Professional Documents
Culture Documents
Chylothorax Original
Chylothorax Original
Uploaded by
Maria CostandachiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chylothorax Original
Chylothorax Original
Uploaded by
Maria CostandachiCopyright:
Available Formats
Chylothorax
Diagnostic and monitoring recommendations:
1. Diagnostic thoracentesis (pleural fluid analysis)
a. WBC>1,000/uL
b. >70% lymphocytes in cell count
c. Triglyceride level >110 mg/dL (if being fed)
2. Lab monitoring of documented chylothoraxa
a. Echocardiogram, MRA, or venogram to evaluate for thrombosis in the left jugular, subclavian,
innominate veins, or superior vena cava.
b. Na, K, Glucose, Ca, BUN, Total protein and albumin at least 2x/week
c. Antithrombin III level 2 x/week until stable, IF ≥25 ml/kg day or thrombosis
d. PT, PTT and Fibrinogen weekly
e. Hct 1x/week
f. Total IgG level q 1 week
g. Direct bilirubin q week if NPO > 2 weeks (Nutrition Service recommendation)
h. Free T4 and TSH q 2 weeks, if using Octreotide
*The above schedule may be altered based on volume of chyle output or clinical stability of the patient.
Treatment:
1. Thoracostomy drainage to maintain lung inflation and approximate the pleural surfaces.
2. If a thrombosis is present, consider thrombolysis or heparin (Refer to guideline for Thrombosis) and consider
Hematology Service consult.
3. NPO and TPN.
4. If thrombus is in the upper venous system, central venous catheters should be placed in the lower body.
5. Fluids should be restricted and diuretics utilized to control edema and reduce chyle flow.
6. Small volume (<25 ml/kg/day) effusions may be replaced with crystalloid or 5% albumin.
HOWEVER, if the coagulation status is abnormal, FFP should be used.
7. Large volume (≥25 ml/kg/day) effusions should be replaced with FFP at a ratio of 0.5-0.75 ml FFP/ml
of chylous output, as long as clotting function and ATIII levels remain normal.
2545 Chicago Ave. S. Suite 512 Minneapolis, MN 55404
(P) 612.813.6475 (F) 612.813.6983 mnneo.org 24/7 CONSULT LINE 1.888.455.BABY
8. Additional volume needs may be met with crystalloid solutions or possibly 5% or 25% albumin,
IF coagulation status normal.
9. Keep serum albumin concentration ≥2 gm/dL with 25% albumin (5 ml/kg).
10. Keep ATIII concentration >50% in first month, >60% @ 1-3 mo, with ATIII concentrate (75 units/kg IV)
or by increasing the ratio of replacement with FFP for chylous output. Consider Hematology consult if there
is a thrombus and consideration is being given to heparin therapy.
11. Octreotide therapy should be considered for large volume losses. Start at 1 mcg/kg/hr by continuous infusion
and increase by 1 mcg/kg/hour each day to max of 10. Note: It is not compatible with most other things and
must be mixed in normal saline or D5W. If separate vascular access is a problem, it may be given
subcutaneously or by IV bolus; starting at 10 mcg/kg/day and increasing rapidly to 40 mcg/kg/day divided
q 6 hours. Glucose must be monitored closely due to propensity to increase blood glucose. If octreotide
works, it usually does so in two weeks. There are significant side effects associated with octreotide and
is generally reserved for a last resort therapy.
12. If after 6 weeks* there is no improvement, consider:
a. Physical or chemical pleurodesis
b. Thorascopic sealing with fibrin glue
c. Ligation of the thoracic duct
d. Pleuroperitoneal shunt (ineffective if RA pressure is >25 mmHg).
*Patients with elevated venous pressure or intravascular clots obstructing the thoracic duct are less likely
to respond to conservative management and a surgical solution may be justified earlier.
13. Documentation of daily output and relevant interventions is highly recommended.
14. Consider Hematology consult, if there is a thrombus and consideration is being given to heparin therapy.
Following resolution of the chylothorax, enteral nutrition is reintroduced with a fat-free formula
(ProViMin with polycose). A stepwise protocol is used to increase volumes and then reintroduce short
and medium chain fats followed by a final step of reintroduction of long chain fats. Please refer to the
ProViMin Feeding Protocol below in Table 1.
ProViMin Recommendations:
The ProViMin regimen is not meant for extended use and should be gradually advanced according to the steps
listed below (Table 1 on next page). Advancement of feedings depends on the patient’s clinical status and
response to the current feeding regimen. The percentage of enteral calories from carbohydrate decreases as
the percentage from fat increases, always maintaining a caloric density of 20 cal/oz. The caloric density should
not routinely be increased at the first 3 or 4 steps because of the higher osmolality of a formula that is high in
carbohydrate and low in fat.
2545 Chicago Ave. S. Suite 512 Minneapolis, MN 55404
(P) 612.813.6475 (F) 612.813.6983 mnneo.org 24/7 CONSULT LINE 1.888.455.BABY
Advance volume as tolerated until medically ready to introduce and advance enteral fat using MCT (Steps
2 – 5, below). As formula volume is increased, decrease dextrose and protein in TPN. Parenteral lipids can be
decreased (0.5-1gm/kg/day minimum) as a source of calories as MCT is increased but should be continued as a
source of essential fatty acids until the patient is tolerating step #6 well and is ready to advance to step #7.
Table 1. ProViMin Recommendations
FORMULATION OF ProViMin COMPOSITION
1. ProViMin + Polycose = 20 cal/oz (no added fat) 88%CHO, 12%Prot, 0.5%Fat
2. ProViMin + Polycose + 10% MCT = 20 cal/oz 77%CHO, 12%Prot, 11%Fat
3. ProViMin + Polycose + 20% MCT = 20 cal/oz 67%CHO, 12%Prot, 21%Fat
4. ProViMin + Polycose + 30% MCT = 20 cal/oz 57%CHO, 12%Prot, 31%Fat
5. ProViMin + Polycose + 40% MCT = 20 cal/oz 46%CHO, 12%Prot, 42%Fat
6. ProViMin + Polycose + MCT + 4% LCT = 20 cal/oz 46%CHO, 12%Prot, 42%Fat
7. ProViMin + Polycose + MCT + 10% LCT = 20 cal/oz 46%CHO, 12%Prot, 42%Fat
8. Change to Enfaport 41% CHO, 14%Prot, 45%Fat
(84% of fat is MCT, 16% LCT)
Skimmed Breast Milk:
Low fat breast milk is available from some breast milk banks. The Lactation Consultants can help moms partially
skim their own milk to use at the point where adequate LCT tolerance has been demonstrated.
Background
Neonatal chylothorax is a serious, potentially life-threatening problem. Causes include: congenital atresia or
hypolasia of the thoracic duct, lymphatic abnormalities lymphangiomatosis), trauma related to birth,
placement of central venous catheters, thoracic, cardiac, or neck surgery, especially involving the esophagus,
aorta, PDA, or diaphragm, thrombosis of the innominate or subclavian vein, obstruction of the superior vena
cava , or increased central venous pressure. If the etiology is post-surgical it typically appears 1-28 days
later (avg. 7 days), often coincidental with the introduction of dietary fat.
2545 Chicago Ave. S. Suite 512 Minneapolis, MN 55404
(P) 612.813.6475 (F) 612.813.6983 mnneo.org 24/7 CONSULT LINE 1.888.455.BABY
The thoracic duct transports up to 150 mL/kg/day of fluid. Flow rate is dependent on diet (any enteral intake at
all increases flow, but especially long chain fats). It contains a combination of lymphatic and gut-derived
substances. Much dietary fat is absorbed directly into the lymphatic system, however, medium and short chain
fatty acids are absorbed directly into the venous system. The thoracic duct is the main vessel for the return of
extravasated proteins to the circulation, giving it a major role in fluid homeostasis. The chemical composition of
chyle is noted below in Table 2.
Table 2. Content of Chyle
Component Amount
Total fat 0.4-5 g/dL
Total cholesterol 65-200 mg/dL
Total protein 2.2-5.9 g/dL
Albumin 1.1-4.1 g/dL
Globulins 1.1-3.1 g/dL
Fibrinogen 16-24 g/dL (>25% of plasma)
Anti-thrombin globulin >25% of plasma
Prothrombin >25% of plasma
Lymphocytes 400-6000/mm3
RBCs 50-600/mm3
Glucose Similar to plasma
Electrolytes Similar to plasma
Calcium 3.4-6 mMol/L
Phosphorus 0.8-4.2 mMol/L
Urea 1.4-3 mMol/L
Pancreatic lipase 0.5-2.4 units/ml
Amylase 50-83 units/ml
AST 22-40 units/ml
Alkaline phosphatase 2-4.8 units/ml
Fat soluble vitamins ??? concentrations
2545 Chicago Ave. S. Suite 512 Minneapolis, MN 55404
(P) 612.813.6475 (F) 612.813.6983 mnneo.org 24/7 CONSULT LINE 1.888.455.BABY
You might also like
- Sample Ultrasound ReportDocument3 pagesSample Ultrasound ReportPapadoveNo ratings yet
- Assignment On TPNDocument14 pagesAssignment On TPNBhawna Joshi100% (8)
- The Ehra Book of Intervntional Electrophysiology - OxfordDocument321 pagesThe Ehra Book of Intervntional Electrophysiology - Oxfordmorris njageNo ratings yet
- Anatomy & Physiology of DengueDocument8 pagesAnatomy & Physiology of DengueYim Yim25% (4)
- Mark K Audio LecturesDocument62 pagesMark K Audio LecturesMelissa Sapp100% (6)
- Nutritional Management of Chyle Leaks: An Update: Nutrition Issues in Gastroenterology, Series #94Document13 pagesNutritional Management of Chyle Leaks: An Update: Nutrition Issues in Gastroenterology, Series #94mmmdeandradeNo ratings yet
- Final Case StudyDocument18 pagesFinal Case Studyapi-487702467100% (1)
- Paracentesis - SIR GGR Survival GuideDocument4 pagesParacentesis - SIR GGR Survival GuidesirrfsNo ratings yet
- Lung Collapse: A Review: Dr. Girish Kukade Radiology Department, AFHDocument61 pagesLung Collapse: A Review: Dr. Girish Kukade Radiology Department, AFHkukadegirishNo ratings yet
- Anatomy MC Question CH 17-22Document4 pagesAnatomy MC Question CH 17-22lmaoheartsNo ratings yet
- Total Parenteral NutritionDocument9 pagesTotal Parenteral NutritionUday Kumar100% (1)
- Keto LogDocument7 pagesKeto LogKim Justin InfantadoNo ratings yet
- Total Parenteral Nutrition in NeonatesDocument5 pagesTotal Parenteral Nutrition in NeonatesRisma WatiNo ratings yet
- CyclosporineDocument24 pagesCyclosporinesanchit_J14No ratings yet
- Chyle LeakDocument15 pagesChyle Leakapi-590506208No ratings yet
- Acute Fatty Liver Versus HELLPDocument44 pagesAcute Fatty Liver Versus HELLPrainmaker77771121100% (1)
- Lipid Lowering AngentDocument22 pagesLipid Lowering AngentDave BraveNo ratings yet
- Fatty Liver Disease of CattleDocument4 pagesFatty Liver Disease of Cattleابراهيم القويعىNo ratings yet
- Neonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualDocument7 pagesNeonatal Parenteral Nutrition: Intensive Care Nursery House Staff ManualNugraha SultanNo ratings yet
- CKD Part 2Document26 pagesCKD Part 2subha95No ratings yet
- Apixaban Eliquis MonographDocument14 pagesApixaban Eliquis MonographTran Minh NgocNo ratings yet
- Liver Cirrhosis Marking KeyDocument5 pagesLiver Cirrhosis Marking KeyChristone “Zuluzulu” ZuluNo ratings yet
- 11 Peri Operative CareDocument43 pages11 Peri Operative CareAdnan MaqboolNo ratings yet
- Total Parenteral NutritionDocument5 pagesTotal Parenteral NutritionjulieNo ratings yet
- Intra LipidDocument5 pagesIntra LipidZeusKimNo ratings yet
- Burns & NutritionDocument36 pagesBurns & NutritionsyedsahibNo ratings yet
- Parenteral Nutrition: Dr. Mehroze Zamir Resident Surgical 4, CHKDocument43 pagesParenteral Nutrition: Dr. Mehroze Zamir Resident Surgical 4, CHKBhagwan DasNo ratings yet
- Metabolic Disorders LONG CHAIN FAT OXIDATION DISORDERSDocument5 pagesMetabolic Disorders LONG CHAIN FAT OXIDATION DISORDERSMahmoud khedrNo ratings yet
- Short Guide Clinical NutritionDocument30 pagesShort Guide Clinical Nutritiontopiq100% (1)
- Acute Kidney Injury (Aki) : MBCHB ViDocument25 pagesAcute Kidney Injury (Aki) : MBCHB ViENOCK BENDERENo ratings yet
- Anaestetic Management of Liver DiseaseDocument86 pagesAnaestetic Management of Liver DiseaseVarun Reddy VNo ratings yet
- Contact Details Name: Hospital Telephone:: This Protocol Has 4 PagesDocument4 pagesContact Details Name: Hospital Telephone:: This Protocol Has 4 PagesCaterina PrepelitaNo ratings yet
- Nutrition Support Internship Case Study 1Document5 pagesNutrition Support Internship Case Study 1api-457873289No ratings yet
- Biochemistry Acute Fatty Liver in Pregnancy Final PPT 1Document21 pagesBiochemistry Acute Fatty Liver in Pregnancy Final PPT 1Gracia Dela CruzNo ratings yet
- Clinical Practice Guidelines: Adrenal Crisis and Acute Adrenal InsufficiencyDocument4 pagesClinical Practice Guidelines: Adrenal Crisis and Acute Adrenal InsufficiencyDianeAbonitaNo ratings yet
- I V E C C S 2004: Luid TherapyDocument5 pagesI V E C C S 2004: Luid TherapyCaraiman RalucaNo ratings yet
- KabivenDocument11 pagesKabivenstylussimoNo ratings yet
- Use of Peptide Growth Factors For Adult Patients With Intestinal Failure2018Document12 pagesUse of Peptide Growth Factors For Adult Patients With Intestinal Failure2018Ramez AntakiaNo ratings yet
- Parental Nutrition TherapyDocument52 pagesParental Nutrition Therapysamarshahab320No ratings yet
- Fluid Therapy - PICU Oct 2010 PDFDocument4 pagesFluid Therapy - PICU Oct 2010 PDFSiti ChodijahNo ratings yet
- Case StudyDocument5 pagesCase Studyapi-247850107No ratings yet
- Diabetic Ketoacidosis (DKA) : BackgroundDocument9 pagesDiabetic Ketoacidosis (DKA) : Backgroundalyssa_flores_3No ratings yet
- Lecture On en and PNDocument92 pagesLecture On en and PNJerrold CruzNo ratings yet
- Dr. Drg. Nur Permatasari, MS. Dr. Dian Nugrahenny, M.BiomedDocument24 pagesDr. Drg. Nur Permatasari, MS. Dr. Dian Nugrahenny, M.BiomedTutde SedanaNo ratings yet
- Post-Surgical Nutritional Management in Dogs and CatsDocument34 pagesPost-Surgical Nutritional Management in Dogs and CatsSuraj_Subedi100% (4)
- Guidance For Intravenous Fluid and Electrolyte Prescription in AdultsDocument8 pagesGuidance For Intravenous Fluid and Electrolyte Prescription in AdultsfrakturhepatikaNo ratings yet
- Contact Details Name: Hospital Telephone:: Carnitine Transporter Deficiency (CTD) - Acute DecompensationDocument4 pagesContact Details Name: Hospital Telephone:: Carnitine Transporter Deficiency (CTD) - Acute DecompensationCaterina PrepelitaNo ratings yet
- Disseminated Intravascular CoagulationDocument37 pagesDisseminated Intravascular CoagulationhipoclaudioNo ratings yet
- 47 TPNDocument7 pages47 TPNKhor Chin PooNo ratings yet
- Biochemical and Biophysical Research CommunicationsDocument6 pagesBiochemical and Biophysical Research CommunicationsMegi LimbaNo ratings yet
- Total Parenteral NutritionDocument9 pagesTotal Parenteral NutritionsaravananNo ratings yet
- Proceedings of The 16th Italian Association of Equine Veterinarians CongressDocument4 pagesProceedings of The 16th Italian Association of Equine Veterinarians CongressCabinet VeterinarNo ratings yet
- High Intake of Saturated Fat, But Not Polyunsaturated Fat, Improves Survival in Heart Failure Despite Persistent Mitochondrial DefectsDocument9 pagesHigh Intake of Saturated Fat, But Not Polyunsaturated Fat, Improves Survival in Heart Failure Despite Persistent Mitochondrial DefectsRoger FaustinoNo ratings yet
- Perioperative Fluid Management in ChildrenDocument31 pagesPerioperative Fluid Management in ChildrenRashmi SahaNo ratings yet
- Disseminated Intravascular CoagulationDocument37 pagesDisseminated Intravascular CoagulationMuhammad Adeeb100% (1)
- Total Parenteral Nutrition-Induced Cholestasis, Prevention and ManagementDocument18 pagesTotal Parenteral Nutrition-Induced Cholestasis, Prevention and ManagementHandre PutraNo ratings yet
- Total Parenteral Nutrition (TPN) and Central Venous Pressure Line (CVP) - Mechinal VentilatorDocument23 pagesTotal Parenteral Nutrition (TPN) and Central Venous Pressure Line (CVP) - Mechinal VentilatorErika Danalle ArceoNo ratings yet
- Burn Patients Review of NutritionDocument3 pagesBurn Patients Review of NutritionStellaMarisAdindaNo ratings yet
- Office Lens 20150921-214721Document1 pageOffice Lens 20150921-214721kNo ratings yet
- Transdermal Drug Delivery SystemDocument99 pagesTransdermal Drug Delivery SystemIshtiaq AhmedNo ratings yet
- 10 2 Neonatal TransfusionDocument6 pages10 2 Neonatal TransfusionfatmaNo ratings yet
- BLOOD - FinalDocument8 pagesBLOOD - FinalanuNo ratings yet
- Modul Lipid 2014Document10 pagesModul Lipid 2014roropujiNo ratings yet
- Fast Facts: Long-Chain Fatty Acid Oxidation Disorders for PatientsFrom EverandFast Facts: Long-Chain Fatty Acid Oxidation Disorders for PatientsNo ratings yet
- Programa AnaliticaDocument51 pagesPrograma AnaliticaMaria CostandachiNo ratings yet
- Lingerie-Lookbook-Fall-High-Summer-2016-Victorias-Secret-Media-Kit (PDFDrive)Document87 pagesLingerie-Lookbook-Fall-High-Summer-2016-Victorias-Secret-Media-Kit (PDFDrive)Maria CostandachiNo ratings yet
- Tekhnologia Poshiva Nizhnego BelyaDocument199 pagesTekhnologia Poshiva Nizhnego BelyaMaria CostandachiNo ratings yet
- CE Mullins AtlasDocument11 pagesCE Mullins AtlasMaria CostandachiNo ratings yet
- Platye Rubashka S Kuliskoy - 161 165 - 48Document20 pagesPlatye Rubashka S Kuliskoy - 161 165 - 48Maria CostandachiNo ratings yet
- 10 1016@j CNC 2019 05 003Document14 pages10 1016@j CNC 2019 05 003Maria CostandachiNo ratings yet
- Ieee Eia Iec Iso 12207 2 (Z Lib - Org)Document110 pagesIeee Eia Iec Iso 12207 2 (Z Lib - Org)Maria CostandachiNo ratings yet
- 1 s2.0 S2590086221000021 MainDocument6 pages1 s2.0 S2590086221000021 MainLuis Ricardo Soto JiménezNo ratings yet
- National Diabetes Control ProgrammeDocument30 pagesNational Diabetes Control ProgrammePinki Barman100% (1)
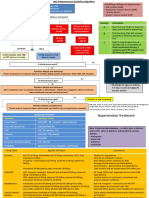
- Hypertension HSE Presentation HSE FormatsDocument18 pagesHypertension HSE Presentation HSE FormatsasepNo ratings yet
- BCH 201 ModuleDocument15 pagesBCH 201 ModuleJoyNo ratings yet
- Clinical Cases PDFDocument98 pagesClinical Cases PDFMuhammad Jawa'd AnwarNo ratings yet
- Scientific Evidence Underlying Contraindications TDocument11 pagesScientific Evidence Underlying Contraindications TChon ChiNo ratings yet
- Medical AbbreviationsDocument6 pagesMedical AbbreviationsEina CarmonaNo ratings yet
- Ketamine: Recent Evidence and Current Uses: DR Alistair Gales and DR Stuart MaxwellDocument6 pagesKetamine: Recent Evidence and Current Uses: DR Alistair Gales and DR Stuart MaxwellErick ToHuNo ratings yet
- Cardiovascular: The Least Likely To Cause Postural Hypotension?Document8 pagesCardiovascular: The Least Likely To Cause Postural Hypotension?Sandeep KannegantiNo ratings yet
- Acid RefluxDocument6 pagesAcid RefluxAnu RNo ratings yet
- CamaristaColeen Mae - PNEUMONIA (Case Study 1)Document31 pagesCamaristaColeen Mae - PNEUMONIA (Case Study 1)Coleen Mae CamaristaNo ratings yet
- Gender Differences in Coronary Heart Disease 06 February 2016Document16 pagesGender Differences in Coronary Heart Disease 06 February 2016Mohamad ZulmiNo ratings yet
- Anti-Glomerular Basement Membrane VasculitisDocument8 pagesAnti-Glomerular Basement Membrane VasculitisDra Daphne Rivero GallegosNo ratings yet
- Respiratory and Circulatory SystemDocument243 pagesRespiratory and Circulatory Systemfiroz77No ratings yet
- Lifepak 20e: Operating InstructionsDocument218 pagesLifepak 20e: Operating InstructionsJorge ArturoNo ratings yet
- From Rapalogs To Anti-Aging FormulaDocument16 pagesFrom Rapalogs To Anti-Aging FormulaCarlos RodriguezNo ratings yet
- Acute Rheumatic FeverDocument20 pagesAcute Rheumatic Feverfaizal samadNo ratings yet
- MEDICAL COMPLICATIONS OF PREGNANCY ModuleDocument12 pagesMEDICAL COMPLICATIONS OF PREGNANCY ModuleWynjoy NebresNo ratings yet
- Suprarenal GlandDocument13 pagesSuprarenal GlandAaa JjjjNo ratings yet
- 4 688957421938278535Document636 pages4 688957421938278535OsamaNo ratings yet
- Atelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Document10 pagesAtelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Gan BangNo ratings yet
- EdemaDocument24 pagesEdemaAnjela Fae Jintalan Amador100% (1)
- General Population (No Diabetes or CKD) Diabetes or CKD PresentDocument2 pagesGeneral Population (No Diabetes or CKD) Diabetes or CKD PresentLalu Ranova100% (1)
- All Clinical CasesDocument118 pagesAll Clinical CasesMichael AbioyeNo ratings yet
- USP of Revolution EVODocument2 pagesUSP of Revolution EVOStrategy AZ TeamNo ratings yet