College and above 98 21.5
considered as good model fit).
Occupational status
For further analysis, descriptive statistics like frequencies and
cross tabulation was performed. Graphical presentation such as Unemployed 16 3.5
bar graph, tables and pie charts were used to present the result
of the study. Housewife 281 61.6
RESULTS private worker 76 16.7
governmental worker 66 14.5
Socio-Demographic Results
NGO 6 1.3
A total of 456 cases were included in this study with 100%
response rate. The mean age of the participants was 28.3 (SD Student 11 2.4
±6.5) years. Among these cases, two hundred forty three (53.3%)
were preeclamptic with severity features (Table 1). Residence
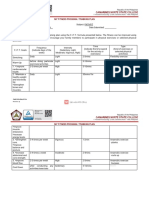
Table 1: Socio-demographic characteristics of women with
Urban 235 51.5
severe preeclampsia / Eclampsia admitted in Amhara regional
state Referral Hospitals, North West Ethiopia, 2018 (n= 456). Rural 221 48.5
Variable Frequency Percent Traditional treatment
use
Maternal age
Yes 268 58.8
Age ≤19 33 7.3
No 188 41.2
Age 20-35 349 76.5
Monthly Family
Age ≥36 74 16.2 income
Religion
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 3
Aynalem GL
Income< 70.2 USA 226 49.6 NB: Total percentage may be more than 100% because they are
dollars not mutually exclusive
Income 70.2-120.9 95 20.8 Time of Treatment And Drugs Given
USA dollars
More than half, 267 (58.6%) of the participants had received
Income>120.9 USA 135 29.6 medications after they developed complications whereas,
dollars 181(41.4%) received as soon as severe preeclampsia/
eclampsia was diagnosed.
Obstetrics Characteristics Magnesium sulfate and Methyl dopa were the most
Two hundred sixty one (57.2%) participants reported that they frequently administered anti-convulsing and anti-
had more than one history of deliveries. Median gestational age hypertensive, drugs administered for 431 (94.5%) and 395
was 38 weeks, which ranged from 21 to 43 weeks. Around 225 (86.6%) respondents respectively.
(49.4%) respondents` gestational age was found to be between
37-40 weeks. 315 (69.1%) respondents had ANC follow up, 346 Variables Associated with Maternal Outcomes of
(75.9%) had no history of abortion, 292 (64%) with severe Severe Preeclampsia/Eclampsia
preeclampsia and eclampsia were unbooked in the Referral
Hospitals of Amhara regional state. Among the study In crudes analysis: Maternal educational status, Residence,
participants: - One hundred seventy two (37.7%), one hundred Monthly family income, Parity, History of abortion perceived,
thirty six (29.8%) and one hundred twenty seven (27.9%) gave Booking status and Time of drug given were significantly
birth through the vagina after initiation, SVD and C/S associated.
respectively. In adjusted analysis: Maternal educational status, Residence,
Monthly family income, Parity, History of abortion perceived,
Maternal Outcome of Severe Preeclampsia/ Booking status and Time of drug given were the predictor
Eclampsia variables (Table 3).
From the total of 456 respondents admitted in Amhara region Table 3: Both bivariate and multivariate analysis table on the
referral Hospitals for severe preeclampsia and eclampsia factors associated with severe preeclampsia/Eclampsia among
management, one hundred seventy two (37.7%) of them end up mothers admitted in Amhara regional state Referral Hospitals,
with unfavorable outcome (Table 2). North West Ethiopia, 2018 (n= 456).
Table 2: Multiple response analysis showing maternal outcomes
of severe preeclampsia and eclampsia among mothers admitted Variables Maternal outcomes COR (95% AOR (95%
in Amhara Regional state Referral Hospitals, North West CI) CI)
Ethiopia, 2018 (n=456). Unfavorable Favorable
Maternal Favorable 284 (62.3%) Maternal
outcomes:- Age
Unfavorable 172(37.7%)
Age≤19 27 6 3.6(1.33,9.8 3.9(0.52,29.
0)* 47)
Types of unfavorable outcomes Frequency Percent
(n=172)
Age 20-35 104 245 0.3(0.20,0.5 1.5(0.37,5.6
7)** 7)
Abruptio placenta 47 27.3
Age≥36 41 33 1 1
HEELPS Syndrome 68 39.5
Educational
DIC 31 18.0
Status
Acute renal failure 95 55.2
Unable to 96 97 6.5(3.38,12. 4.5
read &write 37)** (1.95,12.31)*
PPH 98 56.9
Read & 16 21 5.0(2.07,11. 4.3
Aspiration pneumonia 92 53.4
write 93)** (1.57,11.85)
Pulmonary embolism 3 1.7
Elementary 24 34 4.6(2.10,10.1 4.0
school 0)** (1.53,10.76)
Pulmonary edema 9 5.2
Secondary 23 47 3.2(1.48,6.8 1.9(0.72,5.1
Death 1 0.5
school 9)* 4)
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 4
Aynalem GL
College & 13 85 1 1 When did
above the drug
given
Residence
Late 146 121 7.6(4.68,12. 5.0
Rural 127 93 5.8(3.80,8.8 2.1(1.17,3.7 21)** (1.86,13.22
2)** 2)* )*
Urban 45 191 1 1 Early 26 163 1 1
Monthly
Key:**=p-value<0.001, *=
Family
income value<0.05, 1=Reference
Income 112 114 7.3(4.07,13. 2.8
<70.2 USA 09)** (1.25,6.12)* Discussion
dollars The study has assessed the maternal outcomes of severe pre-
eclampsia/eclampsia and associated factors among the admitted
Income 44 51 6.4(3.31,12. 2.7
from 40)** (1.14,6.46)*
women, North West Ethiopian context. The result shows that
70.2-120.9 out of 456 total cases of severe preeclampsia and eclampsia, one
dollars hundred seventy two (37.7%) ended up with unfavorable
maternal outcomes which is in line with a study done in Addis
Income 16 119 1 1 Ababa (36%), Ethiopia (21) but lower than a study done in
>120.9 USA India (59%) (17). It could be due to the health care set up
dollars difference.
Gravidity There was only one maternal death (0.5%) which is lower than
studies conducted in
Premigravid 76 77 2.1(1.42,3.1 1.9(0.43,8.3
a 7)** 0)
Debre Berhan Referral Hospital (2.5%) (22), India (11.2%) (17)
and Haiti (1.9%) (18).
Multigravid 96 207 1 1 The reason for this difference might be: the time gap as time
a goes on: health care seeking behavior, access to health
institutions and drugs, quality for professionals are likely to
Parity
increase by which each can contribute for death reduction.
Nully para 50 20 6.5(3.64,11. 6.7(1.55,12. In this study sixty eight (39.5%) respondents developed HEELPs
73)** 6)* syndrome which is lower than the study done in Addis Ababa,
Ethiopia (63.96%) (15) and Tanzania
Premipara 49 73 1.8(1.11-2.7 1.7(0.72,3.9
5)* 4) (50.9%) (27). But this finding was higher than the study done in
Mettu Karl Referral Hospital, Ethiopia (12.4%) (28) and Iran
Multipara 73 191 1 1 (4.9%) (29). It could be due to the health care system
differences.
History of
Abortion Maternal educational status was one of the predictor variables
for severe preeclampsia/Eclampsia outcomes. Women who were
Yes 70 41 4.1(3.06,8.0 3.5 unable to read/write were more likely to develop unfavorable
2)** (1.63,7.58)* maternal outcomes of severe pre-eclampsia/eclampsia when
compared with women whose educational statuses were college
No 102 243 1 1 and above (AOR=4.5, 95% CI: 1.95, 12.31). This finding is
supported by other studies done in South East Nigeria (30) and
Booking
Status
Bangladesh (31). It could be due to the fact that uneducated
people`s health care seeking behavior is poor.
Unbooked 146 146 5.2(3.23,8.5 5.8(3.15,9.7 Maternal residence was another positively associated variable.
5)** 2)* The rural women were more likely to develop adverse severe
preeclampsia and eclampsia maternal outcomes than their
Booked 26 136 1 1
counterparts (AOR=2.1, 95% CI: 1.17, 3.72). This is in
agreement with studies done in Jimma university Hospital,
Ethiopia (32), South East Nigeria (30) and India (19). The
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 5
Aynalem GL
possible reason could be due to the fact that urban women and Low Platelet, AOR: Adjusted Odds Ratio, CI: Confidence
could early and easily access the health institutions. Interval. DIC: Disseminated Intravascular Coagulation
Monthly family income was also the other predictor variable for
the response variable. Women whose family monthly income Ethical Approval and Consent for to Participate
was less 70.2 USA dollars were more likely to develop the Ethical clearance letter was obtained from the Ethical Review
unfavorable outcome when compared with women whose Committee of Institution Review Board of the University of
monthly family income was greater than 120.9 USA dollars Gondar.
(AOR= 2.8, 95% CI: 1.25, 6.12) and Respondents whose
monthly family income was between 70.2-120.9 USA dollars Region Referral Hospitals and permission of each Hospital was
were also more likely to develop the adverse severe obtained from Hospital administrative. Written permission
preeclampsia/Eclampsia outcomes compared with those whose letter was also received from Hospital managers and ward
monthly family income was greater than 120.9 USA dollars. coordinators in the study set up.
(AOR=2.7, 95% CI: 1.14, 6.46). This finding is similar with Again before the data collection, written informed consent was
other studies conducted in Bangladesh (31) and India (19). It obtained from the study participants. The purpose of the study
could be due to those whose family income was poor might be was briefly explained to the mothers independently prior to data
late for the health institutions due to transportation cost. collection and they were informed that their participation would
Parity was an additional predictor variable. Women who did not purely voluntary with secured confidentiality. Study participants
have previous delivery were more likely to develop unfavorable were also informed that they had full right not to participate in
outcomes when compared with the multiparas women or withdraw from the study and the quality of care which they
(AOR=6.7, 95%CI: 1.55, 12.6). This finding is in agreement would get would not be affected because of their withdrawal.
with studies done in South East Nigeria and Pakistan (30, 33). It There was no any participant under 18 years old.
could be due to the fact that nully para women`s labour and
placenta deliveries are usually a little bit longer than the multi REFERENCE
para ones and there are supported theories which suggest that
the stem of preeclampsia/Eclampsia is placenta. So, the longer 1. Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS,
Hoffman BL, et al. williams obstetrics. 24th edition. New York
the placenta stayed inside, the higher the complication is likely.
Chicago San Francisco Lisbon London Madrid Mexico City Milan
History of abortion perceived has also been positively associated New Delhi San Juan Seoul Singapore Sydney Toronto: McGraw-Hill
with severe preeclampsia/Eclampsia outcomes. Women who had Education. 2014;30:729.
history of abortion perceived were more likely to develop 2. American, College, of, Obstetricians, Gynecologiste a. hypertension in
unfavorable outcomes than the counterparts (AOR=3.5, 95%CI: pregnancy: American College of Obstetricians and Gynecologiste
1.63, 7.58). This finding is in agreement with the studies done women's health care physicians. 2013;13-20.
in India and Iran (19, 29). 3. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al.
The possible explanation is that abortion may lead to abnormal Global causes of maternal death: a WHO systematic analysis. The
placentation and release of placental factors that contribute to Lancet Global Health. 2014;2(6):e323-e33.
systemic endothelial dysfunction for the next pregnancy that 4. WHO, UNICEF. Trends in maternal mortality: 1990-2015:
might maximize the occurrence of unfavorable outcomes. estimates from WHO, UNICEF, UNFPA, World Bank
Group and the United Nations Population Division. 2015.
Unbooking (not registered) in the referral Hospitals has also
predicted the severe preeclampsia/Eclampsia outcomes. Those 5. Tsigas E. Reducing Preventable Deaths from Preeclampsia.
who were un-booked were more likely to develop the At the harvard Chan School center of excellenc in maternal
unfavorable outcomes when compared with the booked ones and child health. 2017;5.
(AOR=5.8, CI: 3.15, 9.72). This finding is supported by the 6. Pauli M, aimey M, Repke M, John T. Preeclampsia Short-term and
study conducted in South East Nigeria (30). It could be due to Long-term Implications. Obstet Gynecol Clin N Am. 2015;
the fact that the un-booked ones might be delayed for the early 42:299-313.
treatment and complications could be likely to be developed. 7. Phipps E, Prasanna D, Brima W, Jim B. Preeclampsia:
Updates in Pathogenesis, Definitions, and Guidelines.
Late administration of the appropriate drugs has positively been CJASN ePress. April 19, 2016.
associated with the response variable. Women who were
8. WHO. Trends in maternal mortality: 1990 to 2015, WHO,
provided appropriate drugs lately were more likely to develop
UNICEF, UNFPA, World Bank Group and the United
than their counterparts (AOR=5.0, CI: 1.86, 13.22). It could be
Nations Population Division. 2015.
due to the fact that the unfavorable outcomes could be
prevented if treated early. 9. Alan H. DeCherney M, Lauren Nathan M, T. Murphy
Goodwin M, Neri Laufer M. Current Diagnosis &
Limitation of the study: There might be long term Treatment Obstetrics & Gynecology. 10 ed. USA: McGraw-
complications of severe preeclampsia/Eclampsia for the mother Hill Companies, Inc; 2007.
which our study did not address. 10. Liabsuetrakul T, Thida T. Geographical Distribution of Hypertensive
Abbreviations: SVD: Spontaneous Vaginal Delivery, C/S: Disorders in Pregnancy and their Adverse Maternal and Perinatal
Caesarean Section, HEELP: Hemolysis, Elevated Liver enzymes
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 6
Aynalem GL
Outcomes in Thailand. International Journal of Pregnancy & Child DEBRE BERHAN REFERRAL HOSPITAL, NORTH
Birth. 2017; 2(2). SHOA, AMHARA REGION. Ethiop Med J. 2015;2.
11. Arun Jeyabalan M. Epidemiology of preeclampsia: Impact 23. FDRoEPC C. Summary and statistical report of the 2007
of obesity. NIH Public Access. 2013; 71(01).19 population and housing census–population size by age and
12. Federal Ministry of Health. Ethiopia EmONC. Addis sex. Addis Ababa. 2008.
Ababa, Ethiopia: Ethiopian Public Health Institute, 2016. 24. FMOH. Health Care Financing Reform in Ethiopia:
Tegene Legesse, Misra Abdulahi, Dirar A. Trends and Improving Quality and Equity. 2015.
causes of maternal mortality in Jimma University 25. FDRE.Ministry of Health. Health Sector Development
Specialized Hospital. International Journal of Women’s Programme IV. 2015. WageIndicator.org. Ethiopia - Living
Health. 2017. Wage series January 2018.
13. IFOR A. Ministry of Health POLICY AND PRACTICE 26. Edgar M Ndaboine, Albert Kihunrwa, Richard Rumanyika,
INFORMATION FOR ACTION. Addis Ababa, Ethiopia: H Beatrice Im, Massinde AN. Maternal and Perinatal
Federal Ministry of Health; 2014. Outcomes among Eclamptic Patients Admitted to Bugando
14. Maereg Wagnew, Dessalegn M. Trend of Preeclampsia / Medical Centre, Mwanza, Tanzania. African Journal of
Eclampsia, Maternal and Neonatal Outcomes Among Reproductive Health March. 2012;16(1):35.
Women Delivering in Government Hospitals, Addis Ababa, 27. Seyom E, Abera M, Tesfaye M, Fentahun N. Maternal and
Ethiopia. Amref Health Africa. 2018. fetal outcome of pregnancy related hypertension in Mettu
15. Gaym A, Bailey P, Pearson L, Admasu K, Gebrehiwot Y, Karl Referral Hospital, Ethiopia. Journal of ovarian
Ethiopian National Em ONCAT. Disease burden due to research. 2015;8:10.
pre-eclampsia/eclampsia and the Ethiopian health system's 28. Khosravi S, Dabiran S, Lotfi M, Asnavandy M. Prevalence
response. Int J Gynaecol Obstet. 2011;115(1):112-116. of Hypertension and Complications of Hypertensive
16. Neha Saxena*, Amarjeet Kaur Bava, Nandanwar Y. Disorders in Pregnancy. Open Journal of Preventive
Maternal and perinatal outcome in severe preeclampsia and Medicine. 2014(4):860-7.
eclampsia. Int J Reprod Contracept Obstet Gynecol. 2016; 29. Ajah LO. The Feto-Maternal Outcome of Preeclampsia with
5(7):2171-6. Severe Features and Eclampsia in Abakaliki, South-East
17. Raghuraman N, March MI, Hacker MR, Modest AM, Nigeria. Journal of Clinical and Diagnostic Research. 2016.
Wenger J, Narcisse R, et al. 30. Sarker S A, Nazma S, Most L B, Lobaba S L, Md F A, H
18. Adverse maternal and fetal outcomes and deaths related to MK. Pregnancy Induced
preeclampsia and eclampsia in Haiti. Pregnancy 31. Hypertension and Associated Factors among Pregnant
hypertension. 2014;4(4):279-286. Women. J Gynecol Women’s Health. 2017;3(4):21
19. Sutapa Agrawal, Gagandeep K. Walia, Eleonora Staines- 32. Zenebe W, Hailemariam Segni, Woldie M.
Urias ea. Prevalence of and risk factors for eclampsia in HYPERTENSIVE DISORDERS OF
pregnant women in India. Family Medicine and 33. PREGNANCY IN JIMMA UNIVERSITY SPECIALIZED
Community Health. 2017;5(4):225-244. HOSPITAL. Ethiop J Health Sci. 2011;21(3).
20. Guerrier G, Oluyide, Keramarou, Grais R. Factors 34. Shamsi U, Saleem S, Nishtar N. Epidemiology and risk
associated with severe preeclampsia and eclampsia in Jahun, factors of preeclampsia; an overview of observational
Nigeria. International Journal of Women's Health. studies. Al Ameen J Med Sci. 2013;6:29-30
2013:509. 35. Seyedeh Hajar Sharami, Manoush Zendehdel, Mirblouk F,
21. Maereg Wagnew, Muluken Dessalegn, Alemayehu Worku, MaryamAsgharnia. Comparison of Preeclampsia Risk
Nyagero J. Trends of preeclampsia/eclampsia and maternal Factors Regarding to Severity with Control Group. Zahedan
and neonatal outcomes among women delivering in addis J Res Med Sci. 2017; 1(5008).
ababa selected government hospitals, Ethiopia. Pan African 36. Melese et al. Perinatal outcomes of severe preeclampsia/
Medical Journal. 2016;25(2):12-20 eclampsia and associated factors among mothers admitted
22. Wubanchi Terefe, Yeneneh Getachew, Abiy Hiruye, Miliard in Amhara Region referral hospitals, North West Ethiopia,
Derbew, Damen Haile Mariam, Dereje Mammo, et al. BMC Res Notes. 2019;12:147.
PATTERNS OF HYPERTENSIVE DISORDERS OF
PREGNANCY AND ASSOCI-ATED FACTORS AT
Clinics Mother Child Health, Vol.18 Iss.8 No:1000p436 7
You might also like
- 758ea1d4-f2d2-4b49-8ea1-d6a97ebdea6fDocument22 pages758ea1d4-f2d2-4b49-8ea1-d6a97ebdea6fAmsalu ShitaNo ratings yet
- Jurnal PEDocument7 pagesJurnal PEIris BerlianNo ratings yet
- MJMU Volume 50 Issue 4 Pages 155-163-1Document9 pagesMJMU Volume 50 Issue 4 Pages 155-163-1Fred OkelloNo ratings yet
- Maternal and Perinatal Complications of Severe Preeclampsia in Three Referral Hospitals in Yaoundé, CameroonDocument8 pagesMaternal and Perinatal Complications of Severe Preeclampsia in Three Referral Hospitals in Yaoundé, CameroonIke Istofani KNo ratings yet
- BMC Pediatrics PregnancyDocument8 pagesBMC Pediatrics PregnancyMobin Ur Rehman KhanNo ratings yet
- Maternal and Fetal Outcomes in Term Premature Rupture of MembraneDocument6 pagesMaternal and Fetal Outcomes in Term Premature Rupture of MembraneMuhammad Fikri RidhaNo ratings yet
- An Overview of Referral Patients With Severe Preeclampsia in Obstetric and Gynecology Department, Dr. Soetomo Hospital Surabaya in 2011 An OverviewDocument10 pagesAn Overview of Referral Patients With Severe Preeclampsia in Obstetric and Gynecology Department, Dr. Soetomo Hospital Surabaya in 2011 An OverviewAnonymous y6NmP9NHkYNo ratings yet
- Determinants of Pregnancy-Induced Hypertension OnDocument16 pagesDeterminants of Pregnancy-Induced Hypertension Onsanju.sharma3febNo ratings yet
- The Prevalence of Thrombocytopenia and The Associated Factors Among Pregnant Women in Hoima Regional Referral Hospital, Western Uganda.Document11 pagesThe Prevalence of Thrombocytopenia and The Associated Factors Among Pregnant Women in Hoima Regional Referral Hospital, Western Uganda.KIU PUBLICATION AND EXTENSIONNo ratings yet
- Nakimuli2016 Article TheBurdenOfMaternalMorbidityAnDocument8 pagesNakimuli2016 Article TheBurdenOfMaternalMorbidityAnPriscilla AdetiNo ratings yet
- Feto-Maternal Outcomes in Hypertensive Disorders of Pregnancy in A Tertiary Care Hospital: A Retrospective StudyDocument7 pagesFeto-Maternal Outcomes in Hypertensive Disorders of Pregnancy in A Tertiary Care Hospital: A Retrospective StudyIJAR JOURNALNo ratings yet
- Anemia Prevalence, Severity Level and Its Predictors Among Antenatal Care Attending Pregnant Women in Butajira General Hospital Southern EthiopiaDocument9 pagesAnemia Prevalence, Severity Level and Its Predictors Among Antenatal Care Attending Pregnant Women in Butajira General Hospital Southern EthiopiaJournal of Nutritional Science and Healthy DietNo ratings yet
- Abruptio PlacentaeDocument5 pagesAbruptio PlacentaeindahNo ratings yet
- Knowledgeon Preventionand Managementof Preeclampsiaand Eclampsiaamong Nursesin Primary Health SettingDocument8 pagesKnowledgeon Preventionand Managementof Preeclampsiaand Eclampsiaamong Nursesin Primary Health SettingarreyemilieneNo ratings yet
- Trends and Determinants of Maternal Mortality in Mizan-Tepi University Teaching and Bonga General Hospital From 2011 - 2015: A Case Control StudyDocument8 pagesTrends and Determinants of Maternal Mortality in Mizan-Tepi University Teaching and Bonga General Hospital From 2011 - 2015: A Case Control StudyTegenne LegesseNo ratings yet
- Critically Ill Obstetric Patients and Feto-Maternal Outcome: EditorialDocument3 pagesCritically Ill Obstetric Patients and Feto-Maternal Outcome: EditorialMahtosurup GodavarthyNo ratings yet
- Article 233230Document11 pagesArticle 233230arreyemilieneNo ratings yet
- Case Control Study ArtileDocument9 pagesCase Control Study ArtilekubsaNo ratings yet
- Preeclamsia 1Document15 pagesPreeclamsia 1Pu DeanNo ratings yet
- Magnitude of Maternal Complication and Associated Factors Among Mothers Undergone Cesarean Section at Yirgalem General Hospital, SNNPR, EthiopiaDocument10 pagesMagnitude of Maternal Complication and Associated Factors Among Mothers Undergone Cesarean Section at Yirgalem General Hospital, SNNPR, EthiopiaEbenezer AbrahamNo ratings yet
- Incidence and Outcome of Severe Antepartum Hemorrhage at The Teaching Hospital Yalgado Ouédraogo in Burkina FasoDocument12 pagesIncidence and Outcome of Severe Antepartum Hemorrhage at The Teaching Hospital Yalgado Ouédraogo in Burkina Fasoshiffa ramadhantiNo ratings yet
- Maternal and Fetal Complications in Pregnant Epileptic WomenDocument5 pagesMaternal and Fetal Complications in Pregnant Epileptic WomenMedical Record PPDS OBGINNo ratings yet
- Ijgo 12692Document10 pagesIjgo 12692Putri Sari DewiNo ratings yet
- Morbidity and Mortality Amongst Infants of Diabetic Mothers Admitted Into A Special Care Baby Unit in Port Harcourt, NigeriaDocument6 pagesMorbidity and Mortality Amongst Infants of Diabetic Mothers Admitted Into A Special Care Baby Unit in Port Harcourt, Nigeriavighnaharta Online ServicesNo ratings yet
- Medicina 59 01151Document9 pagesMedicina 59 01151Lissaberti AmaliahNo ratings yet
- Bjo12636 PDFDocument9 pagesBjo12636 PDFLuphly TaluvtaNo ratings yet
- Masa UduDocument27 pagesMasa UduAbdulkarim Masa'uduNo ratings yet
- Acute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisDocument6 pagesAcute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisIntan Wahyu CahyaniNo ratings yet
- General Perinatal Medicine: Oral Presentation at Breakfast 1 - Obstetrics and Labour Reference: A2092SADocument1 pageGeneral Perinatal Medicine: Oral Presentation at Breakfast 1 - Obstetrics and Labour Reference: A2092SAElva Diany SyamsudinNo ratings yet
- Fitzpatrick Et Al-2015-BJOG An International Journal of Obstetrics & GynaecologyDocument10 pagesFitzpatrick Et Al-2015-BJOG An International Journal of Obstetrics & GynaecologyCaroline SidhartaNo ratings yet
- IJP Volume 8 Issue 9 Pages 12011-12021Document11 pagesIJP Volume 8 Issue 9 Pages 12011-12021rullyNo ratings yet
- 247-Article Text-1425-1-10-20200122Document11 pages247-Article Text-1425-1-10-20200122Gisela M SilvaNo ratings yet
- Maternity Nurses Performance Regarding Late Ante Partum Hemorrhage: An Educational InterventionDocument11 pagesMaternity Nurses Performance Regarding Late Ante Partum Hemorrhage: An Educational Interventionfebrin nocitaveraNo ratings yet
- Awareness of Pregnancy Induced Hypertension Among Pregnant Women in Tigray Regional State, EthiopiaDocument16 pagesAwareness of Pregnancy Induced Hypertension Among Pregnant Women in Tigray Regional State, EthiopiaWeslley Ferreira100% (1)
- Improving Maternal Health in The Face of TuberculosisDocument8 pagesImproving Maternal Health in The Face of TuberculosisTemitope OkunolaNo ratings yet
- 2016 Article 154Document7 pages2016 Article 154كنNo ratings yet
- Pre-Eclampsia, Eclampsia and Adverse Maternal and Perinatal Outcomes: A Secondary Analysis of The World Health Organization Multicountry Survey On Maternal and Newborn HealthDocument11 pagesPre-Eclampsia, Eclampsia and Adverse Maternal and Perinatal Outcomes: A Secondary Analysis of The World Health Organization Multicountry Survey On Maternal and Newborn HealthMariana CruzNo ratings yet
- PregnancyDocument10 pagesPregnancyمنیر ساداتNo ratings yet
- Research Article: Anaemia in Pregnancy: Prevalence, Risk Factors, and Adverse Perinatal Outcomes in Northern TanzaniaDocument9 pagesResearch Article: Anaemia in Pregnancy: Prevalence, Risk Factors, and Adverse Perinatal Outcomes in Northern TanzaniaMarcelitaTaliaDuwiriNo ratings yet
- Patient's Profile With Hypertension in Pregnancy PatientsDocument6 pagesPatient's Profile With Hypertension in Pregnancy PatientsHendrik SuTopo LidaprajaNo ratings yet
- 9 JurnalDocument83 pages9 JurnalWanda AndiniNo ratings yet
- Hemorrgia Obstetrica 2020Document20 pagesHemorrgia Obstetrica 2020Carolina VargasNo ratings yet
- Risk Factors For Anaemia in Pregnancy in Rural KwaZulu-Natal South Africa Implication For Health Education and Health PromotionDocument6 pagesRisk Factors For Anaemia in Pregnancy in Rural KwaZulu-Natal South Africa Implication For Health Education and Health PromotionedmondNo ratings yet
- Jurnal Analisis 2 Uts Mikrobiologi Dan ParasitologiDocument10 pagesJurnal Analisis 2 Uts Mikrobiologi Dan ParasitologipujiNo ratings yet
- Medip, IJRCOG-7407 ODocument6 pagesMedip, IJRCOG-7407 OKomalNo ratings yet
- Prevalence and Risk Factors of Puerperal Sepsisbamong Reproductive Aged Women at Jinja Regional Referral Hospital From January 2019 To June 2020Document14 pagesPrevalence and Risk Factors of Puerperal Sepsisbamong Reproductive Aged Women at Jinja Regional Referral Hospital From January 2019 To June 2020KIU PUBLICATION AND EXTENSIONNo ratings yet
- Background MasomaDocument18 pagesBackground MasomaPrecious MasomaNo ratings yet
- Partus LamaDocument8 pagesPartus LamaSulis SipinNo ratings yet
- Knowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhanaDocument10 pagesKnowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhananicloverNo ratings yet
- Aisyah HPTDocument10 pagesAisyah HPTBesari Md DaudNo ratings yet
- Prevalence of Preeclampsia and The Associated Risk Factors Among Pregnant Women in BangladeshDocument10 pagesPrevalence of Preeclampsia and The Associated Risk Factors Among Pregnant Women in BangladeshNanda Puspita SariNo ratings yet
- RPPH 16 32Document32 pagesRPPH 16 32forensik24mei koasdaringNo ratings yet
- Clinical Study of Postpartum Eclampsia: Dr. S. K. Rath, Dr. Swati AgrawalDocument3 pagesClinical Study of Postpartum Eclampsia: Dr. S. K. Rath, Dr. Swati AgrawalSulabh ShresthaNo ratings yet
- Jurnal Dehydration of NewbornDocument7 pagesJurnal Dehydration of NewbornRSU Aisyiyah PadangNo ratings yet
- 10 11648 J Ijcd 20200301 13 PDFDocument7 pages10 11648 J Ijcd 20200301 13 PDFJosé Maria Chema Cari VillaNo ratings yet
- Jurnal MaternitasDocument10 pagesJurnal Maternitasasep saepulohNo ratings yet
- Afhs0801 0044 2Document6 pagesAfhs0801 0044 2Noval FarlanNo ratings yet
- Comparative Study of General With Spinal Anesthesia On Maternal Outcomes For Caesarean Delivery Among Preeclamptic Women at Tikur Anbessa Specialized Hospital, Addis Ababa, EthiopiaDocument7 pagesComparative Study of General With Spinal Anesthesia On Maternal Outcomes For Caesarean Delivery Among Preeclamptic Women at Tikur Anbessa Specialized Hospital, Addis Ababa, EthiopiaMuhammad sadadNo ratings yet
- Ijgo 12741Document5 pagesIjgo 12741zainabNo ratings yet
- Financial Modeling Ch1Document21 pagesFinancial Modeling Ch1talilaNo ratings yet
- Fair Value Final 2Document46 pagesFair Value Final 2talilaNo ratings yet
- Trainers ManualDocument31 pagesTrainers ManualtalilaNo ratings yet
- Practice Exercise - Nairobi - BlankDocument4 pagesPractice Exercise - Nairobi - BlanktalilaNo ratings yet
- Final ProposalDocument25 pagesFinal Proposaltalila0% (1)
- Marketing Ext 2012Document7 pagesMarketing Ext 2012talilaNo ratings yet
- Chapter 3 Fundam 1Document18 pagesChapter 3 Fundam 1talilaNo ratings yet
- Practical Attachement FormDocument7 pagesPractical Attachement FormtalilaNo ratings yet
- MarketingDocument11 pagesMarketingtalilaNo ratings yet
- Questionnaires To Be Filled Out by Bank CustomersDocument3 pagesQuestionnaires To Be Filled Out by Bank CustomerstalilaNo ratings yet
- Chapter One Ifa IiDocument5 pagesChapter One Ifa IitalilaNo ratings yet
- New Melke TwoDocument62 pagesNew Melke TwotalilaNo ratings yet
- Haile UpdatedDocument54 pagesHaile UpdatedtalilaNo ratings yet
- Chapter ONE Fundamental I FinalDocument24 pagesChapter ONE Fundamental I FinaltalilaNo ratings yet
- Approach To Metabolic AlkalosisDocument11 pagesApproach To Metabolic AlkalosisJou ÁlvarezNo ratings yet
- Brolucizumab in Neovascular Age Related Macular Degeneration and Diabetic Macular EdemaDocument17 pagesBrolucizumab in Neovascular Age Related Macular Degeneration and Diabetic Macular EdemaKang LimbaNo ratings yet
- Abraxane (Nab Paclitaxel) As Radiation SensitizerDocument46 pagesAbraxane (Nab Paclitaxel) As Radiation SensitizerLokesh ViswanathNo ratings yet
- Module 4Document37 pagesModule 4Jeraline PiezasNo ratings yet
- SPORTS NUTRITION ASSIGNMENT (Specific Sports)Document3 pagesSPORTS NUTRITION ASSIGNMENT (Specific Sports)Young Tri TNo ratings yet
- Recording A 12-Lead Electrocardiogram (ECG)Document4 pagesRecording A 12-Lead Electrocardiogram (ECG)brianNo ratings yet
- CVA-NCPDocument7 pagesCVA-NCPAiza Oronce0% (1)
- Quiz 5 Test Bank PDFDocument37 pagesQuiz 5 Test Bank PDFOnyeka O AniyedeNo ratings yet
- Free T4 - IMMUNOLITE 2000Document36 pagesFree T4 - IMMUNOLITE 2000pyx5pjqqx4No ratings yet
- Nbme 1Document77 pagesNbme 1Rezo BagashviliNo ratings yet
- Migrane.20220709015224Document8 pagesMigrane.20220709015224Laharika KatheramallaNo ratings yet
- Case Study On PITUTARY MACROADENOMADocument15 pagesCase Study On PITUTARY MACROADENOMAanimesh pandaNo ratings yet
- Introduction To Counselling Psychology (1) Deborah OjiamboDocument23 pagesIntroduction To Counselling Psychology (1) Deborah OjiamboNambwere SaidatNo ratings yet
- Pathophysiology of Type 1 DiabetesDocument14 pagesPathophysiology of Type 1 DiabetesBoNo ratings yet
- Orbital CellulitisDocument20 pagesOrbital CellulitissarahNo ratings yet
- 20 Mechanisms of Injuries (MOI) : How COVID - 19 Injections Can Make You Sick... Even Kill YouDocument24 pages20 Mechanisms of Injuries (MOI) : How COVID - 19 Injections Can Make You Sick... Even Kill YouEphrayim Odor100% (1)
- Lesson Plan On ManiaDocument18 pagesLesson Plan On Maniasp2056251No ratings yet
- BMS533 Lab PracticalDocument3 pagesBMS533 Lab PracticalYUSNURDALILA DALINo ratings yet
- Disease Outbreaks and Investigations: DR Leela V Sabapathy Dept of Community Medicine IMUDocument43 pagesDisease Outbreaks and Investigations: DR Leela V Sabapathy Dept of Community Medicine IMULim Wei EnNo ratings yet
- Activity-Training PlanDocument2 pagesActivity-Training PlanSheryn SaleNo ratings yet
- Transmission of Communicable Diseases and InfectionsDocument6 pagesTransmission of Communicable Diseases and InfectionsclubsanatateNo ratings yet
- Developmental Disabilities in Infancy & Childhood: Neurodevelopmental PediatricianDocument75 pagesDevelopmental Disabilities in Infancy & Childhood: Neurodevelopmental PediatricianCarol Rombaoa Serdenia100% (1)
- TrichiasisDocument3 pagesTrichiasisSyamsi KubangunNo ratings yet
- Manual Blood Cells CountDocument29 pagesManual Blood Cells CountKhalid AbdullahNo ratings yet
- Enteric FeverDocument9 pagesEnteric FeverChetan NaikNo ratings yet
- My Journal 2Document11 pagesMy Journal 2FelixNo ratings yet
- Definition and Description of Schizprenia in The DSM-5Document8 pagesDefinition and Description of Schizprenia in The DSM-5Danekka TanNo ratings yet
- Probiotics, Prebiotics, and Synbiotics For The Treatment and Prevetion of Adult Dermatological Diseaases - Acne e DermatiteDocument12 pagesProbiotics, Prebiotics, and Synbiotics For The Treatment and Prevetion of Adult Dermatological Diseaases - Acne e DermatiteElisa BarcelosNo ratings yet
- DR oDocument26 pagesDR oapi-247961469100% (1)
- EMONCDocument17 pagesEMONCJessie OranoNo ratings yet