Professional Documents
Culture Documents
Selective Mutism Clinic - Selective Mutism Treatment For Speech Pathologists-B959e626
Selective Mutism Clinic - Selective Mutism Treatment For Speech Pathologists-B959e626
Uploaded by
ortho KiD'SCopyright:
Available Formats
You might also like
- Perceived Strengths and Difficulties in Emotional Awareness andDocument13 pagesPerceived Strengths and Difficulties in Emotional Awareness andMargarida DiasNo ratings yet
- Late, Lost, and Unprepared: A Parents' Guide To Helping Children With Executive Functioning - Teen & Young AdultDocument5 pagesLate, Lost, and Unprepared: A Parents' Guide To Helping Children With Executive Functioning - Teen & Young Adultsiganemi0% (1)
- Selective Mutism Communication Anxiety Treatment ChildrenDocument19 pagesSelective Mutism Communication Anxiety Treatment ChildrenJelnathleeNo ratings yet
- Victims of CrimeDocument11 pagesVictims of Crimesuela35No ratings yet
- Hangxiety InfographicDocument1 pageHangxiety Infographicapi-548552942No ratings yet
- Making Eye Contact A Multidisciplinary Approach To The Management of AutismDocument1 pageMaking Eye Contact A Multidisciplinary Approach To The Management of AutismMohammad Abubakar SiddiqNo ratings yet
- Social-Emtional Skills To Adolescents With ASDDocument23 pagesSocial-Emtional Skills To Adolescents With ASDThảo NguyễnNo ratings yet
- Autism Spectrum Disorder ASDDocument10 pagesAutism Spectrum Disorder ASDM BORQUEZ QUINTASNo ratings yet
- Early Intervention For Children With Autism Spectrum DisordersDocument14 pagesEarly Intervention For Children With Autism Spectrum DisordersCarlos Charlotte SalvadorNo ratings yet
- Article InfoDocument10 pagesArticle InfoFélix IGNo ratings yet
- Psychosocial Interventions For Dementia: From Evidence To PracticeDocument11 pagesPsychosocial Interventions For Dementia: From Evidence To Practiceariadna17No ratings yet
- The Wall Sensory Integration AssessmentDocument21 pagesThe Wall Sensory Integration AssessmentSelinah Sslengs Seepe100% (1)
- Practical Guidelines For The Assessment and Treatment of Selective MutismDocument11 pagesPractical Guidelines For The Assessment and Treatment of Selective Mutismsylvia_plath27No ratings yet
- Sperger S Yndrome: ¿What Is It?Document2 pagesSperger S Yndrome: ¿What Is It?GINA NAYIBTH LEON VIDALNo ratings yet
- Autism Evaluation Online WorkshopDocument29 pagesAutism Evaluation Online WorkshopQurrat ulainNo ratings yet
- Whitbourne7e IM Ch11Document10 pagesWhitbourne7e IM Ch11Antônio Malvar Martins NetoNo ratings yet
- JPsychother Integ 2014 PerepletchikovaDocument16 pagesJPsychother Integ 2014 PerepletchikovaMaría Andrea Cárdenas PérezNo ratings yet
- Cognitive Clusters in SpecificDocument11 pagesCognitive Clusters in SpecificKarel GuevaraNo ratings yet
- Chicago DBTDocument87 pagesChicago DBTdhani meadowsNo ratings yet
- QR Management of Bipolar Disorder in AdultsDocument8 pagesQR Management of Bipolar Disorder in AdultsShre RanjithamNo ratings yet
- Actionresearch Oct28part2Document26 pagesActionresearch Oct28part2emaryltan0323No ratings yet
- An Update On Psychopharmacological TreatDocument15 pagesAn Update On Psychopharmacological Treatzakayahz3103No ratings yet
- 1 s2.0 S1878747923001654 MainDocument15 pages1 s2.0 S1878747923001654 MainJessie BrionesNo ratings yet
- Introduction To The Diagnostic Manual For Infancy and Early Childhood (DMIC)Document52 pagesIntroduction To The Diagnostic Manual For Infancy and Early Childhood (DMIC)circlestretchNo ratings yet
- Sauve et al. 2020Document14 pagesSauve et al. 2020Ayushi JainNo ratings yet
- Di Maio Week 5 Ebp EssayDocument9 pagesDi Maio Week 5 Ebp Essayapi-741546461No ratings yet
- Course Plan On Psychiatric NSGDocument10 pagesCourse Plan On Psychiatric NSGannu panchal100% (1)
- Psychopathologyslideshare 150721015626 Lva1 App6891Document62 pagesPsychopathologyslideshare 150721015626 Lva1 App6891Arun ChoudharyNo ratings yet
- Improving Overall Function Primary Component of Treatment Pecial Education Personnel or Trained TherapistsDocument4 pagesImproving Overall Function Primary Component of Treatment Pecial Education Personnel or Trained TherapistsSangitha ManiamNo ratings yet
- ADHDDocument21 pagesADHDsakthithirumaraiNo ratings yet
- Right Hemisphere DamageDocument80 pagesRight Hemisphere DamageSweekriti Narayanan100% (2)
- Mount, Marva - Management Ideas For Selective MutismDocument10 pagesMount, Marva - Management Ideas For Selective MutismMaja KobašNo ratings yet
- DSM 5 Neurodevelopmental NOTESDocument27 pagesDSM 5 Neurodevelopmental NOTESmicrobeateria100% (2)
- NDT 9 087Document6 pagesNDT 9 087Gita TikihaiNo ratings yet
- Datgn 20Document14 pagesDatgn 20Sâmara BeckerNo ratings yet
- AutismDocument21 pagesAutismcamelle sisonNo ratings yet
- Framework For ASD Therapy 24.03.18Document6 pagesFramework For ASD Therapy 24.03.18shivanjaniworkNo ratings yet
- Sensory Integration Therapies For Children With Developmental and Behavioral DisordersDocument6 pagesSensory Integration Therapies For Children With Developmental and Behavioral DisordersKevin RadittyaNo ratings yet
- Neurodevelopmental Disorders2023Document62 pagesNeurodevelopmental Disorders2023Chriziel SanchezNo ratings yet
- Weyant Makayla 2022 Autism PosterDocument1 pageWeyant Makayla 2022 Autism Posterapi-578364337No ratings yet
- Orofacial Myofunctional Therapy With Children Ages 0-4Document16 pagesOrofacial Myofunctional Therapy With Children Ages 0-4manu nopeNo ratings yet
- Questionario Sensorial AutismoDocument11 pagesQuestionario Sensorial AutismoLenice GóesNo ratings yet
- SENSORY INTEGRATION For ASDDocument35 pagesSENSORY INTEGRATION For ASDcitra city100% (1)
- Impact of Social Communication Interventions On Infants and Toddlers With or At-Risk For Autism: A Systematic ReviewDocument11 pagesImpact of Social Communication Interventions On Infants and Toddlers With or At-Risk For Autism: A Systematic ReviewpaulyfonoNo ratings yet
- Full Download Understanding Psychology 12th Edition Feldman Solutions ManualDocument35 pagesFull Download Understanding Psychology 12th Edition Feldman Solutions Manualowen7qjim100% (30)
- Alternativas Farmacologicas en AutismoDocument16 pagesAlternativas Farmacologicas en AutismoDerek TantaleánNo ratings yet
- Leiman-2 Dialogical Sequence Analysis in StudyingDocument27 pagesLeiman-2 Dialogical Sequence Analysis in StudyingPriscila OsórioNo ratings yet
- La Intervención en Los Trastornos Dislexicos - Entrenamiento FonológicoDocument7 pagesLa Intervención en Los Trastornos Dislexicos - Entrenamiento FonológicoLesly AgamaNo ratings yet
- Guide For Child Therapy: John McmohanDocument6 pagesGuide For Child Therapy: John McmohanJohn McmohanNo ratings yet
- NDT 331987 Language and Speech Characteristics in AutismDocument11 pagesNDT 331987 Language and Speech Characteristics in AutismAlejandro Cano VillagrasaNo ratings yet
- Actionresearch Oct28part2Document26 pagesActionresearch Oct28part2xray12345No ratings yet
- 2017 Metacognitive StrategiesDocument15 pages2017 Metacognitive StrategiesXimena LainfiestaNo ratings yet
- PsychotherapyDocument23 pagesPsychotherapymariaNo ratings yet
- Actionresearch Oct28part2Document26 pagesActionresearch Oct28part2Dilinesaw BogaleNo ratings yet
- Principles of Clinical Practice For Assessment and InterventionDocument28 pagesPrinciples of Clinical Practice For Assessment and InterventionFam TuongNo ratings yet
- Nrneurol 2015 229Document12 pagesNrneurol 2015 229Renan RRSNo ratings yet
- Clinical Assessment of Social CognitiveDocument12 pagesClinical Assessment of Social CognitivePaulina Negrón DíazNo ratings yet
- (Mora & McAndrew, 2003) - Common-Sense Model of Self-Regulation.Document8 pages(Mora & McAndrew, 2003) - Common-Sense Model of Self-Regulation.CMSNo ratings yet
- Copiii Si Adolescenti + Adulti Cu TSA: Characteristics of DisorderDocument2 pagesCopiii Si Adolescenti + Adulti Cu TSA: Characteristics of DisorderCristian MeleiNo ratings yet
- Div Class Title Auditory Hallucinations in Schizophrenia Helping Patients To Develop Effective Coping Strategies DivDocument6 pagesDiv Class Title Auditory Hallucinations in Schizophrenia Helping Patients To Develop Effective Coping Strategies DivHilda Nurul FatimahNo ratings yet
- Articulo 5 EVALUACIÓN PSICOPATOLÓGICA DEL LENGUAJE EN LA ESQUIZOFRENIA-1Document1 pageArticulo 5 EVALUACIÓN PSICOPATOLÓGICA DEL LENGUAJE EN LA ESQUIZOFRENIA-1Teddy JuniorNo ratings yet
- PROMPT An Overview MSHA Presentation 2018Document85 pagesPROMPT An Overview MSHA Presentation 2018Lays Mandy100% (1)
- Therapeutic Education Direction & Intervention (TEDI): Volume 2: Activity Kits for Special Needs Children: Communication and Gross MotorFrom EverandTherapeutic Education Direction & Intervention (TEDI): Volume 2: Activity Kits for Special Needs Children: Communication and Gross MotorNo ratings yet
- NCP AnxietyDocument3 pagesNCP AnxietyLord James De GuzmanNo ratings yet
- Project On GothicDocument14 pagesProject On GothicMazana ÁngelNo ratings yet
- TEXTO ORIGINAL - What Is ADHD - 4 PagesDocument4 pagesTEXTO ORIGINAL - What Is ADHD - 4 PagesGrace ValenciaNo ratings yet
- 1 Page DSM - Psychotic PDFDocument1 page1 Page DSM - Psychotic PDFRobert FordNo ratings yet
- Apa Research Paper On Eating DisordersDocument7 pagesApa Research Paper On Eating Disordersuifjzvrif100% (1)
- School Refusal Assessment ScaleDocument6 pagesSchool Refusal Assessment Scaleamrut muzumdarNo ratings yet
- Cannabis Dependence RehmDocument18 pagesCannabis Dependence RehmAntonio Tejero PocielloNo ratings yet
- Mse 2Document3 pagesMse 2Charisma PastorNo ratings yet
- 6001.alcohol Induced DementiaDocument4 pages6001.alcohol Induced Dementiajuan_bacha_1No ratings yet
- AdhdDocument2 pagesAdhdAlexander SaladinNo ratings yet
- Pych Preboards QuestionsDocument18 pagesPych Preboards QuestionsPaul Lexus Gomez LorenzoNo ratings yet
- LatahDocument2 pagesLatahKhoirunnisa RahmawatiNo ratings yet
- Psychology PaperDocument5 pagesPsychology PaperBwallace12No ratings yet
- PsyHx and MSEDocument25 pagesPsyHx and MSERazel AnneNo ratings yet
- (Psychiatry) Mental Health Proj Proposal LEC 12 PDFDocument7 pages(Psychiatry) Mental Health Proj Proposal LEC 12 PDFXianne GonzalesNo ratings yet
- IMPULSE-CONTROL DISORDERS-Dr. Mabunga 2Document25 pagesIMPULSE-CONTROL DISORDERS-Dr. Mabunga 2Vasu PatelNo ratings yet
- APPENDIXDocument3 pagesAPPENDIXRon AracoNo ratings yet
- (Download PDF) Antidepressants From Biogenic Amines To New Mechanisms of Action Matthew Macaluso Online Ebook All Chapter PDFDocument42 pages(Download PDF) Antidepressants From Biogenic Amines To New Mechanisms of Action Matthew Macaluso Online Ebook All Chapter PDFsandra.estrada213100% (9)
- Paranoid SchizophreniaDocument12 pagesParanoid Schizophreniakiran mahalNo ratings yet
- The Facts On Tweens and Teens and Dating ViolenceDocument2 pagesThe Facts On Tweens and Teens and Dating ViolenceFilipaTorresCostaNo ratings yet
- Student Example Borderline Personality DisorderDocument12 pagesStudent Example Borderline Personality Disorderapi-284737097No ratings yet
- Female Orgasmic DisorderDocument5 pagesFemale Orgasmic DisorderYamini JohriNo ratings yet
- Maine Northeast Conference On Fetal Alcohol Spectrum DisordersDocument1 pageMaine Northeast Conference On Fetal Alcohol Spectrum DisordersfasdunitedNo ratings yet
- What To Expect From Your ADHD AssessmentDocument1 pageWhat To Expect From Your ADHD AssessmentsamNo ratings yet
- SCHIZOPHRENIA CaseDocument8 pagesSCHIZOPHRENIA Casekrishna BabuNo ratings yet
- Complex Post-Traumatic Stress Disorder. Implications For Individuals With ASDDocument13 pagesComplex Post-Traumatic Stress Disorder. Implications For Individuals With ASDpaul.cotarelo2012No ratings yet
- Jaime Castillo What Happened To Make You Anxious How To Uncover The Little T Traumas That DriveDocument162 pagesJaime Castillo What Happened To Make You Anxious How To Uncover The Little T Traumas That DrivePablo Bando100% (1)
Selective Mutism Clinic - Selective Mutism Treatment For Speech Pathologists-B959e626
Selective Mutism Clinic - Selective Mutism Treatment For Speech Pathologists-B959e626
Uploaded by
ortho KiD'SOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Selective Mutism Clinic - Selective Mutism Treatment For Speech Pathologists-B959e626
Selective Mutism Clinic - Selective Mutism Treatment For Speech Pathologists-B959e626
Uploaded by
ortho KiD'SCopyright:
Available Formats
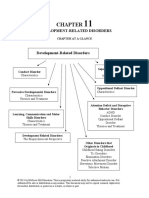
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Selective Mutism Overview
Treatment For What is Selective Mutism? Assessment
Speech Epidemiology and aetiology
Diagnosis
When to assess/treat Speech/language issues
When to refer to a Psychologist
Pathologists Role of Speech Pathologists in
diagnosis/treatment
6-Step Pathway to build talking
◦ Including ‘Sliding In’ and ‘Fast generalisation’
D R ELI ZABE TH WO OD C OC K of speech
D IRE CTO R / Understanding SM as an anxiety disorder
CL INIC AL P S YCHOLO G IS T Key treatment strategies
Treating anxiety through stepladders
S E LEC TIV E M U TIS M CLIN IC, Clinic treatment program
S YD NE Y 5-stage Model of Communication in SM
School treatment program
Variables that affect communication –
“Communication Changers” Transitioning to a new teacher
www.selectivemutism.com.au
admin@selectivemutism.com.au
02 9438 2511
Click
What is Selective Mutism? What SM looks like (5yo)
An Anxiety Disorder
Mute in situations where talking is expected
Communication is variable
◦ Typically – 1-2 peers and not teacher Click
◦ Less common
◦ Talks freely in school but not elsewhere
◦ Mute with immediate family
◦ Whispering to everyone
Visible signs of anxiety – highly variable
Role of SPs in diagnosis/treatment
Diagnosis - DSM-V criteria
DSM-V (within anxiety disorders) SPs cannot formally diagnose SM
Consistent failure to speak in social situations (in which there is However, diagnosis rarely needed
an expectation for speaking, e.g., at school) despite speaking in
other situations Fine to still refer to it as Selective Mutism
Interferes with educational/occupational achievement or social ◦ “Symptoms consistent with a diagnosis of SM”
communication
Speechies have great skills to treat SM
Duration > 1 month (not limited to first school month)
◦ Can be useful to learn additional anxiety-management skills
Not lack of knowledge/comfort with the language
Not better accounted for by a Communication disorder and not
exclusively during course of PDD/ psychotic disorder
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 1
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Differential diagnoses Differential diagnoses
SM alone Speech/language disorder
◦ Usually very easy to diagnose ◦ High comorbidity
◦ Anxiety (in SM) will change communication in different social settings ◦ But if speech disorder alone, would not see such disparity in communication across social settings
Social Anxiety Disorder (SAD) Depression
◦ Usually never completely mute ◦ Extremely severe Depression (usually adolescent) can lead to
shutting down/mutism
◦ May avoid speeches and lack initiation of speech
◦ Usually also accompanied by ASD and poor parent/child relationship
◦ SM may look like SAD in later treatment stages
To aid diagnosis
Just shy? ◦ Flexible assessment needed - Rely on reports from others
◦ Would see limited speech as in Social Anxiety but not mutism ◦ Compare home speech vs anxious situations
◦ Check history of mutism
Stubbornness/Behavioural
◦ Rare for SM not to present in preschool
◦ Would never cause mutism by itself ◦ If looks like social anxiety (e.g., limited talking but no mutism) and has history of mutism/SM, then would diagnose SM
Differential diagnoses - Autism Epidemiology etc.
High comorbidity of SM/ASD
Incidence: 0.7-1.9% children in kindy → 2nd grade (1/140)
But….SM sometimes misdiagnosed as ASD due to social/emotional deficits – and how the child
presents! Lower incidence as age increases (e.g., 1/555 7-15 yr olds)
Important to assess communication/social/emotional symptoms across settings More common in girls than boys
◦ Our clinic stats incl. enquiries: Girl: boy ratio is 1.8 : 1 (1433 cases)
Difficult to diagnose comorbid ASD in early stages of SM
◦ Stay open to possibility of comorbid ASD throughout treatment Typically presents ~ 3 years
◦ Assessment would need to rely on parent/teacher reports and nonverbal play
◦ Better to delay until SM has almost resolved and child can be assessed verbally Treatment typically sought ~ 14m after onset
◦ Could give screening questionnaires early (e.g., CAST; SRS-2) ◦ One study mean diagnosis at 6.5 yrs
Complexities of ASD/SM diagnosis
◦ SM itself causes long-term impairments in social skills
◦ Reduced communication in teenagers with adults is common
Common to have other disorders
(from Kristensen, 2000; no. in sample =54) 55% had 3-7
Common to have other disorders
diagnoses! Disorder Prevalence
Communication disorders 50%
Disorder Prevalence
• Mixed receptive-expressive language disorder 17%
Any developmental disorder / delay 69% • Expressive language disorder 11.5%
Mild mental retardation 8% 63% of SM outpatients • Phonological disorder 43%
in a hospital clinic had
Asperger’s (now ASD) 7% ASD Any other anxiety disorder 74%
(Steffenburg et al., 2018) Another study showed
Developmental coordination disorder 17% • Social phobia 67%
90%
35% of recent clients
Elimination disorders (wetting/soiling) 32% under 12 to our clinic
• Separation anxiety 32%
were above cut-off on • Specific phobia 13%
ASD screening • Generalised anxiety disorder (GAD) 13%
measure (CAST)
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 2
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
It’s not just about the mutism Prognosis
Eating anxiety Social skills deficits ◦ Academic impairments WITH TREATMENT
Toileting anxiety Assertiveness ◦ Social skills deficits ◦ Generally 1-2 years until fully resolved
◦ Poorer self-confidence, ◦ If ASD, much longer
Behavioural issues Teasing / exclusion independence, achievement, social
communication ◦ Longer/harder to treat with increasing
Sleeping issues Depression age
◦ Higher rate of unemployment
Performance anxiety School refusal
◦ 88% of adults with childhood SM
Self-esteem Emotion regulation reported “intense suffering”
Understanding SM as an anxiety disorder
What is anxiety?
Trigger – real or …which triggers the fright/flight
Imagine your biggest fear perceived threat response in your body that gets
you ready to….
run for your life… …or stay and fight
Fight-or-flight response SM child’s worst fears
Hot/ Mind focused on
red face danger/trigger
Faster
breathing Dry mouth
Sweating Racing heart
Tense muscles/ Butterflies/
Tight chest nausea
Need to go to Shaking/
the toilet Trembling
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 3
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
What causes SM? What causes SM?
Not due to trauma • Strong family history of Limited social exp’s Others’ positive/
anxiety Changes in environment negative reactions
It is an anxiety disorder
• Anxious / Parental modelling / Speech/language
shy temperament overprotection deficits (33-50%)
Marital problems (47%) Bilingualism (28%)
Poor parenting style
(84%)
Factors that
increase self-
Genetics Environment
consciousness
about talking
Negative
What keeps the mutism going? reinforcement Child prompted
Ineffective strategies (increase anxiety about communication) to talk
Pressure Negative
Comments/criticism about talking
Unrealistic talking goals reinforcement
Expressing frustration cycle in SM Child/adult’s
Child gets overly
Offering large rewards for ‘talking’ anxiety are
anxious
lowered
Avoidance
Child avoids talking/situations
Others - Talk for them / say “they don’t talk”
Absence of treatment - ‘Wait and see’
Others fear making the SM worse or distressing child Adult Child
Habit
rescues avoids
Model by Steven Kurtz
Thousands of questions without answering leads to….. HABIT!
Positive Child
reinforcement for prompted to
Treatment aims for a brave talking talk
positive Treating fear by facing fear
reinforcement cycle
Brain needs to learn the thing they fear (communication) isn’t life-
threatening
Child answers question
Child gets Only way to learn face the fear
and is rewarded with
overly anxious
labelled praise
Anxiety then reduces with repeated exposure
But….we can’t make children talk!
Therefore, stepladders are needed
Adult gives child
opportunity to Child tries
respond & shapes to avoid
Model by Steven Kurtz verbal behaviour
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 4
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Selective Mutism Clinic - 5-stage Model of Communication
What this stage looks like
STAGE 1: Pre-communication ACHIEVED
NOT ACHIEVED
Stage 2: Stage 4:
Stage 1: Pre- Stage 3:
Communication Indirect
communication Nonverbal Stage 5: Direct
with ‘talking communication
Joining in activities communication communication
buddy’ Communicating
in a relaxed way, Communicating Speaking directly
doing what is Talking with with others via a
with others using ‘talking buddy’ (whisper or voice)
required (e.g., someone the child to person or group
usually talks freely body language, (e.g., parent/
doing work, going writing, typing,
into school, joining with (e.g., parent), friend conveys the
in the anxious texting, etc. message), or
in dance/sport)
situation (e.g., recording device
classroom, shops)
© Not to be used or reproduced without permission of Elizabeth Woodcock, Selective Mutism Clinic, www.selectivemutism.com.au
What this stage looks like What this stage looks like
STAGE 2: Communication with ‘talking buddy’ in anxious situation STAGE 3: Nonverbal Communication
The message is
intended for the
‘talking buddy’ Keychain of pictures
The message is intended for
Stage 4 – Indirect Communication
What this stage looks like the other person, but comes
via the ‘talking buddy’
Talking Tom app
STAGE 4: Indirect Communication
Click
TouchChat
Voice-recording
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 5
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Stage 4 – Indirect Communication Stage 4 – Indirect Communication
‘Voice changing’ apps – masks sound of voice Voice Memos Apps
iPhone – “Voice changing plus” Android – “Voice changer for kids” (E.G., ANDROID - ‘VOICE MEMOS’ OR ‘EASY VOICE RECORDER’) (IPHONE – ‘QUICK VOICE’)
Click
Click
Search
“Voice changer”
Reads text
Stage 4 – Indirect Communication as you type
“Text to speech” apps Stage 5 – Direct communication
Android – “Type and Speak” iPhone – “Text to speech – voice synthesizer” It’s not over until the ‘selective mute’ sings…
Click
What this stage looks like ‘Communication changers’
STAGE 5: Direct Communication
Many factors increase anxiety & mutism
Understanding these will help you to set
goals for the child
If less talking, assume less comfortable, more
anxious
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 6
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
‘Communication changers’ © Selective Mutism Clinic
Communication changers
“Why did they speak in front of the class yesterday but not today?”
Level of Visibility by Audibility by Amount of Task Open to Child's level
Comfort Motivation
structure others others output familiarity being judged of control
Yesterday – playing Bingo (motivation!), Today – personal,
predictable and short (‘Bingo’) open-ended What did you Masked voice Prior role-
do on the Prompting: Tell
what to say vs
sentence
Eye contact play Humour Facts vs
opinions
Rate
difficulty of
goal on a 1-
Game
weekend?
Whispering vs
starter vs voice 10 scale
nonverbal
prompt Distance Familiar
Rehearsal
from listener situation
Voice volume Assertive- Topic of
Sounds ness interest
Reading vs
Child
Audio vs Distance from single Known chooses
listener Rapport
video words answer
questions
Questions: vs
Academic Rewards and
Closed vs Hiding mouth sentences content praise
forced-choice Familiar
Degree of Authority of
vs open-ended activity /
movement listener
topic
Body position Work up
Personal hierarchy of Encourage-
Initiating vs Break in Talking buddy
information peers ment
Body position Number of present
responding
listeners
contact
‘Communication changers’ –
Factors that affect communication
Which
‘communication 1 hr video
Parent(s) Child with
Questionnaires consult with
changers’ could Click without child parents
teacher
be responsible
for the mutism?
Assessment
Assessment - Questionnaires Assessment with parent(s)
alone
Frankfurt Scale of Selective Mutism (FSSM; 3-18yrs) (Gensthaler et al., 2020)
Full clinical developmental interview, PLUS..
Selective Mutism Questionnaire (SMQ) (Bergman, 2012) Child’s Communication and ‘Stage of Communication’
in every situation
School Speech Questionnaire (SSQ) (Bergman, 2012) ◦ Who, Where, How
Factors increased self-consciousness about
Spence Children’s Anxiety Scale (school (child/parent) & preschool (child)) (Spence, 1994) communication
Attitude/management of previous teachers
Revised Manifest Children’s Anxiety Disorder Scale (RCADS) (Child/parent) (Chorpita, 2000)
Previous strategies tried / ‘mistakes’ made
Childhood Autism Screening Test (CAST) Maintaining factors – e.g., pressure to talk
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 7
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
What stage of communication?
Assessment with parent(s) cont.
Changes (school, house)
Speech disorders – cursory assessment Grandparents/
Bilingualism, parent’s accent relatives
Can child talk about the problem?
Park with friends
Child’s attitude towards school / teacher Home with friends
Parents’ / teacher’s skills
Teacher/school’s willingness to help Shop counters
Emotion regulation
Behaviour problems Extracurricular activities Café/restaurants
End of assessment / Prep for meeting child There is no 1 on 1 assessment with child
◦ All assessment information is gathered via
Ask how the child is likely to communicate with you
Assessment parent and school
Teach PRIDE strategies
with child Direct assessment of child occurs through
Discuss ‘Sliding In’ procedure observation during first treatment session
Discuss reward system for session; choose appropriate reward See details later
A second assessment with parent(s) alone is sometimes useful to
cover everything
Assessment
Feedback at end of assessment with school /
Usually video
Invite all relevant school personnel
Families keen for feedback classroom ◦ Must include classroom teacher
Give diagnosis teacher
Discuss your role
Give opinion of severity of SM, problem
formulation Discuss overall program / intensity
Give overview of treatment plan Check knowledge about SM
Discuss length of treatment and factors
that affect this (set up expectations of
commitment)
Prepare them for intense school program
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 8
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Assess child’s communication at school
Assessment with
At desk
classroom teacher
Playground Check eating, toileting, performance anxiety
Peer relationships
News/whole class
Assess teacher’s
◦ Perception of the problem
Teacher 1 on 1 ◦ Willingness
◦ Availability
Small groups ◦ Enthusiasm
◦ Psychological mindedness
Pairs Provide education (see later)
Assessment with When to test/assess speech/language
classroom teacher/team What if there are comorbid speech/language issues?
SM will affect all verbal and even nonverbal tests
Emphasise SM is
◦ Complex and serious Recommend – Treat SM first
◦ Treatable Reconsider the purpose – is it absolutely necessary?
◦ Weigh up pros (e.g., funding) vs cons (e.g., inaccurate
Describe commitment required results)
◦ Requires intensive school program Flexible ways of testing could be considered
◦ Requires main classroom teacher ◦ Nonverbal only
◦ Rely on parent input (e.g., parent observes testing and
provides input re accuracy, or train parent to
implement)
◦ May need to do “Sliding In” with assessor
When to refer to a Psychologist Selective Mutism Clinic
- general rule – when there are significant comorbidities 3-pronged treatment approach
that are treatment-interfering Treatment takes 6m – 2 years School
program
Minor issues can wait Separation Anxiety that causes distress but doesn’t stop child
until later or refer to
external/online Eating/toileting anxiety
programs A note about ASD:
Very important and
Moderate (refer to Minor behavioural issues significant, but due to
online/external difficulties diagnosing,
courses or psych) best to watch and wait Clinic sessions
Anxiety – significant general worry, OCD Community/
(1/week to 4 home goals
weeks)
Severe and significant Depression
- Immediate referral
School refusal
Separation anxiety – if stopping child from getting to school
Significant behavioural/emotional issues (may or may not be in context of ASD)
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 9
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Program structure Occur in parallel
Clinic sessions with
child/parent ‘Sliding In’ Procedure
2a. Clinic assessment with
child/parent ‘Sliding In’
Community goals 4. Person sliding-in
1. moves closer, watches,
Assessment Communication sessions /
then joins the game.
3. After gradually
with ‘Sliding In’ at school removing head- Next: ‘Talking Buddy’
parent(s) (parent/teacher/child)
2. Person sliding-in
phones, person slides away in about 4
steps.
sliding-in sits on
enters and sits at
2b. School assessment with Teacher classroom floor and moves
1. Person sliding-in furthest point away,
teacher closer.
strategies is outside the listening to music
room, door closed. with headphones.
Monthly video If child stops using their voice, or whispers at any point, person sliding-in goes back a
consultations with teacher step. Low voice is ok.
First session
What does the first session with Talk openly about SM and how you’ll be helping
the child look like? Kids usually can’t
I know of lots of explain why they can’t
Be prepared for highly anxious child! other kids who use their voice and
Talk to child very briefly about your role, no questions find it hard to they feel stuck with
Introduce reward chart use their voice getting started
I know it’s hard
Quick chat (things to say slides) I have ideas of
for you to use
Remind parent about PRIDE strategies your voice how we can get
Commence ‘Sliding In’ (30-40 mins) sometimes unstuck. Things
won’t always
Observe parental behaviours
be this way
Discuss overall program with parent while child plays
First session
Talk openly about SM and how you’ll be helping
If you can play the game We’ll just take
with mum when I’m out of small steps doing
the room and use your brave things and
brave voice, you’ll earn one day talking will
stickers on your chart and be much easier Questions
you can earn a cool reward
at the end
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 10
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
A. Prioritise Stage 1 – Pre-communication
Pathway to B. ‘Stage 2 communication’ – talking with
build talking
parent alone in clinic/classroom (if needed)
C. Use ‘Sliding In’ to help child talk to
CLINIC
Same process is
repeated with
Speechie for first time
STEP A
D. Build talking with Speechie 1 on 1
classroom teacher PRIORITISE PRE-
and first peer E. Fast generalisation of speech to other COMMUNICATION
adults/peers 1 on 1
F. Expand talking: More environments,
voice volume, assertive communication
Prioritise Stage 1
Pre-communication
Child is too anxious to do what is expected in the situation
Can look like: freezing, not joining in play, standing, clinging
CLINIC
Ask no questions (as that would expect Stage 3 comm.)
STEP B
Ask no questions Show understanding
ENSURE CHILD
Address any known triggers Label emotions CAN TALK TO
Provide reassurance Remove any expectations
PARENT ALONE IN
Give control by describing the
procedure and expectations
Use distraction/chatting
ROOM (STAGE 2
Help child relax
Give lots of time
COMMUNICATION)
Don’t physically move
When child can’t talk to parent in room alone…
Less than 10% of kids with SM
In clinic, child/parent play structured talking game alone
CLINIC
Use reward system – points for using voice only STEP C
Not practical to spend a lot of time on this, therefore work on mainly at USE ‘SLIDING IN’
school/community TO GENERALISE
TALKING FROM
PARENT TO SPEECH
PATHOLOGIST
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 11
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Sliding In – allows direct transition from Stage 2 to Stage 5 Speechie
Parent
‘Sliding In’ Procedure
A ‘stimulus fading’ technique
Enclosed, undisturbed room, door closed
Sit on floor
Stage 2: Stage 4:
Stage 1: Pre- Stage 3:
Communication Indirect Frequently reward talking
communication Nonverbal Stage 5: Direct
with ‘talking communication
Joining in activities communication communication Keep gently pushing
buddy’ Communicating
in a relaxed way, Communicating Speaking directly ◦ ‘Slide’ forward if child talking for about 1 min
doing what is Talking with with others via a
with others using ‘talking buddy’ (whisper or voice) ◦ Don’t ask permission, just do it
required (e.g., someone the child to person or group
usually talks freely body language, (e.g., parent/
doing work, going writing, typing, Duration to speak to therapist – variable (1 session to months; norm - weeks)
into school, joining with (e.g., parent), friend conveys the
in the anxious texting, etc. message), or
in dance/sport) Subsequent sessions – start at same place you ended last time
situation (e.g., recording device
classroom, shops)
© Not to be used or reproduced without permission of Elizabeth Woodcock, Selective Mutism Clinic, www.selectivemutism.com.au
Sliding In
PRIDE skills to use during ‘Sliding In’ (Steven Kurtz) Role Play Video
Avoid
raise
Questions outside the game
Speechie
Criticism/sarcasm
eflect (EVERY time)
Commands Click
Parent
mitate Negative talk about their not talking
escribe everything Person sliding in – from the time they take off
the first headphone and start to hear the child:
Make comments about the game
nthusiasm Reflect/praise child’s speech
Games for ‘Sliding In’ Sliding In
Any fun game that encourages structured talking
Effective ‘Sliding Ins’
Easy / non-academic Not necessary to change the game often
◦ If you do change games, ‘slide’ back one step
Use games with sentences ◦ Don’t change games at big transition point – e.g., when
Speechie comes into room or start of new session
Only slide closer if there’s a voice, not a whisper (low
voice ok)
Take tinier steps at difficult points for the child
Be prepared to use flexible strategies
◦ e.g., slide close with headphones still on
Avoid eye contact with child, face away whilst ‘Sliding In’
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 12
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Building direct talking
with Speechie
CLINIC Can be with or without parent (mix is best)
STEP D Play variety of structured games
Introduce binary-choice questions
BUILD CHILD’S ◦ Initially about the game
TALKING WITH ◦ Later about other topics
SPEECH ◦ Add a generic option
PATHOLOGIST ◦ “Did you play soccer, basketball, or something else on the
weekend?”
1 ON 1
Go Fish Fairies
Building direct talking Building direct talking
Activities to build communication Build spontaneous talking with ‘Sentence games’
Work up stepladder of difficulty
◦ e.g., personal info / opinions / talking about emotions will be harder
Take turns:
◦ Always keep “Communication changers” in mind Rory’s Story Cubes
1. Read a sentence
‘Silly yes/no questions’ (“Do carrots run?”)
2. Other person:
Practice “I don’t knows” (“How many countries in the world?”)
Easy ‘information’ questions (“How many people live in your house?”) nswers
‘Favourites’ questions (“What’s your favourite clothing?”)
dds extra comment
‘Would you rather’ questions (“Would you rather be incredibly funny or incredibly smart?”)
◦ (See conversationstartersworld.com/would-you-rather-questions-for-kids/)
sks a question back “Do you have any pets?”
Chat open/ended topics (“What are some of your jobs at home?”)
“What did you have for breakfast?”
Video –
Building spontaneous talking using ‘sentence games’
CLINIC
Click
STEP E
FAST
GENERALISATION
OF SPEECH TO
OTHER ADULTS
1 ON 1
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 13
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Fast Generalising
Generalising talking Interview strategy
Fast generalising - considerations
Use structured task/game to quickly generalise to Child writes 5 questions they would like to be asked by others (also
many people write their answers)
◦ Speechie, receptionist, other clinicians
Child writes 5 questions they would like to ask others
Don’t use rating scale at this stage
Rehearse with Speechie then do with any other adults available,
Don’t ask them if they want to (they will say ‘no’!)
supported by Speechie
Tell them what they’re going to do with a warm, firm,
confidence
‘Lend the child your confidence’
Role play and then in vivo
Interview strategy
Please ask Isabella these questions: Interview strategy for non-readers
1. Do you have any pets? [Yes a lizard]
2. What type of lizard is it? [A pygmy bearded dragon]
3. What does your lizard eat? [It eats crickets]
4. How old is your lizard? [3 months old]
5. Does your lizard have toys? [Yes a laser light and ball]
Isabella will ask you these questions:
1. What is your favourite colour?
2. Do you have any pets?
3. How long have you been a teacher for?
4. Where have you been to overseas?
5. Do you prefer winter or summer?
Fast Generalising
Scavenger Hunt Generalising talking – using ‘Scavenger hunt’
Child’s individualised Click
scavenger hunt sheet
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 14
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
CLINIC Expanding speech
STEP F 1. More environments USING KEY STRATEGIES
2. Content 1. Stepladders
EXPAND TALKING:
◦ Assertive 2. Rating scales
STEPLADDERS,
◦ Personal
MORE ◦ Emotional
3. Praise/rewards
ENVIRONMENTS, ◦ Voice volume 4. Role plays
VOICE VOLUME, ◦ Initiating speech 5. Levels of prompting
ASSERTIVE 6. Labelling nonverbals
COMMUNICATION 7. Goals in the moment, and having a plan B
8. Trust and Transparency
Progressing to advanced Stage 5 communication Levels of prompting
Early stage 5 – provide specific prompting
Progressing to advanced Stage 5 – reduce level of prompting
Advanced Stage 5
• Reduce prompting
Sentence
• Reduce structure Nonverbal
starter Vague
Facilitate Stage 5 • Increase academic content Specific prompt
prompt Vaguer
• More spontaneous answers prompt “Jessie
• High structure prompt (Raise
• Harder question types would “Tell the
• e.g., binary-choices “Say one eyebrows
• Assertive like an lady what “Say your
• Increase child’s motivation banana and nod
• Larger audience ice-cream ice-cream order to
• Lower academic content ice-cream head to
• Greetings / manners with the you the lady”
• Rehearsed, easy answers please” gesture to
• 1 on 1 flavour want” order)
____”
Community communication goals
– practicing single words using binary-choice questions Community communication goals
Working on community goals
Pass sheet to waiter: Please ask the following questions Shops
to my daughter who is practising brave talking: ◦ Post office - “Can I have one $1 stamp please?”
◦ Supermarket – “Where are the tissues please?”
1. Do you want a babycino or water?
◦ Chemist – “Excuse me, where are the Band-Aids?”
2. Do you want froth or milk? ◦ Sushi shop – “Can I have a baby avocado please?”
3. Do you want a marshmallow or no marshmallow?
Extra-curricular activities
4. Do you want a pink or white marshmallow? ◦ Soccer
5. Do you want to takeaway or have here? ◦ Music, art, swimming, tennis lessons
6. Do you want to pay by card or cash? Relatives
7. Great, that will be $X please ◦ May need Sliding In or fast generalisation (interview/game)
8. Thanks, here’s your change
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 15
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Graded exposure Graded exposure
Stage 5 - Increase voice volume Goal - “Say that
again using a
number 3 voice”
Stage 5 - Building voice volume – apps
Very low voice iPhone/iPad - DecibelMeter Android – Sound Meter
Loud whisper
3 Medium voice
2 (bit lower than normal voice)
4
Soft whisper
Normal talking voice
Search:
1 5
“Sound level
meter”
Trust & Step-
What happens as SM is resolving? Transparen-
cy
ladders &
ratings
Resembles social anxiety disorder or ‘shyness’ Key treatment
Usually gradual improvements in speech /people spoken to strategies
May mask voice (baby/alien) The balance
Role plays
Responding generally much easier than initiating of tone
Oppositional behaviours may emerge
Motivation of parents/schools usually decreases
Organise social skills training Praise/ Labelling
◦ Social effectiveness therapy (SET-C; 8-16 yrs; Beidel et al. 2014) or PEERS rewards nonverbals
You’re
Key strategies nodding
“Labelling nonverbals” – breaking the habit your head
Key treatment
Once child is saying single words You’re
strategies ◦ Don’t allow nonverbal responses shrugging
your
You’re shoulders
‘Label’ any nonverbals pointing to
the book
Might need extra prompt initially You’re
Labelling
nonverbals
shaking your
head…
Say ‘no’
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 16
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Key strategies Step-
Video – “labelling nonverbals” ladders &
Key treatment ratings
strategies
Click
Step Goal Stage
Key strategies 1 Stand with mum at checkout, carry bags 1
When to use Stepladders Cafe stepladder 2 Hand over money, take change/receipt 3
3 Whisper order to parent, parent tells waiter – 1 word 4
4 As above, but using a few words 4
Use when Stage 5 talking is currently too difficult Say 1 word to mum with binary-choice (“My daughter
5 4
◦ Getting needs met in class (e.g., asking for help) would like an ice-cream, do you want vanilla or choc?”)
Say 1 word to mum with open-ended question (“Which
◦ Communicating with teacher in classroom 6
flavour would you like?”), mum tells waiter
4
◦ Class speeches / news 7
Say 1 word with binary choice but parent prompts child
5
to tell waiter directly
◦ Ordering from canteen Say order direct using sentence with specific prompt
8 5
◦ During whole class activities including roll call (“Say one chocolate ice-cream please”)
◦ Ordering at café 9
Say order with vague prompt (“tell the waiter what you
want”)
5
Use rating scale with child to help work out starting point 10 Child goes up to counter by self to order using sentence 5
11 Say something in conversation to waiter before ordering 5
◦ Listener walks away to provide time for child to Key strategies
tell ‘talking buddy’, can cup hand around mouth
Key strategies ◦ Listener walks small distance away Teach the child to rate goals
Stage 4 – Using a ◦ Listener turns around
’talking buddy’ – ◦ Listener just looks away
stepladder ◦ Listener watches child, child still cups hand
◦ Child puts hand in lap (no cupping)
◦ Child moves hand distance away from buddy’s ear
◦ …half an arm length
◦ …arm length Younger children
can use a
◦ Child looks at floor when answering ’whisper buddy’
◦ Child looks at other person’s feet
◦ …chest…chin
NB. At point where listener hears child,
stop ‘buddy’ from repeating
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 17
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Key strategies
Rating scale for preschoolers
Key treatment
#1 bear #2 bear strategies
Praise/
#3 bear #4 bear rewards
Key strategies Trust &
Using praise / rewards Transpar-
ency
Immediate, frequent praise/points Key treatment
Extra points for behaviours you are shaping strategies
Praise with low emotion, not in front of others
‘Labelled praise’
◦ “Great using a louder volume when you said ‘help please’
Points/stamps add up to larger rewards
Embarrassment is common – push through
Teacher’s enthusiasm/discussion about rewards paramount
Key strategies
Trust and Transparency
Key treatment
Talk about SM and strategies openly
strategies
Never betray trust
◦ e.g., never play video-recordings of child
without their permission Role plays
◦ Let child hear music in headphones during
Sliding In; no tricking
◦ Don’t listen outside door
◦ Knock on door before entering room
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 18
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Key treatment
strategies
The balance
of tone
Key strategies
The balance of tone
Key strategies
Key strategies
Video – demonstrating ‘balance of tone’ Working on goals in the moment
If you are confident that a Give firm, clear instruction of what to say/do
child can do a particular Give lots of time to respond
goal, “lend them your Click ◦ Don’t ‘fill the space’ or rush them to respond
confidence” and Repeat the question if necessary
empathically push them to
achieve that goal If the child communicates as expected, give labelled praise
(quietly if others around)
◦ “Great asking for your ice-cream using a sentence”
◦ Add points etc. to reward system
Key strategies
Working on goals – have a ‘Plan B’
Provide supportive prompting (“you can do it”)
“Plan B” – change a variable to make it easier
◦ Use the ‘Communication Changers’ to guide you
Clinic
◦ Add structure (reframe as a forced-choice question)
◦ Ask person to look away
◦ Give specific prompt of what to say
program
◦ Walk away to practice then go back
◦ Single word
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 19
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
~30 mins work on ‘Pathway to build talking’
Rough (‘Sliding In’ / generalising, etc.)
Working with the parent/child
within-session
structure for Working with family/parent is integral part of treatment
clinic sessions Review ‘Sliding In’ progress at school and make
Education about anxiety, feelings, and SM
recommendations
Community goals
◦ Coaching parent how to work on goals
◦ Role plays
Review community goals for child/parent to work on ◦ In vivo practice – reception, local shops, offices, post office, cafe
/ role play / in vivo practice ◦ Playdates
◦ Building social activities
Strategies to manage anxiety - Relaxation / breathing / meditation
Strategies for child/parent to address
anxiety/emotions
Address any ‘maintaining factors’
Education for child
Pressure from parents/others
Education about anxiety (e.g., ‘Cool kids’ manual)
Emotion regulation problems
Using the rating scale
Negative comments from relatives/others
Storybooks about emotions / SM
People enabling the mutism
Emotion regulation – e.g., Zones of regulation
Biology of anxiety
Starting out
Upskilling parents and outsourcing
Classroom
Behaviour management Educate all
goals/
staff
rewards
• Triple P - free online course - triplep-parenting.net.au
Emotion regulation School
• “Tuning in to kids/teens” - tuningintokids.org.au
Anxiety disorders
program
Generalising School
• Cool kids program (3-17 years), Macquarie University; Child/Teen + parent modules talking consults
• Brave Online (8-17 years), www.brave-online.com; Child/Teen + parent modules
Attachment Communi-
cation
• Circle of security group sessions
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 20
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Starting out
Starting out
Classroom seating
School program
Reduce child’s anxiety / stress
◦ Build familiarity Initially to maximise If no other good
◦ Structure/routine communication at friend, better to
desk have no-one
◦ Prepare the child for changes
◦ Devise ways for child to get needs met
Next most
◦ Build social comfort Friend they can
familiar
Later – part of communicate
◦ Place friends with them in class friend
generalising speech best with
◦ Ensure they are playing with friends in playground
to classmates
Child with SM
Starting out Starting out
Educate peers Educate all staff
Explain the child can talk but is scared
Understand
Request they don’t react if child talks
◦ SM is anxiety
Stop peers answering for the child (‘enabling’) ◦ … and not stubbornness
Stop negative comments or pressure from peers ◦ Communication will vary
Read book Engage the child
YouTube ◦ Chatting, humour, self-disclosure
◦ Without questions 45 min DVD / USB / online recording
to play at staff meeting
www.selectivemutism.com.au
Can you say that
Educate all staff Educate all staff
louder?
If the child communicates… If the child talks don’t… [Prompt too quickly
Allow them to communicate in whatever Don’t stop them from whispering for better speech]
or using devices
Wow, I didn’t
way they feel comfortable
think you’d talk
[Surprise] You talked!
[Comments
about speech]
I’m so happy you
talked that’s so “Hi”
exciting
Keep talking to them as usual
Keep your emotion low (‘poker face’)
[Excitement]
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 21
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Educate all staff Educate all staff “It’s great to see you today.
If the child talks don’t… That’s great talking to If the child is mute… I noticed you have a lunch
order. It looks yummy. I
me, here’s a sticker
[Praise loudly in front hope you enjoy it.”
Oh hi! of others in an [Chat and make them feel
Have you got your embarrassing way] comfortable]
homework?
[Asking more questions]
If you understand
“Hi” the child’s situation,
set appropriate goals
within their Stage of
Communication
Has the cat got
Educate all staff Educate all staff
your tongue?
If the child is mute don’t… [Comments Don’t request manners, greetings, or eye contact
about talking]
Are you going to I’m a bit deaf,
talk to me you’ll have to
tomorrow? speak up You’re not
[Pressure] [Tricking child] even trying
are you?
[Criticism]
Manners Greetings (hello,
Eye contact
When you say (please, thank you) goodbye, waving)
“please” you can
go out to play Difficult skills – leave until final stages – once responding using sentences with range of people
[Consequences]
If child wants to wave hi/bye let them, but don’t push it in the early stages
School consults
Teach specific SM strategies to teacher
• ‘Communication sessions’
School video consultations Main techniques
•
•
‘Sliding In’
Build direct talking
Monthly • Fast generalising of talking to teachers/peers
Review child’s progress • Specific goals to discuss with child
Classroom
◦ Communication sessions / ‘Sliding in’ • Using rating scale
communication • Communication changers, 5 stages
◦ Classroom goals
goals • Stepladders, Role play 1 on 1
Barriers to progress
• Balance of tone
Teach specific strategies • Labelling nonverbals
In person visits only if school progress • Phrasing instructions
Other skills • Rewards
lagging, or to implement fast generalisation • Role plays
• Voice volume
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 22
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
A. Prioritise Pre-communication
B. ‘Stage 2 communication’ – talking with
Pathway to build
talking at school
parent alone in classroom
C. Use ‘Sliding In’ to help child talk to
SCHOOL
teacher for first time
D. Build talking with teacher
STEP A
1 on 1 PRIORITISE PRE-
E. Generalise talking to other COMMUNICATION
teachers/staff/peers 1 on 1
F. Expand talking: Spontaneous talking, all
classes/situations, voice volume,
assertiveness, asking for help, larger groups
Ensure child can talk to parent alone
SCHOOL in classroom (Stage 2 communication)
STEP B Give parent/child regular access to the classroom
Provide regular access to room
ENSURE CHILD
Teacher NOT involved
CAN TALK TO
PARENT ALONE IN Enclosed room / NO interruptions
CLASSROOM Same room as for ‘Sliding In’
(STAGE 2
COMMUNICATION)
School ‘communication sessions’
3, 15-min sessions / week
Teacher, parent, child
SCHOOL Play video ‘Sliding In’ /
STEP C recording
of child’s
building
communica-
tion
voice
USE ‘SLIDING IN’
TO GENERALISE Discuss
TALKING FROM Role play / weekly
PARENT TO rehearsal goals /
CLASSROOM ratings Continue sessions until
◦ Some spontaneous talking
TEACHER
◦ Talked to teacher in classroom
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 23
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
SCHOOL
SCHOOL STEP E
STEP D FAST
BUILD CHILD’S GENERALISATION
TALKING WITH OF SPEECH TO
TEACHER 1 ON 1: OTHER
SAME STRATEGIES TEACHERS/STAFF/
AS WITH CLINICIAN PEERS 1 ON 1
Hardest to
talk to
Fast generalisation to Fast generalisation
Generalising talking to peers
adults
Some kids may require the second adult they build Child orders peers
talking with to have a quick ‘Sliding In’
Then use highly-structured task with range of staff Teacher/child work with one at a time
◦ ‘Interview’ questions (or similar) ◦ In withdrawal room
◦ Teacher to accompany child around school (or another adult ◦ Highly structured, verbal, low academic game
‘talking buddy’)
◦ e.g., Uno verbally
◦ Work quickly through all kids in class
◦ 2-3, 40-minute sessions
Easiest to
talk to
Generalising talking to peers – decision tree
Level A. Not interacting with
children in playground
• Structured activities in playground
• Playdates at home (‘Sliding In’ may be needed)
SCHOOL
Level B. Plays with but doesn’t • Playdates at home
STEP F
talk to any children at school • ‘Sliding In’ best friend at school Expanding talking:
Level C. Talks to one or more Build voice
friends in playground but not in
• Seat next to friends only, away from others
• Teacher give ‘permission’ to talk to friends at desk (set goal)
volume,
classroom assertiveness,
Level D. Talks to 1-2 friends in • ‘Uno game’ with all peers in class
asking for help,
class but not groups/whole-class • Manipulate table seating and small groups talking in groups,
talking in specialist
Level E. Has spoken to all kids in
• Games at desk with friend + 2 others classes
• Literacy groups - build structured talking activities, incl. good friend
class but not whole-class • Easy talking goals in whole-class; Stepladder – speeches
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 24
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Generalising talking
Building talking in groups in the classroom Working on Stage 5
communication at school
Assertiveness
◦ Asking for help, saying ‘no’, don’t have the worksheet
Initiating speech
◦ Give a topic with a box - says 4 things about the topic
Send on verbal errands
Following on Classroom: Change to Manipulate Box of items in office for child to request items from
from Uno Uno game in easy, highly- usual class Specialist teachers ask ‘question of the day’
game with group of 5-6 structured small groups ◦ Tell child the question/answer beforehand
peers 1 on 1 academic • Add structure ◦ Teacher to ask question 1 on 1 at child's desk whilst other
• Swap out 1 children busy
in separate child at a time
game to every task
◦ Then easy academic forced-choice question
room • Swap out 1
• Choose kids
◦ Then open-ended question
carefully
child at a time
Stepladder – Class speech
Step Goal Stage
10 Do talk live with teacher and whole class in the classroom 5
9 Do talk live with teacher and 10 friends in office 5
8 Do talk live with teacher and six friends in office 5
7 Do talk live with teacher and two friends in office 5
6 Do talk live with teacher in office 5
5 Share video / ornament in classroom with whole class 4
4 Share video / ornament with 10 friends in the office 4
3 Share video / ornament with 6 friends of your choice 4
‘Class speech’ stepladder – the final frontier 2 Share video / ornament with 3 friends of your choice 4
C ONSIDE R WHAT “COMMUNIC ATION C HANG E RS” ARE BE ING MANI PULATE D 1 Share video / ornament with teacher in the office 4
Generalising speech to
new year/teacher SM
Start strategies - beginning Term 3
Devote time to selecting appropriate teacher
Storybooks
Generalise current communication to all staff who may take the
year
Understanding Katie
Education for new teacher about SM
Generalise communication to new teacher before class starts –
end Term 4
Place with 2 friends they communicate best with
Normal to regress with new teacher but should regain in a few
weeks
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 25
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Selective Mutism Clinic Webinars
Websites
Webinars available in 3 formats: www.selectivemutism.org
1) Live webinar www.selectivemutism.com.au (Selective Mutism Clinic, Sydney)
2) USB package
www.kurtzpsychology.com/selective-mutism/sm-learning-university/
3) Online recording
www.selectivemutism.com.au/seminars https://childmind.org/guide/parents-guide-how-to-help-a-child-with-selective-mutism/
Selective Mutism Clinic, Sydney
Selective Mutism Australia
SMIRA
Selective Mutism Anxiety & Related Disorders Treatment Center – Smart Center
Parents of Children with Selective Mutism
Resources for teachers/parents References
Cunningham (2001). COPEing with selective mutism. A collaborative school-based approach.
Beidel et al. (2014). The impact of skills training for social anxiety disorder: A randomized controlled
Goetze Kervatt (1999). The Silence Within: A teacher-parent guide to helping selectively mute and shy children. trial. J Anxiety Disord, 28(8), 908-918.
Selective mutism anxiety research and treatment center.
Bergman R. (2012). Treatment for children with Selective Mutism: An integrative behavioral
Goetze Kervatt (2004). Supplement treatment guide to “the silence within”. approach. Programs that work. New York: Oxford University Press.
Gottman (1998). Raising an emotionally intelligent child. Bergman et al. (2013). Integrated behavior therapy for selective mutism: A randomized controlled
pilot study. Behaviour Research & Therapy, 51(10), 680-689.
Johnson & Wintgens (2016). Selective mutism resource manual.
Bunnell et al. (2018). A two-session hierarchy for shaping successive approximations of speech in
Kearney (2010). Helping children with selective mutism and their parents: A guide for school-based professionals. selective mutism: Pilot study of mobile apps and mechanisms of behavior change. Behavior Therapy,
49, 966-980.
Kotrba & Saffer (2018). Overcoming selective mutism: A parent’s field guide.
Carpenter et al. (2014). Extending parent-child interaction therapy for early childhood internalizing
McHolm (2004). COPEing with selective mutism. A companion manual of forms and resources. problems: New advances for an overlooked population. Clin Child Fam Psychol Rev, 17, 340-356.
McHolm, Cunningham, & Vanier (2005). Helping your child with selective mutism. Chorpita (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised
child anxiety and depression scale. Behaviour research and therapy, 38, 835-855.
Shipon-Blum (2003a). Easing school jitters for the selectively mute child (2nd ed.).
Cleator & Hand (2001). How a successful speech and language assessment really is possible. Int Jn of
Shipon-Blum (2003b). The ideal classroom setting for the selectively mute child: A guide for parents, teachers, and Language & Communication Disorders, 36(s1), 126-131.
other health professionals.
References cont. References cont.
Kristensen (2000). Selective mutism and comorbidity with developmental disorder/delay, Gensthaler et al. (2018). Evaluation of a novel parent-rated scale for Selective Mutism.
anxiety disorder, and elimination disorder. J. Am. Acad. Child Adolesc. Psychiatry, 39(2), 249-256. Assessment, 27, 1007-1015.
Kristensen & Torgersen (2001). MCMI-II personality traits and symptom traits in parents of Oerbeck et al. (2014). A randomized controlled trial of a home and school-based intervention for
children with selective mutism: A case-control study. Journal of Abnormal Psychology, 110, 648- selective mutism – defocused communication and behavioural techniques. Child & Adolescent
652. Mental Health, 19, 192-198.
Dr Steven Kurtz (U.S.A.); Video training for parents/clinicians – Rhode et al. (1993). The tough kid book: Practical classroom management strategies. Longmont,
www.kurtzpsychology.com/selective-mutism/sm-learning-university/ CO: Sopris West.
Lyneham et al. (2003). The Cool kids program – Children’s workbook. MUARU: Macquarie Steffenburg et al. (2018). Children with autism spectrum disorders and selective mutism.
University, Sydney. Neuropsychiatric Disease and Treatment, 14, 1163-1169.
Manassis et al. (2016). The use of medication in selective mutism: A systematic review. Eur Child Theodore & Kovac (2012). Augmented self-modeling as an intervention for selective mutism.
Adolescent Psychiatry, 25, 571-578. Psychology in the Schools, 49, 93-103.
Mulligan & Shipon-Blum (2015). Selective Mutism: Identification of subtypes and implications Viana et al., (2009). Selective mutism: A review and integration of the past 15 years. Clinical
for treatment. Jn of Education & Human Development, 4, 79-96. Psychology Review, 29, 57-67.
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 26
www.selectivemutism.com.au; admin@selectivemutism.com.au
Selective Mutism Treatment for Speech Pathologists 14/11/2022
Questions
© Dr Elizabeth Woodcock, Clinical Psychologist / Director
Selective Mutism Clinic, Sydney 27
www.selectivemutism.com.au; admin@selectivemutism.com.au
You might also like
- Perceived Strengths and Difficulties in Emotional Awareness andDocument13 pagesPerceived Strengths and Difficulties in Emotional Awareness andMargarida DiasNo ratings yet
- Late, Lost, and Unprepared: A Parents' Guide To Helping Children With Executive Functioning - Teen & Young AdultDocument5 pagesLate, Lost, and Unprepared: A Parents' Guide To Helping Children With Executive Functioning - Teen & Young Adultsiganemi0% (1)
- Selective Mutism Communication Anxiety Treatment ChildrenDocument19 pagesSelective Mutism Communication Anxiety Treatment ChildrenJelnathleeNo ratings yet
- Victims of CrimeDocument11 pagesVictims of Crimesuela35No ratings yet
- Hangxiety InfographicDocument1 pageHangxiety Infographicapi-548552942No ratings yet
- Making Eye Contact A Multidisciplinary Approach To The Management of AutismDocument1 pageMaking Eye Contact A Multidisciplinary Approach To The Management of AutismMohammad Abubakar SiddiqNo ratings yet
- Social-Emtional Skills To Adolescents With ASDDocument23 pagesSocial-Emtional Skills To Adolescents With ASDThảo NguyễnNo ratings yet
- Autism Spectrum Disorder ASDDocument10 pagesAutism Spectrum Disorder ASDM BORQUEZ QUINTASNo ratings yet
- Early Intervention For Children With Autism Spectrum DisordersDocument14 pagesEarly Intervention For Children With Autism Spectrum DisordersCarlos Charlotte SalvadorNo ratings yet
- Article InfoDocument10 pagesArticle InfoFélix IGNo ratings yet
- Psychosocial Interventions For Dementia: From Evidence To PracticeDocument11 pagesPsychosocial Interventions For Dementia: From Evidence To Practiceariadna17No ratings yet
- The Wall Sensory Integration AssessmentDocument21 pagesThe Wall Sensory Integration AssessmentSelinah Sslengs Seepe100% (1)
- Practical Guidelines For The Assessment and Treatment of Selective MutismDocument11 pagesPractical Guidelines For The Assessment and Treatment of Selective Mutismsylvia_plath27No ratings yet
- Sperger S Yndrome: ¿What Is It?Document2 pagesSperger S Yndrome: ¿What Is It?GINA NAYIBTH LEON VIDALNo ratings yet
- Autism Evaluation Online WorkshopDocument29 pagesAutism Evaluation Online WorkshopQurrat ulainNo ratings yet
- Whitbourne7e IM Ch11Document10 pagesWhitbourne7e IM Ch11Antônio Malvar Martins NetoNo ratings yet
- JPsychother Integ 2014 PerepletchikovaDocument16 pagesJPsychother Integ 2014 PerepletchikovaMaría Andrea Cárdenas PérezNo ratings yet
- Cognitive Clusters in SpecificDocument11 pagesCognitive Clusters in SpecificKarel GuevaraNo ratings yet
- Chicago DBTDocument87 pagesChicago DBTdhani meadowsNo ratings yet
- QR Management of Bipolar Disorder in AdultsDocument8 pagesQR Management of Bipolar Disorder in AdultsShre RanjithamNo ratings yet
- Actionresearch Oct28part2Document26 pagesActionresearch Oct28part2emaryltan0323No ratings yet
- An Update On Psychopharmacological TreatDocument15 pagesAn Update On Psychopharmacological Treatzakayahz3103No ratings yet
- 1 s2.0 S1878747923001654 MainDocument15 pages1 s2.0 S1878747923001654 MainJessie BrionesNo ratings yet
- Introduction To The Diagnostic Manual For Infancy and Early Childhood (DMIC)Document52 pagesIntroduction To The Diagnostic Manual For Infancy and Early Childhood (DMIC)circlestretchNo ratings yet
- Sauve et al. 2020Document14 pagesSauve et al. 2020Ayushi JainNo ratings yet
- Di Maio Week 5 Ebp EssayDocument9 pagesDi Maio Week 5 Ebp Essayapi-741546461No ratings yet
- Course Plan On Psychiatric NSGDocument10 pagesCourse Plan On Psychiatric NSGannu panchal100% (1)
- Psychopathologyslideshare 150721015626 Lva1 App6891Document62 pagesPsychopathologyslideshare 150721015626 Lva1 App6891Arun ChoudharyNo ratings yet
- Improving Overall Function Primary Component of Treatment Pecial Education Personnel or Trained TherapistsDocument4 pagesImproving Overall Function Primary Component of Treatment Pecial Education Personnel or Trained TherapistsSangitha ManiamNo ratings yet
- ADHDDocument21 pagesADHDsakthithirumaraiNo ratings yet
- Right Hemisphere DamageDocument80 pagesRight Hemisphere DamageSweekriti Narayanan100% (2)
- Mount, Marva - Management Ideas For Selective MutismDocument10 pagesMount, Marva - Management Ideas For Selective MutismMaja KobašNo ratings yet
- DSM 5 Neurodevelopmental NOTESDocument27 pagesDSM 5 Neurodevelopmental NOTESmicrobeateria100% (2)
- NDT 9 087Document6 pagesNDT 9 087Gita TikihaiNo ratings yet
- Datgn 20Document14 pagesDatgn 20Sâmara BeckerNo ratings yet
- AutismDocument21 pagesAutismcamelle sisonNo ratings yet
- Framework For ASD Therapy 24.03.18Document6 pagesFramework For ASD Therapy 24.03.18shivanjaniworkNo ratings yet
- Sensory Integration Therapies For Children With Developmental and Behavioral DisordersDocument6 pagesSensory Integration Therapies For Children With Developmental and Behavioral DisordersKevin RadittyaNo ratings yet
- Neurodevelopmental Disorders2023Document62 pagesNeurodevelopmental Disorders2023Chriziel SanchezNo ratings yet
- Weyant Makayla 2022 Autism PosterDocument1 pageWeyant Makayla 2022 Autism Posterapi-578364337No ratings yet
- Orofacial Myofunctional Therapy With Children Ages 0-4Document16 pagesOrofacial Myofunctional Therapy With Children Ages 0-4manu nopeNo ratings yet
- Questionario Sensorial AutismoDocument11 pagesQuestionario Sensorial AutismoLenice GóesNo ratings yet
- SENSORY INTEGRATION For ASDDocument35 pagesSENSORY INTEGRATION For ASDcitra city100% (1)
- Impact of Social Communication Interventions On Infants and Toddlers With or At-Risk For Autism: A Systematic ReviewDocument11 pagesImpact of Social Communication Interventions On Infants and Toddlers With or At-Risk For Autism: A Systematic ReviewpaulyfonoNo ratings yet
- Full Download Understanding Psychology 12th Edition Feldman Solutions ManualDocument35 pagesFull Download Understanding Psychology 12th Edition Feldman Solutions Manualowen7qjim100% (30)
- Alternativas Farmacologicas en AutismoDocument16 pagesAlternativas Farmacologicas en AutismoDerek TantaleánNo ratings yet
- Leiman-2 Dialogical Sequence Analysis in StudyingDocument27 pagesLeiman-2 Dialogical Sequence Analysis in StudyingPriscila OsórioNo ratings yet
- La Intervención en Los Trastornos Dislexicos - Entrenamiento FonológicoDocument7 pagesLa Intervención en Los Trastornos Dislexicos - Entrenamiento FonológicoLesly AgamaNo ratings yet
- Guide For Child Therapy: John McmohanDocument6 pagesGuide For Child Therapy: John McmohanJohn McmohanNo ratings yet
- NDT 331987 Language and Speech Characteristics in AutismDocument11 pagesNDT 331987 Language and Speech Characteristics in AutismAlejandro Cano VillagrasaNo ratings yet
- Actionresearch Oct28part2Document26 pagesActionresearch Oct28part2xray12345No ratings yet
- 2017 Metacognitive StrategiesDocument15 pages2017 Metacognitive StrategiesXimena LainfiestaNo ratings yet
- PsychotherapyDocument23 pagesPsychotherapymariaNo ratings yet
- Actionresearch Oct28part2Document26 pagesActionresearch Oct28part2Dilinesaw BogaleNo ratings yet
- Principles of Clinical Practice For Assessment and InterventionDocument28 pagesPrinciples of Clinical Practice For Assessment and InterventionFam TuongNo ratings yet
- Nrneurol 2015 229Document12 pagesNrneurol 2015 229Renan RRSNo ratings yet
- Clinical Assessment of Social CognitiveDocument12 pagesClinical Assessment of Social CognitivePaulina Negrón DíazNo ratings yet
- (Mora & McAndrew, 2003) - Common-Sense Model of Self-Regulation.Document8 pages(Mora & McAndrew, 2003) - Common-Sense Model of Self-Regulation.CMSNo ratings yet
- Copiii Si Adolescenti + Adulti Cu TSA: Characteristics of DisorderDocument2 pagesCopiii Si Adolescenti + Adulti Cu TSA: Characteristics of DisorderCristian MeleiNo ratings yet
- Div Class Title Auditory Hallucinations in Schizophrenia Helping Patients To Develop Effective Coping Strategies DivDocument6 pagesDiv Class Title Auditory Hallucinations in Schizophrenia Helping Patients To Develop Effective Coping Strategies DivHilda Nurul FatimahNo ratings yet
- Articulo 5 EVALUACIÓN PSICOPATOLÓGICA DEL LENGUAJE EN LA ESQUIZOFRENIA-1Document1 pageArticulo 5 EVALUACIÓN PSICOPATOLÓGICA DEL LENGUAJE EN LA ESQUIZOFRENIA-1Teddy JuniorNo ratings yet
- PROMPT An Overview MSHA Presentation 2018Document85 pagesPROMPT An Overview MSHA Presentation 2018Lays Mandy100% (1)
- Therapeutic Education Direction & Intervention (TEDI): Volume 2: Activity Kits for Special Needs Children: Communication and Gross MotorFrom EverandTherapeutic Education Direction & Intervention (TEDI): Volume 2: Activity Kits for Special Needs Children: Communication and Gross MotorNo ratings yet
- NCP AnxietyDocument3 pagesNCP AnxietyLord James De GuzmanNo ratings yet
- Project On GothicDocument14 pagesProject On GothicMazana ÁngelNo ratings yet
- TEXTO ORIGINAL - What Is ADHD - 4 PagesDocument4 pagesTEXTO ORIGINAL - What Is ADHD - 4 PagesGrace ValenciaNo ratings yet
- 1 Page DSM - Psychotic PDFDocument1 page1 Page DSM - Psychotic PDFRobert FordNo ratings yet
- Apa Research Paper On Eating DisordersDocument7 pagesApa Research Paper On Eating Disordersuifjzvrif100% (1)
- School Refusal Assessment ScaleDocument6 pagesSchool Refusal Assessment Scaleamrut muzumdarNo ratings yet
- Cannabis Dependence RehmDocument18 pagesCannabis Dependence RehmAntonio Tejero PocielloNo ratings yet
- Mse 2Document3 pagesMse 2Charisma PastorNo ratings yet
- 6001.alcohol Induced DementiaDocument4 pages6001.alcohol Induced Dementiajuan_bacha_1No ratings yet
- AdhdDocument2 pagesAdhdAlexander SaladinNo ratings yet
- Pych Preboards QuestionsDocument18 pagesPych Preboards QuestionsPaul Lexus Gomez LorenzoNo ratings yet
- LatahDocument2 pagesLatahKhoirunnisa RahmawatiNo ratings yet
- Psychology PaperDocument5 pagesPsychology PaperBwallace12No ratings yet
- PsyHx and MSEDocument25 pagesPsyHx and MSERazel AnneNo ratings yet
- (Psychiatry) Mental Health Proj Proposal LEC 12 PDFDocument7 pages(Psychiatry) Mental Health Proj Proposal LEC 12 PDFXianne GonzalesNo ratings yet
- IMPULSE-CONTROL DISORDERS-Dr. Mabunga 2Document25 pagesIMPULSE-CONTROL DISORDERS-Dr. Mabunga 2Vasu PatelNo ratings yet
- APPENDIXDocument3 pagesAPPENDIXRon AracoNo ratings yet
- (Download PDF) Antidepressants From Biogenic Amines To New Mechanisms of Action Matthew Macaluso Online Ebook All Chapter PDFDocument42 pages(Download PDF) Antidepressants From Biogenic Amines To New Mechanisms of Action Matthew Macaluso Online Ebook All Chapter PDFsandra.estrada213100% (9)
- Paranoid SchizophreniaDocument12 pagesParanoid Schizophreniakiran mahalNo ratings yet
- The Facts On Tweens and Teens and Dating ViolenceDocument2 pagesThe Facts On Tweens and Teens and Dating ViolenceFilipaTorresCostaNo ratings yet
- Student Example Borderline Personality DisorderDocument12 pagesStudent Example Borderline Personality Disorderapi-284737097No ratings yet
- Female Orgasmic DisorderDocument5 pagesFemale Orgasmic DisorderYamini JohriNo ratings yet
- Maine Northeast Conference On Fetal Alcohol Spectrum DisordersDocument1 pageMaine Northeast Conference On Fetal Alcohol Spectrum DisordersfasdunitedNo ratings yet
- What To Expect From Your ADHD AssessmentDocument1 pageWhat To Expect From Your ADHD AssessmentsamNo ratings yet
- SCHIZOPHRENIA CaseDocument8 pagesSCHIZOPHRENIA Casekrishna BabuNo ratings yet
- Complex Post-Traumatic Stress Disorder. Implications For Individuals With ASDDocument13 pagesComplex Post-Traumatic Stress Disorder. Implications For Individuals With ASDpaul.cotarelo2012No ratings yet
- Jaime Castillo What Happened To Make You Anxious How To Uncover The Little T Traumas That DriveDocument162 pagesJaime Castillo What Happened To Make You Anxious How To Uncover The Little T Traumas That DrivePablo Bando100% (1)