Professional Documents
Culture Documents
Value of PET CT in Primary HPB Tumours
Value of PET CT in Primary HPB Tumours
Uploaded by
lkitkatgirlCopyright:
Available Formats
You might also like
- MSDS - HelizymeDocument10 pagesMSDS - HelizymeNurhari OgiNo ratings yet
- Ineffective Health MaintenanceDocument2 pagesIneffective Health MaintenanceBlessie Fernandez100% (1)
- Prenatal Brochure 2011-FF - Health Power For MinoritiesDocument2 pagesPrenatal Brochure 2011-FF - Health Power For MinoritiesNorma J. Goodwin, MDNo ratings yet
- Clinical Practice in PET CT For The Management of Head and Neck Squamous Cell CancerDocument15 pagesClinical Practice in PET CT For The Management of Head and Neck Squamous Cell CancerlkitkatgirlNo ratings yet
- Ringe Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 1 Protocol Optimization and Lesion Appearance inDocument16 pagesRinge Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 1 Protocol Optimization and Lesion Appearance indynachNo ratings yet
- RENAL ScoreDocument5 pagesRENAL ScoreMurilo CamposNo ratings yet
- Ajr 10 5540Document9 pagesAjr 10 5540Pepe pepe pepeNo ratings yet
- CTA ExtremityDocument8 pagesCTA Extremityrio trisonaNo ratings yet
- Belloni Et Al 2012 Mri of CardiomyopathyDocument11 pagesBelloni Et Al 2012 Mri of CardiomyopathyRadiologyNo ratings yet
- LIVER CALCIFIED MASSES Types AlgorithmDocument11 pagesLIVER CALCIFIED MASSES Types Algorithmcalustre2016No ratings yet
- Ajr 18 20947Document6 pagesAjr 18 20947Amartya PalNo ratings yet
- Solid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaDocument11 pagesSolid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaTạ Minh ZSNo ratings yet
- Cruite Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 2 Protocol Optimization and Lesion Appearance inDocument13 pagesCruite Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 2 Protocol Optimization and Lesion Appearance indynachNo ratings yet
- Dual-Energy CT of The Brain and Intracranial VesselsDocument8 pagesDual-Energy CT of The Brain and Intracranial VesselsMuhammad Rafiee SukmaNo ratings yet
- Current Concepts of Hip Arthroplasty For Radiologists: Part 1, Features and Radiographic AssessmentDocument12 pagesCurrent Concepts of Hip Arthroplasty For Radiologists: Part 1, Features and Radiographic AssessmentGERARDO TORRES RUIZNo ratings yet
- Cancer FibromamelarDocument16 pagesCancer FibromamelarMarcela DuarteNo ratings yet
- AJR Chest Radiography in The ICU Parte II 2012Document10 pagesAJR Chest Radiography in The ICU Parte II 2012wfranelicNo ratings yet
- Radlink Issue 2 2008Document2 pagesRadlink Issue 2 2008RadlinkSingaporeNo ratings yet
- Effect of Patient Size On Radiation Dose of Abdominal MDCT With Automatic Tube Current ModulationDocument6 pagesEffect of Patient Size On Radiation Dose of Abdominal MDCT With Automatic Tube Current Modulationdestian ryanNo ratings yet
- 8 Ortho Oncology - 210217 - 194331Document11 pages8 Ortho Oncology - 210217 - 194331Nabil AhmedNo ratings yet
- AJR Chest Radiography in The ICU Parte I 2012Document9 pagesAJR Chest Radiography in The ICU Parte I 2012wfranelicNo ratings yet
- AVC p2Document14 pagesAVC p2Elena VelcuNo ratings yet
- CT On GI TractDocument10 pagesCT On GI TractRizky Putri Agustina RumapeaNo ratings yet
- Imaging Assessment of Hepatocellular Carcinoma Response To Locoregional and Systemic TherapyDocument19 pagesImaging Assessment of Hepatocellular Carcinoma Response To Locoregional and Systemic Therapyanra kusumaNo ratings yet
- Identifying The Anatomical Variations of The.20Document7 pagesIdentifying The Anatomical Variations of The.20FERNANDO ALVESNo ratings yet
- Radiology of Chest Wall MassesDocument11 pagesRadiology of Chest Wall MassesDevina BumiNo ratings yet
- New Developments of PetDocument59 pagesNew Developments of Petmm_555_ssNo ratings yet
- Chest Radiography in The ICUDocument9 pagesChest Radiography in The ICUNicolás HonoresNo ratings yet
- PosterDocument1 pagePosterKoushul RamjattunNo ratings yet
- Approprate Use NETDocument11 pagesApproprate Use NETkasturi.rangan1234No ratings yet
- Articulo 1recto SuperiorDocument7 pagesArticulo 1recto SuperiorCarolinaNo ratings yet
- Imaging of Cholecystitis: ResidentsDocument8 pagesImaging of Cholecystitis: ResidentsandrefaelNo ratings yet
- Ajr 2Document10 pagesAjr 2Fika FathiaNo ratings yet
- Neoplastic Myelopathies: Continuumaudio Interviewavailable OnlineDocument22 pagesNeoplastic Myelopathies: Continuumaudio Interviewavailable OnlineDalwadi1No ratings yet
- The Evolution of MRI of The Prostate: The Past, The Present, and The FutureDocument13 pagesThe Evolution of MRI of The Prostate: The Past, The Present, and The Futurelintang dmNo ratings yet
- TACE Standards of PracticeDocument17 pagesTACE Standards of PracticeRuminRuNo ratings yet
- ClassificationDocument8 pagesClassificationbarathy.kbNo ratings yet
- R02Y2002N01A0003Document27 pagesR02Y2002N01A0003Roseck BlackNo ratings yet
- Rico Harke Abraham Siagian 021801009 Tugas ResumeDocument18 pagesRico Harke Abraham Siagian 021801009 Tugas ResumeGebrilya TendeanNo ratings yet
- Cross-Sectional Imaging of Intrahepatic Cholangiocarcinoma: Development, Growth, Spread, and PrognosisDocument12 pagesCross-Sectional Imaging of Intrahepatic Cholangiocarcinoma: Development, Growth, Spread, and PrognosisNikos SerifisNo ratings yet
- Document My Assignment TherapyDocument5 pagesDocument My Assignment TherapynanaaishamahmudgazaraNo ratings yet
- 2021 The Use of Fecal Calprotectin Testing in PaediatricDocument24 pages2021 The Use of Fecal Calprotectin Testing in PaediatricKhadijah Rizky SumitroNo ratings yet
- Spe 68328 MsDocument1 pageSpe 68328 MsAbed Alftah AgabNo ratings yet
- CT Mri CCHDocument21 pagesCT Mri CCHrizkianaNo ratings yet
- Analysis of Enhancement Pattern of Flat Gallbladder Wall Thickening On MDCT To Differentiate Gallbladder Cancer From CholecystitisDocument7 pagesAnalysis of Enhancement Pattern of Flat Gallbladder Wall Thickening On MDCT To Differentiate Gallbladder Cancer From CholecystitisSamuel WidjajaNo ratings yet
- Renal Cell Carcinoma: Diagnosis, Staging, and SurveillanceDocument13 pagesRenal Cell Carcinoma: Diagnosis, Staging, and SurveillanceEmanuelleReisNo ratings yet
- Frequency of Egfr Mutations in Lung Adenocarcinoma.40Document8 pagesFrequency of Egfr Mutations in Lung Adenocarcinoma.40Tanaka TanakaNo ratings yet
- Intrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationDocument13 pagesIntrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationIndra PrimaNo ratings yet
- Ajr.12.10010 Aortic RootDocument9 pagesAjr.12.10010 Aortic Rootfranti76No ratings yet
- 2003 Poster SampleDocument1 page2003 Poster SampleDry LandNo ratings yet
- Pet BrochureDocument20 pagesPet BrochureSheikh Hasnain AliNo ratings yet
- Background: Relation Between Hyperlcoagulation With 12 Months of Survival Monitoring On AstrocytomaDocument1 pageBackground: Relation Between Hyperlcoagulation With 12 Months of Survival Monitoring On AstrocytomajhnaidillaNo ratings yet
- TerrenceDocument3 pagesTerrenceVinayak K gowdaNo ratings yet
- Recent Advances in PETCTDocument30 pagesRecent Advances in PETCTDivyaNo ratings yet
- Yty 116Document5 pagesYty 116Intania RatnaNo ratings yet
- Factors Affecting Accuracy of SuvDocument11 pagesFactors Affecting Accuracy of SuvTurkiNo ratings yet
- Lee2017imagerie StadeDocument13 pagesLee2017imagerie StadenimaelhajjiNo ratings yet
- Evaluation of Total Corneal Power MeasurementsDocument7 pagesEvaluation of Total Corneal Power MeasurementsMariana Luzardo bravoNo ratings yet
- Bateni Et Al 2013 Imaging Key Wrist Ligaments What The Surgeon Needs The Radiologist To KnowDocument7 pagesBateni Et Al 2013 Imaging Key Wrist Ligaments What The Surgeon Needs The Radiologist To KnowRadiologyNo ratings yet
- Pvy036 PDFDocument12 pagesPvy036 PDFHimanshu dubeyNo ratings yet
- An Automated System For Liver CT Enhancement and SegmentationDocument6 pagesAn Automated System For Liver CT Enhancement and Segmentationshamalu2011No ratings yet
- What The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyDocument8 pagesWhat The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyQonita Aizati QomaruddinNo ratings yet
- FDG PET CT in The Management of Lymphomas Current Status and FutureDocument19 pagesFDG PET CT in The Management of Lymphomas Current Status and FuturelkitkatgirlNo ratings yet
- The Impact of Infection and Inflammation in OncoloDocument9 pagesThe Impact of Infection and Inflammation in OncololkitkatgirlNo ratings yet
- Uematsu Et Al 2012 Comparison of FDG Pet and Spect For Detection of Bone Metastases in Breast CancerDocument8 pagesUematsu Et Al 2012 Comparison of FDG Pet and Spect For Detection of Bone Metastases in Breast CancerlkitkatgirlNo ratings yet
- The Place of FDG PET CT in Renal Cell Carcinoma - Value and LimitationsDocument7 pagesThe Place of FDG PET CT in Renal Cell Carcinoma - Value and LimitationslkitkatgirlNo ratings yet
- The Value of FDG PET CT Scans To Evaluate Bone Marrow in Haemato-Oncological ConditionsDocument9 pagesThe Value of FDG PET CT Scans To Evaluate Bone Marrow in Haemato-Oncological ConditionslkitkatgirlNo ratings yet
- CYBERBULLYINGDocument2 pagesCYBERBULLYINGAdinda CahayaNo ratings yet
- PHED 10032 Individual, Dual, and Combative SportsDocument52 pagesPHED 10032 Individual, Dual, and Combative SportsMicmic CalivaNo ratings yet
- To Do List For HACCPDocument2 pagesTo Do List For HACCPChâu TrầnNo ratings yet
- Institutionalized ElderlyDocument20 pagesInstitutionalized ElderlySourav DeyNo ratings yet
- Nama Puskesmas/Fasyankes/Pos Kabupaten/Kota Provinsi:: UPT Puskesmas Talaga: Majalengka: Jawa BaratDocument20 pagesNama Puskesmas/Fasyankes/Pos Kabupaten/Kota Provinsi:: UPT Puskesmas Talaga: Majalengka: Jawa BaratNoeNuraeniNo ratings yet
- 2023 GKS-U Application FormsDocument11 pages2023 GKS-U Application FormsNaomi FernándezNo ratings yet
- SOP On Operation and Calibration of Water BathDocument5 pagesSOP On Operation and Calibration of Water Bathfawaz khalilNo ratings yet
- 13.1 Social Sectors Reforms (By Ayussh Sanghi)Document37 pages13.1 Social Sectors Reforms (By Ayussh Sanghi)harmless wolfNo ratings yet
- Effective Study Habit : By: Patra Cleo AlcomendasDocument8 pagesEffective Study Habit : By: Patra Cleo AlcomendasMary Rose S. BonilloNo ratings yet
- 7.artikel JKM Vol. 14 No. 2 Desember 2021 Case Report JKM Edwin Anto Pakpahan 55 63Document9 pages7.artikel JKM Vol. 14 No. 2 Desember 2021 Case Report JKM Edwin Anto Pakpahan 55 63waode apriyaniNo ratings yet
- HeirarchyDocument3 pagesHeirarchyMazikeen LilimNo ratings yet
- Week 7 Guide Questions AnswersDocument7 pagesWeek 7 Guide Questions AnswersKathleenMarieAlforteNo ratings yet
- Service Stream EDP Permit Training Participant WorkbookDocument19 pagesService Stream EDP Permit Training Participant Workbookshana.mxNo ratings yet
- People v. Robiños, G.R. No. 138453, 29 May 2002Document13 pagesPeople v. Robiños, G.R. No. 138453, 29 May 2002Isabella EncarnacionNo ratings yet
- OBSTETRIC NURSING Hand Out UPANG INHOUSE 2022Document7 pagesOBSTETRIC NURSING Hand Out UPANG INHOUSE 2022Mary Ann G. CorsanesNo ratings yet
- Eyhance BrochureDocument2 pagesEyhance Brochuredr.Nurcahya Ardian Bramantha,SpMNo ratings yet
- Isolation and Molecular Characterization of Salmonella Enterica, Escherichia Coli O157-H7 and Shigella Spp. From Meat and Dairy Products in EgyptDocument6 pagesIsolation and Molecular Characterization of Salmonella Enterica, Escherichia Coli O157-H7 and Shigella Spp. From Meat and Dairy Products in EgyptAffan GaffarNo ratings yet
- Minimally Invasive When? How? Why?: Access Cavity Preparation in EndodonticsDocument4 pagesMinimally Invasive When? How? Why?: Access Cavity Preparation in EndodonticsdoctorlupuNo ratings yet
- Bura - Stephane - Beyond ElizaDocument79 pagesBura - Stephane - Beyond ElizaphiloNo ratings yet
- Maternal Lec Week 1 3Document4 pagesMaternal Lec Week 1 3Althea ManarpiisNo ratings yet
- Tyler Twist ProtocolDocument7 pagesTyler Twist ProtocolchinitosNo ratings yet
- Red Orchid - Best PracticesDocument80 pagesRed Orchid - Best PracticeslabiaernestoNo ratings yet
- Nose Unblocking ExerciseDocument1 pageNose Unblocking Exercisebharat panchalNo ratings yet
- SteerBridge JD - CFM-IDIQ San Francisco - Electrical EngineerDocument3 pagesSteerBridge JD - CFM-IDIQ San Francisco - Electrical Engineersmrasteg12No ratings yet
- Anecdotal EvidenceDocument19 pagesAnecdotal EvidenceMedia Development FoundationNo ratings yet
- Bobcat 226 yDocument19 pagesBobcat 226 yEduardoNo ratings yet
- AISA CP Handbook 2016Document83 pagesAISA CP Handbook 2016Rhea EscleoNo ratings yet
Value of PET CT in Primary HPB Tumours
Value of PET CT in Primary HPB Tumours
Uploaded by
lkitkatgirlOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Value of PET CT in Primary HPB Tumours
Value of PET CT in Primary HPB Tumours
Uploaded by
lkitkatgirlCopyright:
Available Formats
N u c l e a r M e d i c i n e a n d M o l e c u l a r I m a g i n g • R ev i ew
Sacks et al.
PET/CT in Primary Hepatobiliary Tumors CME Value of PET/CT
Downloaded from ajronline.org by 2a02:6b68:988e:0:96ba:ea07:aef1:34a2 on 11/17/23 from IP address 2a02:6b68:988e:0:96ba:ea07:aef1:34a2. Copyright ARRS. For personal use only; all rights reserved
SAM
Nuclear Medicine and Molecular Imaging
Review
Value of PET/CT in the
FOCUS ON:
Management of Primary
Hepatobiliary Tumors, Part 2
Ari Sacks1 OBJECTIVE. Primary hepatobiliary malignancies consist of hepatocellular carcinoma,
Patrick J. Peller 2 cholangiocarcinoma, and gallbladder cancer. Benign hepatic lesions include hepatic cysts,
Devaki S. Surasi 3 hemagiomas, adenomas, and focal nodular hyperplasias. The utility of PET/CT in imaging
Luke Chatburn1 primary hepatobiliary lesions varies according to the type and location of the lesion.
Gustavo Mercier 3 CONCLUSION. There is a consistent benefit to the use of PET/CT for detection and
staging, and it ultimately helps to establish the best course of treatment and to determine
Rathan M. Subramaniam 3
prognosis. In addition, PET/CT is very useful in local ablative and systemic therapy
Sacks A, Peller PJ, Surasi DS, Chatburn L, Mercier assessment and surveillance for hepatobiliary malignancies.
G, Subramaniam RM
P
rimary hepatobiliary malignan- [7]. Such state-of-the-art hepatic MRI tech-
cies include liver tumors, cholan- niques may play a role in better characteriza-
giocarcinoma, and gallbladder tion of hepatic lesions in the future.
cancer. Primary hepatic tumors, This article provides an overview of the
malignant or benign, are infrequent [1] and current role of PET and PET/CT in primary
include hepatocellular carcinomas (HCCs), hepatobiliary tumors.
hemagiomas, adenomas, and focal nodular
Keywords: hepatobiliary tumors, PET/CT hyperplasias. There is increased incidence of Hepatocellular Carcinoma
HCC in patients with chronic liver diseases, The liver is the major producer of nondi-
DOI:10.2214/AJR.11.6995 such as hepatitis [2], alcoholic cirrhosis [3], etary glucose, at a rate of 2.0 mg/kg/min,
and systemic immune diseases, especially which helps maintain glucose homeostasis
Received April 1, 2011; accepted without revision
April 7, 2011. HIV [4]. Biliary tree and gallbladder primary [8]. Studies have shown that there are a va-
tumors are rare (< 2% of cancer prevalence) riety of different levels of glucose-6-phos-
1
Boston University School of Medicine, Boston, MA. and are difficult to diagnose at an operable phatase activity and glucose transporters in
2
stage. The epidemiology of gallbladder cancer HCC, leading to variable 18F-FDG uptake
Department of Radiology, Boston Medical Center and
Boston University School of Medicine, Boston, MA.
varies globally, correlating strongly with cho- [9–12]. Torizuka et al. [9] showed that FDG
lelithiasis and Salmonella infection rates [5]. uptake of HCC lesions correlates with the de-
3
Department of Radiology, Boston Medical Center and PET and PET/CT may play a significant role gree of differentiation of the HCC; high-grade
Boston University School of Medicine, 820 Harrison Ave, in the diagnosis, staging, or follow-up of each HCCs have increased FDG uptake (mean [±
FGH Bldg, Level 3, Boston, MA 02118. Address
of these malignancies. SD] standardized uptake value [SUV], 6.89 ±
correspondence to R. M. Subramaniam
(rathan.subramaniam@bmc.org). Newer hepatic MRI techniques have vastly 3.39) compared with low-grade HCCs (mean
improved the ability of MRI to differentiate SUV, 3.21 ± 0.58) (p < 0.005).
CME/SAM between benign and malignant focal hepatic Because of this variability, it is likely that
This article is available for CME/SAM credit. lesions. For example, diffusion-weighted im- FDG PET scans have an increased ability to
See www.arrs.org for more information.
aging has been shown by Koike et al. [6] to detect higher grade HCCs and, alternatively,
WEB differentiate malignant from benign lesions have a decreased ability to detect low-grade
This is a Web exclusive article. by having a lower apparent diffusion coeffi- HCCs, as a result of decreased FDG uptake.
cient and higher relative contrast ratio when The overall sensitivity of FDG PET/CT in
AJR 2011; 197:W260–W265
compared with surrounding liver parenchy- detecting HCC suffers, with a reported range
0361–803X/11/1972–W260 ma. Furthermore, the development of spe- of 50–65% [12–16]. For this reason, FDG
cific MRI hepatobiliary contrast agents im- PET has been determined [14] to be insuf-
© American Roentgen Ray Society proves lesion detection and characterization ficiently sensitive to diagnose primary HCC.
W260 AJR:197, August 2011
PET/CT in Primary Hepatobiliary Tumors
Downloaded from ajronline.org by 2a02:6b68:988e:0:96ba:ea07:aef1:34a2 on 11/17/23 from IP address 2a02:6b68:988e:0:96ba:ea07:aef1:34a2. Copyright ARRS. For personal use only; all rights reserved
A study by Khan et al. [13] found that the achieved via guiding the biopsy of a large ne- In an assessment of dual-tracer (11C-acetate
sensitivity of FDG PET in the diagnosis of crotic tumor (n = 1), identifying distant me- and FDG) PET/CT, Park et al. [25] prospec-
HCC was 55%, compared with 90% for con- tastases (n = 5), monitoring the response to tively evaluated the value of PET/CT using
trast-enhanced CT. Another report, by Wu- treatment with regional therapy (n = 12), and FDG and 11C-acetate tracers for the detection
del et al. [15], involving one of the largest se- detecting recurrence (n = 2). The authors of primary and metastatic HCC. The overall
ries of FDG PET for HCC (n = 91), reported concluded that FDG PET should be consid- sensitivities of FDG, 11C-acetate, and dual-
that the sensitivity of FDG PET for detection ered as part of the staging and management tracer PET/CT in the detection of 110 lesions
of HCC was 64%. of selected patients with HCC. in 90 patients with primary HCC were 60.9%,
Although the sensitivity of FDG PET scans Fusions of FDG PET and CT images have 75.4%, and 82.7%, respectively. The sensitivi-
has been shown to be lower than that of oth- been shown to provide improvement of le- ties according to tumor size (1–2, 2–5, and ≥
er imaging modalities for HCC, it still plays sion detection, localization, and differentia- 5 cm) were 27.2%, 47.8%, and 92.8%, respec-
an important role in prognosis. Because FDG tion between physiologic versus patholog- tively, for FDG and 31.8%, 78.2%, and 95.2%,
uptake acts as a marker of differentiation, ic uptake on both CT and FDG PET images respectively, for 11C-acetate [25]. In that same
SUVs can give insight into the histopatho- alone [21]. The addition of CT images can study, FDG was found to be more sensitive
logic nature of the tumor. Shiomi et al. [17] also be very useful for detecting HCC in cas- than 11C-acetate in detection of extrahepatic
showed that the SUV ratios (SUV ratio of tu- es when the lesion is not FDG avid, because metastases (85.7% vs 77%). The addition of
mor to nontumor in liver) of HCC tumors cor- 70% of HCCs are visible on unenhanced CT 11C-acetate to FDG PET/CT increases the
relate with tumor volume-doubling time (r = as hypodense lesions, and an additional 20% overall sensitivity for the detection of primary
−0.582; p = 0.006). That study also found that are visible as hyperdense lesions [22]. HCC, but not for the detection of extrahepatic
cumulative survival rate can be predicted on FDG PET/CT has been shown to be ben- metastases. This may be the result of in-
the basis of the SUV ratio. The patients were eficial in detecting extrahepatic disease in creased FDG PET sensitivity in the detection
divided into two groups of similar size: group patients with primary HCC (Fig. 1). Kawa- of poorly differentiated HCC tumors, which
A (n = 24) had SUV ratios (as defined as the oka et al. [23] found FDG PET/CT to have are often more likely to be more aggressive,
hepatic tumor-to-nontumor ratio of SUV) of a higher sensitivity for the detection of bone and thus associated with metastases [20].
1.5 or less, and group B (n = 24) had SUV ra- metastases from primary HCC, compared Overall, for identification and staging of HCC
tios greater than 1.5. The authors showed that with MDCT and bone scintigraphy. In that metastasis, Ho et al. [20] found dual-tracer
the cumulative survival rate was significantly study, the mean sensitivity and specificity for PET/CT to have a sensitivity of 98%, a speci-
lower in group B than in group A (p = 0.026). diagnosis of bone metastasis were 41.6% and ficity of 86%, a positive predictive value
Similarly, Kong et al. [18] showed that pa- 94.5% for MDCT, 83.3% and 86.1% for FDG (PPV) of 97%, a negative predictive value
tients with HCC who had mean SUVs of 7 or PET/CT, and 52.7% and 83.3% for bone (NPV) of 90%, and an accuracy of 96%.
higher had a significantly (p = 0.0003) lower scintigraphy, respectively. FDG PET/CT is These values, as expected, are all significantly
median survival time (4 vs 15 months). also very useful for assessing chemoemboli- improved to either imaging modality alone.
Although FDG PET can help to differentiate zation therapy for HCC (Fig. 2). In summary, because of the variable glucose
tumors, it may also be useful in the staging of Because FDG PET has been shown to have metabolism of HCCs, FDG PET has shown
HCC as a complementary modality to CT by limited sensitivity for the detection of some mixed utility in the detection of HCCs, with
detecting unsuspected regional and distant HCC tumors because of their variable FDG up- sensitivities of 55–64% and with larger tumors
metastases [13]. In a study by Yoon et al. [19], take, 11C-acetate-PET has been used to com- visualized better than smaller tumors. FDG
pretreatment FDG PET examinations were plement FDG PET in a dual-tracer PET scan. PET appears to provide insight into the meta-
performed on 87 patients with HCC who un- Ho et al. [20] found that well-differentiated bolic activity of the tumor, with higher FDG
derwent MRI or CT studies, to assess whether HCCs preferentially accumulate 11C-acetate, uptake correlating with higher grade cancers
there were any extrahepatic metastases present whereas poorly differentiated tumors tend to and predicting prognosis. FDG PET has also
in those patients. Extrahepatic metastases were preferentially accumulate FDG. Delbeke et al. been shown to be helpful in the detection of
identified in 24 of 87 patients. All of the extra- [24] suggest that different uptake or tracers by regional and extrahepatic metastases, with a
hepatic metastases were detected by FDG PET. lesions can narrow down a differential diagno- disproportionate number of metastatic HCCs
In addition, FDG PET identified four lymph sis. When a tumor accumulates both tracers, or being FDG avid; FDG PET/CT is the most
node metastases and six bone metastases that only 11C-acetate, HCC is high on the differen- sensitive examination for detecting HCC extra-
had not been found using MRI or CT. TNM tial. Lesions that accumulate only FDG suggest hepatic metastases. Finally, 11C-acetate tracer
stage based on the conventional staging work- a non-HCC malignancy. The remaining le- used in conjunction with FDG was shown in
up was changed in four cases after FDG PET. It sions, which accumulate neither tracer, imply a one study to vastly increase the detection rate
has been proposed by Ho et al. [20] that poorly benign pathologic abnormality. On the basis of of HCC with PET.
differentiated HCCs, which are more likely to tracer avidity to different types of HCC lesions,
metastasize, also tend to be FDG avid; there- dual-tracer PET could lead to increased sensi- Benign Liver Tumors
fore, metastases from HCCs in general are tivity in detecting all HCC. Ho et al. [20] found The most common benign hepatic tumors
more likely to be detected with FDG PET. that none of 23 HCC lesions in their study pop- are hemangiomas, focal nodular hyperpla-
Wudel et al. [15] found that, although only ulation were negative for both tracers (100% sia (FNH), and hepatocellular adenomas.
64% of HCCs accumulated FDG, FDG PET sensitivity using both tracers). HCC tumors All of these benign tumors have been shown
had a clinically significant impact in 26 of 91 with no evident FDG uptake were detected by to take up FDG at a similar rate as normal
patients (28%) with HCC. This impact was 11C-acetate uptake, and vice versa. liver tissue.
AJR:197, August 2011 W261
Sacks et al.
Downloaded from ajronline.org by 2a02:6b68:988e:0:96ba:ea07:aef1:34a2 on 11/17/23 from IP address 2a02:6b68:988e:0:96ba:ea07:aef1:34a2. Copyright ARRS. For personal use only; all rights reserved
Kurtaran et al. [26] showed that malignant et al. [33] retrospectively examined the cases tection of lymph node metastasis were 86%,
liver lesions accumulate more FDG than FNH of 20 patients with cholangiocarcinoma and 68%, and 57%; the sensitivities were 43%,
lesions (mean, 10.07 ± 3.79 and 2.12 ± 0.38, found that FDG PET had sensitivity, specific- 43%, and 43%; and the specificities were
respectively). Furthermore, FNH lesions showed ity, and diagnostic accuracy of 92.3%, 92.9% 100%, 76%, and 64%, respectively.
normal or even decreased accumulation of and 92.6%, respectively. A more recent study Several other studies [40–42] have shown
FDG compared with background liver tissue. investigating FDG PET/CT by Jadvar et al. that FDG PET has distinct advantages at de-
Ho et al. [14] found that FNH lesions can [32] found sensitivity and specificity to be 94% tecting occult metastases that were not diag-
show mildly increased levels of 11C-acetate and 100%, respectively. That study included nosed by standard imaging. Thus, FDG PET/
uptake (11C-acetate SUVmax, 3.59, with a lesion- patients with overt metastatic disease that was CT staging has an important impact on the
to-normal liver ratio of 1.25). Hemangiomas easily detectable by other imaging modalities, selection of adequate therapy [31]. FDG PET
showed poor FDG uptake [27], with an SUV which may have exaggerated the values [32]. has been shown to change surgical manage-
ratio of less than 2. In a prospective study, Kim et al. [30] found ment in 17–30% [31, 34, 43] of patients eval-
To further delineate the imaging role of overall values for sensitivity, specificity, PPV, uated for cholangiocarcinoma, primarily as
PET in evaluating liver masses, Delbeke et NPV, and accuracy of FDG PET/CT in prima- a result of detection of unsuspected or un-
al. [28] were able to show the ability of FDG ry tumor detection were 84.0%, 79.3%, 92.9%, known metastases and, thus, upstaging [43].
PET to differentiate between benign and ma- 60.5%, and 82.9%, respectively. In summary, the sensitivity of FDG PET
lignant hepatic lesions in 110 patients who In 36 patients who underwent imaging for and FDG PET/CT in diagnosing cholangio-
were referred for examination of hepatic le- cholangiocarcinoma, Anderson et al. [34] carcinoma appears to be dependent on both
sions greater than 1 cm at largest diameter. found that the sensitivity for detection with the morphologic characteristics and loca-
The authors found that all benign hepatic le- FDG PET was 85% (n = 22) for a nodular tion of the lesion, with nodular forms and pe-
sions (n = 23), including adenoma and FNH, morphology, but only 18% (n = 14) for an in- ripherally located lesions being easier to de-
had poor uptake and an SUVmax less than filtrating morphology. Periductal infiltrating tect than infiltrating and hilar lesions. FDG
3.5, except for one of three abscesses that cholangiocarcinomas rarely form a focal mass PET and FDG PET/CT have been shown to
had definite uptake. All 66 liver metastases [35], and FDG uptake is, therefore, streaky. be very beneficial in detecting regional and
and 16 of 23 HCCs had avid FDG uptake. These data suggest that FDG PET is accurate distal metastases from cholangiocarcinoma,
In summary, benign liver tumors take up in predicting the presence of nodular cholan- which can affect patient management.
FDG at a similar rate to surrounding tissue, giocarcinoma (mass > 1 cm), but is less effec-
differentiating them from HCCs or metasta- tive for the infiltrating type [32, 34]. Gallbladder Cancer
ses or both on PET. Hemangiomas take up The location of the cholangiocarcinoma Gallbladder cancer is a relatively rare ma-
the least FDG of the non-HCC liver tumors. also plays a role in the ability of FDG PET lignancy that has few specific symptoms or
Liver abscesses may be a source of false-pos- to detect the lesion. The sensitivity of FDG signs. The clinical presentations of gallstone
itive findings on FDG PET. PET/CT in detecting primary hilar or ex- disease and gallbladder cancer are often dif-
trahepatic cholangiocarcinoma tumors was ficult to distinguish. Therefore, symptoms of
Cholangiocarcinoma found to be 18–58.8% [32, 34, 36, 37], sig- gallbladder cancer are often mistakenly in-
Cholangiocarcinoma is notoriously dif- nificantly lower than that of peripheral nod- terpreted as biliary colic or chronic chole-
ficult to diagnose early and is usually fatal ular tumors. One study of 22 patients with cystitis, hampering a timely formation of a
because of its late clinical presentation and primary sclerosing cholangitis [38] showed diagnosis [44]. Radical gallbladder resection
the lack of effective nonsurgical therapeutic that FDG PET/CT of the liver that was per- remains the most effective tools in the man-
modalities [29]. Diagnostic imaging of this formed after a delay (about 120 minutes af- agement of patients with gallbladder cancer,
type of tumor is usually performed with ul- ter injection) was able to differentiate benign in the absence of metastatic disease. Surgery
trasound, CT, or MR cholangiography. Stud- strictures from extrahepatic and hilar cho does not offer any survival benefit in patients
ies show that, although FDG PET/CT has no langiocarcinomas in all 22 lesions by using with distant metastasis [45].
statistically significant advantage over con- SUVmax greater than 3.6 as a threshold. FDG PET takes advantage of the high glu-
trast-enhanced CT, MRI, or MR cholangiog- Although FDG PET and FDG PET/CT cose utilization of gallbladder cancer (Fig.
raphy in the diagnosis of primary biliary tu- have not been shown to be highly beneficial 4). There are only a handful of studies as-
mors [30, 31], it is very valuable in detecting in diagnosing primary cholangiocarcinoma, sessing the role of FDG PET or FDG PET/
regional and distant metastases not seen by they have benefit in the diagnosis of metasta- CT in gallbladder cancer, making solid con-
conventional imaging. ses and staging. Kim et al. [30] found FDG clusions of its role more difficult to establish.
FDG accumulates in cholangiocarcino- PET to have improved accuracy in the diag- In two small series (n = 16 in each) by Koh
ma, which appears to be primarily the result nosis of regional lymph nodes metastases et al. [46] and Rodríguez-Fernández et al.
of increased glucose transporter expression (75.9% vs 60.9%; p = 0.004) and distant me- [47], FDG PET was shown to have sensitiv-
on tumor cells [32]. This increased uptake tastases (88.3% vs 78.7%; p = 0.004) when ity of 75–80% and specificity of 82–87.5%
is especially prominent in nodular or mass- compared with CT (n = 123). Seo et al. [39] in diagnosing gallbladder cancer. Rodríguez-
forming cholangiocarcinomas, which have also found FDG PET to be a more accurate Fernández et al. found two false-positive re-
intense FDG uptake due to increased expres- and specific detector of lymph node metas- sults because of acute cholecystitis. In anoth-
sion of glucose transporter–1 [11] (Fig. 3). tases in 35 patients when compared with ei- er study (n = 14) [31], the authors found the
In assessing the ability of FDG PET to de- ther CT or MRI. Diagnostic accuracies in sensitivity of PET/CT detecting gallbladder
tect and diagnose cholangiocarcinoma, Kluge that study of FDG PET, CT, and MRI for de- cancer to be 100% (14/14).
W262 AJR:197, August 2011
PET/CT in Primary Hepatobiliary Tumors
Downloaded from ajronline.org by 2a02:6b68:988e:0:96ba:ea07:aef1:34a2 on 11/17/23 from IP address 2a02:6b68:988e:0:96ba:ea07:aef1:34a2. Copyright ARRS. For personal use only; all rights reserved
FDG PET appears to have a potential role HIV-1 infected patients. Eur J Intern Med 2005; glucose is useful for predicting the prognosis of
in the assessment of gallbladder wall thicken- 16:113–115 patients with hepatocellular carcinoma (in Kore-
ing, as seen on conventional imaging. Oe et 5. Randi G, Franceschi S, La Vecchia C. Gallbladder an). Korean J Hepatol 2004; 10:279–287
al. [48] found that increased FDG uptake was cancer worldwide: geographical distribution and 19. Yoon KT, Kim JK, Kim do Y, et al. Role of 18F-
able to help distinguish between benign and risk factors. Int J Cancer 2006; 118:1591–1602 fluorodeoxyglucose positron emission tomogra-
malignant gallbladder wall thickening found 6. Koike N, Cho A, Nasu K, et al. Role of diffusion- phy in detecting extrahepatic metastasis in pre-
on ultrasound, CT, or MRI. In their study, four weighted magnetic resonance imaging in the dif- treatment staging of hepatocellular carcinoma.
of 12 patients with gallbladder wall thicken- ferential diagnosis of focal hepatic lesions. World Oncology 2007; 72(suppl 1):104–110
ing on conventional imaging had FDG up- J Gastroenterol 2009; 15:5805–5812 20. Ho CL, Chen S, Yeung DW, Cheng TK. Dual-
take. Three of those four patients were found 7. Seale MK, Catalano OA, Saini S, Hahn PF, tracer PET/CT imaging in evaluation of meta-
to have gallbladder cancer, whereas none Sahani DV. Hepatobiliary-specific MR contrast static hepatocellular carcinoma. J Nucl Med 2007;
of the non-FDG-avid thickened walls were agents: role in imaging the liver and biliary tree. 48:902–909
linked to a diagnosis of gallbladder cancer. RadioGraphics 2009; 29:1725–1748 21. Czernin J, Schelbert HR. PET/CT in cancer pa-
Nishiyama et al. [49] showed that a delayed 8. Raddatz D, Ramadori G. Carbohydrate metabo- tient management: introduction. J Nucl Med
(146 ± 14 minutes after injection) FDG PET lism and the liver: actual aspects from physiology 2007; 48(suppl 1):2S–3S
scan led to increased FDG uptake of lesions and disease. Z Gastroenterol 2007; 45:51–62 22. Iannaccone R, Piacentini F, Murakami T, et al.
and increased lesion-to-background contrast, 9. Torizuka T, Tamaki N, Inokuma T, et al. In vivo Hepatocellular carcinoma in patients with nonal-
when compared with early-scan (62 ± 8 min- assessment of glucose metabolism in hepatocel- coholic fatty liver disease: helical CT and MR
utes after injection) FDG PET. Shukla et al. lular carcinoma with FDG-PET. J Nucl Med 1995; imaging findings with clinical-pathologic com-
[45] found that FDG PET/CT had a slightly 36:1811–1817 parison. Radiology 2007; 243:422–430
better accuracy (91.6% vs 87.5%) than did 10. Salem N, MacLennan GT, Kuang Y, et al. Quanti- 23. Kawaoka T, Aikata H, Takaki S, et al. FDG positron
MDCT in determining tumor resectability in tative evaluation of 2-deoxy-2[F-18]fluoro-D- emission tomography/computed tomography for the
patients with incidental gallbladder cancer glucose-positron emission tomography imaging detection of extrahepatic metastases from hepatocel-
and no distant metastases. on the woodchuck model of hepatocellular carci- lular carcinoma. Hepatol Res 2009; 39:134–142
It appears that the roles of FDG PET and noma with histological correlation. Mol Imaging 24. Delbeke D, Pinson CW. 11C-acetate: a new tracer
FDG PET/CT in gallbladder cancer have not Biol 2007; 9:135–143 for the evaluation of hepatocellular carcinoma. J
been studied sufficiently to make conclu- 11. Lee JD, Yang WI, Park YN, et al. Different glu- Nucl Med 2003; 44:222–223
sive statements about their clinical value. At cose uptake and glycolytic mechanisms between 25. Park JW, Kim JH, Kim SK, et al. A prospective
this time, however, these modalities seem to hepatocellular carcinoma and intrahepatic mass- evaluation of 18F-FDG and 11C-acetate PET/CT
be useful in differentiating malignant wall forming cholangiocarcinoma with increased (18) for detection of primary and metastatic hepatocel-
thickening and benign wall thickening, and F-FDG uptake. J Nucl Med 2005; 46:1753–1759 lular carcinoma. J Nucl Med 2008; 49:1912–1921
in the preoperative diagnostic algorithm to 12. Roh MS, Jeong JS, Kim YH, Kim MC, Hong SH. 26. Kurtaran A, Becherer A, Pfeffel F, et al. 18F-fluo-
assess proper surgical candidates. Diagnostic utility of GLUT1 in the differential rodeoxyglucose (FDG)-PET features of focal
diagnosis of liver carcinomas. Hepatogastroen- nodular hyperplasia (FNH) of the liver. Liver
Conclusion terology 2004; 51:1315–1318 2000; 20:487–490
In summary, the utility of PET and PET/ 13. Khan MA, Combs CS, Brunt EM, et al. Positron 27. Son HB, Han CJ, Kim BI, et al. Evaluation of
CT in imaging primary hepatobiliary lesions emission tomography scanning in the evaluation various hepatic lesions with positron emission to-
varies according to the type and location of of hepatocellular carcinoma. J Hepatol 2000; mography (in Korean). Taehan Kan Hakhoe Chi
the tumor. There is a consistent benefit to the 32:792–797 2002; 8:472–480
use of PET for detection and staging, which 14. Ho CL, Yu SC, Yeung DW. 11C-acetate PET imag- 28. Delbeke D, Martin WH, Sandler MP, Chapman
ultimately helps to establish the best course ing in hepatocellular carcinoma and other liver WC, Wright JK Jr, Pinson CW. Evaluation of be-
of treatment and to determine prognosis. masses. J Nucl Med 2003; 44:213–221 nign vs malignant hepatic lesions with positron
15. Wudel LJ Jr, Delbeke D, Morris D, et al. The role emission tomography. Arch Surg 1998; 133:510–
References of [18F]fluorodeoxyglucose positron emission to- 515, discussion 515–516
1. Bosch FX, Ribes J, Díaz M, Cléries R. Primary mography imaging in the evaluation of hepatocel- 29. Ishak K, Anthony PP, Sobin LH. Histological typ-
liver cancer: worldwide incidence and trends. lular carcinoma. Am Surg 2003; 69:117–124, dis- ing of tumours of the liver, 2nd ed. WHO interna-
Gastroenterology 2004; 127(suppl 1):S5–S16 cussion 124–126 tional histological classification of tumours. New
2. Oliveri F, Brunetto MR, Actis GC, Bonino F. 16. Rose AT, Rose DM, Pinson CW, et al. Hepatocel- York, NY: Springer, 1994
Pathobiology of chronic hepatitis virus infection lular carcinoma outcomes based on indicated 30. Kim JY, Kim MH, Lee TY, et al. Clinical role of
treatment strategy. Am Surg 1998; 64:1128–1134, 18F-FDG PET-CT in suspected and potentially
and hepatocellular carcinoma (HCC). Ital J Gas-
troenterol 1991; 23:498–502 discussion 1134–1135 operable cholangiocarcinoma: a prospective
3. Fabris C, Toniutto P, Falleti E, et al. MTHFR 17. Shiomi S, Nishiguchi S, Ishizu H, et al. Useful- study compared with conventional imaging. Am J
C677T polymorphism and risk of HCC in patients ness of positron emission tomography with fluo- Gastroenterol 2008; 103:1145–1151
with liver cirrhosis: role of male gender and alco- rine-18-fluorodeoxyglucose for predicting out- 31. Petrowsky H, Wildbrett P, Husarik DB, et al. Im-
hol consumption. Alcohol Clin Exp Res 2009; come in patients with hepatocellular carcinoma. pact of integrated positron emission tomography
33:102–107 Am J Gastroenterol 2001; 96:1877–1880 and computed tomography on staging and man-
4. Murillas J, Del Río M, Riera M, et al. Increased 18. Kong YH, Han CJ, Lee SD, et al. Positron emis- agement of gallbladder cancer and cholangiocar-
incidence of hepatocellular carcinoma (HCC) in sion tomography with fluorine-18-fluorodeoxy- cinoma. J Hepatol 2006; 45:43–50
AJR:197, August 2011 W263
Sacks et al.
Downloaded from ajronline.org by 2a02:6b68:988e:0:96ba:ea07:aef1:34a2 on 11/17/23 from IP address 2a02:6b68:988e:0:96ba:ea07:aef1:34a2. Copyright ARRS. For personal use only; all rights reserved
32. Jadvar H, Henderson RW, Conti PS. [F-18]fluoro- strictures using delayed 18F-FDG PET/CT: pre- 206:57–65
deoxyglucose positron emission tomography and liminary results for 22 patient studies. J Nucl Med 44. Fong Y, Kemeny N, Lawrence TS. Cancer of the
positron emission tomography: computed tomog- 2005; 46:1158–1163 liver and biliary tree. In: DeVita VT Jr, Hellman
raphy in recurrent and metastatic cholangiocarci- 39. Seo S, Hatano E, Higashi T, et al. Fluorine-18 S, Rosenberg SA (eds.). Cancer: principles and
noma. J Comput Assist Tomogr 2007; 31:223–228 fluorodeoxyglucose positron emission tomogra- practice of oncology, 6th ed. Philadelphia, PA:
33. Kluge R, Schmidt F, Caca K, et al. Positron emis- phy predicts lymph node metastasis, P-glycopro- Lippincott Williams & Wilkins, 2001:1187–1202
sion tomography with [(18)F]fluoro-2-deoxy-D- tein expression, and recurrence after resection in 45. Shukla PJ, Barreto SG, Arya S, et al. Does PET-
glucose for diagnosis and staging of bile duct can- mass-forming intrahepatic cholangiocarcinoma. CT scan have a role prior to radical re-resection
cer. Hepatology 2001; 33:1029–1035 Surgery 2008; 143:769–777 for incidental gallbladder cancer? HPB (Oxford)
34. Anderson CD, Rice MH, Pinson CW, Chapman 40. Moon CM, Bang S, Chung JB, et al. Usefulness of 2008; 10:439–445
WC, Chari RS, Delbeke D. Fluorodeoxyglucose 18F-fluorodeoxyglucose positron emission tomog- 46. Koh T, Taniguchi H, Yamaguchi A, Kunishima S,
PET imaging in the evaluation of gallbladder car- raphy in differential diagnosis and staging of Yamagishi H. Differential diagnosis of gallblad-
cinoma and cholangiocarcinoma. J Gastrointest cholangiocarcinomas. J Gastroenterol Hepatol der cancer using positron emission tomography
Surg 2004; 8:90–97 2008; 23:759–765 with fluorine-18-labeled fluoro-deoxyglucose
35. Nakeeb A, Pitt HA, Sohn TA, et al. Cholangiocar- 41. Kim YJ, Yun M, Lee WJ, Kim KS, Lee JD. Use- (FDG-PET). J Surg Oncol 2003; 84:74–81
cinoma: a spectrum of intrahepatic, perihilar, and fulness of 18F-FDG PET in intrahepatic cholan- 47. Rodríguez-Fernández A, Gómez Río M, Llamas
distal tumors. Ann Surg 1996; 224:463–473, dis- giocarcinoma. Eur J Nucl Med Mol Imaging Elvira JM, et al. Positron-emission tomography
cussion 473–475 2003; 30:1467–1472 with fluorine-18-fluoro-2-deoxy-D-glucose for
36. Li J, Kuehl H, Grabellus F, et al. Preoperative as- 42. Ramos-Font C, Santiago Chinchilla A, Rodrí- gallbladder cancer diagnosis. Am J Surg 2004;
sessment of hilar cholangiocarcinoma by dual-mo- guez-Fernández A, Rebollo Aquirre AC, Gómez 188:171–175
dality PET/CT. J Surg Oncol 2008; 98:438–443 Río M, Llamas Elvira JM. Gallbladder cancer 48. Oe A, Kawabe J, Torii K, et al. Distinguishing be-
37. Kato T, Tsukamoto E, Kuge Y, et al. Clinical role staging with 18F-FDG PET-CT (in Spanish). Rev nign from malignant gallbladder wall thickening
of (18)F-FDG PET for initial staging of patients Esp Med Nucl 2009; 28:74–77 using FDG-PET. Ann Nucl Med 2006; 20:699–703
with extrahepatic bile duct cancer. Eur J Nucl 43. Corvera CU, Blumgart LH, Akhurst T, et al. 18F- 49. Nishiyama Y, Yamamoto Y, Fukunaga K, et al.
Med Mol Imaging 2002; 29:1047–1054 fluorodeoxyglucose positron emission tomogra- Dual-time-point 18F-FDG PET for the evaluation
38. Reinhardt MJ, Strunk H, Gerhardt T, et al. Detec- phy influences management decisions in patients of gallbladder carcinoma. J Nucl Med 2006;
tion of Klatskin’s tumor in extrahepatic bile duct with biliary cancer. J Am Coll Surg 2008; 47:633–638
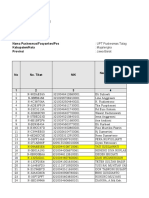
Fig. 1—56-year-old patient with hepatitis C and advanced
hepatocellular carcinoma.
A–C, Maximum intensity projection (MIP) PET (A), axial CT (B),
and fused PET/CT (C) images show multiple hepatic lesions
(arrow, B and C), including dominant lesion in segment 5/8 with
maximum standardized uptake value (SUVmax) of 3.6.
D–F, MIP PET (D), axial CT (E), and fused PET/CT (F) images
show large necrotic hypermetabolic peripancreatic lymph
node (arrow, E and F) with SUVmax of 8.5.
W264 AJR:197, August 2011
PET/CT in Primary Hepatobiliary Tumors
Downloaded from ajronline.org by 2a02:6b68:988e:0:96ba:ea07:aef1:34a2 on 11/17/23 from IP address 2a02:6b68:988e:0:96ba:ea07:aef1:34a2. Copyright ARRS. For personal use only; all rights reserved
Fig. 2—47-year-old man with hepatitis B and C and elevated
α-fetoprotein levels.
A, Axial T1-weighted MRI scan shows lesion (arrow)
measuring 4.5 × 3.5 cm in segment 2 of liver. Patient underwent
chemoembolization of liver lesion. PET/CT performed 20 days later
showed residual hepatic disease with pulmonary metastases.
B, Axial fused PET/CT shows large necrotic 9.9 × 4.7 × 9.9
cm mass (arrow) in left lobe of liver with hypermetabolic rim,
consistent with patient’s history of chemoembolization of
large hepatocellular carcinoma.
C, PET/CT shows hypermetabolic lesion (arrow) in middle lobe
of right lung with maximum standardized uptake value (SUVmax)
of 2.6, consistent with pulmonary metastasis. Patient received
systemic chemotherapy with Sorafenib (Nexavar, Bayer
HealthCare) for 3 months, and follow-up PET/CT revealed
significant worsening of disease in both liver and lung.
D, Axial fused PET/CT shows interval increase in extent and
degree of hypermetabolic activity, with SUVmax of 6.6, surrounding
large centrally photopenic defect (arrow) within left lobe of liver.
E and F, CT in lung window (E) and fused PET/CT (F) show
multiple hypermetabolic pulmonary nodules consistent with
progression of pulmonary metastases.
Fig. 3—65-year-old man with history of ulcerative colitis
requiring colectomy and primary sclerosing cholangitis.
A, CT scan performed during his hospitalization for
coronary artery bypass graft revealed low-attenuation
mass (arrow) in left lobe of liver.
B and C, PET/CT shows intensely FDG-avid 6 × 5 cm mass
(arrow, B and C) with central area of decreased activity
(necrosis). No distant metastases were identified. Biopsy
revealed cholangiocarcinoma, and mass was successfully
resected.
Fig. 4—75-year-old female smoker who presented with
right upper quadrant pain.
A, Contrast-enhanced CT revealed mass (arrow) anterior
to gallbladder, arising from liver or gallbladder. Biopsy
revealed gallbladder cancer.
B and C, PET/CT shows intensely FDG-avid mass (arrow,
B) arising from anterior wall of gallbladder and second
FDG-avid right apical lung mass (arrow, C). With biopsy-
confirmed non-small-cell lung cancer, patient received
palliative therapy for both malignancies.
F O R YO U R I N F O R M AT I O N
The Self-Assessment Module accompanying this article can be accessed via www.ajronline.org at the article link
labeled “CME/SAM.”
The American Roentgen Ray Society is pleased to present these Self-Assessment Modules (SAMs) as part of its
commitment to lifelong learning for radiologists. Each SAM is composed of two journal articles along with questions,
solutions, and references, which can be found online. Read each article, then answer the accompanying questions and
review the solutions online. After submitting your responses, you'll receive immediate feedback and benchmarking data
to enable you to assess your results against your peers.
Continuing medical education (CME) and SAM credits are available in each issue of the AJR and are free to ARRS
members. Not a member? Call 1-866-940-2777 (from the U.S. or Canada) or 703-729-3353 to speak to an ARRS
membership specialist and begin enjoying the benefits of ARRS membership today!
AJR:197, August 2011 W265
You might also like
- MSDS - HelizymeDocument10 pagesMSDS - HelizymeNurhari OgiNo ratings yet
- Ineffective Health MaintenanceDocument2 pagesIneffective Health MaintenanceBlessie Fernandez100% (1)
- Prenatal Brochure 2011-FF - Health Power For MinoritiesDocument2 pagesPrenatal Brochure 2011-FF - Health Power For MinoritiesNorma J. Goodwin, MDNo ratings yet
- Clinical Practice in PET CT For The Management of Head and Neck Squamous Cell CancerDocument15 pagesClinical Practice in PET CT For The Management of Head and Neck Squamous Cell CancerlkitkatgirlNo ratings yet
- Ringe Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 1 Protocol Optimization and Lesion Appearance inDocument16 pagesRinge Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 1 Protocol Optimization and Lesion Appearance indynachNo ratings yet
- RENAL ScoreDocument5 pagesRENAL ScoreMurilo CamposNo ratings yet
- Ajr 10 5540Document9 pagesAjr 10 5540Pepe pepe pepeNo ratings yet
- CTA ExtremityDocument8 pagesCTA Extremityrio trisonaNo ratings yet
- Belloni Et Al 2012 Mri of CardiomyopathyDocument11 pagesBelloni Et Al 2012 Mri of CardiomyopathyRadiologyNo ratings yet
- LIVER CALCIFIED MASSES Types AlgorithmDocument11 pagesLIVER CALCIFIED MASSES Types Algorithmcalustre2016No ratings yet
- Ajr 18 20947Document6 pagesAjr 18 20947Amartya PalNo ratings yet
- Solid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaDocument11 pagesSolid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaTạ Minh ZSNo ratings yet
- Cruite Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 2 Protocol Optimization and Lesion Appearance inDocument13 pagesCruite Et Al 2012 Gadoxetate Disodium Enhanced Mri of The Liver Part 2 Protocol Optimization and Lesion Appearance indynachNo ratings yet
- Dual-Energy CT of The Brain and Intracranial VesselsDocument8 pagesDual-Energy CT of The Brain and Intracranial VesselsMuhammad Rafiee SukmaNo ratings yet
- Current Concepts of Hip Arthroplasty For Radiologists: Part 1, Features and Radiographic AssessmentDocument12 pagesCurrent Concepts of Hip Arthroplasty For Radiologists: Part 1, Features and Radiographic AssessmentGERARDO TORRES RUIZNo ratings yet
- Cancer FibromamelarDocument16 pagesCancer FibromamelarMarcela DuarteNo ratings yet
- AJR Chest Radiography in The ICU Parte II 2012Document10 pagesAJR Chest Radiography in The ICU Parte II 2012wfranelicNo ratings yet
- Radlink Issue 2 2008Document2 pagesRadlink Issue 2 2008RadlinkSingaporeNo ratings yet
- Effect of Patient Size On Radiation Dose of Abdominal MDCT With Automatic Tube Current ModulationDocument6 pagesEffect of Patient Size On Radiation Dose of Abdominal MDCT With Automatic Tube Current Modulationdestian ryanNo ratings yet
- 8 Ortho Oncology - 210217 - 194331Document11 pages8 Ortho Oncology - 210217 - 194331Nabil AhmedNo ratings yet
- AJR Chest Radiography in The ICU Parte I 2012Document9 pagesAJR Chest Radiography in The ICU Parte I 2012wfranelicNo ratings yet
- AVC p2Document14 pagesAVC p2Elena VelcuNo ratings yet
- CT On GI TractDocument10 pagesCT On GI TractRizky Putri Agustina RumapeaNo ratings yet
- Imaging Assessment of Hepatocellular Carcinoma Response To Locoregional and Systemic TherapyDocument19 pagesImaging Assessment of Hepatocellular Carcinoma Response To Locoregional and Systemic Therapyanra kusumaNo ratings yet
- Identifying The Anatomical Variations of The.20Document7 pagesIdentifying The Anatomical Variations of The.20FERNANDO ALVESNo ratings yet
- Radiology of Chest Wall MassesDocument11 pagesRadiology of Chest Wall MassesDevina BumiNo ratings yet
- New Developments of PetDocument59 pagesNew Developments of Petmm_555_ssNo ratings yet
- Chest Radiography in The ICUDocument9 pagesChest Radiography in The ICUNicolás HonoresNo ratings yet
- PosterDocument1 pagePosterKoushul RamjattunNo ratings yet
- Approprate Use NETDocument11 pagesApproprate Use NETkasturi.rangan1234No ratings yet
- Articulo 1recto SuperiorDocument7 pagesArticulo 1recto SuperiorCarolinaNo ratings yet
- Imaging of Cholecystitis: ResidentsDocument8 pagesImaging of Cholecystitis: ResidentsandrefaelNo ratings yet
- Ajr 2Document10 pagesAjr 2Fika FathiaNo ratings yet
- Neoplastic Myelopathies: Continuumaudio Interviewavailable OnlineDocument22 pagesNeoplastic Myelopathies: Continuumaudio Interviewavailable OnlineDalwadi1No ratings yet
- The Evolution of MRI of The Prostate: The Past, The Present, and The FutureDocument13 pagesThe Evolution of MRI of The Prostate: The Past, The Present, and The Futurelintang dmNo ratings yet
- TACE Standards of PracticeDocument17 pagesTACE Standards of PracticeRuminRuNo ratings yet
- ClassificationDocument8 pagesClassificationbarathy.kbNo ratings yet
- R02Y2002N01A0003Document27 pagesR02Y2002N01A0003Roseck BlackNo ratings yet
- Rico Harke Abraham Siagian 021801009 Tugas ResumeDocument18 pagesRico Harke Abraham Siagian 021801009 Tugas ResumeGebrilya TendeanNo ratings yet
- Cross-Sectional Imaging of Intrahepatic Cholangiocarcinoma: Development, Growth, Spread, and PrognosisDocument12 pagesCross-Sectional Imaging of Intrahepatic Cholangiocarcinoma: Development, Growth, Spread, and PrognosisNikos SerifisNo ratings yet
- Document My Assignment TherapyDocument5 pagesDocument My Assignment TherapynanaaishamahmudgazaraNo ratings yet
- 2021 The Use of Fecal Calprotectin Testing in PaediatricDocument24 pages2021 The Use of Fecal Calprotectin Testing in PaediatricKhadijah Rizky SumitroNo ratings yet
- Spe 68328 MsDocument1 pageSpe 68328 MsAbed Alftah AgabNo ratings yet
- CT Mri CCHDocument21 pagesCT Mri CCHrizkianaNo ratings yet
- Analysis of Enhancement Pattern of Flat Gallbladder Wall Thickening On MDCT To Differentiate Gallbladder Cancer From CholecystitisDocument7 pagesAnalysis of Enhancement Pattern of Flat Gallbladder Wall Thickening On MDCT To Differentiate Gallbladder Cancer From CholecystitisSamuel WidjajaNo ratings yet
- Renal Cell Carcinoma: Diagnosis, Staging, and SurveillanceDocument13 pagesRenal Cell Carcinoma: Diagnosis, Staging, and SurveillanceEmanuelleReisNo ratings yet
- Frequency of Egfr Mutations in Lung Adenocarcinoma.40Document8 pagesFrequency of Egfr Mutations in Lung Adenocarcinoma.40Tanaka TanakaNo ratings yet
- Intrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationDocument13 pagesIntrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationIndra PrimaNo ratings yet
- Ajr.12.10010 Aortic RootDocument9 pagesAjr.12.10010 Aortic Rootfranti76No ratings yet
- 2003 Poster SampleDocument1 page2003 Poster SampleDry LandNo ratings yet
- Pet BrochureDocument20 pagesPet BrochureSheikh Hasnain AliNo ratings yet
- Background: Relation Between Hyperlcoagulation With 12 Months of Survival Monitoring On AstrocytomaDocument1 pageBackground: Relation Between Hyperlcoagulation With 12 Months of Survival Monitoring On AstrocytomajhnaidillaNo ratings yet
- TerrenceDocument3 pagesTerrenceVinayak K gowdaNo ratings yet
- Recent Advances in PETCTDocument30 pagesRecent Advances in PETCTDivyaNo ratings yet
- Yty 116Document5 pagesYty 116Intania RatnaNo ratings yet
- Factors Affecting Accuracy of SuvDocument11 pagesFactors Affecting Accuracy of SuvTurkiNo ratings yet
- Lee2017imagerie StadeDocument13 pagesLee2017imagerie StadenimaelhajjiNo ratings yet
- Evaluation of Total Corneal Power MeasurementsDocument7 pagesEvaluation of Total Corneal Power MeasurementsMariana Luzardo bravoNo ratings yet
- Bateni Et Al 2013 Imaging Key Wrist Ligaments What The Surgeon Needs The Radiologist To KnowDocument7 pagesBateni Et Al 2013 Imaging Key Wrist Ligaments What The Surgeon Needs The Radiologist To KnowRadiologyNo ratings yet
- Pvy036 PDFDocument12 pagesPvy036 PDFHimanshu dubeyNo ratings yet
- An Automated System For Liver CT Enhancement and SegmentationDocument6 pagesAn Automated System For Liver CT Enhancement and Segmentationshamalu2011No ratings yet
- What The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyDocument8 pagesWhat The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyQonita Aizati QomaruddinNo ratings yet
- FDG PET CT in The Management of Lymphomas Current Status and FutureDocument19 pagesFDG PET CT in The Management of Lymphomas Current Status and FuturelkitkatgirlNo ratings yet
- The Impact of Infection and Inflammation in OncoloDocument9 pagesThe Impact of Infection and Inflammation in OncololkitkatgirlNo ratings yet
- Uematsu Et Al 2012 Comparison of FDG Pet and Spect For Detection of Bone Metastases in Breast CancerDocument8 pagesUematsu Et Al 2012 Comparison of FDG Pet and Spect For Detection of Bone Metastases in Breast CancerlkitkatgirlNo ratings yet
- The Place of FDG PET CT in Renal Cell Carcinoma - Value and LimitationsDocument7 pagesThe Place of FDG PET CT in Renal Cell Carcinoma - Value and LimitationslkitkatgirlNo ratings yet
- The Value of FDG PET CT Scans To Evaluate Bone Marrow in Haemato-Oncological ConditionsDocument9 pagesThe Value of FDG PET CT Scans To Evaluate Bone Marrow in Haemato-Oncological ConditionslkitkatgirlNo ratings yet
- CYBERBULLYINGDocument2 pagesCYBERBULLYINGAdinda CahayaNo ratings yet
- PHED 10032 Individual, Dual, and Combative SportsDocument52 pagesPHED 10032 Individual, Dual, and Combative SportsMicmic CalivaNo ratings yet
- To Do List For HACCPDocument2 pagesTo Do List For HACCPChâu TrầnNo ratings yet
- Institutionalized ElderlyDocument20 pagesInstitutionalized ElderlySourav DeyNo ratings yet
- Nama Puskesmas/Fasyankes/Pos Kabupaten/Kota Provinsi:: UPT Puskesmas Talaga: Majalengka: Jawa BaratDocument20 pagesNama Puskesmas/Fasyankes/Pos Kabupaten/Kota Provinsi:: UPT Puskesmas Talaga: Majalengka: Jawa BaratNoeNuraeniNo ratings yet
- 2023 GKS-U Application FormsDocument11 pages2023 GKS-U Application FormsNaomi FernándezNo ratings yet
- SOP On Operation and Calibration of Water BathDocument5 pagesSOP On Operation and Calibration of Water Bathfawaz khalilNo ratings yet
- 13.1 Social Sectors Reforms (By Ayussh Sanghi)Document37 pages13.1 Social Sectors Reforms (By Ayussh Sanghi)harmless wolfNo ratings yet
- Effective Study Habit : By: Patra Cleo AlcomendasDocument8 pagesEffective Study Habit : By: Patra Cleo AlcomendasMary Rose S. BonilloNo ratings yet
- 7.artikel JKM Vol. 14 No. 2 Desember 2021 Case Report JKM Edwin Anto Pakpahan 55 63Document9 pages7.artikel JKM Vol. 14 No. 2 Desember 2021 Case Report JKM Edwin Anto Pakpahan 55 63waode apriyaniNo ratings yet
- HeirarchyDocument3 pagesHeirarchyMazikeen LilimNo ratings yet
- Week 7 Guide Questions AnswersDocument7 pagesWeek 7 Guide Questions AnswersKathleenMarieAlforteNo ratings yet
- Service Stream EDP Permit Training Participant WorkbookDocument19 pagesService Stream EDP Permit Training Participant Workbookshana.mxNo ratings yet
- People v. Robiños, G.R. No. 138453, 29 May 2002Document13 pagesPeople v. Robiños, G.R. No. 138453, 29 May 2002Isabella EncarnacionNo ratings yet
- OBSTETRIC NURSING Hand Out UPANG INHOUSE 2022Document7 pagesOBSTETRIC NURSING Hand Out UPANG INHOUSE 2022Mary Ann G. CorsanesNo ratings yet
- Eyhance BrochureDocument2 pagesEyhance Brochuredr.Nurcahya Ardian Bramantha,SpMNo ratings yet
- Isolation and Molecular Characterization of Salmonella Enterica, Escherichia Coli O157-H7 and Shigella Spp. From Meat and Dairy Products in EgyptDocument6 pagesIsolation and Molecular Characterization of Salmonella Enterica, Escherichia Coli O157-H7 and Shigella Spp. From Meat and Dairy Products in EgyptAffan GaffarNo ratings yet
- Minimally Invasive When? How? Why?: Access Cavity Preparation in EndodonticsDocument4 pagesMinimally Invasive When? How? Why?: Access Cavity Preparation in EndodonticsdoctorlupuNo ratings yet
- Bura - Stephane - Beyond ElizaDocument79 pagesBura - Stephane - Beyond ElizaphiloNo ratings yet
- Maternal Lec Week 1 3Document4 pagesMaternal Lec Week 1 3Althea ManarpiisNo ratings yet
- Tyler Twist ProtocolDocument7 pagesTyler Twist ProtocolchinitosNo ratings yet
- Red Orchid - Best PracticesDocument80 pagesRed Orchid - Best PracticeslabiaernestoNo ratings yet
- Nose Unblocking ExerciseDocument1 pageNose Unblocking Exercisebharat panchalNo ratings yet
- SteerBridge JD - CFM-IDIQ San Francisco - Electrical EngineerDocument3 pagesSteerBridge JD - CFM-IDIQ San Francisco - Electrical Engineersmrasteg12No ratings yet
- Anecdotal EvidenceDocument19 pagesAnecdotal EvidenceMedia Development FoundationNo ratings yet
- Bobcat 226 yDocument19 pagesBobcat 226 yEduardoNo ratings yet
- AISA CP Handbook 2016Document83 pagesAISA CP Handbook 2016Rhea EscleoNo ratings yet